Abstract
The quadriceps tendon is an infrequently used graft option for anterior cruciate ligament reconstruction despite favorable clinical results in the literature with low donor site morbidity. It is a versatile graft that can be harvested with bone or as a soft tissue graft alone. In addition, it can be used for anatomic, double-bundle, transtibial, and all-inside reconstructions. The unique characteristics of the quadriceps tendon allow for the ability to harvest a single-bundle large-diameter graft and minimize disruption of normal anatomy, which makes the quadriceps tendon an excellent choice for all-inside techniques. Recently developed minimally invasive harvest techniques described in this note allow for a reproducible predictable and efficient harvest through a small incision.
There are many different techniques used for modern anterior cruciate ligament (ACL) reconstruction. Currently, many surgeons are using an “all-inside” ACL reconstruction technique because of proposed benefits of decreased bone removal, diminished surgical trauma, decreased postoperative pain, and improved cosmesis.1, 2, 3 All-inside ACL reconstructions generally require shorter grafts to allow for proper tension within the 2 created blind sockets. Bone–patellar tendon–bone autografts are often difficult to use when considering an all-inside ACL reconstruction because of the inability to appropriately shorten the graft. The original all-inside ACL reconstruction, as described by Morgan, used an allograft, but he and others have modified this technique for alternative soft tissue autografts.1, 3, 4, 5
Preoperative Planning
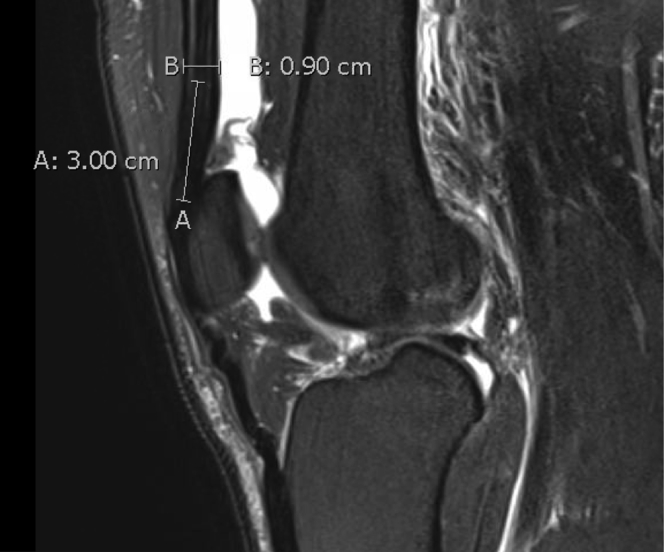
If a magnetic resonance imaging has been obtained preoperatively, the thickness of the quadriceps tendon can be reliably estimated. We routinely measure the thickness of the tendon at the midsagittal patella, 3 cm proximal to the proximal pole (Fig 1).6 We prefer a partial thickness harvest if possible, although full thickness grafts can be intentionally taken for patients with thinner tendons.
Fig 1.
The thickness of the quadriceps tendon graft can be measured by the thickness of the tendon at the midsagittal patella, 3 cm proximal to the proximal pole of the patella.
Surgical Technique
Graft Harvest
A tourniquet is placed on the thigh, the operative leg is placed in a circumferential leg holder with the well leg in a lithotomy positioner, and the foot of the bed dropped (Video 1). If graft harvest is performed after arthroscopy, we find that suctioning all arthroscopic fluid out of the knee minimizes capsular distention deep to the quadriceps tendon and makes full thickness rents less likely. With the leg flexed to 90°, the proximal pole and the medial and lateral borders of the patella are marked. It is important to distinguish the lateral border of the patella from the lateral trochlear ridge. A 1.5- to 2-cm vertical mark is made extending proximal from the proximal pole of the patella, just lateral to the midpoint (Fig 2). The skin and subcutaneous tissue is injected with local anesthetic (or saline) to distend the tissue off the tendon. A longitudinal incision is made with a No. 15 blade, and the subcutaneous tissue is excised. It is critical to ellipse out the underlying subcutaneous tissue for adequate visualization through the small incision. A Ray-Tech sponge over a key elevator is used to sweep tissue off of the anterior quadriceps tendon and anterior patella. An Army-Navy retractor is placed into the proximal apex of the incision, and an arthroscope is inserted with the fluid turned off. While looking down at the tendon, the vastus medialis is identified, as is the proximal apex of the rectus femoris tendon. A mark is placed on the anterior thigh at the point of maximum transillumination, marking the rectus tendon. The distance between this mark and the superior pole of the patella is measured to confirm the graft length of >6.5 cm (Fig 3). Perforating blood vessels that may be transected or damaged during the harvest are identified and coagulated using an arthroscopic electrocautery device.
