Abstract
There is growing evidence that heightened sensitivity to unpredictability is a core mechanism of anxiety disorders. In adults, multiple anxiety disorders have been associated with a heightened startle reflex in anticipation of unpredictable threat. Child and adolescent anxiety has been linked to an increased startle reflex across baseline, safety, and threat conditions. However, it is unclear whether anxiety in youth is related to the startle reflex as a function of threat predictability. In a sample of 90 8 to 14 year-old girls, the present study examined the association between anxiety symptom dimensions and startle potentiation during a no, predictable, and unpredictable threat task. Depression symptom dimensions were also examined given their high comorbidity with anxiety and mixed relationship with the startle reflex and sensitivity to unpredictability. To assess current symptoms, participants completed the self-report Screen for Child Anxiety Related Emotional Disorders and Children’s Depression Inventory. Results indicated that social phobia symptoms were associated with heightened startle potentiation in anticipation of unpredictable threat and attenuated startle potentiation in anticipation of predictable threat. Negative mood and negative self-esteem symptoms were associated with attenuated and heightened startle potentiation in anticipation of unpredictable threat, respectively. All results remained significant after controlling for the other symptom dimensions. The present study provides initial evidence that anxiety and depression symptom dimensions demonstrate unique associations with the startle reflex in anticipation of unpredictable threat in children and adolescents.
Keywords: adolescence, anxiety, childhood, depression, startle, unpredictability
Anxiety disorders are the most prevalent class of mental illness in the United States (Kessler, Chiu, Demler, Merikangas, & Walters, 2005) and women are afflicted at twice the rate of men (Lewinsohn, Gotlib, Lewinsohn, Seeley, & Allen, 1998). Childhood and adolescence are critical periods for the emergence of anxiety symptoms and syndromes, and epidemiological studies indicate that the lifetime prevalence of anxiety disorders in adolescence is approximately 31.9% (Merikangas et al., 2010). Childhood and adolescent anxiety often follows a chronic trajectory and persists into adulthood (Beesdo, Knappe, & Pine, 2009), where it is associated with a host of adverse consequences (e.g., poor health, social and work impairment; Aderka et al., 2012; Ramsawh, Stein, Belik, Jacobi, & Sareen, 2009; Stein et al., 2005) and significant economic burden (Baxter, Vos, Scott, Ferrari, & Whiteford, 2014). In addition to anxiety disorders, increased anxiety symptoms in early adolescence have been associated with future psychopathology and poorer outcomes (Bosquet & Egeland, 2006; Cole, Peeke, Martin, Truglio, & Seroczynski, 1998; Dahne, Banducci, Kurdziel, & MacPherson, 2014; McLaughlin & King, 2015). To address this major public health concern research has begun to focus on early identification and prevention, and one way this has been accomplished is through a better understanding of the etiopathogenesis of anxiety disorders and symptoms.
There are several prominent etiological models of anxiety disorders (e.g., Barlow, 2000; Bouton, Mineka, & Barlow, 2001; Mineka & Zinbarg, 2006). A common element across most of these models is that individuals with elevated anxiety are characterized by a heightened sensitivity to aversive or threatening stimuli. This hypothesis has been supported using a variety of measures, including an attentional bias toward threat (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & van IJzendoorn, 2007; Cisler & Koster, 2010) and increased amygdala activation (Etkin & Wager, 2007; Rauch, Shin, & Wright, 2003). Another way the association between anxiety and sensitivity to aversive or threatening stimuli has been examined is through the use of the startle eye blink reflex. The startle reflex is a cross-species response to an abrupt, intense stimulus, and is a well-documented psychophysiological indicator of defense system activation (Lang, 1995; Vrana, Spence, & Lang, 1988). The startle reflex is most often elicited by presenting a loud, acoustic white noise probe and is potentiated (i.e., increased) during aversive states, such as fear and anxiety (Blumenthal et al., 2005; Lang, Bradley, & Cuthbert, 1998).
In adults, anxiety disorders and symptoms have been associated with an increased startle reflex at baseline (Morgan, Grillon, Southwick, Davis, & Charney, 1995), during aversive/threat conditions (Grillon, Ameli, Foot, & Davis, 1993; Grillon, Ameli, Goddard, Woods, & Davis, 1994; Grillon, Morgan, Davis, & Southwick, 1998a; Hamm, Cuthbert, Globisch, & Vaitl, 1997; Morgan et al., 1995), and across entire tasks (Grillon, Morgan, Davis, & Southwick, 1998b). However, there have been inconsistent and null results, and startle potentiation has been shown to differ across anxiety disorders (Craske et al., 2009; Grillon & Baas, 2003; Lang & McTeague, 2009; Vaidyanathan, Patrick, & Cuthbert, 2009). One potential explanation for the varied results is that anxiety disorders are heterogeneous both within-disorders, such that two individuals who receive the same diagnosis can present with very different symptom profiles, and between-disorders, such that several anxiety disorders have few overlapping symptoms (Mineka, Watson, & Clark, 1998). The use of categorical diagnoses or total symptom counts may obfuscate underlying relationships between core elements of the disorders and an increased startle reflex.
In children and adolescents, anxiety disorders and symptoms have been associated with an increased startle reflex during baseline (Borelli et al., 2015; Quevedo, Smith, Donzella, Schunk, & Gunnar, 2010), safety (Barker, Reeb-Sutherland, & Fox, 2014; Borelli et al., 2015; Reeb-Sutherland et al., 2009; Waters et al., 2014), and aversive/threat conditions (Waters et al., 2014). In addition, children of parents with an anxiety disorder have demonstrated an increased startle reflex across multiple conditions (Grillon, Dierker, & Merikangas, 1997; Kujawa, Glenn, Hajcak, & Klein, 2015; Merikangas, Avenevoli, Dierker, & Grillon, 1999), and an increased startle reflex during safety cues has been shown to prospectively predict first onset of anxiety disorders (Craske et al., 2013). These studies indicate that an increased startle reflex in children and adolescents is associated with both concurrent anxiety and risk for anxiety disorders. However, these findings have spanned a number of different experimental conditions (e.g., baseline, safety periods, and threat periods), suggesting there may be common characteristics or features of those conditions that impact the association between anxiety and the startle reflex.
There is growing evidence that predictability is an important characteristic that impacts the startle reflex and differentiates the emotional states of fear and anxiety (Barlow, 2000; Davis, 1998; Grillon, Baas, Lissek, Smith, & Milstein, 2004). Fear is elicited by imminent threat and facilitates immediate behavioral changes, such as fighting or fleeing. Anxiety is associated with threat that is less certain or impending, and prompts hypervigilance and sustained defensive preparedness. The distinction between fear and anxiety has been well-supported by animal (Davis, 1998), psychophysiological (Grillon et al., 2004), and pharmacological studies (Grillon et al., 2006; Perkins et al., 2009). Fear and anxiety are also represented in the Research Domain Criteria (RDoC; Insel et al., 2010) matrix by the separate Negative Valence System constructs ‘acute’ and ‘potential’ threat, respectively (NIMH, 2011).
To experimentally delineate between fear and anxiety, Grillon and colleagues developed a no, predictable, and unpredictable threat (NPU-threat) startle task (Schmitz & Grillon, 2012). The task consists of three within-subject conditions: 1) no threat (participants are safe from an aversive stimulus), 2) predictable threat (the aversive stimulus is signaled by a short duration cue), and 3) unpredictable threat (the aversive stimulus is not signaled). The no threat condition serves as a control condition while the predictable and unpredictable threat conditions model the states of fear and anxiety, respectively. Throughout the task, the startle eye blink reflex to acoustic probes (e.g., loud white noise) is recorded as an index of defense system activation across experimental conditions. In adults, the startle reflex is potentiated in anticipation of both predictable and unpredictable threat relative to no threat (Grillon et al., 2004; Nelson, Hajcak, & Shankman, 2015), and females, relative to males, exhibit a heightened startle reflex in anticipation of unpredictable threat (Grillon, 2008). Furthermore, relative to non-anxious controls, individuals with panic disorder and posttraumatic stress disorder exhibit a heightened startle reflex in anticipation of unpredictable threat, although the association with predictable threat has been mixed (Grillon, Lissek, et al., 2008; Grillon, Pine, et al., 2009; Shankman et al., 2013). Together, these studies provide initial evidence that unpredictability impacts the association between anxiety and the startle reflex. However, these investigations have been limited to adult samples that focused on categorical diagnoses rather than continuous symptom dimensions that may better capture the multidimensional nature of anxiety (Markon, Chmielewski, & Miller, 2011).
To date only one study has examined the startle reflex during the NPU-threat task in children and adolescents. Specifically, in a sample of 7 to 17 year-olds the startle reflex was potentiated in anticipation of predictable and unpredictable threat relative to no threat, and the effect for unpredictable threat was greater in girls relative to boys (Schmitz et al., 2011). These results replicate the adult literature and introduce the possibility that a heightened sensitivity to unpredictability also plays a key role in youth anxiety. However, in the same study the authors found no associations between state or trait anxiety and the startle reflex during either predictable or unpredictable threat condition. One important limitation to this study was the use of a broad, non-specific measure of anxiety that did not adequately assess diverse symptomatology in children and adolescents. Therefore, the current study attempted to replicate the only previous investigation of the startle reflex during the NPU-threat task in youth (Schmitz et al., 2011), and sought to examine more specific variation in anxiety phenomenology in relation to sensitivity to predictable and unpredictable threat.
