Abstract
Idiopathic adhesive capsulitis of the shoulder is a relatively common condition that results in pain and loss of motion due to capsular thickening and fibrosis. Most cases are successfully treated with conservative management including physical therapy and intra-articular steroid injections. If conservative management fails, arthroscopic capsular release allows precise release of thickened capsular tissue with a lower risk of complications and less soft-tissue trauma than manipulation under anesthesia alone. Arthroscopic capsular release in the beach-chair position typically requires some degree of manipulation to release the inferior capsule, which is often not visualized intraoperatively. In this technique article and video, we describe and demonstrate a technique of arthroscopic capsular release in the lateral decubitus position, providing a clear view of the inferior capsule, which facilitates a complete, 360° capsular release and mitigates the need for any manipulation under anesthesia.
Idiopathic adhesive capsulitis of the shoulder is a relatively common condition that results in pain and loss of motion as a result of capsular thickening and fibrosis.1 Associated conditions include diabetes, thyroid disorders, and female gender.1 Clinically, patients experience stages of freezing, frozen, and thawing in which the shoulder becomes painful, range of motion is decreased, and there is a gradual return of motion over 6 to 12 months. The majority of patients experience symptomatic relief in 6 to 12 months, with physical therapy and intra-articular cortisone injections used to help relieve pain and possibly to accelerate recovery.2 Despite this, almost half of patients with adhesive capsulitis have been reported to have some residual pain and loss of motion at long-term follow-up after nonoperative management.3, 4
For patients who fail conservative interventions, arthroscopic capsular release is the mainstay treatment option.5 Manipulation under anesthesia (MUA) without arthroscopic capsular release is effective6 but may result in iatrogenic injury,7, 8 including fracture. Arthroscopic capsular release involves selective release of the capsule, often with electrocautery, in order to minimize the risk of iatrogenic injury as compared with MUA (Table 1). Secondarily, this may decrease postoperative pain and facilitate early participation in physical therapy. Arthroscopic capsular release performed in the beach-chair position has shown rapid short-term improvements beginning 1 week after surgery as well as promising long-term outcomes with a significant reduction in pain severity and frequency and improved range of motion compared with the contralateral uninvolved shoulder.9, 10 These improvements were maintained or continued to increase at a mean of 7 years postoperatively.9
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| We prefer the use of an arthroscopic basket to complete the inferior capsular release while minimizing potential for damage to the axillary nerve. | Pad and carefully position all bony prominences and the contralateral arm when positioning patient in lateral decubitus position. |
| Document detailed examination both in the office and under anesthesia, including range of motion in all planes. | Careful dissection near the 6 o'clock position to avoid axillary nerve damage. |
| Visualization of rotator cuff musculature circumferentially confirms complete capsular release. | Postoperative therapy should begin postoperative day 1 with aggressive range of motion and home continuous passive motion. Delays in therapy can compromise outcomes. |
Arthroscopic capsular release is generally described in the beach-chair position.11 Some degree of manipulation is often used to complete the release of the inferior capsule due to difficulty accessing this region and the proximity of the axillary nerve.11 The benefits of beach-chair versus lateral decubitus positioning have been debated in the literature, mostly regarding arthroscopic instability procedures.12 Potential advantages of arthroscopic capsular release in the lateral position include increased glenohumeral joint space resulting from lateral and axial traction, improved visualization of and access to the inferior capsule and labrum, and better cerebral perfusion (Table 2). In addition, the capsular tissues are under traction, which causes the capsule to retract when cut because it is under tension, exposing the rotator cuff musculature to ensure complete release.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Improved glenohumeral joint lateral and axial distraction allowing better visualization and instrumented release of inferior capsule. | Unfamiliar setup and orientation for surgeon accustomed to beach-chair shoulder arthroscopy. |
| Reduces or eliminates need for manipulation under anesthesia due to complete 360° capsular release, which could reduce risk of iatrogenic damage from manipulation. | May be more difficult to perform any concomitant subacromial or open procedures. |
| Capsular tissues are under tension, facilitating selective release and visualization of completed release due to capsular retraction after release. | Potential for damage to axillary nerve while releasing the 6 o'clock position. |
| Potential for less postoperative bleeding and pain due to controlled release without manipulation. |
We describe our technique for arthroscopic 360° capsular release in the lateral decubitus position.