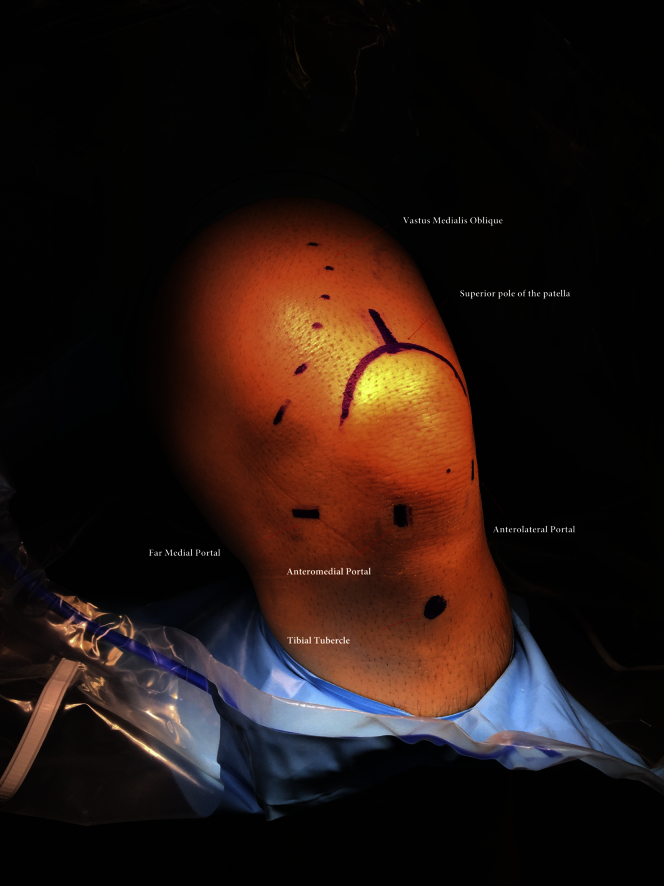
Fig 2.
With the leg flexed to 90°, the vastus medialis oblique is palpated and its border marked. The proximal pole and the medial and lateral borders of the patella are marked. Keep in mind the importance of distinguishing the lateral border of the patella from the lateral trochlear ridge. A 2-cm vertical mark is made extending proximally from the proximal pole. At this point, our anterolateral, anteromedial, and far medial portal sites may also be marked.
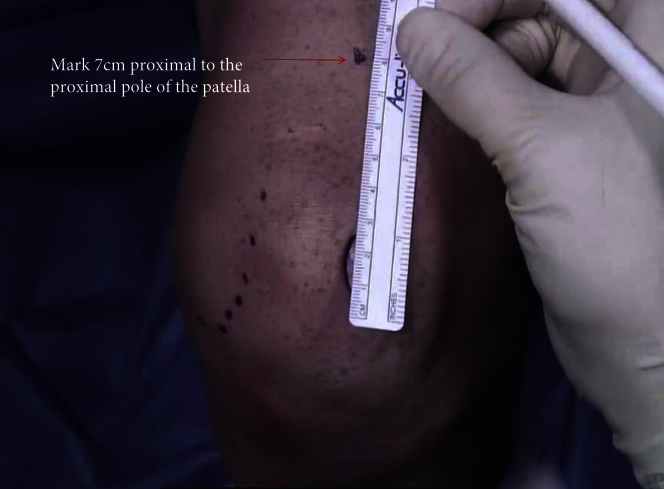
Fig 3.
Measurement is performed 6.5 cm proximal to the proximal pole of the patella and a mark is made. The skin should tranilluminate at least this far up when the arthroscope is inserted to confirm a graft length of >6.5 cm.
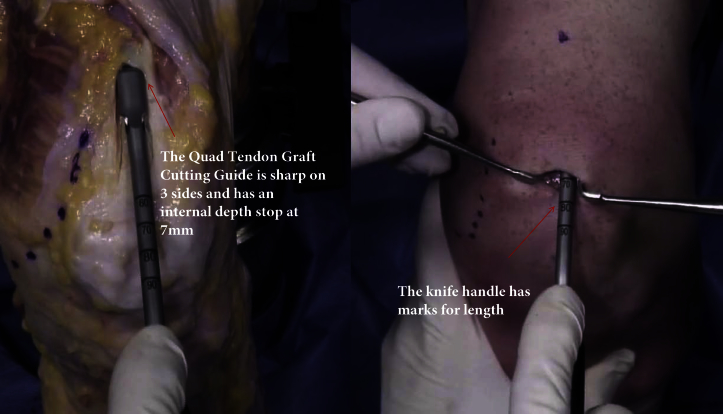
The Athrex (Naples, FL) quadriceps harvest knife is used for graft harvest. The design of the blade limits the depth of the cut to 7 mm. The triple blade edges allow for either a “pull” or “push” cutting technique either from the point of transillumination to the proximal pole of the patella, or the reverse (Fig 4). In general, we recommend a “push” technique. The knife handle has marks for reference for graft length, measured from the proximal pole of the patella. A No. 15-blade knife is used to connect the 2 vertical incisions just off the superior pole of the patella. The depth of the vertical limbs can be used as a reference for graft thickness when harvesting the partial thickness graft. A thin fat layer exists deep to the tendon and superficial to capsule, which should, if encountered, alert the surgeon to avoid deeper dissection or the risk of capsular violation. Careful dissection with the scalpel and/or metzenbaum scissors is carried proximally, and the graft end is controlled with an Allis clamp. It is very important to trim down the distal 2 cm of the graft to the desired circumference. If this is not done, the graft will have larger ends compared with the mid-substance of the graft after graft preparation. Once 2 to 3 cm of graft has been elevated, a FiberLoop suture is used to whipstitch the tendon (4 throws), starting 2 cm proximal to the tendon end, and exiting the central portion of the graft (the needle is not cut from the suture) (Fig 5). With traction on the sutures, metzenbaum scissors can be used to dissect the graft proximally if desired. With firm tension on the sutures, the Arthrex Quadriceps Tendon Stripper/Cutter is used to strip, and then cut the graft proximally once the desired graft length is achieved. This is measured with the Stripper/Cutter handle (Fig 6). For all-inside ACL reconstructions, we prefer to harvest grafts 6.5 to 7 cm in length. Grafts tend to shorten a few millimeters with preparation. Grafts longer than 7 cm should be shortened if an all-inside technique is used.
