Abstract
The impact of interventions to increase physical activity (PA) may vary as a function of participants' barriers to PA. The aim of this paper is to determine whether individual barriers (demographic, physical health, psychological health, neighborhood factors, perceived barriers to PA, social support for PA) moderate treatment effects on increases in PA. Three treatment conditions tested the relative efficacy of a group-based PA intervention alone or supplemented by either personal or automated phone calls made between group meetings. From 2010 to 2012, 284 African American women (ages 40–65) living in the Chicago, IL, area were randomized to one of the three treatment conditions. Data collection occurred at baseline as well as 24 and 48 weeks after baseline. Moderation of intervention effects by barriers to PA were tested across four outcome measures (self-reported moderate-vigorous PA, self-reported walking, accelerometer steps, and aerobic fitness) using multilevel mixed-effects analyses. Significant condition by barrier interaction effects for the accelerometer steps outcome were found for material hardships, general health, depressive symptoms, neighborhood crime rate, and perceived barriers to PA. For aerobic fitness, intervention effects were moderated by material hardships and perceived pain. Increases in the outcome variables were greater for the conditions in which group sessions were supplemented with personal and/or automated calls. Among participants with greater barriers to PA, supplementing the intervention group meetings with between-session personal and/or automated phone calls may be an effective way to strengthen intervention effects. These results may inform the use of treatment supplements in the context of adaptive interventions.
Keywords: Physical activity, African American, Women, Intervention moderation
Highlights
-
•
Women in all three intervention conditions increased physical activity.
-
•
Between-group telephone calls benefited women with specific barriers.
-
•
Problem solving during telephone calls may be mechanism of effect.
-
•
Adaptive intervention research should test telephone calls for non-responders.
1. Introduction
African American women have a higher prevalence of hypertension, cardiovascular disease, diabetes and obesity compared to non-Hispanic White women (Mozaffarian et al., 2015). Physical activity (PA) is a well-established method of reducing disease risks associated with inactivity and obesity (Mozaffarian et al., 2015). Current guidelines recommend participating in moderate PA (brisk walking) for 150 min/week in episodes of at least 10 min (US Department of Health and Human Services, 2008). However, only 35% of Chicago-area African American women meet these recommendations compared to 47% of women countywide (Liao et al., 2011).
Many African American women have substantial barriers to PA. Frequently reported barriers to leisure-time PA include demands of work, school, home, children, partners, and social obligations (Pekmezi et al., 2013, Siddiqi et al., 2011); mental fatigue from physically demanding jobs (Forthofer et al., 2016); perceptions that “leisure time” does not exist for them (Airhihenbuwa et al., 1995, Yeager et al., 1993); or is an unaffordable indulgence (Kriska and Rexroad, 1998, Wilbur et al., 2002); and that adequate PA is obtained by living a “busy life” (Wilbur et al., 2002). Additional barriers include health problems (Bopp et al., 2006) that may develop or worsen when obese, sedentary individuals increase their PA. Neighborhood environmental characteristics also present barriers to PA, including concerns about harassment, feeling unsafe at local parks, and gang activity (Baruth et al., 2014). Neighborhood socioeconomic factors have been linked to health behaviors such as PA (Diez Roux, 2016). Inequitable distribution of resources such as exercise facilities, walkable sidewalks, and street lights may present additional barriers to increasing PA among lower income African American women (Mama et al., 2015).
In addition to limiting levels of PA, barriers to PA may also moderate the impact of interventions to increase PA. To date, few studies examine moderators of intervention effects on PA among adults (Luten et al., 2016). The existing studies of moderation in PA interventions often focus on demographic factors such as gender (Luten et al., 2016, Wilcox et al., 2009), age (van Stralen et al., 2010, Wilcox et al., 2009), and education (Luten et al., 2016). These studies also have identified psychosocial moderators, including self-efficacy (Luten et al., 2016), motivation (van Stralen et al., 2010), and social support (Wilcox et al., 2009).
A review of 29 PA interventions with African American women finds that, although many interventions used some type of cultural adaptation, participants generally received the same intervention regardless of their individual barriers to PA (Whitt-Glover and Kumanyika, 2009). Evidence from moderation analyses, coupled with recent developments in adaptive interventions, suggest that participants may benefit from customizing interventions based on characteristics of the individual (Wilbur et al., 2016).
Among the recommendations provided by the 2010 Scientific Statement from the American Heart Association for interventions to promote PA changes are (a) use of group sessions with cognitive-behavioral strategies; (b) use of motivational interviewing (MI) for individuals resistant to behavioral change; and (c) use of electronic-based programs (Artinian et al., 2010). A review of PA interventions confirmed that theory-driven group interventions combining guidance, self-management and on-going support were effective in increasing PA among disadvantaged African American women (Cleland et al., 2012). MI is a client-centered counseling approach designed to explore and resolve ambivalence about changing behavior (Miller and Rollnick, 2002). A study of the use of MI telephone in healthy African Americans found an increase in PA, but the effect was not greater than culturally targeted materials alone (Resnicow et al., 2005). Group support supplemented by MI either by phone or in person may be successful in helping women overcome barriers to becoming more physically active. For women who report being self-conscious and/or feeling guilty when they do not become more physically active, automated telephone systems offer anonymity liked by participants (Ingram et al., 2011, Kaplan et al., 2003) and have the advantage of reducing reliance on reading skills needed for mailed materials.
Building upon focus groups with African American women (Wilbur et al., 2002), we developed a culturally relevant PA intervention, the Women's Lifestyle PA Program (Ingram et al., 2011). Using a randomized clinical trial (RCT), we tested three study conditions designed to increase adherence to lifestyle PA in midlife (ages 40–65) African American women. Women in all three conditions attended six group meetings. In addition to group meetings, one condition received 11 MI telephone calls, one condition received 11 automated telephone calls with motivational problem-solving tips, and one condition received no additional support. All three conditions had significant improvements in PA, but there were no significant differences between conditions (Wilbur et al., 2015). By testing moderators of the three intervention conditions within this RCT, we expect to identify specific factors that may explain variation in treatment effects and inform development of future customization in the context of adaptive interventions.
The aim of this paper is to determine whether individual barriers (demographic, physical health, psychological health, neighborhood factors, perceived barriers to PA, social support for PA) moderate treatment effects on increases in PA. The specific research question is: What are the modifiers of treatment impact on change in adherence to PA?
2. Methods
2.1. Design
Three treatment conditions were compared using a cluster-randomized, Latin-square design in which the order of intervention delivery was counterbalanced across six sites (Winer, 1971). Full details of the design are available elsewhere (Wilbur et al., 2015). Institutional Review Boards from two universities approved the study (registered clinical trial NCT01700894).
2.2. Sample
The sample consisted of 288 African American women between the ages of 40 and 65, who were sedentary (participated in moderate-vigorous PA < 3 times per week), had access to a telephone, and could attend group meetings (Wilbur et al., 2015, Wilbur et al., 2013). Those with health issues that interfered with PA were excluded. Six sites were in areas that were either predominantly African American (> 90%) or near low-income census tracts (U. S. Census Bureau, 2014).