Surgical Technique
Preoperative Setup
The procedure is performed under interscalene block with conscious sedation. The patient is positioned in the lateral decubitus position, taking care to pad all bony prominences, an axillary roll placed under the contralateral arm, and the neck placed in a neutral position. An examination under anesthesia is performed to document motion in all planes (external and internal rotation with arm at the side, forward flexion, abduction, and external and internal rotation with the arm abducted to 90°; Video 1). The arm is prepped and draped sterilely and placed in a lateral distraction device (Spider 2 Limb Positioner, Smith and Nephew, Andover, MA; Fig 1).
Fig 1.
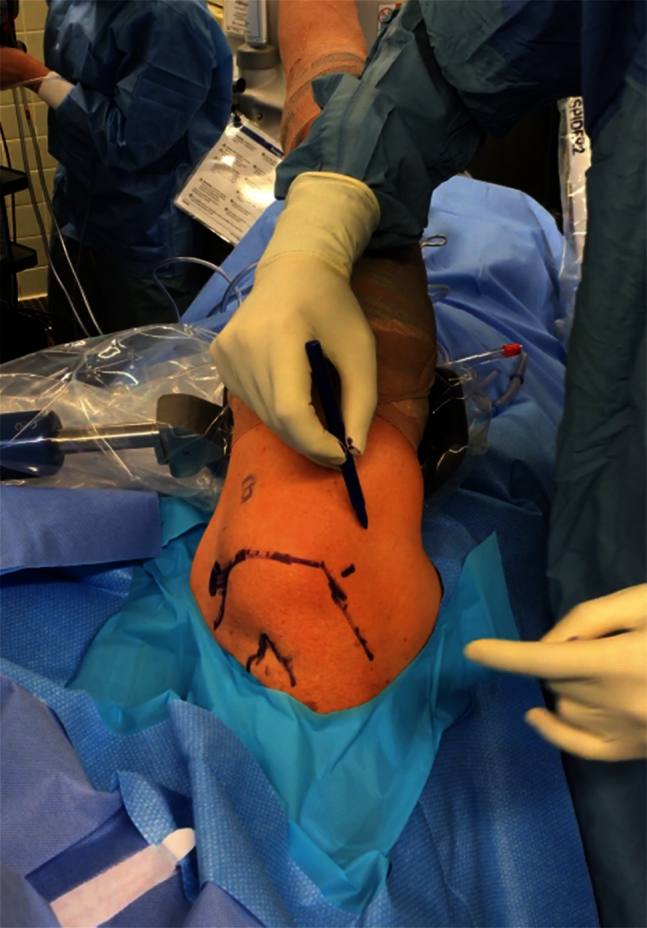
Patient is positioned in the lateral decubitus position with a lateral distraction device. In this case, the right shoulder is prepped and draped. Markings are made of the bony landmarks including the acromion, clavicle, and coracoid in order to define the locations of the anterior and posterior portals. The posterior viewing portal is positioned just off the posterolateral corner of the acromion, and an anterior rotator interval working portal is made just lateral to the coracoid.
Portal Placement
The bony landmarks are marked, and a posterior portal is established just off the posterolateral corner of the acromion. An anterior portal in the rotator interval is then established via spinal needle localization. Diagnostic arthroscopy is performed, generally showing capsulitis and capsular thickening and fibrosis (Fig 2). It is important to determine and document the status of the rotator cuff, articular cartilage, and biceps tendon.
Fig 2.
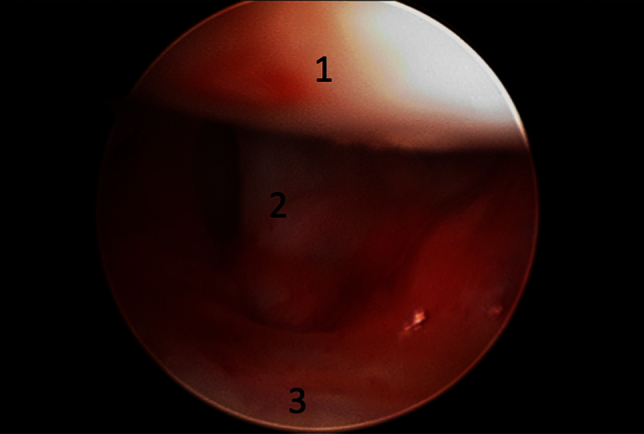
Diagnostic arthroscopy is performed in the lateral decubitus position on the right shoulder with posterior viewing portal showing capsulitis and capsular thickening. 1, humeral head; 2, subscapularis; 3, glenoid.
