Abstract
Objectives
The aim of this study is to determine how intimate partner violence against HIV-positive women affects safe infant feeding practices in Lusaka, Zambia.
Methods
A cross-sectional face-to-face survey was conducted with 320 married postpartum women at a large public health center in Lusaka, Zambia in 2014. Variables were measured using previously validated instruments. Data were analyzed using simple and multivariate logistic regression in Stata 12.
Results
Thirty-seven percent of women reported early mixed infant feeding. Women who experienced intimate partner violence had 2.8 higher adjusted odds of early mixed infant feeding (p<0.001). Women who experienced emotional violence had 1.9 higher adjusted odds of early mixed infant feeding (p<0.05). Women who experienced sexual violence had 2.3 higher adjusted odds of early mixed infant feeding (p<0.01). There is also a dose-response relationship between IPV and early mixed infant feeding. Lastly, disclosing one’s HIV-positive status to the husband was associated with at least 67% lower adjusted odds of early mixed feeding (p<0.05).
Conclusions
Intimate partner violence against HIV-positive women, in particular emotional and sexual violence, increases the likelihood of early mixed feeding, putting infants at increased risk of both mother-to-child transmission of HIV and other infant morbidities. Intimate partner violence should be given increased attention within the context of infant feeding and HIV in sub-Saharan African settings.
Keywords: intimate partner violence, domestic violence, breastfeeding, prevention of mother-to-child transmission, HIV, sub-Saharan Africa, Zambia, exclusive breastfeeding
Introduction
Child survival and the prevention of mother-to-child transmission of HIV (PMTCT) are current global health priorities. However, sub-optimal infant feeding practices in high HIV prevalence settings, such as Zambia, may be undermining these goals (Torpey et al., 2010). Currently, the Zambian Ministry of Health with guidance from the World Health Organization (WHO) recommends HIV-infected women use antiretroviral (ARV) intervention while practicing exclusive breastfeeding for the first 6 months of life. After 6 months, the mother should introduce complementary foods and continue breastfeeding for at least 12 months (ZMOH, 2010). This feeding strategy offers the best balance of protection from other morbidities, such as diarrheal disease and respiratory infections, and postnatal mother-to-child transmission of HIV (Bahl et al., 2005; WHO, 2010). Conversely, mixed infant feeding (i.e., breast milk in addition to other food) during the first 6 months of life is strongly discouraged among HIV-positive women due to the increased risk of both other diseases, namely diarrhea, and HIV transmission (Coovadia et al., 2007; Coutsoudis et al., 2001; Iliff et al., 2005).
The most recent Zambian Demographic and Health Survey (DHS) reports a high prevalence of exclusive breastfeeding for the first six months of life (73%) in the general population (CSO, 2014). However, HIV-infected women tend to introduce other food and wean their infants significantly earlier than HIV-uninfected women (Omari, Luo, Kankasa, Bhat, & Bunn, 2003). This in part may be due to the fact that HIV-related stigma prevents HIV-infected women from feeding infants in ways that are outside of perceived cultural norms, particularly if they have not disclosed their HIV status to family members (Farquhar et al., 2001).
Despite the recognition that fear of abuse often hinders women from disclosing they are HIV-infected to male partners (Maman, Mbwambo, Hogan, Kilonzo, & Sweat, 2001), the influence of intimate partner violence (IPV) has not been adequately examined in relation to infant feeding in the context of HIV. Recently, Misch and Yount (2014) report that experiences with lifetime sexual IPV is associated with reduced odds of exclusive breastfeeding among the general population of women in Liberia, Ghana, and Kenya. There is also some evidence from Uganda (Karamagi et al., 2007) and the United States indicating that IPV is associated with sub-optimal infant feeding (Silverman, Decker, Reed, & Raj, 2006). Conversely, Misch and Yount (2014) also report that sexual IPV in Zambia is associated with increased odds of exclusive breastfeeding in the general population of women, making the relationship between IPV and breastfeeding inconclusive. In addition, no studies to the author’s knowledge have specifically examined the relationship between breastfeeding practices and IPV among women who are living with HIV. The objective of this article is to determine if IPV against HIV-positive women’s is associated with early mixed infant feeding in Lusaka, Zambia. The secondary aim of this study is to determine if different forms of IPV affect safe infant feeding practices differentially and if there is a dose-response relationship between IPV and sub-optimal infant feeding.
Methods
Study Design
The results of this study are from a larger mixed methods study examining the effects of gender power dynamics within couples and HIV-positive women’s adherence to protocols across the PMTCT cascade of care, including safe infant feeding practices, in Lusaka, Zambia. The study was conducted with postpartum HIV-positive women attending a large public health center for pediatric immunizations. Data were collected from April to August of 2014 by four trained local research assistants through a face-to-face survey using closed-ended questions. The questionnaire was pretested during a pilot study in March of 2014 and evaluated by a panel of experts in Lusaka. Research assistants verbally administered the survey in the local languages on paper forms in a private location at the health center after the participant completed their health care visit. The questionnaire was written in English, but translated into the two most commonly spoken dialects in Lusaka. Participants received a small travel reimbursement for their time. Written informed consent or a thumbprint was obtained from all participants.
