Abstract
Femoral head fractures after posterior dislocation of the hip are uncommon and are conventionally treated by an open method. Hip arthroscopy can be a valuable treatment option for the management of femoral head fractures. Arthroscopy allows for a less invasive option when compared with arthrotomy and can allow faster recovery with minimal soft-tissue injury. We describe the arthroscopic reduction and internal fixation of Pipkin type I femoral head fractures with a detailed stepwise description of the surgical technique, including technical pearls and pitfalls, potential complications, and advantages and disadvantages.
Femoral head fractures after posterior dislocation of the hip are relatively uncommon and are often associated with a poor functional outcome.1, 2, 3, 4 The Pipkin and Brumback systems are used to classify this fracture pattern.4, 5 The previous guidelines for management of Pipkin type I femoral head fractures recommended conservative management for undisplaced fractures and open excision of displaced fracture fragments. Considering the complex and interdependent circulation of the hip joint, open excision may put the compromised circulation at further risk, a risk that is multiplied by the potential morbidity of the arthrotomy itself.5, 6, 7
Hip arthroscopy has gained popularity in recent years for the management of various hip disorders, particularly femoroacetabular impingement.8, 9 Its role in the management of femoral head fractures remains relatively unexplored, however, with only a few reported cases in the literature and no long-term follow-up results.1, 6, 10, 11 We describe the technique of arthroscopic reduction and internal fixation of Pipkin type I femoral head fractures.
Preoperative Radiologic Evaluation
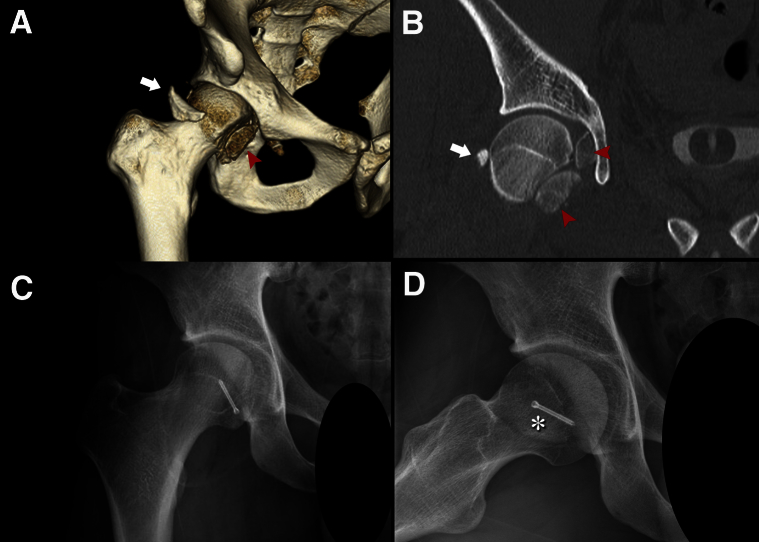
A detailed skeletal survey and radiologic examination including 3-dimensional computed tomography (CT) should be performed. In the presented case, a Pipkin type I femoral head fracture with a large infrafoveal displaced fracture fragment in the cotyloid fossa and a posterior acetabular rim fracture (<20% of the posterior wall) displaced anteriorly are seen (Fig 1 A and B).
Fig 1.
(A, B) Preoperative computed tomography images showing 2 infrafoveal femoral head fracture fragments (red arrowheads) with an anteriorly displaced posterior acetabular rim fracture fragment (white arrows). (C, D) Postoperative anteroposterior and frog-leg lateral radiographs at last follow-up showing a well-united fracture fragment (asterisk) and maintained joint space.
Surgical Technique
This technical note describes our technique of arthroscopic osteosynthesis for an infrafoveal femoral head fracture (Video 1). The details are summarized in Table 1. The advantages and disadvantages of the arthroscopic technique for fracture fixation are listed in Table 2.
Table 1.
