Abstract
Background
Little is known about characteristic profiles of substance use – and their individual- and neighborhood-level correlates – among high-risk youth.
Objectives
To identify characteristic substance misuse profiles among youth entering an urban emergency department (ED) and explore how those profiles relate to individual- and community-level factors.
Methods
Individual-level measures came from screening surveys administered to youth aged 14–24 at an ED in Flint, Michigan (n = 878); alcohol outlet and crime data came from public sources. Binary misuse indicators were generated by using previously established cut-points on scores of alcohol and drug use severity. Latent class analysis (LCA) identified classes of substance use; univariate tests and multinomial models identified correlates of class membership.
Results
Excluding non-misusers (51.5%), LCA identified three classes: marijuana-only (27.9%), alcohol/marijuana (16.1%), and multiple substances (polysubstance) (4.6%). Moving from non-misusers to polysubstance misusers, there was an increasing trend in rates of: unprotected sex, motor vehicle crash, serious violence, weapon aggression, and victimization (all p < .001). Controlling for individual-level variables, polysubstance misusers lived near more on-premises alcohol outlets than non-misusers (RRR = 1.42, p = .01) and marijuana-only misusers (RRR = 1.31, p = .03). Alcohol/marijuana misusers were more likely to live near high violent crime density areas than non-misusers (RRR = 1.83, p = .01), and were also more likely than marijuana-only misusers to live in areas of high drug crime density (RRR = 1.98, p = .03). No other relationships were significant.
Conclusion
Substance-misusing youth seeking ED care have higher risk for other problem behaviors and neighborhood-level features display potential for distinguishing between use classes. Additional research to elucidate at-risk sub-populations/locales has potential to improve interventions for substance misuse by incorporating geographic information.
Keywords: Polysubstance use, neighborhood, violence, problem behaviors
Introduction
Previous studies indicate that substance users often report polysubstance use (1–4) – the co-occurring use of multiple substances. Polysubstance use in youth is a forerunner of substance use problems later in life (1) and polysubstance users are more susceptible to associated negative outcomes, such as major depression (5), than other substance users. A common approach to jointly studying use of multiple substances is to identify homogeneous classes of substance use using latent class analysis (LCA) (5–12). Restricting focus to drugs other than tobacco, several researchers have independently identified subsets of the substance-using population composed of: drinkers (6,9,10,12), marijuana users (5–7,12), alcohol and marijuana users (9,10,12), and polysubstance users (5,6,8–10) which includes nonmedical prescription drug use and illicit drug use beyond marijuana. These studies have characterized the level of heterogeneity in substance use profiles in various populations and individual-level correlates of particular substance use profiles, but none have focused primarily on high-risk youth, on behavioral comorbidities, or on community-level risk factors.
Substance misuse and associated problem behaviors
Researchers hypothesize that substance misuse arises among a cluster of problem behaviors that first appears during adolescence (13,14). These problem behaviors include violence (15–17), sexual risk behaviors (7,8,18–20), and high-risk driving habits (21–23). These behaviors’ similar roles in signifying rebellion or indicating common psychological distresses may explain their frequent co-occurrence (24), and also suggest that targeting multiple problem behaviors with a single intervention is sensible. Indeed, previous researchers have successfully intervened on multiple problem behaviors simultaneously (25,26) and have observed intervention effects on behaviors not explicitly intervened upon (27). This indicates that understanding substance misuse dynamics represents an opening to reduce rates of its associated behavioral comorbidities.
Community-level characteristics and substance misuse
Understanding spatially indexed correlates of health outcomes to inform decision-making/intervention strategies has been recognized as an important emerging field in public health (28), and ecological theories suggest this thinking is applicable to substance use behavior. In particular, social disorganization theory suggests that socially disorganized communities lack resources required to regulate the behavior of its residents, resulting in higher rates of delinquency (29), including substance use (30). A complimentary theory indicates that stress incurred by residence in certain types of neighborhoods may translate into increased substance use rates (31). Researchers have examined neighborhood-level effects on substance use outcomes (for a review, see (31)), with mixed results, possibly because researchers have often focused on a single substance. Analyzing how neighborhood features are associated with an individual's substance use profile may be more rigorous approach that, heretofore, has not been explored.
While it is difficult to fully characterize community context purely from data – which suggests a second possible explanation for inconsistent findings – examining the effects of key community-level measurements is an important first step in understanding whether neighborhood features are related to particular substance use profiles. Specifically, a wide breadth of violence research has focused on alcohol outlets, both because of the association between alcohol outlet concentration and indicators of social disorganization, such as violence (32–37), and because of their status as potentially modifiable aspects of the built environment. Given the link between substance use and violence (15–17), a link between more deleterious substance use profiles and higher outlet density appears plausible. In a parallel manner, due to the relationship between social disorganization and delinquency, links between area-level crime rates and propensity for substance use have been hypothesized (31). Identification of community-level correlates of substance use profiles is a key aim – and innovation – of this study.
Study overview
This study uses data from a screening survey administered to individuals aged 14–24 presenting to the emergency department (ED) at a Level-1 trauma center in Flint, Michigan, to study heterogeneity in substance misuse profiles in this population, and how the resulting profiles map onto other individual-level problem behaviors (violence involvement, sexual risk behaviors, high-risk driving behavior). Given that individuals in resource poor areas often use the ED for primary care services (38,39), and that youth entering an urban ED are at increased risk for substance use and its behavioral comorbidities (15,20), this sample represents a broad subset of a high-risk population. In addition, successful substance use interventions in the ED (26,40,41) indicate this is a highly intervenable population. Using the individuals’ home address, individual data was merged with community-level data from public sources to investigate whether alcohol outlet and crime locations are associated with particular substance misuse profiles in this population, after controlling for individual-level characteristics. Specifically, this study aims to address previously discussed gaps in the literature by identifying: (a) the characteristic substance misuse profiles present among at-risk youth and young adults in an urban setting; (b) how substance misuse profiles map onto other problem behaviors; (c) whether alcohol outlet and/or crime concentration are associated with particular substance misuse profiles. The hypotheses behind this work are that increased alcohol outlet density and crime rates will correspond to more deleterious substance misuse profiles, and that those profiles will correspond to greater propensity for other problem behaviors.