Anterior Release
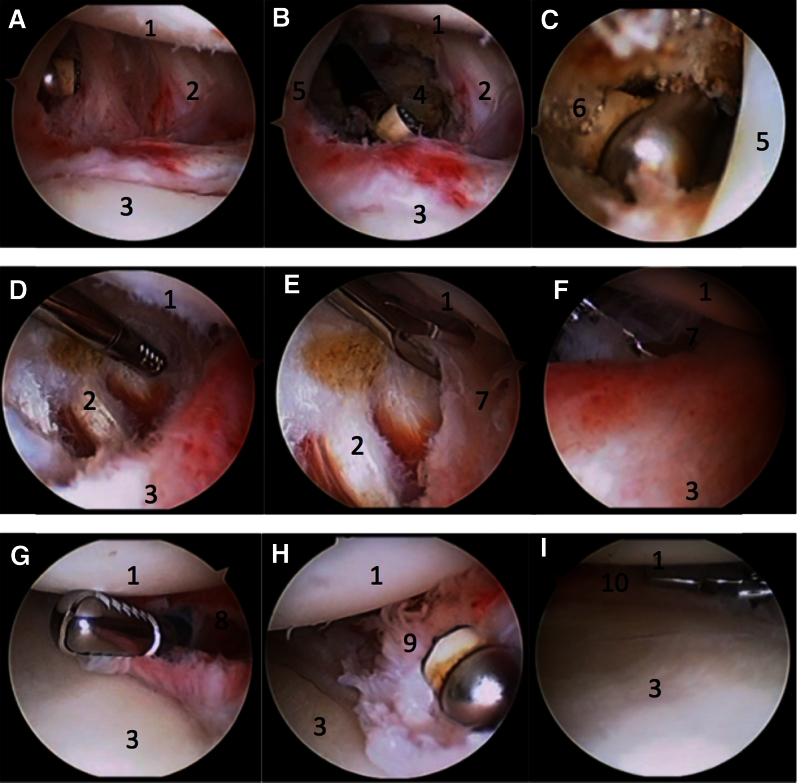
An arthroscopic shaver (Dyonics Platinum Incisors Elite 4.5 mm, Smith and Nephew) and radiofrequency (RF) ablation device (Super Turbovac 90, Smith and Nephew) are used to thoroughly release the rotator interval (Fig 3A) from the biceps tendon to the superior edge of the subscapularis tendon and down to the coracoid (Fig 3B). The RF is taken above the long head of the biceps tendon to release the anterior superior capsule (Fig 3C). The capsule is then released posterior to the subscapularis in a superior to inferior direction, visualizing the subscapularis muscle fibers lying just anterior to the glenoid (Fig 3D). The RF and shaver are used more superiorly followed by a basket more inferiorly (Table 1) taking care to remain close to the labrum and release only the capsular layer in the anteroinferior location due to the proximity of the axillary nerve at the 6 o'clock position (Fig 3 E and F).
Fig 3.
Capsular release in the lateral decubitus position is performed on a right shoulder. The steps of the release are shown. (A) A posterior viewing portal is used with an anterior working portal to begin by releasing the rotator interval with a radiofrequency (RF) device. (B) The rotator interval is released from the biceps tendon to the superior edge of the subscapularis tendon and down to the coracoid. (C) The anterior superior capsule is released above the biceps without damaging the underlying supraspinatus. (D) The RF and shaver are used to then release the anterior capsule lying posterior to the subscapularis until the subscapularis muscle is visualized. (E, F) At the inferior position, we use an arthroscopic basket, which we find provides a more precise release to decrease potential damage to the nearby axillary nerve. The camera is switched to view from anteriorly in order to complete the posterior release. (G) The shaver and RF are used to complete the posterior superior capsular release. (H) The RF device is used to continue the posterior release inferiorly. (I) We prefer to use a basket to complete the most inferior capsular release. 1, humeral head; 2, subscapularis; 3, glenoid; 4, coracoid; 5, long head of the biceps tendon; 6, anterior superior capsule beneath the supraspinatus; 7, anterior inferior capsule; 8, posterosuperior capsule; 9, posterior capsule; 10, posterior inferior capsule.