Pearls and Pitfalls
| Pearls |
| A probe should be used for reduction of infrafoveal femoral head fracture fragments. |
| Fluoroscopic and arthroscopic visualization should be used for better screw placement. |
| A grasper should be used from the anterior portal to maintain fracture reduction. |
| The distal accessory anterior portal should be used to insert the screw perpendicularly to the fracture site. |
| A radiopaque headless cannulated compression screw is preferable for fracture fixation. This is helpful for evaluation of screw migration in the postoperative period. |
| Use a loop of Vicryl lassoed around the neck of the screw will help to retrieve the screw if it becomes mal-tracked in the soft tissues. Just before the screw is fully tightened, the Vicryl loop is pulled or cut out. |
| The joint capsule should be released with an arthroscopic knife to improve accessibility of surgical instruments. To avoid iatrogenic instability, interportal capsulotomy should not be performed. |
| Small loose osteochondral fragments should be removed from the central compartment. |
| The traction time should be minimized to avoid complications related to traction. |
| Joint congruity and stability should be checked under fluoroscopy by dynamic range of motion. |
| Pitfalls |
| The surgeon may need to convert to an open procedure if there is failure to obtain reduction. |
| There is a risk of transient sciatic or femoral nerve neurapraxia with a prolonged traction time. |
| There is a risk of fluid extravasation in the case of medial acetabular wall fracture. |
| There is a need for additional capsular release of the intact anterior joint capsule. |
| Hip arthroscopy should be used for fracture fixation only after the surgeon has gained significant experience with femoroacetabular impingement management. |
Table 2.
Advantages and Disadvantages of Arthroscopic Reduction and Internal Fixation of Femoral Head Fracture
| Advantages |
| Limited soft-tissue disruption occurs around the fracture. |
| Assessment and treatment of concomitant post-traumatic intra-articular pathology are possible. |
| There is minimal damage to the already compromised blood supply of the femoral head. |
| It is possible to ensure anatomic reduction of the articular surface. |
| There is less operative-site morbidity as compared with arthrotomy. |
| Early postoperative rehabilitation is possible. |
| Disadvantages |
| There is a steep learning curve. |
| Patient positioning on the distraction unit can be difficult in the case of associated ipsilateral lower-extremity injury. |
| The procedure is technically demanding. |
| A prolonged traction time can increase the risk of traction-induced lower-limb neurapraxia. |
The patient is placed in the supine position on a hip arthroscopy distraction unit (Smith & Nephew, Andover, MA). For the central compartment, the affected limb is kept in traction with the hip in 20° of abduction, internal rotation, and 5° of flexion, and during examination of the peripheral compartment, the traction is released and the limb is kept in 45° of flexion. The anterolateral and anterior portals are used as viewing and working portals, respectively.
The posterolateral portal is used for managing posterior lesions and as an inflow portal. Several distal accessory anterior portals are made as required throughout the procedure.
First, the peripheral compartment is explored. By use of a 70° arthroscope, the joint space is examined and the blood clot is aspirated, with removal of small osteochondral fragments. Capsulotomy is extended around each portal for better instrument manipulation.
