Abstract
Background
In the setting of persistently high risk for maternal mortality and severe obstetric morbidity, little is known about the relationship between hospital delivery volume and maternal outcomes.
Objective
The objectives of this analysis were (i) to determine maternal risk for severe morbidity during delivery hospitalizations by hospital delivery volume in the United States; and (ii) to characterize, by hospital volume, the risk for mortality in the setting of severe obstetrical morbidity – a concept known as failure to rescue.
Study Design
This cohort study evaluated 50,433,539 delivery hospitalizations across the United States from 1998 to 2010. The main outcome measures were (i) severe morbidity defined as a composite of any one of fifteen diagnoses representative of acute organ injury and critical illness, and (ii) failure to rescue, defined as death in the setting of severe morbidity.
Results
The prevalence of severe morbidity rose from 471.2 to 751.5 cases per 100,000 deliveries from 1998 to 2010, an increase of 59.5%. Failure to rescue was highest in 1998 (1.5%), decreased to 0.6% in 2007, and rose to 0.9% in 2010. In models adjusted for comorbid risk and hospital factors, both low and high annualized delivery volume were associated with increased risk for failure to rescue and severe morbidity. However, the relative importance of hospital volume for both outcomes compared to other factors was relatively small.
Conclusions
While low and high delivery volume are associated with increased risk for both failure to rescue and severe maternal morbidity, other factors, in particular characteristics of individual centers, may be more important in determining outcomes.
Introduction
The burdens of maternal mortality and severe obstetrical morbidity and childbirth in the developed world have been increasing.1-3 Dramatic advances in perinatal care over the last three decades have not been paralleled by improvements in maternal care. National organizations, including the American Congress of Obstetricians and Gynecologists (ACOG), American Board of Obstetrics and Gynecology (ABOG), the Society for Maternal-Fetal Medicine (SMFM), Amnesty International, and the National Institute of Child Health and Human development (NICHD)4 have all recently issued policy recommendations to increase awareness of the causes of maternal mortality and to promote improved care of pregnant women.
Referral and/or transfer of complicated patients to centers with expertise, facilities, and staffing to care for mothers at high risk for mortality have been proposed as a means of reducing maternal death and severe morbidity.4 However, little is known regarding maternal care at low-volume obstetrical centers in the United States; scant data is available on comorbid risk factors, incidence of life threatening complications, and how often death occurs in the setting of severe morbidity. Outcomes at low-volume hospitals may be critically important given that as of 2008, 58% of hospitals providing obstetrical care performed less than 1000 deliveries a year, and an additional 21% performed 1000 to 2000 deliveries a year.5 In other medical specialties, higher procedural volume has been associated with improved outcomes for high-risk interventions such as lung transplantation6 and complex cancer surgery;7 however, for some lower risk procedures, volume has been associated with lesser8 or no benefit.9
Given the critical importance of determining the relationship between hospital volume and maternal outcomes, this analysis had two main objectives: (i) to determine maternal risk for severe morbidity by hospital delivery volume in the United States; and (ii) to characterize, by hospital volume, the risk for death in the setting of severe morbidity – a concept known as failure rescue.
Methods
Data from the Nationwide Inpatient Sample (NIS) from the Agency for Healthcare Research and Quality were used for this analysis. The NIS is the largest publicly available, all-payer inpatient database in the United States. The NIS dataset contains a random sample of approximately 20% of hospital discharges within the United States, and through 2011 all hospitalizations for individual centers were included. The sampling frame for the NIS includes nonfederal, general, and specialty-specific hospitals throughout the United States as well as both academic and community facilities. The NIS included approximately 8 million hospital stays from 45 states in 2010.10 Due to the de-identified nature of the data set, institutional review board exemption was obtained from Columbia University, NY to perform this analysis.
We analyzed women who were hospitalized for a delivery between 1998 and 2010. Patients were identified using ICD-9 billing codes V27 and 650. Utilization of these codes obtains greater than 95% of delivery hospitalizations.11 For each hospital, we calculated the total number of delivery hospitalizations and divided this by the number of years in which a hospital had at least one delivery. To avoid including emergency deliveries occurring in hospitals that do not otherwise provide obstetrical services, centers with annualized delivery volume of less than 50 were excluded; prior analyses evaluating obstetric volume have used this threshold.12 In addition to annualized delivery volume, hospital characteristics included location (urban versus rural), teaching status (teaching versus nonteaching), hospital bed size, hospital ownership (government, private non-profit, or private investor), and region (Eastern, Midwest, South, or West). Patient transfers from other hospitals were excluded, given that their outcome could have been dependent on care received from the transferring center. Within the NIS, sampling weights can be used to provide national estimates. These sampling weights were applied to determine rates of all risk factors and outcomes in the aggregate population, which are reported per 100,000 deliveries; similarly sampling weights were utilized in the unadjusted and adjusted analyses. As per the data use agreement for the Nationwide Database from the Healthcare Cost and Utilization Project, individual cells with ≤10 cases are not reported.
