Abstract
Objectives
Family caregivers (FCGs) play an important role in the quality of life (QOL) of lung cancer patients. FCGs experience significant psychological distress related to their caregiving role, but there is relatively little data about FCG QOL after cancer surgery. We sought to describe QOL trajectories for patients and their FCGs after lung cancer surgery.
Methods
This is a secondary analysis of a larger, prospective QOL study, testing the effectiveness of an interdisciplinary palliative care intervention for lung cancer patients and FCGs in a single institution. The intervention included interdisciplinary care planning and formal education sessions for both patients and FCGs. This subset analysis included patients who underwent surgery and had a matching FCG with complete QOL data (41 pairs of patients and caregivers out of 112 surgical patients). Patient QOL was assessed with the Functional Assessment of Cancer Therapy-Lung tool. FCG QOL was assessed with the FCG version of the City of Hope QOL tool. Psychological distress was assessed using the Distress Thermometer.
Results
Psychological distress levels were highest for patients (3.8/10) and FCGs (5.1/10) before surgery. Distress levels decreased among patients at six (2.9/10) and 12 weeks (2.2/10, p = .001) later, but remained elevated among FCGs (4.2/10 and 4.4/10, p = 0.157). Compared with usual care, patients in the intervention group reported improved physical and functional QOL outcomes at 12 weeks (p < .01), but there was no significant benefit seen for FCGs in any domain (p > .05).
Conclusions
FCGs of lung cancer patients experience significant psychological distress. FCGs continue to have impaired QOL 3 months after surgery. The trajectory of QOL for FCGs does not mirror that of patients. Our palliative care intervention showed improved QOL outcomes for this subset of patients but was not effective for their FCGs.
Trial Registration
NCI sponsored, trial identifier NCT00823667 https://clinicaltrials.gov/show/NCT00823667.
Keywords: Quality of Life, Lung Cancer, Family Caregiver, Surgery, Psychological Distress
Introduction
Due to changes in the healthcare environment as well as advances in surgical care, patients are discharged from the hospital earlier and earlier following major surgery. This is despite an aging population with greater comorbidities. As such, a greater proportion of the caregiver burden has fallen on informal family caregivers (FCGs).1 Previous studies have demonstrated that FCGs of cancer patients experience decreased quality of life (QOL) and psychological distress related to their caregiver role.2
Lung cancer patients often require significant care due to extensive comorbidities. The median age at lung cancer diagnosis is 70.3 Chronic obstructive pulmonary disease (COPD) and other smoking related illnesses are common.4 Patients with lung cancer report greater levels of psychological distress than other types of cancer.5 Baseline quality of life in these patients is often significantly lower than the general population.6 These issues may be exacerbated by side effects of treatments. There is extensive data illustrating the significant impact of pulmonary resection on patient QOL.7 In the period immediately following surgery for lung cancer, patients experience pain, fatigue, and decreased physical function. It may take patients three months or longer to regain physical quality of life.8
There is an increasing awareness of the importance of FCGs in helping patients cope with cancer. A number of studies have examined interventions for FCGs of cancer patients.9 Psychological, informational, and group interventions have all demonstrated varying degrees of improvements in FCG QOL and caregiver burden. There is relatively little data about interventions specific for FCGs of patients with lung cancer and there is even less information about surgical patients.