To maximize study retention, women provided multiple means of contacting them and were compensated $40 for completing each study assessment (baseline, 24, and 48 weeks). At study completion, participants were given a pedometer.
2.3. Intervention
2.3.1. Group meetings
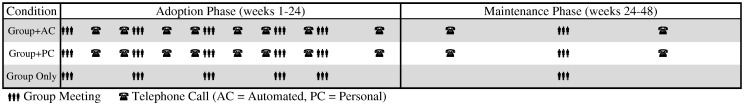
The group meeting component of the intervention was identical across all study conditions and consisted of five, two-hour group meetings over a 24-week adoption phase followed by a sixth “booster” meeting midway through the 24-week maintenance phase (Fig. 1). The intervention was manualized and six group facilitators were predominately female African American registered nurses.
Fig. 1.
Phases of the intervention by treatment condition.
2.3.2. Individual goal-setting and feedback
The goal was to increase each woman's PA above baseline by at least 3000 steps per day (Wilde et al., 2001), at a moderate walking pace to reduce joint load in individuals who may be overweight or obese (Browning and Kram, 2007). Baseline steps were obtained from blocked (no data displayed) accelerometers worn the week before the first group meeting. Weight loss was not mentioned with participants; rather, the primary goal was maintaining one's weight.
2.3.3. Group discussion
Consistent with the social cognitive theory (Bandura, 1997), group discussions began with a short DVD featuring African American women demonstrating skills, sharing experiences, and talking about challenges. The facilitator then led a 40-minute discussion, providing role-modeling and encouraging problem solving. All discussions addressed barriers and misinformation identified in earlier focus groups (Ingram et al., 2011, Wilbur et al., 2002). The last group discussion focused on anticipating such disincentives and handling relapses.
2.3.4. Personal motivational telephone calls
Six groups (96 participants) received the personal call condition (Group + PC). Between group meetings, these women received calls from their nurse facilitator, who used motivational interviewing techniques to help participants explore and resolve ambivalence about increasing their PA (Emmons and Rollnick, 2001) and tailored the discussion to match each woman's needs, experiences, barriers, motivation, and confidence (Resnicow et al., 1999). During maintenance, one motivational call was made before and one after the booster group meeting (total 2). If barriers were present, women were prompted to solve their own barriers. Only then did the facilitator ask permission to provide information or advice that had worked for other people.
2.3.5. Automated motivational telephone calls
Six groups (97 participants) received the automated call condition (Group + AC) between group visits. The content and scheduled delivery was structured to match the person-delivered calls and was recorded by an African American singer/actress. Each call offered menu selections for information. The 15 topics (23 items) included ways to incorporate PA into daily life and the benefits of becoming more active, with the tips and information changing to reflect seasons of the year (Appendix). To conclude the call, participants were asked to enter their next step goal and their confidence (0 − 10) in meeting the goal. Women with confidence below 8 were encouraged to adjust goals to increase confidence. Each call ended with advice matched to program content (Appendix).
2.3.6. No telephone calls
Six groups (95 women) had no contact (group only) except reminder calls for upcoming meetings and automated reminder calls to report steps in the automated telephone computer-linked system.
2.4. Measures
Baseline measures of demographic characteristics, health status, neighborhood characteristics, perceived barriers to PA, and social support for PA were used to model barriers to increases in PA. Each barrier was dichotomized to ease interpretation and utilization of the results.
2.4.1. Demographic characteristics
Demographics included presence of children and baseline employment. Material hardship was measured using questions from the U.S. Census Bureau's Survey of Income and Program Participation (Bauman, 1998) about food adequacy and ability to meet housing, utility, telephone, and medical expenses.
2.4.2. Health status
Health status measures included general health, global pain, body mass index, and depressive symptoms. General health was measured with an item from the Behavioral Risk Factor Surveillance System asking participants to their overall health status from excellent to poor (Behavioral Risk Factor Surveillance System, 2010).
Global pain was measured using as the sum of four items assessing pain (average, worst, least, and interference with PA) on a 10-point rating scale. In the current sample, this measure demonstrated good internal consistency (α = 0.86).
2.4.2.1. Body mass index
Height was measured to the nearest 1/16 in. using the Seca Portable Stadiometer Model 213. Weight was measured to the nearest 1/4 lb using a balance beam digital scale (Seca Brand SE 803 scale), with participants standing in light clothing and without shoes. Body mass index (BMI) was calculated by dividing weight (kilograms) by height (meters) squared (wt/ht2); (American College of Sports Medicine, 2010).
The 20-item Center for Epidemiological Studies-Depression (CES-D) scale was used to measure current depressive symptoms (Radloff, 1977). Items were rated on a 4-point scale and summed for a total score. A score of 16 or above represents the criteria for elevated depression (Boyd et al., 1982). This scale demonstrated good internal consistency in the current sample (α = 0.81).
2.4.3. Neighborhood characteristics
Neighborhood characteristics were assessed with a subjective measure of neighborhood walkability as well as violent crime rate. Neighborhood walkability was measured with a 28-item version of the Neighborhood Environment Walkability Scale (NEWS; (Cerin et al., 2006). The NEWS measures respondents' perceptions of characteristics in their neighborhoods that are conducive to walking. The scale demonstrated good internal consistency (α = 0.88) in the current sample.
Rates (incidence per 100,000 residents) of aggravated assaults/batteries for the 2009 calendar year were obtained from the Chicago Police Department and Illinois State Police (United States Department of Justice, 2013). Rates within Chicago were calculated for each census tract, while suburban rates were calculated for the entire community.
2.4.4. Perceived barriers to physical activity
Perceived barriers to PA were measured with 15 items from the Twin City Walking Survey (Forsyth et al., 2009) supplemented with two items from the St. Louis Environment and Physical Activity Instrument (lack of child-care assistance and lack of a safe place to be physically active); (Brownson et al., 2004) and one item created by the authors based on focus groups used to develop the intervention (fear that hairstyle would be ruined); (Ingram et al., 2011, Wilbur et al., 2002). The scale demonstrated good internal consistency (α = 0.82) in the current sample.
2.4.5. Social support
Social support was measured using Sallis' Social Support and Exercise Survey (Sallis et al., 1987) with modifications to assess support for PA. The measure consists of 13 activities rated on a 5-point scale separately from support for family and from friends. Both scales demonstrated excellent internal consistency (α = 0.92 for each) in the current sample.
2.4.6. Adherence to physical activity
Adherence to PA at baseline, 24, and 48 weeks was assessed directly by self-reported PA questionnaires and by accelerometry. Adherence was also measured indirectly by an aerobic fitness field test.
2.4.6.1. Self-reported PA
Minutes per week of moderate to vigorous lifestyle PA were measured with the 30-item, Community Healthy Activity Model Program for Seniors (CHAMPS) PA questionnaire (Stewart et al., 2001). Developed for middle-aged and older adults and adapted for use with African Americans (Resnicow et al., 2003), the CHAMPS covers a variety of daily activities by asking participants to estimate the frequency and average total amount of time spent weekly doing each activity over the past two weeks. Each item has an assigned metabolic equivalent (MET) value based on the 2000 Compendium of Physical Activities (Ainsworth et al., 2000), with moderate physical activities defined by MET values ≥ 3.0 to < 6.0 and vigorous by MET values ≥ 6.0. We calculated the average minutes per week for overall moderate to vigorous physical activities. Six-month reliability for moderate-vigorous intensity PA was ICC = 0.66 (Stewart et al., 2001).