Methods
Study design and site
The current study presents cross-sectional screening data collected as part of the Flint Youth Injury study, a two-year longitudinal study examining substance use, violent injury, and criminal justice outcomes among a cohort of assault-injured drug using youth (age 14–24), and a comparison cohort of drug-using non-assaulted youth seeking ED care. The study was conducted at Hurley Medical Center, a Level-1 trauma center in Flint, Michigan. All individual-level measurements were taken from the screening survey administered for entry into the study. All protocols were sanctioned by the Institutional Review Boards at the University of Michigan. An NIH certificate of confidentiality was obtained.
Participant screening occurred 12/2009 to 9/2011, 24 hours/day Thursday–Monday, excluding 2am–5am on Tuesdays/Wednesdays. The exclusion period was required due to resource constraints for staffing and Tuesday/Wednesday from 2am–5am represents the lowest volume days and times. Research assistants identified candidates through electronic patient logs and approached candidates in waiting or treatment areas. Study staff approached all assault-injured patients, defined as those intentionally injured by another person. For each assault-injured patient screened, the next age group- (age 14–17, 18–20, 21–24) and gender-balanced non-assault-injured counterpart was approached. Staff did not approach those presenting for child abuse, sexual assault, or those who were currently incarcerated. Those with any conditions precluding consent (e.g., insufficient cognitive function; schizophrenia), as determined by research assistants, were not screened. Patients granting consent self-administered a computer-based survey; their answers were not visible to friends, family, or medical/research staff at the time of assessment. Each participant received a $1.00 gift. All participants provided consent; in the case of minors we obtained both parental consent and youth assent.
Individual-level data
Demographic variables – age, gender, race, education, living situation, government assistance – were measured using validated instruments (42,43). Race was reduced to an indicator of African-American because its distribution was primarily concentrated on two values (91.0% of all individuals screened report African American or Caucasian/other as their race). The government assistance variable was an indicator of whether the participant (or, for minors, their parents) received government assistance. Home addresses were obtained from each participant, which was used for subsequent linkage with community-level variables. The geocoding success rate for the home addresses was 100%.
Past 6-month substance use was ascertained with the Alcohol Use Disorders Identification Test consumption questions (AUDIT-C) (44) for alcohol and the Smoking and Substance Involvement Screening Test (ASSIST) (45) for all other substances. The AUDIT-C was modified from its original timeline of 12 months to coincide with the follow-up period of the subsequent longitudinal study (6 months). Given the noted robustness of the AUDIT to minor changes in the questions (46), we do not believe this modification affects validity of the scale. The AUDIT-C consisted of three questions and the ASSIST – which was administered for nine separate substances (marijuana, cocaine/crack, methamphetamine, hallucinogens, street opioids, inhalants, prescription stimulants, opioids, and sedatives) – consisted of six questions. These questions were converted to summary scores using standard scoring methods (44,47). Based on NIDA-recommended cut-points, misuse of a particular substance was defined as an ASSIST sum ≥ 4 (47). Alcohol misuse was defined as an AUDIT-C sum ≥ 3 for minors and ≥ 4 for adults, as justified previously (48). Because very few people reported methamphetamine (2 people) or inhalant (1 person) misuse, those substances were excluded from the analysis.
Questions from the National Longitudinal Study of Adolescent Health (42) were used to assess other past 6-month problem behavioral outcomes. Motor vehicle crashes, self-described serious violence involvement, weapon (gun/knife) victimization, or weapon aggression were reduced to a binary indicator of whether the individual had any instances of the given behavior over the previous 6 months. Unprotected sex was coded “Yes” if the individual reported sexual encounters with acquaintances and used condoms “rarely” or “never”.
Community-level data
Alcohol outlet data (address, license type) was obtained from the Michigan Liquor Control Commission in April 2012. All addresses were successfully geocoded. Alcohol outlet concentration was quantified by the number of alcohol outlets within ¼ mile (Euclidean distance) of the home address. This buffer was chosen to reflect proximity in the sense of easily walkable, indicating likely familiarity with the area. Using license types, we distinguished between outlets that do (“on-premises”) and do not (“package”) serve alcohol on-premises. Perfect alignment with the study period was impossible, due to the non-availability of retrospective licensing records. However, given little qualitative change in the spatial distribution of alcohol outlets between 4/2012 and 3/2016, this slight misalignment is unlikely to have substantive importance.
Crime data for 12/2009 to 9/2011, including the location of the nearest street corner for every police-involved incident and the nature of the crime, was obtained from the Flint Police Department, and geo-coded with a success rate of >99%. Using NIBRS categorizations (49), violent (assault, homicide, robbery, sex offenses–forcible) and drug crimes were isolated. Violent and drug crime concentration at an individual's home address was quantified by calculating a Gaussian kernel density estimate of the crime density (as in (37)), and evaluating the density at the home location. Density measurements were reduced to the indicator that the given density was in the top decile of the city, which other researchers have previously used to indicate high crime concentration (33). Because these data were only available within the Flint city limits, only residents of Flint were included in the analysis.
Statistical analysis
LCA (50) was used to identify heterogeneity in the joint distribution of the substance misuse indicators analyzed here. For a given number of input classes, the model returns the misuse probabilities for each latent class and posterior probabilities of class membership for each individual. Following previous work (51), the Bayesian information criterion (BIC) was used to select the number of classes. Prior to LCA, individuals (n = 452) reporting no misuse on all substances were removed. There were two reasons for this: (i) individuals reporting no substance misuse represent a clinically meaningful reference group; and (ii) this choice made the resulting groups more cleanly separated, indicating more reliable inference about the subsequent between-group comparisons. To ensure a parsimonious model, a maximum of five latent classes were considered. All models were fit using the flexmix package in R (52,53).