The present study tested whether anxiety symptomatology in late childhood and early adolescence was associated with the startle reflex in anticipation of predictable and unpredictable threat. The sample consisted of 90 8 to 14 year-old girls who completed a self-report measure of anxiety symptomatology and the NPU-threat startle task. Self-reported anxiety during the different threat conditions was also assessed at the end of the task. As previously mentioned, girls, relative to boys, demonstrate increased rates of anxiety (Lewinsohn et al., 1998) and heightened sensitivity to unpredictable threat (Grillon, 2008; Schmitz et al., 2011). Therefore, the present study focused on girls only in order to increase variability in anxiety symptoms and the startle reflex in anticipation of unpredictable threat. The age range of the sample spanned late childhood and early adolescence, a period during which there is a marked increase in social phobia (Beesdo et al., 2009; Merikangas et al., 2010). Importantly, social phobia has been previously linked to intolerance of uncertainty (Boelen & Reijntjes, 2009; Carleton, Collimore, & Asmundson, 2010; Whiting et al., 2014) and an increased startle reflex in anticipation of public speaking (Cornwell, Heller, Biggs, Pine, & Grillon, 2011; Cornwell, Johnson, Berardi, & Grillon, 2006), an uncertain and unpredictable threat. Therefore, it was hypothesized that greater social phobia symptoms would be associated with increased startle and self-reported anxiety in anticipation of unpredictable (but not predictable) threat. Panic/somatic and general anxiety symptoms were also examined given the previous relationship between panic disorder and generalized anxiety disorder diagnoses and sensitivity to unpredictability in adults (Dugas, Buhr, & Ladouceur, 2004; Grillon et al., 2008; Shankman et al., 2013).
Finally, anxiety often co-occurs with depression (Kessler et al., 2005), but research on depression and the startle reflex has been mixed. For example, in adults a number of studies have found that depression is associated with a blunted emotion-modulated startle response (Allen, Trinder, & Brennan, 1999; Dichter & Tomarken, 2008; Kaviani et al., 2004; Taubitz, Robinson, & Larson, 2013; Taylor-Clift, Morris, Rottenberg, & Kovacs, 2011). However, one study found that a sad mood induction enhanced the startle reflex to unpredictable (but not predictable) threat, although the mood induction also increased state anxiety (Robinson, Overstreet, Letkiewicz, & Grillon, 2012). Other studies have reported that major depressive disorder was associated with increased startle across all conditions (Grillon, Franco-Chaves, Mateus, Ionescu, & Zarate, 2013) or was unrelated to startle during the NPU-threat task (Shankman et al., 2013). Few studies have examined the association between depression and the startle reflex in children and adolescents. For example, one study of 8 to 12 year-olds found that depression symptoms were associated with an increased startle reflex during a threat condition (Borelli, Sbarra, Crowley, & Mayes, 2011). Therefore, as a secondary aim the present study also examined different types of continuous depression symptom dimensions. There were no specific hypotheses for these analyses given the relatively limited and mixed literature on depression, the startle reflex, and sensitivity to unpredictability.
Methods
Participants
Participants included a subset of girls who completed the NPU-threat task at the baseline assessment of a larger longitudinal study in adolescents on cognitive and emotional development (total N = 317). The sample included 116 girls between the ages of 8 and 14 (M = 12.92, SD = 1.51). Racial/ethnic background was 83.6% Caucasian, 2.6% Black, 10.3% Latino, and 3.4% ‘Other’, and 63.3% of parents who accompanied the participant to the lab session (91.4% moms) had a bachelor’s degree or greater. Participants who completed the NPU-threat task were slightly older than the remainder of the overall sample who did not complete the task (M = 12.21, SD = 1.94), F(1, 315) = 11.49, p < .001, but the two groups did not differ on any other demographic (ps > .26). Participants were recruited from the community using online and flier postings, and a commercial mailing list of families with an 8 to 14 year-old girl within a 30 mile radius of Stony Brook University. Inclusion criteria were fluency in English and ability to read and understand questionnaires. Exclusion criteria were the presence of a significant developmental or medical disability. Participants were allowed to meet criteria for anxiety or depressive disorders or any other psychiatric disorder. Participants were financially compensated. Informed consent was obtained from all individual participants included in the study, and the research protocol was approved by the Institutional Review Board at Stony Brook University.
Measures
Screen for Child Anxiety Related Emotional Disorders (SCARED)
The SCARED (Birmaher et al., 1997) is a 41-item self-report instrument of childhood anxiety symptoms over the last 3 months. Each item is rated on a 3-point Likert scale ranging from 0 (not true or hardly ever true) to 2 (true or often true). The SCARED produces a total score (41 items; Cronbach’s α = .92) and five symptom dimensions, including general anxiety (9 items; α = .87), panic/somatic (13 items; α = .82), separation anxiety (8 items; α = .68), school phobia (4 items; α = .72), and social phobia (7 items; α = .86). The SCARED has been shown to be a reliable and valid measure of child and adolescent anxiety symptomatology (Birmaher et al., 1999; Hale, Crocetti, Raaijmakers, & Meeus, 2011; Monga et al., 2000), and higher scores on the SCARED have been associated with home, school, and social impairment (Langley et al., 2014). The present study focused on the symptom dimensions general anxiety, panic/somatic, and social phobia as they have previously been associated with sensitivity to unpredictability and uncertainty (Boelen & Reijntjes, 2009; Dugas et al., 2004; Grillon et al., 2009).
Children’s Depression Inventory (CDI)
The CDI (Kovacs, 1985) is a 27-item self-report measure of depression symptomatology over the last two weeks in school-aged children and adolescents. Each item is rated on a 0 to 2 scale, with greater numbers indicating increased symptom severity. The CDI produces a total score (27 items; α = .89) and five symptom dimensions, including anhedonia (8 items; α = .75), ineffectiveness (4 items; α = .64), interpersonal problems (4 items; α = .30), negative mood (6 items; α = .73), and negative self-esteem (5 items; α = .77). The reliability and validity of the CDI have been shown to be in the acceptable range (Nelson III, Politano, Finch Jr., Wendel, & Mayhall, 1987; Saylor, Edwards, & McIntosh, 1987; Saylor, Finch, Spirito, & Bennett, 1984; Smucker, Craighead, Craighead, & Green, 1986). The present study focused on the subscales anhedonia, negative mood, and negative self-esteem; the ineffectiveness and interpersonal problems subscales demonstrated poor internal consistency and were not retained for subsequent analyses.
Stimuli
All stimuli were administered using PSYLAB (Contact Precision Instruments, London, UK). Acoustic startle probes were 40-ms duration, 100-dB bursts of white noise with near-instantaneous rise time presented binaurally through headphones. The aversive stimulus was a black and white fearful female face (NimStim image 01_FE_O; Tottenham et al., 2009) presented simultaneously with a 1-s duration, 85-dB female scream played through computer speakers approximately two feet in front of the participant (i.e., the “screaming lady”; Lau et al., 2008).
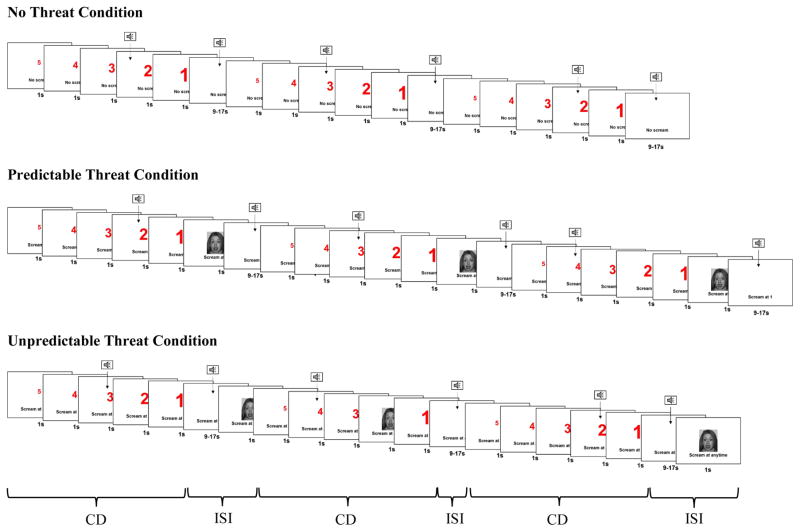
Procedure
After electrode placement, participants were seated approximately two feet in front of a 19-in. computer monitor. Participants first completed a 2.5-min baseline habituation task during which four acoustic startle probes were administered. Next, participants were provided instructions on the developmentally-modified variant of the NPU-threat task (Schmitz & Grillon, 2012). The task included three within-subjects conditions (see Figure 1): no scream (N), predictable scream (P), and unpredictable scream (U). Text at the bottom of the screen informed participants of the current condition by displaying “no scream”, “scream at 1”, or “scream at any time”. Each condition lasted 60 s, during which a 5-s visual countdown (i.e., the cue) was presented four times. The interstimulus interval (i.e., time between the countdowns during the 60-s condition) ranged from 9 to 17 s during which only the text describing the condition was on the screen. In the no threat condition, the screaming lady was never presented. In the predictable threat condition, the screaming lady was presented every time the countdown reached 1. In the unpredictable threat condition, the screaming lady was presented at any time (i.e., during the countdown or interstimulus interval). Startle probes were presented both during the countdown (2–4 s following countdown onset) and interstimulus interval (5–14 s following interstimulus interval onset). The time intervals between the screaming lady and subsequent startle probes were always greater than 10 s to ensure that subsequent probes were not affected by prior presentations of the screaming lady.
Figure 1.
Schematic of the no, predictable, and unpredictable threat (NPU-threat) task. CD = countdown; ISI = interstimulus interval.