In order to further investigate the effect of lung cancer surgery on QOL of patients and FCGs, we performed a subset analysis of data collected as part of a broader National Cancer Institute-supported Program Project investigating an interdisciplinary palliative care intervention for patients with lung cancer and their FCGs.10, 11
Methods
Study Design
This paper presents secondary analysis of QOL, symptoms, and psychological distress data for surgically-treated patients and their FCGs in an NCI-supported Program Project that tested the effectiveness of an interdisciplinary palliative care intervention in lung cancer. The study was a prospective, quasi-experimental trial with a tandem enrollment design where enrollment into the usual care group occurred first, followed by the intervention group. FCG enrollment occurred at the time a matching patient was consented. The palliative care intervention consisted of a comprehensive baseline QOL assessment for both patients and FCGs, interdisciplinary care planning, and four education sessions by a research nurse provided to the patient and four sessions separately provided for the FCG. Interdisciplinary care plans were developed in a weekly meeting attended by thoracic surgeons, medical oncologists, nurses, pain specialists, pulmonologist, physical therapist, social worker, chaplain, dietitian, physical therapist, and other members of the research team. Care planning included recommendations for symptom management and supportive-care referrals for patients and available community resources for FCGs. Accrual occurred between November 2009 and August 2014, with data collection ending in September 2014. The study was performed at an NCI-designated Comprehensive Cancer Center located in Southern California. All study protocols, procedures, and data safety monitoring plan were approved by the institutional review board.
Participants
For this analysis, we included survivors that met the following inclusion criteria: 1) those with histologic diagnosis of stage I-III resectable NSCLC; 2) age 18 years or older; 3) underwent curative intent surgery; 4) had no previous history of cancer within three years of enrollment; 5) completed baseline assessments preoperatively; and 6) had a matching FCG enrolled in the study. An FCG refers to either a family member or friend identified by the patient as being the primary caregiver. All participants completed written informed consent prior to study participation.
Patient-Reported Outcome Measures
Quality of life and symptoms were assessed using the Functional Assessment of Cancer Therapy-Lung (FACT-L) tool. The FACT-L contains 27 items with questions divided into the physical, social/family, emotional, and functional well-being domains. An additional lung cancer subscale (LCS) is included to assess disease-specific symptoms. All items are scored on a 5-point Likert scale (0=not at all; 4=very much). Higher scores indicate better QOL, and the total score ranges from 0 to 140.12 The Functional Assessment of Chronic Illness Therapy-Spirituality Subscale (FACIT-Sp-12) was used to assess spiritual well-being. This is a 12-item, 5-point Likert scale measure that assesses sense of meaning, peace, and faith in illness. Total score ranges from 0 to 48, and higher score indicate better spiritual well-being.13 Psychological distress was assessed using the Distress Thermometer (DT). The DT is an efficient, low burden method to evaluate distress, based on a scale of 0 to 10 (0=no distress; 10=extreme distress).14 Demographic and health status data (age, gender, race/ethnicity, education level, marital status, living situation, employment, religious preference, annual household income, co-morbidities, smoking history) were self-reported by patients at baseline. Disease and treatment characteristics, including stage of disease and type of surgical procedure were obtained through electronic medical records (EMR). All survivors completed baseline assessments prior to surgery, and were re-assessed at 6 and 12 weeks following surgery.
Family Caregiver-Reported Outcome Measures
FCG QOL was assessed using the FCG version of the City of Hope QOL Tool (COH-QOL-FCG). This is a 37 item instrument that measures FCG QOL in the physical, psychological, social, and spiritual well being domains. Items are rated on a 1–10 scale, with higher scores representing worse QOL. The test-retest reliability was r=.89 and internal consistency was alpha r=.69.15 Perceived caregiving skills preparedness was assessed using Archbold’s Caregiving Preparedness Scale. This eight-item scale evaluates FCG’s comfort with the physical and emotional patient needs and are scored from 0 to 4, with higher scores representing better preparedness. Internal consistency ranges from 0.88 to 0.93.16 The Distress Thermometer was also used to assess psychological distress for FCGs.17 FCGs completed baseline assessments prior to surgery, and were re-assessed at 7 and 12 weeks following surgery.
Statistical Analysis
Data were analyzed using the Statistical Package for the Social Sciences, v. 21. (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.) Scores were computed for study outcome scales and subscales. Descriptive statistics were computed on baseline, 6- and 12-week data (the primary end-point of the studies) for all outcome variables. Repeated measures Analysis of Variance (RMANOVA) was conducted over time for patient and FCG outcomes in order to understand the trajectory from pre-op to immediate post-op to longer term outcomes related to having surgery for early stage lung cancer. Differences in outcomes measures were tested using factorial analysis of covariance controlling for baseline scores. Means were adjusted for baseline scores as covariates.