Comorbid risk factors were determined by a review of the literature.2,13-21 Medical, obstetric, and demographic conditions shown to be predictive of severe maternal morbidity were included in the analysis.16,20 Based on data from the United Kingdom comorbid risk factors such as diabetes, hypertensive diseases of pregnancy, and substance abuse have also been shown to be associated with increased risk for mortality.22,23 To summarize comorbid risk, a validated index specifically designed for use in obstetric patient populations that includes demographic and medical risk factors (such as congenital heart disease, hypertension, and diabetes) predictive of maternal death and acute organ injury was included in the adjusted models.16,20 Risk factors included in the index are assigned a weight; patients with a score of 0 have the lowest risk of severe morbidity with increasing score associated with increased risk. In the initial study used to calculate the comorbidity index risk for severe morbidity was 0.68% with a score of 0 compared to 10.9% with a score >10. For categorical analyses, patients were classified based on the following scores: 0, 1, 2, 3, 4, ≥5. The following patient demographic characteristics were additionally evaluated: maternal age, race (white, black, Hispanic), year of discharge, zip-code income, and payer status.
For outcomes, measures and diagnoses of severe morbidity were reviewed in the research literature.14-16 This analysis utilized fifteen diagnoses of acute organ injury and critical illness also analyzed in the validated obstetric comorbidity index: acute heart failure, acute liver disease, acute myocardial infarction, acute renal failure, disseminated intravascular coagulation, coma, delirium, puerperal cerebrovascular disorders, pulmonary edema, pulmonary embolism, sepsis, shock, status asthmaticus, and status epilepticus.12,16 Incidence rates of severe morbidity and failure to rescue were calculated. Failure to rescue was defined as death in the setting of one of the fifteen acute organ injury diagnoses representative of severe maternal morbidity. The concept of failure to rescue has arisen from the growing recognition that one of the most important determinants of outcomes may not be the occurrence of a complication, but how a life-threatening condition is managed.24-27 Failure-to-rescue as an outcome to evaluate how patient outcomes may differ based on institutional and provider factors. While evaluation failure-to-rescue with administrative data cannot determine causality, such analyses can demonstrate potentially clinically significant associations.
Annualized hospital delivery volume was analyzed in two ways: (i) for the unadjusted analyses volume was analyzed categorically, and (ii) for the adjusted analyses volume was analyzed continuously. For the unadjusted analyses, delivery volume was classified into one of four categories: 50 to 500 deliveries (very low volume), 501 to 1000 deliveries (low volume), 1001 to 2000 deliveries (medium volume), and >2000 (high volume). Prior analyses have used varying obstetric volume cutoffs;28,29 the volume categories used in this analysis were chosen because they represent easily interpretable and clinically meaningful distinctions in obstetric volume.
Adjusted risks for severe maternal morbidity and failure to rescue in relation to annualized delivery volume were evaluated via a generalized linear mixed effects model with a Poisson distribution and a log link function to account for hospital clustering. Restricted cubic splines are nonparametric smoothing procedures that do not necessitate restriction on the shape of distribution, and this methodology allows flexibility in presenting the non-linear relationship between continuous predictors and outcome and was used to model annualized hospital delivery volume.30,31 The appropriate numbers of knots for annualized delivery volume in the models were determined by the likelihood-ratio test.30 A five-piece restricted cubic spline with knot locations at annualized hospital volumes of 377 (5th percentile of the patient population), 1252 (28th percentile), 2170 (50th percentile), 3437 (73th percentile), and 7163 (95th percentile) was applied to the regression model for severe morbidity; another 5-piece restricted cubic spine model was developed for failure to rescue with knot locations at 432 (5th percentile of patients), 1478 (28th percentile), 2378 (50th percentile), 3600 (73th percentile), and 7433 (95th percentile). These models account for patient demographics and hospital characteristics as well as comorbid risk. The results of the individual cubic spline regressions for severe morbidity and failure to rescue are presented visually as smoothed lines with risk ratios (with 95% confidence intervals) with annualized delivery volume of 1000 as the reference.
