Abstract
Purpose
Both substance use and depression are common in adolescence and often comorbid. Past research has produced conflicting results on whether there is a temporal relationship and if so, in which direction it operates and how it may vary by sex. We examined the longitudinal associations between substance use frequency and depressive symptoms from adolescence into young adulthood, and whether the associations were moderated by sex.
Methods
With data from Waves I, III, and IV of the National Longitudinal Study of Adolescent to Adult Health (n=9816), we used growth curve models to test if depressive symptoms predicted marijuana use or binge drinking frequency (Self-Medication Model) or if substance use frequency predicted depressive symptoms (Stress Model). Moderation by sex and age was tested for both potential pathways.
Results
Increases in adolescent depressive symptoms, compared to no symptoms, were associated with a steeper predicted increase in marijuana use frequency from adolescence to young adulthood. Increases in persistent binge drinking or marijuana use frequency had concurrent positive associations with depressive symptoms from adolescence to young adulthood, and these associations were significantly stronger for females compared to males.
Conclusions
The results support the Self-Medication Model for marijuana use but also provide modest support for the Stress Model, that substance use is associated with depressive symptoms, especially for females.
Keywords: Depression, substance use, adolescent development, gender
Both substance use and depressive symptoms increase in adolescence (12–19 year olds), are often comorbid, and are associated with negative outcomes.1–6 Nearly one third of U.S. high school students report current alcohol use, approximately one quarter report current marijuana use; together these are the two most commonly used substances in adolescence and thus the focus of these analyses.7 Up to one in five adolescents have experienced a major depressive episode.3 Youth with a major depressive episode in the past year are more than twice as likely to report marijuana use compared to youth without a major depressive episode in the past year.8 Comorbidity between substance use and depression is concerning because it is associated with worse outcomes than either alone, including increases in substance use, longer depressive episodes, more severe mental health issues, delays in substance abuse recovery, and elevated suicide risk.9
The comorbidity between substance use and depression indicates there may be a causal relationship between them. Understanding in which direction the process operates could inform how to target and integrate substance use and depression screening, newly covered preventive services under the Affordable Care Act.10 Theories suggest alternative directions for this relationship. First, the Self-Medication Model asserts depression leads to substance use as an attempt to ameliorate symptoms.11 Second, our Stress Model hypothesizes substance use leads to depression by increasing strain in peer and parental relationships or social isolation and thereby interpersonal stress.12,13 Processes entailed in these Models are complicated by biological sex and developmental change. In general, adolescent females are more likely to report experiencing depression than males.14,15 By comparison, adolescent males generally report use of a wider range of substances and at a higher frequency compared to females.5,7,16 Developmentally, initiation of substance use is concentrated in adolescence yet the quantity and frequency of substance use typically peak between 18–25 years of age in the United States.5 The complications from biological sex and developmental change likely inform the conflicting results from prior literature, even when we concentrate on studies using longitudinal designs.
Previous studies of the Self-Medication Model differ across development and by sex. Hooshmand et al. followed 4,000 U.S. adolescents through high school and found those reporting higher depressive symptoms early had faster increases in marijuana use.17 De Graaf et al., with a sample of over 7,000 from a different developmental stage (late adolescence to young adulthood) found that major depression predicted alcohol dependence.18 However, an analysis using data on a sample followed from adolescence into emerging adulthood found no evidence for depression predicting increases in substance use, measured in clusters along with sexual risk behavior.19 Previous studies of the Self-Medication Model have also found differences by biological sex. A study with a sample of over 600 African American adolescents who were surveyed annually for six years starting in high school found depression predicted marijuana use, but only in males.9 But, Mushquash et al. with a sample of 200 undergraduate women found depressive symptoms predicted increases in heavy episodic drinking one week later.20
Though the empirical results are mixed, there is greater theoretical support for males self-medicating depressive symptoms compared to females. First, a systematic review and separate meta-analysis both concluded females are more likely to use most emotion regulation and coping strategies compared to men.21,22 The dominant coping mechanism for males was impulsive reward-seeking behavior, especially using alcohol.21 Second, depressive symptoms can be a violation of traditional male gender norms like invulnerability and so males may have greater incentive to self-medicate.23 Given these factors, we hypothesized there would be greater support for the Self-Medication Model for males compared to females (Hypothesis 1).