Fig 4.
The Arthrex quadriceps harvest knife is sharp on 3 sides and allows for either a “pull” or “push” technique for cutting the tendon. The tendon may be cut either proximally to distally or the reverse. We recommend the “push technique.” The blade is designed to prevent the operator from cutting the tendon too deep. After the cut is made, the 2 vertical incisions just off the superior pole of the patella are connected using a No. 15 blade. There is a thin layer of fat between the tendon and capsule. If a patch of fat is encountered, the surgeon should be alerted that it is through the tendon and should avoid deeper dissection or the risk of capsular violation.
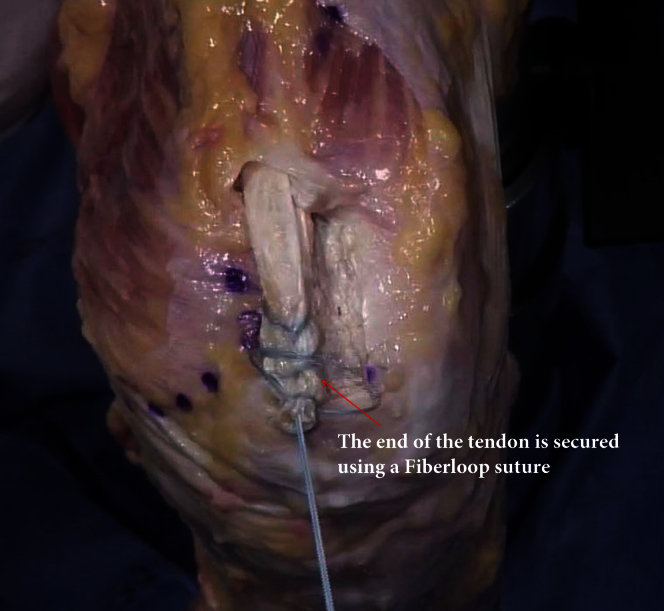
Fig 5.
Once several centimeters of graft have been freed from the distal tendon, a FiberLoop suture is used to whipstitch the tendon (4 throws), starting 2 cm proximal to the tendon end and exiting the core of the graft.
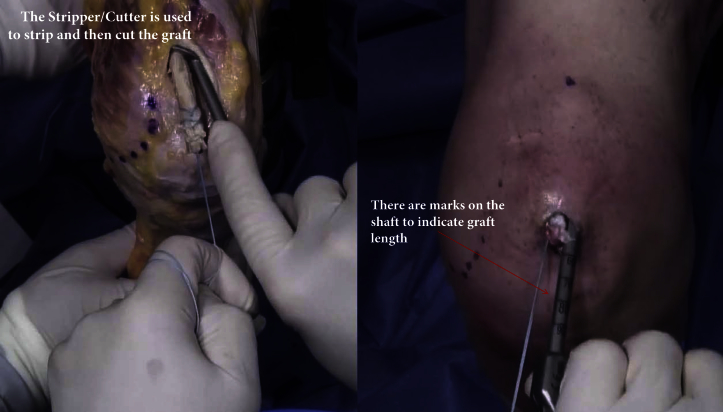
Fig 6.
The stripper/cutter is designed to strip and then cut the graft from distal to proximal once the desired graft length is achieved. There are marks on the handle to indicate length. Once the desired length is stripped. The handle is squeezed, and the graft will be cut from the quadriceps tendon. For an all-inside technique, we generally prefer to harvest 6.5-7 cm in length. If the harvested graft is longer than this, it should be shortened.
The harvested graft is then brought to the back table. An Army-Navy retractor is placed back in the proximal apex of the wound and the arthroscope is reinserted to confirm partial thickness harvest or identify a capsular rent. Any capsular rents can be closed. If a partial thickness harvest is confirmed, the skin can simply be closed in a standard fashion.
Graft Preparation
The fiber loop end of the graft is secured to the graft preparation clamp. An Allis clamp is placed on the free end of the graft and is held by the assistant (Video 1). It is vital to trim the free side of the graft to the desired diameter, because the end of the graft will increase between 0.5 mm and 1 mm after being tubulerized by the fiber loop. A fiber loop is used to whipstitch the graft in the same manner as was done during graft harvest, starting 2 cm away from the end of the tendon, and locking the last stitch as it exits the central portion of the tendon. The diameter of each graft end is then measured. A decision can then be made as to which side of the graft will be for the femur or tibia. Unlike when grafts are passed through the tibial tunnel, the surgeon has the flexibility to place the larger diameter end in the femoral tunnel, which may be very helpful in revision settings.