The task consisted of two presentations of each 60-s condition (no threat, predictable threat, and unpredictable threat); during each condition, the countdown appeared three times. Conditions were presented in one of the following orders (counterbalanced): PNUPNU or UNPUNP. All participants were administered 12 screaming lady presentations (6 during the predictable threat condition, 6 during the unpredictable threat condition) and 36 startle probes (12 during the no threat condition, 12 during the predictable threat condition, and 12 during the unpredictable threat condition) during the countdown and interstimulus interval (with an equal number of startle probes occurring during the countdown and interstimulus interval). At the end of the task, participants rated how anxious they felt during the countdown and interstimulus interval of each condition and how anxious they felt when they heard the scream on a scale ranging from 1 (not at all) to 7 (extremely).
Physiological Recording and Processing
Startle eye blink electromyography (EMG) was recorded using PSYLAB (Contact Precision Instruments, London, UK) and measured from two 4-mm Ag/AgCl electrodes placed over the orbicularis oculi muscle beneath the left eye. A ground electrode was placed on the midline of the back of the neck. EMG activity was sampled at 1000 Hz and filtered between 30 and 500 Hz. Offline, EMG activity was rectified (i.e., data points were converted into absolute values) in a 200 ms window, beginning 50 ms before the onset of the startle probe, and a 6-point running average was applied to the rectified data to smooth out sharp peaks. Peak amplitude of the startle reflex was determined in the 20–150-ms time frame following the startle probe onset relative to baseline (i.e., average EMG activity in the 50 ms preceding the startle probe onset). Blinks were scored as non-responses if EMG activity during the 20–150-ms post-probe time frame did not produce a blink peak that was visually differentiated from baseline activity. Blinks were scored as missing if the baseline period was contaminated with noise, movement artifact, or if a spontaneous or voluntary blink began before minimal onset latency and thus interfered with the probe-elicited blink response. Blink magnitude (i.e., averages include values of 0 for non-response trials) was examined as this is a more conservative estimate of the startle response (Blumenthal et al., 2005).
Data Analysis
Twenty-six participants were excluded from data analysis due to equipment malfunction (n = 9), having less than 50% good trials in any single condition due to artifacts (n = 4) or non-responses (n = 6), or refusing to complete the task (n = 7), resulting in a final sample of 90 girls. Participants included in data analyses did not differ on any demographic or clinical characteristic from participants who were not included in analyses (ps > .14). To examine the startle reflex during the NPU-threat task across all participants, a Condition (no threat, predictable threat, unpredictable threat) X Cue (countdown vs. interstimulus interval) repeated measures analysis of variance (ANOVA) was conducted, and Condition X Cue interactions were followed-up by conducting separate repeated measures ANOVAs for each level of cue. To examine the association between anxiety and depression symptoms and sensitivity to predictable and unpredictable threat, startle potentiation was calculated during the threat relative to no threat conditions. Specifically, startle potentiation during predictable threat was calculated by subtracting the startle reflex during the no threat countdown from the predictable threat countdown (i.e., PCD-NCD). Startle potentiation during unpredictable threat was calculated by subtracting the startle reflex during the no threat interstimulus interval and countdown from the unpredictable interstimulus interval and countdown (i.e., UCD+ISI − NCD+ISI). The startle reflex during the interstimulus interval and countdown were averaged together as the participant was safe and in danger during both phases of the no threat and unpredictable threat conditions, respectively. Next, a two-step approach was employed to test the relationship between anxiety and depression symptoms and startle potentiation during the predictable and unpredictable threat conditions. In the first step, bivariate relationships were examined by conducting separate linear regressions with each symptom dimension as an independent variable and startle potentiation as the dependent variable. In the second step, a multiple linear regression was conducted with all symptom dimensions as simultaneous independent variables and startle potentiation as the dependent variable. For both steps, separate analyses were conducted for predictable and unpredictable threat. Identical analyses were conducted for self-reported anxiety; five participants did not complete the self-reported anxiety ratings and were excluded from those analyses. In all repeated measures analyses, Greenhouse-Geisser epsilons (G-Gε) are reported when assumptions of sphericity were violated. All analyses were conducted in IBM SPSS Statistics, Version 22.0 (Armonk, NY, USA).
Results
Sample Characteristics
Table 1 presents descriptive statistics and correlation coefficients between age and the anxiety and depression symptom dimensions. As expected, all symptoms were moderately correlated with each other. Age was positively correlated with all symptom dimensions, including anhedonia at a trend level (p < .06), but was not correlated with startle or self-reported anxiety potentiation during either the predictable or unpredictable threat condition (ps > .26).
Table 1.
Correlation Coefficients between Age and the Symptom Dimensions
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Age | - | .25 | .32 | .29 | .20 | .25 | .36 |
| SCARED | |||||||
| 2. Panic/somatic | - | .68 | .47 | .63 | .49 | .45 | |
| 3. General anxiety | - | .53 | .51 | .50 | .49 | ||
| 4. Social phobia | - | .41 | .40 | .33 | |||
| CDI | |||||||
| 5. Anhedonia | - | .68 | .59 | ||||
| 6. Negative mood | - | .66 | |||||
| 7. Negative self-esteem | - | ||||||
|
| |||||||
| M | 4.21 | 5.86 | 5.27 | 2.17 | 1.91 | 0.98 | |
| SD | 3.91 | 4.43 | 3.75 | 2.37 | 2.02 | 1.41 | |
| Range | 0–18 | 0–17 | 0–14 | 0–11 | 0–9 | 0–6 | |
Note. All bolded correlations were significant at p < .05. CDI = Children’s Depression Inventory; M = mean; SCARED = Screen for Child Anxiety Related Disorders; SD = standard deviation.
The present study focused on dimensional measures of anxiety symptomatology; however, it is important to determine the percentage of participants who reported symptomatology in the clinical range. Examination of the anxiety symptoms indicated 26 participants (28.9%) had a total score greater than or equal to the clinical cutoff of 25. This percentage varied across the general anxiety (clinical cutoff value: 9; n = 24, 20.0%), panic/somatic (clinical cutoff value: 7; n = 19, 16.7%), and social phobia (clinical cutoff value: 8; n = 29, 22.2%) subscales.
Screaming Lady Rating
Participants rated the screaming lady as mildly anxiety-provoking (M = 2.87, SD = 1.66), but no anxiety or depression symptom dimension was correlated with the scream rating (ps > .20).
Startle Reflex
Across the entire sample, participants on average had 6.65% (SD = 11.60) of trials missing due to artifacts and 5.28% (SD = 9.44) of trials were non-responses. The average number of trials (out of 6) included in each condition was comparable (no threat interstimulus interval: M = 5.56 trials, SD = 0.86, range 3–6; no threat countdown: M = 5.62, SD = 0.80, range 3–6; predictable threat interstimulus interval: M = 5.52, SD = 0.95, range 3–6; predictable threat countdown: M = 5.67, SD = 0.65, range 3–6); unpredictable threat interstimulus interval: M = 5.56, SD = 0.94, range 3–6; unpredictable threat countdown: M = 5.69, SD = 0.82, range 3–6).
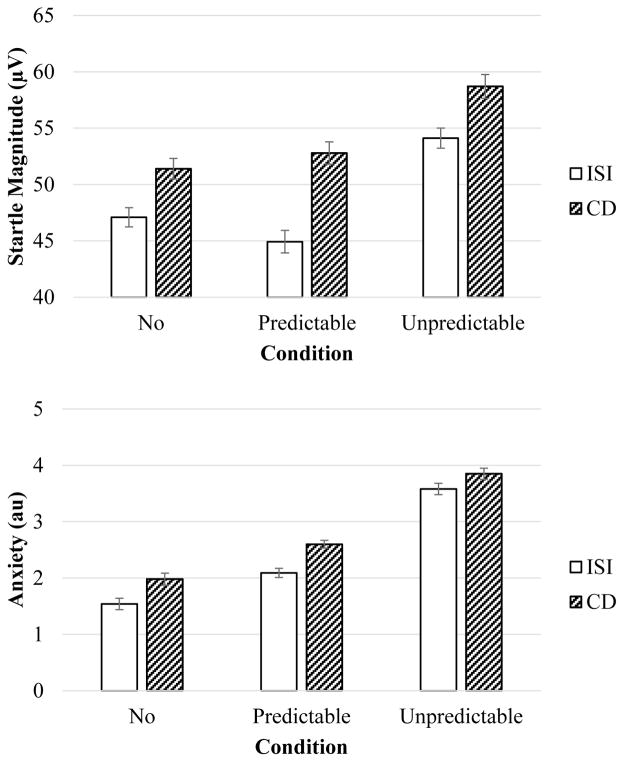
Figure 2 (top) displays the startle reflex means (and standard errors). Results indicated a main effect of condition, F(2, 178) = 25.27, p < .001, G-Gε = .88, ηp2 = .22, and cue, F(1, 89) = 33.26, p < .001, ηp2 = .27, which were qualified by a Condition X Cue interaction, F(2, 178) = 3.36, p < .05, ηp2 = .04. The Condition X Cue interaction was followed-up by conducting separate repeated measures ANOVAs for each level of cue. During the countdown, startle differed between conditions, F(2, 178) = 13.59, p < .001, G-Gε = .90, ηp2 = .13, due to greater startle during the unpredictable threat relative to the no threat, F(1, 89) = 24.02, p < .001, ηp2 = .21, and predictable threat conditions, F(1, 89) = 12.19, p < .001, ηp2 = .12, but there was no difference between the no threat and predictable threat conditions, F(1, 89) = 1.26, ns. While the startle reflex did not differ between the no threat and predictable threat conditions, the difference between the countdown and interstimulus interval for these conditions did differ, F(1, 89) = 5.93, p < .05, ηp2 = .06, such that startle potentiation during the countdown (relative to the interstimulus interval) was greater during the predictable threat compared to no threat condition. Startle during the interstimulus interval also differed between conditions, F(2, 178) = 25.40, p < .001, ηp2 = .22, due to greater startle during the unpredictable threat relative to the no threat, F(1, 89) = 29.94, p < .001, ηp2 = .25, and predictable threat conditions, F(1, 89) = 37.42, p < .001, ηp2 = .30, but there was no difference between the no threat and predictable threat conditions, F(1, 89) = 3.02, ns.1
Figure 2.
