Abstract
Background
Hypertension is a significant risk factor for intracerebral hemorrhage (ICH). While ethnic/racial disparities related to hypertension and ICH have been reported, these previous studies were limited by a lack of Hispanics and inadequate power to analyze by ICH location. In the current study, while overcoming these prior limitations, we investigated whether there was variation by ethnicity/race of treated and untreated hypertension as risk factors for ICH.
Methods
The Ethnic/Racial Variations of ICH (ERICH) study is a prospective, multicenter, case-control study of ICH among whites, blacks, and Hispanics. Cases were enrolled from 42 recruitment sites. Controls matched to cases 1:1 by age (±5 years), sex, ethnicity/race, and metropolitan area were identified by random-digit dialing. Subjects were interviewed to determine history of hypertension and use of anti-hypertensive medications. Cases and controls within ethnic groups were compared using conditional logistic regression. Multivariable conditional logistic regression models were computed for ICH as an overall group and separately for the location subcategories deep, lobar, and infratentorial (brainstem/cerebellar).
Results
958 white, 880 black, and 766 Hispanic ICH cases were enrolled. For ICH cases, untreated hypertension was higher in blacks (43.6%, p<0.0001) and Hispanics (46.9%, p<0.0001) versus whites (32.7%). In multivariable analyses adjusted for alcohol use, anticoagulation, hypercholesterolemia, education, and medical insurance status, treated hypertension was a significant risk factor across all locations of ICH in whites (odds ratio [OR] 1.57, 95% CI 1.24–1.98, p<0.0001), blacks (OR 3.02, 2.16–4.22, <0.0001), and Hispanics (OR 2.50, 1.73–3.62, <0.0001). Untreated hypertension was a substantially greater risk factor for all three racial/ethnic groups across all locations of ICH: whites (OR 8.79, 5.66–13.66, <0.0001), blacks (OR 12.46, 8.08–19.20, <0.0001), Hispanics (OR 10.95, 6.58–18.23, <0.0001). There was an interaction between race/ethnicity and ICH risk (P<0.0001).
Conclusions
Untreated hypertension confers a greater ICH risk in blacks and Hispanics relative to whites across all anatomic locations of ICH. Accelerated research efforts are needed to improve overall hypertension treatment rates and to monitor the impact of such efforts on racial/ethnic disparities in stroke.
Keywords: hypertension, intracerebral hemorrhage, stroke, race, ethnicity
Subject Terms: Hypertension, Intracranial Hemorrhage, Cerebrovascular Disease/Stroke, Race and Ethnicity
Intracerebral hemorrhage (ICH) comprises about 10% of strokes but 50% of stroke mortality.1, 2 Survivors of ICH often have significant morbidity.3 Hypertension is a major public health problem, with annual costs directly attributable to hypertension projected to increase by $130.4 billion from 2010 to 2030.4 Hypertension is the single most important risk factor for all types of stroke,5 and untreated hypertension is a significant risk factor for hemorrhagic stroke.6, 7
There are important ethnic/racial disparities related to hypertension and stroke, including ICH. Blacks have higher rates of hypertension compared with whites,1 are more likely to develop hypertension at an earlier age, are more likely to experience complications,8 and have hypertension that is more difficult to control.9 ICH patients are on average younger than those with ischemic stroke, and a disproportionally large number of these younger patients are from ethnic/racial minorities.10, 11 Although Hispanics have lower reported rates of hypertension,12 they are less likely to be screened and treated.13, 14
We reported in 2004 that untreated and treated hypertension were significant risk factors for hemorrhagic stroke, including ICH and subarachnoid hemorrhage, in a biracial population.6 We did not adequately assess differences in ICH by type and location of hemorrhage, and Hispanics were underrepresented in that study. Given the ethical ramifications, randomized trials cannot assess the risk of untreated versus treated hypertension for ICH; however, case-control studies may allow a robust evaluation of the differential risk for ICH conferred by treated and untreated hypertension. We examined the hypothesis that untreated and treated hypertension are significant risk factors for ICH in white, black, and Hispanic patients, and we analyzed the proportion of untreated hypertension in ICH patients in these three ethnic/racial groups. To the best of our knowledge, this is the first report to quantify the impact of both treated and untreated hypertension for ICH risk in blacks, whites and Hispanics.
METHODS
The Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study is a prospective, multicenter, case-control study of ICH among white, black, and Hispanic patients. The study protocol has been previously published.2 There were 19 clinical recruitment centers and 42 total recruitment sites. In order to minimize the effect of early mortality following ICH, which is a common barrier to patient recruitment and can result in survival bias, cases were enrolled using hot-pursuit. This enrollment strategy involves early identification of ICH cases through active screening of admission logs from the emergency department, neurology service, neurosurgery service, neurosurgical/neurological intensive care unit, and general admission logs at each recruitment site.2 Potential cases were reviewed by site investigators. Controls, matched 1:1 to cases by age (±5 years), sex, ethnicity/race, and metropolitan area, were recruited using two random-digit dialing centers. A more detailed description of control recruitment methodology is included in the online supplement. Institutional Review Board approval at each participating center was required before initiation of study enrollment. Informed consent was obtained from each enrolled subject or legally authorized representative.