Previous studies of the Stress Model also differ across development and by sex. Fergusson et al., with a sample of over 1,000 late adolescents followed into emerging adulthood, tested both potential directions of the association between alcohol abuse or dependence and depression, and found the best fitting model was leading from alcohol to depression; a recent review came to the same conclusion.24,25 In contrast, a study of emerging adults followed over a short period of time found alcohol use did not predict increases in depressive symtpoms.20 For marijuana, a review and two longitudinal studies of adolescents followed into emerging and young adulthood, respectively, found an increasing marijuana use trajectory, or at least weekly use, predicted later depression.26–28 However, a study of adolescents followed into emerging adulthood found no relationship between marijuana use and later depression.9 This Model is also complicated by sex. A longitudinal survey following over 1,000 African Americans from age six to 42 found increased alcohol or marijuana use in adolescence predicted psychological distress in young adulthood but only for males.29 By comparison, a study found substance use and sexual risk behavior in adolescence predicted depression in emerging adulthood, especially for females.19
Amid mixed empirical results, there are theoretical reasons to expect the Stress Model to be more robust among females than males. First, substance use can conflict with traditional female gender norms and this norm violation could predict a stronger depressive response.30 Second, female norm violation could also predict strain in their school connectedness or peer and parental relationships or increased social isolation. Compared to males, females are more perceptive of and have stronger negative reactions to interpersonal stress and stress can be associated with a depressive response.12,13,31 Given these factors, we hypothesized there would be greater support for the Stress Model for females compared to males (Hypothesis 2).
The large literatures on adolescent substance use and depression share some limitations, which this paper aims to address. Much of the research is based on non-representative samples, tests only one direction, and does not test moderation by sex.9,17,28,30,32,33,6 This project addresses these important limitations by using data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative sample, testing both potential directions of the association as well as moderation by sex.
Methods
Sample
Add Health has a nationally representative sample of U.S. adolescents who were in grades 7–12 in the 1994–95 school year (Wave I). There have been four in-home interviews to date. The present analysis sample is restricted to respondents interviewed at Wave I, Wave III (ages 18 to 26), and Wave IV (ages 24 to 32), with valid sampling weights (N=12,288) and who had complete data on all variables of interest (N=9,816, 80%). Data from Wave II were not used as Wave I seniors were not followed by design. Details of the Add Health study are described elsewhere.34 All Add Health procedures were approved by the Institutional Review Board at the University of North Carolina, Chapel Hill. These analyses were deemed exempt.
Measures
Depressive symptoms were measured using nine items from the Center for Epidemiologic Studies Depression Scale (CES-D) available at Waves I, III, and IV (alpha at Wave III=0.80). The items ask about frequency of symptoms in the past week from rarely (0) to most of the time (3); the summed score for the scale ranges from 0 to 27 and the 12-month re-test reliability is high.35 The CES-D is not a diagnostic tool.
The substances measured included alcohol (binge drinking) and marijuana. We measured frequency of substance use rather than ever use to better capture levels of risk taking. The frequency of binge drinking, defined as consuming 5 or more drinks in a row, is assessed in the past 12 months with an ordinal variable ranging from 0 (never) to 6 (every day or nearly every day). Marijuana use frequency is assessed in the past 30 days; the measures at Waves I and III were continuous and assessed instances of use. At Wave IV the measure was ordinal and assessed days of use, mirroring the binge drinking frequency measure.34 To make the marijuana use frequency measures comparable across the waves, the measures at Waves I and III were recoded to capture days of use, assuming an instance of use was equivalent to a day of use, and adapted to match the ordinal measure at Wave IV.
Multiple covariates were included in the model as both depressive symptoms and substance use can vary across sociodemographic characteristics. The covariates included respondent’s self-identified race/ethnicity (Hispanic and non-Hispanic White, Black, Asian, Native American, and Other) and the highest educational attainment of the parents (less than high school, high school graduate, some college, or college graduate or higher) as a proxy for socioeconomic status of the parental home.5 Frequency of child maltreatment, ranging from never to four or more times, was included as a potential confounder as it can be significantly associated with both depressive symptoms and substance use.36 Child maltreatment was self-reported and defined as emotional, physical, or sexual abuse before age 18 or physical or supervisory neglect at or before the Wave III interview. Finally, retrospective measures were included to control for pre-Wave I levels of the dependent variable, including a depression diagnosis, drinking a full alcoholic beverage, and using marijuana.
