Abstract
Issue: The estimation of foetal weight is an integral part of prenatal care and obstetric routine. In spite of its known susceptibility to errors in cases of underweight or overweight babies, important obstetric decisions depend on it. In the present contribution we have examined the accuracy and error distribution of 35 weight estimation formulae within the normal weight range of 2500–4000 g. The aim of the study was to identify the weight estimation formulae with the best possible correspondence to the requirements of clinical routine.
Materials and Methods: 35 clinically established weight estimation formulae were analysed in 3416 foetuses with weights between 2500 and 4000 g. For this we determined and compared the mean percentage error (MPE), the mean absolute percentage error (MAPE), and the proportions of estimates within the error ranges of 5, 10, 20 and 30 %. In addition, separate regression lines were calculated for the relationship between estimated and actual birth weights for the weight range 2500–4000 g. The formulae were thus examined for possible inhomogeneities.
Results: The lowest MPE were achieved with the Hadlock III and V formulae (0.8 %, STW 9.2 % or, respectively, −0.8 %, STW 10.0 %). The lowest absolute error (6.6 %) as well as the most favourable frequency distribution in cases below 5 % and 10 % error (43.9 and 77.5) were seen for the Halaska formula. In graphic representations of the regression lines, 16 formulae revealed a weight overestimation in the lower weight range and an underestimation in the upper range. 14 formulae gave underestimations and merely 5 gave overestimations over the entire tested weight range.
Conclusion: The majority of the tested formulae gave underestimations of the actual birth weight over the entire weight range or at least in the upper weight range. This result supports the current strategy of a two-stage weight estimation in which a formula is first chosen after a pre-estimation of the weight range.
Key words: biometry, foetal weight estimation, regression formula
Zusammenfassung
Fragestellung: Die fetale Gewichtsschätzung ist integraler Bestandteil der Schwangerenvorsorge und des geburtshilflichen Alltags. Trotz ihrer bei unter- und übergewichtigen Kindern bekannten Fehleranfälligkeit, hängen wichtige geburtshilfliche Entscheidungen von ihr ab. In der vorliegenden Arbeit wird die Genauigkeit und die Fehlerverteilung von 35 Gewichtsformeln innerhalb des normalen Gewichtsbereichs von 2500–4000 g untersucht. Ziel der Untersuchung war es, Gewichtsformeln zu finden, die den Anforderungen des klinischen Alltags bestmöglich entsprechen.
Material und Methodik: 35 klinisch etablierte Gewichtsschätzformeln wurden an 3416 Feten mit einem Gewicht zwischen 2500 und 4000 g analysiert. Hierbei wurden der mittlere prozentuale Fehler (MPF), der mittlere absolute prozentuale Fehler (MAPF), der Anteil der Schätzungen innerhalb eines Fehlerbereichs von 5, 10, 20 und 30 % ermittelt und verglichen. Darüber hinaus wurden für den Zusammenhang von Schätz- zu tatsächlichem Geburtsgewicht getrennte Regressionsgeraden für den Gewichtsbereich 2500–4000 g berechnet. Die Formeln wurden somit auf eine mögliche Inhomogenität überprüft.
Ergebnisse: Der kleinste MPF wurde mittels den Hadlock-III- und -V-Formeln erzielt (0,8 %, STW 9,2 % bzw. −0,8 %, STW 10,0 %). Den geringsten absoluten Fehler (6,6 %) sowie die günstigste Häufigkeitsverteilung bei Fällen unter 5 % und 10 % Fehler (43,9 und 77,5) wies die Halaska-Formel auf. In der grafischen Darstellung der Regressionsgeraden zeigen 16 Formeln eine Gewichtsüberschätzung im unteren Gewichtsbereich und eine -unterschätzung im oberen Bereich. 14 Formeln unterschätzen und lediglich 5 Formeln überschätzen über den getesteten Gewichtsbereich.
Schlussfolgerung: Die Mehrheit der Formeln unterschätzt im vollständigen oder zumindest oberen Gewichtsbereich das tatsächliche Geburtsgewicht. Die Ergebnisse unterstützen aktuelle Ansätze eines 2-stufigen Vorgehens der Gewichtsschätzung, bei der die Formel erst nach Voreinschätzung des Gewichtsbereichs gewählt wird.
Schlüsselwörter: Biometrie, fetale Gewichtsschätzung, Regressionsformel
Introduction
For almost 4 decades foetal biometrics have been an integral part of established prenatal care according to maternity policy guidelines. Besides bodily integrity, biometry serves to estimate foetal weight and thus the age-appropriate development. While the first formulae for weight estimation were based solely on measurement of the biparietal diameter (BPD), the further development of numerous formulae based on combinations of biometric markers then led to an advantage over clinical estimation methods such as inspection and palpation 1, 2, 3, 4, 5.
For the great majority of weight estimation formulae it holds that they have been developed by means of regression analyses based on relatively small collectives of average term infants. The mean percentage error (MPE) as well as the mean absolute percentage error (MAPE) of the formulae depend on the weight itself. It is thus not surprising both for underweight infants or, respectively, pre-term infants as well as for infants with macrosomia, that the weight estimations can exhibit a clinically relevant error susceptibility 6, 7, 8. However, it is just this delineation of the normal weight collective from the abnormally under- or overweight fetuses that is of decisive importance for the prenatal and obstetric management. Interuterine growth retardation as well as macrosomia carry significant risks for not only neonatal but also for maternal morbidity and mortality 9, 10, 11. A differentiation from the normal collective can only be made when at least the weight estimation can reliably be classified in this range. The spread of this weight range with 2500 to 4000 g is, however, considered to be very wide. It is thus of interest as to which weight estimation formula exhibits not only the lowest but also the most stable errors within this range or, respectively, the largest independence on the weight range of the infant.
Accordingly, in this study we have examined by means of linear regressions how and to what extent deviations between the estimated weight and the actual birth weight in the range 2500 to 4000 g vary and which estimation formula exhibits the lowest constant estimation error in this situation.
Materials and Methods
Description of the study collective
For this retrospective study the perinatal database of the Department of Obstetrics and Gynecology at the University of Tübingen was searched for live births with a birth weight between 2500 and 4000 g in the period from 2010 to 2014. Infants with structural malformations of chromosomal aberrations were excluded from the analysis.