2.4.6.2. Accelerometer
Women were given a Lifecorder EX (NL2200) accelerometer and instructed to wear it daily during waking hours throughout the study. The accelerometer stores 200 days of steps and records time, date, total steps, and bout steps for each hour of the day using a piezo-electric strain gauge (Crouter et al., 2005). Lifecorder steps compared to observed steps were accurate to ± 1–3% (Crouter et al., 2003). The Lifecorder EX does not record non-walking activity such as swimming or biking.
Step counts were selected as the accelerometry measure to match the study focus on increasing walking. The present study used adaptations of criteria (4 + more days with 10 + hours of wear time) used by Troiano and colleagues (Troiano et al., 2008). Data were screened to exclude days with < 1200 steps, the minimum number of steps taken by participants on over 98% of days during blinded baseline measurement. Fewer than 1200 steps likely represented either a device malfunction or failure to wear the accelerometer for an adequate amount of time. Weeks with fewer than three days of valid data were excluded from analyses. Days with valid step data in the week prior to the first group meeting were summed and divided by the total number of days with valid data to obtain mean baseline steps per day. The steps accumulated during weeks with valid data in the month before and after the 24- and 48-week assessments were summed and divided by the total number of weeks with valid data to obtain mean steps per day at 24 and 48 weeks.
2.4.6.3. Aerobic fitness
An estimate of aerobic fitness was determined with the 2-minute step test, a part of the Senior Fitness Test recommended for use in low fit older adults (Rikli and Jones, 1999). In this field test participants step in place, lifting their knees to designated point over a two-minute period. Intraclass reliability was 0.89. Criterion validity was established with treadmill time to 85% predicted maximum heart rate (Rikli and Jones, 1999).
2.5. Analysis
2.5.1. Coding of barriers to physical activity change
All measures of barriers were dichotomized such that a value of one was in the direction hypothesized to represent the presence of a barrier to increasing PA. For BMI and depression, cutoffs were based on established thresholds: 40 (morbidly obese) for BMI and 16 (sub-clinical depressive symptoms) for depression. The remaining continuous measures were dichotomized at natural breaks in the distributions or at approximately the top quartile of participants.
2.5.2. Data analytic strategy
Differential intervention effects on changes in adherence to PA by presence of baseline barriers were examined using a series of multilevel mixed-effects analyses. These analyses included condition and barriers as between-person factors (level 2) and time as a within-person factor (level 1). The effect of primary interest was the three-way interaction of barriers x condition x time. Planned contrasts were used to evaluate differential change over time (from baseline through 48 weeks) for the Group + AC and Group + PC conditions relative to the Group-only condition. Planned contrasts were examined and interpreted only for overall three-way interaction effects significant at the p < 0.10 level. Significance levels of p < 0.05 were used for all other statistical tests. Effect sizes were estimated using baseline standard deviations as the denominator.
3. Results
3.1. Sample description
Of the 288 women who completed baseline assessments and were randomized, 260 (90.3%) completed the study (i.e., 24- and 48-week assessments) and were included in these analyses. Age was the only demographic difference (Table 1) between completers (M = 53.5, SD = 6.5) and non-completers (M = 49.3, SD = 5.8).
Table 1.
Participant characteristics at baseline by study condition; Chicago, Illinois.
| Intervention condition |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n = 260) | Group only (n = 88) | Group + AC (n = 86) | Group + PC (n = 86) | p | |||||
| Age, M (SD) | 53.5 (6.5) | 53.6 (6.4) | 53.3 (6.9) | 53.5 (6.3) | 0.945 | ||||
| MVPA (min/week), M (SD) | 151.1 (217.4) | 150.0 (225.6) | 181.4 (198.4) | 121.9 (225.3) | 0.200 | ||||
| Leisure time MVPA (min/week), M (SD) | 109.8 (174.3) | 113.5 (189.3) | 126.3 (150.4) | 89.5 (180.4) | 0.373 | ||||
| Walking (min/week), M (SD) | 165.8 (204.5) | 145.7 (183.4) | 179.0 (190.4) | 173.2 (237.0) | 0.520 | ||||
| Accelerometer steps (steps/day), M (SD) | 5643.9 (2219.8) | 5345.8 (1957.7) | 5710.7 (2392.0) | 5866.6 (2275.0) | 0.335 | ||||
| Aerobic fitness (steps/2 min), M (SD) | 82.8 (15.9) | 83.3 (15.6) | 84.9 (16.6) | 80.1 (15.4) | 0.126 | ||||
| n | % | n | % | n | % | n | % | ||
|---|---|---|---|---|---|---|---|---|---|
| Married or living with partner | 101 | 38.8 | 39 | 44.3 | 27 | 31.4 | 35 | 40.7 | 0.198 |
| One or more children under age 18 | 95 | 36.5 | 29 | 33.0 | 32 | 37.2 | 34 | 39.5 | 0.658 |
| Education college or higher | 128 | 49.2 | 49 | 55.7 | 43 | 50.0 | 36 | 41.9 | 0.187 |
| Employed (full-time or part-time) | 193 | 74.2 | 62 | 70.5 | 59 | 68.6 | 72 | 83.7 | 0.047 |
| Family income | 0.759 | ||||||||
| <$20,000 | 30 | 12.1 | 11 | 13.1 | 11 | 13.6 | 8 | 9.6 | |
| $20,000–$39,999 | 66 | 26.6 | 19 | 22.6 | 26 | 32.1 | 21 | 25.3 | |
| $40,000–$59,999 | 55 | 22.2 | 20 | 23.8 | 17 | 21.0 | 18 | 21.7 | |
| ≥$60,000 | 97 | 39.1 | 34 | 40.5 | 27 | 33.3 | 36 | 43.4 | |
| Economic hardship | 0.166 | ||||||||
| No hardship | 142 | 55.7 | 44 | 51.8 | 43 | 50.6 | 55 | 64.7 | |
| One hardship | 57 | 22.4 | 24 | 28.2 | 18 | 21.2 | 15 | 17.6 | |
| More than one hardship | 56 | 22.0 | 17 | 20.0 | 24 | 28.2 | 15 | 17.6 |
Note: numbers may not total the full sample size due to missing data.
At baseline, there were no differences by condition for any of the five measures of adherence to PA (Table 1). Slightly more than one-third of participants had one or more children under the age of 18 and nearly half reported having a college degree or higher. Nearly 60% reported a family income under $60,000 and 44% reported one or more material hardships in the past year. The only significant demographic difference by study condition was for employment. The women in the Group + PC condition were more likely to be employed than the other two conditions. For most barriers (Table 2), one-fourth to one-third of participants were coded positive.
Table 2.