Analysis
The data set was structured by age instead of wave to capture developmental change from adolescence to young adulthood. Linear mixed effects models were used to estimate inter-and intra-individual change (i.e., population average and individual-specific growth curves) in binge drinking frequency, marijuana use frequency, and depressive symptoms. Nine models were fit for each independent and dependent variable pairing. The first four models were used to estimate the growth curve of the dependent variable. We started with an unadjusted model, adding covariates, testing a random slope by age, then interacting the age terms with sex to test inter-individual differences in the intra-individual intercept and trend. The next three models test a temporal association between dual growth curves (i.e., whether the intercept or adolescent measure of one curve is significantly associated with the intercept and trend in another curve). Finally, the last two models test concurrent associations between dual growth curves at each age. For all eligible models, we tested moderation by sex and fit a random intercept by respondent ID and a random slope by age. We report the variance estimates for the random effects, where applicable. We also calculated the intraclass correlation coefficient (ICC) to get an estimate of the proportion of variance in the outcome that is due to variance between individuals, and report the percent change in the ICC across the models.
Results
Across the developmental trajectory from adolescence to young adulthood in the Add Health sample, the prevalence of binge drinking and marijuana use increases from adolescence to emerging adulthood and then decreases slightly in young adulthood. For example, from ages 14 to 16, only 25% of respondents report any binge drinking, but this increases to 55% between ages 20 to 22 and then decreases to 38% between ages 32 to 34 (Table 1). For marijuana use, the proportion of respondents reporting any use increases from 14% at ages 14 to 16, to 25% at ages 20 to 22, and then decreases to 17% for ages 32 to 34. Depressive symptoms follow an opposite pattern, starting higher in adolescence, decreasing in emerging adulthood and then increasing slightly in young adulthood. For example, the mean CES-D for ages 14 to 16 is 5.72; this decreases to 4.28 at ages 23 to 25 but then increases again to 5.08 between ages 29 to 31.
Table 1.
Characteristics of the analysis sample by age
| Age (years)a N (weighted percentage) |
||||||||
|---|---|---|---|---|---|---|---|---|
| 11–13a | 14–16 | 17–19 | 20–22 | 23–25 | 26–28 | 29–31 | 32–34 | |
| Binge drinking frequency | N=1494 | N=5080 | N=4276 | N=4822 | N=4378 | N=4517 | N=4692 | N=189 |
| None | 1376 (0.91) | 3865 (0.75) | 2540 (0.54) | 2465 (0.47) | 2182 (0.45) | 2215 (0.46) | 2563 (0.52) | 116 (0.62) |
| 1–2 days/year | 57 (0.04) | 495 (0.10) | 560 (0.14) | 784 (0.16) | 773 (0.18) | 809 (0.19) | 795 (0.17) | 28 (0.13) |
| ≤1 x/month | 19 (0.02) | 305 (0.06) | 382 (0.10) | 494 (0.12) | 499 (0.12) | 530 (0.12) | 514 (0.11) | 11 (0.04) |
| 2–3 days/month | 17 (0.01) | 176 (0.04) | 346 (0.09) | 417 (0.09) | 396 (0.10) | 443 (0.10) | 353 (0.08) | 12 (0.07) |
| 1–2 days/week | 13 (0.01) | 140 (0.03) | 318 (0.09) | 472 (0.11) | 363 (0.10) | 360 (0.09) | 290 (0.07) | 13 (0.07) |
| 3–5 days/week | 8 (0.01) | 63 (0.02) | 100 (0.03) | 160 (0.04) | 130 (0.03) | 122 (0.03) | 133 (0.03) | 8 (0.07) |
| Every day/almost | 4 (0.00) | 36 (0.01) | 30 (0.01) | 30 (0.01) | 35 (0.01) | 38 (0.01) | 44 (0.01) | --b |
| Marijuana use frequency | ||||||||
| None | 1430 (0.95) | 4390 (0.86) | 3412 (0.78) | 3705 (0.75) | 3534 (0.79) | 3733 (0.81) | 4006 (0.85) | 162 (0.83) |
| 1 day | 22 (0.02) | 178 (0.03) | 201 (0.05) | 227 (0.05) | 188 (0.05) | 142 (0.03) | 157 (0.03) | 7 (0.03) |