Recruited ICH patients were self-reported non-Hispanic white, non-Hispanic black, or Hispanic, ≥ 18 years of age, and residents of an area within 75 miles of one of the 19 recruitment centers. A distance of 100 miles was allowed if the population center had fewer than 1 million people. Informed consent was provided by the patient or legal representative. ICH was defined as a spontaneous, nontraumatic, and abrupt onset of severe headache, focal neurologic deficit, or altered level of consciousness associated with a focal blood collection in the brain parenchyma. ICH due to trauma, aneurysm, tumor, dural venous sinus thrombosis, vascular malformation, malignancy associated coagulopathy, or hemorrhagic conversion of an ischemic stroke were excluded. ICH volume was determined by imaging review undertaken centrally.
Among the items on baseline interview, participants (both cases and controls) were asked if they have ever been diagnosed as having hypertension (“history of hypertension”) and they were asked to provide a list of all medications they took in the two weeks prior to ICH onset (for cases) or prior to interview (for controls). There were 34 ICH cases and 2 controls for which hypertension status was unknown, therefore, hypertension variables were missing for these subjects. Elevated blood pressure at the time of study enrollment was not used to define “hypertension” for the present analysis because, for cases, ICH itself can result in elevated blood pressure. Treated hypertension was defined as a history of hypertension plus use of antihypertensive medications. Untreated hypertension was defined as a history of hypertension without use of antihypertensive medications.
STATISTICAL ANALYSIS
Cases and controls within ethnic groups were compared using conditional logistic regression. ICH volumes, being heavily skewed, were natural log transformed to best approximate distributional assumptions. Multivariable conditional logistic regression models were computed for ICH as an overall group and separately for the location subcategories deep, lobar, and infratentorial (brainstem/cerebellar). In each multivariable model, those with untreated hypertension and treated hypertension were compared with those without hypertension after adjusting for other risk factor variables. To begin each multivariable model, variables with p ≤ 0.1 from the univariate analyses were included with subsequent backward elimination. Odds ratios (OR), corresponding confidence intervals (CI), and p-values (significance <0.05) were calculated.
RESULTS
A total of 958 white, 880 black, and 766 Hispanic case-control pairs were enrolled between September 2010 and September 2015. Demographic information is shown for ICH cases by ethnicity/race in Table 1 and by hypertensive status in eTable 1. Among cases of ICH, untreated hypertension was higher in blacks (43.6%, p<0.0001) and Hispanics (46.9%, p<0.0001) compared with whites (32.7%). Medical insurance coverage was identified as a potentially important factor related to access to care and subsequently seeking medical evaluation and treatment. Therefore, the analysis was adjusted for whether a subject had medical insurance, and after this adjustment, a significant difference persisted for the proportion of untreated hypertension in ICH for whites versus Hispanics (p=0.0064), but not for whites versus blacks (p=0.12). After adjusting for medical insurance status and age, given higher mean age for white ICH cases (68.6 years) compared with blacks (58.0 years) and Hispanics (59.3 years), there were no significant differences in untreated hypertension for black (p=0.81) and Hispanic (p=0.14) ICH cases versus whites.
Table 1.