Cutpoints for barriers to increasing physical activity; Chicago, Illinois.
| Variable | M (SD) | Range | Cutpointa | Cases above/below cutpoint n (%) |
|---|---|---|---|---|
| Demographic | ||||
| Children in household | – | Y/N | Y | 94 (36.5) |
| Employed | – | Y/N | Y | 193 (74.2) |
| Number of hardships | 0.66 (0.82) | 0–2 | ≥ 2 | 56 (22.0) |
| Physical health | ||||
| General health | 3.25 (0.80) | 1–5 | < 3 | 34 (13.2) |
| Pain | 9.26 (5.62) | 4–34 | ≥ 11 | 82 (32.4) |
| BMI (kg/m2) | 35.30 (7.51) | 21–61 | ≥ 40 | 59 (22.7) |
| Psychological health | ||||
| Depression | 8.78 (7.12) | 0–38 | ≥ 16 | 40 (15.4) |
| Neighborhood characteristics | ||||
| Perceived walkability | 3.08 (0.42) | 1.6–3.9 | ≤ 2.8 | 64 (24.8) |
| Assault/battery rate | 649.30 (519.03) | 0–2564 | ≥ 1000 | 69 (26.8) |
| Perceived barriers to PA | ||||
| Perceived barriers for PA | 22.62 (9.74) | 0–55 | ≥ 29 | 68 (26.4) |
| Social support | ||||
| Support from family | 2.10 (1.08) | 1–5 | ≤ 1.5 | 95 (37.1) |
| Support from friends | 2.16 (1.06) | 1–5 | ≤ 1.5 | 85 (34.0) |
Variables were dichotomized as indicated such that a value of one represented a barrier to adherence in increasing physical activity (i.e., a lower likelihood of increasing PA).
3.2. Interaction between condition and barriers on change in adherence
For self-reported minutes of MVPA per week, there was a significant (p < 0.10) interaction between condition and perceived barriers to PA (Table 3). Among those with high perceived barriers, participants in the Group + AC condition increased their MVPA by 45 min per week more than those in the Group-Only condition and by 75 min more than those in the Group + PC condition; however, both differences were non-significant. There were no significant interaction effects for self-reported measures of leisure time MVPA or walking.
Table 3.
Change in adherence to physical activity by condition for participants with barriers to increasing physical activity; Chicago, Illinois.
| Barrier | 3-way interactiona |
Slope estimatesb |
Slope contrastsc |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AC |
PC |
G |
AC-G |
PC-G |
AC-PC |
|||||||||
| F | p | Est | SE | Est | SE | Est | SE | d | p | d | p | d | p | |
| MVPA (min/week) | ||||||||||||||
| Demographic | ||||||||||||||
| Children in household | 1.48 | 0.229 | 81.09 | 32.37 | 96.40 | 31.41 | 183.36 | 34.01 | − 0.47 | 0.030 | − 0.40 | 0.061 | − 0.07 | 0.735 |
| Employed | 0.94 | 0.394 | 97.63 | 24.01 | 82.60 | 21.73 | 109.84 | 23.42 | − 0.06 | 0.716 | − 0.13 | 0.395 | 0.07 | 0.643 |
| Number of hardships | 0.47 | 0.628 | 74.37 | 37.48 | 54.50 | 47.41 | 144.71 | 44.53 | − 0.32 | 0.228 | − 0.42 | 0.167 | 0.09 | 0.743 |
| Physical health | ||||||||||||||
| General health | 0.58 | 0.561 | 112.50 | 55.87 | 76.61 | 49.52 | 65.83 | 61.76 | 0.22 | 0.576 | 0.05 | 0.892 | 0.17 | 0.631 |
| Pain | 0.41 | 0.665 | 85.50 | 37.16 | 48.87 | 33.37 | 91.44 | 36.44 | − 0.03 | 0.909 | − 0.20 | 0.390 | 0.17 | 0.464 |
| BMI | 0.34 | 0.712 | 48.16 | 42.37 | 58.82 | 42.37 | 126.43 | 40.30 | − 0.36 | 0.182 | − 0.31 | 0.249 | − 0.05 | 0.859 |
| Psychological health | ||||||||||||||
| Depression | 0.14 | 0.868 | 96.14 | 55.77 | 76.41 | 46.25 | 154.04 | 51.30 | − 0.27 | 0.446 | − 0.36 | 0.262 | 0.09 | 0.786 |
| Neighborhood characteristics | ||||||||||||||
| Perceived walkability | 0.04 | 0.960 | 81.18 | 44.82 | 56.88 | 37.72 | 101.09 | 38.54 | − 0.09 | 0.737 | − 0.20 | 0.413 | 0.11 | 0.679 |
| Assault/battery rate | 0.07 | 0.933 | 75.28 | 35.58 | 75.63 | 37.94 | 130.15 | 45.08 | − 0.25 | 0.340 | − 0.25 | 0.356 | 0.00 | 0.995 |
| Perceived barriers to PA | ||||||||||||||
| Perceived barriers for PA | 2.34 | 0.099 | 138.95 | 35.96 | 63.75 | 42.61 | 94.06 | 36.91 | 0.21 | 0.385 | − 0.14 | 0.591 | 0.35 | 0.179 |
| Social support | ||||||||||||||
| Support from family | 1.07 | 0.345 | 42.14 | 35.55 | 97.02 | 32.74 | 130.74 | 29.97 | − 0.41 | 0.058 | − 0.16 | 0.448 | − 0.25 | 0.257 |
| Support from friends | 0.27 | 0.765 | 83.78 | 35.68 | 67.25 | 32.75 | 92.07 | 33.31 | − 0.04 | 0.865 | − 0.11 | 0.596 | 0.08 | 0.733 |
| Leisure time MVPA (min/week) | ||||||||||||||
| Demographic | ||||||||||||||
| Children in household | 1.25 | 0.289 | 86.95 | 27.83 | 83.60 | 27.00 | 152.84 | 29.23 | − 0.38 | 0.104 | − 0.40 | 0.083 | 0.02 | 0.931 |
| Employed | 1.24 | 0.290 | 92.29 | 20.59 | 80.00 | 18.64 | 89.03 | 20.09 | 0.02 | 0.910 | − 0.05 | 0.742 | 0.07 | 0.659 |
| Number of hardships | 0.45 | 0.639 | 81.88 | 32.49 | 34.00 | 41.10 | 105.00 | 38.61 | − 0.13 | 0.647 | − 0.41 | 0.209 | 0.27 | 0.362 |
| Physical health | ||||||||||||||
| General health | 0.16 | 0.855 | 92.73 | 48.08 | 71.25 | 42.62 | 72.50 | 53.15 | 0.12 | 0.778 | − 0.01 | 0.985 | 0.12 | 0.738 |
| Pain | 0.17 | 0.840 | 76.50 | 31.97 | 49.84 | 28.71 | 94.90 | 31.35 | − 0.11 | 0.681 | − 0.26 | 0.290 | 0.15 | 0.535 |
| BMI | 0.17 | 0.844 | 67.11 | 36.44 | 54.47 | 36.44 | 104.64 | 34.66 | − 0.22 | 0.456 | − 0.29 | 0.319 | 0.07 | 0.807 |
| Psychological health | ||||||||||||||
| Depression | 1.17 | 0.312 | 69.55 | 47.66 | 66.56 | 39.52 | 165.58 | 43.84 | − 0.55 | 0.139 | − 0.57 | 0.095 | 0.02 | 0.962 |
| Neighborhood characteristics | ||||||||||||||
| Perceived walkability | 0.05 | 0.953 | 56.91 | 38.54 | 56.56 | 32.44 | 83.48 | 33.13 | − 0.15 | 0.602 | − 0.15 | 0.562 | 0.00 | 0.994 |
| Assault/battery rate | 0.03 | 0.966 | 67.61 | 30.51 | 65.94 | 32.53 | 84.71 | 38.65 | − 0.10 | 0.729 | − 0.11 | 0.711 | 0.01 | 0.970 |