Substance use classes were compared both descriptively and using multinomial regression. For both analyses, individuals reporting any substance misuse were assigned to groups based on their maximum posterior probability. Univariate tests were based on the non-parametric permutation-based framework implemented in R (54). In accordance with the previously stated hypotheses, substance use classes were viewed as ordinal with regard to other behavioral outcomes and community-level variables (i.e., we hypothesize an increasing trend), and nominal with regard to demographics. Multinomial logistic regression was used to examine the joint effects of individual-level demographics and community-level variables in predicting class membership. Due to non-availability of software for fitting multinomial models with random effects, within-neighborhood clustering was not modeled. Sensitivity analyses with ordinary logistic models comparing two substance use classes showed small block-group-level random effect variances and extremely similar fixed effects in all cases that reliably converged. Non-convergent scenarios were likely due to relatively small samples (e.g., marijuana-only/polysubstance) for estimating mixed effects logistic models. Demographics (race, gender, age, government assistance), reason for ED visit, indicators of each other problem behavior, and each crime and alcohol outlet variable were controlled for in all models. In accordance with the hypothesis that members of more deleterious substance use classes will have higher rates of other problem behaviors, and will live in neighborhoods with more crimes/alcohol outlets, the corresponding hypothesis tests will be upper-tailed. The R package nnet was used to fit these models (55).
Results
Of the 849 assault-injured patients approached, 718 consented; of the 846 non-assault-injured patients approached, 730 consented, for a total of 1448 individuals screened. A complete description of participation rates and reasons for non-participation is published elsewhere (56). By restricting to the 878 individuals residing within the Flint city limits, those presenting to the ED for violent injury (55.5% of the 878) were oversampled, but no significant differences were seen in the substance misuse rates for any of the ten substances. The 878 participants included were 50.7% female, 71.6% African American, and had an average age of 19.7 (SD = 2.6); 74.7% were on public assistance (or, for minors, their parents). Among the 134 block groups in Flint, 126(94.0%) are represented in these data by at least one member of the analytic sample. Among those 126 block groups, the average (SD) number of participants living there is 6.97 (4.73), and the median (Q1,Q3) is 6(4, 10). A total of 178 alcohol outlets were within ¼ mile of at least one home address (113 package outlets, 14 on-premises outlets, and 51 were both). There were 628 drug crimes and 10,271 violent crimes in our database.
Latent class analysis
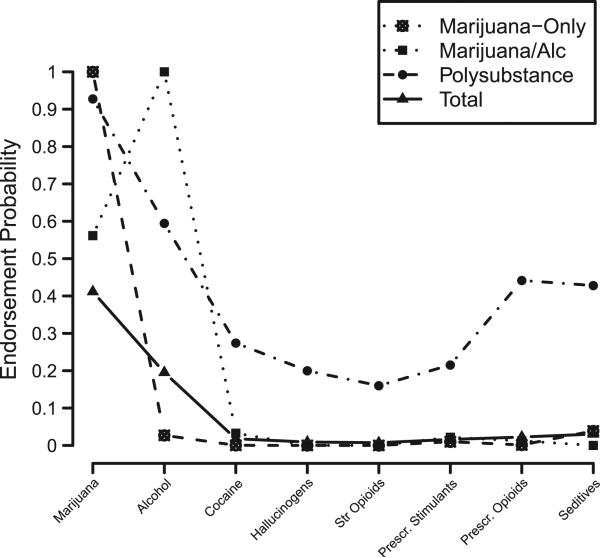
Among the 48.5% (n = 426) of the sample that reported past 6-month misuse of at least one substance, BIC favored a three-class solution (BIC1 = 1830:147; BIC2 = 1739:76; BIC3 = 1683:66; BIC4 = 1737.91; BIC5 = 1787:46). Model-estimated substance misuse probabilities within each latent class are shown in Figure 1. Restricting only to the n = 426 used for LCA, the model yields a relative entropy of 0.86, indicating good separation (57); if the no-misuse group is included and assumed known with certainty, this value increases to 0.94.
Figure 1.
Model estimated misuse rates for each substance within each class of substance misusers. The no-substance-misuse class was omitted. The “Total Sample” line does include the 51.5% of the sample that reported no substance misuse.
One class (marijuana-only), comprising 27.9% (n = 245) of the sample, included individuals with universal endorsement of marijuana misuse but very low misuse rates for all other substances. A second class (alcohol/marijuana), containing 16.1% (n = 141) of the sample, included alcohol misusers (100.0%) with a substantial chance of marijuana misuse (59.5%), but miniscule rates for other substances. The final class (polysubstance), containing the remaining 4.6% (n = 40), included individuals with elevated misuse probabilities for all substances, including a 92.5% rate of marijuana misuse, 60.0% alcohol misuse rate, and misuse rates ranging from 20.0% to 57.5% for the remaining six substances.
Characteristics of latent classes
Table 1 displays comparisons between the four groups on substance use, individual demographics, other behavioral outcomes, and alcohol outlets and crime. Groups differed by age, male, race, and reason for ED entry (all p < .001). Members of the no-misuse group were less likely to be male (non-misusers: 39.4%, all others: 59.7%), and less likely to have been screened due to a violent injury (non-misusers: 48.9%, all others: 62.3%). The alcohol/marijuana using class and the polysubstance class were older, and less likely to be African American than their counterparts. There was an increasing trend in the endorsement rates of all five problem behaviors tested (all p < .001); for example, 10.0% of non-misusers, 18.0% of marijuana-only misusers, 19.1% of alcohol/marijuana misusers, and 35.0% of polysubstance misusers reported sex with an acquaintance, using condoms “Rarely” or “Never”. In addition, members of the no-misuse group had lower rates for the other problem behaviors than all three substance misuse classes (all p < .001). There was an increasing trend in the number of on-premises outlets near the home (p = .041) (increasing from an average of 0.3 in both the non-misusing and marijuana-only groups to an average of 0.7 in the polysubstance group) and % living in the top decile of drug crime rates (p = .049) (increasing from 8.7% among non-misusers and marijuana-only misusers combined to 16.0% in alcohol/marijuana misusers and polysubstance misusers combined), but none with regard to package alcohol outlets (p = .675) or residence in high-density areas of violent crime density (p = .663).