Demographic Information for ICH Cases by Ethnicity/Race
| White Cases | Black Cases | Hispanic Cases | p-value | |
|---|---|---|---|---|
|
| ||||
| n | 958 | 880 | 766 | |
|
| ||||
| Average Age, years (SD)* | 68.6 (13.4) | 58.0 (11.9) | 59.3 (13.5) | <0.0001 |
|
| ||||
| Female, n (%) | 422 (44.1) | 398 (45.2) | 328 (42.8) | 0.6177 |
|
| ||||
| Hypertension, n (%) | 685 (72.3) | 753 (86.6) | 582 (77.4) | <0.0001 |
|
| ||||
| Untreated Hypertension, n (%)** | 224 (32.7) | 328 (43.6) | 273 (46.9) | <0.0001 |
|
| ||||
| Heavy Alcohol Use, n (%) | 64 (6.8) | 96 (11.3) | 78 (10.4) | 0.0020 |
|
| ||||
| Hypercholesterolemia, n (%) | 450 (49.5) | 278 (33.6) | 279 (38.5) | <0.0001 |
|
| ||||
| Anticoagulant Use, n (%) | 133 (13.9) | 41 (4.7) | 55 (7.2) | <0.0001 |
|
| ||||
| Education Level n (%) | ||||
|
| ||||
| Less than High School | 87 (9.1) | 193 (22.1) | 352 (46.9) | |
|
| ||||
| High School | 301 (31.6) | 315 (36.0) | 225 (30.0) | |
|
| ||||
| Greater than High School | 565 (59.3) | 366 (41.9) | 174 (23.2) | <0.0001 |
|
| ||||
| Medical Insurance Status n (%) | 851 (88.8) | 580 (65.9) | 492 (64.2) | <0.0001 |
|
| ||||
| Location | ||||
| -Lobar n (%) | 400 (43.0) | 202 (23.3) | 207 (28.0) | |
| -Deep n (%) | 429 (46.1) | 544 (62.8) | 410 (55.4) | |
| -Brainstem n (%) | 36 (3.9) | 58 (6.7) | 44 (5.9) | |
| -Cerebellum n (%) | 66 (7.1) | 63 (7.3) | 79 (10.7) | <0.0001 |
|
| ||||
| ICH Volume: Geometric Mean (95% CI)*** | 11.5 (10.6, 12.5) | 8.7 (8.0, 9.5) | 11.3 (10.3, 12.4) | <0.0001 |
|
| ||||
| MRI Imaging, n | 274 | 286 | 299 | |
|
| ||||
| Microbleed Positive n (%) | 126 (46.0) | 170 (59.4) | 147 (49.2) | |
|
| ||||
| Mean number of microbleeds (95% CI)**** | 18.0 (10.6–25.3) | 14.5 (9.8–19.2) | 11.6 (7.6–15.6) | |
P-values for individual ethnic/racial groups are as follows: blacks and Hispanics, p=0.0357, blacks and whites, p<0.0001, Hispanics and whites, p<0.0001
Untreated hypertension is presented in reference to the number of subjects with a diagnosis of hypertension
P-values for individual ethnic/racial groups are as follows: blacks and Hispanics, p<0.0001, blacks and whites, p<0.0001, Hispanics and whites, p=0.7675
Mean number of microbleeds is calculated from the total microbleed positive cases, not from the total number of cases with MRI imaging data available
Univariate analyses comparing cases and controls were computed for each of the three ethnic/racial groups (Tables 2–4). To evaluate treated and untreated hypertension as risk factors for ICH, multivariable analyses were controlled for frequent alcohol use, hypercholesterolemia, education, medical insurance status, and anticoagulant use (Figure, eTable 2). Treated hypertension was a significant risk factor across all locations of ICH in whites (OR 1.57), blacks (OR 3.02), and Hispanics (OR 2.50). Untreated hypertension was a substantially greater risk factor across all locations of ICH for all three racial/ethnic groups: whites (OR 8.79), blacks (OR 12.46), Hispanics (OR 10.95). A formal test of interaction between race/ethnicity and ICH risk was highly significant, including separate statistical models for treated and untreated hypertension (P<0.0001 for both).
Table 2.
Univariate Analyses for White ICH Cases and Controls
| White Cases | White Controls | OR (95% CI) | p-value | |
|---|---|---|---|---|
| n | 958 | 958 | ||
| Age mean (%) | 68.6 (13.4) | 68.4 (12.9) | matched | |
| Number Female n (%) | 422 (44.1) | 422 (44.1) | matched | |
| Diagnosis of Hypertension n (%) | 685 (72.3) | 494 (51.6) | 2.41 (1.98, 2.94) | <0.0001 |
| Treated Hypertension n (%) | 461 (48.6) | 459 (47.9) | 1.69 (1.37, 2.09) | <0.0001 |
| Untreated Hypertension n (%) | 224 (23.6) | 35 (3.7) | 10.17 (6.72, 15.36) | <0.0001 |
| No Diagnosis of Hypertension n (%) | 263 (27.7) | 464 (48.4) | Reference | |
| Heavy Alcohol Use n (%) | 64 (6.8) | 52 (5.5) | 1.26 (0.86, 1.84) | 0.2448 |
| Hypercholesterolemia n (%) | 450 (49.5) | 498 (52.0) | 0.87 (0.72, 1.05) | 0.1598 |
| Anticoagulant Use n (%) | 133 (13.9) | 63 (6.6) | 2.40 (1.73, 3.34) | <0.0001 |
| Education Level: n (%) | ||||
| Less than High School | 87 (9.1) | 25 (2.6) | 6.29 (3.73, 10.61) | <0.0001 |
| High School | 301 (31.6) | 145 (15.1) | 3.36 (2.59, 4.36) | <0.0001 |
| Greater than High School | 565 (59.3) | 788 (82.3) | Reference | |
| Medical Insurance Status n (%) | 851 (88.8) | 919 (95.9) | 0.31 (0.21, 0.47) | <0.0001 |
Table 4.