Startle magnitude (top) and self-reported anxiety (bottom) during the NPU-threat task. Error bars represent standard error. au = arbitrary units; CD = countdown; ISI = interstimulus interval.
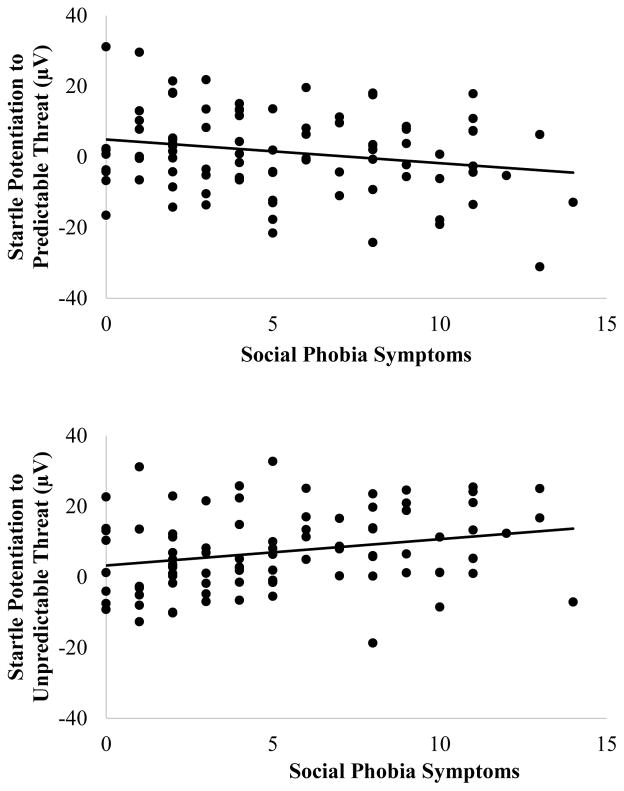
For the anxiety and depression symptom analyses (see Table 2), results indicated that social phobia symptoms were associated with heightened startle potentiation in anticipation of unpredictable threat and attenuated startle potentiation in anticipation of predictable threat (see Figure 3 for scatterplots).2 There were no other bivariate associations between anxiety and depression symptoms and startle potentiation. As shown in Table 3, multiple regression analyses confirmed that the association between social phobia and startle potentiation in anticipation of predictable and unpredictable threat remained significant even after controlling for the other symptom dimensions.3 In addition, these results indicated that negative mood and negative self-esteem symptoms were associated with attenuated and heightened, respectively, startle potentiation in anticipation of unpredictable threat.4
Table 2.
Linear Regressions with the Symptom Dimensions as the Independent Variables and Startle Potentiation to Predictable and Unpredictable Threat as the Dependent Variables
| Startle Potentiation
|
||||||
|---|---|---|---|---|---|---|
| Predictable Threat | Unpredictable Threat | |||||
| R2 | F | β | R2 | F | β | |
| SCARED | ||||||
| General anxiety | <.01 | 0.31 | .06 | <.01 | 0.11 | .03 |
| Panic/somatic | <.01 | 0.02 | −.01 | <.01 | 0.19 | .05 |
| Social phobia | .05 | 4.10* | −.21* | .07 | 6.12* | .26* |
| CDI | ||||||
| Anhedonia | <.01 | 0.15 | .04 | <.01 | 0.02 | .01 |
| Negative mood | <.01 | 0.05 | .03 | <.01 | 0.24 | −.05 |
| Negative self-esteem | <.01 | 0.14 | −.04 | .02 | 1.78 | .14 |
Note. Startle potentiation to predictable threat was calculated by subtracting the startle reflex during the no threat countdown from the predictable threat countdown. Startle potentiation to unpredictable threat was calculated by subtracting the startle reflex during the no threat interstimulus interval and countdown from the unpredictable threat interstimulus interval and countdown. CDI = Children’s Depression Inventory; SCARED = Screen for Child Anxiety Related Emotional Disorders.
p < .05.
Figure 3.
Scatterplots depicting the association between social phobia symptoms and startle potentiation in anticipation of predictable (top) and unpredictable (bottom) threat. Startle potentiation to predictable threat was calculated by subtracting the startle reflex during the no threat countdown from the predictable threat countdown. Startle potentiation to unpredictable threat was calculated by subtracting the startle reflex during the no threat interstimulus interval and countdown from the unpredictable threat interstimulus interval and countdown.
Table 3.
Multiple Regressions with the Symptom Dimensions as the Independent Variables and Startle Potentiation to Predictable and Unpredictable Threat as the Dependent Variables
| Startle Potentiation
|
||||||
|---|---|---|---|---|---|---|
| Predictable Threat | Unpredictable Threat | |||||
| R2 | F | β | R2 | F | β | |
| .10 | 1.81 | .14 | 2.39* | |||
| SCARED | ||||||
| General anxiety | .27 | −.14 | ||||
| Panic/somatic | −.09 | .01 | ||||
| Social phobia | −.35** | .36** | ||||
| CDI | ||||||
| Anhedonia | .14 | −.04 | ||||
| Negative mood | .08 | −.31* | ||||
| Negative self-esteem | −.15 | .31* | ||||
Note. Startle potentiation to predictable threat was calculated by subtracting the startle reflex during the no threat countdown from the predictable threat countdown. Startle potentiation to unpredictable threat was calculated by subtracting the startle reflex during the no threat interstimulus interval and countdown from the unpredictable threat interstimulus interval and countdown. CDI = Children’s Depression Inventory; SCARED = Screen for Child Anxiety Related Emotional Disorders.
p < .05,
p < .01.
Self-Reported Anxiety
Figure 1 (bottom) displays self-reported anxiety means (and standard errors). Results indicated a main effect of condition, F(2, 168) = 116.82, p < .001, G-Gε = .77, ηp2 = .58, such that participants reported greater anxiety during the unpredictable threat condition relative to the no threat, F(1, 84) = 144.23, p < .001, ηp2 = .63, and predictable threat condition, F(1, 84) = 138.96, p < .001, ηp2 = .62, and greater anxiety during the predictable threat relative to the no threat condition, F(1, 84) = 29.56, p < .001, ηp2 = .26. There was also a main effect of cue, F(1, 84) = 32.54, p < .001, ηp2 = .28, such that participants reported greater anxiety during the countdown relative to the interstimulus interval. However, there was no Condition X Cue interaction, F(2, 168) = 0.26, ns.
Anxiety and depression symptom analyses revealed no associations with self-reported anxiety potentiation to either predictable or unpredictable threat for both the bivariate and multiple regression analyses (ps > .15).
Discussion
In a sample of 90 8 to 14 year-old girls, the present study examined the association between anxiety and depression symptom dimensions and startle potentiation in anticipation of predictable and unpredictable threat. Across all participants, the startle reflex results during the NPU-threat task largely replicated the one previous investigation in children and adolescents (Schmitz et al., 2011), such that startle was heightened in anticipation of predictable and unpredictable threat relative to no threat. However, the present study provided novel evidence of an association between anxiety symptoms and startle potentiation. Specifically, social phobia symptoms were associated with heightened startle potentiation in anticipation of unpredictable threat and attenuated startle potentiation in anticipation of predictable threat. Furthermore, greater negative mood and negative self-esteem symptoms were associated with attenuated and heightened startle potentiation in anticipation of unpredictable threat, respectively, but they were unrelated to startle potentiation for predictable threat. Multiple regression analyses confirmed that all results remained significant even after controlling for the other symptom dimensions. These results provide initial evidence that anxiety and depression symptom dimensions demonstrate unique associations with defense system activation in anticipation of unpredictable threat in children and adolescents.
The present study adds to the extant literature on anxiety and the startle reflex in children and adolescents. Previous studies have indicated that both anxiety disorders and symptoms in youth are associated with an increased startle reflex (Barker et al., 2014; Borelli et al., 2015; Quevedo et al., 2010; Reeb-Sutherland et al., 2009; Waters et al., 2014); however, these associations have spanned baseline, safety, and threat conditions. Interestingly, most of these conditions contain some element of uncertainty or unpredictability. For example, baseline conditions typically involve the administration of unpredictable startle probes while focusing on a fixation cross or viewing a blank screen. Safety conditions signal temporary safety as they frequently precede threat conditions, and it is often unclear how long the safety period will last. Threat conditions can also contain elements of unpredictability and uncertainty, including administration of threat that is not completely predictable (e.g., administering threat at the offset of a cue, but it is unknown when exactly the cue will end) or the use of a threat reinforcement rate that is less than 100%. Indeed, a recent study found that greater intolerance of uncertainty was associated with increased startle potentiation while anticipating threat with a 50% reinforcement rate (i.e., less frequent, more uncertain) relative to a 75% reinforcement rate (i.e., more frequent, less uncertain; Chin, Nelson, Jackson, & Hajcak, 2016). In the present study, the predictable and unpredictable threat conditions were matched on all features except for the temporal predictability of threat, and anxiety symptoms were only associated with an increased startle reflex in anticipation of unpredictable (but not predictable) threat. Unpredictability may be a common element of baseline, safety, and threat conditions that at least partially contributes to the heightened startle reflex observed in youth with elevated anxiety.