Table 1.
Characteristics of each substance use group.
| Non-misusers (n = 451) | MJ-only (n = 245) | Alc & MJ (n = 141) | Polysubstance (n = 40) | |
|---|---|---|---|---|
| Substance misuse rates | ||||
| % Marijuana*** | 0.0 | 100.0 | 59.5 | 92.5 |
| % Alcohol*** | 0.0 | 0.0 | 100.0 | 60.0 |
| % Cocaine*** | 0.0 | 0.0 | 4.3 | 30.0 |
| % Hallucinogens*** | 0.0 | 0.0 | 0.0 | 25.0 |
| % Street opioids*** | 0.0 | 0.0 | 0.0 | 20.0 |
| % Prescription stimulants*** | 0.0 | 1.2 | 2.8 | 22.5 |
| % Prescription opioids*** | 0.0 | 0.0 | 0.7 | 57.5 |
| % Sedatives*** | 0.0 | 4.5 | 0.0 | 50.0 |
| Individual demographics | ||||
| Age M (SD)*** | 19.2 (2.8) | 19.8 (2.4) | 21.1 (2.2) | 20.4 (2.1) |
| % Male*** | 39.4 | 60.8 | 57.4 | 62.5 |
| % African American*** | 74.6 | 76.3 | 63.8 | 37.5 |
| % Government Aid | 74.1 | 73.7 | 79.4 | 72.5 |
| % Violent injury group*** | 48.9 | 62.4 | 61.7 | 65.0 |
| Other behavioral outcomes | ||||
| % Unprotected sex*** | 10.0 | 18.0 | 19.1 | 35.0 |
| % Motor vehicle crash*** | 3.1 | 6.5 | 10.0 | 15.0 |
| % Serious violence*** | 52.9 | 66.9 | 70.2 | 82.5 |
| % Weapon victimization*** | 48.0 | 66.9 | 65.9 | 70.0 |
| % Weapon aggression*** | 8.8 | 22.0 | 24.1 | 22.5 |
| Alcohol outlets and crime | ||||
| # On-premises outlets within 1/4 mile M (SD)* | 0.3 (0.8) | 0.3 (0.8) | 0.4 (1.1) | 0.7 (1.5) |
| # Package stores within 1/4 mile M (SD) | 0.8 (0.9) | 0.9 (0.9) | 0.8 (0.9) | 0.9 (1.0) |
| % in top decile violent crime density | 19.5 | 23.7 | 24.1 | 12.5 |
| % in top decile drug crime density* | 9.7 | 6.9 | 15.6 | 17.5 |
Notes. Tests in the “other behavioral outcomes” and “alcohol outlets and crime” categories treat substance use categories as ordinal, moving from “Non-misusers” to “Polysubstance”. MJ-only: Marijuana-only misuse class. Alc & MJ: Alcohol/Marijuana misuse class.
p < .05
**p < .01
p < .001.
Multinomial logistic regression
In Table 2 covariate effects, expressed as risk ratios of being in each substance misuse class, relative to the no-misuse group, are shown. As before, males and older individuals are less likely to be in the no-misuse group, and African Americans are less likely to be in the poly-substance class than the no-misuse group (Table 2), the marijuana-only group (RRR = 0.21, p < .001), and the alcohol/marijuana group (RRR = 0.36, p = .006). Similarly, African Americans are less likely to be in the alcohol/marijuana group than the marijuana-only group (RRR = 0.59, p = .019).
Table 2.
Multinomial logistic regression analysis of substance use groups.
| MJ-only | Alc & MJ | Polysubstance | |
|---|---|---|---|
| Individual demographics | |||
| Age | 1.13 (1.05–1.20)*** | 1.38 (1.26–1.51)*** | 1.18 (1.02–1.36)* |
| Male | 2.85 (2.00–4.06)*** | 2.82 (1.82–4.39)*** | 2.84 (1.34–6.01)** |
| African American | 1.26 (0.84–1.89) | 0.75 (0.47–1.19) | 0.27 (0.13–0.57)** |
| Government aid | 1.22 (0.82–1.80) | 1.65 (0.99–2.77) | 1.03 (0.46–2.32) |
| Violent injury group | 1.24 (0.84–1.83) | 1.06 (0.65–1.74) | 0.94 (0.41–2.17) |
| Other behavioral outcomes | |||
| Unprotected sex | 1.90 (1.18–3.08)* | 1.77 (1.01–3.11)* | 4.16 (1.91–9.02)*** |
| Motor vehicle crash | 1.81 (0.83–3.94) | 2.39 (1.03–5.52)* | 3.85 (1.23–12.05)** |
| Serious violence | 1.53 (1.02–2.31)* | 1.83 (1.08–3.11)* | 3.33 (1.22–9.08)** |
| Weapon aggression | 2.40 (1.48–3.89)*** | 2.87 (1.62–5.06)*** | 2.35 (0.95–5.82) |
| Weapon victimization | 1.36 (0.92–2.00) | 1.38 (0.85–2.25) | 1.54 (0.66–3.59) |
| Alcohol outlets and crime | |||
| # On-premises stores within 1/4 mile | 1.08 (0.88–1.33) | 1.14 (0.91–1.42) | 1.42 (1.07–1.89)* |
| # Package stores within 1/4 mile | 1.13 (0.93–1.37) | 0.99 (0.78–1.26) | 0.95 (0.65–1.40) |
| In top decile of drug crime density | 0.60 (0.32–1.14) | 1.19 (0.62–2.28) | 0.89 (0.33–2.43) |
| In top decile of violent crime density | 1.17 (0.76–1.79) | 1.83 (1.08–3.11)* | 1.28 (0.43–3.81) |
Notes. Table entries represent risks of being in each group, relative to the Non-misusing group. MJ-only: Marijuana-only misuse class. Alc & MJ: Alcohol/Marijuana misuse class.
p < .05
p < .01
p < .001.
