Abstract
Worry, the core component of generalized anxiety disorder, is associated with disordered eating. However, it is unclear whether worry is a precursor to disordered eating or whether worry is a consequence of disordered eating (or both). The current study tested if worry prospectively predicted disordered eating symptoms and vice-versa across six months. Young adult women (N = 300) completed a measure of worry and disordered eating at Time 1, and two months and six months later. A prospective path model utilizing structural equation modeling investigated if worry predicted disordered eating (and vice-versa). Worry prospectively predicted drive for thinness across both two and six months while controlling for previous levels of worry. In the opposite direction, drive for thinness did not predict worry over time. There were no prospective relationships between worry and bulimia or body dissatisfaction. Therefore, interventions focusing on decreasing worry could be effective in preventing and treating excessive concerns about thinness and their associated impairment.
Keywords: disordered eating, anorexia nervosa, drive for thinness, worry, anxiety, generalized anxiety disorder
1. Introduction
Anxiety disorders are highly comorbid with eating disorders (Bulik, Sullivan, Fear, & Joyce, 1997; Godart, Flament, Lecrubier, & Jeammet, 2000; Kaye et al., 2004), with anxiety disorders typically predating the onset of eating disorders (Bulik et al., 1997; Godart et al., 2000; Kaye et al., 2004; Swinbourne & Touyz, 2007). However, most of the existing research examining the relationship between anxiety disorders and eating disorders is retrospective (e.g., Bulik et al., 1997; Godart et al., 2000; Kaye et al., 2004). To our knowledge, there have been only two studies examining prospective relationships between anxiety and eating disorders (Buckner, Silgado, & Lewinsohn, 2010; Zaider, Johnson, & Cockell, 2002). However, these two prospective studies have reported conflicting findings, likely because the temporal relations between anxiety and eating disorder vary depending on which anxiety disorder and eating disorder are examined (Buckner et al., 2010). Although there is burgeoning literature examining the comorbidity between dimensions underlying eating disorders and anxiety disorders (Altman & Shankman, 2009; Halmi et al., 2005; Levinson et al., 2013; Levinson & Rodebaugh, 2012; Milos, Spindler, Ruggiero, Klaghofer, & Schnyder, 2002; Morgan, Wolfe, Metzger, & Jimerson, 2007), there is little literature addressing the comorbidity between generalized anxiety disorder (GAD) and eating disorders specifically. GAD is an anxiety disorder characterized by excessive worry (American Psychiatric Association, 2013). Prevalence research shows that GAD is highly comorbid with eating disorders, with lifetime prevalence ranging from 13–55% in bulimia nervosa (BN) and 13–49% in anorexia nervosa (AN) (Garfinkel et al., 1995; Godart et al., 2003; Kaye et al., 2004; Pallister & Waller, 2008; Schwalberg, Barlow, Alger, & Howard, 1992; Swinbourne & Touyz, 2007).
Despite high levels of comorbidity between GAD and the eating disorders, few studies have examined the temporal sequence between GAD and eating disorders, and the research that does exist has produced mixed findings and has mostly relied on patient retrospective reports (e.g., Godart et al., 2003; Schwalberg et al., 1992). Only one study has examined the prospective relationship between GAD and eating disorders, and results showed that GAD was associated with increased prevalence of BN and binge eating disorder (BED) in adolescents over time (Zaider et al., 2002). However, it is unclear if GAD symptoms prospectively predict restrictive symptoms, as no study has examined the prospective relationship between GAD or its core dimensions and underlying core dimensions of AN (e.g., drive for thinness). Prospective research is needed to clarify the temporal relation between GAD and eating disorders and to test if there are aspects of GAD that specifically predict certain dimensional aspects of disordered eating (e.g., drive for thinness, bulimia, body dissatisfaction).
