Abstract
Osteophytes are physiological bony outgrowths that develop at the margins of the articular surfaces during the progression of osteoarthritis; they are associated with active endochondral bone formation processes and expressions of various growth factors. We believe they could be a source of bone grafts as a result of a potentially strong osteoinductive effect. Moreover, osteophytes can be easily harvested by arthroscopy in patients undergoing open-wedge high tibial osteotomy (OW-HTO) for medial unicompartmental knee osteoarthritis. Therefore, we have been using osteophyte autografts for osteotomy gaps in OW-HTO with positive preliminary results indicating rapid bone healing of osteotomy sites. In this technical note, we introduce a technique for harvesting autologous osteophytes by arthroscopy and implanting them into the gap formed after OW-HTO. We expect that autologous osteophyte grafting can be a useful method for accelerating bone union and therefore enabling weight bearing from an early stage after surgery, which will lead to an early return to social activities.
High tibial osteotomy (HTO) has been developed as an effective surgical intervention for patients with medial compartmental osteoarthritis of the knee caused by varus deformity, excessive loading on the medial compartment, and so on.1 In recent years, OW-HTO has become increasingly popular compared with closed-wedge HTO because the latter requires an additional osteotomy of the fibula and has a potential risk of complications such as peroneal nerve injury. However, a gap formed at the site of the osteotomy might be a disadvantage of OW-HTO because the gap can cause problems such as delayed bone union or loss of correction.2, 3 To resolve issues resulting from this gap, various bone grafts such as autologous iliac bone or bone graft substitutes are implanted into the gap at the osteotomy site. The results obtained after implantation of these materials have been evaluated by many studies.4, 5, 6, 7
Osteophytes are physiological bony outgrowths that develop mostly at the margins of the articular surfaces with the progression of osteoarthritis. The development of osteophytes is associated with the process of endochondral bone formation and expression of various growth factors such as transforming growth factor β, insulin-like growth factor 1, bone morphogenetic proteins, and cartilage-derived morphogenetic proteins.8, 9, 10, 11, 12 From the surgical viewpoint, osteophytes can be easily harvested by arthroscopy in patients with osteoarthritis of the knee. Therefore, osteophytes could be a source of bone grafts with an osteoinductive effect. We present a technique for harvesting autologous osteophytes by arthroscopy and implanting them into the osteotomy gap formed after OW-HTO (Video 1, Tables 1 and 2).
Table 1.
Pearls and Pitfalls
| Pearls |
| Making the anteromedial portal more medially than the conventional one is helpful in approaching the osteophytes at the medial edge of the medial femoral condyle. |
| The surgeon should identify the border between the osteophytes and the original cartilage margin and then cut off the osteophytes from the original cartilage margins with a 4-mm chisel and a hammer. |
| Adjusting the knee flexion angle according to the locations of the osteophytes can be helpful to harvest the osteophytes at the medial edge of the medial femoral condyle. |
| The osteotomy gap is filled with the harvested osteophytes including fibrous tissue, cartilage, and bones that were cut into small pieces. |
| The osteophytes should be packed sufficiently into the lateral hinge point. |
| Pitfalls |
| The surgeon must be careful not to cut into the ACL and PCL femoral attachments with the chisel. |
| The surgeon should carefully check all the compartments of the knee joint so as not to leave osteophyte fragments inside the knee joint. |
| The risk of damaging normal cartilage can be prevented by carefully identifying the border between the osteophytes and the original cartilage margin. |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Table 2.
Advantages, Risks, and Limitations of Autologous Osteophyte Grafting in OW-HTO
| Advantages |
| Harvesting and implantation of autologous osteophyte grafts are easy in OW-HTO. |
| Additional skin incision is unnecessary. |
| Bone-healing periods are shortened. |
| Knee extension is improved. |
| Risks and limitations |
| Bone fragments may be left inside the knee joint. |
| Hemarthrosis may be prolonged. |
| Small amounts of the harvested osteophytes may be prepared in early OA. |
| A prospective, randomized, comparative study should be carried out in the future. |
OA, osteoarthritis; OW-HTO, open-wedge high tibial osteotomy.
