Abstract
Introduction
Given the expected increase in the number of patients with osteoporosis and fragility fractures it is important to have concise information on trends in prescription rates of anti-osteoporosis drugs (AOD).
Methods
We undertook a retrospective observational study using the UK Clinical Practice Research Datalink (CPRD) in the UK between 1990 and 2012 in subjects 50 years or older, stratified by age, sex, geographic region and ethnicity. Yearly prescription incidence rates of any AOD and of each specific AOD were calculated as the number of patients first prescribed these AODs per 10,000 person-years (py).
Results
In women, yearly rates of first prescription of any AOD increased from 1990-2006 (from 2.3 to 169.7 per 10,000 py), followed by a plateau and a 12% decrease in the last three years. In men, a less steep increase from 1990-2007 (from 1.4 to 45.3 per 10,000 py) was followed by a plateau from 2008 onwards. Yearly rates of first prescription of any AOD increased up to the age of 85-89 years (248.9 per 10,000 py in women and 119.3 in men). There were marked differences between ethnic groups and regions. Bisphosphonates were the most frequently prescribed AODs: etidronate till 2000, and then subsequently alendronate.
Conclusion
We have demonstrated marked secular changes in rates of anti-osteoporosis drug prescription over the last two decades. The plateau (and decrease amongst women) in rates in recent years, set against an ever ageing population is worrying, suggesting that the well-documented care gap in osteoporosis treatment persists. The differences in prescription rates by geographic location and ethnicity raise intriguing questions in relation to underlying fracture rates, provision of care and health behaviour.
Summary
We studied the prescription incidence of anti-osteoporosis drugs (AOD) from 1990-2012 in the UK CPRD. Overall AOD prescription incidence showed a strong increase from 1990- 2006, followed by a plateau in both sexes and a decrease amongst women in the last three years.
Keywords: Osteoporosis, epidemiology, anti-osteoporosis drugs, AOD, fracture, secular trends
Introduction
Osteoporosis is a disease most common in the elderly population and is characterized by low bone mass and disruption of bone micro-architecture, rendering the individual susceptible to fragility fractures. Currently, there are an estimated 3 million persons with osteoporosis in the UK (1) and this number is expected to increase due to the increasing longevity of the population. In the European Union (EU) the number of individuals with osteoporosis is expected to rise from 28 million in 2010 to 34 million in 2025 (2). It is estimated that osteoporosis leads to nearly 9 million fractures per year in the EU (3). Over 300,000 patients present with fragility fractures to hospitals in the UK each year (4), resulting in substantial morbidity, often leading to a reduced quality of life, an increased risk of future fracture (5), decreased life expectancy (6) and high costs (7). It is therefore of huge importance (both for the individual and for society) that appropriate medical treatment is initiated in those at high risk for fragility fractures, and in those who have already experienced one.
During the last two decades there have been significant advances in medications to treat osteoporosis and to reduce fracture risk (8). Despite the advances in the development of pharmacological interventions and the publication of practice guidelines (9) only a minority of patients with an increased risk for fragility fracture actually receive appropriate treatment (10–14).
Studies presenting recent data on prescription trends of anti-osteoporosis drugs (AODs) in the UK are scarce (15,16). We therefore studied the rates of prescription of different AODs in the UK from year 1991 to 2012 in men and women aged 50 years or over and stratified by age, geographic region and ethnicity.
Methods
Data sources
We conducted a retrospective observational study using data from the UK Clinical Practice Research Datalink (CPRD), formerly known as the General Practice Research Database. In the health care system in the UK (the National Health Service, NHS) general practitioners (GPs) play a pivotal role, providing primary health care for 98% of the population and referring patients for specialist consultations or hospital admissions. The medical records of the GPs contain prospective information on demographics, prescriptions and diagnoses made by GPs and diagnoses from specialist consultations, outpatient visits and hospitalizations (17). The CPRD is a widely used computerized database of clinical primary care records that from its inception in 1987 stores information on around 10 million patients registered with a general practice, with active patients covering 6.9% of the UK population. The geographic distribution of the participating GP-practices and the demographic distribution of the patients are broadly representative of the general UK population (17). Clinical data for each patient are captured and stored in CPRD using Read codes (18). Data quality assessments are performed at the practice level (17). Independent validation studies (19,20) and reviews (21–23) have reported that the clinical data in the CPRD are in general of high quality. We used the ethnicity classification as developed and tested by Mathur (24), for which a high level of concordance within and across NHS sources was found in an analysis of CPRD records of ethnicity. This research was conducted in accordance with the principles of the Helsinki declaration and the protocol for this study was approved by CPRD’s Independent Scientific Advisory Committee. All data on patients were stored anonymously in CPRD and, therefore, informed consent was not required for this study.