Conducting the biometric study
In the framework of routine care in our perinatal centre, each pregnant woman undergoes an untrasound scan close to term. This examination is mainly intended to confirm the position of the infant, to estimate the amount of amniotic fluid and to determine the estimated foetal weight (EFW) on the basis of the usual biometry-based weight estimation formulae. The biparietal (BPD) and occipito-frontal diameters (OFD) of the head are measured at the level of the transventricular plane from the outer bone margin to the outer bone margin on the opposite side. Head circumference (HC) was either determined directly by means of the ellipse or trace function or calculated from the distances (HC = 2.325 × [OFD2 + BPD2]1/2) 12. The foetal abdomen was measured by means of its transverse and anterior-posterior diameters (ATD, APD) at the level of the stomach and the umbilical vein-ductus venosus complex. The abdominal circumference was calculated from these values (AC = π × [ATD + APD/2]). The femural length (FL) is measured as the distance between the diaphyses. The individual measurements, the estimated foetal weight (EFW) as well as the obstetrically relevant maternal characteristics were stored in the perinatal database. The birth weight (BW) was determined immediately after delivery by the responsible midwife, obstetrician or neonatologist and documented. For each of the included pregnancies the last ultrasound examination prior to delivery in which at least one measurement of each BPD, OFD, ATD, APD and FL was carried out was documented. Pregnancies with incomplete measurements or for which the last measurement was taken more than 7 days prior to delivery were excluded from the study. Each pregnancy was included only once in the study.
Statistical analysis
In each included case the EFW was determined by means of the published formulae according to Birnholz, Combs, Campbell, Ferrero, Hadlock, Halaska, Hansmann, Hart, Higginbottom, Jordaan, Persson, Merz, Mielke, Ott, Rose and McCallum, Sabbagha, Schild, Schillinger, Scott, Shepard, Shinozuka, Siemer, Thurnau, Vintzileos, Warsof, Weiner and Woo 3, 4, 5, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38. The corresponding formulae are listed in Table 1. The accuracies of the various formulae were determined and compared by means of the mean percentage error (MPE = [EFW− BW]/BW × 100) and the mean absolute percentage error (MAPE = |(EFW – BW)|/BW × 100). Hereby the MPE represents the systematic error of the formula. Its standard deviation (SD) reflects the random elements in the prediction error. The 95 % confidence intervals (CI) for the MPE were calculated and were used to test for a significant deviation against 0.
Table 1 Survey of the 35 weight estimation formulae.
| Author | Data | Formula |
|---|---|---|
| AC = abdominal circumference, HC = head circumference, FL = femur length, BPD = biparietal diameter, AD = abdominal diameter, GA = gestational age, MW = maternal weight | ||
| Birnholz 13 | BPD, OFD, ATD | 3.42928 × (BPD × OFD/1.264)0.5 × AD2/1 000 + 41.218 [g, mm] |
| Combs 14 | HC, AC, FL | 0.23718 × AC2 × FL + 0.03312 × HC3 [g, cm] |
| Campbell 15 | AC | e(− 4.564 + 0.282 × AC − 0.00331 × AC²) [kg, cm] |
| Ferrero 16 | AC, FL | 10(0.77125 + 0.13244 × AC − 0.12996 × FL − 1.73588 × AC²/1 000 + 2.18984 × FL/AC) [g, cm] |
| Hadlock I 4 | BPD, HC, AC, FL | 10(1.3596 + 0.0064 × HC + 0.0424 × AC + 0.174 × FL + 0.00061 × BPD × AC − 0.00386 × AC × FL) [g, cm] |
| Hadlock II 4 | AC, FL | 10(1.304 + 0.05281 × AC + 0.1938 × FL − 0.004 × AC × FL) [g, cm] |
| Hadlock III 4 | BPD, AC, FL | 10(1.335–0.0034 × AC × FL + 0.0316 × BPD + 0.0457 × AC + 0.1623 × FL) [g, cm] |
| Hadlock IV 4 | HC, AC, FL | 10(1.326–0.00326 × AC × FL + 0.0107 × HC + 0.0438 × AC + 0.158 × FL) [g, cm] |
| Hadlock V 5 | BPD, AC | 10(1.1134 + 0.05845 × AC − 0.000604 × AC² − 0.007365 × BPD² + 0.000595 × BPD × AC + 0.1694 × BPD) [g, cm] |
| Hadlock VI 5 | HC, AC, FL | 10(1.5662–0.0108 × HC + 0.0468 × AC + 0.171 × FL + 0.00034 × HC² − 0.0003685 × AC × FL) [g, cm] |
| Halaska 17 | BPD, AC, FL | 10(0.64041 × BPD − 0.03257 × BPD² + 0.00154 × AC × FL) [g,cm] |