Univariate Analyses for Hispanic ICH Cases and Controls
| Hispanic Cases | Hispanic Controls | OR (CI) | p-value | |
|---|---|---|---|---|
| N | 766 | 766 | ||
| Average Age | 59.3 (13.5) | 58.9 (13.4) | Matched | |
| Number Female n (%) | 328 (42.8) | 328 (42.8) | Matched | |
| Diagnosis of Hypertension n (%) | 582 (77.4) | 365 (47.7) | 4.30 (3.30, 5.61) | <0.0001 |
| Treated Hypertension | 309 (41.1) | 320 (41.8) | 2.43 (1.82, 3.24) | <0.0001 |
| Untreated Hypertension n (%) | 273 (36.3) | 45 (5.9) | 14.44 (9.38, 22.22) | <0.0001 |
| No Diagnosis of Hypertension n (%) | 170 (22.6) | 400 (52.3) | Reference | |
| Heavy alcohol Use | 78 (10.4) | 16 (2.1) | 5.77 (3.20, 10.40) | <0.0001 |
| Hypercholesterolemia | 279 (38.5) | 361 (47.5) | 0.68 (0.54, 0.85) | 0.0008 |
| Anticoagulant Use | 55 (7.2) | 20 (2.6) | 3.33 (1.87, 5.94) | <0.0001 |
| Education Level: n (%) | ||||
| Less than High School | 352 (46.9) | 184 (24.2) | 4.74 (3.56, 6.31) | <0.0001 |
| High School | 225 (30.0) | 171 (22.4) | 3.12 (2.33, 4.17) | <0.0001 |
| Greater than High School | 174 (23.2) | 407 (53.4) | Reference | |
| Medical Insurance Status n (%) | 492(64.2) | 654 (85.4) | 0.22 (0.16, 0.30) | <0.0001 |
Figure.
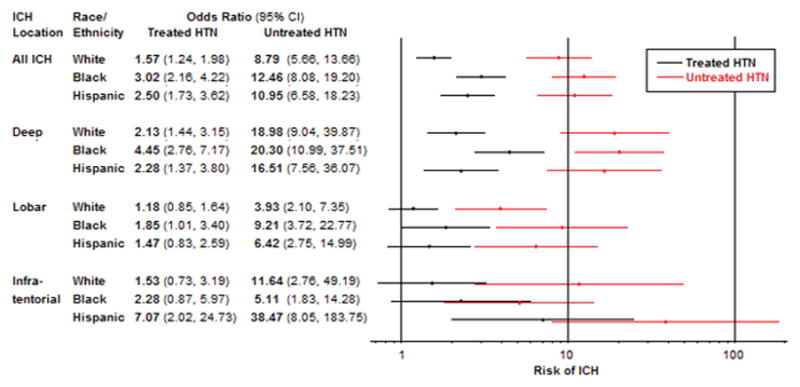
Multivariable Analyses: Risk of ICH Associated with Treated and Untreated Hypertension by ICH Location and Ethnicity/Race.
Controlled for frequent alcohol use, hypercholesterolemia, education, medical insurance status, and anticoagulant use, with the exception that anticoagulant use was not included in the model of brainstem/cerebellum ICH in blacks. Cases and controls were matched for age, ethnicity/race, sex, and metropolitan area.
For deep ICH, treated hypertension was a significant risk factor in whites (OR 2.13), blacks (OR 4.45), and Hispanics (OR 2.28), and untreated hypertension was a much more substantial risk factor for deep ICH: whites (OR 18.98), blacks (OR 20.30), and Hispanics (OR 16.51). In lobar ICH, treated hypertension was a significant risk factor in blacks (OR 1.85), but not in whites (OR 1.18), or Hispanics (OR 1.47), whereas untreated hypertension was a significant risk factor in all three ethnic groups: whites (OR 3.93), blacks (OR 9.21), and Hispanics (OR 6.42). Finally, in patients with infratentorial ICH, treated hypertension was a significant risk factor in Hispanics (OR 7.07), but not in whites (OR 1.53), or blacks (OR 2.28). Untreated hypertension was a significant risk factor for infratentorial ICH in all three ethnic groups: whites (OR 11.64), blacks (5.11), and Hispanics (OR 38.47).
DISCUSSION
We found that both untreated and treated hypertension were significant risk factors for ICH in white, black, and Hispanic patients, with untreated hypertension representing a substantially greater risk. Over a decade ago, we found results similar to the current study for untreated and treated hypertension and concluded that about one fourth of hemorrhagic strokes could be prevented if all hypertensive patients were treated.6 A separate study from the same time period verified that untreated hypertension was a significant risk factor for lobar ICH.7 The current investigation supports the critical role of untreated hypertension as a risk factor for ICH in all three ethnicities, with greater risk noted in blacks and Hispanics compared with whites.