| Perceived barriers to PA | ||||||||||||||
| Perceived barriers for PA | 1.49 | 0.228 | 110.95 | 30.80 | 63.33 | 36.50 | 69.38 | 31.61 | 0.24 | 0.347 | − 0.03 | 0.901 | 0.27 | 0.320 |
| Social support | ||||||||||||||
| Support from family | 0.81 | 0.448 | 46.80 | 30.39 | 80.81 | 27.98 | 102.77 | 25.61 | − 0.32 | 0.160 | − 0.13 | 0.563 | − 0.20 | 0.411 |
| Support from friends | 0.05 | 0.952 | 68.58 | 30.40 | 49.25 | 27.90 | 78.88 | 28.38 | − 0.06 | 0.805 | − 0.17 | 0.457 | 0.11 | 0.640 |
| Walking (min/week) | ||||||||||||||
| Demographic | ||||||||||||||
| Children in household | 0.52 | 0.593 | 100.55 | 30.94 | 133.46 | 30.01 | 126.98 | 32.50 | − 0.13 | 0.556 | 0.03 | 0.884 | − 0.16 | 0.446 |
| Employed | 1.41 | 0.246 | 102.08 | 22.76 | 119.79 | 20.60 | 102.22 | 22.20 | 0.00 | 0.996 | 0.09 | 0.562 | − 0.09 | 0.564 |
| Number of hardships | 0.72 | 0.486 | 92.19 | 35.53 | 109.00 | 44.95 | 45.44 | 42.22 | 0.23 | 0.398 | 0.31 | 0.304 | − 0.08 | 0.769 |
| Physical health | ||||||||||||||
| General health | 1.35 | 0.261 | 154.77 | 52.66 | 203.04 | 46.68 | 97.50 | 58.22 | 0.28 | 0.466 | 0.52 | 0.158 | − 0.24 | 0.493 |
| Pain | 1.56 | 0.212 | 120.90 | 35.19 | 128.95 | 31.6 | 66.35 | 34.51 | 0.27 | 0.269 | 0.31 | 0.182 | − 0.04 | 0.865 |
| BMI | 0.48 | 0.618 | 110.53 | 40.06 | 158.68 | 40.06 | 140.00 | 38.11 | − 0.14 | 0.594 | 0.09 | 0.736 | − 0.24 | 0.396 |
| Psychological health | ||||||||||||||
| Depression | 1.55 | 0.215 | 41.59 | 52.67 | 129.84 | 43.67 | 154.62 | 48.45 | − 0.55 | 0.115 | − 0.12 | 0.704 | − 0.43 | 0.198 |
| Neighborhood characteristics | ||||||||||||||
| Perceived walkability | 0.35 | 0.702 | 54.71 | 42.42 | 87.5 | 35.70 | 55.11 | 36.47 | 0.00 | 0.994 | 0.16 | 0.526 | − 0.16 | 0.555 |
| Assault/battery rate | 0.03 | 0.970 | 88.61 | 33.58 | 100.00 | 35.80 | 96.62 | 42.54 | − 0.04 | 0.883 | 0.02 | 0.952 | − 0.06 | 0.817 |
| Perceived barriers to PA | ||||||||||||||
| Perceived barriers for PA | 0.33 | 0.719 | 119.37 | 34.58 | 157.08 | 40.98 | 124.69 | 35.49 | − 0.03 | 0.915 | 0.16 | 0.551 | − 0.18 | 0.483 |
| Social support | ||||||||||||||
| Support from family | 0.30 | 0.744 | 93.30 | 34.14 | 109.11 | 31.43 | 124.46 | 28.77 | − 0.15 | 0.486 | − 0.07 | 0.719 | − 0.08 | 0.733 |
| Support from friends | 0.34 | 0.714 | 117.48 | 34.66 | 99.25 | 31.81 | 84.57 | 32.35 | 0.16 | 0.488 | 0.07 | 0.747 | 0.09 | 0.699 |
| Accelerometer steps (steps/day) | ||||||||||||||
| Demographic | ||||||||||||||
| Children in household | 1.05 | 0.354 | 159.3 | 272.3 | 790.1 | 243.6 | − 54.7 | 305.6 | 0.09 | 0.602 | 0.37 | 0.032 | − 0.28 | 0.086 |
| Employed | 0.84 | 0.432 | 339.8 | 185.7 | 545.2 | 165.7 | 38.6 | 184.5 | 0.13 | 0.251 | 0.22 | 0.043 | − 0.09 | 0.410 |
| Number of hardships | 3.37 | 0.037 | − 199.9 | 286.5 | 1149.2 | 357.6 | 105.1 | 348.0 | − 0.13 | 0.500 | 0.46 | 0.038 | − 0.59 | 0.004 |
| Physical health | ||||||||||||||
| General health | 2.42 | 0.092 | − 822.1 | 433.8 | 683.0 | 357.8 | − 153.3 | 521.5 | − 0.29 | 0.326 | 0.37 | 0.188 | − 0.66 | 0.008 |
| Pain | 0.08 | 0.924 | 115.4 | 269.4 | 567.6 | 273.4 | 113.2 | 292.6 | 0.00 | 0.996 | 0.20 | 0.258 | − 0.20 | 0.240 |
| BMI | 0.21 | 0.807 | 81.4 | 302.5 | 239.7 | 351.3 | 109.0 | 339.6 | − 0.01 | 0.952 | 0.06 | 0.789 | − 0.07 | 0.733 |
| Psychological health | ||||||||||||||
| Depression | 4.96 | 0.008 | 1083.5 | 383.1 | 760.6 | 360.4 | − 573.3 | 375.8 | 0.73 | 0.002 | 0.59 | 0.011 | 0.14 | 0.540 |
| Neighborhood characteristics | ||||||||||||||
| Perceived walkability | 0.26 | 0.773 | − 155.8 | 329.4 | 391.5 | 309.1 | 14.2 | 297.7 | − 0.07 | 0.702 | 0.17 | 0.381 | − 0.24 | 0.227 |
| Assault/battery rate | 2.46 | 0.088 | 828.2 | 271.7 | 755.8 | 279.0 | − 88.7 | 340.6 | 0.40 | 0.037 | 0.37 | 0.057 | 0.03 | 0.853 |
| Perceived barriers to PA | ||||||||||||||
| Perceived barriers for PA | 2.65 | 0.073 | − 24.9 | 274.6 | 1153.7 | 332.8 | 7.0 | 290.8 | − 0.01 | 0.937 | 0.51 | 0.010 | − 0.52 | 0.007 |
| Social support | ||||||||||||||
| Support from family | 0.37 | 0.690 | 386.4 | 261.6 | 499.0 | 243.4 | 212.6 | 237.3 | 0.08 | 0.623 | 0.13 | 0.401 | − 0.05 | 0.753 |
| Support from friends | 0.51 | 0.603 | 405.8 | 277.8 | 636.3 | 249.0 | 54.4 | 283.7 | 0.15 | 0.377 | 0.26 | 0.125 | − 0.10 | 0.538 |
| Aerobic fitness (steps/2 min) | ||||||||||||||
| Demographic | ||||||||||||||
| Children in household | 0.24 | 0.783 | 2.97 | 1.70 | 5.21 | 1.66 | 3.06 | 1.78 | − 0.01 | 0.970 | 0.13 | 0.378 | − 0.14 | 0.346 |
| Employed | 0.36 | 0.698 | 2.96 | 1.23 | 3.90 | 1.15 | 3.19 | 1.19 | − 0.01 | 0.893 | 0.04 | 0.666 | − 0.06 | 0.575 |
| Number of hardships | 4.00 | 0.020 | 1.56 | 1.94 | 8.75 | 2.50 | − 0.97 | 2.38 | 0.16 | 0.411 | 0.61 | 0.005 | − 0.45 | 0.024 |
| Physical Health | ||||||||||||||
| General health | 1.93 | 0.147 | 5.40 | 2.90 | 8.54 | 2.64 | 0.21 | 3.23 | 0.32 | 0.233 | 0.52 | 0.047 | − 0.20 | 0.425 |
| Pain | 3.50 | 0.032 | 6.66 | 1.95 | 3.29 | 1.75 | 1.11 | 1.87 | 0.35 | 0.041 | 0.14 | 0.394 | 0.21 | 0.201 |
| BMI | 2.62 | 0.075 | 7.49 | 2.21 | 2.94 | 2.32 | 2.92 | 2.06 | 0.29 | 0.132 | 0.00 | 0.993 | 0.28 | 0.158 |
| Psychological health | ||||||||||||||
| Depression | 0.02 | 0.976 | 4.05 | 3.04 | 4.74 | 2.46 | 3.77 | 2.60 | 0.02 | 0.944 | 0.06 | 0.786 | − 0.04 | 0.860 |
| Neighborhood characteristics | ||||||||||||||
| Perceived walkability | 0.06 | 0.942 | 3.49 | 2.33 | 5.11 | 2.05 | 4.85 | 2.02 | − 0.09 | 0.659 | 0.02 | 0.929 | − 0.10 | 0.603 |
| Assault/battery rate | 0.87 | 0.420 | 3.05 | 1.85 | 7.38 | 1.96 | 3.86 | 2.36 | − 0.05 | 0.787 | 0.22 | 0.253 | − 0.27 | 0.109 |