We prefer adjustable loop suspensory fixation. This type of fixation provides room for graft adjustment in both the femoral and tibial tunnels after the graft is passed. The previously placed FiberLoop is passed through the loop of the Arthrex TightRope RT. The needle is passed through the central portion of the graft exiting the surface of the graft 5 mm away from the end of the graft. Three or 4 subsequent whipstitches are placed in the graft. The needle is then cut from the suture, and the 2 limbs of the suture are wrapped around the graft in opposite directions from each other and tied. The end of the suture can be passed through the needle, and the knot can be shuttled into the mid-substance of the tendon, before suture tails are cut (Fig 7). The length of the femoral adjustable loop button is shortened to the length of the potential femoral tunnel + 5 mm (Fig 8). The same process is repeated on the other end of the graft using a TightRope RT. The diameters are then remeasured and appropriate size flip cutters are selected.
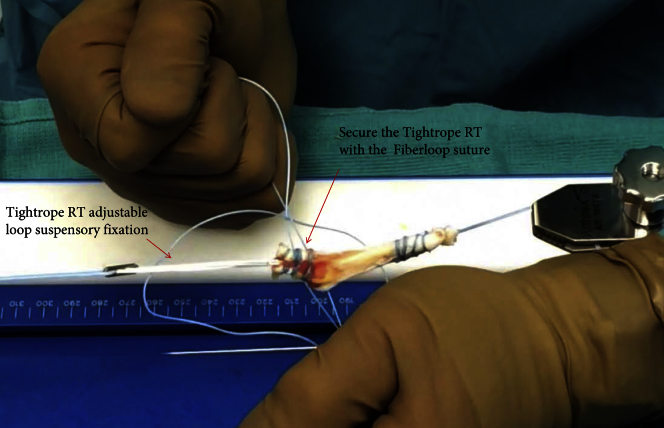
Fig 7.
We prefer adjustable loop suspensory fixation as this provides room for graft adjustment in both the femoral and tibial tunnels after graft passage. The previously placed FiberLoop suture is passed through the loop of the TightRope RT and the needle is passed through the central portion of the graft exiting the surface 5 mm away from the end of the graft. Throw 3-4 whipstitches in the graft and then cut the needle from the suture. Wrap the 2 limbs of the suture around the graft in opposite directions and tie to each other. If desired, the end suture can be threaded through a needle and the knot can be shuttled into the substance of the tendon before cutting the tails.
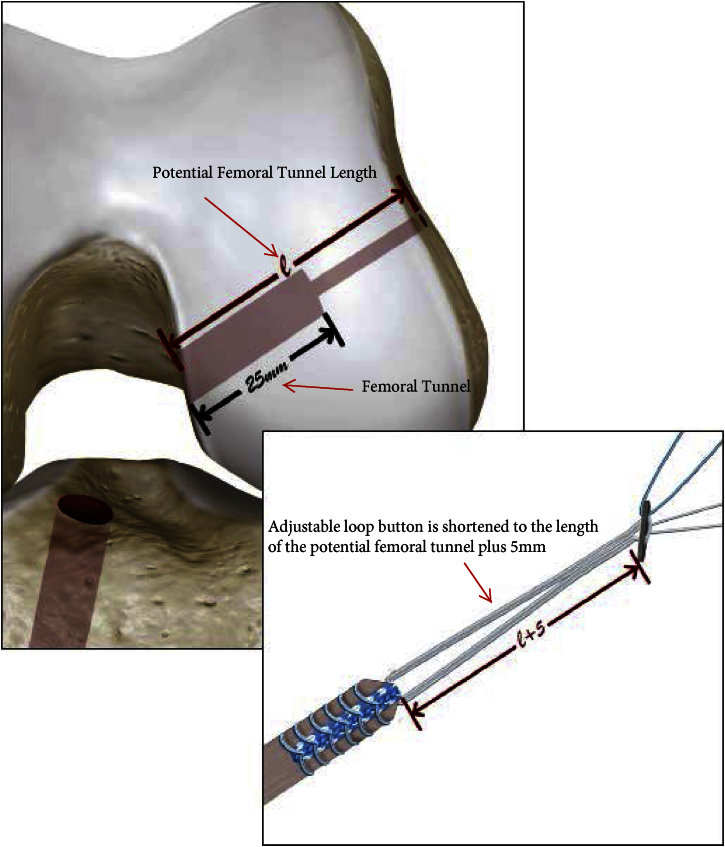
Fig 8.
Illustration of the potential femoral tunnel length represented by “e.” The adjustable loop button is adjusted to be the length of the potential femoral tunnel plus 5 mm. The reason for adding 5 mm is to allow the button to completely exit and engage the lateral femur, but also not have so much slack that it can be pulled through the iliotibial band inadvertently. The depth of the drilled tunnel should be approximately 25 mm, as 20 mm of graft needs to be able to fit inside the tunnel.