Surgical Technique
Indication
This technique was applied in patients undergoing OW-HTO for medial unicompartmental knee osteoarthritis with osteophytes. The exclusion criteria were as follows: symptomatic osteoarthritis of the lateral compartment of the knee, systemic inflammatory arthritis of the knee joint including infection, acute or chronic osteomyelitis of the tibia, and heavy smokers. All patients were informed about the procedure, as well as the possible risks and benefits of this study. This technique was carried out only in patients from whom consent was obtained. The institutional review board approved the study (Hamanomachi Hospital, approval No. 201244).
Preoperative Setup
The patient is positioned supine on the operating table under general and/or spinal anesthesia with a tourniquet inflated to 280 to 300 mm Hg. A lateral thigh support and a foot support attached to the operating table are useful to keep the operative knee at 90° of flexion. The opposite leg is placed lower than the operative leg, facilitating the approach to the medial side of the operative knee during the procedures (Fig 1).
Fig 1.
Patient positioning on operating table. With a lateral thigh support and a foot support, the operative knee (left) is placed at 90° of knee flexion during the procedure. The opposite leg (right) is placed lower than the operative leg.
Portal Placement and Diagnostic Arthroscopy
After the skin is sterilized and draped with an arthroscopic pouch drape, knee arthroscopy is performed using the anterolateral and anteromedial portals to evaluate all of the knee compartments. The anterolateral portal is made to be adjacent to the patellar tendon. Meanwhile, the anteromedial portal is made at the middle point between the patellar tendon and the medial edge of the medial femoral condyle, which is useful to harvest the osteophytes at the medial femoral condyle. Arthroscopic debridement including meniscectomy or synovectomy is applied, if necessary.
Arthroscopic Autologous Osteophyte Harvesting
First, the osteophytes at the tibial eminence in front of the anterior cruciate ligament (ACL) are carefully inspected and identified; they are then harvested using a 4-mm chisel and a hammer with the knee in a slightly flexed position (Fig 2). This procedure should be performed carefully to prevent the chisel from cutting into the tibial ACL attachment. Then, the osteophytes at the intercondylar notch are inspected, and the border between the osteophytes and the original cartilage margin is identified. Next, the osteophytes are cut off arthroscopically from the original cartilage margins with a 4-mm chisel and a hammer and are then harvested out of the knee joint through an anterior portal with a curette rongeur (Fig 3). During this procedure, it is necessary to be careful not to damage the femoral attachments of the ACL and the posterior cruciate ligament. Meanwhile, the osteophytes at the intercondylar notch are considered to cause the extension loss of the knee joint because they impinge on the anterior part of the tibial eminence in the knee-extended position. Therefore, one of the tips is to arthroscopically identify the osteophytes causing the impingement and extension loss and cut off these osteophytes as much as possible. For the osteophytes at the medial edge of the medial femoral condyle, like those at the tibial eminence and the intercondylar notch, it is essential to identify the border between the osteophytes and the original cartilage margin before osteophyte resection (Fig 4). The osteophytes are then cut off from the original cartilage margin using a 4-mm chisel inserted through the anteromedial portal and a hammer (Fig 5). The most important point during this procedure is to adjust the knee flexion angle according to the locations of the osteophytes. All of the resected osteophyte fragments should then be extracted from the joint with a curette rongeur.
Fig 2.
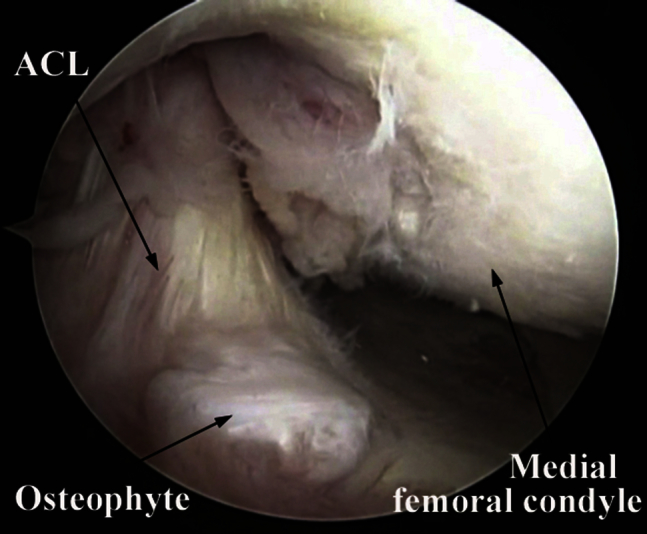
Intraoperative image from anterolateral portal (left knee, viewed with 4-mm, 30° arthroscope). The osteophytes at the tibial eminence in front of the anterior cruciate ligament (ACL) are visualized.