| Hansmann 18 | BPD, AD, GA, | − 0.001665958 × AD3 + 0.4133629 × AD2 − 0.5580294 × AD − 0.01231535 × BPD3 + 3.702 × BPD2 − 330.1811 × BPD − 0.4937199 × (GA + 1)3 + 55.958061 × (GA + 1)2 − 2 034.3901 × (GA + 1) + 32 768.19 [g, mm] |
| Higginbottom 20 | AC | 0.0816 × AC3 [g, cm] |
| Jordaan 21 | BPD, HC, AC | 10(2.3231 + 0.02904 × AC + 0.0079 × HC − 0.0058 × BPD) [kg, cm] |
| Merz I 22 | BPD, AC | − 3 200.40479 + 157.07186 × AC + 15.90391 × BPD × BPD [g, cm] |
| Merz II 22 | AC | 0.1 × AC3 [g, cm] |
| Ott 26 | HC, AC, FL | 10(− 2.0661 + 0.04355 × HC + 0.05394 × AC − 0.0008582 × HC × AC + 1.2594 × FL/AC) [kg, cm] |
| Rose-McCallum 27 | BPD, AD, FL | e(0.143 × [BPD + AD + FL] + 4.198) [g, cm] |
| Sabbagha 28 | GA, HC, AC, FL | − 55.3–16.35 × (GA + HC + 2 × AC + FL) + 0.25838 × (GA + HC + 2 × AC + FL)2 [g, cm] |
| Schild I 29 | femaleBPD, AC, FL | − 4 035.275 + 1.143 × BPD3 + 1 159.878 × AC0.5 + 10.079 × FL3 − 81.277 × FL2 [g, cm] |
| Schild I 29 | maleBPD, HC, AC, FL | 1 913.853 × log10(BPD) + 0.01323 × HC3 + 55.532 × AC2 − 13 602.664 × AC0.5 − 0.721 × AC3 + 2.31 × FL3 [g, cm] |
| Schillinger 30 | BPD, ATD | 397.7 × BPD + ATD − 4 387 [g, cm] |
| Shepard 32 | BPD, AC | 10(− 1.7492 + 0.166 × BPD + 0.046 × AC − 0.002546 × AC × BPD) [kg,cm] |
| Shinozouka 33 | BPD, AC, FL | 1.07 × BPD3 + 3.42 × ATD2 × FL [g, cm] |
| Warsof 3 | BPD, AC | 10(− 1.599 + 0.144 × BPD + 0.032 × AC − 0.000111 × BPD² × AC) [kg, cm] |
| Woo 38 | BPD, AC, FL | 10(1,13705 + 0,15549 × BPD + 0.0464 × AC − 0.00279682 × BPD × AC + 0.037769 × FL − 0.000494529 × AC × FL) [g, cm] |
| Vinzeleos 36 | BPD, AC | 10(1.879 + 0.084 × BPD + 0.026 × AC) [g, cm] |
| Persson 23 | BPD, AD, FL | BPD0.972 × ([AD1 + AD2]/2)1.743 × FL0.367 × 10(− 2.646) [g, cm] |
| Schild II 39 | HC, AC, FL | 5 381.193 + 150.324 × HC + 2.069 × FL3 + 0.0232 × AC3 − 6 235.478 × LOG(HC) [g, cm] |
| Scott 31 | HC, AC, FL | 10(0.66 × LOG(HC) + 1.04 × LOG(AC) + 0.985 × LOG(FL)) [g, cm] |
| Siemer 34 | BPD, AC, FL | − 5 948.336 + 2 101.261 × LN(AC) + 15.613 × FL2 + 0.0577 × BPD3 [g, cm] |
| Thurnau 35 | BPD, AC | (9–337 × BPD × AC) − 229 [g, cm] |
| Weiner I 37 | HC, AC, FL | 10(1.6961 + 0.02253 × HC + 0.01645 × AC + 0.06439 × FL) [g, cm] |
| Weiner II 37 | HC, AC | 10(1.6575 + 0.04035 × HC + 0.01285 × AC) [g, cm] |
| Mielke I 24 | BPD, ATD, FL | e(3.067510 + 0.01677 × BPD + 0.000412 × ATD² + 0.040611 × FL − 0.000000006027957 × BPD² × ATD² − 0.000005086 × ATD² × FL) [g, cm] |
| Mielke II 25 | BPD, ATD, FL | e(3.704706 + 0.033276 × BPD + 0.000093048 × ATD² + 0.010570 × FL − 0.00000002477864 × BPD² × ATD² + 0.000002009 × ATD² × FL) [g,cm] |
For each estimation formula the proportions of the weight estimations with percentage errors of ≤ 5, ≤ 10, ≤ 20 and ≤ 30 % were calculated.
The relationship between the estimated and the actual birth weights was examined by means of a liner regression analysis. The extent of the estimation error in dependence on the actual birth weight could be estimated with the help of the regression.
Results
Demographic characteristics
Altogether 3416 pregnancies were included in the study after consideration of the inclusion criteria. The average age of the mothers amounted to 31.1 years. The average weight of the mothers was 76.9 kg (SD ± 14.7 kg, range 31.0–160.2 kg). On average the gestational age at birth was 39 + 1 weeks (interquartile range [IQR] 38 + 0–40 + 1 SSW). The gender distribution was balanced. The average weight at birth amounted to 3181 g. In the majority of the cases the ultrasound examination was performed at a maximum of 1 day before delivery (56.6 %). 34.3 % of the examinations were made 2–5 days before delivery and 9.1 % on days 6 or 7 prior to birth.
Mean percentage error and mean absolute percentage error
The MPE and MAPE values for the 35 employed formulae are listed in Table 2. The largest overestimation was seen for the Birnholz formula with an MPE of − 12.2 % while the clearest underestimation was found with the Mielke I formula (MPF = 46.0 %). It should be emphasised that the lowest percentage errors were found for the Hadlock III formula (0.8 %) and the Hadlock V formula (− 0.8 %). In a comparison of all formulae the standard deviations varied between 6.4 % (Schild II) and 16.4 % (Hadlock IV).
Table 2 MPE and MAPE values including standard deviations for all 35 formulae in the birth weight range from 2 500–4 000 g.