Within the adjusted models, Akaike information criteria (AIC) were used to evaluate the relative importance of each covariate on severe maternal morbidity and failure to rescue by removing one covariate at a time from the model.6 A larger AIC indicates a greater importance for the given variable omitted from the model. The likelihood ratio test (LRT) compares the fit of a full model (including all variables) to a reduced model omitting a specified variable thereby indicating the statistical significance of the omitted variable. All analyses were performed with SAS 9.4 (SAS Institute, Cary, NC).
Results
A total of 50,433,539 deliveries were included in the analysis of which there were 284,883 cases of severe maternal morbidity and 2,795 cases of failure to rescue. Failure to rescue accounted for 78.7% of the 3,550 deaths in the cohort. 3,995,340 (7.9%) deliveries occurred at very low volume centers, 6,678,632 (13.2%) at low volume centers, 12,719,964 (25.2%) at moderate volume centers, and 27,039,603 (53.6%) at high volume centers. This cohort of patients represents a national estimate based on sampling weights from the NIS applied to an original population of 10,325,140 deliveries from 2,832 hospitals. Very low and low volume centers were more likely to be rural, nonteaching, located in the Midwest or South, and serve lower-income patients (Table 1). Most risk factors for severe morbidity and/or mortality were prevalent at a higher rate at moderate and high volume hospitals. Rates of potentially high-risk conditions such as pulmonary hypertensions, congenital heart disease, and systemic lupus were all highest at high volume hospitals. However, deliveries in the setting of many risk factors, such as previous cesarean delivery, gestational hypertension, mild or unspecified preeclampsia, and asthma, were not uncommon at very low and low volume centers (Table 2).
Table 1. Demographics and Hospital Characteristics by Annualized Delivery Volume.
| Volume category | 50-500 | 501-1000 | 1001-2000 | >2000 | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | % | n | % | n | % | n | % | |
| Number of deliveries | 3995340 | 7.9 | 6678632 | 13.2 | 12719964 | 25.2 | 27039603 | 53.6 |
| Age (years) | ||||||||
| <20 | 421012 | 10.5 | 604792 | 9.1 | 960861 | 7.6 | 1699089 | 6.3 |
| 20-24 | 1349406 | 33.8 | 1998147 | 29.9 | 3325647 | 26.1 | 6129449 | 22.7 |
| 25-29 | 1136512 | 28.4 | 1932605 | 28.9 | 3632024 | 28.6 | 7550169 | 27.9 |
| 30-34 | 715802 | 17.9 | 1391837 | 20.8 | 3015584 | 23.7 | 7142120 | 26.4 |
| ≥35 | 372609 | 9.3 | 751250 | 11.2 | 1785848 | 14.0 | 4518775 | 16.7 |
| Discharge year | ||||||||
| 1998 | 319923 | 8.0 | 542169 | 8.1 | 917855 | 7.2 | 1670289 | 6.2 |
| 1999 | 316950 | 7.9 | 492742 | 7.4 | 1001132 | 7.9 | 1777928 | 6.6 |
| 2000 | 323248 | 8.1 | 517540 | 7.7 | 985485 | 7.7 | 1989851 | 7.4 |
| 2001 | 294499 | 7.4 | 570009 | 8.5 | 954945 | 7.5 | 1926590 | 7.1 |
| 2002 | 299284 | 7.5 | 527086 | 7.9 | 946281 | 7.4 | 2139245 | 7.9 |
| 2003 | 293283 | 7.3 | 531976 | 8.0 | 919554 | 7.2 | 2101735 | 7.8 |
| 2004 | 300295 | 7.5 | 492668 | 7.4 | 968214 | 7.6 | 2234461 | 8.3 |
| 2005 | 309023 | 7.7 | 503136 | 7.5 | 1060452 | 8.3 | 2133574 | 7.9 |
| 2006 | 296637 | 7.4 | 515463 | 7.7 | 1089574 | 8.6 | 2156567 | 8.0 |