Results
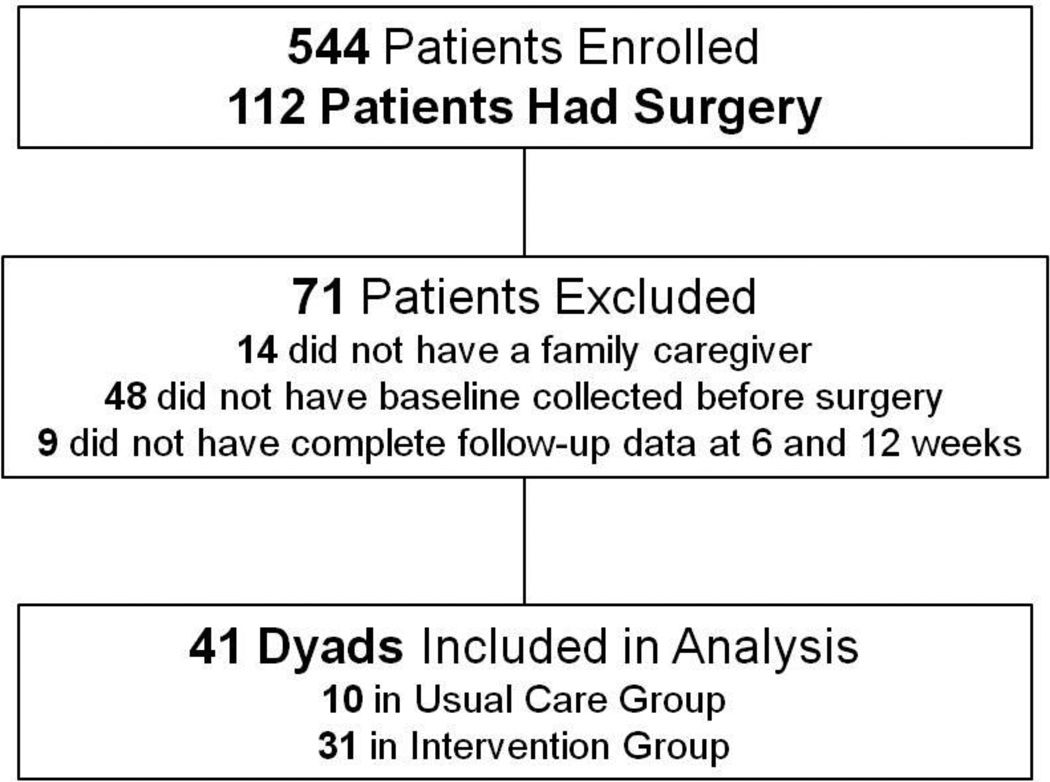
A total of 544 patients and 366 FCGs were enrolled in the study, and 112 patients underwent surgery. Because the purpose of this analysis was to describe the impact of lung cancer surgery on patients and their FCGs, we chose to only include patients who underwent surgical resection for their lung cancer, had a designated FCG, had baseline data that were collected before surgery, and had complete follow-up data (complete QOL surveys at all time points) after surgery. Based on these criteria, 41 pairs of patients and FCGs (N=82; 20 usual care, 62 intervention) were included in the analysis (Figure 1). The majority of both patients and FCGs were women (56% and 59%). The majority of patients (23/41, 56%) underwent thoracoscopic surgery and nearly all underwent lobectomy or bilobectomy (40/41, 98%). Table 1 presents sociodemographic and clinical characteristics for patients and FCGs.
Figure 1. Patient and Family Caregiver Dyads with complete pre-operative and post-operative QOL data were included in this analysis.
Table 1.