| MPE (%) | MAPE (%) | |||||
|---|---|---|---|---|---|---|
| Mean value | SD | Confidence interval | Mean value | SD | ||
| Lower limit | Upper limit | |||||
| Halaska | 0.9 | 8.1 | 0.6 | 1.2 | 6.6 | 4.8 |
| Schild I | 1.9 | 8.2 | 1.6 | 2.2 | 6.8 | 5.0 |
| Shinozuka | − 1.5 | 8.9 | − 1.8 | − 1.2 | 7.2 | 5.4 |
| Sabbagha | 2.8 | 8.6 | 2.5 | 3.1 | 7.3 | 5.4 |
| Hadlock III | 0.8 | 9.2 | 0.5 | 1.1 | 7.4 | 5.5 |
| Hadlock I | 2.5 | 8.9 | 2.2 | 2.8 | 7.5 | 5.5 |
| Ott | 3.9 | 8.5 | 3.6 | 4.2 | 7.5 | 5.5 |
| Hadlock V | − 0.8 | 10.0 | − 1.1 | − 0.5 | 8.0 | 6.1 |
| Combs | 5.6 | 8.1 | 5.3 | 5.9 | 8.1 | 5.7 |
| Hadlock II | 3.6 | 9.6 | 3.3 | 3.9 | 8.3 | 6.1 |
| Merz I | − 5.0 | 9.3 | − 5.3 | − 4.7 | 8.4 | 6.5 |
| Rose-McCallum | − 1.9 | 10.5 | − 2.2 | − 1.6 | 8.5 | 6.5 |
| Shepard | − 1.9 | 10.6 | − 2.2 | − 1.6 | 8.5 | 6.6 |
| Warsof | 3.2 | 10.1 | 2.9 | 3.5 | 8.5 | 6.3 |
| Ferrero | − 3.5 | 10.3 | − 3.8 | − 3.2 | 8.6 | 6.6 |
| Hadlock VI | 6.2 | 8.7 | 5.9 | 6.5 | 8.7 | 6.2 |
| Campbell | 5.0 | 9.9 | 4.7 | 5.5 | 8.9 | 6.7 |
| Persson | 6.4 | 9.0 | 6.1 | 6.7 | 9.0 | 6.4 |
| Hansmann | − 7.3 | 9.1 | − 7.6 | − 7.0 | 9.3 | 7.1 |
| Jordaan | 5.0 | 10.6 | 4.7 | 5.3 | 9.5 | 6.9 |
| Schillinger | − 9.6 | 9.3 | − 9.9 | − 9.3 | 10.9 | 7.8 |
| Vinzeleos | − 7.0 | 12.9 | − 7.4 | − 6.6 | 11.5 | 9.1 |
| Higginbottom | 9.2 | 13.1 | 8.8 | 9.6 | 13.1 | 9.2 |
| Hadlock IV | 3.4 | 16.4 | 2.9 | 3.9 | 13.3 | 10.0 |
| Weiner I | 12.9 | 8.9 | 12.6 | 13.2 | 13.6 | 7.7 |
| Birnholz | − 12.2 | 11.7 | − 12.6 | − 11.8 | 13.9 | 9.8 |
| Merz II | − 11.3 | 16.1 | − 11.8 | − 10.8 | 15.4 | 12.2 |
| Siemer | 16.7 | 6.6 | 16.5 | 16.9 | 16.8 | 6.4 |
| Thurnau | 17.0 | 7.0 | 6.8 | 7.2 | 17.1 | 6.8 |
| Scott | 17.6 | 6.8 | 17.4 | 17.8 | 17.6 | 6.7 |
| Woo | 17.9 | 7.3 | 17.7 | 18.1 | 18.0 | 7.1 |
| Weiner II | 19.7 | 9.9 | 19.4 | 20.0 | 20.1 | 9.1 |
| Schild II | 23.0 | 6.4 | 22.8 | 23.2 | 23.0 | 6.3 |
| Mielke II | 25.8 | 10.7 | 25.5 | 26.1 | 25.9 | 10.5 |
| Mielke I | 46.0 | 8.1 | 45.7 | 46.3 | 46.0 | 8.1 |
20 formulae (Halaska, Schild I, Shinozuka, Sabbagha, Hadlock III, Hadlock I, Ott, Hadlock V, Combs, Hadlock II, Merz I, Rose-McCallum, Shepard, Warsof, Ferrero, Hadlock VI, Campbell, Persson, Hansmann, Jordaan) exhibited MAPE values of ≤ 10 %. Of special interest is the Halaska formula that showed the best value of 6.6 %. Six formulae gave MAPE values in the intermediate error range of 10.1 to ≤ 15 % and further 9 formulae had MAPE values in the critical region of ≥ 15.1 %.
Table 3 presents the frequency distribution of differences between actual birth weight and estimated birth weight for the indivdual formulae in the weight range of 2500–4000 g. The favourable performance of the Halaska formula is again confirmed here. With use of the Halaska formula for birth weight estimation, 43.85 % of the cases lie below the 5 % and 77.52 % below the 10 % error level. Altogether there were 22 formulae for which more than half of the estimated values showed a deviation of ≤ 10 %. For four formulae (Weiner II, Schild II, Mielke II and Mielke I), on the other hand, estimations of more than half of the cases gave rise to clinical questionable deviations of more than 20 %.
Table 3 Frequency distribution between estimated and actual birth weights in the birth weight range of 2 500–4 000 g.
| Formula | Difference between actual and estimated birth weight less than: | |||
|---|---|---|---|---|
| 5 percent | 10 percent | 20 percent | 30 percent | |
| Halaska | 43.85 % | 77.52 % | 98.77 % | 100.00 % |
| Schild I | 43.62 % | 76.38 % | 98.27 % | 99.97 % |
| Shinozuka | 41.98 % | 73.07 % | 97.51 % | 99.77 % |
| Sabbagha | 41.31 % | 71.72 % | 97.98 % | 99.88 % |
| Hadlock III | 40.28 % | 71.49 % | 97.19 % | 99.82 % |
| Hadlock I | 40.60 % | 71.46 % | 97.34 % | 99.94 % |
| Ott | 39.99 % | 70.32 % | 97.28 % | 99.91 % |
| Hadlock V | 37.76 % | 68.68 % | 95.52 % | 99.56 % |
| Combs | 36.15 % | 67.10 % | 96.34 % | 99.94 % |
| Hadlock II | 36.48 % | 65.49 % | 95.64 % | 99.74 % |
| Merz I | 37.88 % | 66.04 % | 94.06 % | 99.39 % |
| Rose-McCallum | 35.63 % | 65.52 % | 93.97 % | 99.44 % |
| Shepard | 35.98 % | 65.66 % | 93.91 % | 99.06 % |
| Ferrero | 35.51 % | 64.17 % | 93.53 % | 99.36 % |
| Hadlock VI | 32.96 % | 62.76 % | 94.67 % | 99.80 % |
| Campbell | 34.75 % | 62.09 % | 93.03 % | 99.33 % |
| Persson | 32.90 % | 60.69 % | 93.62 % | 99.82 % |
| Hansmann | 34.02 % | 61.62 % | 91.36 % | 98.59 % |
| Jordaan | 32.11 % | 58.96 % | 90.95 % | 99.33 % |
| Schillinger | 27.20 % | 52.78 % | 86.74 % | 97.80 % |
| Vinzeleos | 28.37 % | 52.69 % | 83.55 % | 95.70 % |
| Higginbottom | 22.72 % | 43.41 % | 76.49 % | 95.49 % |
| Hadlock IV | 21.98 % | 44.15 % | 76.87 % | 93.88 % |
| Weiner I | 15.13 % | 35.51 % | 78.60 % | 98.19 % |
| Birnholz | 21.02 % | 40.63 % | 75.09 % | 92.83 % |
| Merz II | 21.75 % | 40.31 % | 69.85 % | 88.00 % |
| Siemer | 4.42 % | 16.10 % | 66.63 % | 99.24 % |
| Thurnau | 4.33 % | 15.37 % | 65.13 % | 97.95 % |
| Woo | 3.60 % | 13.55 % | 59.69 % | 95.84 % |
| Weiner II | 5.56 % | 14.72 % | 48.71 % | 86.24 % |
| Schild II | 0.50 % | 2.49 % | 30.85 % | 86.56 % |
| Mielke II | 2.72 % | 7.52 % | 28.69 % | 64.08 % |
| Mielke I | 0.00 % | 0.00 % | 0.09 % | 3.28 % |
Regression analysis between estimation error and actual birth weight
The determination of regression lines was able to demonstrate by means of graphic plots the variance of the deviations between estimated and actual birth weights over the entire weight range. Fig. 1 shows the 16 formulae that exhibited an intersection with the ideal regression line (x [actual birth weight] = y [estimated birth weight]). A common feature of all formulae is that they move up from a region of weight overestimation in the lower range to a region of underestimation.