| 2–3 days | 22 (0.02) | 189 (0.04) | 193 (0.05) | 201 (0.05) | 158 (0.04) | 146 (0.04) | 104 (0.02) | -- |
| 1 day/week | 5 (0.00) | 88 (0.02) | 106 (0.02) | 122 (0.03) | 84 (0.02) | 51 (0.01) | 34 (0.01) | 3 (0.02) |
| 2 days/week | 7 (0.00) | 68 (0.01) | 89 (0.03) | 109 (0.02) | 85 (0.02) | 89 (0.02) | 84 (0.02) | -- |
| 3–5 days/week | 5 (0.00) | 86 (0.02) | 129 (0.03) | 187 (0.04) | 131 (0.04) | 116 (0.03) | 128 (0.03) | -- |
| Every day/almost | 3 (0.00) | 81 (0.02) | 146 (0.04) | 271 (0.06) | 198 (0.05) | 240 (0.06) | 179 (0.04) | 11 (0.09) |
| Depressive symptoms (0–27), m | 4.90 (3.87) | 5.72 (4.25) | 5.66 (4.23) | 4.52 (4.07) | 4.28 (3.87) | 5.12 (4.09) | 5.08 (4.10) | 6.08 (4.47) |
Age is continuous in all of the statistical models but was condensed into categories for this table
Dash indicates fewer than three respondents
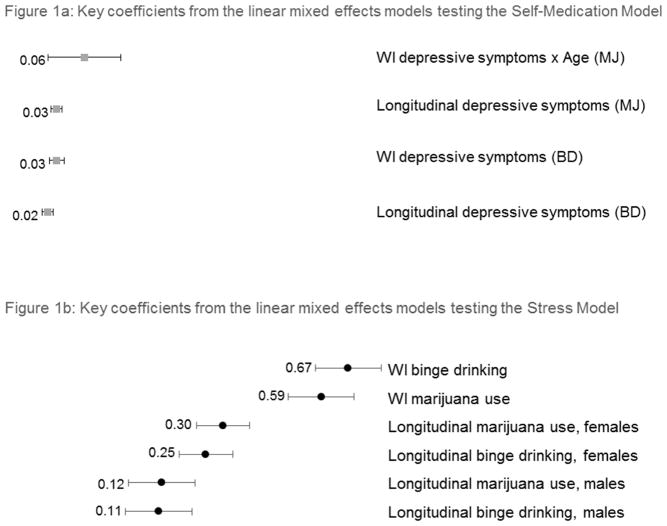
Figure 1 is a plot of the key coefficients from the linear mixed effects models (see supplemental tables). The data labels show coefficient magnitude, organized from highest at the top of the figure to lowest at the bottom, text labels identify the coefficient.
Figure 1.
Key coefficients from the linear mixed effects models
aBinge drinking frequency (BD), marijuana use frequency (MJ), Wave I (WI), dependent variable noted with parentheses in Figure 1a
The grey squares in Figure 1a show results from models testing the Self-Medication Model (i.e., the independent variable is depressive symptoms). Depressive symptoms in adolescence, a Wave I measure, were significantly associated with higher binge drinking frequency in adolescence (b=0.03, p<0.001). The concurrent relationship across the ages was also significant (b=0.02, p<0.001). None of the interactions tested with the adolescent or time-varying (longitudinal) measure of depressive symptoms were significant. Depressive symptoms in adolescence were significantly associated with a steeper slope in marijuana use frequency with age (b=0.06, p<0.01). The concurrent relationship for depressive symptoms and the marijuana use frequency growth curve was also significant (b=0.03, p<0.001). The interactions between the longitudinal depressive symptom measure and the substance use frequency growth curves were not statistically significant. Self-Medication Models fit with a random slope for age failed to converge.
The black circles in Figure 1b show results from analyses testing the Stress Model (i.e., independent variable was substance use frequency). Binge drinking frequency in adolescence was significantly associated with a higher level of depressive symptoms in adolescence (b=0.67, p<0.001). The concurrent positive relationship across the ages between binge drinking frequency and the depressive symptom growth curve was also significant and moderated by sex such that the relationship is stronger for females (b=0.25, p<0.001) compared to males (b=0.11, p<0.01). Marijuana use frequency in adolescence was also significantly associated with higher adolescent depressive symptoms (b=0.59, p<0.001). The concurrent relationship across the ages was significant and moderated by sex, again indicating a stronger relationship for females (b=0.30, p<0.001) compared to males (b=0.12, p<0.001). All of the relevant models testing the Stress Model were fit with a random slope for age, allowing further heterogeneity in the growth curves.
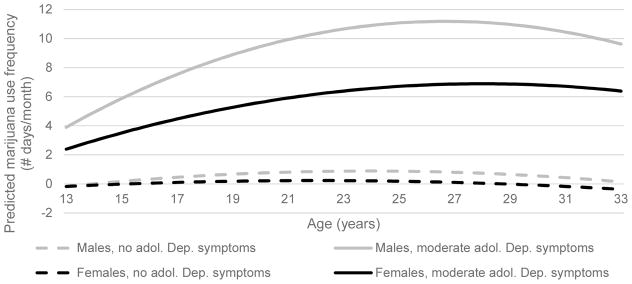
Figure 2 shows the predicted growth curve of marijuana use frequency across age and how growth varies by sex and depressive symptoms (Self-Medication Model). There is an increase in predicted marijuana use frequency across age for those with moderate depressive symptoms in adolescence, especially males, but not for adolescents with no depressive symptoms.