A formal test of interaction between race and hypertension was highly significant, which suggests that untreated hypertension confers a greater ICH risk in blacks and Hispanics relative to whites, or in blacks relative to Hispanics and whites. We acknowledge that the odds ratios for the risk conferred by untreated hypertension for all three groups suggest great risk for all three, but the significant test for interaction and the larger odds ratios do suggest a consistent direction of greater risk in blacks, particularly. Compared with whites, blacks and Hispanics with ICH and a history of hypertension were significantly more likely to have their hypertension untreated. However, after adjusting for medical insurance status there was no longer a significant difference in untreated hypertension for black versus white ICH cases, while a significant difference persisted for Hispanics compared to whites. In a prior report of hypertensive patients, only 58% of uninsured had a blood pressure check within the previous 6 months, compared with 82% of privately insured. Uninsured individuals had lower odds of adequate blood pressure control than privately insured (adjusted odds ratio 0.63, 95% CI 0.44–0.92). Even among individuals treated for hypertension, the uninsured had lower odds of adequate control than privately insured (adjusted odds ratio 0.42, 95% CI 0.23–0.73).15
The enrollment of Hispanics, lacking in prior reports,6, 7 was an important strength of the current study. Survey data from the Pew Research Center found that 45% of Hispanics without a healthcare provider had health insurance.16 The related literature suggests factors in the Hispanic population beyond access to care, such as delay in seeking care and stopping treatments when symptoms resolve, that adversely affect successfully obtaining treatment.17 It has also been noted that Hispanics are less likely to be screened and treated specifically for hypertension.13 Over a 10 year period, despite overall increases in antihypertensive medication use and blood pressure control in adults in the United States, Mexican Americans with hypertension were noted to be less likely to take antihypertensive medication than non-Hispanic whites.14 Improved understanding of factors contributing to antihypertensive treatment adherence in Hispanics is warranted, along with efforts to improve adherence.
Given that white ICH cases were older compared to blacks and Hispanics, we further adjusted the analysis of untreated hypertension rates for age in addition to medical insurance status. In this model the proportion of untreated hypertension in ICH cases was no longer significantly different among the three ethnic/racial groups. Our findings contribute to the larger literature related to persistent ethnic/racial disparities of hypertension diagnosis and treatment, as well as ethnic/racial differences in cardiovascular diseases, including hemorrhagic stroke.
Notably, blacks have an increased risk of ICH at younger ages. The risk of ICH at 45 years of age was more than five times higher for blacks than whites, but only about one third as great for blacks at age 85.11 Similar results were found in a large pooled cohort with over 263,489 person-years of follow-up.10 Over 20 years ago, it was reported that the risk of ICH was 2.3 times higher in blacks than whites for those under 75 years of age,3 and a more recent study found that blacks had 2.90 times greater risk of stroke than whites at 45 years of age, 1.66 times greater risk at 65 years of age, and that about one quarter of the racial disparity in increased stroke risk was attributable to systolic hypertension.18 Because of this increased incidence of ICH at younger ages, blacks have substantial years of life lost and increased years with disability. We also found a significantly lower age for black and Hispanic ICH patients compared with whites. Our results reinforce previous reports and represent a call to action for efforts to mitigate the unrelenting contribution of unrecognized and untreated hypertension in racial/ethnic minorities to stroke disparities.
Our finding that treated hypertension is also a significant risk factor for ICH is consistent with prior literature in stroke,19 and specifically hemorrhagic stroke.6 Though the risk for treated hypertension could be attributed to poor treatment adherence or inadequate control of blood pressure despite treatment, recent evidence suggests that the interaction might be more complex. In a large cohort study of 26,875 black and white patients, it was reported that although pharmacologic treatment to maintain normotensive status markedly reduced risk of stroke, those treated still had higher risk than normotensive individuals who did not require treatment.20 The increased risk for treated hypertension compared with normotension was also found in a study of men with stroke, myocardial infarction, and mortality from coronary artery disease.19 Acknowledgment of a residual risk for treated hypertension, even with normotensive status from that treatment, has provided further evidence for the importance of prevention,20 such as nutritional strategies,21 and the need for ongoing educational efforts related to hypertension.22
We found that treated hypertension was a significant risk factor for ICH in all three ethnic groups. In addition, we found that treated hypertension was a more substantial risk factor in Hispanics (OR 2.5) compared with whites (OR 1.6), and highest overall in blacks (OR 3.0). Blacks have higher rates of treatment resistance to hypertension medications, but the mechanisms of such resistance have not been adequately studied and identified.23 In a large randomized trial of hypertension medication, black women had the lowest blood pressure control rate (59%), whereas non-black men had the highest rate of control (70%).24 Compared with whites, blacks were more likely to be aware of their hypertension (OR 1.31, 95% CI 1.07–1.59), those aware of their hypertension were more likely to be on treatment (OR 1.69, 95% CI 1.40–2.05), but those treated were still less likely to have their blood pressure controlled (OR 0.73, 95% CI 0.64–0.83).9 Using NHANES data from two separate periods, Hertz et al. found that although blood pressure control rates improved in both blacks and whites, there was actually an increase in the ethnic/racial disparity in blood pressure control for those treated, with control of blood pressure in 59.7% of whites but only 48.9% of blacks (p<.001).25 Finally, recent evidence suggests that for a given degree of hypertension, there is a differential stroke risk for blacks vs. whites. Specifically, for each 10 mm Hg increase in systolic blood pressure, there was an 8% increased risk of stroke in whites, but a 24% increased risk in blacks.26 Our test of interaction confirmed that the risk ICH in our cohort did depend on race/ethnicity, consistent with these prior reports. Further research is needed to elucidate the ethnic/racial disparities of mechanisms of hypertension treatment resistance and increased stroke risk.23
Hypertension is the predominant risk factor for deep ICH, while cerebral amyloid angiopathy (CAA) is an important etiology of lobar ICH and more common in the elderly.27 While many studies suggest that hypertension has a less important role in lobar than deep ICH,28 a subgroup analysis of the PROGRESS trial reported that blood pressure treatment is likely to provide protection against all types of ICH, including CAA-related ICH.29 We found that in all three ethnic/racial groups, apart from blacks with untreated hypertension and brainstem/cerebellar ICH, both untreated and treated hypertension conferred less risk for lobar ICH than for all ICH, deep ICH, and brainstem/cerebellar ICH. However, untreated hypertension remained an important risk factor for lobar ICH, particularly in blacks and Hispanics. (Figure, eTable 2).