ACL Reconstruction
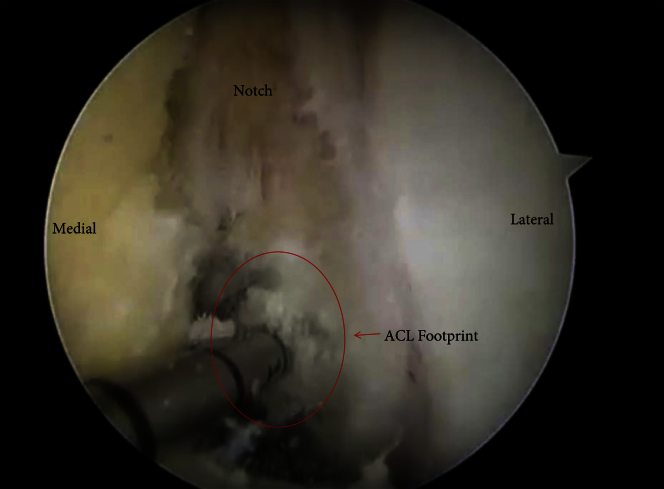
We use 3 arthroscopic portals: the standard anterior lateral portal, anterior medial (AM) portal that is just off the medial patella tendon, and an auxiliary far medial (FM) portal (Fig 2). The FM portal is first localized with a spinal needle, and should enter the joint just above the medial meniscus, and a transverse incision is made with the same trajectory. The FM portal incision should be large enough for later graft passage. For identifying the placement of the femoral tunnel, we look through the AM portal with the arthroscope. We drill anatomic tunnels centered on the bifurcate ridge in the center of the ACL femoral origin (Fig 9). No matter which femoral drilling technique a surgeon uses, it is vital to accurately measure the “potential femoral tunnel length.” The average “potential tunnel length” is typically between 30 and 40 mm, but no more than a 25-mm tunnel is needed with a 7-cm graft. This may be modified based on graft length, patient size, and potential femoral tunnel length. A looped graft-passing suture is placed in the femoral tunnel (Fig 10). The arthroscope is then switched to the anterior lateral portal and the tibial footprint marked in the center of the tibial footprint along the medial tibial eminence at a spot parallel to the posterior aspect anterior horn of the lateral meniscus. The tibial flip cutter guide is then placed through the AM portal, and the flip cutter device is drilled into the knee, deployed, and a 25-mm tibial socket is prepared (Fig 11). A looped suture is then placed into the joint. The arthroscope camera is turned to face the FM portal and the looped suture is pulled out of the FM portal under direct vision. It is key to make sure that the FM portal is clear of fat, and is large enough to allow the selected size graft through. After the looped suture is removed from the FM portal, it is attached to its proximal limbs using a snap. With the arthroscope still visualizing the FM portal, a grasper is placed through the exactly same FM portal opening ensuring that no soft tissue bridge is created. The looped suture from the femoral tunnel is then pulled out of the FM portal.
Fig 9.
Viewing from the anterior medial portal with the arthroscope and drilling through the far medial portal, we drill the femoral tunnel in the center of the bifurcate ridge in the center of the anterior cruciate ligament (ACL) femoral origin. The tunnel is drilled to 25 mm. The average “potential tunnel length” is normally 30-40 mm, but no more than a 25-mm tunnel is needed for a 7-cm graft.
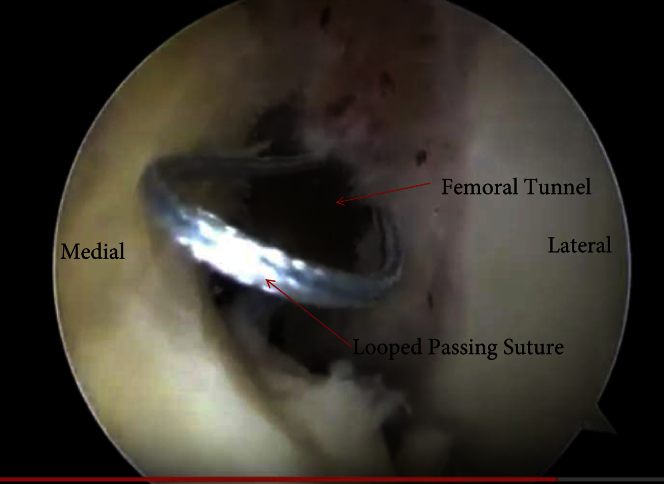
Fig 10.
A looped passing suture is pulled through the newly drilled femoral tunnel until the loop is visible at the mouth of the tunnel. This will be used to grab the sutures of the TightRope RT to pull through the femoral tunnel.