Figure 2.
Relationship between adolescent depressive symptoms and marijuana use frequency growth curve (Self-Medication Model)a
aAdolescent (adol), dep (depressive)
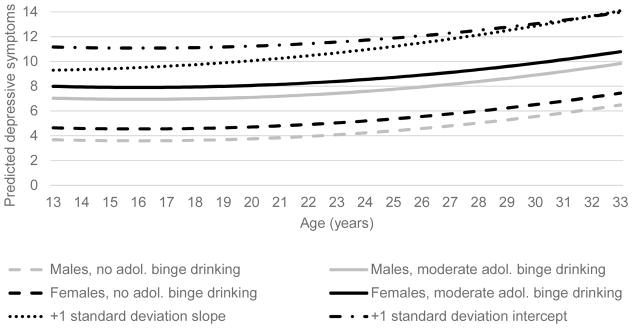
Figure 3 shows the predicted growth curve of depressive symptoms across age and how growth varies by sex and binge drinking frequency (Stress Model). The figure displays an increase in predicted depressive symptoms in adolescence with an increase in binge drinking frequency in adolescence and a higher starting point in adolescence for females compared to males. Similar results were found for marijuana use frequency. The top two lines in the figure show variation from the mean predicted depressive growth curve from the random effects in the model. Specifically, they illustrate the predicted growth curve going above the threshold for likely depression (10 on the CES-D) given a one standard deviation increase in the intercept or the slope.
Figure 3.
Relationship between adolescent binge drinking frequency and depressive symptoms growth curve (Stress Model)a
aAdolescence (adol.)
There is meaningful within- and between-individual variation in the growth curves. The ICCs decreased across the models when additional predictors were added, indicating the predictor and control variables explained some of the between-individual variation in the outcome, as expected. For example, for the Self-Medication Models, the ICCs decreased by 30% from the unadjusted to fully-adjusted models (0.27 to 0.19) when binge drinking frequency was the dependent variable and by 23% (0.30 to 0.23) when marijuana use frequency was the outcome. For the Stress Models, the ICCs decreased by 18% (0.34 to 0.28).
Discussion
We used Add Health data to fit growth curve models testing both directions of the potential relationship between substance use and depressive symptoms from adolescence to young adulthood; we also tested moderation by sex. Overall and consistent with prior research, substance use frequency seems to increase during adolescence and start declining in emerging adulthood; by comparison, depressive symptoms seem to gradually increase from emerging to young adulthood.5,37 The ICCs decreased meaningfully across the models, indicating our hypothesized predictor and control variables explained considerable variation in growth curves between respondents. Hypothesis 1 asserted there would be greater support for the Self-Medication Model among males compared to females, which was not supported in the current analysis. Rather, the findings support the Self-Medication Model for both males and females as there was a significant relationship between depressive symptoms in adolescence and the slope of marijuana use frequency from adolescence to young adulthood. Hypothesis 2 asserted the Stress Model would be more applicable for females compared to males, and was partially supported. When we tested the association between longitudinal measures of both binge drinking and marijuana use frequency and the depressive symptom growth curve, the association was significantly moderated by sex in both cases, indicating a stronger positive concurrent relationship across the developmental time period for females compared to males. We deem this only partial support for Hypothesis 2 because the associations significantly moderated by sex were concurrent and not directional.
Our results indicate adolescents may self-medicate depressive symptoms with marijuana use. The results supporting the Self-Medication Model for marijuana use for both males and females are consistent with some prior studies.9,17,18 However, other longitudinal studies using different methods found marijuana use predicted depression and not the other way around, indicating methodological differences add complexity.26–28 Additionally, a similar prior study of over 600 African American adolescents found evidence for depression predicting marijuana use but only in males indicating future research should examine three-way interactions by age, race, and sex.9
We expected to see evidence for adolescents self-medicating depressive symptoms with binge drinking but found no evidence to support this, consistent with some prior literature.17,20 Potential explanations include conceptual and methodological complications. For example, a study with a large sample followed from late adolescence into young adulthood found evidence for depression predicting alcohol, but used alcohol dependence as their measure, which is conceptually different than binge drinking frequency.18 Further, another longitudinal study found evidence for females self-medicating depressive symptoms with alcohol, though examined a one-week timespan compared to the years used in this and many prior studies, a key methodological difference.20 We especially expected to see evidence for self-medication with alcohol for males, as a prior review found.22 However, binge drinking is a normative social activity for males, especially at these ages. If only a minority are self-medicating, the relationship may be hard to find.38 Future research could examine males self-medicating with alcohol at ages when binge drinking is less common.