In adults, multiple anxiety disorders, including panic disorder (Grillon et al., 2008; Shankman et al., 2013) and posttraumatic stress disorder (Grillon et al., 2009), have been associated with a heightened startle reflex to unpredictable threat. The one previous study to examine the NPU-threat task in children and adolescents found no association between anxiety and the startle reflex (Schmitz et al., 2011); however, that study only assessed broad state and trait anxiety. The present study examined more specific variation in anxiety phenomenology, and results indicated that social phobia symptoms specifically were associated with heightened startle potentiation in anticipation of unpredictable threat. Social phobia has previously been associated with an increased startle reflex during fearful imagery (McTeague et al., 2009), anticipation of public speaking (Cornwell et al., 2011, 2006), and across an entire task (Larsen, Norton, Walker, & Stein, 2002). However, the present study is the first to demonstrate an association between social phobia symptoms and startle potentiation as a function of the predictability of threat. This finding has important clinical implications as a heightened sensitivity to unpredictability may be a vulnerability factor that, in combination with stressful life experiences, contributes to the develop of particular forms of psychopathology. Indeed, late childhood and early adolescence are periods during which peer interactions and negative evaluation carry increased importance (Haller, Cohen Kadosh, Scerif, & Lau, 2015), and social phobia may be a prominent developmentally-relevant expression of this vulnerability. Early identification and prevention efforts should consider targeting sensitivity to unpredictability and uncertainty as a common factor that transcends emotional disorders (Boswell, Thompson-Hollands, Farchione, & Barlow, 2013).
In contrast to unpredictable threat, social phobia demonstrated the opposite relationship with predictable threat. Specifically, social phobia symptoms were associated with attenuated startle potentiation in anticipation of predictable threat. These results suggest that, when threat is imminent, individuals with social phobia symptoms may engage in immobilization or freezing prior to initiating overt action (e.g., fight or flight, as part of the defense cascade; Fanselow, 1994; Lang, Bradley, & Cuthbert, 1997). Alternatively, individuals with social phobia symptoms may engage in some form of emotion regulation or avoidance strategy, which have previously been shown to attenuate the startle reflex (Dillon & LaBar, 2005; Jackson, Malmstadt, Larson, & Davidson, 2000; Lissek et al., 2007).
There were no associations between panic/somatic and general anxiety symptoms and sensitivity to predictable or unpredictable threat. While panic disorder begins to emerge in childhood and adolescence (Beesdo et al., 2009), a large proportion of first-onset cases occur across young adulthood (Kessler, Berglund, & Demler, 2005). Therefore, a heightened sensitivity to unpredictable threat may play a more prominent role in the development of adult-onset panic disorder and symptoms. Generalized anxiety disorder is a highly heterogeneous condition that has demonstrated mixed associations with emotionality reactivity. For example, worry, the cardinal symptom of generalized anxiety disorder, has been postulated to serve as a verbal linguistic, thought-based activity that inhibits emotional reactivity (Borkovec, Alcaine, & Behar, 2004; Borkovec & Inz, 1990). However, research on generalized anxiety disorder and the startle reflex has been mixed, including one study that found the disorder was associated with an increased startle reflex (Ray et al., 2009) and another study that found it was unrelated to the startle reflex in anticipation of predictable or unpredictable threat (Grillon et al., 2009). It is possible that various features of generalized anxiety disorder (e.g., emotional distress, avoidance) are differentially related to the startle reflex, and additional research is needed to better understand what (if any) aspects of generalized anxiety contribute to increased defensive motivation.
For depression, two symptom dimensions demonstrated unique (and opposing) relationships with sensitivity to unpredictable threat. Specifically, negative mood was associated with attenuated startle potentiation in anticipation of unpredictable threat. This result is consistent with previous research indicating that depressed and dysphoric mood are associated with reduced emotion-modulated startle (Allen et al., 1999; Dichter et al., 2009; Kaviani et al., 2004; Taubitz et al., 2013; Taylor-Clift et al., 2011). In contrast, negative self-esteem was associated with heightened startle potentiation in anticipation of unpredictable threat. In other words, in addition to increased social phobia symptoms, children and adolescents with heightened sensitivity to unpredictable threat also experienced increased self-dislike and a poor subjective emotional evaluation of the self. Together, these findings highlight the importance of considering the heterogeneity of depression in relation to emotional responding.
The similar relationship between social phobia and negative self-esteem symptom dimensions and sensitivity to unpredictable threat provides intriguing evidence regarding the comorbidity of anxiety and depression. Comorbidity can arise for a number of different reasons (Klein & Riso, 1993). For example, a heightened sensitivity to unpredictable threat may be a common vulnerability factor for both anxiety and depression. Alternatively, it may be a unique vulnerability factor for anxiety, with comorbid depression arising from anxiety-related impairment. Research on social phobia has generally supported the latter explanation (Cummings, Caporino, & Kendall, 2014; Silk, Davis, McMakin, Dahl, & Forbes, 2012), and it is possible that the increased negative self-esteem is a precursor to more severe depression symptomatology. However, it is important to note that this hypothesis is speculative as the data in the present study were collected cross-sectionally. Longitudinal research is needed to more definitely test how a heightened sensitivity to unpredictable threat contributes to the development of different anxiety and depression symptoms.
The negative mood and negative self-esteem symptom dimensions did not demonstrate significant bivariate correlations with startle potentiation in anticipation of unpredictable threat, but the associations emerged in a multiple regression. These results indicate the presence of mutual suppressor effects, when two correlated predictor variables have the opposite effect on a criterion variable, but the associations are obscured when examined separately (MacKinnon et al., 2000; Watson et al., 2013). The suppressor effect finding is not particularly surprising as other symptom dimensions have demonstrated similar effects in relation to psychophysiological measures of threat and reward sensitivity (Jackson, Nelson, & Hajcak, 2016; Nelson, Kessel, Jackson, & Hajcak, 2016; Nelson, Liu, Sarapas, & Shankman, in press). Together, these results highlight the importance of considering the multidimensional nature of anxiety and depression when examining potential underlying mechanisms.
In contrast to the startle reflex, there were no associations between anxiety and depression symptom dimensions and self-report emotion ratings to predictable or unpredictable threat. Emotion ratings are susceptible to multiple individual and methodological influences, including demand characteristics (Orne, 1962), ceiling effects (Lishner, Cooter, & Zald, 2008), and prior beliefs (Robinson & Clore, 2002), and these (and other) factors could have contributed to the null findings. These results further support the utility the psychophysiological unit of analysis when examining mechanisms of psychopathology in children and adolescents (Shankman & Gorka, 2015).
The present study had several limitations that warrant consideration. First, the sample was limited to 8 to 14 year-old girls, and it is unclear whether these results generalize to boys or younger children. In addition, the sample was recruited from the community, which may have limited the ability to capture relationships between particular symptoms and the startle reflex that are more apparent in clinical populations. Second, all measures were collected cross-sectionally, which limits causal interpretations regarding anxiety, depression, and sensitivity to unpredictable threat. Third, social phobia accounted for a relatively small proportion of variance in startle potentiation to predictable and unpredictable threat. However, this is not unexpected as the symptom and startle measures shared no method variance. Finally, the NPU-threat task used just one aversive stimulus (i.e., the “screaming lady”), and it is possible that the findings for social phobia (but not general anxiety or panic/somatic) symptoms were due to the social elements of the aversive stimulus. Additional research is needed to determine whether the relationship between anxiety and depression symptom dimensions and sensitivity to unpredictable threat varies as a function of the type of aversive stimulus (e.g., social vs. physical threat).
In conclusion, the present study found that, in a sample of 8 to 14 year-old girls, anxiety and depression symptom dimensions demonstrated unique relationships with startle potentiation in anticipation of predictable and unpredictable threat. Social phobia symptoms were associated with heightened startle potentiation to unpredictable threat and attenuated startle potentiation to predictable threat. Negative mood and negative self-esteem symptoms were associated with attenuated and heightened startle potentiation to unpredictable threat, respectively. These results support theoretical models and extant evidence indicating that sensitivity to unpredictability is a discrete dimension that relates to multiple forms of psychopathology (Barlow, 2000; Davis, 1998; Grillon et al., 2004; Grupe & Nitschke, 2013; Lake & LaBar, 2011), and provides novel evidence extending this relationship to anxiety and depression symptoms in children and adolescents.
Acknowledgments
This study was funded by National Institute of Mental Health grants R01MH097767 awarded to G.H. and K01MH107808 awarded to B.D.N. The authors have no conflicts of interest to report. We would like the thank Emily Hale-Rude, Elizabeth Parisi, and Kreshnik, Burani for their assistance on this project.
Footnotes
To examine whether condition order (n = 48 predictable threat first; n = 42 unpredictable threat first) impacted the startle reflex, a Condition (no threat, predictable threat, unpredictable threat) X Cue (countdown vs. interstimulus interval) X Order (predictable threat first vs. unpredictable threat first) mixed-measures ANOVA was conducted with condition and cue entered as within-subjects factors and order entered as a between-subjects factor. Results indicated a Condition X Order interaction, F(2, 176) = 34.32, p < .001, ηp2 = .28. Follow-up analyses indicated that the startle reflex was greater during the unpredictable threat condition when it was presented first, F(1, 88) = 11.46, p < .001; however, order did not impact the startle reflex during the no threat or predictable threat conditions. Importantly, order did not moderate any relationship between anxiety or depression symptoms and the startle potentiation during the predictable or unpredictable threat condition.