Limitations of our study include the classification of hypertension based on history as opposed to blood pressure measurements. We also defined treated hypertension as a “history of treatment” without information regarding the blood pressure response to treatment. From the available data, it was not possible to provide an analysis including actual blood pressure values. Given that patient awareness of hypertension is a concern for such a study design, we note an increase in the number of patients aware of their high blood pressure over the past several decades.22 We recognize that patients with untreated hypertension may have had other factors, not identified in our study, which contributed to the increased risk of ICH such as additional comorbidities, variations in access to and quality of medical care, and different treatment adherence behaviors. However, we also note the primacy of hypertension as a risk factor for cardiovascular disease, with improved control of hypertension identified as the most likely factor that has decreased stroke mortality.30
Strengths of our investigation include the multiple centers for recruitment and the multi-ethnic patients studied with large samples sizes, allowing for the analysis of risk factors in whites, blacks, and Hispanics. As a result, we were able to present, as far as we are aware, the first report of treated and untreated hypertension as risk factors for ICH in all three of these ethnic/racial groups. In comparison, randomized trials are not feasible because it is unethical to randomize subjects to non-treatment of hypertension. Also, cohort studies can have difficulty accruing ICH cases, such as a recent study that noted only 62 ICH events despite 156,876 person-years of exposure.11
CONCLUSION
We provide compelling evidence that both treated and untreated hypertension are important risk factors for ICH. Our findings also confirm the importance of untreated hypertension as a risk factor for lobar ICH, particularly in minority populations. There are major ethnic/racial disparities in the proportions of ICH patients with hypertension that receive treatment. Given that untreated hypertension confers a greater ICH risk in blacks and Hispanics relative to whites, accelerated research efforts are needed to improve overall hypertension treatment rates, better define mechanisms of hypertension treatment resistance, particularly in minorities, and to monitor the impact of such efforts on racial/ethnic disparities in stroke.
Supplementary Material
Table 3.
Univariate Analyses for Black ICH Cases and Controls
| Black Cases | Black Controls | OR (95% CI) | p-value | |
|---|---|---|---|---|
| N | 880 | 880 | ||
| Average Age | 58.0 (11.9) | 58.0 (11.8) | Matched | |
| Number Female n (%) | 398 (45.2) | 398 (45.2) | Matched | |
| Diagnosis of Hypertension n (%) | 753 (86.5) | 533 (60.6) | 4.47 (3.42, 5.84) | <0.0001 |
| Treated Hypertension n (%) | 425 (48.9) | 465 (52.9) | 2.75 (2.07, 3.65) | <0.0001 |
| Untreated Hypertension n (%) | 328 (37.7) | 68 (7.7) | 12.83 (8.81, 18.69) | <0.0001 |
| No Diagnosis of Hypertension n (%) | 117 (13.5) | 346 (39.4) | Reference | |
| Heavy alcohol Use | 96 (11.3) | 33 (3.8) | 3.75 (2.39, 5.88) | <0.0001 |
| Hypercholesterolemia | 278 (33.6) | 359 (40.9) | 0.70 (0.57, 0.86) | 0.0007 |
| Anticoagulant Use | 41 (4.7) | 11 (1.3) | 3.73 (1.92, 7.25) | 0.0001 |
| Education Level: n (%) | ||||
| Less than High School | 193 (22.1) | 82 (9.3) | 4.00 (2.93, 5.47) | <0.0001 |
| High School | 315 (36.0) | 196 (22.3) | 2.73 (2.15, 3.47) | <0.0001 |
| Greater than High School | 366 (41.9) | 602 (68.4) | Reference | |
| Medical Insurance Status n (%) | 580 (65.9) | 756 (85.9) | 0.28 (0.21, 0.37) | <0.0001 |
CLINICAL PERSPECTIVE.