Fig 3.

Cutting off osteophytes (left knee, viewed with 4-mm, 30° arthroscope). A 4-mm chisel inserted from the anteromedial portal and a hammer are used to cut off the osteophytes at the intercondylar notch from the original cartilage margin.
Fig 4.
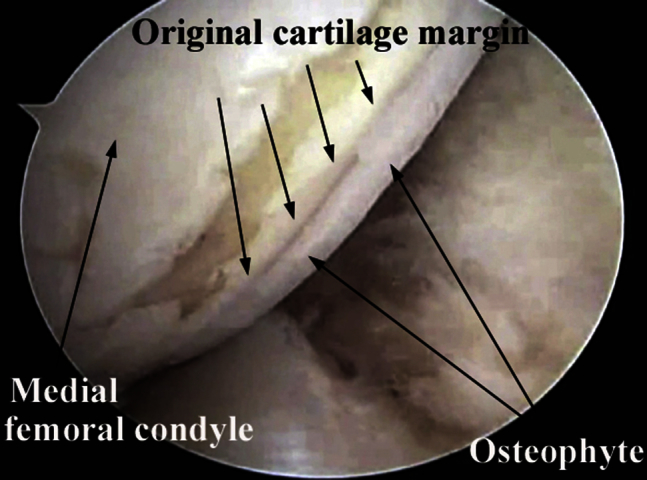
Intraoperative image from anterolateral portal (left knee, viewed with 4-mm, 30° arthroscope). The border between the osteophytes and the original cartilage margin at the medial edge of the medial femoral condyle is identified.
Fig 5.
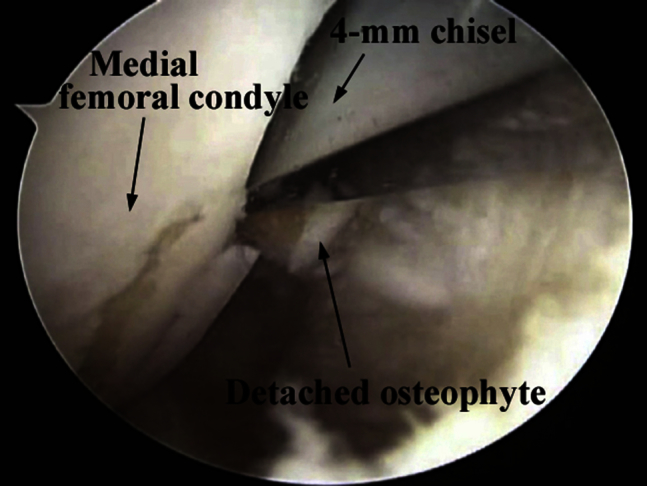
Harvesting of osteophytes at medial edge of medial femoral condyle (left knee, viewed with 4-mm, 30° arthroscope). With a 4-mm chisel inserted from the anteromedial portal and a hammer, the osteophytes at the medial edge of the medial femoral condyle are detached from the original cartilage. Adjusting the knee flexion angle according to the locations of the osteophytes can be helpful to harvest the osteophytes.
Finally, the surgeon should check all the compartments of the knee joint so as not to leave osteophyte fragments inside the knee joint. In general, it is unnecessary to insert a drain into the knee joint.
Open-Wedge HTO
A 5-cm longitudinal incision is made midway between the tibial tubercle and the posteromedial tibial cortex. The tendons of the pes anserinus and the superficial medial collateral ligament (sMCL) are sharply incised into an L shape at their furthest anterior and distal insertion through a periosteal incision and reflected as a flap until the starting point of the osteotomy is exposed (approximately 35 mm distal to the medial proximal tibial joint surface). A Cobb elevator is helpful in reflecting the sMCL and underlying periosteum. Special care should be taken to preserve the sMCL for later repair.