The four research assistants were all individuals who had previously participated in data collection for health research. They also attended a three-day training led by the primary investigator, which included in-depth discussion of research ethics and minimizing research bias. The study was designed and implemented in accordance with the World Health Organization Ethical and Safety Recommendations for Research on Domestic Violence Against Women (WHO, 2001). Women who reported IPV during the study were offered referrals to the Young Women’s Christian Association (YWCA) in Lusaka for counseling and victim support services. The study was approved by the Colorado Multiple Institutional Review Board (COMIRB) and the Excellence in Research Ethics and Science (ERES) Converge in Lusaka, Zambia.
Participants
The a priori sample size calculation demonstrated that at least 274 participants were needed to conduct a two-tailed z-test Poisson regression to detect a rate ratio of at least 1.2 with a power of 0.80 and alpha of 0.05 (Faul, Erdfelder, Lang, & Buchner, 2007). However, 320 participants were enrolled to account for potential missing data and incomplete surveys. Eligibility criteria for the study included: being female, HIV seropositive, over the age of 18 years, currently married/living with a man as if married, and the mother of an infant between three to nine months of age. Infant age criterion was selected to capture the postpartum PMTCT protocols and infant feeding practices, align with the pediatric immunization schedule in Zambia, and limit recall bias.
Recruitment for the study took place during routine pediatric immunizations in the Maternal and Child Health Department of one of the largest public health centers in Lusaka. The health center has a catchment population of over 160,000 individuals living in the surrounding low socio-economic areas. Nurses determined eligibility for the study using the infant’s “Under-Five Card,” a mother’s copy of her child’s health record that she is required to bring to all pediatric health care visits and includes the child’s birth date, height and weight, immunizations, medications, and PMTCT. If women were HIV-positive and had an infant three to nine months of age, nurses verbally invited women to go to a designated space where research assistants conducted informed consent, asked additional screening questions, and administered the survey to eligible consenting participants.
Measurement
Infant feeding, the outcome of interest for this article, was measured using previously validated questions from the Zambian Demographic and Health Survey (ZDHS) (CSO and Macro International Inc., 2009). Women were asked if they were currently breastfeeding, if they had ever breastfed the child, and if they had given any food from a list of 11 possible items, such as cow’s milk, infant formula, and porridge. If women reported yes to any of the food items, they were asked at what age the infant was first given the specific food. Those who reported giving any food prior to 6 months and breastfeeding were classified as practicing early mixed feeding.
IPV, the independent variable of interest, was measured using the Domestic Violence Module from ZDHS (CSO and Macro International Inc., 2009), which is based on the Revised Conflict Tactics Scale (CTS2). The DHS Domestic Violence Module was first developed and standardized in 2000 and has been used in more than 80 surveys, including throughout sub-Saharan Africa (MacQuarrie, Winter, & Kishor, 2014). Questions include any experiences with sexual, physical, and emotional violence from a woman’s current male partner. There are three possible events for emotional violence; seven possible events for physical violence; and two possible events for sexual violence. Dummy variables were created for: 1) experiencing any IPV; 2) expereincing emotional IPV; 3) expereincing physical IPV; and 4) expereincing sexual IPV. In addition, the number of violent events was calculated by summing the total number of specific emotional, physical, or sexual events a woman reported out of a total of 12 possible events on the survey.
If women reported experincing a violent event, she was also asked about the frequency of violence in the past year. A frequency of IPV in the past year score was created by summing how frequently each violent event occurred in the past year (often=3, sometimes=2, rarely ever=1), yielding a scale from 0 (no violent events in the past year) to 36 (experiencing every violent event often in the past year). Lastly, women were asked if they had self-disclosed their HIV-positive staus to the husband/partner, if their husband/partner had been tested for HIV, and the result of his most recent HIV test.
Covariates measured on the survey include: woman’s age in years; infant’s age in months; parity; women’s highest educational attainment; knowledge of MTCT through breastfeeding; HIV status disclosure to the husband; and a standardized wealth index. The wealth index was developed using principal component analysis (PCA) based on a list of 21 possible household assets on the survey, which is the recommended method using the DHS household assets measure (Filmer and Pritchett, 2001).
Data Cleaning and Analysis
Survey data were double entered into CSPro and exported into Stata 12 for analysis. Surveys with more than 50% missing data were not included in the analyses (n=4). Missing data (2.3%) on the other surveys were imputed using multivariate chained equations (Raghunathan, Lepkowski, Hoewyk, & Solenberger, 2001; van Buuren, Brand, Groothuis-Oudshoorn, & Rubin, 2006). Data converged indicating that the model was a good fit for the data set (StataCorp, 2009). Simple logistic regression models highlighted significant relationships at the bivariate level, which were then tested under multivariate conditions adjusting for covariates.