What is new?
As the largest case-control study of treated and untreated hypertension as risk factors for intracerebral hemorrhage (ICH), the presented research substantially contributes to this literature and associated ethnic/racial disparities.
We enrolled large numbers of white, black, and Hispanic ICH case-control pairs, thereby having adequate power to also analyze hypertension risk by ICH location, a common limitation of prior studies.
By including Hispanics, often lacking in other investigations, we report novel findings that, like blacks, Hispanics also have increased risk of ICH conferred by treated and untreated hypertension relative to whites.
What are the clinical implications?
This study reinforces the previously reported importance of hypertension as a critical risk factor for ICH.
Our findings also include notable associated ethnic/racial disparities for blacks and Hispanics compared to whites, such as higher rates of untreated hypertension and higher ICH risk conferred by both treated and untreated hypertension.
Clinical implications include a renewed call for hypertension prevention and treatment to reduce ICH risk.
Our results also highlight the importance of efforts to lessen the associated ethnic/racial disparities, including, but not limited to: access to medical care, compliance with prescribed medication regimens, and a better understanding of medication treatment resistance.
Acknowledgments
Sources of Funding:
National Institutes of Health U01-NS069763: Ethnic/Racial Variations in Intracerebral Hemorrhage (ERICH)
Funding to support overall conduct of the study, data collection, management, and analysis
Footnotes
Disclosures: None
Authorship Statement: I, Kyle B. Walsh, had full access to all of the data in the study and I take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das S. Heart disease and stroke statistics--2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–60. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Woo D, Rosand J, Kidwell C, McCauley JL, Osborne J, Brown MW, West SE, Rademacher EW, Waddy S, Roberts JN, Koch S, Gonzales NR, Sung G, Kittner SJ, Birnbaum L, Frankel M, Testai FD, Hall CE, Elkind MS, Flaherty M, Coull B, Chong JY, Warwick T, Malkoff M, James ML, Ali LK, Worrall BB, Jones F, Watson T, Leonard A, Martinez R, Sacco RI, Langefeld CD. The Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study protocol. Stroke. 2013;44:e120–5. doi: 10.1161/STROKEAHA.113.002332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Broderick JP, Brott T, Tomsick T, Huster G, Miller R. The risk of subarachnoid and intracerebral hemorrhages in blacks as compared with whites. N Engl J Med. 1992;326:733–6. doi: 10.1056/NEJM199203123261103. [DOI] [PubMed] [Google Scholar]
- 4.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 5.Dubow J, Fink ME. Impact of hypertension on stroke. Current atherosclerosis reports. 2011;13:298–305. doi: 10.1007/s11883-011-0187-y. [DOI] [PubMed] [Google Scholar]
- 6.Woo D, Haverbusch M, Sekar P, Kissela B, Khoury J, Schneider A, Kleindorfer D, Szaflarski J, Pancioli A, Jauch E, Moomaw C, Sauerbeck L, Gebel J, Broderick J. Effect of untreated hypertension on hemorrhagic stroke. Stroke. 2004;35:1703–8. doi: 10.1161/01.STR.0000130855.70683.c8. [DOI] [PubMed] [Google Scholar]
- 7.Woo D, Kaushal R, Chakraborty R, Woo J, Haverbusch M, Sekar P, Kissela B, Pancioli A, Jauch E, Kleindorfer D, Flaherty M, Schneider A, Khatri P, Sauerbeck L, Khoury J, Deka R, Broderick J. Association of apolipoprotein E4 and haplotypes of the apolipoprotein E gene with lobar intracerebral hemorrhage. Stroke. 2005;36:1874–9. doi: 10.1161/01.STR.0000177891.15082.b9. [DOI] [PubMed] [Google Scholar]
- 8.Odedosu T, Schoenthaler A, Vieira DL, Agyemang C, Ogedegbe G. Overcoming barriers to hypertension control in African Americans. Cleveland Clinic journal of medicine. 2012;79:46–56. doi: 10.3949/ccjm.79a.11068. [DOI] [PubMed] [Google Scholar]
- 9.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, Graham A, Howard V. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke study. Stroke. 2006;37:1171–8. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 10.Sturgeon JD, Folsom AR, Longstreth WT, Jr, Shahar E, Rosamond WD, Cushman M. Risk factors for intracerebral hemorrhage in a pooled prospective study. Stroke. 2007;38:2718–25. doi: 10.1161/STROKEAHA.107.487090. [DOI] [PubMed] [Google Scholar]
- 11.Howard G, Cushman M, Howard VJ, Kissela BM, Kleindorfer DO, Moy CS, Switzer J, Woo D. Risk factors for intracerebral hemorrhage: the REasons for geographic and racial differences in stroke (REGARDS) study. Stroke. 2013;44:1282–7. doi: 10.1161/STROKEAHA.111.000529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ariesen MJ, Claus SP, Rinkel GJ, Algra A. Risk factors for intracerebral hemorrhage in the general population: a systematic review. Stroke. 2003;34:2060–5. doi: 10.1161/01.STR.0000080678.09344.8D. [DOI] [PubMed] [Google Scholar]