Sociodemographic and Clinical Characteristics
| Characteristic | Patients (N = 41) | Family Caregivers (N = 41) | ||
|---|---|---|---|---|
| N | % | N | % | |
| Age (mean ± SD) | 67 ± 13 | 61 ± 14 | ||
| Female | 23 | 56 | 24 | 59 |
| Usual Care | 10 | 24 | 10 | 24 |
| Intervention | 31 | 76 | 31 | 76 |
| Race/Ethnicity | ||||
| Asian | 1 | 2 | 3 | 7 |
| Black | 1 | 2 | 1 | 2 |
| Latino | 3 | 7 | 4 | 10 |
| White | 36 | 88 | 36 | 78 |
| Other/Mixed | 1 | 2 | ||
| Religion | ||||
| Protestant | 18 | 44 | 19 | 46 |
| Catholic | 9 | 22 | 9 | 22 |
| Jewish | 1 | 2 | 4 | 10 |
| None | 10 | 24 | 7 | 17 |
| Other | 3 | 7 | 1 | 2 |
| Married/Partnered | 33 | 81 | 35 | 85 |
| Relationship to Patient | ||||
| Spouse/partner | 30 | 73 | ||
| Child | 8 | 20 | ||
| Other | 3 | 7 | ||
| Cancer Stage | ||||
| I | 19 | 46 | ||
| II | 12 | 29 | ||
| III | 10 | 24 | ||
| Surgery Type | ||||
| Open | 18 | 44 | ||
| Thoracoscopic | 23 | 56 | ||
| Lobectomy/Bilobectomy | 40 | 98 | ||
| Wedge | 1 | 2 | ||
Psychological Distress Trajectories
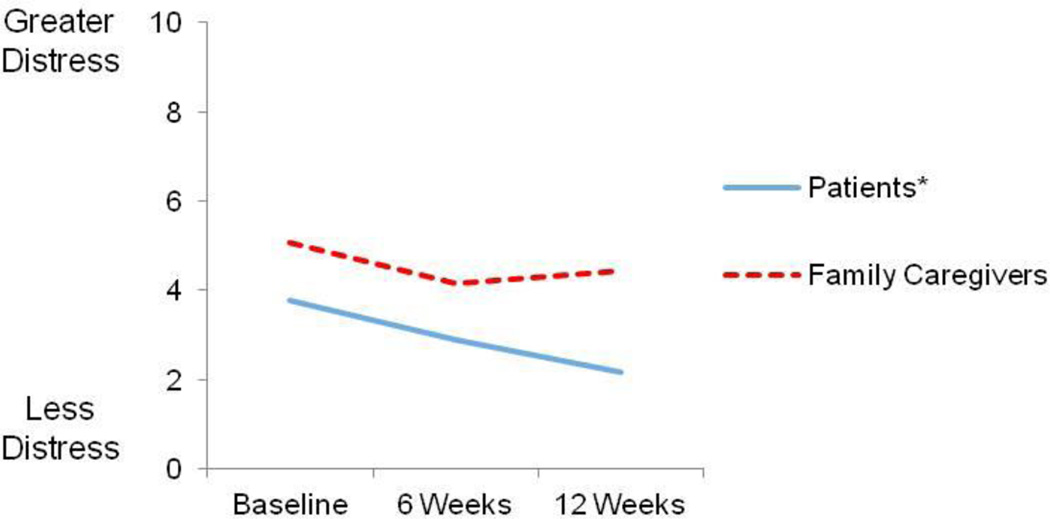
Both patients and FCGs reported significant baseline psychological distress (Figure 2). Mean distress levels were highest for patients (3.8/10) and FCGs (5.1/10) before surgery, then decreased six weeks after surgery for both groups respectively (2.9/10 and 4.2/10). Patients’ mean distress scores continued to decrease at 12 weeks to a relatively low level (2.2/10, p = .001), but FCGs distress did not improve from six to 12 weeks (4.4/10, p = .157).