Results
Participant and Relationship Characteristics
Table 1 presents the sample characteristics stratified by infant feeding practices. The average age of women in the study was 29 years. The average age of infants was 6 months. Only 14% of participants had completed secondary school. Knowledge that HIV can be transmitted through breast milk from a mother to her infant was almost universal (96%). Women had been in their current relationship for almost 7 years on average and over 91% reported they had disclosed to the husband they were HIV-positive. Lastly, the majority of women (60%) reported experiencing at least one physically, sexually, or emotionally violent event in their current relationship. Emotional violence was the most commonly reported type of violence.
Table 1.
Sample Characteristics Stratified by Infant Feeding Practices
| Variable | Total (n=320) M / % |
No Mixed Feeding <6 mos. (n=202) M / % |
Mixed Feeding <6 months (n=118) M / % |
Test of Difference p-value |
|---|---|---|---|---|
| Demographic Characteristics | ||||
| Age (in years) | 29.1 | 28.8 | 29.5 | 0.262 |
| Infant age at time of survey: | ||||
| 3 mos. | 22.8% | 27.7% | 14.4% | 0.007 |
| 4–5 mos. | 26.3% | 25.2% | 28.0% | 0.594 |
| 6–9 mos. | 50.9% | 47.0% | 57.6% | 0.068 |
| Parity | 3.4 | 3.3 | 3.7 | 0.054 |
| Completed primary education | 72.0% | 71.8% | 72.0% | 0.961 |
| Completed secondary education | 13.7% | 16.8% | 8.5%+ | 0.040 |
| Wealth score (standardized index) | 0.02 | −0.02 | 0.730 | |
| Knowledge of MTCT through breast milk | 95.9% | 97.0% | 91.5% | 0.037 |
| Sexual Relationship Characteristics | ||||
| Length of relationship (years) | 6.7 | 7.0 | 6.1 | 0.160 |
| Discordant couple (n=254)1 | 35.1% | 33.6% | 37.9% | 0.486 |
| Disclosed HIV status to partner | 91.6% | 95.3% | 85.6% | 0.004 |
| Intimate partner Violence | ||||
| Any IPV | 60.8% | 52.5% | 75.4% | 0.000 |
| Physical IPV | 31.6% | 28.7% | 36.4% | 0.152 |
| Emotional IPV | 40.3% | 35.1% | 49.2% | 0.014 |
| Sexual IPV | 34.4% | 26.7% | 47.5% | 0.000 |
| Mean IPV events | 1.7 | 1.5 | 2.1 | 0.005 |
| Frequency of IPV | 3.62 | 3.1 | 4.6 | 0.004 |
| Total | 100% | 63% | 37% | |
Among couples where women reported knowing the partner’s status
Infant Feeding Practices and Bivariate Associations
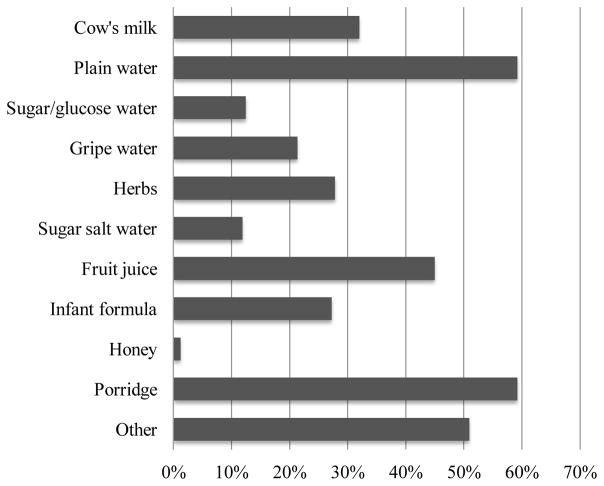
The most prevalent type of infant feeding during the infant’s first six months of life was exclusive breastfeeding (see Table 1). However, a substantial portion of women (37%) reported early mixed feeding. Porridge and plain water were the two most commonly cited food items given to the infant prior to six months (see Figure 1). Characteristics associated with an increased odds of early mixed infant feeding in the unadjusted models include: the infant being 4–5 months of age compared to less than 4 moths of age (p<0.01); the mother not having completed secondary education (p<0.05); lack of HIV and breastfeeding knowledge (p<0.05); lack of self-disclosure of HIV status to the husband (p<0.01); experiencing any IPV (p<0.001); experiencing emotional IPV (p<0.05); experiencing sexual IPV (p<0.001); the number of violent events experienced (p<0.01); and the frequency of violence in the past year (p<0.01).
Figure 1.
Reported Food/Liquids Given to Infants Prior to Six Months Among HIV-Infected Women Practicing Mixed Feeding (n=118)
Early Mixed Infant Feeding and Intimate Partner Violence
In the adjusted models, experiencing any IPV remained significantly associated with early mixed feeding after adjusting for covariates (see Table 2). Women who experienced IPV from their husband had 2.9 higher adjusted odds of early mixed feeding compared to women who did not experience IPV (p<0.001). Similar to the unadjusted models, physical violence did not significantly affect the adjusted odds of early mixed feeding (aOR 1.39, p=0.221; data not shown in table). However, emotional and sexual violence were both positively associated with higher adjusted odds of early mixed feeding. Women who experienced emotional violence had 1.9 higher adjusted odds of early mixed feeding compared to women that did not experience emotional violence (p<0.05; see Table 3). Women who experienced sexual violence had 2.3 higher adjusted odds of early mixed feeding compared to women who did not experience sexual violence (p<0.01; see Table 4).