Study population and derivation of anti-osteoporosis drug (AOD) prescription rates
The study population consisted of women and men aged 50 years or older who were registered at participating general practices and recorded in CPRD, and were active between 1990 and 2012 inclusive. All prescriptions of AOD from 1990 until 2012 were identified including the oral bisphosphonates (BPs: alendronate, risedronate, etidronate, ibandronate, clodronate) and strontium ranelate. Intravenous BPs such as zoledronic acid were not captured in CRPD, and rates of teriparatide, denosumab and calcitonin prescription were too low to enable meaningful analysis. All patients were followed-up from the index date (start of valid data collection) to 1) a first prescription of any AOD, after which the follow-up for the prescription of that specific AOD was terminated, or 2) the date of transfer of the patient out of the practice area or the patient’s death as recorded in the CPRD database, whichever came first. The incidence of first prescriptions was calculated by dividing the number of first prescriptions by the total number of persons at risk in each calendar period, presenting the incidence as number of prescriptions per 10,000 person years (py), both for each specific AOD separately and for any AOD. The analysis of individual specific AODs included the rate of first prescriptions of all specific AODs, and also when patients switched drug to that specific medication. Therefore, the rates of first prescription of any AODs are lower than the sum of the rates of each specific AOD. We stratified the analysis by sex, age, geographic locations and ethnicity.
Results
Incidence of first oral anti-osteoporosis drug prescription
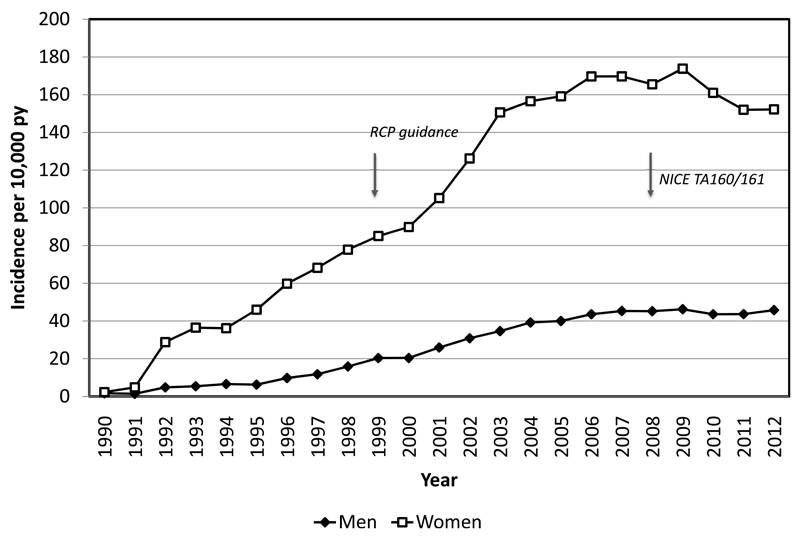
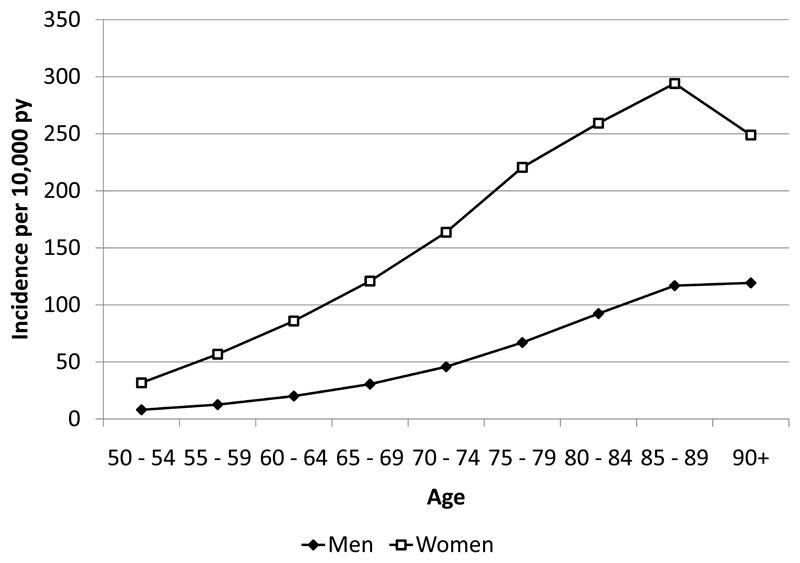
In women the rate of first prescriptions of any AOD increased steeply from 1990 to 2002 (2.3 per 10,000 py in 1990 to 169.7 per 10,000 py in 2006) (Figure 1). Subsequently there was a plateau followed by a 12.4% decrease in the last three years, from 173.8 per 10,000 py in 2009 (when the incidence was highest) to 152.2 per 10,000 py in 2012 (Figure 1). In men, a less steep increase from 1990 till 2007 (from 1.4 to 45.3 prescriptions per 10,000 py) was observed, followed by a plateau. The incidence of prescriptions for any AOD increased with age, being highest in women age 85-89 years, in which the incidence was 294.1 per 10,000 py in women and in the 90+ years age group in men, with an incidence of 119.3 per 10,000 py (Figure 2).