Posterior Release
Once the anterior portion of the release is complete, the camera is switched to view from the anterior portal. The posterosuperior capsule is then released using a shaver and RF (Fig 3G). Then the RF and basket are used to release the posteroinferior capsule (Fig 3H), again, exhibiting caution inferiorly and releasing the capsule from the capsulolabral junction to minimize risk of iatrogenic injury to the axillary nerve located approximately in the 6 o'clock position (Fig 3I). Care is also taken to protect the labrum and articular surfaces from iatrogenic damage. Complete capsular release of 360° is confirmed by arthroscopic visualization of the rotator cuff musculature circumferentially (Fig 4A-C).
Fig 4.
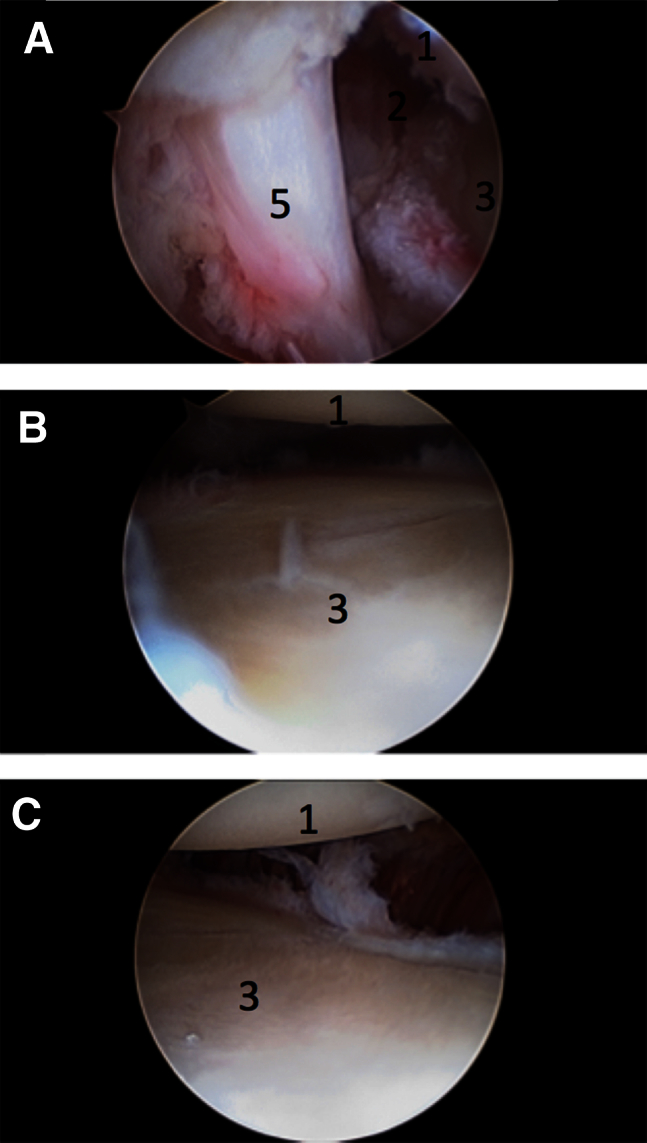
Arthroscopic images from the lateral decubitus position in a right shoulder demonstrate completed 360° capsular release from the posterior viewing portal (A) anteriorly and (B) inferiorly. (C) The posterior release is viewed from the anterior portal. 1, humeral head; 2, subscapularis; 3, glenoid; 5, long head of the biceps tendon.
Postrelease Examination
The arm is released from the traction device, and an examination under anesthesia is repeated, documenting improvements in the aforementioned positions. Typically, an MUA is not required, as complete, circumferential capsular release has been achieved. In cases of idiopathic adhesive capsulitis, subacromial decompression is not performed; however, in cases of traumatic or postoperative adhesive capsulitis, subacromial decompression is routinely performed.
Postoperative Protocol
The patient is placed into a standard arm sling and discharged on the same day of surgery to home. Range of motion is immediately encouraged. The sling is discontinued on postoperative day 1. Outpatient physical therapy begins on postoperative day 1, emphasizing aggressive active and passive range of motion exercises along with scapular and rotator cuff reactivation with strengthening initiated once motion is near normal. Home continuous passive motion devices are used for 4 weeks postoperatively.