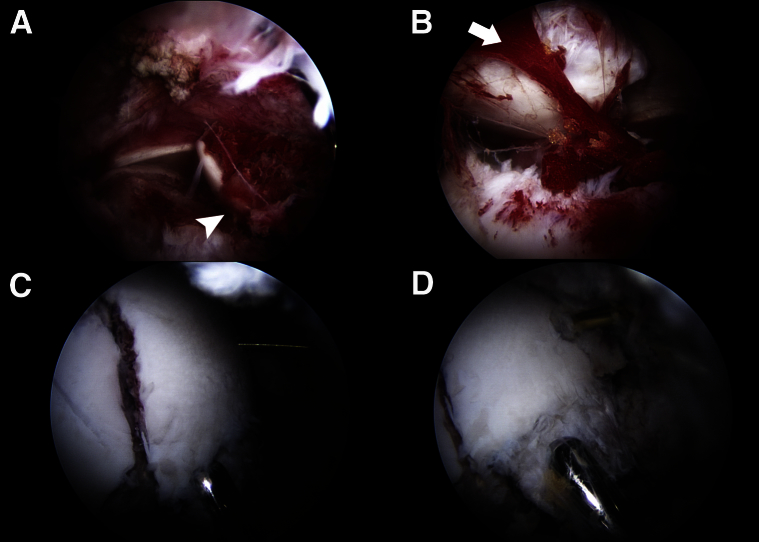
In this case, the larger anteroinferior fragment involving approximately 30% of the femoral head was seen incarcerated between the anterior acetabular wall and femoral head. It was mobilized from the central compartment to the anterior peripheral compartment and gently reverted using a probe (Fig 2A, Video 1). Then, traction was applied to the limb to explore the central compartment with the hip in 20° of abduction and 5° of flexion. The smaller posteroinferior fragment, in the cotyloid fossa, was removed (Fig 2B). Again, traction was released, and under direct visualization, anatomic reduction was accomplished with the hip in 30° of flexion, abduction, and external rotation. The reduction was obtained and maintained throughout the fixation using a grasper passed through the anterior portal and was temporarily secured using a Kirschner wire. By use of the distal accessory anterior portal, a threaded guidewire was inserted to obtain sufficient purchase without penetrating the femoral head cartilage. The position of the guidewire was checked and confirmed under fluoroscopy. A 3.0-mm-long threaded headless cannulated compression screw (Synthes, Paoli, PA) was used for fracture fixation. A loop of Vicryl (Ethicon, Somerville, NJ) was lassoed around the neck of the screw for easy screw retrieval if it became mal-tracked through the soft tissue. The screw was inserted perpendicularly to the fracture site over the guidewire, and interfragmentary compression was achieved (Fig 2 C and D). We tried to minimize the traction time (<30 minutes) throughout the procedure. An intraoperative fluoroscopic evaluation of stability showed a stable joint, so the posterior acetabular rim fracture fragment (involving <20% of the posterior acetabular wall) was excised and the torn posterior labrum was debrided. The anterior and superior labra were found to be intact. Except for cartilage abrasion at the superior femoral head-neck junction, the rest of the articular cartilage of the acetabulum and the remaining femoral head was grossly intact. Postoperative radiographs showed acceptable reduction with maintained joint space (Fig 1 C and D).
Fig 2.
(A) Supine arthroscopic view of the right hip through the anterolateral portal using a 70° arthroscope with the hip in 45° of flexion without traction. The femoral head fracture fragment (arrowhead) is shown to be incarcerated between the anterior acetabular wall and femoral head in the peripheral compartment. (B) Supine arthroscopic view of the central compartment of the right hip through the anterolateral portal using a 70° arthroscope with the hip in 20° of abduction and 5° of flexion in traction. The smaller posteroinferior fragment is in the cotyloid fossa (arrow). (C) Supine arthroscopic view of the peripheral compartment of the right hip through the anterolateral portal using a 70° arthroscope with the hip in 30° of flexion, abduction, and external rotation. Anatomic reduction has been obtained and is maintained with the help of a grasper passed through the anterior portal and guidewire inserted through the distal accessory anterior portal. (D) Supine arthroscopic view of the peripheral compartment of the right hip through the anterolateral portal using a 70° arthroscope with the hip in 30° of flexion, abduction, and external rotation. Interfragmentary compression is obtained using a 3.0-mm-long threaded headless cannulated compression screw (with a loop of Vicryl lassoed around the neck of the screw) passed over the guidewire through the distal accessory anterior portal.
Postoperative Rehabilitation
Continuous passive motion and circumduction exercises are started on day 1 and non–weight-bearing mobilization on day 3. Until 6 weeks, 90° of flexion and up to 10° of rotation are permitted. Partial weight bearing with 2 crutches for 4 weeks and 1 crutch for another 4 weeks is allowed. Full weight bearing is advised after radiologic confirmation of no screw migration at 2 months. Competitive sports are allowed 6 months postoperatively.