Many problem behaviors were associated with substance use group. All three substance use classes had higher rates of unprotected sex and serious violence than the no-misuse group (Table 2). There were no other significant differences between the three substance-using groups on rates of serious violence, with the largest effect size being the polysubstance group, relative to the marijuana-only group (RRR = 2.18, p = .067). The polysubstance group had higher rates of unprotected sex than the no-misuse group (Table 2), the marijuana-only (RRR = 2.18, p = .023) group, and the alcohol/marijuana group (RRR = 2.34, p = .020). Relative to the no-misuse group, car crashes were more common among the alcohol/marijuana group and the polysubstance group (Table 2). Car crashes were more prevalent among the polysubstance group than the marijuana-only group, but this effect was not significant (RRR = 2.13, p = .087). Weapon aggression was more prevalent among the marijuana-only group and the alcohol/marijuana group than among the no-misuse group (Table 2); there were no other significant distinctions between substance use groups based on weapon aggression or victimization.
Associations between substance use group and crime/alcohol outlets are shown in the final section of Table 2. On-premises alcohol outlet density was higher among the polysubstance group, relative to the no-misuse group (Table 2), and the marijuana-only group (RRR = 1.31, p = .034), but not to the alcohol/marijuana group (RRR = 1.25, p = .069). The alcohol/marijuana group had higher rates of residence near areas of high violent crime density than the non-misusing group (Table 2), but not the marijuana-only group (RRR = 1.56, p = .05) or the polysubstance group (RRR = 1.42, p = .27). The alcohol/marijuana group had higher rates of residence near areas of high drug crime density than the marijuana-only group (RRR =1.98, p = .03), but not non-users (RRR = 1.19, p = .30) or polysubstance users (RRR = 1.33, p = .29). There was no evidence that the polysubstance group had higher rates of residents near areas of high drug crime density than the marijuana-only group (RRR = 1.49, p = .23). There were no between-group differences with regard to package outlet concentration.
Discussion
In this study, substance use profiles of youth seeking care in an urban ED were analyzed and four characteristic profiles were identified: non-misusers, marijuana-only misusers, alcohol/marijuana misusers, and poly-substance misusers. Moving from the non-misusing group to the polysubstance misuse group, increasing trends in rates of unprotected sex, traffic crashes, and three indicators of violence involvement were observed. Community-level indicators of crime and alcohol outlet concentration were associated with substance misuse profiles. Specifically, (a) polysubstance users are more likely to live near more on-premises alcohol outlets than individuals reporting no substance misuse or marijuana-only misuse; (b) alcohol/marijuana misusers were more like than non-misusers to live near areas of high violent crime density; (c) marijuana-only misusers were less likely like than alcohol/marijuana misusers to live near areas of high drug crime density. These results show promise for future research that includes objective measures of neighborhood factors that may increase risk for substance use and other problem behaviors.
Analogs to the profiles identified in this population – non-misusers, marijuana-only misusers, alcohol/marijuana misusers, and polysubstance misusers – have each been identified in several previous studies (5,6,9,10). Except in analogous studies of Native Americans (9) and those restricted to drug users (7,11), the prevalence of none/little use (51.5%) was smaller than other studies (5,6,8,10,12), although differences from our 6-month timeframe, e.g. lifetime abuse/dependence (5), past-month for tobacco/alcohol and past-year for other drugs (6), past month (8,10), and past 3-months (12), should be noted. The lower prevalence of low-risk substance use behavior underscores this as a high-risk population, which is amplified by the higher rates of other problem behaviors in all three classes of substance misusers.
Substance use and other problem behaviors
Many researchers have reported on the link between substance use and other problem behaviors but our study is novel in its focus on how substance use classes map onto problem behavior endorsement rates. The results presented here show an increasing trend in all problem behavior endorsement rates – unprotected sex, motor vehicle crash, violence involving hospitalization, weapon aggression, and weapon victimization – moving from the non-misusing group to the polysubstance group. Having observed successful intervention on multiple behaviors simultaneously (25,26) and intervention effects on behaviors not specifically addressed by an intervention (27), these results suggest that a multi-pronged intervention approach may be fruitful.
An additional finding was that rates of each problem behavior were substantially lower in the non-misusing group. This indicates that substance misusing urban youth – independently of which substances – represent a critical focus for problem behavior prevention efforts. For example, this suggests that screening for any substance misuse may be effective when the goal is to target a broad population at risk for problem behavior involvement. Given that the small number of polysubstance users in the current study limited the ability to fully clarify the differences between groups, future studies with a larger sample size from a comparable population are needed to help to clarify potentially important between-group differences.
Alcohol outlets, crime, and substance use profiles
This study was the first to investigate the association between substance use profiles and alcohol outlet and crime density. The results shown here indicate that on-premises alcohol outlets near one's home is associated with increased likelihood of polysubstance use, relative to both the no-misuse group and the marijuana-only group. Given that a majority of the sample was not of legal age to purchase alcohol, an investigation of whether under-enforcement of existing policies is associated with polysubstance use is warranted. However, researchers often envision alcohol outlets as correlates of social disorganization (58), which provides an alternative explanation. Residence in an area of high drug crime density increases the probability of membership in the alcohol/marijuana class, relative to the marijuana-only class. Similarly, alcohol/marijuana misusers are more likely to live in high violent crime density areas than non-misusers. These findings suggest that neighborhood-level features could play a role in the etiology of substance misuse. However, the unexpected finding that on-premises – but not package – outlet density increases polysubstance misuse risk requires further investigation. Prior work indicates alcohol outlet types are not homogeneous in how they modulate assault risk, and even that different types of on-premises outlets can confer different risks (33), but this dynamic is not well understood with regard to substance use, and the alcohol outlet typology available here (on-premises vs. not) is insufficiently granular for this purpose.