| Perceived barriers to PA | ||||||||||||||
| Perceived barriers for PA | 0.46 | 0.634 | 2.64 | 1.86 | 4.49 | 2.40 | 1.50 | 1.99 | 0.07 | 0.676 | 0.19 | 0.338 | − 0.12 | 0.541 |
| Social support | ||||||||||||||
| Support from family | 1.62 | 0.199 | 0.41 | 1.84 | 5.50 | 1.73 | 3.88 | 1.57 | − 0.22 | 0.154 | 0.10 | 0.488 | − 0.32 | 0.045 |
| Support from friends | 1.22 | 0.298 | 3.52 | 1.86 | 7.26 | 1.77 | 3.60 | 1.82 | 0.00 | 0.976 | 0.23 | 0.151 | − 0.23 | 0.147 |
Notes:
The overall test of the three-way interaction of barrier × condition × time. Slope contrasts were not interpreted unless the three-way interaction was significant at p < 0.10.
The slopes estimates represent the coefficient for linear change over time (per assessment) among participants who were coded positive for each obstacle to adherence to physical activity.
The contrasts are presented in units of standardized mean differences in rates of change (effect size d). Effect sizes were estimated using pooled standard deviations of the baseline outcome measures.
For accelerometer steps per day, there were significant interactions between study condition and five barriers: (a) material hardships, (b) general health, (c) depression, (d) neighborhood assault rate, and (e) perceived barriers to PA. Among those with material hardships, participants in the Group + PC condition showed increases in accelerometer steps per day relative to participants in the both the Group-Only and Group + AC conditions such that participants in the Group + PC condition increased by 1044 steps per day more than those in the Group-Only condition (1149.2 vs. 105.1) and by 1349 steps per day more than those in the Group + AC condition. These differences translated into estimated effects sizes of d = 0.46 and d = 0.59, respectively. Among those with poor general health, participants in the Group + PC condition showed increases of 1505 steps per day more than those in the Group + AC condition (d = 0.66). Among those with elevated depressive symptoms, participants in the Group + AC condition as well as the Group + PC condition showed increases of 1657 steps per day more than those in the Group-Only condition (d = 0.73). In addition, those in the Group + PC condition increased by 1376 steps per day more than those in the Group-Only condition d = 0.59). Among those living in neighborhoods with high assault rates, participants in the Group + AC condition showed increases of 917 steps per day more than those in the Group-Only condition (d = 0.40). Finally among those with high perceived barriers, participants in the Group + PC condition showed increases of 1146 steps per day more than those in the Group-Only condition (d = 0.51).
For aerobic fitness, there were significant interactions between study condition and two barriers: (a) number of hardships and (b) perceived pain. Among those with two or more hardships, participants in the Group + PC condition increased the number of steps taken during the fitness test by 9.7 more than those in the Group-Only condition (d = 0.61). For those with higher pain scores, participants in the Group + AC condition increased the number of steps taken during the fitness test by 5.6 more than those in the Group-Only condition (d = 0.35).
4. Discussion
By examining barriers to PA as moderators of treatment effects, we were able to identify specific barriers associated with differential impact of supplemental calls between group sessions. The most notable of these effects were found for participants with elevated depressive symptoms. For these participants, both call conditions improved their number of steps significantly more than the Group-Only condition. These findings are important in the context of research linking depressive symptoms to lower levels of PA (Patten et al., 2009, van Gool et al., 2003) and showing that PA interventions led to reductions in depressive symptoms (Conn, 2010). The MI and problem-solving focus of the telephone calls may have improved self-efficacy for PA, which may be particularly important for participants with depressive symptoms (Kangas et al., 2015). In addition, the MI and problem solving were likely for overcoming specific barriers to PA such as material hardships, neighborhood crime, and perceived barriers to PA. Additional research is needed to understand the mechanism of these moderation effects.
These results build upon prior analyses of moderation of PA interventions in important ways. First, all potential moderators were selected based on an a priori rationale that they served to interfere with increasing PA. Prior studies have often included demographic variables without specific hypotheses about the direction of moderation (Luten et al., 2016, van Stralen et al., 2010, Wilcox et al., 2009). Second, the design of the present study allowed tests of moderation of intervention supplements rather than testing moderation of treatment versus control groups. Testing moderation of supplemental phone calls is more directly informative for future research building adaptive interventions. The problem-solving focus of the telephone calls may explain their benefit for women facing barriers to PA. Finally, this study focused on a sample of African American women, a population at particular risk for negative health outcomes associated with inactivity. These results contribute to a small but growing literature regarding moderators of PA interventions.