From adolescence to young adulthood, persistent binge drinking or marijuana use are concurrently positively associated with depressive symptoms, especially for females. This indicates partial support for the Stress Model among females and is consistent with some prior literature.19,24,26–28 However, again, race/ethnicity complicate the picture. A study of African American and Puerto Rican women followed from adolescence into young adulthood found those with increasing marijuana use frequency had higher depressive symptoms in concordance with our results.28 But, a similar longitudinal study of African American children followed into adulthood found substance use in adolescence predicted psychological distress in adulthood only for males.29 In the prior study including Puerto Rican women, the women with increasing use frequency were also more likely to have a substance use disorder in adulthood.28 This indicates the underlying mechanism here may be substance dependence or abuse, signaled by a persistent pattern of substance use across development, rather than increased interpersonal stress from risk behavior. Indeed two analyses found marijuana use was only associated with later depression when it was weekly or daily use and another only found an association between alcohol and later depression when measuring alcohol dependence.24,26,27
The results of this study should be considered in the context of its limitations. First, the ordinal substance use measures were treated as continuous, though various robustness checks indicate the results are stable to variations in the measures (results not shown). Second, though linear mixed effects models remove potential bias from time-invariant unobserved characteristics, the results could still be biased by time-varying unobserved characteristics. Third, the Add Health data allow the developmental time period from adolescence into young adulthood to be studied; however, with only three waves of data (i.e., developmental periods) with the entire sample, it is more difficult to find variation in the growth curves. Though the adolescent data was collected two decades ago, the prevalence of our key variables have not changed neither has the likely relationships between them.39 Fourth, complete case analysis increased the proportion missing but is recommended for analysis of Add Health data; multiple imputation was not a viable option for the items with the highest proportion missing.40
This paper addressed several limitations in past literature by using data from a nationally representative sample followed from adolescence into young adulthood and testing both potential directions of the association between substance use and depressive symptoms, as well as possible moderation by sex. The results indicate youth may self-medicate their depressive symptoms with marijuana use and that both marijuana use and binge drinking are concurrently associated with depressive symptoms, especially among females. So, both Models were supported and there was modest evidence suggesting the Stress Model is a better fit for females than males. These results inform efforts to screen adolescents for depression or substance use. For example, youth screening positive for depression or an increase in depressive symptoms should also be screened for marijuana use, and youth, especially females, screening positive for persistent binge drinking or marijuana should be targeted for depression prevention programs or at least flagged as at risk for depressive symptoms. Future research should examine moderation in these pathways by both sex and race/ethnicity as well as variation in results across different longitudinal methods and conceptualizations of substance use frequency and/or abuse/dependence.
Supplementary Material
Implications and Contribution.
Adolescents may medicate depressive symptoms with marijuana use. Persistent binge drinking or marijuana use from adolescence to young adulthood associated with higher concurrent depressive symptoms, associations were stronger for females.
Acknowledgments
We are grateful to the Carolina Population Center for training support (T32 HD007168) and for general support (R24 HD050924). Effort by Wilkinson was supported by grant F31DA036961 from the National Institute on Drug Abuse, starting August 15th, 2014. Effort by Halpern and Herring was supported by grant R01 HD057046 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (PI: CT Halpern). This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations.
Footnotes
The authors have no conflicts of interest to disclose.
Previous poster presentation: American Public Health Association Annual Meeting, Nov. 2015
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Andra L. Wilkinson, Email: wilkina@live.unc.edu.
Carolyn Tucker Halpern, Email: carolyn_halpern@unc.edu.
Amy H. Herring, Email: amy_herring@unc.edu.
Meghan Shanahan, Email: shanahan@unc.edu.
Susan Ennett, Email: sennett@email.unc.edu.
Jon Hussey, Email: jon_hussey@unc.edu.
Kathleen Mullan Harris, Email: kathie_harris@unc.edu.