Future studies have potential to improve intervention by incorporating geographic information. The results presented suggest that interventions localized to areas of higher on-premises alcohol outlet concentration may reach more polysubstance users. Similarly, if a central goal of a particular substance use intervention were to also reduce rates of unprotected sex, then targeting areas of higher on-premises alcohol outlet density may be sensible, given that polysubstance users had the highest rates of unprotected sex. Given the tremendous potential for effective geographically based health interventions (28), analogous studies in other geographic settings are in order to investigate this possibility.
Limitations
Study limitations should be noted. First, the economically disadvantaged nature of Flint may limit general-izability. However, the results may be applicable to youth living in other economically distressed settings. Similarly, the study design only permits inference on the population of youth entering the ED, as opposed to the general population. Yet, urban ED entrants represent a broadly at-risk population and may represent a uniquely intervenable population due to the “teachable moment” presented by ED entry (59). Second, the community-level measures available are limited. For example, differential effects of different types of alcohol outlets have been documented (33), but Michigan's alcohol outlet licensing data does not permit typology beyond “on-premises” and “package store”. This aggregation of potentially heterogeneous outlet types may attenuate some effects seen here. In addition, high levels of demographic segregation in Flint (60) make identifying neighborhood effects more difficult due to confounding of individual- and community-level effects. These limitations make the identification of some significant links all the more encouraging. Third, the wide age range should be mentioned because it presents the possibility of censoring in the no-misuse group, particularly among the youngest individuals. However, recent data suggests that a large majority of substance users from the general population initiate before age 17 (61). Combined with propositions that individuals residing in inner city communities begin the period of emerging adulthood as early as age 14 (62), this suggests the average age of initiation may be even younger in our study population. Finally, we note the limitation of using straight-line distances for the alcohol outlet buffers, namely that these buffers do not account for the presence of physical impediments (e.g., bodies of water) that may render Euclidean distance less meaningful. However, walking distances – which are the conceptual basis of our buffers – are not necessarily restricted to road networks. Given possible drawbacks to both definitions of distances, we made this specification on the basis of practical simplicity.
Conclusions
Addressing the public health epidemic of substance use and its associated comorbidities requires studying the populations at greatest risk, identifying the characteristic substance use profiles present in those populations, and determining what factors are associated with the most problematic classes. Given the results shown here, further research is required to determine drivers of heterogeneity in substance use profiles in at-risk populations, including positive community factors that may help protect youth from the risks they face. Such future research has the potential to shift our focus from individual-level interventions to neighborhood-changing activities that engage the larger community in creating contexts that promote healthful outcomes instead of increasing the odds of substance use and other problem behaviors.
Acknowledgments
Funding
We disclose the role of NIDA R01 024646 (PI: Cunningham) in funding this work and thank the project staff, and well as the staff and patients at Hurley Medical Center for making this work possible. Dr. Goldstick's effort was also supported by NIDA R03 DA039003-02 (PI: Goldstick) and Dr. Stoddard is supported by NIDA grant K01-DA034765 (PI: Stoddard).
References
- 1.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national survey results on drug use, 1975–2012: Volume I, Secondary school students. Institute for Social Research, The University of Michigan; Ann Arbor: 2013. [Google Scholar]
- 2.Brière FN, Fallu JS, Descheneaux A, Janosz M. Predictors and consequences of simultaneous alcohol and cannabis use in adolescents. Addict Behav. 2011;36:785–788. doi: 10.1016/j.addbeh.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 3.Redonnet B, Chollet A, Fombonne E, Bowes L, Melchior M. Tobacco, alcohol, cannabis and other illegal drug use among young adults: the socioeconomic context. Drug Alcohol Depend. 2012;121:231–239. doi: 10.1016/j.drugalcdep.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Hakkarainen P, Metso L. Joint use of drugs and alcohol. Eur Addict Res. 2009;15:113–120. doi: 10.1159/000209244. [DOI] [PubMed] [Google Scholar]
- 5.Agrawal A, Lynskey MT, Madden PA, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102:94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- 6.Conway KP, Vullo GC, Nichter B, Wang J, Compton WM, Iannotti RJ, Simons-Morton B. Prevalence and patterns of polysubstance use in a nationally representative sample of 10th graders in the United States. J Adolesc Health. 2013;52:716–723. doi: 10.1016/j.jadohealth.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trenz RC, Scherer M, Duncan A, Harrell PT, Moleko AG, Latimer WW. Latent class analysis of polysubstance use, sexual risk behaviors, and infectious disease among South African drug users. Drug Alcohol Depend. 2013;132:441–448. doi: 10.1016/j.drugalcdep.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Connell CM, Gilreath TD, Hansen NB. A multiprocess latent class analysis of the co-occurrence of substance use and sexual risk behavior among adolescents. J Stud Alcohol Drugs. 2009;70:943. doi: 10.15288/jsad.2009.70.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitesell NR, Beals J, Mitchell CM, Novins DK, Spicer P, Manson SM, AI-SUPERPFP Team Latent class analysis of substance use: comparison of two American Indian reservation populations and a national sample. J Stud Alcohol Drugs. 2006;67:32. doi: 10.15288/jsa.2006.67.32. [DOI] [PubMed] [Google Scholar]