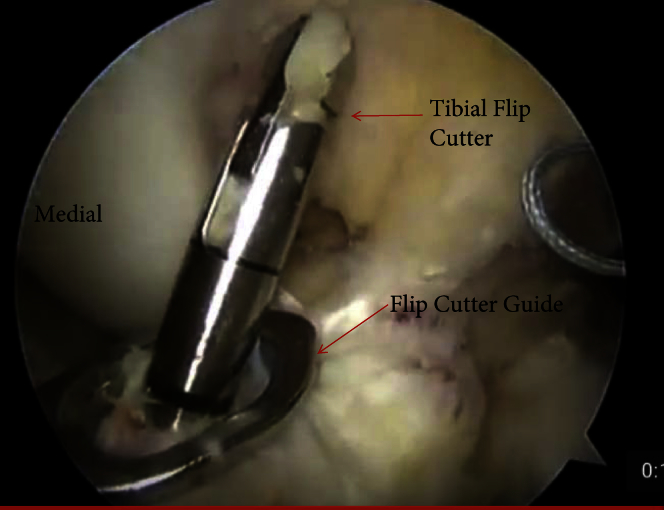
Fig 11.
Viewing from the anterior lateral portal, the tibia footprint is identified and marked with an awl approximately 2 mm anterior to the posterior aspect of the anterior horn of the lateral meniscus. The tibial flip cutter guide is placed via the anterior medial portal and the flip cutter device is drilled into the knee, deployed, and a 25-mm tibial tunnel is prepared. After this is accomplished, another looped suture should be introduced through the tibial tunnel and pulled through the far medial portal.
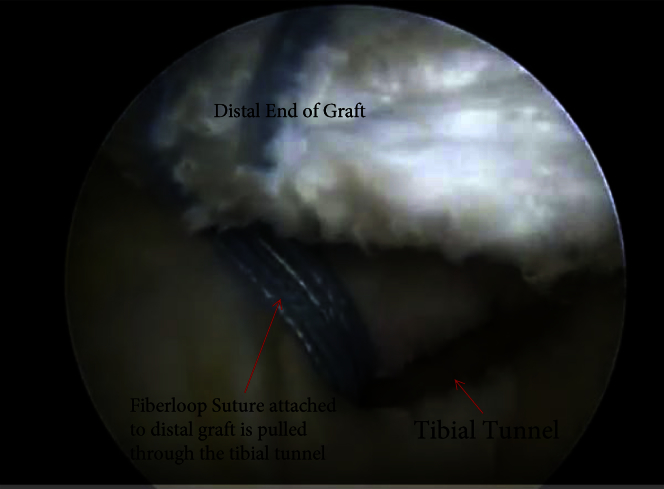
Graft Passage
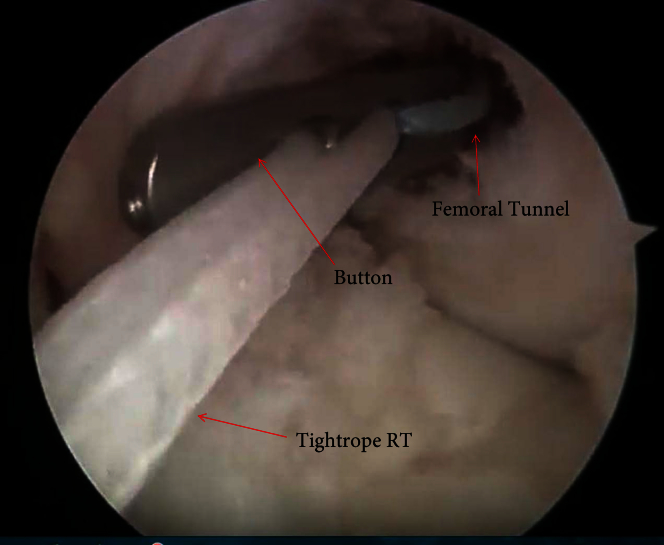
The sutures from the femoral TightRope RT are placed in the looped suture and through the femoral tunnel and out through the lateral thigh. The graft is then pulled through the FM portal until the proximal end of the graft reaches the intra-articular portion of the femoral tunnel (Fig 12). If the “potential femoral tunnel measurement” and the loop shortening were done correctly, the button should be deployed outside the femoral cortex. This can be confirmed by performing the “tight rope bounce” maneuver (thus there is no need for intraoperative imaging). The “tight rope bounce” maneuver is performed by grabbing all 4 sutures from the TightRope RT in one hand and the sutures from the distal side of the graft in the other hand. Enough tension is placed on the TightRope RT sutures to pull the button away from the cortex by a few millimeters, and then a swift pull is placed on the tibial sutures. The surgeon should feel an abrupt stop as the button engages the cortex. Note that the reason why we preshorten the tight rope is to avoid pulling the button through and deploying it outside of the iliotibial band. Once the femoral button is deployed, the loop is shortened until the sutures of the graft enter the tunnel. When no sutures remain in the joint, 20 mm of graft (the amount sutured using the fiber loop) is in the tunnel. The sutures from the distal end of the graft are then placed through the loop of the tibial passing suture. The passing suture is then pulled out of the tibia bringing the tibial end of the graft into the tibial tunnel (Fig 13). Again the FiberLoop sutures should be in the tibial tunnel ensuring 20 mm of graft in the tunnel.
Fig 12.