This study has a few limitations. Because these are secondary analyses, the original study was neither designed nor powered to test the moderated effects presented in this paper. For ease of analysis and interpretation, barriers were dichotomized; however, most measures did not have clinical guidelines to inform cutoff scores. As such, the cutoffs that were selected may not represent optimal scores for dichotomization. Further, generalizability is likely limited by the focus on urban African American midlife women who self-selected for study participation.
Despite the noted limitations, the present study provides evidence that intervention supplements (between-group telephone calls) may provide significant benefits for participants facing more and greater barriers to increasing adherence to PA, especially depression. Although not designed to test the impact of adaptive interventions, these results are consistent with the concept that treatment augmentation may be necessary for some participants based on pre-existing characteristics or treatment non-response (Almirall et al., 2014). Future studies should employ research designs to specifically test adaptive interventions to increase adherence to PA.
The following are the supplementary data related to this article.
Personal motivation telephone calls: topics and final advice.
Funding
The study was funded by National Institute of Nursing Research grant number R01NR004134.
Acknowledgement
The authors gratefully acknowledge the study participants and research collaborators Diana M. Ingram, PhD, MPH; Lynne Braun PhD, RN, FAAN; Phyllis Pelt, MSN, RN; Edith V. Ocampo, MS; Shannon Halloway, PhD, RN; and Judith McDevitt, PhD, RN.
References
- Ainsworth B.E., B. D.R., Jr., Strath S.J. Comparison of three methods for measuring the time spent in physical activity. Med. Sci. Sports Exerc. 2000;32:S457–S464. doi: 10.1097/00005768-200009001-00004. [DOI] [PubMed] [Google Scholar]
- Airhihenbuwa C.O., Kumanyika S., Agurs T.D., Lowe A. Perceptions and beliefs about exercise, rest, and health among African-Americans. Am. J. Health Promot. 1995;9:426–429. doi: 10.4278/0890-1171-9.6.426. [DOI] [PubMed] [Google Scholar]
- Almirall D., Nahum-Shani I., Sherwood N.E., Murphy S.A. Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research. Transl. Behav. Med. 2014;4:260–274. doi: 10.1007/s13142-014-0265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Sports Medicine . eighth ed. Lippincott Williams & Wilkins; Philadelphia: 2010. ACSM's Guidelines for Exercise Testing and Prescription. [Google Scholar]
- Artinian N.T., Fletcher G.F., Mozaffarian D. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. W.H. Freeman and Company; New York: 1997. Self-efficacy: The Exercise of Control. [Google Scholar]
- Baruth M., Sharpe P.A., Parra-Medina D., Wilcox S. Perceived barriers to exercise and healthy eating among women from disadvantaged neighborhoods: results from a focus groups assessment. Women Health. 2014;54:336–353. doi: 10.1080/03630242.2014.896443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman K.J. U.S. Census Bureau, Population Divison; Washington, DC: 1998. Direct Measure of Poverty as an Indicator of Economic Need: Evidence from the Survey of Income and Program Participation. [Google Scholar]
- Behavioral Risk Factor Surveillance System . 2010. Behavioral Risk Factor Surveillance System Questionnaire. [Google Scholar]
- Bopp M., Wilcox S., Laken M. Factors associated with physical activity among African-American men and women. Am. J. Prev. Med. 2006;30:340–346. doi: 10.1016/j.amepre.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Boyd J.H., Weissman M.M., Thompson W.D., Myers J.K. Screening for depression in a community sample. Understanding the discrepancies between depression symptom and diagnostic scales. Arch. Gen. Psychiatry. 1982;39:1195–1200. doi: 10.1001/archpsyc.1982.04290100059010. [DOI] [PubMed] [Google Scholar]
- Browning R.C., Kram R. Effects of obesity on the biomechanics of walking at different speeds. Med. Sci. Sports Exerc. 2007;39:1632–1641. doi: 10.1249/mss.0b013e318076b54b. [DOI] [PubMed] [Google Scholar]
- Brownson R.C., Chang J.J., Eyler A.A. Measuring the environment for friendliness toward physical activity: a comparison of the reliability of 3 questionnaires. Am. J. Public Health. 2004;94:473–483. doi: 10.2105/ajph.94.3.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census Bureau U.S. 2014. State and County Quick Facts. [Google Scholar]
- Cerin E., Saelens B.E., Sallis J.F., Frank L.D. Neighborhood Environment Walkability Scale: validity and development of a short form. Med. Sci. Sports Exerc. 2006;38:1682–1691. doi: 10.1249/01.mss.0000227639.83607.4d. [DOI] [PubMed] [Google Scholar]
- Cleland C.L., Tully M.A., Kee F., Cupples M.E. The effectiveness of physical activity interventions in socio-economically disadvantaged communities: a systematic review. Prev. Med. 2012;54:371–380. doi: 10.1016/j.ypmed.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Conn V.S. Depressive symptom outcomes of physical activity interventions: meta-analysis findings. Ann. Behav. Med. Publ. Soc. Behav. Med. 2010;39:128–138. doi: 10.1007/s12160-010-9172-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouter S.E., Schneider P.L., Karabulut M., B. D.R., Jr. Validity of 10 electronic pedometers for measuring steps, distance, and energy cost. Med. Sci. Sports Exerc. 2003;35:1455–1460. doi: 10.1249/01.MSS.0000078932.61440.A2. [DOI] [PubMed] [Google Scholar]
- Crouter S.E., Schneider P.L., B. D.R., Jr. Spring-levered versus piezo-electric pedometer accuracy in overweight and obese adults. Med. Sci. Sports Exerc. 2005;37:1673–1679. doi: 10.1249/01.mss.0000181677.36658.a8. [DOI] [PubMed] [Google Scholar]
- Diez Roux A.V. Neighborhoods and health: what do we know? What should we do? Am. J. Public Health. 2016;106:430–431. doi: 10.2105/AJPH.2016.303064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmons K.M., Rollnick S. Motivational interviewing in health care settings: opportunities and limitations. Am. J. Prev. Med. 2001;20:68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- Forsyth A., Oakes J.M., Schmitz K.H. Test-retest reliability of the Twin Cities Walking Survey. J. Phys. Act. Health. 2009;6:119–131. doi: 10.1123/jpah.6.1.119. [DOI] [PubMed] [Google Scholar]