Additionally, the prospective research to date has focused primarily on categorical diagnoses, rather than underlying dimensions. Clearly, there is a need to elucidate temporal sequences not only between specific anxiety disorders and specific eating disorders, but also between dimensions of anxiety (e.g., worry) and disordered eating (e.g., drive for thinness). This idea is consistent with initiatives from the Research Domain Criteria (Insel et al., 2010). One of the core cognitive symptoms of GAD is worry. Worry is conceptualized as negative thoughts or fears regarding negative events that may occur in the future (Borkovec, Ray, & Stober, 1998). Existing research suggests that individuals with an eating disorder diagnosis endorse higher levels of worry than controls and that higher levels of worry are associated with eating disorder symptoms in this population (Sassaroli et al., 2005; Startup et al., 2013; Sternheim et al., 2012). A closer read of this literature suggests that worry might be more strongly related to behaviors and cognitions characteristic of AN more so than BN. Specifically, some literature suggests that worry is more closely related to an AN diagnosis than to a BN diagnosis (Sternheim et al., 2012) and to characteristics more commonly associated with AN, such as drive for thinness, than to characteristics more commonly associated with BN, such as bulimic symptoms (Sassaroli et al., 2005).
Overall, the literature suggests that worry is associated with a diagnosis of an eating disorder and disordered eating symptoms. However, all of the studies reviewed above have been limited to cross-sectional designs. It is necessary to examine the relation between disordered eating and worry longitudinally in order to understand how the relationships between worry and disordered eating develop and maintain themselves across time. The current study tested the prospective relations between worry and disordered eating symptoms in women college students. Women college students are at high risk for developing disordered eating pathology (Delinsky & Wilson, 2008; Striegel-Moore, Silberstein, Frensch, & Rodin, 1989), with one study reporting that 12.9% of college women are at high risk for disordered eating (Reinking & Alexander, 2005). The high risk for disordered eating in college students makes them an excellent sample for the purpose of this study (e.g., they are at risk, yet still exhibit a full range of scores thus preventing restriction of range) (Pearson, 1903; Thorndike, 1949). Study hypotheses were that (a) worry would significantly prospectively predict disordered eating symptoms and (b) indicators of disordered eating would not prospectively predict worry, as anxiety disorders typically precede the development of eating disorders (Bulik et al., 1997; Godart et al., 2000; Kaye et al., 2004).
2. Materials and Methods
2.1 Participants
Undergraduate women recruited from the Washington University subject pool were invited to participate in this longitudinal study for either course credit (during Time 1) or a chance to win a gift card (during Time 2). All individuals who were female and could speak and read English were eligible for participation. Three-hundred women undergraduate students enrolled in the study. Participants’ median age was 18.00 (SD = 1.05; Range = 17 – 23). All participants gave informed consent.
2.2 Measures
The Eating Disorder Inventory-2 (EDI-2; Garner, 1991)
The EDI-2 is a 91-item self-report questionnaire that measures core features associated with AN and BN, and is considered one of the gold standard measures of eating disorder psychopathology. The EDI-2 consists of eleven subscales, three of which were utilized in this study: (1) drive for thinness, (2) bulimia, and (3) body dissatisfaction. The drive for thinness subscale reflects a desire to lose weight and a fear of weight gain, and is a core feature of AN, although also relevant to other eating disorders (Bruch, 1973; Garner, Olmsted, & Polivy, 1983). The bulimia subscale indicates a tendency towards episodes of bingeing and purging (Garner et al., 1983). The body dissatisfaction subscale reflects disturbances in body image (Garner et al., 1983). The factor structure, reliability and validity of the EDI-2 has been demonstrated in clinical and non-clinical samples (Eberenz & Gleaves, 1994; Spillane, Boerner, Anderson, & Smith, 2004; Thiel & Paul, 2006). In the current study, internal consistencies were adequate (αs = 0.76 – 0.90).
The Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990)
The PSWQ is a self-report questionnaire that measures worry. The PSWQ has been demonstrated to be valid and reliable in clinical and non-clinical samples (Meyer et al., 1990), and is considered to be a gold standard measure of worry. Eleven items were included in the current study, as research has shown that the elimination of certain PSWQ items results in higher validity, reliability, and a stronger factor structure in young adult samples (Hopko et al., 2003). In the current study, internal consistencies were excellent (αs = 0.96).
2.3 Procedures
Participants completed all the measures listed above at baseline (Time 1), two months (Time 2), and six months (Time 3). Missing data were estimated (see procedures below) allowing data from all 300 participants to be used. Participants who completed the second and third session did not differ on any measure from participants who did not. All study materials and procedures were reviewed and approved by the Institutional Review Board at Washington University in St. Louis. Data from this study have been utilized to create a measure of fear of food, but this work does not overlap with the data presented in the current study (Levinson & Byrne, 2015).