- 10.Blow FC, Walton MA, Barry KL, Murray RL, Cunningham RM, Massey LS, Chermack ST, Booth BM. Alcohol and drug use among patients presenting to an inner-city emergency department: a latent class analysis. Addict Behav. 2011;36:793–800. doi: 10.1016/j.addbeh.2010.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrell PT, Mancha BE, Petras H, Trenz RC, Latimer WW. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug Alcohol Depend. 2012;122(3):220–227. doi: 10.1016/j.drugalcdep.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bohnert KM, Walton MA, Resko S, Berry KT, Chermack ST, Zucker RA, Zimmerman MA, et al. Latent class analysis of substance use among adolescents presenting to urban primary care clinics. Am J Drug Alcohol Abuse. 2014;40:44–50. doi: 10.3109/00952990.2013.844821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jessor R. Risk behavior in adolescence: a psychosocial framework for understanding and action. J Adolesc Health. 1991;12:597–605. doi: 10.1016/1054-139x(91)90007-k. [DOI] [PubMed] [Google Scholar]
- 14.Gabriel RM, Hopson T, Haskins M, Powell KE. Building relationships and resilience in the prevention of youth violence. Am J Preventative Med. 1995;12:48–55. [PubMed] [Google Scholar]
- 15.Walton MA, Cunningham RM, Goldstein AL, Chermack ST, Zimmerman MA, Bingham CR, Shope JT, et al. Rates and correlates of violent behaviors among adolescents treated in an urban emergency department. J Adolesc Health. 2009;45:77–83. doi: 10.1016/j.jadohealth.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chermack ST, Blow FC. Violence among individuals in substance abuse treatment: the role of alcohol and cocaine consumption. Drug Alcohol Depend. 2002;66:29–37. doi: 10.1016/s0376-8716(01)00180-6. [DOI] [PubMed] [Google Scholar]
- 17.Swahn MH, Donovan JE. Correlates and predictors of violent behavior among adolescent drinkers. J Adolesc Health. 2004;34:480–492. doi: 10.1016/j.jadohealth.2003.08.018. [DOI] [PubMed] [Google Scholar]
- 18.Fisher JC, Bang H, Kapiga SH. The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sexually Transmitted Dis. 2007;34:856–863. doi: 10.1097/OLQ.0b013e318067b4fd. [DOI] [PubMed] [Google Scholar]
- 19.Kalichman SC, Leickness SC, Vermaak R, Jooste S, Cain D. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (Shebeens) in Cape Town, South Africa. Prev Sci. 2008;9:55–62. doi: 10.1007/s11121-008-0085-x. [DOI] [PubMed] [Google Scholar]
- 20.Walton MA, Resko S, Whiteside L, Chermack ST, Zimmerman M, Cunningham RM. Sexual risk behaviors among teens at an urban emergency department: relationship with violent behaviors and substance use. J Adolesc Health. 2011;48:303–305. doi: 10.1016/j.jadohealth.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shope JT, Waller PF, Raghunathan TE, Patil SM. Adolescent antecedents of high-risk driving behavior into young adulthood: substance use and parental influences. Accid Anal Prev. 2001;33:649–658. doi: 10.1016/s0001-4575(00)00079-8. [DOI] [PubMed] [Google Scholar]
- 22.Elliott MR, Shope JT, Raghunathan TE, Waller PF. Gender differences among young drivers in the association between high-risk driving and substance use/environmental influences. J Stud Alcohol. 2006;67:252. doi: 10.15288/jsa.2006.67.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bingham CR, Shope JT. Adolescent developmental antecendents of risky driving among young adults. J Stud Alcohol Drugs. 2004;65:84. doi: 10.15288/jsa.2004.65.84. [DOI] [PubMed] [Google Scholar]
- 24.Costa F. Problem-Behavior Theory ~ A Brief Overview. Available at: http://www.colorado.edu/ibs/jessor/pb_theory.html.
- 25.Cunningham RM, Bernstein SL, Walton M, Broderick K, Vaca FE, Woolard R, Bernstein E, et al. Alcohol, tobacco, and other drugs: future directions for screening and intervention in the emergency department. Acad Emergency Med. 2009;16:1078–1088. doi: 10.1111/j.1553-2712.2009.00552.x. [DOI] [PubMed] [Google Scholar]
- 26.Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. J Am Med Assoc. 2010;304:527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gentilello LM, Rivara FP, Donovan DM, Jurkovich GJ, Daranciang E, Dunn CW, Viillaveces A, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann. Surg. 1999;230:473. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rushton G. Public health, GIS, and spatial analytic tools. Annu Rev Public Health. 2003;24:43–56. doi: 10.1146/annurev.publhealth.24.012902.140843. [DOI] [PubMed] [Google Scholar]
- 29.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychological Bull. 2000;126:309. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- 30.Esbensen F-A, Huizinga D. Community structure and drug use: from a social disorganization perspective. Justice Q. 1990;7:691–709. [Google Scholar]
- 31.Karriker-Jaffe KJ. Areas of disadvantage: A systematic review of effects of area-level socioeconomic status on substance use outcomes. Drug Alcohol Rev. 2011;30:84–95. doi: 10.1111/j.1465-3362.2010.00191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Resko SM, Walton MA, Bingham CR, Shope JT, Chermack ST, Zimmerman M, Blow FC, Cunningham RM. Alcohol availability and youth violence: a multi-level analysis of the role of outlet density. Am J Community Psychol. 2010;46:252–262. doi: 10.1007/s10464-010-9353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lipton R, Yang X, Braga A, Goldstick J, Newton M, Rura M. The geography of violence, alcohol outlets and drug arrests in Boston. Am J Public Health. 2013;103:657–664. doi: 10.2105/AJPH.2012.300927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lipton R, Gruenewald P. The spatial dynamics of violence and alcohol outlets. J Stud Alcohol. 2002;63:187–195. doi: 10.15288/jsa.2002.63.187. [DOI] [PubMed] [Google Scholar]