Sutures from the TightRope RT are threaded through the looped suture in the femur and pulled out the lateral thigh. The graft is pulled through the far medial portal until the graft reaches the intra-articular portion of the femoral tunnel. The button should be deployed on the lateral cortex of the femur. The graft is pulled into the tunnel until the sutures are no longer visible. This ensures that at least 20 mm of graft is in the tunnel.
Fig 13.
After the femoral side is secured, the sutures from the distal end of the graft are placed through the loop of the tibial passing suture and pulled through the tibia. The graft is pulled into the tibial tunnel and the FiberLoop sutures should be in the tunnel ensuring that 20 mm of graft is in the tunnel.
Graft Tensioning
With tension applied to the tibial fixation sutures, the knee is cycled approximately 20 times. The knee is placed at full extension and the tibial side secured. It is vital to have the knee fully extended during tensioning so that the patient does not lose terminal extension. To ensure that no laxity remains in the graft, the femoral side is then maximally shortened.
The tibial side can be fixed with either an adjustable loop button, or a tie-over-post screw. If a button is used, it is attached to the graft identical to the femoral side. If a screw is used, we prefer the Arthrex low profile flat-headed screw, which does not require a washer.
A review of the major pearls and pitfalls of the described technique is outlined in Table 1.
Table 1.
Pearls and Pitfalls
| Full symmetric range of motion should be obtained before surgery. |
| If a magnetic resonance imaging has been obtained preoperatively, tendon thickness may be assessed for preoperative planning and determination if a partial or full thickness graft is needed. |
| In general, we prefer partial thickness tendon harvest unless the tendon thickness is less than 6 mm. |
| Suction fluid out of knee before graft harvest if done after diagnostic scope to decrease the risk of capsular violation. |
| Failure to stay in the center of the tendon may damage perforating vessels and increase the risk of hematoma. |
| Ellipse underlying fat for adequate visualization through the small incision. |
| Dissecting too deeply may violate the capsule and increase postoperative hematoma risk. Be aware of the thin layer of fat under the tendon that can alert the surgeon to avoid deeper dissection. |
| Trim down the distal 2 cm of the graft as graft preparation will add to graft diameter. |
| Grafts greater than 7 cm may be shortened if using the all-inside technique. |
| Shorten the adjustable loop button to the potential femoral tunnel length plus 5 mm. This prevents the button from being deployed outside the iliotibial band. |
| The far medial portal needs to be big enough to allow graft passage. |
| Pull graft into tunnels until no suture remains in the joint (this will ensure 20 mm of graft in the tunnels). |
| Tension graft with the patient in full extension to avoid losing terminal extension. |
Discussion
There has been little reported literature regarding all-inside techniques with a quadriceps tendon autograft. In 1999, Leitman et al.1 described their surgical technique and results after all-inside ACL reconstruction with a quadriceps tendon bone block autograft. The authors reported all patients returned to their preinjury activity level, with no kneeling pain or patellofemoral pain. No significant differences were noted on side-to-side KT-1000 testing. One patient required revision for infection, and one required revision for subsequent trauma.
Previous authors have shown excellent results with quadriceps tendon grafts for ACL reconstruction.7, 8, 9, 10, 11, 12 A quadriceps allograft has several advantages over other grafts. Compared with a bone–patellar tendon–bone autograft, there is a lower incidence of anterior knee pain, and the graft size is more predictable than hamstring grafts and does not compromise the dynamic stability provided by the hamstrings.13 Additional advantages and disadvantages can be found in Table 2. Historically, quadriceps tendon harvest has required larger incisions. The technique presented in this note is a modification of our previously published technique.13 We have since transitioned largely to all-inside ACL reconstructions, and new minimally invasive instrumentation is developed. We believe that all-inside ACL reconstruction with a quadriceps tendon autograft harvested via this technique is easy, reproducible, and less disruptive to normal anatomy when compared with other surgical techniques.
Table 2.
Quadriceps Autograft
| Advantages |
| Low donor site morbidity |
| Minimally invasive incision |
| Predictable graft size |
| Favorable clinical outcomes |
| Large graft that fills footprint and has larger intra-articular volume |
| Favorable histology and biomechanics |
| Versatile—can be used with many techniques and in primary and revision settings |
| Reproducible, quick, easy harvest with newly developed instrumentation |
| Can be harvested with or without patellar bone plug |
| Maintains dynamic stability of medial hamstrings |
| Disadvantages |
| Lack of bone-to-bone healing |
| Learning curve |
| Unfamiliarity of surgeons with graft harvest |
| Risk of donor site hematoma |
| Risk of rectus femoris retraction if harvest passes the myotendinous junction |
Footnotes
The authors report the following potential conflicts of interests or sources of funding: H.S.S. receives support from Arthrex. J.W.X. receives support from Arthrex and Conmed.