2.4 Statistical Analysis
Mplus Version 7.1 (Muthen & Muthen, 1998–2012) was used for all analyses. The MLR estimator, an Mplus option for maximum likelihood estimation with robust standard errors, was used to report standardized path estimates. MLR was used because it is robust to potential non-normal data and is able to estimate missing data efficiently (Muthen & Muthen, 1998–2012). Model fit was evaluated using the comparative fit index (CFI) (Bentler, 1990), the Tucker-Lewis incremental fit index (TLI) (Tucker & Lewis, 1973), the root mean square error of approximation (RMSEA) (Steiger & Lind, 1980), and the standardized root mean square residual (SRMR) (Jöreskog & Sörbom, 1981). For the CFI and TLI, values above or equal to .90 were considered adequate and above or equal to .95 were considered very good (Hu & Bentler, 1999). For the RMSEA and SRMR, values below or equal to .08 were considered adequate and below or equal to .05 were considered very good (Hu & Bentler, 1999).
Three prospective three-wave models with each of the disordered eating outcomes (drive for thinness, bulimia, and body dissatisfaction) and worry spanning from initial assessment (Time 1) to two months later (Time 2) to six months later (Time 3) were tested. All models were adjusted for baseline levels of the outcome variable. The paths from Time 1 to Time 2 to Time 3 were constrained to increase power and because there was no reason to believe that Time 1 to Time 2 should differ from Time 2 to Time 3. All missing data for Time 2 and Time 3 were efficiently estimated because the MLR estimator was used.
3. Results
3.1 Participant Characteristics
Three-hundred undergraduate women completed all the previously stated measures at baseline (Time 1). The majority of the participants were in their first year of college (n = 164; 57.1%); 27.9% (n = 80) second year, 8% (n = 23) third year, 6.3% (n = 18) fourth year, and 0.7% (n = 2) fifth year of college. Two months later (Time 2), participants (n = 274; 91.3%) returned for a second session, and six months later, participants (n = 190; 63.3%) completed a third session online. The majority of the participants (n = 182, 60.7%) were Caucasian; 27.3% (n = 82) Asian, 4.0% Black (n = 12), 2.7% (n = 8) Hispanic, 5.0% (n = 15) multi-racial, and 1 participant reported ethnicity as not listed. Participants’ median BMI was 21.21 (SD = 3.08; Range = 16.04 – 34.43).
3.2 Structural Equation Models
Model 1. Drive for Thinness
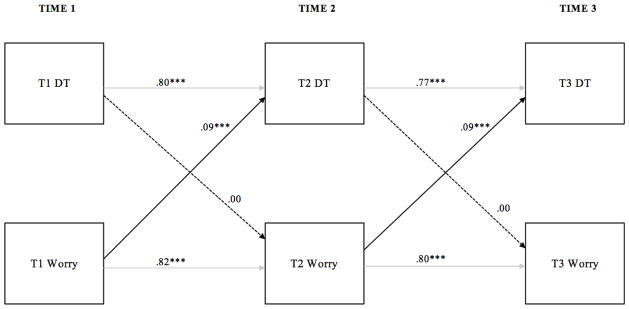
Time 1, Time 2, and Time 3 worry and drive for thinness were included in the first model. Model fit was very good (CFI = 0.99, TLI = 0.99, RMSEA = 0.05, SRMR = 0.03). As can be seen in Figure 1, worry prospectively predicted drive for thinness across all time-points, but not vice-versa.
Figure 1.
A three-wave prospective model of worry and drive for thinness. Solid lines indicate significant relationships; dashed lines indicate non-significant relationships. Autoregressive parameters are shown in gray to ease interpretation. Time 1 = initial assessment point;
Time 2 = measures collected two months after Time 1; Time 3 = measures collected six months after Time 1. DT = drive for thinness. *** p < 0.001.
Model 2. Bulimia
Time 1, Time 2 and, Time 3 worry and bulimia were included in the second model. Model fit was very good (CFI = 1.00, TLI = 1.00, RMSEA = 0.00, SRMR = 0.02). Worry did not predict bulimia prospectively (bs = 0.05, ps = 0.13 – 0.14), nor did bulimia predict worry prospectively (bs = 0.01, ps = 0.84).