Table 2.
Logistic Regression Results for the Adjusted Odds of Early Mixed Infant Feeding by Experiencing IPV
| Mixed Infant Feeding (n=320) | ||
|---|---|---|
| Variable | aOR (95% CI) | p-value |
| Any IPV | 2.86 (1.68–4.87) | 0.000 |
| Age | 0.98 (0.93–1.04) | 0.580 |
| Infant age | ||
| 3 mos. | 0.42 (0.20–0.90) | 0.025 |
| 4–5 mos. (reference) | 1.00 | |
| 6–9 mos. | 1.22 (0.68–2.18) | 0.493 |
| Parity | 1.27 (1.03–1.56) | 0.026 |
| Highest educational attainment | 0.96 (0.76–1.21) | 0.728 |
| Knowledge MTCT | 0.20 (0.06–0.65) | 0.007 |
| Wealth | 1.08 (0.83–1.41) | 0.566 |
| Disclosed Status | 0.35 (0.14–0.86) | 0.023 |
Table 3.
Logistic Regression Results for the Adjusted Odds of Early Mixed Infant Feeding by Experiencing Emotional Violence
| Mixed Infant Feeding (n=320) | ||
|---|---|---|
| Variable | aOR (95% CI) | p-value |
| Emotional IPV | 1.87 (1.14–3.06) | 0.013 |
| Age | 0.98 (0.92–1.04) | 0.508 |
| Infant age | ||
| 3 mos. | 0.45 (0.21–0.94) | 0.034 |
| 4–5 mos. (reference) | 1.00 | |
| 6–9 mos. | 1.28 (0.73–2.28) | 0.388 |
| Parity | 1.28 (1.04–1.57) | 0.019 |
| Highest educational attainment | 0.97 (0.77–1.23) | 0.826 |
| Knowledge MTCT | 0.21 (0.07–0.65) | 0.007 |
| Wealth | 1.11 (0.85–1.44) | 0.440 |
| Disclosed Status | 0.30 (0.12–0.74) | 0.009 |
Table 4.
Logistic Regression Results for the Adjusted Odds of Early Mixed Infant Feeding by Experiencing Sexual Violence
| Mixed Infant Feeding (n=320) | ||
|---|---|---|
| Variable | aOR (95% CI) | p-value |
| Sexual IPV | 2.25 (1.36–3.72) | 0.002 |
| Age | 0.98 (0.92–1.04) | 0.470 |
| Infant age | ||
| 3 mos. | 0.48 (0.21–0.95) | 0.035 |
| 4–5 mos. (reference) | 1.00 | |
| 6–9 mos. | 1.17 (0.66–2.08) | 0.584 |
| Parity | 1.27 (1.03–1.56) | 0.026 |
| Highest educational attainment | 0.96 (0.76–1.22) | 0.756 |
| Knowledge MTCT | 0.23 (0.08–0.73) | 0.012 |
| Wealth | 1.08 (0.83–1.40) | 0.586 |
| Disclosed Status | 0.33 (0.14–0.83) | 0.018 |
In addition, there appears to be a dose-response relationship between IPV and mixed infant feeding with women who experience more violence events and more frequent IPV more likely to practice early mixed feeding. For each additional violent event a woman experienced she had 17% higher adjusted odds of early mixed feeding (p<0.05; see Table 5). Lastly, for each increase in the frequency of IPV score, a woman had 17% higher adjusted odds of early mixed feeding (p<0.05; see Table 6).
Table 5.
Logistic Regression Results for the Adjusted Odds of Early Mixed Infant Feeding by the Number of Violent Events
| Mixed Infant Feeding (n=320) | ||
|---|---|---|
| Variable | aOR (95% CI) | p-value |
| Number of IPV events | 1.17 (1.04–1.33) | 0.012 |
| Age | 1.00 (0.92–1.04) | 0.476 |
| Infant age | ||
| 3 mos. | 0.42 (0.19–0.88) | 0.022 |
| 4–5 mos. (reference) | 1.00 | |
| 6–9 mos. | 1.23 (0.69–2.17) | 0.481 |
| Parity | 1.29 (1.05–1.58) | 0.017 |
| Highest educational attainment | 0.98 (0.77–1.23) | 0.833 |
| Knowledge MTCT | 0.22 (0.07–0.69) | 0.009 |
| Wealth | 1.11 (0.86–1.45) | 0.414 |
| Disclosed Status | 0.36 (0.14–0.92) | 0.032 |
Table 6.