Fig. 1.
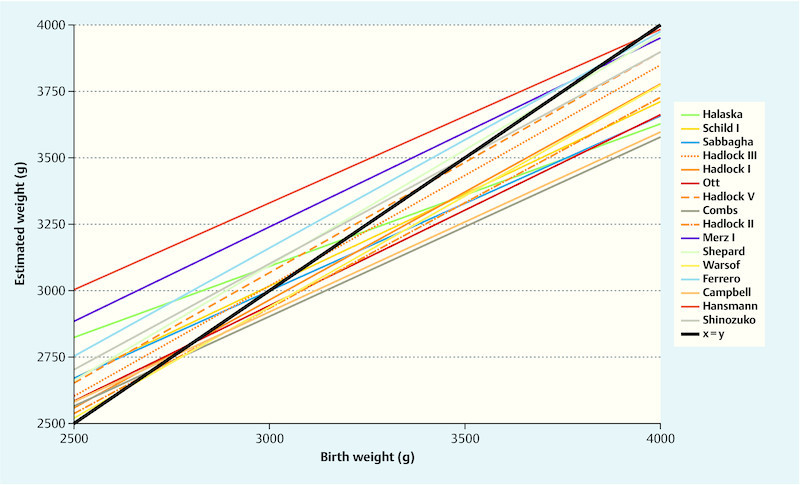
Actual and estimated birth weights. The listed regression formulae have an intersection with the ideal regression formula y = x for birth weights between 2500 and 4000 g.
Fig. 2 shows the distribution of 5 formulae that always resulted in overestimations of the birth weight. Estimations according to the Rose-McCullum formula were nearest and almost parallel to the ideal line. Fig. 3, on the other hand, illustrates the distribution of the 14 formulae that always led to an underestimation of the birth weight. Markedly different courses can be clearly seen here. Whereas in the lower weight range the formula according to Jordaan is closest to the ideal this is true for the Schild II formula in the upper weight range.
Fig. 2.
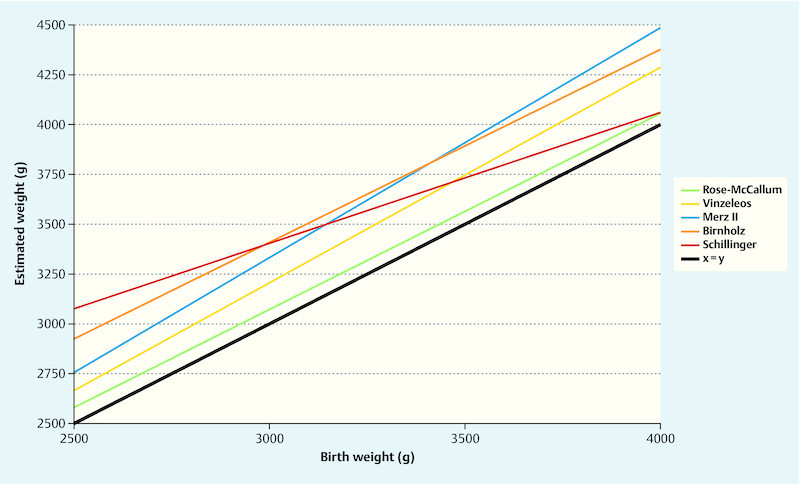
Actual and estimated birth weights. In the weight range from 2500 to 4000 g the listed regression formulae do not have an intersection point with the ideal regression formula y = x. On average the estimated weight was higher than the actual birth weight.
Fig. 3.
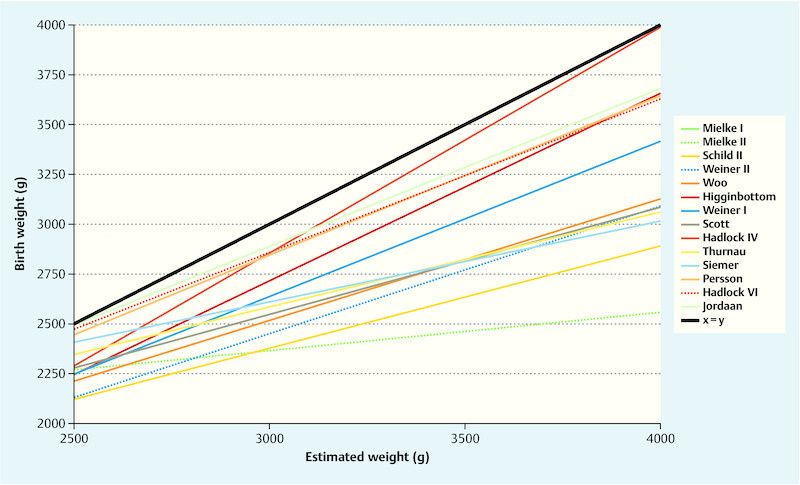
Actual and estimated birth weights. In the weight range from 2500 to 4000 g the listed regression formulae do not have an intersection point with the ideal regression formula y = x. On average the estimated weight was lower than the actual birth weight. The plot according to the Mielke I formula lies below the illustrated region.