Model 3. Body Dissatisfaction
Time 1, Time 2, and Time 3 worry and body dissatisfaction were included in the third model. Model fit was adequate (CFI = 0.97, TLI = 0.96, RMSEA = 0.09, SRMR = 0.04). Worry did not predict body dissatisfaction prospectively (bs = 0.00, ps = 0.95), nor did body dissatisfaction predict worry prospectively (bs = 0.00, ps = 0.99).
4. Discussion
Worry predicted drive for thinness while controlling for previous levels of drive for thinness across six months. In contrast, disordered eating did not predict future worry in this study, and worry did not prospectively predict bulimia and body dissatisfaction. These findings suggest that, over time, the relationship between worry and disordered eating may be more closely related to dimensions associated with AN than to characteristics more closely associated with BN. These findings also suggest that disordered eating does not elevate the risk for worry, rather, worry might elevate the risk for drive for thinness specifically.
Consistent with previous retrospective research (Bulik et al., 1997; Godart et al., 2000; Kaye et al., 2004), results from this prospective study suggest that worry may be a precursor to symptoms of disordered eating such as drive for thinness, rather than a consequence of disordered eating. This finding adds to the literature testing if anxiety disorders/anxiety symptoms precede eating disorders, typically follow, or appear simultaneously with eating disorders (Buckner et al., 2010; Bulik et al., 1997; Godart et al., 2003, 2000; Kaye et al., 2004). Findings from this study suggest that worry, a core cognitive component of anxiety, may lead to later concerns about thinness.
Why might worry lead to concerns about thinness? It may be that worry about other more general aspects may develop into worry specifically about being thin over time. The study sample consisted of participants who were at the beginning of a semester in college, many in their very first semester of college, which is a stressful transition period. Furthermore, this time period is typically associated with weight gain (Delinsky & Wilson, 2008), which might have enhanced worries about thinness. This heightened stress and fear of weight gain might serve as a catalyst propelling individuals, who were predisposed to worry in general, to worry specifically about thinness. In the current sample, the participant median age was 18-years old, which is a high-risk period for the development of an eating disorder (Halmi, Casper, Eckert, Goldberg, & Davis, 1979) and a time where the participants may begin to have specific worries about their weight. Of course, this theory needs to be tested further in future research.
One additional possible explanation for why general worry might lead to disordered eating is that disordered eating may serve to regulate general anxiety or worry. Various theories propose that individuals with eating disorders engage in eating disorder behaviors (e.g. restricting, exercising) to change their emotional experiences (Wildes, Ringham, & Marcus, 2010), and that engaging in eating disordered behaviors may allow individuals with AN to avoid experiencing negative emotions (Schmidt & Treasure, 2006; Wildes et al., 2010). It may be that individuals predisposed to worry in general use worries about thinness specifically as a way to avoid more general worries (or to possibly preoccupy themselves with a specific, possible controllable, worry). Taken with findings from the current study, this research suggests that worrying about thinness could possibly serve as a distraction from anxiety experienced from worries characteristic of GAD, such as family, relationships, or career. Of course this theory is tentative, and future research is needed to identify the mechanisms that lead from worry to drive for thinness across time.
The prospective relation between worry and drive for thinness is concerning because drive for thinness is associated with disordered eating patterns, psychosomatic symptoms, and psychological distress (Keski-Rahkonen et al., 2005). Furthermore drive for thinness is a core feature of AN and is also relevant to other eating disorders (Bruch, 1973; Garner et al., 1983). Findings from this study add to other research which has found that worry is associated with multiple forms of psychopathology, including post-traumatic stress disorder, depression, and paranoia, although the domains of worry may vary among these disorders (Freeman et al., 2013; Ladouceur et al., 1999; Starcevic, 1995). Additionally, findings from this study add to the hypothesis that worry is a transdiagnostic process which may contribute to various psychological disorders (Ehring & Watkins, 2008; Harvey, 2004; McEvoy, Watson, Watkins, & Nathan, 2013). It is possible that targeting worry could possibly decrease both GAD and disordered eating, as well as other comorbid disorders.