Figure 1.
Prescription incidence rates of any AOD in the UK from 1990 -2012 in women (F) and men (M) aged 50 and over per 10,000 py per year. Arrows show the dates of guidance from the Royal College of Physicians and the National Institute for Health and Care Excellence regarding osteoporosis in women.
Figure 2.
Prescription incidence rates of any AOD in the UK from 1990 -2012 in women (F) and men (M) aged 50 and over per 10,000 py by 5-year age-band.
Differences in prescriptions by geographic location and ethnicity
There were marked regional differences in the rates of prescription for AODs (Table 1). In women the lowest incidence was seen in the East Midlands and the highest incidence in Northern Ireland, where highest incidence in men was also observed. The lowest incidence in men was found in Yorkshire and the Humber region. There were also a marked differences by ethnicity (Table 2). The biggest differences were observed in women, were the incidence in black women was only 46% of that in white and Asian women.
Table 1.
Prescription incidence rates of oral AOD in women (F) en men (M) aged 50 and over per 10,000 py in different regions from 1990 – 2012.
| Any* |
Bisphosphonate |
Alendronate |
Risedronate |
Etidronate |
Ibandronate |
Clodronate |
Strontium |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | F | M | F | M | F | M | F | M | F | M | F | M | F | M | |
| East Midlands | 95.4 | 26.7 | 94.9 | 26.5 | 69.8 | 19.3 | 18.3 | 4.4 | 23.4 | 4.6 | 3.9 | 0.5 | 1.5 | 1.2 | 2.4 | 0.1 |
| East of England | 122.2 | 33.2 | 119.1 | 32.6 | 98.2 | 26.4 | 24.0 | 5.4 | 21.3 | 4.4 | 4.5 | 0.6 | 1.5 | 0.9 | 8.0 | 1.1 |
| North East | 118.1 | 34.8 | 117.2 | 34.4 | 94.6 | 28.7 | 31.3 | 6.8 | 18.1 | 3.6 | 3.5 | 0.3 | 1.1 | 0.8 | 4.5 | 0.6 |
| North West | 126.5 | 32.9 | 125.0 | 32.5 | 102.0 | 25.7 | 23.0 | 5.6 | 19.7 | 4.2 | 8.8 | 1.0 | 1.1 | 0.6 | 5.0 | 0.5 |
| Northern Ireland | 161.4 | 42.2 | 159.6 | 41.7 | 89.0 | 22.2 | 75.1 | 19.8 | 25.2 | 4.6 | 13.9 | 2.0 | 1.2 | 0.1 | 7.9 | 1.0 |
| Scotland | 141.2 | 35.5 | 139.4 | 35.1 | 121.2 | 29.8 | 29.1 | 6.0 | 13.9 | 2.2 | 6.4 | 0.6 | 1.1 | 0.8 | 5.9 | 0.5 |
| South Central | 123.8 | 33.5 | 121.8 | 33.0 | 106.4 | 28.1 | 24.7 | 5.2 | 12.3 | 2.6 | 5.2 | 0.6 | 0.9 | 0.8 | 6.5 | 0.8 |
| South East Coast | 133.5 | 34.8 | 129.4 | 33.9 | 107.4 | 27.8 | 24.3 | 5.2 | 18.9 | 3.8 | 7.3 | 0.8 | 1.1 | 0.9 | 12.1 | 0.7 |
| South West | 140.0 | 40.5 | 137.0 | 39.7 | 116.5 | 33.2 | 24.5 | 6.1 | 19.8 | 4.6 | 7.0 | 0.7 | 1.1 | 0.8 | 10.7 | 0.6 |
| Wales | 138.4 | 37.1 | 135.4 | 36.6 | 115.5 | 30.3 | 26.0 | 5.9 | 16.3 | 3.7 | 8.9 | 0.9 | 1.0 | 1.1 | 9.4 | 1.0 |
| West Midlands | 119.2 | 30.2 | 117.2 | 29.9 | 96.8 | 24.0 | 20.1 | 4.1 | 18.2 | 3.8 | 6.6 | 0.6 | 2.0 | 1.0 | 7.2 | 0.6 |
| Yorkshire, Humber | 99.1 | 25.9 | 98.3 | 25.7 | 67.0 | 16.7 | 31.2 | 7.7 | 21.8 | 3.9 | 3.7 | 0.6 | 0.9 | 0.8 | 2.8 | 0.2 |
| London | 131.6 | 29.8 | 128.4 | 29.0 | 108.1 | 24.0 | 21.0 | 3.7 | 17.9 | 2.9 | 5.5 | 0.4 | 1.6 | 1.1 | 10.0 | 0.3 |
Any = the rate of new prescriptions any oral anti-osteoporosis medication per 10,000 py
Table 2.