Logistic Regression Results for the Adjusted Odds of Early Mixed Infant Feeding by the Frequency of Violence in the Past Year
| Mixed Infant Feeding (n=320) | ||
|---|---|---|
| Variable | aOR (95% CI) | p-value |
| Frequency of IPV score | 1.08 (1.02–1.14) | 0.011 |
| Age | 0.98 (0.92–1.04) | 0.453 |
| Infant age | ||
| 3 mos. | 0.41 (0.20–0.87) | 0.021 |
| 4–5 mos. (reference) | 1.00 | |
| 6–9 mos. | 1.23 (0.70–2.17) | 0.479 |
| Parity | 1.29 (1.05–1.58) | 0.016 |
| Highest educational attainment | 0.97 (0.77–1.23) | 0.824 |
| Knowledge MTCT | 0.22 (0.07–0.69) | 0.009 |
| Wealth | 1.12 (0.86–1.46) | 0.403 |
| Disclosed Status | 0.37 (0.15–0.94) | 0.036 |
Early Mixed Infant Feeding and HIV Status Disclosure
Self-disclosure of the woman’s HIV-positive status to her husband significantly decreased the adjusted odds that a woman would practice early mixed infant feeding (see Tables 2–6). Women who disclosed they were HIV-positive to their husband had more than a 67% reduced adjusted odds of practicing mixed infant feeding compared to women who did not disclose they were positive to the male partner (p<0.05).
Early Mixed Infant Feeding and Other Covariates
In addition to relationship characteristics, several individual-level characteristics were also associated with the adjusted odds of early mixed infant feeding (see Table 2–6). First, not surprisingly, knowledge that HIV can be transmitted through breast milk was associated with at least a 77% reduced adjusted odds of mixed infant feeding (p<0.05). Second, having more children was associated with higher adjusted odds of mixed infant feeding: for each additional child, a woman had at least 27% higher adjusted odds of mixed feeding (p<0.05). Finally, older infants under six months were more likely to be mixed fed than younger infants: infants that were less than 4 months of age had at least 52% reduced odds of being mixed fed compared to infants that were 4 to 5 months of age (p<0.05).
Discussion
Although the majority of HIV-positive women in this study reported exclusive breastfeeding, over one-third of participants practiced early mixed feeding, increasing the risk of HIV infection and infant mortality (Coovadia et al., 2007; Coutsoudis et al., 2001; Iliff et al., 2005) as well as malnutrition into early childhood (Kumar et al., 2006). The proportion of women practicing early mixed infant feeding in this study is higher than what is reported from the 2014 Zambian DHS in the general population. This supports the argument that HIV-infected women may introduce other foods earlier than HIV-uninfected women (Omari, Luo, Kankasa, Bhat, & Bunn, 2003). Appropriate pre- and post-natal counseling regarding infant feeding in the context of HIV is thus critical to ensure HIV-positive women understand the benefitis of exclusive breastfeeding to six months. Indeed, lack of knowledge regarding MTCT through breast milk was a significant predictor of early mixed feeding in the present study, which provides additional support for the growing body of literature indicating that appropriate knowledge–delivered through the health care system–on HIV and breastfeeding is a critical for sustained exclusive breastfeeding (Kimani-Murage et al., 2014; Madiba & Letsoalo, 2013; Tuthill, McGrath, & Young, 2014).
Factors outside of the health care setting, however, also significantly influence optimal infant feeding practices among postpartum women living with HIV in this Zambian context. In the present study, IPV–particularly emotional and sexual IPV–was associated with higher adjusted odds of HIV-positive women practicing early mixed feeding. Moreover, increased violent events and more frequent violence in the past year were also associated with higher adjusted odds of early mixed feeding. In settings where IPV is common, such as Zambia, this is a major concern with far-reaching infant morbidity and mortality consequences. To the author’s knowledge, this is the first study to establish that IPV victimization from a current husband negatively affects safe infant practices among HIV-infected women in sub-Saharan Africa. Although IPV and gender inequality are receiving increasing attention, much more effort is urgently needed at the policy and institutional-level, such as screening for IPV during PMTCT counseling.
The findings of this study run somewhat contrary to the findings of Misch and Yount (2014) who report using the DHS data that lifetime sexual IPV increases the adjusted odds of exclusive breastfeeding in Zambia. It is likely, however, that lifetime experiences with different forms of IPV have differing effects on women’s health behaviors than current IPV experiences. For example, some forms of lifetime IPV may result in women’s compensatory behaviors and improved infant feeding outcomes while current experiences of IPV result in deficits and difficulties with breastfeeding (Kendall-Tackett, 2007; Levendosky et al., 2003). Additionally, HIV-positive women have unique infant feeding experiences compared to the general population of women due to HIV-related stigma (Farquhar et al., 2001).
IPV victimization likely affects HIV-positive women’s infant feeding practices through several social and biological mechanisms. First, women who are fearful of IPV are less likely to disclosure they are HIV-infected to the male partners (Maman et al., 2001); making infant feeding that is outside of perceived cultural norms difficult. However, IPV remained significantly associated with sub-optimal feeding even after adjusting for HIV status disclosure to the male partner in the present study.