References
- 1.Kessler R, McGonagle K, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Arch Gen Psychiatry1. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. http://www.ncbi.nlm.nih.gov/pubmed/8279933. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher JM. Adolescent depression and educational attainment: Results using sibling fixed effects. Health Econ. 2010;19:855–871. doi: 10.1002/hec. [DOI] [PubMed] [Google Scholar]
- 3.Williams SB, O’Connor EA, Eder M, Whitlock EP. Screening for child and adolescent depression in primary care settings: A systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2009;123(4):e716–e735. doi: 10.1542/peds.2008-2415. [DOI] [PubMed] [Google Scholar]
- 4.Haydon A, McRee A, Halpern CT. Risk-taking behavior. In: Bradford Brown P, Prinstein M, editors. Encyclopedia of Adolescence. Vol. 3. San Diego, CA: Elsevier Inc; 2011. pp. 255–263. [DOI] [Google Scholar]
- 5.Chassin L, Hussong A, Beltran I. Adolescent substance use. In: Lerner R, Steinberg L, editors. Handbook of Adolescent Psychology. 3. Hoboken, NJ: John Wiley & Sons, Inc; 2009. pp. 723–764. [Google Scholar]
- 6.Armstrong T, Costello J. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol. 2002;70(6):1224–1239. doi: 10.1037//0022-006X.70.6.1224. [DOI] [PubMed] [Google Scholar]
- 7.Kann L, Kinchen S, Shanklin S, et al. Youth Risk Behavior Surveillance — United States, 2013. MMWR. 2014;63(4):1–168. [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration. [Accessed March 22, 2016];Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings. http://www.samhsa.gov/data/sites/default/files/NSDUHmhfr2013/NSDUHmhfr2013.pdf. Published 2014.
- 9.Repetto PB, Zimmerman MA, Caldwell CH. A longitudinal study of depressive symptoms and marijuana use in a sample of inner-city African Americans. J Res Adolesc. 2008;18(3):421–447. doi: 10.1111/j.1532-7795.2008.00566.x. [DOI] [Google Scholar]
- 10.United States Department of Health and Human Services. [Accessed May 21, 2015];Preventive services covered under the Affordable Care Act. http://www.hhs.gov/healthcare/facts/factsheets/2010/07/preventive-services-list.html. Published 2012.
- 11.Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harv Rev Psychiatry. 1997;4(5):231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- 12.Rudolph KD. Gender differences in emotional responses to interpersonal stress during adolescence. J Adolesc Heal. 2002;30(4S):3–13. doi: 10.1016/S1054-139X(01)00383-4. [DOI] [PubMed] [Google Scholar]
- 13.Ge X, Lorenz F, Conger R, Elder G, Simons R. Trajectories of stressful life events and depressive symptoms during adolescence. Dev Psychol. 1994;30(4):467–483. doi: 10.1037/0012-1649.30.4.467. [DOI] [Google Scholar]
- 14.Essau CA, Lewinsohn PM, Seeley JR, Sasagawa S. Gender differences in the developmental course of depression. J Affect Disord. 2010;127:185–190. doi: 10.1016/j.jad.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008;115(2):291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- 16.Evans-Polce RJ, Vasilenko SA, Lanza ST. Changes in gender and racial/ethnic disparities in rates of cigarette use, regular heavy episodic drinking, and marijuana use: Ages 14 to 32. Addict Behav. 2015;41:218–222. doi: 10.1016/j.addbeh.2014.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hooshmand S, Willoughby T, Good M. Does the direction of effects in the association between depressive symptoms and health-risk behaviors differ by behavior? A longitudinal study across the high school years. J Adolesc Heal. 2012;50(2):140–147. doi: 10.1016/j.jadohealth.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 18.de Graaf R, Bijl R, Spijker J, Beekman A, Vollebergh W. Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance use disorders - Findings from the Netherlands Mental Health Survey and Incidence Study. Soc Psychiatry Psychiatr Epidemiol. 2003;38(1):1–11. doi: 10.1007/s00127-003-0597-4. [DOI] [PubMed] [Google Scholar]
- 19.Hallfors DD, Waller MW, Bauer D, Ford CA, Halpern CT. Which comes first in adolescence--sex and drugs or depression? Am J Prev Med. 2005;29(3):163–170. doi: 10.1016/j.amepre.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Mushquash AR, Stewart SH, Sherry SB, Sherry DL, Mushquash CJ, MacKinnon AL. Depressive symptoms are a vulnerability factor for heavy episodic drinking: A short-term, four-wave longitudinal study of undergraduate women. Addict Behav. 2013;38:2180–2186. doi: 10.1016/j.addbeh.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Tamres LK, Janicki D, Helgeson VS. Sex differences in coping behavior: A meta-analytic review and an examination of relative coping. Personal Soc Psychol Rev. 2002;6(1):2–30. doi: 10.1207/S15327957PSPR0601. [DOI] [Google Scholar]