- 35.Gruenewald PJ, Freisthler B, Remer L, LaScala EA, Treno A. Ecological models of alcohol outlets and violent assaults: crime potentials and geospatial analysis. Addiction. 2006;101:666–677. doi: 10.1111/j.1360-0443.2006.01405.x. [DOI] [PubMed] [Google Scholar]
- 36.Gruenewald PJ. The spatial ecology of alcohol problems: niche theory and assortative drinking. Addict. 2007;102:870–878. doi: 10.1111/j.1360-0443.2007.01856.x. [DOI] [PubMed] [Google Scholar]
- 37.Goldstick J, Brenner A, Lipton R, Mistry R, Aiyer S, Reischl T, Zimmerman M. A spatial analysis of heterogeneity in the link between alcohol outlets and assault victimization: differences across victim sub-populations. Violence Victims. 2015;30:649–662. doi: 10.1891/0886-6708.VV-D-13-00187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pines JM, Hilton JA, Weber EJ, Alkemade AJ, Shabanah HA, Anderson PD, Bernhard M, et al. International perspective on emergency department crowding. Acad Emergency Med. 2011;18:1358–1370. doi: 10.1111/j.1553-2712.2011.01235.x. [DOI] [PubMed] [Google Scholar]
- 39.Niska R, Bhuiya F, Xu J. National hospital ambulatory medical care survey: 2007 emergency department summary. National Health Care Stat Rep. 2010;26:1–31. [PubMed] [Google Scholar]
- 40.Bonar EE, Walton MA, M CR, Chermack ST, Bohnert AS, Barry KL, Booth BM, Blow FC. Computer-enhanced interventions for drug use and HIV risk in the emergency room: preliminary results on psychological precursors of behavior change. J Subst Abuse Treat. 2014;46:5–14. doi: 10.1016/j.jsat.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cunningham RM, Chermack ST, Ehrlich PF, Carter PM, Booth BM, Blow FC, Barry KL, Walton MA. Alcohol interventions among underage drinkers in the ED: a randomized controlled trial. Pediatr. 2015;136:783–793. doi: 10.1542/peds.2015-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chantala K, Tabor J. National Longitudinal Study of Adolescent Health: Strategies to perform a design-based analysis using the Add Health data. Available at: http://www.cpc.unc.edu/projects/addhealth/documentation/guides/weight1.pdf.
- 43.Handelsman L, Stein JA, Grella CE. Contrasting predictors of readiness for substance abuse treatment in adults and adolescents: a latent variable analysis of DATOS and DATOS-A participants. Drug Alcohol Depend. 2005;80:63–81. doi: 10.1016/j.drugalcdep.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 44.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Internal Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 45.Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, de Lacerda RB, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addict. 2008;103:1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- 46.Barbor TF, Higgins-Biddle JC, Saunders JB, Montero MG. World Health Organization Department of Mental Health and Substance Dependence, editor. The alcohol use disorders identification test (AUDIT): guidelines for use in primary care. 2001 [Google Scholar]
- 47.National Institute on Drug Abuse “NIDA Quick Screen V1.0”. Available at: http://www.drugabuse.gov/nidamed/screening/nmassist.pdf.
- 48.Goldstick J, Lipton R, Carter P, Stoddard SA, Newton M, Reischl T, Walton M, et al. The effect of neighborhood context on the relationship between substance use and weapons aggression in urban adolescents entering the ED. Subst Use Misuse. 2015;50:674–684. doi: 10.3109/10826084.2014.998235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Federal Bureau of Investigations National Incident Based Reporting System (NIBRS) Categories. Available at: http://www.fbi.gov/about-us/cjis/ucr/nibrs/nibrscategories.pdf.
- 50.McCutcheon AL. Latent class analysis. Sage; Newbury Park, CA: 1987. [Google Scholar]
- 51.Nylund KL, Asparouhob T, Muthén BO, Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model. 2007;14:535–569. [Google Scholar]
- 52.Leisch F. FlexMix: A general framework for finite mixture models and latent class regression in R. 2003 [Google Scholar]
- 53.Grün B, Leisch F. FlexMix version 2: finite mixtures with concomitant variables and varying and constant parameters. J Stat Software. 2008;28:1–35. [Google Scholar]
- 54.Hothorn T, Hornik K, van de Wiel MA, Zeiles A. Implementing a class of permutation tests: the coin package. J Stat Software. 2008;28:1–23. [Google Scholar]
- 55.Venables WN, Ripley BD. Modern applied statistics with S. 4th ed. Springer; New York: 2002. [Google Scholar]
- 56.Cunningham RM, Ranney M, Newton M, Woodhull W, Zimmerman M, Walton MA. Characteristics of youth seeking emergency care for assault injuries. Pediatrics. 2014;133:96–105. doi: 10.1542/peds.2013-1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ram N, Grimm K. Growth mixture modeling: a method for identifying differences in longitudinal change among unobserved groups. Int J Behav Dev. 2009;33:565–576. doi: 10.1177/0165025409343765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Snowden AJ, Pridemore WA. Alcohol outlets, social disorganization, land use, and violence in a large college town: direct and moderating effects. Criminal Justice Rev. 2013;38:29–49. [Google Scholar]
- 59.Maio RF, Shope JT, Blow FC, Gregor MA, Zakrajsek JS, Weber JE, Nypaver MM. A randomized controlled trial of an emergency department–based interactive computer program to prevent alcohol misuse among injured adolescents. Ann Emergency Med. 2005;45:420–429. doi: 10.1016/j.annemergmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 60.U.S. Census Flint, Michigan segregation: Dissimilarity indices. 2010 Retrieved from http://www.censusscope.org/us/m2640/chart_dissimilarity.html.
- 61.Substance Abuse and Mental Health Services Administration Substance Abuse and Mental Health Services Administration, editor. The TEDS report: age of substance use initiation among treatment admissions aged 18 to 30. 2014:1–6. [PubMed] [Google Scholar]
- 62.Arnett JJ. Conceptions of the transition to adulthood among emerging adults in American ethnic groups. New Directions Child Adolesc Dev. 2003:63–76. doi: 10.1002/cd.75. 2003. [DOI] [PubMed] [Google Scholar]