In contrast, worry did not prospectively predict bulimia and body dissatisfaction. This finding is in line with previous research that suggests that worry is more strongly correlated to behaviors and cognitions characteristic of AN more so than BN (Sassaroli et al., 2005; Sternheim et al., 2012). The lack of prospective relationship between worry and bulimia, as well as body dissatisfaction, may be because worry about general aspects develops into worry specifically about being thin over time, but does not translate into binging and purging behaviors or body image disturbance.
Several limitations of the current study should be considered. First, the time course was brief (six-months). Future research should test these hypotheses over a longer time course. Second, the sample consisted of college-aged women. Research shows that worry predicts drive for thinness in college, but future research should-determine whether these findings translate to younger adolescents, as research shows that the age of onset of AN peaks at 18 years (the average age of the study sample), as well as 14 ½ years (Halmi et al., 1979). Third, other potential correlates (e.g., neuroticism, stress) were not included. Future research should integrate multiple risk factors to create a comprehensive prospective model of eating disorder and anxiety risk. Fourth, the study relied on an unselected sample of undergraduates. Therefore, the findings are limited in their ability to inform the nature of these relationships in clinical samples. No definite conclusions about the influence of worry on AN specifically can be made, as the sample was non-clinical and drive for thinness, although a core feature of AN, is also relevant to other eating disorders.
If findings from this study are replicated, future research should investigate the mechanisms by which worry leads to drive for thinness. Future prevention research should also investigate whether decreasing general worry can prevent eating disorders. This research could lead to clinical interventions targeting worry as an adjunct treatment for eating disorders. For example, future clinical trials could examine the effectiveness of adding components targeting worry to improve current cognitive-behavioral treatments for AN. Pathological worry has been successfully targeted in individuals with GAD using cognitive-behavioral treatment (Covin, Ouimet, Seeds, & Dozois, 2008). A substantial portion of individuals who undergo cognitive-behavioral treatment for AN fail to fully recover (Pike, Walsh, Vitousek, Wilson, & Bauer, 2003), and adding a component targeting worry could potentially help improve current cognitive-behavioral treatments for AN.
4.1 Conclusion
In conclusion, we found that worry prospectively predicts drive for thinness, but that disordered eating does not predict worry over time. These findings are an important step towards understanding how anxiety and worry contribute to disordered eating across time.
Highlights.
We tested prospective associations between worry and disordered eating pathology.
Worry predicted drive for thinness across six months.
Drive for thinness did not predict worry over time.
Worry did not predict bulimia and body dissatisfaction over time.
These findings help to elucidate how worry contributes to disordered eating.
Acknowledgments
Role of Funding Sources
This research was funded by F31-MH096433 to Cheri A. Levinson. The funding source had no role in the study design, analysis, interpretation of the data, in writing the manuscript, and in the decision to submit the manuscript for publication.
We want to thank all of the research assistants in the Anxiety and Psychotherapy Laboratory who collected data for this study.
Footnotes
Contributors
Both authors wrote the manuscripts and conducted the statistical analysis.