Two guidewires are inserted parallel with each other from the starting point of the osteotomy at the medial tibial cortex toward the lateral tibial cortex, while aiming at the tip of the fibular head. Then, the first oblique osteotomy is carried out along and below the guidewires using an oscillating saw. The second frontal ascending osteotomy is started 10 mm or more proximal to the insertion of the patellar tendon and combined with the first osteotomy plane (L-shaped biplane osteotomy). Thin osteotomes are useful for completing a series of osteotomy procedures. Under radioscopy, the first osteotomy site is opened with a bone spreader until the desired correction is achieved.
Autologous Osteophyte Grafting
Figure 6 shows the autologous osteophyte grafts immediately after being harvested. The autologous osteophyte grafts are cut into small pieces with bone rongeur forceps. The gap formed after the osteotomy is filled with the harvested osteophytes including fibrous tissue, cartilage, and bones that have been cut into small pieces. In particular, the osteophytes should be packed sufficiently into the lateral hinge point (Fig 7).
Fig 6.

Autologous osteophyte grafts just after harvesting.
Fig 7.
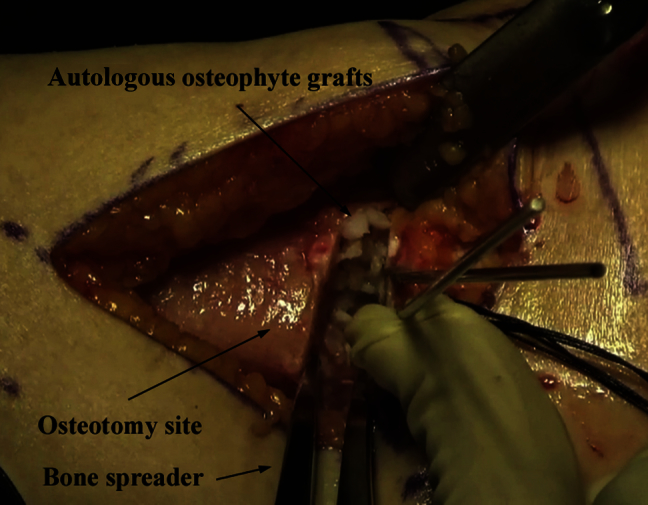
Implantation of osteophytes (left knee). The osteotomy site is opened with a bone spreader under fluoroscopic control until the desired angular correction is achieved. All of the osteophytes, having been cut into small pieces, including fibrous tissue, cartilage, and bones, are packed into the osteotomy gap, particularly into the lateral hinge point.
Fixation With Locking Plate and Screws
Either a TomoFix plate (Synthes, Paoli, PA) or a TRIS plate (Olympus, Tokyo, Japan) is then inserted into a subcutaneous tunnel formed on the medial side of the tibia. The plate is fixed with 8 locking screws. The reflected L-shaped flap of the tendons of the pes anserinus and sMCL is sutured and secured to the anterior remnant of the periosteum over the osteotomy gap. This procedure can also be helpful in preserving the hematoma at the osteotomy gap. The wound is closed after a surgical drain is placed.
Postoperative Rehabilitation
Active and passive range-of-motion exercises, including continuous passive motion exercises and quadriceps muscle–strengthening exercises, are started 2 days after the operation. Patients are permitted to start partial weight bearing with 2 crutches 1 week after the operation. Full weight bearing is allowed 4 weeks after the operation. Patients are permitted to resume normal sports activities including jogging 3 months after the operation.