Figure 2. Patient and Family Caregiver Psychological Distress Over Time.
Possible scores range from 0 to 10. * p < .05.
Quality of Life Trajectories
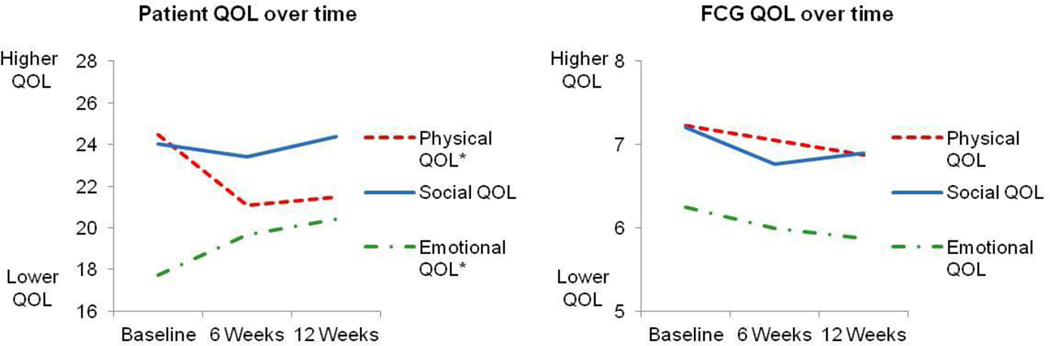
As seen in Figure 3, mean patient emotional QOL scores improved from a baseline of 17.7±4.9 before surgery to 19.7±4.1 six weeks after surgery and continued to improve at 12 weeks after surgery (20.4±3.5, p = .001). Mean physical and social QOL declined immediately after surgery, but improved from 6 to 12 weeks (p = .001 and 0.581 respectively).
Figure 3. Patient and FCG QOL trajectories.
Patient physical and social QOL possible scores range from 0 to 28, emotional QOL from 0 to 24. FCG QOL possible scores range from 0 to 10. * p < .05
In contrast, FCGs did not experience statistically significant changes in their QOL scores and their overall trajectories were different than the patient QOL trajectories, as shown in Figure 3. Unlike the patients, FCG mean emotional QOL scores did not improve after surgery (6.2±1.4, 6.0±1.3, and 5.9±1.2 at baseline, six weeks, and 12 weeks after surgery, p = 0.2). Likewise, although not statistically significant, there was a downward trend for both physical QOL among FCGs (p = 0.3). Social QOL scores had similar trajectories for both patients and FCGs, without statistically significant changes during the study period (p = 0.58 and 0.12 respectively). Spiritual QOL among FCGs also did not significantly change from baseline to 12 weeks (mean 6.5 ± 1.4 to mean 6.4 ± 1.4, p = 0.28).
Caregiver preparedness scores in this group were relatively high at baseline (mean 3.8/4 ± 0.7, mean ± SD) and remained high at 6 weeks (mean 3.7/4 ± 0.8) and 12 weeks (mean 3.8/4 ± 0.7), with no significant changes throughout the study period (p=0.72). There were also no significant differences in preparedness scores between the usual care and intervention groups.
Intervention
The interdisciplinary palliative care intervention appeared to have a greater impact on patients than FCGs. At 12 weeks, patients in the intervention group reported significantly better physical and functional QOL compared to patients in the usual care group, along with better scores on the lung cancer subscale (Table 2). However, there were no significant differences in QOL scores between the usual care group and intervention group for FCGs (Table 3).
Table 2.