Discussion
In this technical note, we describe a technique of arthroscopic capsular release with the patient in the lateral decubitus position. Classically, this procedure has been described in the beach-chair position, but as demonstrated in the video, the lateral decubitus position improves visualization and access to the inferior capsule. This facilitates a complete 360° capsular release, mitigates the need for an MUA, and minimizes the risk for iatrogenic injury. Ultimately, complete release of the inferior capsule in the lateral decubitus position has been shown to improve range of motion, including abduction, and internal and external rotation.13
The primary concern regarding the release of the inferior capsule is injury to the axillary nerve due to its close proximity. The nerve passes inferiorly to the subscapularis muscle and lies immediately adjacent to the capsule before entering the quadrangular space. In order to perform this procedure safely, the anatomic relationship of the nerve to the joint capsule must be known. Jerosch et al.14 demonstrated that the axillary nerve is in close relation to the capsule between the 5 and 7 o'clock positions, therefore care should be taken when operating in this vicinity. During the 360° release as described in this technique, the surgeon may avoid nerve injury by identifying the nerve by passing a blunt instrument adjacent to the insertion of the long head of the triceps on the infraglenoid tubercle of the scapula. Risk of injury may be further reduced by the use of an arthroscopic biter in the axillary pouch and performing the capsular release at the capsulolabral junction.
In a randomized trial, Chen et al.15 examined the impact of releasing the inferior and posterior portion of the inferior glenohumeral ligament (270° capsular release) compared with release of the anterior capsule only (180° capsular release) in patients with idiopathic adhesive capsulitis. In this study, it was found that extending the release resulted in a more rapid improvement of range of motion. Massoud et al.16 performed a prospective cohort study examining different treatment modalities for adhesive capsulitis including operative intervention with capsular release in the lateral decubitus position. The investigators found that in patients with diabetes mellitus, capsular release in the lateral position produced good outcomes with maximum relief of pain and improved function 3 months postoperatively.
The advantages and disadvantages of lateral decubitus patient positioning versus beach-chair have been well described.17 Ultimately, surgeons' preference for patient positioning based on training experience is a key factor, as their level of comfort dictates decision-making. The advantages of performing an arthroscopic shoulder surgery in the lateral decubitus position includes the ability to use traction to increase visualization, particularly in the axillary recess and inferior glenohumeral joint, and improved cerebral perfusion. For capsular release specifically, the lateral decubitus position permits improved access for release of the inferior capsule, allowing for a full 360° release, which is a technical challenge in the beach-chair position. When performed in beach chair, MUA may be needed to augment the procedure in order to address inflamed/scarred capsular tissue inferiorly. However, numerous complications can result, including shoulder dislocation, labral lesions, nerve palsy, humeral fracture, and rotator cuff tear. By performing the release of the inferior capsule arthroscopically, one can avoid these potentially serious complications.
In conclusion, the arthroscopic 360° capsular release in the lateral decubitus position provides a comprehensive surgical treatment for patients with adhesive capsulitis by addressing inflamed/scarred capsular tissue in its entirety and obviating the need for MUA when performed in the beach-chair position.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.H. receives support from Nuvasive and Novartis. A.R. receives support from the American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons, Orthopedics, Orthopedics Today, SAGE, SLACK, Wolters Kluwer Health, Arthrex, Saunders/Mosby-Elsevier, Ossur, and Smith & Nephew; N.V. receives support from American Shoulder and Elbow Surgeons, Arthroscopy Association Learning Center, Journal of Knee Surgery, SLACK, Minivasive, Orthospace, Smith & Nephew, Arthroscopy, Vindico Medical Orthopedics Hyperguide, Cymedica, Omeros, Arthrex, Arthrosurface, DJ Orthopaedics, Athletico, ConMed Linvatec, Miomed, and Mitek.
Supplementary Data
A technique for 360° arthroscopic capsular release for adhesive capsulitis of the shoulder in the lateral decubitus position is presented using a combination of external and arthroscopic video as well as narration of the critical steps. The patient is positioned in the lateral decubitus position with the right shoulder prepped and draped. Preoperative examination under anesthesia is performed, demonstrating decreased range of motion especially in external rotation. A posterior viewing portal is used initially with an anterior working portal to complete the anterior release using an arthroscopic shaver and radiofrequency device. Subsequently, the anterior portal is used for viewing with the posterior working portal to complete the posterior release. A basket is used for inferior release both anteriorly and posteriorly.