Second, the stress related to IPV may physically inhibit the release of oxytocin, the hormone that facilitates the flow of breast milk (Lawrence & Lawrence, 1985), leading to difficulties producing enough milk to practice exclusive breastfeeding for six months. Third, IPV against women increases the risk of emotional distress, depression, and post-traumatic stress disorder (PTSD), which are known barriers to medical adherence in general (Ellsberg, Jansen, Heise, Watts, & Garcia-Moreno, 2008), which may similarly hinder HIV-piositive women’s ability to follow the recommended infant feeding strategies. Finally, sexual IPV in particular may result in an acute aversion to exclusive breastfeeding because the practice involves a sometimes-sexualized organ (Klingelhafer, 2007)–although the applicability of this hypothesis within the African context is debatable.
In addition to IPV, this study provides evidence from Zambia to the growing body of literature linking women’s disclosure of an HIV-infected status to following the recommended infant feeding practices (Doherty et al., 2007; Doherty, Chopra, Nkonki, Jackson, & Greiner, 2006; Fadnes et al., 2010; Farquhar et al., 2001; Madiba & Letsoalo, 2013; Onono, Cohen, Jerop, Bukusi, & Turan, 2014; Sibeko, Coutsoudis, Nzuza, & Gray-Donald, 2009). Since exclusive breastfeeding is often perceived as being abnormal in Zambia (Omari et al., 2003), disclosing one’s HIV status to the husband/partner may help a woman justify why she is practicing a certain infant feeding strategy as well as garner support from the husband in order to follow the recommend protocols.
This study has several limitations. First, due to it’s cross-sectional nature, the study cannot establish causality, but has found compelling associations. Second, some of the infants in this study were only 3 to 5 months of age; women may have introduced complementary foods prior to 6 months but after the survey was completed. Thus, the proportion of women practicing exclusive breastfeeding may be slightly overestimated. Third, all data are based on self-reporting and vulnerable to social desirability, recall, and acquiescence biases. Lastly, the sample was purposively selected and not random, which limits the generalizability of findings to other populations outside of low socio-economic areas in urban sub-Saharan Africa.
Conclusion
Over one-third of the HIV-infected postpartum Zambian women in this study practiced early mixed infant feeding, increasing the risk of HIV transmission through breast milk as well as other infant morbidities. IPV against women is an important predictor of HIV-positive mother’s safe infant feeding practices. In particular, emotional and sexual violence negatively affect adherence to sustained exclusive breastfeeding. PMTCT programs should prioritize interventions aimed at capturing women in violent relationships and providing appropriate counseling and referrals in order to improve optimal infant feeding practices among women living with HIV.
Significance.
This is the first study to report a quantitative association between suboptimal infant feeding practices among HIV-positive women and experiencing intimate partner violence.
References
- Bahl R, Frost C, Kirkwood BR, Edmond K, Martines J, Bhandari N, Arthur P. Infant feeding patterns and risks of death and hospitalization in the first half of infancy: multicentre cohort study. Bull World Health Organ. 2005;83(6):418–426. /S0042-96862005000600009. [PMC free article] [PubMed] [Google Scholar]
- Boy A, Salihu HM. Intimate partner violence and birth outcomes: a systematic review. Int J Fertil Womens Med. 2004;49(4):159–164. [PubMed] [Google Scholar]
- Breastfeeding and HIV International Transmission Study Group. Late postnatal transmission of HIV-1 in breast-fed children: an individual patient data meta-analysis. J Infect Dis. 2004;189(12):2154–2166. doi: 10.1086/420834. [DOI] [PubMed] [Google Scholar]
- Buskens I, Jaffe A, Mkhatshwa H. Infant feeding practices: realities and mind sets of mothers in Southern Africa. AIDS Care. 2007;19(9):1101–1109. doi: 10.1080/09540120701336400. [DOI] [PubMed] [Google Scholar]
- Campbell J, Jones AS, Dienemann J, Kub J, Schollenberger J, O’Campo P, … Wynne C. Intimate partner violence and physical health consequences. Arch Intern Med. 2002;162(10):1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- Chisenga M, Siame J, Baisley K, Kasonka L, Filteau S. Determinants of infant feeding choices by Zambian mothers: a mixed quantitative and qualitative study. Matern Child Nutr. 2011;7(2):148–159. doi: 10.1111/j.1740-8709.2010.00264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra M, Rollins N. Infant feeding in the time of HIV: rapid assessment of infant feeding policy and programmes in four African countries scaling up prevention of mother to child transmission programmes. Arch Dis Child. 2008;93(4):288–291. doi: 10.1136/adc.2006.096321. [DOI] [PubMed] [Google Scholar]