Patient Outcomes at 12 weeks.
| Outcome | Usual Care (N=10) | Intervention (N = 31) |
P valuea |
||
|---|---|---|---|---|---|
| Mean ± SD |
Adjusted Mean |
Mean ± SD |
Adjusted Mean |
||
| Physical QOLb | 14.9 ± 8.1 | 15.3 | 23.6 ± 3.1 | 23.5 | < .01 |
| Social QOLb | 22.4 ± 5.3 | 22.7 | 25.0 ± 4.3 | 24.9 | 0.21 |
| Emotional QOLc | 18.2 ± 3.7 | 18.7 | 21.2 ± 3.2 | 20.9 | 0.08 |
| Functional QOLb | 15.0 ± 5.0 | 16.1 | 20.0 ± 3.5 | 19.6 | < .01 |
| Lung Cancer Subscaled |
20.4 ± 4.8 | 21.3 | 27.2 ± 3.8 | 26.9 | < .01 |
QOL indicates quality of life; SD, standard deviation.
These are the P values for the main effect of group.
Possible scores range from 0 to 28, with higher scores indicating better QOL.
Possible scores range from 0 to 24, with higher scores indicating better QOL.
Possible scores range from 0 to 24, with higher scores indicating better QOL.
Table 3.
Family Caregiver Outcomes at 12 weeks.
| Usual Care (N = 10) | Intervention (N = 31) | ||||
|---|---|---|---|---|---|
| Outcome | Mean ± SD | Adjusted Mean | Mean ± SD | Adjusted Mean | P valuea |
| Physical QOLb | 7.2 ± 1.4 | 6.8 | 6.8 ± 2.0 | 6.9 | 0.87 |
| Social QOLb | 6.2 ± 2.1 | 6.3 | 7.1 ± 1.1 | 7.1 | 0.09 |
| Emotional QOLb | 5.7 ± 1.9 | 5.8 | 5.9 ± 0.9 | 5.9 | 0.85 |
| Functional QOLb | 6.2 ± 1.3 | 6.3 | 6.5 ± 1.4 | 6.5 | 0.70 |
QOL indicates quality of life; SD, standard deviation.
These are the P values for the main effect of group.
Possible scores range from 0 to 10, with higher scores indicating better QOL.
Discussion
Patients experience psychological distress and decreased QOL related to lung cancer and its surgical treatment. Although much is known about patient outcomes after thoracic surgery, much less is known about FCGs. In this subset analysis of a palliative care intervention for lung cancer patients and their FCGs, we found that the QOL trajectories of FCGs did not necessarily mirror that of patients. Patients’ emotional QOL improved after surgery and continued to improve from six to 12 weeks, whereas FCGs did not have any improvement in emotional QOL. Patients’ physical QOL declined in the first six weeks after surgery, but improved slightly from six to 12 weeks. FCGs physical QOL remained relatively stable throughout the time period.
Interestingly, FCG reported greater levels of psychological distress compared to patients, indicating that it may be more distressing to have a loved one experience illness than to experience an illness for oneself. The patients in our study had relief of psychological distress after surgery, which is similar to what other studies have found, despite increased fatigue and decreased physical QOL.18 It is unclear why FCGs did not experience similar relief of psychological distress after surgery and why emotional QOL did not improve, as it did for patients. Dissimilarity in distress between cancer patients and caregivers is not an unusual finding. Others have reported significant incongruence between patient and family member perceptions of patient symptoms, with family members tending to rate physical function worse than patients.19, 20 Kim and colleagues found significant dissimilarity in psychological distress between cancer patients and caregivers.21 They also reported that partner’s distress levels as well as dissimilarity in distress of the couple played important roles in one’s QOL. It may be distressing for FCGs to witness the significant decline in patients’ physical functioning. FCGs may also be experiencing greater caregiver burden due to the decline in patient physical function, which may in turn impact their own level of psychological distress and emotional QOL.