Discussion
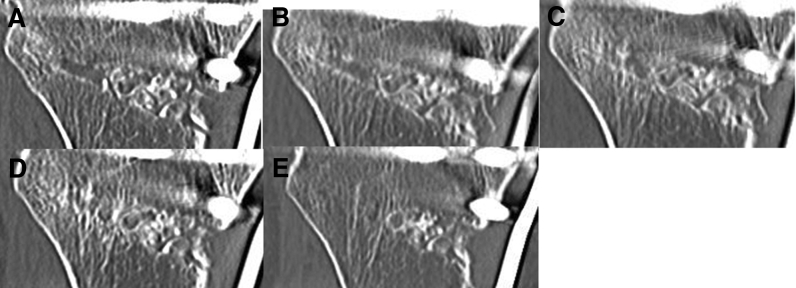
Staubli et al.13, 14 summarized the results of OW-HTO without bone grafting (with the TomoFix plate used as the fixation device). They concluded that OW-HTO with the TomoFix plate was effective in the treatment of unicompartmental gonarthrosis even without implantation of harvested bone or bone substitute materials. The bone-healing process after OW-HTO without bone grafting has also been evaluated. El-Assal et al.15 reported that bone healing was confirmed with radiographic images at 3 months postoperatively on average (12.4 weeks). Meanwhile, Brosset et al.16 examined radiographic images of 51 cases treated with OW-HTO without bone grafting and observed bone healing at 4.5 months postoperatively on average. In our study the bone-healing process was evaluated with computed tomography in 11 consecutive patients (3 male and 8 female patients) who underwent OW-HTO with autologous osteophyte grafting (Fig 8). The average age of the patients was 60.6 years. As a result, bone healing was observed at 5.3 weeks postoperatively on average. The computed tomography images provided us with an impression that the bone-healing process advanced favorably in OW-HTO with autologous osteophyte grafting compared with previous studies.15, 16 We also assessed bone healing in a patient who had undergone OW-HTO operations with bone grafting (autologous osteophyte grafting) in one knee and without bone grafting in the other knee. Bone healing at the site of osteotomy was accelerated more obviously for the knee treated with autologous osteophyte grafting than that for the knee without bone grafting (Fig 9).
Fig 8.
Coronal views of computed tomography images with multiplanar reconstruction (right knee). (A) At 4 weeks postoperatively, the osteotomy sites appear white. (B) At 6 weeks postoperatively, cloudy and thin trabecular continuity is observed between the osteophytes and the osteotomy sites. (C) At 8 weeks postoperatively, mature trabecular continuity is observed between the osteophytes and the osteotomy sites. (D, E) At 12 weeks and 24 weeks postoperatively, osteophyte grafts gradually become obscure from the lateral hinge toward the medial site.
Fig 9.
Coronal views of computed tomography images with multiplanar reconstruction (right knee at 4 weeks [A], 8 weeks [B], and 12 weeks [C] postoperatively and left knee at 4 weeks [D], 8 weeks [E], and 12 weeks [F] postoperatively). This patient underwent open-wedge high tibial osteotomy on both knees; the right knee was treated with autologous osteophyte grafting, and the left knee was treated without bone grafting. Bone healing at the osteotomy site was accelerated more obviously for the right knee than for the left knee.
According to Dodds and Gowen,17 an osteophyte contains all the components of the bone-remodeling cycle including the endochondral ossification process. Several studies have shown that osteophytes express various growth factors, such as insulin-like growth factors; transforming growth factor type β1, type β2, and type β3; platelet-derived growth factor; and interleukins 1β and 6.8, 9, 10, 11, 18 Meanwhile, several researchers have suggested that bone morphogenetic proteins play an important role in the growth and development of bones and have the ability to induce and promote the formation of cartilage and bone at an ectopic site.19, 20, 21, 22 There is a possibility that these growth factors expressed in osteophytes exert an anabolic effect on the surrounding osteogenic cells at the graft sites and promote bone healing.
Our technique would be advantageous in shortening the bone-healing period and improving range of motion, especially increasing extension through the resection of the osteophytes at the tibial eminence in front of the ACL and the intercondylar notch. Moreover, this technique requires no additional skin incision, differing from autologous iliac crest bone grafting. Meanwhile, disadvantages of this technique are the possibility of leaving bone fragments inside the knee joint and the prolonged hemarthrosis of the knee joint. However, we have not encountered these complications. We consider that a careful and deliberate operation can prevent such unfavorable events from occurring.
As a major limitation, this technical note is based on neither a randomized controlled trial nor a comparative study between the use and nonuse of bone grafts. We consider that a prospective, randomized, comparative study between an operative technique using autologous osteophyte grafts and an operative technique not using any grafts is necessary to verify the validity of our hypothesis.