Conflicts of Interests
The authors have no conflicts of interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Altman SE, Shankman SA. What is the association between obsessive–compulsive disorder and eating disorders? Clinical Psychology Review. 2009;29(7):638–646. doi: 10.1016/j.cpr.2009.08.001. http://doi.org/10.1016/j.cpr.2009.08.001. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) 2013. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. http://doi.org/10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Ray WJ, Stober J. Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Cognitive Therapy and Research. 1998;22(6):561–576. http://doi.org/10.1023/A:1018790003416. [Google Scholar]
- Bruch H. Eating disorders: obesity, anorexia nervosa, and the person within. Basic Books; New York: 1973. [Google Scholar]
- Buckner JD, Silgado J, Lewinsohn PM. Delineation of differential temporal relations between specific eating and anxiety disorders. Journal of Pyschiatric Research. 2010;44(12):781–787. doi: 10.1016/j.jpsychires.2010.01.014. http://doi.org/10.1016/j.jpsychires.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Fear JI, Joyce PR. Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatrica Scandinavica. 1997;96(2):101–107. doi: 10.1111/j.1600-0447.1997.tb09913.x. http://doi.org/10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- Covin R, Ouimet AJ, Seeds PM, Dozois DJ. A meta-analysis of CBT for pathological worry among clients with GAD. Journal of Anxiety Disorders. 2008;22(1):108–116. doi: 10.1016/j.janxdis.2007.01.002. http://doi.org/10.1016/j.janxdis.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Delinsky SS, Wilson GT. Weight gain, dietary restraint, and disordered eating in the freshman year of college. Eating Behaviors. 2008;9(1):82–90. doi: 10.1016/j.eatbeh.2007.06.001. http://doi.org/10.1016/j.eatbeh.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Eberenz KP, Gleaves DH. An examination of the internal consistency and factor structure of the eating disorder inventory-2 in a clinical sample. International Journal of Eating Disorders. 1994;16(4):371–379. doi: 10.1002/1098-108x(199412)16:4<371::aid-eat2260160406>3.0.co;2-w. http://doi.org/10.1002/1098-108x(199412)16:4<371::aid-eat2260160406>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Ehring T, Watkins ER. Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy. 2008;1(3):192–205. http://doi.org/10.1521/ijct.2008.1.3.192. [Google Scholar]
- Freeman D, Thompson C, Vorontsova N, Dunn G, Carter LA, … Garety P, et al. Paranoia and post-traumatic stress disorder in the months after a physical assault: a longitudinal study examining shared and differential predictors. Psychological Medicine. 2013;43(12):2673–2684. doi: 10.1017/S003329171300038X. http://doi.org/10.1017/S003329171300038X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom DS, Kennedy S, … Woodside DB. Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups. American Journal of Psychiatry. 1995;152(7):1052–1058. doi: 10.1176/ajp.152.7.1052. http://doi.org/10.1176/ajp.152.7.1052. [DOI] [PubMed] [Google Scholar]
- Garner DM. Manual for Eating Disorder Inventory. Odessa, FL: Psychological Assessment Resources, Inc; 1991. Eating Disorder Inventory-2. [Google Scholar]
- Garner DM, Olmsted MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2(2):15–34. http://doi.org/10.1002/1098-108x(198321)2:23.0.co;2-6. [Google Scholar]
- Godart NT, Flament MF, Curt F, Perdereau F, Lang F, … Venisse JL, et al. Anxiety disorders in subjects seeking treatment for eating disorders: a DSM-IV controlled study. Psychiatry Research. 2003;117(3):245–258. doi: 10.1016/s0165-1781(03)00038-6. http://doi.org/10.1016/s0165-1781(03)00038-6. [DOI] [PubMed] [Google Scholar]
- Godart NT, Flament MF, Lecrubier Y, Jeammet P. Anxiety disorders in anorexia nervosa and bulimia nervosa: co-morbidity and chronology of appearance. European Psychiatry. 2000;15(1):38–45. doi: 10.1016/s0924-9338(00)00212-1. http://doi.org/10.1016/s0924-9338(00)00212-1. [DOI] [PubMed] [Google Scholar]
- Halmi KA, Casper RC, Eckert ED, Goldberg SC, Davis JM. Unique features associated with age of onset of anorexia nervosa. Psychiatry Research. 1979;1(2):209–215. doi: 10.1016/0165-1781(79)90063-5. http://doi.org/http://dx.doi.org/10.1016/0165-1781(79)90063-5. [DOI] [PubMed] [Google Scholar]