- Forthofer M., Burroughs-Girardi E., Stoisor-Olsson L., Wilcox S., Sharpe P.A., Pekuri L.M. Use of formative research and social network theory to develop a group walking intervention: Sumter County on the move! Eval. Program Plann. 2016;58:28–34. doi: 10.1016/j.evalprogplan.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram D., Wilbur J., McDevitt J., Buchholz S. Women's walking program for African American women: expectations and recommendations from participants as experts. Women Health. 2011;51:566–582. doi: 10.1080/03630242.2011.606357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kangas J.L., Baldwin A.S., Rosenfield D., Smits J.A.J., Rethorst C.D. Examining the moderating effect of depressive symptoms on the relation between exercise and self-efficacy during the initiation of regular exercise. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2015;34:556–565. doi: 10.1037/hea0000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan B., Farzanfar R., Friedman R.H. Personal relationships with an intelligent interactive telephone health behavior advisor system: a multimethod study using surveys and ethnographic interviews. Int. J. Med. Inform. 2003;71:33–41. doi: 10.1016/s1386-5056(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Kriska A.M., Rexroad A.R. The role of physical activity in minority populations. Womens Health Issues. 1998;8:98–103. doi: 10.1016/S1049-3867(97)00103-5. [DOI] [PubMed] [Google Scholar]
- Liao Y., Bang D., Cosgrove S. Surveillance of health status in minority communities — Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. Morb. Mortal. Wkly. Report Surveillance Summ. 2011;60:1–44. [PubMed] [Google Scholar]
- Luten K.A., Dijkstra A., Reijneveld S.A., de Winter A.F. Moderators of physical activity and healthy eating in an integrated community-based intervention for older adults. Eur. J. Pub. Health. 2016;26:645–650. doi: 10.1093/eurpub/ckw051. [DOI] [PubMed] [Google Scholar]
- Mama S.K., McCurdy S.A., Evans A.E., Thompson D.I., Diamond P.M., Lee R.E. Using community insight to understand physical activity adoption in overweight and obese African American and Hispanic women: a qualitative study. Health Educ. Behav. Off. Publ. Soc. Public Health Educ. 2015;42:321–328. doi: 10.1177/1090198114557128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W., Rollnick S. Guilford Press; New York: 2002. Motivational Interviewing. [Google Scholar]
- Mozaffarian D., Benjamin E.J., Go A.S. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2015;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- Patten S.B., Williams J.V.A., Lavorato D.H., Eliasziw M. A longitudinal community study of major depression and physical activity. Gen. Hosp. Psychiatry. 2009;31:571–575. doi: 10.1016/j.genhosppsych.2009.08.001. [DOI] [PubMed] [Google Scholar]
- Pekmezi D., Marcus B., Meneses K. Developing an intervention to address physical activity barriers for African-American women in the deep south (USA) Women's Health (Lond. Engl.) 2013;9:301–312. doi: 10.2217/whe.13.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D Scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977:385–401. [Google Scholar]
- Resnicow K., Baranowski J., Ahluwalia J., Braithwaite R. Cultural sensitivity in public health: defined and demystified. Ethn. Dis. 1999;9:10–21. [PubMed] [Google Scholar]
- Resnicow K., McCarty F., Blissett D., Wang T., Heitzler C., Lee R.E. Validity of a modified CHAMPS physical activity questionnaire among African-Americans. Med. Sci. Sports Exerc. 2003;35:1537–1545. doi: 10.1249/01.MSS.0000084419.64044.2B. [DOI] [PubMed] [Google Scholar]
- Resnicow K., Jackson A., Blissett D. Results of the healthy body healthy spirit trial. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2005;24:339–348. doi: 10.1037/0278-6133.24.4.339. [DOI] [PubMed] [Google Scholar]
- Rikli R.E., Jones C.J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999:129–161. [Google Scholar]
- Sallis J.F., Grossman R.M., Pinski R.B., Patterson T.L., Nader P.R. The development of scales to measure social support for diet and exercise behaviors. Prev. Med. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- Siddiqi Z., Tiro J.A., Shuval K. Understanding impediments and enablers to physical activity among African American adults: a systematic review of qualitative studies. Health Educ. Res. 2011;26:1010–1024. doi: 10.1093/her/cyr068. [DOI] [PubMed] [Google Scholar]
- Stewart A., Mills K.M., King A.C., Haskell W.L., Gillis D., Ritter P.L. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med. Sci. Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Troiano R.P., Berrigan D., Dodd K.W., Masse L.C., Tilert T., McDowell M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- United States Department of Justice, F.B. of I . Vol. 2012. 2013. Crime in the United States. [Google Scholar]
- US Department of Health and Human Services . U.S. Government Printing Office; Washington, DC: 2008. 2008 Physical Activity Guidelines for Americans (ODPHP Publication No. U0036) [Google Scholar]
- van Gool C.H., Kempen G.I.J.M., Penninx B.W.J.H., Deeg D.J.H., Beekman A.T.F., van E. Relationship between changes in depressive symptoms and unhealthy lifestyles in late middle aged and older persons: results from the longitudinal aging study Amsterdam. Age Ageing. 2003;32:81–87. doi: 10.1093/ageing/32.1.81. [DOI] [PubMed] [Google Scholar]
- van Stralen M.M., de Vries H., Bolman C., Mudde A.N., Lechner L. Exploring the efficacy and moderators of two computer-tailored physical activity interventions for older adults: a randomized controlled trial. Ann. Behav. Med. Publ. Soc. Behav. Med. 2010;39:139–150. doi: 10.1007/s12160-010-9166-8. [DOI] [PubMed] [Google Scholar]
- Whitt-Glover M.C., Kumanyika S.K. Systematic review of interventions to increase physical activity and physical fitness in African-Americans. Am. J. Health Promot. AJHP. 2009;23:S33–S56. doi: 10.4278/ajhp.070924101. [DOI] [PubMed] [Google Scholar]
- Wilbur J., Chandler P., Dancy B., Choi J., Plonczynski D. Environmental, policy and cultural factors related to physical activity in urban, African American women. Women Health. 2002;36:17–28. doi: 10.1300/J013v36n02_02. [DOI] [PubMed] [Google Scholar]
- Wilbur J., Buchholz S.W., Ingram D.M. Effectiveness, efficiency, duration, and costs of recruiting for an African American women's lifestyle physical activity program. Res. Nurs. Health. 2013;36:487–499. doi: 10.1002/nur.21550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilbur J., Miller A.M., Fogg L. Randomized clinical trial of the women's lifestyle physical activity program for African-American women: 24- and 48-week outcomes. Am. J. Health Promot. AJHP. 2015 doi: 10.1177/0890117116646342. [DOI] [PubMed] [Google Scholar]
- Wilbur J., Kolanowski A.M., Collins L.M. Utilizing MOST frameworks and SMART designs for intervention research. Nurs. Outlook. 2016;64:287–289. doi: 10.1016/j.outlook.2016.04.005. [DOI] [PubMed] [Google Scholar]
- Wilcox S., Dowda M., Dunn A., Ory M.G., Rheaume C., King A.C. Predictors of increased physical activity in the active for life program. Prev. Chronic Dis. 2009;6:A25. [PMC free article] [PubMed] [Google Scholar]
- Wilde B.E., Sidman C.L., Corbin C.B. A 10,000 step count as a physical activity target for sedentary women. Res. Q. Exerc. Sport. 2001;72:411–414. doi: 10.1080/02701367.2001.10608977. [DOI] [PubMed] [Google Scholar]
- Winer B.J. McGraw-Hill Book Company; New York: 1971. Statistical Principles in Experimental Design. [Google Scholar]
- Yeager K.K., Macera C.A., Merrit R. Socioeconomic influences on leisure-time sedentary behavior among women. Health Values. 1993;17:50–54. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Personal motivation telephone calls: topics and final advice.