Prescription incidence rates of oral AOD in women (F) and men (M) aged 50 and over in different ethnic groups per person years from 1990 - 2012
| Any* |
Bisphosphonate |
Alendronate |
Risedronate |
Etidronate |
Ibandronate |
Clodronate |
Zoledronate |
Strontium |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | F | M | F | M | F | M | F | M | F | M | F | M | F | M | F | M | |
| White | 149.7 | 41.1 | 146.7 | 40.4 | 125.0 | 34.0 | 28.7 | 6.6 | 17.5 | 3.8 | 7.7 | 0.8 | 1.3 | 0.9 | 0.2 | 0.1 | 9.6 | 1.3 |
| Black | 68.6 | 16.8 | 67.1 | 16.7 | 58.9 | 12.6 | 8.6 | 2.6 | 3.5 | 0.7 | 2.6 | 0.2 | 1.9 | 1.6 | 0.0 | 0.0 | 3.1 | 0.5 |
| Sth Asian | 149.5 | 30.8 | 146.5 | 29.7 | 133.0 | 26.9 | 23.0 | 3.3 | 9.5 | 1.5 | 7.0 | 0.7 | 0.9 | 0.5 | 0.1 | 0.1 | 9.2 | 1.5 |
| Mixed | 95.6 | 26.0 | 93.6 | 26.0 | 82.6 | 19.0 | 9.3 | 3.0 | 7.5 | 0.8 | 3.7 | 2.3 | 1.2 | 2.3 | 0.0 | 0.0 | 8.1 | 0.0 |
| Unknown | 104.1 | 25.9 | 102.5 | 25.6 | 78.3 | 18.9 | 22.6 | 5.0 | 19.7 | 3.9 | 5.5 | 0.6 | 1.2 | 0.9 | 0.1 | 0.0 | 5.4 | 0.5 |
Any = the rate of new prescriptions any oral anti-osteoporosis medication per 10,000 py
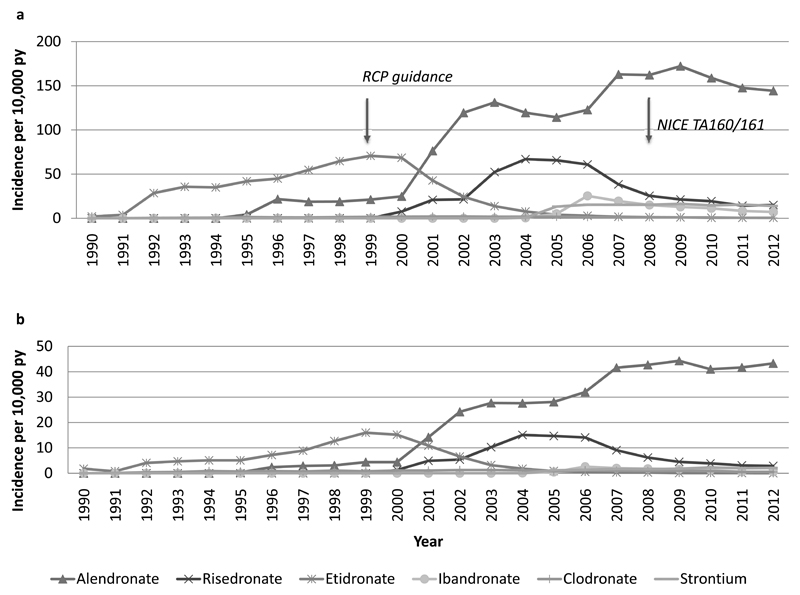
Specific medications
Bisphosphonates were the most frequently prescribed AODs. From 1990 to 1995 etidronate was the only available treatment option in both sexes and remained the dominant BP till 2000 after which the incidence of etidronate rapidly decreased to (nearly) zero (Figure 3). Prescriptions of alendronate started to appear in 1995 after which there was a gradual increase till 2000 (incidence 76.3 and 14.2 per 10,000 py in women and men, respectively. Thereafter there was a steep rise in rates until 2003 (131.2 and 27.7 per 10,000 py in women and men, respectively). After a plateau amongst men and a reduction in prescription rates in women till 2006, the incidence in both sexes increased again to peak in 2009 (172.2 in women and 44.3 per men per 10,000 py). From then on there was a plateau in men and a decrease in women. Risedronate first appeared in 2000 and prescription rates increased strongly till 2004 with a peak incidence per 10,000 py of 66.9 in women and 15.1 in men. Subsequently there was a plateau till 2006 followed by a decrease after which the incidence in the last years levelled out to around 15 per 10,000 py in women and 3 per 10,000 py in men. Ibandronate appeared in 2004. In women the incidence peaked after 2 years at 25.4 per 10,000 py followed by a steady decrease in incidence whilst in men the incidence did rise materially. At the end of the 22 year study period, alendronate accounted for over 90% of AOD prescriptions in both sexes. Prescriptions for strontium ranelate first appeared in 2004 and rose gradually in women to reach a plateau of around 15 per 10,000 py, whereas in men the incidence remained very low.