Across the entire sample the startle reflex was not potentiated during the predictable threat countdown relative to the no threat countdown, but the difference between the countdown and interstimulus interval was greater during the predictable threat relative to no threat condition. Therefore, additional analyses were conducted to examine the association between anxiety and depression symptoms and startle potentiation during the countdown relative to interstimulus interval for the predictable threat and no threat conditions. Regression analyses indicated social phobia symptoms were associated with attenuated startle potentiation to the predictable threat countdown relative to interstimulus interval at a trend level, β = −.20, p < .06. There were no other significant correlations between anxiety or depression symptom dimensions and startle potentiation to the no threat or predictable threat condition (ps > .37). Similarly, multiple regression analyses indicated that social phobia symptoms were associated with attenuated startle potentiation to the predictable threat countdown relative to interstimulus interval even after controlling for the other symptom dimensions, β = −.30, p < .05. Together, these results suggest that the association between social phobia symptoms and startle potentiation to predictable threat was present regardless of the comparison condition.
Age and pubertal status, measured via the child-report Pubertal Development Scale (Petersen, Crockett, Richards, & Boxer, 1988), were also examined as potential moderators of the relationship between anxiety and depression symptoms and startle potentiation to predictable or unpredictable threat. Results indicated neither developmental measure moderated the relationship between symptoms and startle potentiation (ps > .10).
The negative mood and negative self-esteem subscales were positively correlated with each other, but did not demonstrate bivariate relationships with startle potentiation to unpredictable threat. However, the subscales demonstrated opposing relationships with startle potentiation to unpredictable threat after controlling for the other symptom dimensions. This pattern of results is consistent with reciprocal suppressor effects, when two correlated predictor variables have the opposite relationship with a criterion variable, but these associations are obscured when each are only examined separately (MacKinnon et al., 2000; Watson et al., 2013). To verify this interpretation, additional linear regressions were conducted with just negative mood and negative self-esteem entered as simultaneous independent variables and startle potentiation to unpredictable threat entered as the dependent variable. Results indicated that greater negative self-esteem was associated with heightened startle potentiation to unpredictable threat, β = .31, p < .05, and greater negative mood was associated with attenuated startle potentiation to unpredictable threat at a trend level, β = −.25, p < 07. Moreover, when social phobia was included as an independent variable, negative self-esteem, β = .27, p < .05, negative mood, β = −.35, p < .05, and social phobia, β = .31, p < .01, were all significantly associated with startle potentiation to unpredictable threat. These results confirm that negative mood and negative self-esteem demonstrated reciprocal suppressor effects, and social phobia provided additional suppressor effects on negative mood.
As part of the overarching longitudinal study, participants and their parent were also administered the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children (Kaufman et al., 1997). In the final sample of 90 participants, four participants met criteria for current social anxiety disorder. Similar to the continuous social phobia symptom measure, participants with current social anxiety disorder demonstrated greater startle potentiation in anticipation of unpredictable threat (M = 17.78, SD = 8.46) relative to those with no social anxiety disorder (M = 6.68, SD = 10.87), F(1, 88) = 4.04, p < .05, ηp2 = .04. However, there were no group differences in startle potentiation during the predictable threat condition, F(1, 88) = 0.58, ns. These results suggest that both categorical and continuous measures of social phobia were associated with heightened sensitivity to unpredictable threat.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Aderka IM, Hofmann SG, Nickerson A, Hermesh H, Gilboa-Schechtman E, Marom S. Functional impairment in social anxiety disorder. Journal of Anxiety Disorders. 2012;26:393–400. doi: 10.1016/j.janxdis.2012.01.003. [DOI] [PubMed] [Google Scholar]
- Allen NB, Trinder J, Brennan C. Affective startle modulation in clinical depression: Preliminary findings. Biological Psychiatry. 1999;46:542–550. doi: 10.1016/S0006-3223(99)00025-6. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van IJzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- Barker TV, Reeb-Sutherland BC, Fox NA. Individual differences in fear potentiated startle in behaviorally inhibited children. Developmental Psychobiology. 2014;56:133–141. doi: 10.1002/dev.21096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH. Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist. 2000;55:1247–1263. doi: 10.1037/0003-066X.55.11.1247. [DOI] [PubMed] [Google Scholar]
- Baxter AJ, Vos T, Scott KM, Ferrari AJ, Whiteford HA. The global burden of anxiety disorders in 2010. Psychological Medicine. 2014:1–12. doi: 10.1017/S0033291713003243. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. The Psychiatric Clinics of North America. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Blumenthal TD, Cuthbert BN, Filion DL, Hackley S, Lipp OV, Van Boxtel A. Committee report: Guidelines for human startle eyeblink electromyographic studies. Psychophysiology. 2005;42:1–15. doi: 10.1111/j.1469-8986.2005.00271.x. [DOI] [PubMed] [Google Scholar]
- Boelen PA, Reijntjes A. Intolerance of uncertainty and social anxiety. Journal of Anxiety Disorders. 2009;23:130–135. doi: 10.1016/j.janxdis.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Borelli JL, Ruiz SK, Crowley MJ, Mayes LC, Reyes ADL, Lewin AB. Children’s obsessive compulsive symptoms and fear-potentiated startle responses. Journal of Obsessive-Compulsive and Related Disorders. 2015;6:101–107. doi: 10.1016/j.jocrd.2015.06.006. [DOI] [Google Scholar]
- Borelli JL, Sbarra DA, Crowley MJ, Mayes LC. Mood symptoms and emotional responsiveness to threat in school-aged children. Journal of Clinical Child and Adolescent Psychology. 2011;40:220–232. doi: 10.1080/15374416.2011.546047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec T, Alcaine O, Behar E. Generalized Anxiety Disorder: Advances in Research and Practice. New York: Guilford Press; 2004. Avoidance theory of worry and generalized anxiety disorder; pp. 77–108. [Google Scholar]
- Borkovec TD, Inz J. The nature of worry in generalized anxiety disorder: A predominance of thought activity. Behaviour Research and Therapy. 1990;28:153–158. doi: 10.1016/0005-7967(90)90027-G. [DOI] [PubMed] [Google Scholar]
- Bosquet M, Egeland B. The development and maintenance of anxiety symptoms from infancy through adolescence in a longitudinal sample. Development and Psychopathology. 2006;18:517–550. doi: 10.1017/S0954579406060275. [DOI] [PubMed] [Google Scholar]
- Boswell JF, Thompson-Hollands J, Farchione TJ, Barlow DH. Intolerance of uncertainty: A common factor in the treatment of emotional disorders. Journal of Clinical Psychology. 2013;69:630–645. doi: 10.1002/jclp.21965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouton ME, Mineka S, Barlow DH. A modern learning theory perspective on the etiology of panic disorder. Psychological Review. 2001;108:4–32. doi: 10.1037//0033-295X.108.1.4. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Collimore KC, Asmundson GJG. “It’s not just the judgements—It’s that I don’t know”: Intolerance of uncertainty as a predictor of social anxiety. Journal of Anxiety Disorders. 2010;24:189–195. doi: 10.1016/j.janxdis.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Chin B, Nelson BD, Jackson F, Hajcak G. Intolerance of uncertainty and startle potentiation in relation to different threat reinforcement rates. International Journal of Psychophysiology. 2016;99:79–84. doi: 10.1016/j.ijpsycho.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Cisler JM, Koster EHW. Mechanisms of attentional biases towards threat in anxiety disorders: An integrative review. Clinical Psychology Review. 2010;30:203–216. doi: 10.1016/j.cpr.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole DA, Peeke LG, Martin JM, Truglio R, Seroczynski AD. A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of Consulting and Clinical Psychology. 1998;66:451–60. doi: 10.1037/0022-006X.66.3.451. [DOI] [PubMed] [Google Scholar]
- Cornwell BR, Heller R, Biggs A, Pine DS, Grillon C. Becoming the center of attention in social anxiety disorder: Startle reactivity to a virtual audience during speech anticipation. The Journal of Clinical Psychiatry. 2011;72:942–948. doi: 10.4088/JCP.09m05731blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell BR, Johnson L, Berardi L, Grillon C. Anticipation of public speaking in virtual reality reveals a relationship between trait social anxiety and startle reactivity. Biological Psychiatry. 2006;59:664–666. doi: 10.1016/j.biopsych.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Craske MG, Rauch SL, Ursano R, Prenoveau J, Pine DS, Zinbarg RE. What is an anxiety disorder? Depression and Anxiety. 2009;26:1066–1085. doi: 10.1002/da.20633. [DOI] [PubMed] [Google Scholar]
- Craske MG, Taylor KBW, Waters AM, Epstein A, Naliboff B, Ornitz E. Elevated responding to safe conditions as a specific risk factor for anxiety versus depressive disorders: Evidence from a longitudinal investigation. Journal of Abnormal Psychology. 2013;121:315–324. doi: 10.1037/a0025738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin. 2014;140:816–845. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahne J, Banducci AN, Kurdziel G, MacPherson L. Early adolescent symptoms of social phobia prospectively predict alcohol use. Journal of Studies on Alcohol and Drugs. 2014;75:929–936. doi: 10.15288/jsad.2014.75.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis M. Are different parts of the extended amygdala involved in fear versus anxiety? Biological Psychiatry. 1998;44:1239–1247. doi: 10.1016/S0006-3223(98)00288-1. [DOI] [PubMed] [Google Scholar]