Alternatively, these results may simply be a reflection of the relative efficacy of the palliative care intervention for patients vs. the intervention for FCGs. In this subset analysis, patients in the intervention group reported better QOL at 12 weeks compared to the usual care group, but there was no difference between groups for FCGs. In the larger study, which included non-operative patients, we did find that FCGs who received the intervention had better QOL than those that received usual care, so it may be possible that the FCG intervention was not as effective for FCGs of surgical patients. One randomized clinical trial of caregiver-assisted coping skills training for lung cancer found that the training was more beneficial to patients with Stage II and III cancer, whereas an education and support intervention was more helpful for patients/caregivers with Stage I cancer, which likely included a higher percentage of patients undergoing surgery and a lower percentage of patients receiving chemotherapy.22 In the postoperative setting, patients experience abrupt decreases in their functional capacity as opposed to the more gradual decline that non-surgical patients often experience. The FCG education sessions and care plans may not have adequately prepared FCGs for the post-operative caregiving. It is clear that we need better information about the unique stressors for FCGs during this period, so we can better prepare FCGs for the demands of caregiving after surgery.
The data should be interpreted with the understanding that this was an unplanned subset analysis. The results reflect a relatively small number of patients who were part of the larger cohort. In addition, it is unclear how combining data from the intervention and usual care groups may have influenced the results. The incongruity we found between patient and FCG QOL may have been more a reflection of the relative impact of the intervention on the different populations. Also, the relatively small samples sizes prevented us from doing a more detailed analysis of possible interaction effects. However, the results are in general agreement with previous studies that have shown incongruity between patient and FCG QOL assessment and may be valuable in guiding the direction of future research in this area. Qualitative studies may help identify specific aspects of the intervention that may be more impactful for FCGs. Larger studies could also potentially help identify sub-groups of FCGs who may require more support as well as sub-groups that may respond better to QOL interventions.
HIGHLIGHTS.
Family caregivers of lung cancer patients experience significant psychological distress.
Patients report improved emotional quality of life after lung cancer surgery.
Family caregivers did not have similar improvement in quality of life.
Acknowledgments
The research described was supported by grant P01 CA136396 from the National Cancer Institute. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute or NIH.
The authors thank Gwen Uman, PhD for assistance with statistical analysis and consultation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no relevant conflicts of interest to declare.
References
- 1.Chambers A, Routledge T, Pilling J, Scarci M. In elderly patients with lung cancer is resection justified in terms of morbidity, mortality and residual quality of life? Interact Cardiovasc Thorac Surg. 2010 Jun;10(6):1015–1021. doi: 10.1510/icvts.2010.233189. [DOI] [PubMed] [Google Scholar]
- 2.Fujinami R, Otis-Green S, Klein L, Sidhu R, Ferrell B. Quality of life of family caregivers and challenges faced in caring for patients with lung cancer. Clin J Oncol Nurs. 2012 Dec;16(6):E210–E220. doi: 10.1188/12.CJON.E210-E220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howlader NNA, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, editors. SEER Cancer Statistics Review, 1975–2012. Bethesda, MD: National Cancer Institute; 2015. http://seer.cancer.gov/csr/1975_2012/ [Google Scholar]