- Coovadia HM, Rollins NC, Bland RM, Little K, Coutsoudis A, Bennish ML, Newell ML. Mother-to-child transmission of HIV-1 infection during exclusive breastfeeding in the first 6 months of life: an intervention cohort study. Lancet. 2007;369(9567):1107–1116. doi: 10.1016/S0140-6736(07)60283-9. [DOI] [PubMed] [Google Scholar]
- Coutsoudis A, Pillay K, Kuhn L, Spooner E, Tsai WY, Coovadia HM. Method of feeding and transmission of HIV-1 from mothers to children by 15 months of age: prospective cohort study from Durban, South Africa. AIDS. 2001;15(3):379–387. doi: 10.1097/00002030-200102160-00011. [DOI] [PubMed] [Google Scholar]
- CSO and Macro International Inc. Zambia Demographic and Health Survey 2007. Calverton, Maryland, USA: Central Statistical Office (CSO), Ministry of Health (MOH), Tropical Diseases Research Centre (TDRC), University of Zambia, & Macro International Inc; 2009. [Google Scholar]
- CSO, M., and ICF International. Zambia Demographic and Health Survey 2013–14. Rockville, Maryland, USA: Central Statistical Office, Ministry of Health, and ICF International; 2014. [Google Scholar]
- Doherty T, Chopra M, Nkonki L, Jackson D, Persson LA. A longitudinal qualitative study of infant-feeding decision making and practices among HIV-positive women in South Africa. J Nutr. 2006;136(9):2421–2426. doi: 10.1093/jn/136.9.2421. [DOI] [PubMed] [Google Scholar]
- Doherty T, Chopra M, Jackson D, Goga A, Colvin M, Persson LA. Effectiveness of the WHO/UNICEF guidelines on infant feeding for HIV-positive women: results from a prospective cohort study in South Africa. AIDS. 2007;21(13):1791–1797. doi: 10.1097/QAD.0b013e32827b1462. [DOI] [PubMed] [Google Scholar]
- Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet. 2008;371(9619):1165–1172. doi: 10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- Emenike E, Lawoko S, Dalal K. Intimate partner violence and reproductive health of women in Kenya. Int Nurs Rev. 2008;55(1):97–102. doi: 10.1111/j.1466-7657.2007.00580.x. [DOI] [PubMed] [Google Scholar]
- Fadnes LT, Engebretsen IM, Moland KM, Nankunda J, Tumwine JK, Tylleskar T. Infant feeding counselling in Uganda in a changing environment with focus on the general population and HIV-positive mothers - a mixed method approach. BMC Health Serv Res. 2010;10:260. doi: 10.1186/1472-6963-10-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquhar C, Mbori-Ngacha DA, Bosire RK, Nduati RW, Kreiss JK, John GC. Partner notification by HIV-1 seropositive pregnant women: association with infant feeding decisions. AIDS. 2001;15(6):815–817. doi: 10.1097/00002030-200104130-00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavioral Research Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Filmer D, Pritchett L. Estimating Wealth Effect Without Expenditure Data or Tears: An Application to Educational Enrollments in States of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Iliff PJ, Piwoz EG, Tavengwa NV, Zunguza CD, Marinda ET, Nathoo KJ, … Humphrey JH. Early exclusive breastfeeding reduces the risk of postnatal HIV-1 transmission and increases HIV-free survival. AIDS. 2005;19(7):699–708. doi: 10.1097/01.aids.0000166093.16446.c9. [DOI] [PubMed] [Google Scholar]
- Karamagi CA, Tumwine JK, Tylleskar T, Heggenhougen K. Intimate partner violence and infant morbidity: evidence of an association from a population-based study in eastern Uganda in 2003. BMC Pediatr. 2007;7:34. doi: 10.1186/1471-2431-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall-Tackett KA. Violence against women and the perinatal period: The impact of lifetime violence and abuse on pregnancy, postpartum, and breastfeeding. Trauma, Violence, & Abuse. 2007;8(3):344–353. doi: 10.1177/1524838007304406. [DOI] [PubMed] [Google Scholar]
- Klingelhafer SK. Sexual abuse and breastfeeding. Journal of Human Lactation. 2007;23(2):194–197. doi: 10.1177/0890334407300387. [DOI] [PubMed] [Google Scholar]
- Kimani-Murage EW, Wekesah F, Wanjohi M, Kyobutungi C, Ezeh AC, Musoke RN, … Griffiths P. Factors affecting actualisation of the WHO breastfeeding recommendations in urban poor settings in Kenya. Matern Child Nutr. 2014 doi: 10.1111/mcn.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobin AB, Sheth NU. Levels of adherence required for virologic suppression among newer antiretroviral medications. Ann Pharmacother. 2011;45(3):372–379. doi: 10.1345/aph.1P587. [DOI] [PubMed] [Google Scholar]
- Kumar D, Goel NK, Mittal PC, Misra P. Influence of infant-feeding practices on nutritional status of under-five children. Indian Journal of Pediatrics. 2006;73(5):417–421. doi: 10.1007/BF02758565. [DOI] [PubMed] [Google Scholar]
- Lawrence RA, Lawrence RA. Breastfeeding, a guide for the medical profession. 2. St. Louis: Mosby; 1985. [Google Scholar]