- Dichter GS, Felder JN, Petty C, Bizzell J, Ernst M, Smoski MJ. The effects of psychotherapy on neural responses to rewards in major depression. Biological Psychiatry. 2009;66:886–897. doi: 10.1016/j.biopsych.2009.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dichter GS, Tomarken AJ. The chronometry of affective startle modulation in unipolar depression. Journal of Abnormal Psychology. 2008;117:1–15. doi: 10.1037/0021-843X.117.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon DG, LaBar KS. Startle modulation during conscious emotion regulation is arousal-dependent. Behavioral Neuroscience. 2005;119:1118–1124. doi: 10.1037/0735-7044.119.4.1118. [DOI] [PubMed] [Google Scholar]
- Dugas MJ, Buhr K, Ladouceur R. The role of intolerance of uncertainty in etiology and maintenance. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorder: Advances in research and practice. New York: Guilford Press; 2004. pp. 143–163. [Google Scholar]
- Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. The American Journal of Psychiatry. 2007;164:1476–1488. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanselow MS. Neural organization of the defensive behavior system responsible for fear. Psychonomic Bulletin & Review. 1994;1:429–438. doi: 10.3758/BF03210947. [DOI] [PubMed] [Google Scholar]
- Grillon C. Greater sustained anxiety but not phasic fear in women compared to men. Emotion. 2008;8:410–413. doi: 10.1037/1528-3542.8.3.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grillon C, Ameli R, Foot M, Davis M. Fear-potentiated startle: relationship to the level of state/trait anxiety in healthy subjects. Biological Psychiatry. 1993;33:566–574. doi: 10.1016/0006-3223(93)90094-T. [DOI] [PubMed] [Google Scholar]
- Grillon C, Ameli R, Goddard A, Woods SW, Davis M. Baseline and fear-potentiated startle in panic disorder patients. Biological Psychiatry. 1994;35:431–439. doi: 10.1016/0006-3223(94)90040-X. [DOI] [PubMed] [Google Scholar]
- Grillon C, Baas J. A review of the modulation of the startle reflex by affective states and its application in psychiatry. Clinical Neurophysiology. 2003;114:1557–1579. doi: 10.1016/S1388-2457(03)00202-5. [DOI] [PubMed] [Google Scholar]
- Grillon C, Baas JMP, Pine DS, Lissek S, Lawley M, Ellis V, Levine J. The benzodiazepine alprazolam dissociates contextual fear from cued fear in humans as assessed by fear-potentiated startle. Biological Psychiatry. 2006;60:760–766. doi: 10.1016/j.biopsych.2005.11.027. [DOI] [PubMed] [Google Scholar]
- Grillon C, Baas JP, Lissek S, Smith K, Milstein J. Anxious responses to predictable and unpredictable aversive events. Behavioral Neuroscience. 2004;118:916–924. doi: 10.1037/0735-7044.118.5.916. [DOI] [PubMed] [Google Scholar]
- Grillon C, Dierker L, Merikangas KR. Startle modulation in children at risk for anxiety disorders and/or alcoholism. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:925–932. doi: 10.1097/00004583-199707000-00014. [DOI] [PubMed] [Google Scholar]
- Grillon C, Franco-Chaves JA, Mateus CF, Ionescu DF, Zarate CA. Major depression is not associated with blunting of aversive responses: Evidence for enhanced anxious anticipation. PloS One. 2013;8:e70969. doi: 10.1371/journal.pone.0070969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grillon C, Lissek S, Rabin S, McDowell D, Dvir S, Pine DS. Increased anxiety during anticipation of unpredictable but not predictable aversive stimuli as a psychophysiologic marker of panic disorder. American Journal of Psychiatry. 2008;165:898–904. doi: 10.1176/appi.ajp.2007.07101581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grillon C, Morgan CA, Davis M, Southwick SM. Effect of darkness on acoustic startle in Vietnam veterans with PTSD. American Journal of Psychiatry. 1998a;155:812–817. doi: 10.1176/ajp.155.6.812. [DOI] [PubMed] [Google Scholar]
- Grillon C, Morgan CA, Davis M, Southwick SM. Effects of experimental context and explicit threat cues on acoustic startle in Vietnam veterans with posttraumatic stress disorder. Biological Psychiatry. 1998b;44:1027–1036. doi: 10.1016/S0006-3223(98)00034-1. [DOI] [PubMed] [Google Scholar]
- Grillon C, Pine DS, Lissek S, Rabin S, Bonne O, Vythilingam M. Increased anxiety during anticipation of unpredictable aversive stimuli in posttraumatic stress disorder but not in generalized anxiety disorder. Biological Psychiatry. 2009;66:47–53. doi: 10.1016/j.biopsych.2008.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grupe DW, Nitschke JB. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective. Nature Reviews Neuroscience. 2013;14:488–501. doi: 10.1038/nrn3524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale WW, Crocetti E, Raaijmakers QAW, Meeus WHJ. A meta-analysis of the cross-cultural psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED) Journal of Child Psychology and Psychiatry and Allied Disciplines. 2011;52:80–90. doi: 10.1111/j.1469-7610.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- Haller SPW, Cohen Kadosh K, Scerif G, Lau JYF. Social anxiety disorder in adolescence: How developmental cognitive neuroscience findings may shape understanding and interventions for psychopathology. Developmental Cognitive Neuroscience. 2015;13:11–20. doi: 10.1016/j.dcn.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamm AO, Cuthbert BN, Globisch J, Vaitl D. Fear and the startle reflex: Blink modulation and autonomic response patterns in animal and mutilation fearful subjects. Psychophysiology. 1997;34:97–107. doi: 10.1111/j.1469-8986.1997.tb02420.x. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, … Wang P. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jackson DC, Malmstadt JR, Larson CL, Davidson RJ. Suppression and enhancement of emotional responses to unpleasant pictures. Psychophysiology. 2000;37:515–522. doi: 10.1111/1469-8986.3740515. [DOI] [PubMed] [Google Scholar]
- Jackson F, Nelson BD, Hajcak G. The uncertainty of errors: Intolerance of uncertainty is associated with error-related brain activity. Biological Psychology. 2016;113:52–58. doi: 10.1016/j.biopsycho.2015.11.007. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, … Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kaviani H, Gray JA, Checkley SA, Raven PW, Wilson GD, Kumari V. Affective modulation of the startle response in depression: Influence of the severity of depression, anhedonia, and anxiety. Journal of Affective Disorders. 2004;83:21–31. doi: 10.1016/j.jad.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Kessler R, Berglund P, Demler O. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Riso LP. Basic Issues in Psychopathology. New York: Guilford Press; 1993. Psychiatric disorders: Problems of boundaries and comorbidity; pp. 19–26. [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kujawa A, Glenn CR, Hajcak G, Klein DN. Affective modulation of the startle response among children at high and low risk for anxiety disorders. Psychological Medicine. 2015;45:2647–2656. doi: 10.1017/S003329171500063X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake JI, LaBar KS. Unpredictability and uncertainty in anxiety: A new direction for emotional timing research. Frontiers in Integrative Neuroscience. 2011:5. doi: 10.3389/fnint.2011.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang, Bradley, Cuthbert . Attention and orienting: Sensory and motivational processes. New York: Lawrence Erlbaum Associates, Inc; 1997. Motivated attention: Affect, activation, and action; pp. 97–135. [Google Scholar]
- Lang PJ. The emotion probe. Studies of motivation and attention. American Psychologist. 1995;50:372–385. doi: 10.1037/0003-066X.50.5.372. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Bradley MM, Cuthbert BN. Emotion, motivation, and anxiety: Brain mechanisms and psychophysiology. Biological Psychiatry. 1998;44:1248–1263. doi: 10.1016/S0006-3223(98)00275-3. [DOI] [PubMed] [Google Scholar]
- Lang PJ, McTeague LM. The anxiety disorder spectrum: Fear imagery, physiological reactivity, and differential diagnosis. Anxiety, Stress & Coping. 2009;22:5–25. doi: 10.1080/10615800802478247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langley AK, Falk A, Peris T, Wiley JF, Kendall PC, Ginsburg G, … Piacentini J. The child anxiety impact scale: Examining parent- and child-reported impairment in child anxiety disorders. Journal of Clinical Child and Adolescent Psychology. 2014;43:579–591. doi: 10.1080/15374416.2013.817311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen DK, Norton GR, Walker JR, Stein MB. Analysis of startle responses in patients with panic disorder and social phobia. Cognitive Behaviour Therapy. 2002;31:156–169. doi: 10.1080/165060702321138555. [DOI] [Google Scholar]
- Lau JYF, Lissek S, Nelson EE, Lee Y, Roberson-Nay R, Poeth K, … Pine DS. Fear conditioning in adolescents with anxiety disorders: Results from a novel experimental paradigm. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:94–102. doi: 10.1097/chi.0b01e31815a5f01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Gotlib IH, Lewinsohn M, Seeley JR, Allen NB. Gender differences in anxiety disorders and anxiety symptoms in adolescents. Journal of Abnormal Psychology. 1998;107:109–117. doi: 10.1037/0021-843X.107.1.109. [DOI] [PubMed] [Google Scholar]
- Lishner D, Cooter A, Zald D. Addressing measurement limitations in affective rating scales: Development of an empirical valence scale. Cognition & Emotion. 2008;22:180–192. doi: 10.1080/02699930701319139. [DOI] [Google Scholar]