- 22.Nolen-Hoeksema S. Emotion regulation and psychopathology: the role of gender. Annu Rev Clin Psychol. 2012;8:161–187. doi: 10.1146/annurev-clinpsy-032511-143109. [DOI] [PubMed] [Google Scholar]
- 23.Courtenay W. Constructions of masculinity and their influence on men’s well-being: A theory of gender and health. Soc Sci Med. 2000;50(10):1385–1401. doi: 10.1016/S0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- 24.Fergusson DM, Boden JM, Horwood LJ. Tests of causal links between alcohol abuse or dependence and major depression. Arch Gen Psychiatry. 2009;66(3):260–266. doi: 10.1001/archgenpsychiatry.2008.543. [DOI] [PubMed] [Google Scholar]
- 25.Boden JM, Fergusson DM. Alcohol and depression. Addiction. 2011;106:906–914. doi: 10.1111/j.1360-0443.2010.03351.x. [DOI] [PubMed] [Google Scholar]
- 26.Degenhardt L, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98(11):1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- 27.Patton G, Coffey C, Carlin J, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: cohort study. BMJ. 2002;325:1195–1198. doi: 10.1186/1471-2458-9-467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pahl K, Brook J, Koppel J. Trajectories of marijuana use and psychological adjustment among urban African American and Puerto Rican Women. Psychol Med. 2011;41(8):1775–1783. doi: 10.1055/s-0029-1237430.Imprinting. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Green KM, Zebrak KA, Robertson JA, Fothergill KE, Ensminger ME. Interrelationship of substance use and psychological distress over the life course among a cohort of urban African Americans. Drug Alcohol Depend. 2012;123:239–248. doi: 10.1016/j.drugalcdep.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Byrnes JP, Miller DC, Schafer WD. Gender differences in risk taking: A meta-analysis. Psychol Bull. 1999;125(3):367–383. doi: 10.1037/0033-2909.125.3.367. [DOI] [Google Scholar]
- 31.McDade TW, Hawkley LC, Cacioppo JT. Psychosocial and behavioral predictors of inflammation in middle-aged and older adults: The Chicago health, aging, and social relations study. Psychosom Med. 2006;68(3):376–381. doi: 10.1097/01.psy.0000221371.43607.64. [DOI] [PubMed] [Google Scholar]
- 32.Costello DM, Swendsen J, Rose JS, Dierker LC. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. J Consult Clin Psychol. 2008;76(2):173–183. doi: 10.1037/0022-006X.76.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Needham BL. Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Soc Sci Med. 2007;65(6):1166–1179. doi: 10.1016/j.socscimed.2007.04.037. [DOI] [PubMed] [Google Scholar]
- 34.Harris KM. [Accessed March 22, 2016];The Add Health study: Design and accomplishments. http://www.cpc.unc.edu/projects/addhealth/data/guides/DesignPaperWIIV.pdf. Published 2013.
- 35.Eaton W, Muntaner C, Smith C, Tien A, Ybarra M. Center for Epidemiologic Studies Depression scale: Review and revision (CESD and CESD-R) In: Maruish M, editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. 3. Mahwah, NJ: Lawrence Erlbaum; 2004. pp. 363–377. [Google Scholar]
- 36.Stein J, Leslie M, Nyamathi A. Relative contributions of parent substance use and childhood maltreatment to chronic homelessness, depression, and substance abuse problems among homeless women: Mediating roles of self-esteem and abuse in adulthood. Child Abus Negl. 2002;26(10):1011–1027. doi: 10.1016/S0145-2134(02)00382-4. [DOI] [PubMed] [Google Scholar]
- 37.Pratt L, Brody D. Depression in the United States household population, 2005–2006. NCHS Data Brief. 2008;(7):1–8. [PubMed] [Google Scholar]
- 38.Nolen-Hoeksema S. Emotion regulation and psychopathology: The role of gender. Annu Rev Clin Psychol. 2012;8:161–187. doi: 10.1146/annurev-clinpsy-032511-143109. [DOI] [PubMed] [Google Scholar]
- 39.Child Trends. [Accessed April 18, 2016];Databank. http://www.childtrends.org/databank/
- 40.Chen P, Chantala K. [Accessed March 22, 2016];Guidelines for Analyzing Add Health Data. https://www.cpc.unc.edu/projects/addhealth/data/guides/wt-guidelines.pdf. Published 2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.