Discussion
Management of periarticular fracture-dislocations of the hip is challenging. Traditionally, undisplaced Pipkin type I fractures are treated conservatively and the displaced fragments undergo open excision. Open excision has some disadvantages because of the associated morbidity of the arthrotomy and the risk of further damage to the already compromised blood supply of the femoral head after dislocation. Labral tears, chondral and intra-articular loose fragments, and ligamentum teres injury often accompany traumatic dislocations of the hip.12 Hip arthroscopy yields less morbidity, causes minimal soft-tissue damage, and allows early rehabilitation. It is used mainly for the management of femoroacetabular impingement, postinjury removal of osteochondral fractures, labral repair, and internal and external snapping hip syndrome.13 Yamamoto et al.11 stressed the importance of hip arthroscopy in hip trauma cases for the removal of small loose osteochondral fragments in neglected Thompson-Epstein type I and II dislocations, which are often not detected on CT and can eventually lead to osteoarthritis. Lansford and Munns6 reported arthroscopic excision of the femoral head fragment in Pipkin type I fractures after fracture-dislocation. Similarly, Matsuda1 reported arthroscopic fixation for a Pipkin type II fracture. Recently, Park et al.10 reported arthroscopic fixation of a similar fracture pattern in a 50-year-old female patient.
Patient selection is important when using the described technique. This technique is contraindicated in hemodynamically unstable patients who cannot tolerate a prolonged surgical time, and special caution should be taken in patients with associated abdominal injury who are at increased risk of abdominal compartment syndrome and retroperitoneal fluid extravasation.14 In addition, in patients with associated neurologic injury, the traction time should be minimized as much as possible to prevent further aggravation of initial nerve injury due to prolonged traction.
Preoperative planning with CT interpretation is important. In some cases it may be difficult to obtain arthroscopic reduction and fixation, and it may be necessary to convert to open arthrotomy; this should be explained preoperatively to patients.
Initial surgical experience with arthroscopic femoroacetabular impingement management is advisable to produce acceptable results with arthroscopic fixation of periarticular fractures around the hip. If performed meticulously, hip arthroscopy can provide all the benefits of anatomic reduction with the added advantages of minimal surgical soft-tissue injury and early rehabilitation in post-traumatic cases.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical procedure for arthroscopic reduction and internal fixation of femoral head fracture. The affected side was the right hip. The patient was positioned supine with the anterolateral portal used as the viewing portal and anterior portal used as the working portal. The peripheral compartment was visualized first with the limb in 45° of flexion. After evacuation of the fracture hematoma, the larger anteroinferior fracture fragment was seen and was mobilized from the central compartment to the anterior peripheral compartment with a probe. The fragment was gently reverted using the probe, and bone-to-bone apposition was obtained. Traction was applied, and the central compartment was explored to remove the smaller posteroinferior fragment in the cotyloid fossa. Traction was released, and the peripheral compartment was accessed with the limb in 30° of flexion, abduction, and external rotation. Under direct visualization, the anteroinferior fracture fragment was anatomically reduced using a grasper. By use of the distal accessory anterior portal, a guidewire was passed for temporary fixation of the fracture fragment. A 3-mm headless cannulated compression screw, with a lasso of Vicryl around the neck, was inserted perpendicular to the fracture site over the guidewire, and interfragmentary compression was obtained. After confirmation of joint stability under fluoroscopy, the smaller posterior acetabular rim fracture fragment and torn posterior labrum were excised. The anterior and superior labra were found to be intact, and the suction seal of the labrum was maintained.