- Lissek S, Orme K, Mcdowell DJ, Johnson LL, Luckenbaugh DA, Baas JM, … Grillon C. Emotion regulation and potentiated startle across affective picture and threat-of-shock paradigms. Biological Psychology. 2007;76:124–133. doi: 10.1016/j.biopsycho.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prevention Science. 2000;1:173–181. doi: 10.1023/A1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE, Chmielewski M, Miller CJ. The reliability and validity of discrete and continuous measures of psychopathology: A quantitative review. Psychological Bulletin. 2011;137:856–879. doi: 10.1037/a0023678. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, King K. Developmental trajectories of anxiety and depression in early adolescence. Journal of Abnormal Child Psychology. 2015;43:311–323. doi: 10.1007/s10802-014-9898-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTeague LM, Lang PJ, Laplante MC, Cuthbert BN, Strauss CC, Bradley MM. Fearful imagery in social phobia: Generalization, comorbidity, and physiological reactivity. Biological Psychiatry. 2009;65:374–382. doi: 10.1016/j.biopsych.2008.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Avenevoli S, Dierker L, Grillon C. Vulnerability factors among children at risk for anxiety disorders. Biological Psychiatry. 1999;46:1523–1535. doi: 10.1016/S0006-3223(99)00172-9. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Mineka S, Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: It’s not what you thought it was. American Psychologist. 2006;61:10–26. doi: 10.1037/0003-066X.61.1.10. [DOI] [PubMed] [Google Scholar]
- Monga S, Birmaher B, Chiappetta L, Brent D, Kaufman J, Bridge J, Cully M. Screen for Child Anxiety-Related Emotional Disorders (SCARED): Convergent and divergent validity. Depression and Anxiety. 2000;12:85–91. doi: 10.1002/1520-6394(2000)12:2<85::AID-DA4>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Morgan CA, Grillon C, Southwick SM, Davis M, Charney DS. Fear-potentiated startle in posttraumatic stress disorder. Biological Psychiatry. 1995;38:378–385. doi: 10.1016/0006-3223(94)00321-S. [DOI] [PubMed] [Google Scholar]
- Nelson WM, III, Politano PM, Finch AJ, Jr, Wendel N, Mayhall C. Children’s Depression Inventory: Normative data and utility with emotionally disturbed children. Journal of the American Academy of Child and Adolescent Psychiatry. 1987;26:43–48. doi: 10.1097/00004583-198701000-00009. [DOI] [PubMed] [Google Scholar]
- Nelson BD, Hajcak G, Shankman SA. Event-related potentials to acoustic startle probes during the anticipation of predictable and unpredictable threat. Psychophysiology. 2015;52:887–894. doi: 10.1111/psyp.12418. [DOI] [PubMed] [Google Scholar]
- Nelson BD, Kessel EM, Jackson F, Hajcak G. The impact of an unpredictable context and intolerance of uncertainty on the electrocortical response to monetary gains and losses. Cognitive, Affective, & Behavioral Neuroscience. 2016;16:153–163. doi: 10.3758/s13415-015-0382-3. [DOI] [PubMed] [Google Scholar]
- Nelson BD, Liu H, Sarapas C, Shankman SA. Journal of Experimental Psychopathology. NIMH. NIMH Research Domain Criteria (RDoC); 2011. Intolerance of uncertainty mediates the relationship between panic and the startle reflex in anticipation of unpredictable threat. in press. Retrieved from http://www.nimh.nih.gov/research-priorities/rdoc/nimh-research-domain-criteria-rdoc.shtml. [Google Scholar]
- Orne MT. On the social psychology of the psychological experiment: With particular reference to demand characteristics and their implications. American Psychologist. 1962;17:776–783. doi: 10.1037/h0043424. [DOI] [Google Scholar]
- Perkins AM, Ettinger U, Davis R, Foster R, Williams SCR, Corr PJ. Effects of lorazepam and citalopram on human defensive reactions: Ethopharmacological differentiation of fear and anxiety. The Journal of Neuroscience. 2009;29:12617–12624. doi: 10.1523/jneurosci.2696-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17:117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Quevedo K, Smith T, Donzella B, Schunk E, Gunnar M. The startle response: Developmental effects and a paradigm for children and adults. Developmental Psychobiology. 2010;52:78–89. doi: 10.1002/dev.20415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsawh HJ, Stein MB, Belik SL, Jacobi F, Sareen J. Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. Journal of Psychiatric Research. 2009;43:926–933. doi: 10.1016/j.jpsychires.2009.01.009. [DOI] [PubMed] [Google Scholar]
- Rauch SL, Shin LM, Wright CI. Neuroimaging studies of amygdala function in anxiety disorders. Annals of the New York Academy of Sciences. 2003;985:389–410. doi: 10.1197/j.aem.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Ray WJ, Molnar C, Aikins D, Yamasaki A, Newman MG, Castonguay L, Borkovec TD. Startle response in generalized anxiety disorder. Depression and Anxiety. 2009;26:147–154. doi: 10.1002/da.20479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeb-Sutherland BC, Helfinstein SM, Degnan KA, Pérez-Edgar K, Henderson HA, Lissek S, … Fox NA. Startle response in behaviorally inhibited adolescents with a lifetime occurrence of anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:610–617. doi: 10.1097/CHI.0b013e31819f70fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson MD, Clore GL. Belief and feeling: Evidence for an accessibility model of emotional self-report. Psychological Bulletin. 2002;128:934–960. doi: 10.1037/0033-2909.128.6.934. [DOI] [PubMed] [Google Scholar]
- Robinson OJ, Overstreet C, Letkiewicz A, Grillon C. Depressed mood enhances anxiety to unpredictable threat. Psychological Medicine. 2012;42:1397–1407. doi: 10.1017/S0033291711002583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saylor CF, Edwards GL, McIntosh JA. Children’s Depression Inventory: Reliability over repeated administrations. Journal of Clinical Child Psychology. 1987;16:339–341. doi: 10.1207/s15374424jccp1604_7. [DOI] [Google Scholar]
- Saylor CF, Finch AJ, Spirito A, Bennett B. The children’s depression inventory: A systematic evaluation of psychometric properties. Journal of Consulting and Clinical Psychology. 1984;52:955–967. doi: 10.1037/0022-006X.52.6.955. [DOI] [PubMed] [Google Scholar]
- Schmitz A, Grillon C. Assessing fear and anxiety in humans using the threat of predictable and unpredictable aversive events (the NPU-threat test) Nature Protocols. 2012;7:527–532. doi: 10.1038/nprot.2012.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz A, Merikangas K, Swendsen H, Cui L, Heaton L, Grillon C. Measuring anxious responses to predictable and unpredictable threat in children and adolescents. Journal of Experimental Child Psychology. 2011;110:159–170. doi: 10.1016/j.jecp.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankman SA, Gorka SM. Psychopathology research in the RDoC era: Unanswered questions and the importance of the psychophysiological unit of analysis. International Journal of Psychophysiology. 2015;98:330–337. doi: 10.1016/j.ijpsycho.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankman SA, Nelson BD, Sarapas C, Robison-Andrew EJ, Campbell ML, Altman SE, … Gorka SM. A psychophysiological investigation of threat and reward sensitivity in individuals with panic disorder and/or major depressive disorder. Journal of Abnormal Psychology. 2013;122:322–338. doi: 10.1037/a0030747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Davis S, McMakin DL, Dahl RE, Forbes EE. Why do anxious children become depressed teenagers? The role of social evaluative threat and reward processing. Psychological Medicine. 2012;42:2095–2107. doi: 10.1017/S0033291712000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smucker MR, Craighead WE, Craighead LW, Green BJ. Normative and reliability data for the Children’s Depression Inventory. Journal of Abnormal Child Psychology. 1986;14:25–39. doi: 10.1007/BF00917219. [DOI] [PubMed] [Google Scholar]
- Stein MB, Roy-Byrne PP, Craske MG, Bystritsky A, Sullivan G, Pyne JM, … Sherbourne CD. Functional impact and health utility of anxiety disorders in primary care outpatients. Medical Care. 2005;43:1164–1170. doi: 10.1097/01.mlr.0000185750.18119.fd. [DOI] [PubMed] [Google Scholar]
- Taubitz LE, Robinson JS, Larson CL. Modulation of the startle reflex across time by unpleasant pictures distinguishes dysphoric from non-dysphoric women. International Journal of Psychophysiology. 2013;87:124–129. doi: 10.1016/j.ijpsycho.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor-Clift A, Morris BH, Rottenberg J, Kovacs M. Emotion-modulated startle in anxiety disorders is blunted by co-morbid depressive episodes. Psychological Medicine. 2011;41:129–139. doi: 10.1017/S003329171000036X. [DOI] [PubMed] [Google Scholar]
- Tottenham N, Tanaka JW, Leon AC, McCarry T, Nurse M, Hare TA, … Nelson C. The NimStim set of facial expressions: Judgments from untrained research participants. Psychiatry Research. 2009;168:242–249. doi: 10.1016/j.psychres.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidyanathan U, Patrick CJ, Cuthbert BN. Linking dimensional models of internalizing psychopathology to neurobiological systems: Affect-modulated startle as an indicator of fear and distress disorders and affiliated traits. Psychological Bulletin. 2009;135:909–942. doi: 10.1037/a0017222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrana SR, Spence EL, Lang PJ. The startle probe response: A new measure of emotion? Journal of Abnormal Psychology. 1988;97:487–491. doi: 10.1037/0021-843X.97.4.487. [DOI] [PubMed] [Google Scholar]
- Waters AM, Nazarian M, Mineka S, Zinbarg RE, Griffith JW, Naliboff B, … Craske MG. Context and explicit threat cue modulation of the startle reflex: Preliminary evidence of distinctions between adolescents with principal fear disorders versus distress disorders. Psychiatry Research. 2014;217:93–99. doi: 10.1016/j.psychres.2014.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Chmielewski M, Kotov R. The value of suppressor effects in explicating the construct validity of symptom measures. Psychological Assessment. 2013;25:929–941. doi: 10.1037/a0032781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiting SE, Jenkins WS, May AC, Rudy BM, Davis TE, Reuther ET. The role of intolerance of uncertainty in social anxiety subtypes. Journal of Clinical Psychology. 2014;70:260–272. doi: 10.1002/jclp.22024. [DOI] [PubMed] [Google Scholar]