Figure 3.
Prescription incidence rates of specific AOD in the UK from 1990 -2012 in women (A) and men (B) aged 50 and over per 10,000 py per year. Arrows show the dates of guidance from the Royal College of Physicians and the National Institute for Health and Care Excellence regarding osteoporosis in women.
Discussion
We observed a rapid increase in the rate of first anti-osteoporosis drug prescription in women from 1990 to 2003 followed by a gradual further increase to 2006, followed by stabilization till 2009 after which the incidence decreased. In men there was a similar increase, followed by a plateau from 2006 onwards. Additionally, we demonstrated marked differences in rates of AOD prescription by geographic location and ethnicity.
The increase in prescriptions is a positive trend, which, as can be expected, was more pronounced in women than in men. The rapid increase in AOD prescriptions from 1990 to 2006 as shown in our results accords with trends in AOD use seen in other studies (25–27), as does the higher prescription rates in women compared to men. In a study from the UK using the CPRD database (15), prescribing of BP to women 40 years or older increased throughout the entire study period from 1991 to 2005. It is unclear whether this increase in rates of AOD prescribing is a reflection of an increase in osteoporosis incidence, a narrowing of the treatment gap or other factors, although we have recently demonstrated no overall change in age- and sex-adjusted rates of all fractures over the same calendar period (28). We did observe increases in some fracture types however, such as hip fracture in men and vertebral fracture in both sexes. A recent study from the UK using the CPRD (16) to determine the probability of initiating with anti-osteoporosis therapy after hip fracture showed an increase from 7% in 2000 to 46% in 2010, suggesting that a narrowing of the treatment-gap might have contributed to the increase of AOD prescriptions. As in other studies (29) we also found that BPs (especially alendronate) were the dominant AOD. An explanation for this finding might be that oral AOD are the first line treatment options according to the guidelines for primary and secondary prevention of fractures in the UK (30,31), with second line treatments usually initiated by a medical specialist in secondary care. A further CPRD study has shown that in 2008 almost all patients were treated with oral BPs and only 0.3% of patients were treated with other AOD (32), which is in accordance with our results.
We observed that the incidence of oral BP prescriptions no longer increased after 2006 and in women even decreased from 2009 onwards, although potentially stabilised from 2011-2012. Whilst the decrease in prescribing amongst women is relatively modest, the downward trend is concerning, and is consistent with the results of other studies. A study from Ontario, Canada, examining trends in AOD use in GP practices, found a marked increase in the annual rate from 2000 to 2007, after which the increase slowed down and stabilized in 2008 and 2009 (27). A study from the USA (33) using data from the Medical Expenditure Panel Survey (based on household interviews and pharmacy surveys) examined trends in oral bisphosphonate use among patients aged 55 years or older from 1996 to 2012. A greater than 50% decline in oral bisphosphonate use occurring from 2008 to 2012 was found to coincide with media reports of safety concerns with bisphosphonates, namely osteonecrosis of the jaw, atrial fibrillation and atypical femur fractures. A relationship between negative publicity and decline in overall AOD dispensing from 2007 onwards was also observed in a study from Australia (34) using administrative claims data from 4649 participants over 75 years old. A US investigation used pharmaceutical marketing research databases to describe trends in dispensed prescriptions and sales of BPs for osteoporosis treatment (35). In this study, a 46% increase in prescriptions for oral bisphosphonates from 2000 to 2007 was observed with a subsequent 53% decline from 2008 to 2012. It is possible that the fear of side effects of bisphosphonates (in patients and doctors) can explain the plateauing (and in women in the last three years even decrease) of the incidence of bisphosphonate prescriptions observed in our study, although these more serious side effects occur relatively rarely (36). These sentiments appear to have been embraced by physicians and patients alike, and provide a salutary lesson with regard to how the benefits and risks of these medications are portrayed to the public and primary care physicians (37). As expected we observed an increase in AOD prescription rates with age. This is clearly congruent with the age-related increase in fracture incidence in persons over 50 years of age in the UK (38). For all age groups, the incidence of AOD prescription was higher in women than in men, as is true for fracture incidence in the UK (38).
There were marked regional differences in the AOD prescription rates, which were highest in Northern Ireland in both sexes, potentially at least partly explained by this region having the greatest fracture rates in the UK (38). Similarly, the relatively high rates in both sexes in Scotland, South-West and Wales correspond well with the fracture incidence rates in these regions (38). However the regional variations in fracture incidence cannot fully explain the regional variation in prescription rates. For instance in women the fracture incidence is 34% higher in Scotland than in London whereas the difference in prescription is only 7% (38). Other factors likely to contribute to the regional variation in rates are differences in socioeconomic status across the country (39), differences in access to DXA and in education level. We observed marked variation in AOD prescription rates by ethnicity, such that the incidence in black women was half that in white and Asian women. The lower fracture risk in black women and men (38) is however probably not the only explanation for these differences. In a population of individuals in Indiana, USA, who either had sustained a fragility fracture or had been diagnosed to have osteoporosis, the odds-ratio of receiving treatment was one-third lower among black patients (40). A similar result was found in a study using data from the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2010 (41).