Supplementary Data
Video showing our method of graft harvesting and graft preparation for a quadriceps tendon autograft. The patient's left leg is placed in a circumferential leg holder and the graft is harvested in 90° of flexion. An incision is made just proximal to the proximal pole of the patella and the overlying tissues are elevated off the tendon using a key elevator. A mark is made on the skin 7 cm proximal to the patella to determine graft length. Arthrex Quadriceps Tendon Graft Cutting Guide is used to cut the tendon medially and laterally in the proximal direction to the desired graft length. The distal end of the graft is then removed sharply from the patella, taking care to tapper the end of the tendon. After 2-3 cm of graft has been elevated, the free end is secured with a FiberLoop whipstitch. The Arthrex Quad Tendon Stripper/Cutter is then used to strip and cut the tendon. The graft is then taken to the back table and the remaining free end is whipstitched in the same fashion as the first using a FiberLoop. Once the femoral side is identified, a TightRope RT is secured to the femoral end of the graft. The previously placed FiberLoop is passed through the loop of the TightRope RT. The needle is passed through the graft and 3 or 4 subsequent whipstitches are placed in the graft. The needle is then cut from the suture, and the 2 limbs of suture are wrapped around the graft in opposite directions from each other and tied. Both ends of the tendons are then resized and the graft is ready for passage.
References
- 1.Leitman E.H., Morgan C.D., Grawl D.M. Quadriceps tendon anterior cruciate ligament reconstruction using the all-inside technique. Oper Tech Sports Med. 1999;7:179–188. [Google Scholar]
- 2.Lubowitz J.H., Schwartzberg R., Smith P. Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy. 2013;29:1195–1200. doi: 10.1016/j.arthro.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Benea H., d'Astorg H., Klouche S., Bauer T., Tomoaia G., Hardy P. Pain evaluation after all-inside anterior cruciate ligament reconstruction and short term functional results of a prospective randomized study. Knee. 2014;21:102–106. doi: 10.1016/j.knee.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Lubowitz J.H., Amhad C.H., Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 5.Lubowitz J.H. No-tunnel anterior cruciate ligament reconstruction: The transtibial all-inside technique. Arthroscopy. 2006;22:900.e1–900.e11. doi: 10.1016/j.arthro.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Xerogeanes J.W., Mitchell P.M., Karasev P.A., Kolesov I.A., Romine S.E. Anatomic and morphological evaluation of the quadriceps tendon using 3-dimensional magnetic resonance imaging reconstruction: Applications for anterior cruciate ligament autograft choice and procurement. Am J Sports Med. 2013;41:2392–2399. doi: 10.1177/0363546513496626. [DOI] [PubMed] [Google Scholar]
- 7.Lund B., Nielsen T., Faunø P., Christiansen S.E., Lind M. Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy. 2014;30:593–598. doi: 10.1016/j.arthro.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 8.Slone H.S., Romine S.E., Premkumar A., Xerogeanes J.W. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: A comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015;31:541–554. doi: 10.1016/j.arthro.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 9.Iriuchishima T, RyuK,Okano T, SurugaM,AizawaS, Fu FH. The evaluation of muscle recovery after anatomical singlebundle ACL reconstruction using a quadriceps autograft [published online April 7, 2016]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4124-z. [DOI] [PubMed]
- 10.Geib T.M., Shelton W.R., Phelps R.A., Clark L. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: Intermediate-term outcome. Arthroscopy. 2009;25:1408. doi: 10.1016/j.arthro.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Schulz A., Lange, Gille J. Anterior cruciate ligament reconstruction using bone plug-free quadriceps tendon autograft: Intermediate-term clinical outcome after 24-36 months. Open Access J Sports Med. 2013;4:243–249. doi: 10.2147/OAJSM.S49223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kohl S., Stutz C., Decker S. Mid-term results of transphyseal anterior cruciate ligament reconstruction in children and adolescents. Knee. 2014;21:80–85. doi: 10.1016/j.knee.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Slone H.S., Xerogeanes J.W. Anterior cruciate ligament reconstruction with quadriceps tendon autograft. JBJS Essent Surg Tech. 2014;4:e16-e16. doi: 10.2106/JBJS.ST.N.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video showing our method of graft harvesting and graft preparation for a quadriceps tendon autograft. The patient's left leg is placed in a circumferential leg holder and the graft is harvested in 90° of flexion. An incision is made just proximal to the proximal pole of the patella and the overlying tissues are elevated off the tendon using a key elevator. A mark is made on the skin 7 cm proximal to the patella to determine graft length. Arthrex Quadriceps Tendon Graft Cutting Guide is used to cut the tendon medially and laterally in the proximal direction to the desired graft length. The distal end of the graft is then removed sharply from the patella, taking care to tapper the end of the tendon. After 2-3 cm of graft has been elevated, the free end is secured with a FiberLoop whipstitch. The Arthrex Quad Tendon Stripper/Cutter is then used to strip and cut the tendon. The graft is then taken to the back table and the remaining free end is whipstitched in the same fashion as the first using a FiberLoop. Once the femoral side is identified, a TightRope RT is secured to the femoral end of the graft. The previously placed FiberLoop is passed through the loop of the TightRope RT. The needle is passed through the graft and 3 or 4 subsequent whipstitches are placed in the graft. The needle is then cut from the suture, and the 2 limbs of suture are wrapped around the graft in opposite directions from each other and tied. Both ends of the tendons are then resized and the graft is ready for passage.