Discussion
In the present study we have, on the basis of measurements of 3416 foetuses, shown that the smallest MPEs can be obtained with the Hadlock III and V formulae (0.8 %, SD 9.2 % or, respectively, − 0.8 %, SD 10.0 %). The lowest absolute error (6.6 %) as well as the most favourable frequency distribution for cases with lower than 5 % and 10 % errors (43.9 and 77.5) were seen for the Halaska formula. This corresponds to the expected values from comparable preliminary work. The majority of the weight estimation formulae were developed for average infants weighing between 2500–4000 g and exhibited thereby a relatively low absolute percentage error of between 6–10 %, just as in our series 40, 41, 42. Merely 5 formulae consistently showed overestimations of weight. 14 formulae underestimated the foetal weight over the entire weight range, 16 did so in the upper weight region.
There are numerous possibilities to improve the weight estimations. With regard to the accuracy of sonographic measurements, several studies have shown that practical sonographic experience or, respectively, targeted training on patients or simulators can reduce the errors 41, 43. Also a time window between measurements and delivery of ≤ 7 days can help to reduce errors 44. Another option, especially for heavier infants, is an optimisation of the weight estimation through a combination of ultrasound findings with maternal and pregnancy-specific parameters such as gestational age, parity, gender of the foetus, and maternal height or weight. The presumed benefit of such an elaborate procedure is, however, a subject of controversial discussion in the current literature 45, 46, 47. Nevertheless, there is consensus that maternal obesity increases the estimation errors 48, 49.
Ultimately, the estimation errors of sonographic formulae must be considered as being intrinsic to the method. In a study of 628 new-born infants, Kehl et al. could reduce the systematic error to a minimum by means of postnatally performed measurements. Even so, the MPEs of the employed formulae were between 7.42 and 8.77 %. The proportion of estimations with an error of under 10 % amounted to between 74.6 and 81.3 %. Under consideration of the 95 % limits of agreement, the estimations were in a range of ± 500 g. These key data for optimal weight estimations are in agreement with our results when using the best formulae such as those according to Halaska or Hadlock.
Our data show that many formulae exhibit a variable susceptibility to error within the normal weight range. This observation supports the attempts of current research groups to use a two-step procedure for weight estimations. In a first such step the weight range, for example, is delineated by measurement of the AC and the formula chosen in dependence on this result. It has been demonstrated that those formulae that had been specifically developed for foetuses with an abdominal circumference of less than 290 mm exhibited a significantly better MAPE (7.13–7.61 %) and markedly more measurements with an error of less than 10 % in comparison with the Warsof and Hadlock formulae 50. An analogous result has been determined for infants with an AC greater than 360 mm 51. The so-called Zürich method follows a similar strategy. In this case, the product of the AC and the FL is calculated. When this value is < 24 600 the Hadlock formula is used, for larger values the Merz formula 52. Our data confirm that in the upper weight range the Merz formula enables a better weight estimation than the Hadlock formula.
A further strategy for improvement involves the implementation of 3D measurements, as a rule in the standardised determination of a volume from the foetal thigh region. At least in cases of manifest gestational diabetes, an improvement in weight estimation through 3D measurements seems to be possible because just in such pregnancies the soft tissue mantle does especially influence the weight of the foetus 53.
On a critical note, it must be realised that the validity of the present data is limited due to the retrospective nature of the study. The monocentric data acquisition represents a further limitation. However, this is relativised somewhat by the large number of participating investigators with varying degrees of training and experience.
Conclusions
When judged by the MPE and MAPE results, the formulae according to Hadlock and Halaska exhibit the lowest errors. Most of the formulae tend to underestimate the weight to varying degress depending on the weight class. This supports current efforts to apply a two-step procedure.
Footnotes
Conflict of Interest The authors declare that they have no conflicts of interest.
Supporting Information
References
- 1.Willocks J, Donald I, Duggan T C. et al. Foetal cephalometry by ultrasound. J Obstet Gynaecol Br Commonw. 1964;71:11–20. doi: 10.1111/j.1471-0528.1964.tb04236.x. [DOI] [PubMed] [Google Scholar]
- 2.Loeffler F E. Clinical foetal weight prediction. J Obstet Gynaecol Br Commonw. 1967;74:675–677. doi: 10.1111/j.1471-0528.1967.tb03779.x. [DOI] [PubMed] [Google Scholar]
- 3.Warsof S L, Gohari P, Berkowitz R L. et al. The estimation of fetal weight by computer-assisted analysis. Am J Obstet Gynecol. 1977;128:881–892. doi: 10.1016/0002-9378(77)90058-8. [DOI] [PubMed] [Google Scholar]
- 4.Hadlock F P, Harrist R B, Sharman R S. et al. Estimation of fetal weight with the use of head, body, and femur measurements–a prospective study. Am J Obstet Gynecol. 1985;151:333–337. doi: 10.1016/0002-9378(85)90298-4. [DOI] [PubMed] [Google Scholar]