In conclusion, we have introduced a surgical technique for accelerating bone healing at the open-wedge osteotomy site. We expect that this method will enable weight bearing from an early stage after surgery, which will lead to an early return to social activities.
Acknowledgment
The authors thank Kisato Saito for editorial assistance in the preparation of the article.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical technique of autologous osteophyte grafting for open-wedge high tibial osteotomy in a right knee. The patient is positioned supine on the operating table under general and/or spinal anesthesia. Images obtained through a 4-mm, 30° arthroscope inserted from the anterolateral portal are used to show the technique for harvesting autologous osteophytes. The osteophytes are cut off arthroscopically with a 4-mm chisel and a hammer and then removed from the knee joint with a curette rongeur. The harvested grafts are cut into small pieces with bone rongeur forceps. After the osteotomy site is opened by a bone spreader under fluoroscopic control until the desired angular correction is achieved, all osteophytes, having been cut into small pieces, are implanted into the osteotomy gap, particularly into the lateral hinge point.
References
- 1.Floerkenmeier S., Staubli A.E., Schroeter S., Goldhahn S., Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: A retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2013;21:170–180. doi: 10.1007/s00167-012-2087-2. [DOI] [PubMed] [Google Scholar]
- 2.Schröter S., Freude T., Kopp M.M. Smoking and unstable hinge fractures cause delayed gap filling irrespective of early weight bearing after open wedge osteotomy. Arthroscopy. 2015;31:254–265. doi: 10.1016/j.arthro.2014.08.028. [DOI] [PubMed] [Google Scholar]
- 3.Warden S.J., Morris H.G., Crossley K.M., Brukner P.D., Bennell K.L. Delayed and non-union following opening wedge high tibial osteotomy: Surgeons' results from 182 completed cases. Knee Surg Sports Traumatol Arthrosc. 2005;13:34–37. doi: 10.1007/s00167-003-0485-1. [DOI] [PubMed] [Google Scholar]
- 4.Lash N.J., Feller J.A., Batty L.M., Wasiak J., Richmond A.K. Bone grafts and bone substitutes for opening-wedge osteotomies of the knee: A systematic review. Arthroscopy. 2015;31:720–730. doi: 10.1016/j.arthro.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Ozalay M., Sahin O., Akpinar S., Ozkoc G., Cinar M., Cesur N. Remodeling potentials of biphasic calcium phosphate granules in open-wedge high tibial osteotomy. Arch Orthop Trauma Surg. 2009;129:747–752. doi: 10.1007/s00402-008-0781-9. [DOI] [PubMed] [Google Scholar]
- 6.Takeuchi R., Ishikawa H., Aratake M. Medial opening wedge high tibial osteotomy with early full weight bearing. Arthroscopy. 2009;25:46–53. doi: 10.1016/j.arthro.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 7.van Hemert W.L., Willems K., Anderson P.G., van Heerwaarden R.J., Wymenga A.B. Tricalcium phosphate granules or rigid wedge preforms in open wedge high tibial osteotomy: A radiological study with a new evaluation system. Knee. 2004;11:451–456. doi: 10.1016/j.knee.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Dodds R.A., Merry K., Littlewood A., Gowen M. Expression of mRNA for IL1 beta, IL6 and TGF beta 1 in developing human bone and cartilage. J Histochem Cytochem. 1994;42:733–744. doi: 10.1177/42.6.8189035. [DOI] [PubMed] [Google Scholar]
- 9.Horner A., Kemp P., Summers C. Expression and distribution of transforming growth factor-beta isoforms and their signaling receptors in growing human bone. Bone. 1998;23:95–102. doi: 10.1016/s8756-3282(98)00080-5. [DOI] [PubMed] [Google Scholar]
- 10.Middleton J., Arnott N., Walsh S., Beresford J. Osteoblasts and osteoclasts in adult human osteophyte tissue express the mRNAs for insulin-like growth factors I and II and the type 1 IGF receptor. Bone. 1995;16:287–293. doi: 10.1016/8756-3282(94)00040-9. [DOI] [PubMed] [Google Scholar]