- 4.Samson P, Robinson CG, Bradley J, et al. The National Surgical Quality Improvement Program risk calculator does not adequately stratify risk for patients with clinical stage I non-small cell lung cancer. J Thorac Cardiovasc Surg. 2015 Aug 24; doi: 10.1016/j.jtcvs.2015.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001 Jan-Feb;10(1):19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 6.Visser MR, van Lanschot JJ, van der Velden J, Kloek JJ, Gouma DJ, Sprangers MA. Quality of life in newly diagnosed cancer patients waiting for surgery is seriously impaired. J Surg Oncol. 2006 Jun 1;93(7):571–577. doi: 10.1002/jso.20552. [DOI] [PubMed] [Google Scholar]
- 7.Poghosyan H, Sheldon LK, Leveille SG, Cooley ME. Health-related quality of life after surgical treatment in patients with non-small cell lung cancer: a systematic review. Lung Cancer. 2013 Jul;81(1):11–26. doi: 10.1016/j.lungcan.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Win T, Sharples L, Wells FC, Ritchie AJ, Munday H, Laroche CM. Effect of lung cancer surgery on quality of life. Thorax. 2005 Mar;60(3):234–238. doi: 10.1136/thx.2004.031872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harding R, List S, Epiphaniou E, Jones H. How can informal caregivers in cancer and palliative care be supported? An updated systematic literature review of interventions and their effectiveness. Palliat. Med. 2012 Jan;26(1):7–22. doi: 10.1177/0269216311409613. [DOI] [PubMed] [Google Scholar]
- 10.Raz DJ, Sun V, Kim JY, et al. Long-Term Effect of an Interdisciplinary Supportive Care Intervention for Lung Cancer Survivors After Surgical Procedures. Ann Thorac Surg. 2016 Feb;101(2):495–503. doi: 10.1016/j.athoracsur.2015.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrell B, Sun V, Hurria A, et al. Interdisciplinary Palliative Care for Patients With Lung Cancer. J Pain Symptom Manage. 2015 Dec;50(6):758–767. doi: 10.1016/j.jpainsymman.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P. Reliability and validity of the Functional Assessment of Cancer Therapy-Lung (FACT-L) quality of life instrument. Lung Cancer. 1995 Jun;12(3):199–220. doi: 10.1016/0169-5002(95)00450-f. [DOI] [PubMed] [Google Scholar]
- 13.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp) Ann Behav. Med. 2002 Winter;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 14.Graves KD, Arnold SM, Love CL, Kirsh KL, Moore PG, Passik SD. Distress screening in a multidisciplinary lung cancer clinic: prevalence and predictors of clinically significant distress. Lung Cancer. 2007 Feb;55(2):215–224. doi: 10.1016/j.lungcan.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrell BR, Grant M, Chan J, Ahn C, Ferrell BA. The impact of cancer pain education on family caregivers of elderly patients. Oncol Nurs Forum. 1995 Sep;22(8):1211–1218. [PubMed] [Google Scholar]
- 16.Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Res Nurs Health. 1990 Dec;13(6):375–384. doi: 10.1002/nur.4770130605. [DOI] [PubMed] [Google Scholar]
- 17.Zwahlen D, Hagenbuch N, Carley MI, Recklitis CJ, Buchi S. Screening cancer patients' families with the distress thermometer (DT): a validation study. Psychooncology. 2008 Oct;17(10):959–966. doi: 10.1002/pon.1320. [DOI] [PubMed] [Google Scholar]
- 18.Oh S, Miyamoto H, Yamazaki A, et al. Prospective analysis of depression and psychological distress before and after surgical resection of lung cancer. Gen Thorac Cardiovasc Surg. 2007 Mar;55(3):119–124. doi: 10.1007/s11748-006-0084-4. [DOI] [PubMed] [Google Scholar]
- 19.Lyons KS, Lee CS, Bennett JA, et al. Symptom incongruence trajectories in lung cancer dyads. J Pain Symptom Manage. 2014 Dec;48(6):1031–1040. doi: 10.1016/j.jpainsymman.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Lobchuk MM, Kristjanson L, Degner L, Blood P, Sloan JA. Perceptions of symptom distress in lung cancer patients: I. Congruence between patients and primary family caregivers. J Pain Symptom Manage. 1997 Sep;14(3):136–146. doi: 10.1016/s0885-3924(97)00022-5. [DOI] [PubMed] [Google Scholar]
- 21.Kim Y, Kashy DA, Wellisch DK, Spillers RL, Kaw CK, Smith TG. Quality of life of couples dealing with cancer: dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Ann Behav. Med. 2008 Apr;35(2):230–238. doi: 10.1007/s12160-008-9026-y. [DOI] [PubMed] [Google Scholar]
- 22.Porter LS, Keefe FJ, Garst J, et al. Caregiver-assisted coping skills training for lung cancer: results of a randomized clinical trial. J Pain Symptom Manage. 2011 Jan;41(1):1–13. doi: 10.1016/j.jpainsymman.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]