- 5.Hadlock F P, Harrist R B, Carpenter R J. et al. Sonographic estimation of fetal weight. The value of femur length in addition to head and abdomen measurements. Radiology. 1984;150:535–540. doi: 10.1148/radiology.150.2.6691115. [DOI] [PubMed] [Google Scholar]
- 6.Hoopmann M, Bernau B, Hart N. et al. Do specific weight formulas for fetuses ≤ 1500 g really improve weight estimation? Ultraschall in Med. 2010;31:48–52. doi: 10.1055/s-0028-1109481. [DOI] [PubMed] [Google Scholar]
- 7.Hoopmann M, Abele H, Wagner N. et al. Performance of 36 different weight estimation formulae in fetuses with macrosomia. Fetal Diagn Ther. 2010;27:204–213. doi: 10.1159/000299475. [DOI] [PubMed] [Google Scholar]
- 8.Abele H, Hoopmann M, Wagner N. et al. Accuracy of sonographic fetal weight estimation of fetuses with a birth weight of 1500 g or less. Eur J Obstet Gynecol Reprod Biol. 2010;153:131–137. doi: 10.1016/j.ejogrb.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 9.American College of Obstetricians and Gynecologists . ACOG Practice bulletin no. 134: fetal growth restriction. Obstet Gynecol. 2013;121:1122–1133. doi: 10.1097/01.AOG.0000429658.85846.f9. [DOI] [PubMed] [Google Scholar]
- 10.Gyurkovits Z, Kálló K, Bakki J. et al. Neonatal outcome of macrosomic infants: an analysis of a two-year period. Eur J Obstet Gynecol Reprod Biol. 2011;159:289–292. doi: 10.1016/j.ejogrb.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Henriksen T. The macrosomic fetus: a challenge in current obstetrics. Acta Obstet Gynecol Scand. 2008;87:134–145. doi: 10.1080/00016340801899289. [DOI] [PubMed] [Google Scholar]
- 12.Schmidt U, Temerinac D, Bildstein K. et al. Finding the most accurate method to measure head circumference for fetal weight estimation. Eur J Obstet Gynecol. 2014;178:153–156. doi: 10.1016/j.ejogrb.2014.03.047. [DOI] [PubMed] [Google Scholar]
- 13.Birnholz J C. An algorithmic approach to accurate ultrasonic fetal weight estimation. Invest Radiol. 1986;21:571–576. doi: 10.1097/00004424-198607000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Combs C A, Jaekle R K, Rosenn B. et al. Sonographic estimation of fetal weight based on a model of fetal volume. Obstet Gynecol. 1993;82:365–370. [PubMed] [Google Scholar]
- 15.Campbell S, Wilkin D. Ultrasonic measurement of fetal abdomen circumference in the estimation of fetal weight. Br J Obstet Gynaecol. 1975;82:689–697. doi: 10.1111/j.1471-0528.1975.tb00708.x. [DOI] [PubMed] [Google Scholar]
- 16.Ferrero A, Maggi E, Giancotti A. et al. Regression formula for estimation of fetal weight with use of abdominal circumference and femur length: a prospective study. J Ultrasound Med. 1994;13:823–833. doi: 10.7863/jum.1994.13.11.823. [DOI] [PubMed] [Google Scholar]
- 17.Halaska M G, Vlk R, Feldmar P. et al. Predicting term birth weight using ultrasound and maternal characteristics. Eur J Obstet Gynecol. 2006;128:231–235. doi: 10.1016/j.ejogrb.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 18.Hansmann M, Schuhmacher H, Voigt U. Stuttgart: Thieme; 1978. Mehrparametrische nicht lineare Gewichtsschätzung mittels Ultraschall unter Berücksichtigung des Gestationsalters. [Google Scholar]
- 19.Hart N C, Hilbert A, Meurer B. et al. Macrosomia: a new formula for optimized fetal weight estimation. Ultrasound Obstet Gynecol. 2010;35:42–47. doi: 10.1002/uog.7493. [DOI] [PubMed] [Google Scholar]
- 20.Higginbottom J. Estimation of fetal weight. Ultrasound Med Biol. 1977;3:59. doi: 10.1016/0301-5629(77)90124-7. [DOI] [PubMed] [Google Scholar]
- 21.Jordaan H V, Dunn L J. A new method of evaluating fetal growth. Obstet Gynecol. 1978;51:659–665. [PubMed] [Google Scholar]
- 22.Merz E, Lieser H, Schicketanz K H. et al. [Intrauterine fetal weight assessment using ultrasound. A comparison of several weight assessment methods and development of a new formula for the determination of fetal weight] Ultraschall Med. 1988;9:15–24. doi: 10.1055/s-2007-1011588. [DOI] [PubMed] [Google Scholar]
- 23.Marsál K. Antenatal diagnosis of intrauterine growth retardation by ultrasound. Int J Technol Assess Health Care. 1992;8 01:160–169. doi: 10.1017/s0266462300013064. [DOI] [PubMed] [Google Scholar]
- 24.Mielke G, Pietschbreitfeld B, Salinas R. et al. A new formula for prenatal ultrasonographic weight estimation in extremely preterm fetuses. Gynecol Obstet Invest. 1995;40:84–88. doi: 10.1159/000292311. [DOI] [PubMed] [Google Scholar]
- 25.Mielke G, Pietschbreitfeld B, Regele B. et al. An accurate method for sonographic estimation of the weight of very preterm fetuses. Gynecol Obstet Invest. 1997;43:98–103. doi: 10.1159/000291830. [DOI] [PubMed] [Google Scholar]
- 26.Ott W J, Doyle S, Flamm S. et al. Accurate ultrasonic estimation of fetal weight. Prospective analysis of new ultrasonic formulas. Am J Perinatol. 1986;3:307–310. doi: 10.1055/s-2007-999885. [DOI] [PubMed] [Google Scholar]
- 27.Rose B I, McCallum W D. A simplified method for estimating fetal weight using ultrasound measurements. Obstet Gynecol. 1987;69:671–675. [PubMed] [Google Scholar]
- 28.Sabbagha R, Minogue J, Tamura R. et al. Estimation of birth-weight by use of ultrasonographic formulas targeted to large-for-gestational-age, appropriate-for-gestational-age, and small-for-gestational-age fetuses. Am J Obstet Gynecol. 1989;160:854–862. doi: 10.1016/0002-9378(89)90301-3. [DOI] [PubMed] [Google Scholar]
- 29.Schild R L, Sachs C, Fimmers R. et al. Sex-specific fetal weight prediction by ultrasound. Ultrasound Obstet Gynecol. 2004;23:30–35. doi: 10.1002/uog.942. [DOI] [PubMed] [Google Scholar]