- Halmi KA, Tozzi F, Thornton LM, Crow S, Fichter MM, Kaplan AS, … Bulik CM. The relation among perfectionism, obsessive-compulsive personality disorder and obsessive-compulsive disorder in individuals with eating disorders. International Journal of Eating Disorders. 2005;38(4):371–374. doi: 10.1002/eat.20190. http://doi.org/10.1002/eat.20190. [DOI] [PubMed] [Google Scholar]
- Harvey AG. Cognitive behavioural processes across psychological disorders: A transdiagnostic approach to research and treatment. Oxford University Press; 2004. [Google Scholar]
- Hopko DR, Reas DL, Beck JG, Stanley MA, Wetherell JL, Novy DM, Averill PM. Assessing worry in older adults: confirmatory factor analysis of the Penn State Worry Questionnaire and psychometric properties of an abbreviated model. Psychological Assessment. 2003;15(2):173–183. doi: 10.1037/1040-3590.15.2.173. http://doi.org/10.1037/1040-3590.15.2.173. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. http://doi.org/10.1080/10705519909540118. [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, … Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. http://doi.org/10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL: Analysis of linear structural relationships by the method of maximum likelihood (versión V) Chicago: National Educational Resources Inc; 1981. [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K the Price Foundation Collaborative Group. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. American Journal of Psychiatry. 2004;161(12):2215–2221. doi: 10.1176/appi.ajp.161.12.2215. http://doi.org/10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- Keski-Rahkonen A, Bulik CM, Neale BM, Rose RJ, Rissanen A, Kaprio J. Body dissatisfaction and drive for thinness in young adult twins. International Journal of Eating Disorders. 2005;37(3):188–199. doi: 10.1002/eat.20138. http://doi.org/10.1002/eat.20138. [DOI] [PubMed] [Google Scholar]
- Ladouceur R, Dugas MJ, Freeston MH, Rhéaume J, Blais F, Boisvert JM, … Thibodeau N. Specificity of generalized anxiety disorder symptoms and processes. Behavior Therapy. 1999;30(2):191–207. http://doi.org/10.1016/s0005-7894(99)80003-3. [Google Scholar]
- Levinson CA, Byrne M. The fear of food measure: A novel measure for use in exposure therapy for eating disorders. International Journal of Eating Disorders. 2015;48(3):271–283. doi: 10.1002/eat.22344. http://doi.org/10.1002/eat.22344. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL. Social anxiety and eating disorder comorbidity: The role of negative social evaluation fears. Eating Behaviors. 2012;13(1):27–35. doi: 10.1016/j.eatbeh.2011.11.006. http://dx.doi.org/10.1016/j.eatbeh.2011.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL, White EK, Menatti AR, Weeks JW, Iacovino JM, Warren CS. Social appearance anxiety, perfectionism, and fear of negative evaluation. Distinct or shared risk factors for social anxiety and eating disorders? Appetite. 2013;67:125–133. doi: 10.1016/j.appet.2013.04.002. http://dx.doi.org/10.1016/j.appet.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEvoy PM, Watson H, Watkins ER, Nathan P. The relationship between worry, rumination, and comorbidity: Evidence for repetitive negative thinking as a transdiagnostic construct. Journal of Affective Disorders. 2013;151(1):313–320. doi: 10.1016/j.jad.2013.06.014. http://doi.org/10.1016/j.jad.2013.06.014. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. http://dx.doi.org/10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Milos G, Spindler A, Ruggiero G, Klaghofer R, Schnyder U. Comorbidity of obsessive-compulsive disorders and duration of eating disorders. International Journal of Eating Disorders. 2002;31(3):284–289. doi: 10.1002/eat.10013. http://doi.org/10.1002/eat.10013. [DOI] [PubMed] [Google Scholar]
- Morgan JC, Wolfe BE, Metzger ED, Jimerson DC. Obsessive-compulsive characteristics in women who have recovered from bulimia nervosa. International Journal of Eating Disorders. 2007;40(4):381–385. doi: 10.1002/eat.20363. http://doi.org/10.1002/eat.20363. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 7. Los Angeles, CA: 1998. [Google Scholar]
- Pallister E, Waller G. Anxiety in the eating disorders: understanding the overlap. Clinical Psychology Review. 2008;28(3):366–386. doi: 10.1016/j.cpr.2007.07.001. http://doi.org/10.1016/j.cpr.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Pearson K. Mathematical contributions to the theory of evolution. XI. On the influence of natural selection on the variability and correlation of organs. Philosophical Transactions of the Royal Society of London. Series A, Containing Papers of a Mathematical or Physical Character. 1903:1–66. [Google Scholar]