- Levendosky AA, Huth-Bocks AC, Shapiro DL, Semel MA. The impact of domestic violence on the maternal child relationship and preschool-age children’s functioning. Journal of Family Psychology. 2003;17(3):275–287. doi: 10.1037/0893-3200.17.3.275. [DOI] [PubMed] [Google Scholar]
- Madiba S, Letsoalo R. HIV disclosure to partners and family among women enrolled in prevention of mother to child transmission of HIV program: implications for infant feeding in poor resourced communities in South Africa. Glob J Health Sci. 2013;5(4):1–13. doi: 10.5539/gjhs.v5n4p1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S, Mbwambo J, Hogan NM, Kilonzo GP, Sweat M. Women’s barriers to HIV-1 testing and disclosure: Challenges for HIV-1 voluntary counselling and testing. AIDS Care. 2001;13(5):595–603. doi: 10.1080/09540120120063223. [DOI] [PubMed] [Google Scholar]
- Martin M, Del Cacho E, Codina C, MT, De Lazzari E, Mallolas J, et al. Relationship between adherence level, type of the antiretroviral regimen, and plasma HIV type 1 RNA viral load: a prospective cohort study. AIDS Res Hum Retroviruses. 2008;24:1263–1268. doi: 10.1089/aid.2008.0141. [DOI] [PubMed] [Google Scholar]
- Misch ES, Yount KM. Intimate partner violence and breastfeeding in Africa. Matern Child Health J. 2014;18(3):688–697. doi: 10.1007/s10995-013-1294-x. [DOI] [PubMed] [Google Scholar]
- Nachega JB, Hislop M, Dowdy DW, Chaisson RE, Regensberg L, Maartens G. Adherence to nonnucleoside reverse transcriptase inhibitor-based HIV therapy and virologic outcomes. Ann Intern Med. 2007;146(8):564–573. doi: 10.7326/0003-4819-146-8-200704170-00007. [DOI] [PubMed] [Google Scholar]
- Nachega JB, Marconi VC, van Zyl GU, Gardner EM, Preiser W, Hong SY, … Gross R. HIV treatment adherence, drug resistance, virologic failure: evolving concepts. Infect Disord Drug Targets. 2011;11(2):167–174. doi: 10.2174/187152611795589663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Statistical Office, & ICF Macro. Malawi Demographic and Health Survey 2010. Zomba, Malawi, and Calverton, Maryland, USA: NSO and ICF Macro; 2011. [Google Scholar]
- Omari AA, Luo C, Kankasa C, Bhat GJ, Bunn J. Infant-feeding practices of mothers of known HIV status in Lusaka, Zambia. Health Policy Plan. 2003;18(2):156–162. doi: 10.1093/heapol/czg020. [DOI] [PubMed] [Google Scholar]
- Onono MA, Cohen CR, Jerop M, Bukusi EA, Turan JM. HIV serostatus and disclosure: implications for infant feeding practice in rural south Nyanza, Kenya. BMC Public Health. 2014;14:390. doi: 10.1186/1471-2458-14-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghunathan TE, Lepkowski JM, Hoewyk JV, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27:85–95. [Google Scholar]
- Silverman JG, Decker MR, Reed E, Raj A. Intimate partner violence around the time of pregnancy: association with breastfeeding behavior. J Womens Health (Larchmt) 2006;15(8):934–940. doi: 10.1089/jwh.2006.15.934. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–245. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata 11 Multiple-Imputation Reference Manual. College Station, TX: Stata Press; 2009. [Google Scholar]
- Sibeko L, Coutsoudis A, Nzuza S, Gray-Donald K. Mothers’ infant feeding experiences: constraints and supports for optimal feeding in an HIV-impacted urban community in South Africa. Public Health Nutr. 2009;12(11):1983–1990. doi: 10.1017/S1368980009005199. [DOI] [PubMed] [Google Scholar]
- Torpey K, Kasonde P, Kabaso M, Weaver MA, Bryan G, Mukonka V, … Colebunders R. Reducing pediatric HIV infection: estimating mother-to-child transmission rates in a program setting in Zambia. Journal of Aquired Immune Deficiency Syndrome. 2010;54(4):415–422. doi: 10.1097/QAI.0b013e3181e36616. [DOI] [PubMed] [Google Scholar]
- Tuthill E, McGrath J, Young S. Commonalities and differences in infant feeding attitudes and practices in the context of HIV in sub-Saharan Africa: a metasynthesis. AIDS Care. 2014;26(2):214–225. doi: 10.1080/09540121.2013.813625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S, JPL, Brand CGM, Groothuis-Oudshoorn, Rubin DB. Fully conditional specification in multivariate imputation. Journal of Statistical Computation and Simulation. 2006;76:1049–1064. [Google Scholar]
- WHO. Guidelines on HIV and infant feeding: Prinicples and recommendations for infant feeding in the context of HIV and a summary of evidence. Geneva, Switzerland: WHO, UNAIDS, UNFPA, UNICEF; 2010. [Google Scholar]
- WHO. Programmatic Update: Use of Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants. Executive Summary. 2012 2013 from http://www.who.int/hiv/PMTCT_update.pdf.
- WHO. HIV/AIDS> Data and Statistics. 2015 Retrieved May 7, 2015, from http://www.who.int/hiv/data/en/
- Bweupe M, Chitembo L, Maswenyeho S, Murless E, Mwale J, Tambatamba B, Vwalika C, Mbewe R, editors. ZMOH. PMTCT 2010 National Protocol Guidelines: Integrated Prevention of other-to-Child Transmission of HIV. Zambia Ministry of Health; 2010. [Google Scholar]