- 30.Schillinger H, Müller R, Wode J. et al. [Intrauterine weight determination of the fetus using ultrasonics] Arch Gynakol. 1975;219:399–401. doi: 10.1007/BF00669149. [DOI] [PubMed] [Google Scholar]
- 31.Scott F, Beeby P, Abbott J. et al. New formula for estimating fetal weight below 1000 g: comparison with existing formulas. J Ultrasound Med. 1996;15:669–672. doi: 10.7863/jum.1996.15.10.669. [DOI] [PubMed] [Google Scholar]
- 32.Shepard M J, Richards V A, Berkowitz R L. et al. An evaluation of two equations for predicting fetal weight by ultrasound. Am J Obstet Gynecol. 1982;142:47–54. doi: 10.1016/s0002-9378(16)32283-9. [DOI] [PubMed] [Google Scholar]
- 33.Shinozuka N, Okai T, Kohzuma S. et al. Formulas for fetal weight estimation by ultrasound measurements based on neonatal specific gravities and volumes. Am J Obstet Gynecol. 1987;157:1140–1145. doi: 10.1016/s0002-9378(87)80278-8. [DOI] [PubMed] [Google Scholar]
- 34.Siemer J, Hilbert A, Hart N. et al. A new sonographic weight formula for fetuses. Ultraschall in Med. 2009;30:47–51. doi: 10.1055/s-2007-963645. [DOI] [PubMed] [Google Scholar]
- 35.Thurnau G R, Tamura R K, Sabbagha R. et al. A simple estimated fetal weight equation based on real-time ultrasound measurements of fetuses less than thirty-four weeksʼ gestation. Am J Obstet Gynecol. 1983;145:557–561. doi: 10.1016/0002-9378(83)91195-x. [DOI] [PubMed] [Google Scholar]
- 36.Vintzileos A M, Campbell W A, Rodis J F. et al. Fetal weight estimation formulas with head, abdominal, femur, and thigh circumference measurements. Am J Obstet Gynecol. 1987;157:410–414. doi: 10.1016/s0002-9378(87)80182-5. [DOI] [PubMed] [Google Scholar]
- 37.Weiner C P, Sabbagha R E, Vaisrub N. et al. Ultrasonic fetal weight prediction: role of head circumference and femur length. Obstet Gynecol. 1985;65:812–817. [PubMed] [Google Scholar]
- 38.Woo J, Wan M. An evaluation of fetal weight prediction using a simple equation containing the fetal femur length. J Ultrasound Med. 1986;5:453–457. doi: 10.7863/jum.1986.5.8.453. [DOI] [PubMed] [Google Scholar]
- 39.Schild R L, Fell K, Fimmers R. et al. A new formula for calculating weight in the fetus of < or = 1600 g. Ultrasound Obstet Gynecol. 2004;24:775–780. doi: 10.1002/uog.1741. [DOI] [PubMed] [Google Scholar]
- 40.Melamed N, Yogev Y, Meizner I. et al. Sonographic fetal weight estimation: which model should be used? J Ultrasound Med. 2009;28:617–629. doi: 10.7863/jum.2009.28.5.617. [DOI] [PubMed] [Google Scholar]
- 41.Siemer J, Egger N, Hart N. et al. Fetal weight estimation by ultrasound: comparison of 11 different formulae and examiners with differing skill levels. Ultraschall Med. 2008;29:159–164. doi: 10.1055/s-2007-963165. [DOI] [PubMed] [Google Scholar]
- 42.Nahum G G, Stanislaw H. Ultrasonographic prediction of term birth weight: How accurate is it? Am J Obstet Gynecol. 2003;188:566–574. doi: 10.1067/mob.2003.155. [DOI] [PubMed] [Google Scholar]
- 43.Haist M, Schauf B, Kagan K O. et al. Verbesserung der Ergebnisqualität durch standardisiertes Training am Ultraschallsimulator. Geburtsh Frauenheilk. 2010;70:844–848. [Google Scholar]
- 44.Faschingbauer F, Raabe E, Heimrich J. et al. Accuracy of sonographic fetal weight estimation: influence of the scan-to-delivery interval in combination with the applied weight estimation formula. Arch Gynecol Obstet. 2016;294:487–493. doi: 10.1007/s00404-015-3989-2. [DOI] [PubMed] [Google Scholar]
- 45.Nahum G G, Stanislaw H. Fetal macrosomia is predicted earlier by combination birth-weight estimation methods than by ultrasound alone. Ultrasound Obstet Gynecol. 2009;34:122. doi: 10.1002/uog.6417. [DOI] [PubMed] [Google Scholar]
- 46.Mazouni C, Rouzier R, Ledu R. et al. Development and internal validation of a nomogram to predict macrosomia. Ultrasound Obstet Gynecol. 2007;29:544–549. doi: 10.1002/uog.3999. [DOI] [PubMed] [Google Scholar]
- 47.Balsyte D, Schäffer L, Burkhardt T. et al. Sonographic prediction of macrosomia cannot be improved by combination with pregnancy-specific characteristics. Ultrasound Obstet Gynecol. 2009;33:453–458. doi: 10.1002/uog.6282. [DOI] [PubMed] [Google Scholar]
- 48.Aksoy H, Aksoy U, Karadag O I. et al. Influence of maternal body mass index on sonographic fetal weight estimation prior to scheduled delivery. J Obstet Gynaecol Res. 2015;41:1556–1561. doi: 10.1111/jog.12755. [DOI] [PubMed] [Google Scholar]
- 49.Heer I M, Kumper C, Vogtle N. et al. Analysis of factors influencing the ultrasonic fetal weight estimation. Fetal Diagn Ther. 2008;23:204–210. doi: 10.1159/000116742. [DOI] [PubMed] [Google Scholar]
- 50.Kehl S, Koerber C, Hart N. et al. New sonographic method for fetuses with small abdominal circumference improves fetal weight estimation. Ultraschall Med. 2012;33:469–473. doi: 10.1055/s-0031-1273407. [DOI] [PubMed] [Google Scholar]
- 51.Kehl S, Koerber C, Hart N. et al. New sonographic method for fetuses with a large abdominal circumference improves fetal weight estimation. Ultraschall Med. 2012;33:265–269. doi: 10.1055/s-0029-1245834. [DOI] [PubMed] [Google Scholar]
- 52.Balsyte D Schäffer L Zimmermann R et al. Optimized sonographic weight estimation of fetuses over 3500 g using biometry-guided formula selection Ultraschall Med 2015[Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 53.Pagani G, Palai N, Zatti S. et al. Fetal weight estimation in gestational diabetic pregnancies: comparison between conventional and three-dimensional fractional thigh volume methods using gestation-adjusted projection. Ultrasound Obstet Gynecol. 2014;43:72–76. doi: 10.1002/uog.12458. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