The differing incidence patterns for the individual AODs are consistent with licensing and external guidance and provide insights in to the effects of such events. Thus etidronate was the first BP in general use, but prescriptions markedly decreased with the introduction of alendronate and risedronate, which provided more convenient dosing, and more robust anti-fracture efficacy (42,43). A possible factor explaining the rapid rise of alendronate prescription incidence from 2000 is the introduction of a once-weekly formulation in that year. In a study also using the CPRD but in which prescriptions of daily and weekly alendronate were monitored separately, a sharp rise of the prescription of the once-weekly formulation starting in the year 2000 was observed (15). A similar trend, albeit less pronounced, was observed after the introduction of the once-weekly formulation of risedronate in 2002 (15). A further possible factor driving the increased incidence of BP prescription was the demise in Hormone Replacement Therapy prescriptions following publication of the results of the oestrogen plus progesterone arm of the Women’s Health Initiative trial in 2002 (44). In 1999 the UK Royal College of Physicians issued guidance on the assessment and treatment of osteoporosis, which may also have contributed to the rise in alendronate prescription (45). The introduction of the first generic alendronate formulation in August 2005 may explain the further increase in prescriptions between 2005 and 2008-2009, as well as a plateauing and subsequent decline in the incidence of risedronate prescriptions, both trends likely to have been consolidated by the TA160 and 161 appraisals from the National Institute of Health and Care Excellence in which generic alendronate was the first-line treatment recommendation (30,31) for both primary and secondary osteoporosis therapy.
We used a very large population-based cohort with robust capture of prescription data. Our study has several limitations however. First, since the CPRD database is a primary care database, initial AOD prescriptions by medical specialists are potentially missing. However, such prescriptions are continued in primary care, so in this case a second primary care prescription after a missed first secondary care prescription would be captured. Second, only first prescriptions were counted, therefore we have no data on the persistence of AOD and we have no information on compliance and adherence. Since adherence and persistence in AOD users is often low, this factor may result in an overestimation of AOD use in our study. Third, no information is available on the individual fracture risk and therefore we are not able to make judgments on the appropriateness of prescriptions nor can we detect a care gap in those individuals eligible for but not receiving AOD treatment. We are therefore unable to determine whether the observed decrease in incidence of AOD prescription in women is a consequence of increased under-treatment (e.g. a widening of the care gap), results from better treatment targeting or other factors. An important strength of our study is that, although CPRD only covers 7% of the UK population, the GP practices are widely distributed around the UK, and the dataset has been shown to be generally representative of the UK population (17,46).
In conclusion, yearly prescription rates of anti-osteoporosis medications increased steeply in women from 1990 to 2009, followed by a decrease, while in men a less steep increase stabilized from 2007 on. Prescription rates were substantially higher in women than in men and increased with age in women and men, with marked regional and ethnic differences. The demonstrated plateau of prescription rates in both sexes, and decrease amongst women in recent years, are concerning, and clearly illustrate the need for renewed efforts to properly present the benefits of these treatments to patients and healthcare practitioners in order to close this expanding treatment gap.
Highlights.
In UK CPRD we documented rates of anti-osteoporosis treatment by age, sex, ethnicity, geographic location and calendar time.
In women, annual rates of first prescription increased from 1990-2006 followed by a plateau and a 12% decrease 2009-2012.
In men, prescription rates increased less steeply from 1990-2007 and then levelled from 2008 onwards.
There were marked differences in anti-osteoporosis treatment rates by ethnicity and geographic location within the UK.
Acknowledgements
The work was supported by a grant from the National Osteoporosis Society. This work was further supported by grants from the Medical Research Council, British Heart Foundation, Arthritis Research UK, National Institute for Health Research (NIHR) Southampton Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust, and NIHR Musculoskeletal Biomedical Research Unit, University of Oxford.
Footnotes
Conflicts of Interest
R.Y. van der Velde, C. E. Wyers, E. Teesselink, P. P. M. M. Geusens, J. P. W van den Bergh, F. de Vries, C. Cooper, N. C. Harvey, T. P. van Staa report no conflicts of interest.
References
- 1. [Accessed the 14th of december 2015];National Osteoporosis Society. URL: http://www.nos.uk.