References
- 1.Neviaser A.S., Neviaser R.J. Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg. 2011;19:536–542. doi: 10.5435/00124635-201109000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Levine W.N., Kashyap C.P., Bak S.F., Ahmad C.S., Blaine T.A., Bigliani L.U. Nonoperative management of idiopathic adhesive capsulitis. J Shoulder Elbow Surg Am. 2007;16:569–573. doi: 10.1016/j.jse.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Hand C., Clipsham K., Rees J.L., Carr A.J. Long-term outcome of frozen shoulder. J Shoulder Elbow Surg Am. 2008;17:231–236. doi: 10.1016/j.jse.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Shaffer B., Tibone J.E., Kerlan R.K. Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am. 1992;74:738–746. [PubMed] [Google Scholar]
- 5.Ogilvie-Harris D.J., Biggs D.J., Fitsialos D.P., MacKay M. The resistant frozen shoulder. Manipulation versus arthroscopic release. Clin Orthop Relat Res. 1995:238–248. [PubMed] [Google Scholar]
- 6.Farrell C.M., Sperling J.W., Cofield R.H. Manipulation for frozen shoulder: long-term results. J Shoulder Elbow Surg Am. 2005;14:480–484. doi: 10.1016/j.jse.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Loew M., Heichel T.O., Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg Am. 2005;14:16–21. doi: 10.1016/j.jse.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Magnussen R.A., Taylor D.C. Glenoid fracture during manipulation under anesthesia for adhesive capsulitis: a case report. J Shoulder Elbow Surg Am. 2011;20:e23–e26. doi: 10.1016/j.jse.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 9.Le Lievre H.M., Murrell G.A. Long-term outcomes after arthroscopic capsular release for idiopathic adhesive capsulitis. J Bone Joint Surg Am. 2012;94:1208–1216. doi: 10.2106/JBJS.J.00952. [DOI] [PubMed] [Google Scholar]
- 10.Barnes C.P., Lam P.H., Murrell G.A. Short-term outcomes after arthroscopic capsular release for adhesive capsulitis. J Shoulder Elbow Surg Am. 2016;25:e256–e264. doi: 10.1016/j.jse.2015.12.025. [DOI] [PubMed] [Google Scholar]
- 11.Arce G. Primary frozen shoulder syndrome: arthroscopic capsular release. Arthrosc Tech. 2015;4:e717–e720. doi: 10.1016/j.eats.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frank R.M., Saccomanno M.F., McDonald L.S., Moric M., Romeo A.A., Provencher M.T. Outcomes of arthroscopic anterior shoulder instability in the beach chair versus lateral decubitus position: a systematic review and meta-regression analysis. Arthroscopy. 2014;30:1349–1365. doi: 10.1016/j.arthro.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Jerosch J. 360 degrees arthroscopic capsular release in patients with adhesive capsulitis of the glenohumeral joint—indication, surgical technique, results. Knee Surg Sports Traumatol Arthrosc. 2001;9:178–186. doi: 10.1007/s001670100194. [DOI] [PubMed] [Google Scholar]
- 14.Jerosch J., Filler T.J., Peuker E.T. Which joint position puts the axillary nerve at lowest risk when performing arthroscopic capsular release in patients with adhesive capsulitis of the shoulder? Knee Surg Sports Traumatol Arthrosc. 2002;10:126–129. doi: 10.1007/s00167-001-0270-y. [DOI] [PubMed] [Google Scholar]
- 15.Chen J., Chen S., Li Y., Hua Y., Li H. Is the extended release of the inferior glenohumeral ligament necessary for frozen shoulder? Arthroscopy. 2010;26:529–535. doi: 10.1016/j.arthro.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 16.Massoud S.N., Pearse E.O., Levy O., Copeland S.A. Operative management of the frozen shoulder in patients with diabetes. J Shoulder Elbow Surg Am. 2002;11:609–613. doi: 10.1067/mse.2002.127301. [DOI] [PubMed] [Google Scholar]
- 17.Li X., Eichinger J.K., Hartshorn T., Zhou H., Matzkin E.G., Warner J.P. A comparison of the lateral decubitus and beach-chair positions for shoulder surgery: advantages and complications. J Am Acad Orthop Surg. 2015;23:18–28. doi: 10.5435/JAAOS-23-01-18. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A technique for 360° arthroscopic capsular release for adhesive capsulitis of the shoulder in the lateral decubitus position is presented using a combination of external and arthroscopic video as well as narration of the critical steps. The patient is positioned in the lateral decubitus position with the right shoulder prepped and draped. Preoperative examination under anesthesia is performed, demonstrating decreased range of motion especially in external rotation. A posterior viewing portal is used initially with an anterior working portal to complete the anterior release using an arthroscopic shaver and radiofrequency device. Subsequently, the anterior portal is used for viewing with the posterior working portal to complete the posterior release. A basket is used for inferior release both anteriorly and posteriorly.