References
- 1.Matsuda D.K. A rare fracture, an even rarer trauma: The arthroscopic reduction and internal fixation of an isolated femoral head fracture. Arthroscopy. 2009;25:408–412. doi: 10.1016/j.arthro.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 2.Ledere S., Tauber M., Karpik S. Fractures of the femoral head. A multicenter study. Unfallchirurg. 2007;110:513–520. doi: 10.1007/s00113-007-1246-2. [in German] [DOI] [PubMed] [Google Scholar]
- 3.Park M.S., Yoon S.J., Choi S.M. Hip arthroscopic management for femoral head fractures and posterior acetabular wall fractures (Pipkin type IV) Arthrosc Tech. 2013;2:e221–e225. doi: 10.1016/j.eats.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stannard J.P., Harris H.W., Volgas D.A. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res. 2000;(377):44–56. doi: 10.1097/00003086-200008000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Pipkin G. Treatment of grade IV fracture dislocation of hip. J Bone Joint Surg Am. 1957;39:1027–1042. [PubMed] [Google Scholar]
- 6.Lansford T., Munns S.W. Arthroscopic treatment of Pipkin type I femoral head fractures: A report of 2 cases. J Orthop Trauma. 2012;26:e94–e96. doi: 10.1097/BOT.0b013e3182323f4f. [DOI] [PubMed] [Google Scholar]
- 7.Kalhor M., Beck M. Capsular and pericapsular contributions to acetabular and femoral head perfusion. J Bone Joint Surg Am. 2009;91:409–418. doi: 10.2106/JBJS.G.01679. [DOI] [PubMed] [Google Scholar]
- 8.Philippon M.J., Schenker M.L. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25:299–308. doi: 10.1016/j.csm.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Kelly B.T., Weiland D.E., Schenker M.L. Arthroscopic labral repair in the hip: Surgical technique and review of literature. Arthroscopy. 2005;21:1496–1504. doi: 10.1016/j.arthro.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Park M.S., Her I.S., Cho H.M. Internal fixation of femoral head fractures (Pipkin I) using hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014;22:898–901. doi: 10.1007/s00167-013-2821-4. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto Y., Ide T., Ono T. Usefulness of arthroscopic surgery in hip trauma cases. Arthroscopy. 2003;19:269–273. doi: 10.1053/jars.2003.50033. [DOI] [PubMed] [Google Scholar]
- 12.Philippon M.J., Kuppersmith D.A., Wolff A.B. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:169–174. doi: 10.1016/j.arthro.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Polesello G.C., Pereira G.R., Ricioli J.W. Current possibilities for hip arthroplasty. Rev Bras Ortop. 2014;49:103–110. doi: 10.1016/j.rboe.2014.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stabile K.J., Neumann J.A., Mannava S., Howse E.A., Stubbs A.J. Arthroscopic treatment of bucket-handle labral tear and acetabular fracture. Arthrosc Tech. 2014;3:e283–e287. doi: 10.1016/j.eats.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical procedure for arthroscopic reduction and internal fixation of femoral head fracture. The affected side was the right hip. The patient was positioned supine with the anterolateral portal used as the viewing portal and anterior portal used as the working portal. The peripheral compartment was visualized first with the limb in 45° of flexion. After evacuation of the fracture hematoma, the larger anteroinferior fracture fragment was seen and was mobilized from the central compartment to the anterior peripheral compartment with a probe. The fragment was gently reverted using the probe, and bone-to-bone apposition was obtained. Traction was applied, and the central compartment was explored to remove the smaller posteroinferior fragment in the cotyloid fossa. Traction was released, and the peripheral compartment was accessed with the limb in 30° of flexion, abduction, and external rotation. Under direct visualization, the anteroinferior fracture fragment was anatomically reduced using a grasper. By use of the distal accessory anterior portal, a guidewire was passed for temporary fixation of the fracture fragment. A 3-mm headless cannulated compression screw, with a lasso of Vicryl around the neck, was inserted perpendicular to the fracture site over the guidewire, and interfragmentary compression was obtained. After confirmation of joint stability under fluoroscopy, the smaller posterior acetabular rim fracture fragment and torn posterior labrum were excised. The anterior and superior labra were found to be intact, and the suction seal of the labrum was maintained.