- 2.Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. page 82-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006 Dec;17(12):1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 4.British Orthopaedic Association. The care of patients with fragility fracture. 2007 [Google Scholar]
- 5.Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35(2):375–382. doi: 10.1016/j.bone.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 6.Sernbo I, Johnell O. Consequences of a hip fracture: a prospective study over 1 year. Osteoporos Int. 1993 May;3(3):148–153. doi: 10.1007/BF01623276. [DOI] [PubMed] [Google Scholar]
- 7.Burge RT, Worley D, Johansen A, et al. The cost of osteoporotic fractures in the UK: projections for 2000-2020. Journal of Medical Economics. 4:51–52. [Google Scholar]
- 8.Ström O, Borgström F, Kanis J, Compston J, Cooper C, McCloskey EV, Jönsson B. Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2011;6:59–155. doi: 10.1007/s11657-011-0060-1. [DOI] [PubMed] [Google Scholar]
- 9.Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M, National Osteoporosis Guideline Group (NOGG) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas. 2009 Feb 20;62(2):105–108. doi: 10.1016/j.maturitas.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 10.Vaile J, Sullivan L, Bennet C, Bleasel J. First Fracture Project: addressing the osteoporosis care gap. Intern Med J. 2007 Oct;37(10):717–720. doi: 10.1111/j.1445-5994.2007.01496.x. [DOI] [PubMed] [Google Scholar]
- 11.Nayak S, Roberts MS, Greenspan SL. Factors associated with diagnosis and treatment of osteoporosis in older adults. Osteoporos Int. 2009 Nov;20(11):1963–1976. doi: 10.1007/s00198-008-0831-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE. Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systemic review. Osteoporos Int. 2004 Oct;15(10):767–778. doi: 10.1007/s00198-004-1675-5. [DOI] [PubMed] [Google Scholar]
- 13.Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD. Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum. 2006 Apr;35(5):293–305. doi: 10.1016/j.semarthrit.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Balasubramanian A, Tosi L, Lane J, Dirschl R, Ho P-R, O’Malley C. Declining rates of osteoporosis management following fragility fractures in the U.S, 2000 through 2009. J Bone Joint Surg Am. 2014 Apr 2;96(7):e52. doi: 10.2106/JBJS.L.01781. [DOI] [PubMed] [Google Scholar]
- 15.Watson J, Wise L, Green J. Prescribing of hormone therapy for menopause, tibolone, and bisphosphonates in women in the UK between 1991 and 2005. Eur J Clin Pharmacol. 2007 Sep;63(9):843–849. doi: 10.1007/s00228-007-0320-6. [DOI] [PubMed] [Google Scholar]
- 16.Klop C, Gibson-Smith D, Elders PJ, Welsing PM, Leufkens HG, Harvey NC, Bijlsma JW, van Staa T-P, de Vries F. Anti-osteoporosis drug prescribing after hip fracture in the UK: 2000 - 2010. Osteoporos Int. 2015 Jul;26(7):1919–1928. doi: 10.1007/s00198-015-3098-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams T, van Staa T-P, Puri S, Eaton S. Recent advances in the utility and use of the General Practice Research Database as an example of a UK Primary Care Data resource. Ther Adv Drug Saf. 2012 Apr;3(2):89–99. doi: 10.1177/2042098611435911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chisholm J. The Read clinical classification. BMJ. 1990 Apr 28;300(6732):1092. doi: 10.1136/bmj.300.6732.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Staa T-P, Wegman S, de Vries F, Leufkens B, Cooper C. Use of statins and risk of fractures. Jama. 2001 Apr 11;285(14):1850–1855. doi: 10.1001/jama.285.14.1850. [DOI] [PubMed] [Google Scholar]
- 20.van Staa T-P, Abenhaim L, Cooper C, Zhang B, Leufkens HG. The use of a large pharmacoepidemiological database to study exposure to oral corticosteroids and risk of fractures: validation of study population and results. Pharmacoepidemiol Drug Saf. 2000 Sep;9(5):359–366. doi: 10.1002/1099-1557(200009/10)9:5<359::AID-PDS507>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 21.Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010 Mar;60(572):e128–136. doi: 10.3399/bjgp10X483562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herrett E, Thomas SL, Smeeth L. Validity of diagnoses in the general practice research database. Br J Gen Pract. 2011 Jul;61(588):438–439. doi: 10.3399/bjgp11X583092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol. 2010 Jan;69(1):4–14. doi: 10.1111/j.1365-2125.2009.03537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mathur R, Bhaskaran K, Chaturvedi N, Leon DA, vanStaa T, Grundy E, Smeeth L. Completeness and usability of ethnicity data in UK-based primary care and hospital databases. J Public Health (Oxf) 2014;36:684–92. doi: 10.1093/pubmed/fdt116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jaglal SB, Weller I, Mamdani M, Hawker G, Kreder H, Jaakkimainen L, Adachi JD. Population trends in BMD testing, treatment, and hip and wrist fracture rates: are the hip fracture projections wrong? J Bone Miner Res. 2005 Jun;20(6):898–905. doi: 10.1359/JBMR.041231. [DOI] [PubMed] [Google Scholar]
- 26.Huot L, Couris CM, Tainturier V, Jaglal S, Colin C, Schott AM. Trends in HRT and anti-osteoporosis medication prescribing in a European population after the WHI study. Osteoporos Int. 2008 Jul;19(7):1047–1054. doi: 10.1007/s00198-008-0587-1. [DOI] [PubMed] [Google Scholar]
- 27.Wang L, Shawn Tracy C, Moineddin R, Upshur RE. Osteoporosis prescribing trends in primary care: a population-based retrospective cohort study. Prim Health Care Res Dev. 2013 Jan;14(1):1–6. doi: 10.1017/S1463423612000114. [DOI] [PubMed] [Google Scholar]
- 28.van der Velde RY, Wyers CE, Curtis EM, Geussens PPMM, van den Bergh JPW, de Vries F, Cooper C, van Staa TP, Harvey NC. Secular trends in fracture incidence in the UK between 1990 and 2012. Osteoporos Int. doi: 10.1007/s00198-016-3650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Devold HM, Doung GM, Tverdal A, Furu K, Meyer HE, Falch JA, Sogaard AJ. Prescriptions of anti-osteoporosis drugs during 2004-2007- a nationwide register study in Norway. Eur J Clin Pharmacol. 2010 Mar;66(3):299–306. doi: 10.1007/s00228-009-0746-0. [DOI] [PubMed] [Google Scholar]
- 30.National Institute for Health and Care Excellence. TA160 Osteoporosis-primary prevention. 2008/2011 Available at: https://www.nice.org.uk/guidance/ta160.