- 13.Viruell-Fuentes EA, Ponce NA, Alegria M. Neighborhood context and hypertension outcomes among Latinos in Chicago. Journal of immigrant and minority health/Center for Minority Public Health. 2012;14:959–67. doi: 10.1007/s10903-012-9608-4. [DOI] [PubMed] [Google Scholar]
- 14.Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126:2105–14. doi: 10.1161/CIRCULATIONAHA.112.096156. [DOI] [PubMed] [Google Scholar]
- 15.Duru OK, Vargas RB, Kermah D, Pan D, Norris KC. Health insurance status and hypertension monitoring and control in the United States. American journal of hypertension. 2007;20:348–53. doi: 10.1016/j.amjhyper.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 16.Hispanics and Healthcare in the United States: Access, Information, and Knowledge. Pew Research Center; Washington D.C: Aug 13, 2008. http://www.pewhispanic.org/2008/08/13/hispanics-and-health-care-in-the-united-states-access-information-and-knowledge/ [Google Scholar]
- 17.Hispanics and Heart Disease, Stroke. American Heart Association; Jul, 2015. http://www.heart.org/HEARTORG/Conditions/More/MyHeartandStrokeNews/Hispanics-and-Heart-Disease-Stroke_UCM_444864_Article.jsp#.VqNItIUrLDd. [Google Scholar]
- 18.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, Rhodes JD, Soliman EZ, Moy CS, Judd SE, Howard VJ. Traditional risk factors as the underlying cause of racial disparities in stroke: lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–75. doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Almgren T, Persson B, Wilhelmsen L, Rosengren A, Andersson OK. Stroke and coronary heart disease in treated hypertension -- a prospective cohort study over three decades. Journal of internal medicine. 2005;257:496–502. doi: 10.1111/j.1365-2796.2005.01497.x. [DOI] [PubMed] [Google Scholar]
- 20.Howard G, Banach M, Cushman M, Goff DC, Howard VJ, Lackland DT, McVay J, Meschia JF, Muntner P, Oparil S, Rightmyer M, Taylor HA. Is blood pressure control for stroke prevention the correct goal? The lost opportunity of preventing hypertension. Stroke. 2015;46:1595–600. doi: 10.1161/STROKEAHA.115.009128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47:296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- 22.Jones DW, Hall JE. The national high blood pressure education program: thirty years and counting. Hypertension. 2002;39:941–2. doi: 10.1161/01.hyp.0000018303.61360.28. [DOI] [PubMed] [Google Scholar]
- 23.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–26. doi: 10.1161/CIRCULATIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 24.Cushman WC, Ford CE, Cutler JA, Margolis KL, Davis BR, Grimm RH, Black HR, Hamilton BP, Holland J, Nwachuku C, Papademetriou V, Probstfield J, Wright JT, Jr, Alderman MH, Weiss RJ, Piller L, Bettencourt J, Walsh SM. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT) Journal of clinical hypertension (Greenwich, Conn) 2002;4:393–404. doi: 10.1111/j.1524-6175.2002.02045.x. [DOI] [PubMed] [Google Scholar]
- 25.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Archives of internal medicine. 2005;165:2098–104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 26.Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, Safford MM, Cushman M, Glasser SP, Howard VJ. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA internal medicine. 2013;173:46–51. doi: 10.1001/2013.jamainternmed.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woo D, Sauerbeck LR, Kissela BM, Khoury JC, Szaflarski JP, Gebel J, Shukla R, Pancioli AM, Jauch EC, Menon AG, Deka R, Carrozzella JA, Moomaw CJ, Fontaine RN, Broderick JP. Genetic and environmental risk factors for intracerebral hemorrhage: preliminary results of a population-based study. Stroke. 2002;33:1190–5. doi: 10.1161/01.str.0000014774.88027.22. [DOI] [PubMed] [Google Scholar]
- 28.Rosand J, Greenberg SM. Beyond hypertension: unraveling the causes of intracerebral hemorrhage. Stroke. 2002;33:1195–6. [PubMed] [Google Scholar]
- 29.Arima H, Tzourio C, Anderson C, Woodward M, Bousser MG, MacMahon S, Neal B, Chalmers J. Effects of perindopril-based lowering of blood pressure on intracerebral hemorrhage related to amyloid angiopathy: the PROGRESS trial. Stroke. 2010;41:394–6. doi: 10.1161/STROKEAHA.109.563932. [DOI] [PubMed] [Google Scholar]
- 30.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, Kissela BM, Kittner SJ, Lichtman JH, Lisabeth LD, Schwamm LH, Smith EE, Towfighi A. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45:315–53. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