- 11.Okazaki K., Jingushi S., Ikenoue T. Expression of insulin-like growth factor I messenger ribonucleic acid in developing osteophytes in murine experimental osteoarthritis and in rats inoculated with growth hormone-secreting tumor. Endocrinology. 1999;140:4821–4830. doi: 10.1210/endo.140.10.7053. [DOI] [PubMed] [Google Scholar]
- 12.Zoricic S., Maric I., Bobinac D., Vukicevic S. Expression of bone morphogenetic proteins and cartilage-derived morphogenetic proteins during osteophyte formation in humans. J Anat. 2003;202(pt 3):269–277. doi: 10.1046/j.1469-7580.2003.00158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Staubli A.E., De Simoni C., Babst R., Lobenhoffer P. TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia—Early results in 92 cases. Injury. 2003;34(suppl 2):B55–B62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 14.Staubli A.E., Jacob H.A. Evolution of open-wedge high-tibial osteotomy: Experience with a special angular stable device for internal fixation without interposition material. Int Orthop. 2010;34:167–172. doi: 10.1007/s00264-009-0902-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El-Assal M.A., Khalifa Y.E., Abdel-Hamid M.M., Said H.G., Bakr H.M. Opening-wedge high tibial osteotomy without bone graft. Knee Surg Sports Traumatol Arthrosc. 2010;18:961–966. doi: 10.1007/s00167-010-1104-6. [DOI] [PubMed] [Google Scholar]
- 16.Brosset T., Pasquier G., Migaud H., Gougeon F. Opening wedge high tibial osteotomy performed without filling the defect but with locking plate fixation (TomoFixTM) and early weight-bearing: Prospective evaluation of bone union, precision and maintenance of correction in 51 cases. Orthop Traumatol Surg Res. 2011;97:705–711. doi: 10.1016/j.otsr.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 17.Dodds R.A., Gowen M. The growing osteophyte: A model system for the study of human bone development and remodeling in situ. J Histotechnol. 1994;17:37–45. [Google Scholar]
- 18.Horner A., Bord S., Kemp P., Grainger D., Compston J.E. Distribution of platelet-derived growth factor (PDGF) A chain mRNA, protein, and PDGF-alpha receptor in rapidly forming human bone. Bone. 1996;19:353–362. doi: 10.1016/s8756-3282(96)00217-7. [DOI] [PubMed] [Google Scholar]
- 19.Bosemark P., Isaksson H., McDonald M.M., Little D.G., Tägil M. Augmentation of autologous bone graft by a combination of bone morphogenic protein and bisphosphonate increased both callus volume and strength. Acta Orthop. 2013;84:106–111. doi: 10.3109/17453674.2013.773123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reddi A.H. Role of morphogenetic proteins in skeletal tissue engineering and regeneration. Nat Biotechnol. 1998;16:247–252. doi: 10.1038/nbt0398-247. [DOI] [PubMed] [Google Scholar]
- 21.Wozney J.M., Rosen V. Bone morphogenetic protein and bone morphogenetic protein gene family in bone formation and repair. Clin Orthop Relat Res. 1998:26–37. [PubMed] [Google Scholar]
- 22.Wozney J.M., Rosen V., Celeste A.J., Mitsock L.M., Whitters M.J., Kriz R.W. Novel regulators of bone formation. Molecular clones and activities. Science. 1988;242:1528–1534. doi: 10.1126/science.3201241. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique of autologous osteophyte grafting for open-wedge high tibial osteotomy in a right knee. The patient is positioned supine on the operating table under general and/or spinal anesthesia. Images obtained through a 4-mm, 30° arthroscope inserted from the anterolateral portal are used to show the technique for harvesting autologous osteophytes. The osteophytes are cut off arthroscopically with a 4-mm chisel and a hammer and then removed from the knee joint with a curette rongeur. The harvested grafts are cut into small pieces with bone rongeur forceps. After the osteotomy site is opened by a bone spreader under fluoroscopic control until the desired angular correction is achieved, all osteophytes, having been cut into small pieces, are implanted into the osteotomy gap, particularly into the lateral hinge point.