- Pike KM, Walsh BT, Vitousek K, Wilson GT, Bauer J. Cognitive behavior therapy in the posthospitalization treatment of anorexia nervosa. American Journal of Psychiatry. 2003;160(11):2046–2049. doi: 10.1176/appi.ajp.160.11.2046. http://doi.org/10.1176/appi.ajp.160.11.2046. [DOI] [PubMed] [Google Scholar]
- Reinking MF, Alexander LE. Prevalence of disordered-eating behaviors in undergraduate female collegiate athletes and nonathletes. Journal of Athletic Training. 2005;40(1):47. [PMC free article] [PubMed] [Google Scholar]
- Sassaroli S, Bertelli S, Decoppi M, Crosina M, Milos G, Ruggiero GM. Worry and eating disorders: A psychopathological association. Eating Behaviors. 2005;6(4):301–307. doi: 10.1016/j.eatbeh.2005.05.001. http://doi.org/10.1016/j.eatbeh.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Schmidt U, Treasure J. Anorexia nervosa: Valued and visible. A cognitive-interpersonal maintenance model and its implications for research and practice. British Journal of Clinical Psychology. 2006;45(3):343–366. doi: 10.1348/014466505x53902. http://doi.org/10.1348/014466505x53902. [DOI] [PubMed] [Google Scholar]
- Schwalberg MD, Barlow DH, Alger SA, Howard LJ. Comparison of bulimics, obese binge eaters, social phobics, and individuals with panic disorder on comorbidity across DSM-III—R anxiety disorders. Journal of Abnormal Psychology. 1992;101(4):675–681. doi: 10.1037//0021-843x.101.4.675. http://doi.org/10.1037//0021-843x.101.4.675. [DOI] [PubMed] [Google Scholar]
- Spillane NS, Boerner LM, Anderson KG, Smith GT. Comparability of the Eating Disorder Inventory-2 between women and men. Assessment. 2004;11(1):85–93. doi: 10.1177/1073191103260623. http://doi.org/10.1177/1073191103260623. [DOI] [PubMed] [Google Scholar]
- Starcevic V. Pathological worry in major depression: A preliminary report. Behaviour Research and Therapy. 1995;33(1):55–56. doi: 10.1016/0005-7967(93)e0028-4. http://doi.org/10.1016/0005-7967(93)E0028-4. [DOI] [PubMed] [Google Scholar]
- Startup H, Lavender A, Oldershaw A, Stott R, Tchanturia K, Treasure J, Schmidt U. Worry and rumination in anorexia nervosa. Behavioural and Cognitive Psychotherapy. 2013;41(03):301–316. doi: 10.1017/S1352465812000847. http://doi.org/10.1017/s1352465812000847. [DOI] [PubMed] [Google Scholar]
- Steiger JH, Lind JC. Statistically based tests for the number of common factors. annual meeting of the Psychometric Society; Iowa City, IA. 1980. [Google Scholar]
- Sternheim L, Startup H, Saeidi S, Morgan J, Hugo P, Russell A, Schmidt U. Understanding catastrophic worry in eating disorders: process and content characteristics. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43(4):1095–1103. doi: 10.1016/j.jbtep.2012.05.006. http://doi.org/10.1016/j.jbtep.2012.05.006. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Silberstein LR, Frensch P, Rodin J. A prospective study of disordered eating among college students. International Journal of Eating Disorders. 1989;8(5):499–509. http://doi.org/10.1002/1098-108X(198909)8:5<499::AID-EAT2260080502>3.0.CO;2-A. [Google Scholar]
- Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: A review. European Eating Disorders Review. 2007;15(4):253–274. doi: 10.1002/erv.784. [DOI] [PubMed] [Google Scholar]
- Thiel A, Paul T. Test–retest reliability of the Eating Disorder Inventory 2. Journal of Psychosomatic Research. 2006;61(4):567–569. doi: 10.1016/j.jpsychores.2006.02.015. http://doi.org/10.1016/j.jpsychores.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Thorndike RL. Personnel selection; test and measurement techniques. Oxford, England: Wiley; 1949. [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. http://doi.org/10.1007/BF02291170. [Google Scholar]
- Wildes JE, Ringham RM, Marcus MD. Emotion avoidance in patients with anorexia nervosa: initial test of a functional model. The International Journal of Eating Disorders. 2010;43(5):398–404. doi: 10.1002/eat.20730. http://doi.org/10.1002/eat.20730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaider TI, Johnson JG, Cockell SJ. Psychiatric disorders associated with the onset and persistence of bulimia nervosa and binge eating disorder during adolescence. Journal of Youth and Adolescence. 2002;31(5):319–329. http://doi.org/10.1023/A:1015694623574. [Google Scholar]