- 31.National Institute for Health and Care Excellence. TA161 Osteoporosis-secondary prevention. 2008/2011 Available at: https://www.nice.org.uk/guidance/ta161.
- 32.Feudjo-Tepie M, Ferguson S, Roddam A, Taylor A, Bayly J, Critchlow C. Comorbidities, bone-sparing agent prescription history and their determinations among postmenopausal women in UK primary care settings: a retrospective database study. Arch Osteoporos. 2015;10:41. doi: 10.1007/s11657-015-0233-4. [DOI] [PubMed] [Google Scholar]
- 33.Jha S, Wang Z, Laucis N, Bhattacharyya T. Trends in Media Reports, Oral Bisphosphonate Prescriptions, and Hip Fractures 1996-2012: An Ecological Analysis. J Bone Miner Res. 2015 Dec;30(12):2179–2187. doi: 10.1002/jbmr.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peeters G, Tett SE, Duncan EL, Mishra GD, Dobson AJ. Osteoporosis medication dispensing for older Australian women from 2002 to 2010: influences of publications, guidelines, marketing activities and policy. Pharmacoepidemiol Drug Saf. 2014 Dec;23(12):1303–1311. doi: 10.1002/pds.3703. [DOI] [PubMed] [Google Scholar]
- 35.Wysowski DK, Greene P. Trends in osteoporosis treatment with oral and intravenous bisphosphonates in the United States, 2002-2012. Bone. 2013 Dec;57(2):423–428. doi: 10.1016/j.bone.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 36.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014 Jan;29(1):1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 37.Kanis JA, Svedbom A, Harvey N, McCloskey EV. The osteoporosis treatment gap. J Bone Miner Res. 2014 Sep;29(9):1926–8. doi: 10.1002/jbmr.2301. [DOI] [PubMed] [Google Scholar]
- 38.Curtis EM, van der Velde RY, Moon RJ, van den Bergh JPW, Geusens PPMM, de Vries F, van Staa T-P, Cooper C, Harvey NC. Epidemiology of fractures in the United Kingdom 1988-2012: variation with age, sex, geography, ethnicity and socioeconomic status. Bone. 2016 Jun;87:19–26. doi: 10.1016/j.bone.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.ONS. UK Census. 2011. [Google Scholar]
- 40.Liu Z, Weaver J, de Papp A, Li Z, Martin J, Allen K, Hui S, Imel EA. Disparities in osteoporosis treatments. Osteoporos Int. 2016 Feb;27(2):509–519. doi: 10.1007/s00198-015-3249-0. [DOI] [PubMed] [Google Scholar]
- 41.Cunningham TD, Di Pace BS, Ullal J. Osteoporosis treatment disparities: a 6-year aggregate analysis from national survey data. Osteoporos Int. 2014 Sep;25(9):2199–2208. doi: 10.1007/s00198-014-2747-9. [DOI] [PubMed] [Google Scholar]
- 42.Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 43.Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH, 3rd, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999 Oct;282(14):1344–1352. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 44.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of oestrogens plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002 Jul;288(3):321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 45.Royal College of Physicians. Osteoporosis: clinical guidelines for prevention and treatment. RCP; London: 1999. [Google Scholar]
- 46.Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T-P, Smeeth L. Data Resource Profile: Clinical Practice Research Datalink (CPRD) Int J Epidemiol. 2015 Jun;44(3):827–836. doi: 10.1093/ije/dyv098. [DOI] [PMC free article] [PubMed] [Google Scholar]