| 2007 | 315523 | 7.9 | 503902 | 7.5 | 972971 | 7.6 | 2530658 | 9.4 |
| 2008 | 297924 | 7.5 | 495864 | 7.4 | 1049418 | 8.3 | 2188405 | 8.1 |
| 2009 | 328690 | 8.2 | 560429 | 8.4 | 937987 | 7.4 | 2123926 | 7.9 |
| 2010 | 300060 | 7.5 | 425648 | 6.4 | 916097 | 7.2 | 2066375 | 7.6 |
| Household income by ZIP code | ||||||||
| Lowest quartile | 1035952 | 25.9 | 1358262 | 20.3 | 2248024 | 17.7 | 4785709 | 17.7 |
| Second quartile | 1631562 | 40.8 | 2077377 | 31.1 | 3216154 | 25.3 | 5221307 | 19.3 |
| Third quartile | 910518 | 22.8 | 1763445 | 26.4 | 3311374 | 26.0 | 6683046 | 24.7 |
| Highest quartile | 309366 | 7.7 | 1354525 | 20.3 | 3632455 | 28.6 | 9983036 | 36.9 |
| Unknown | 107942 | 2.7 | 125022 | 1.9 | 311956 | 2.5 | 366504 | 1.4 |
| Insurance status | ||||||||
| Medicare | 27417 | 0.7 | 41142 | 0.6 | 56650 | 0.4 | 118574 | 0.4 |
| Medicaid | 1887247 | 47.2 | 2851435 | 42.7 | 4896513 | 38.5 | 9604893 | 35.5 |
| Private | 1791125 | 44.8 | 3354606 | 50.2 | 6826356 | 53.7 | 15762226 | 58.3 |
| Self pay | 138544 | 3.5 | 207729 | 3.1 | 493217 | 3.9 | 902320 | 3.3 |
| Other | 128984 | 3.2 | 208964 | 3.1 | 405253 | 3.2 | 616780 | 2.3 |
| Unknown | 22023 | 0.6 | 14755 | 0.2 | 41976 | 0.3 | 34808 | 0.1 |
| Race | ||||||||
| White | 2135872 | 53.5 | 3226749 | 48.3 | 5365328 | 42.2 | 9991168 | 37.0 |
| Black | 203089 | 5.1 | 466168 | 7.0 | 1385910 | 10.9 | 2931176 | 10.8 |
| Hispanic | 290315 | 7.3 | 720112 | 10.8 | 2106320 | 16.6 | 5479109 | 20.3 |
| Other/unknown | 1366063 | 34.2 | 2265603 | 33.9 | 3862406 | 30.4 | 8638149 | 31.9 |
| Hospital size | ||||||||
| Small | 1227763 | 30.7 | 1390149 | 20.8 | 1411269 | 11.1 | 1474606 | 5.5 |
| Medium | 1352044 | 33.8 | 2268198 | 34.0 | 4342721 | 34.1 | 5463350 | 20.2 |
| Large | 1394664 | 34.9 | 2991148 | 44.8 | 6925018 | 54.4 | 20006777 | 74.0 |
| Unknown | 20869 | 0.5 | 29137 | 0.4 | 40956 | 0.3 | 94869 | 0.4 |
| Hospital Location | 0.0 | 0.0 | ||||||
| Rural | 2769004 | 69.3 | 2213178 | 33.1 | 916945 | 7.2 | 185037 | 0.7 |
| Urban | 1205467 | 30.2 | 4436316 | 66.4 | 11762062 | 92.5 | 26759697 | 99.0 |
| Unknown | 20869 | 0.5 | 29137 | 0.4 | 40956 | 0.3 | 94869 | 0.4 |
| Hospital Region | ||||||||
| Northeast | 636683 | 15.9 | 953850 | 14.3 | 2543895 | 20.0 | 4404609 | 16.3 |
| Midwest | 1319028 | 33.0 | 2137932 | 32.0 | 2903945 | 22.8 | 4570405 | 16.9 |
| South | 1326037 | 33.2 | 2488972 | 37.3 | 4452019 | 35.0 | 10302657 | 38.1 |
| West | 713592 | 17.9 | 1097879 | 16.4 | 2820106 | 22.2 | 7761931 | 28.7 |
| Hospital Teaching | ||||||||
| Non-teaching | 3771998 | 94.4 | 5459540 | 81.7 | 8235508 | 64.7 | 9140368 | 33.8 |
| Teaching | 125272 | 3.1 | 1066592 | 16.0 | 4262130 | 33.5 | 17371700 | 64.2 |
| Unknown | 98071 | 2.5 | 152500 | 2.3 | 222327 | 1.7 | 527534 | 2.0 |
| Hospital Owner | ||||||||
| Government | 880615 | 22.0 | 685789 | 10.3 | 860395 | 6.8 | 899632 | 3.3 |
| Private non-profit | 633342 | 15.9 | 1585432 | 23.7 | 2765877 | 21.7 | 5487735 | 20.3 |
| Private investor | 419902 | 10.5 | 967905 | 14.5 | 2098852 | 16.5 | 1516178 | 5.6 |
| Unknown/other | 2061481 | 51.6 | 3439506 | 51.5 | 6994840 | 55.0 | 19136058 | 70.8 |
| Comorbidity Index | ||||||||
| 0 | 552216 | 13.8 | 932905 | 14.0 | 1707980 | 13.4 | 3446830 | 12.7 |
| 1 | 158091 | 4.0 | 282035 | 4.2 | 559045 | 4.4 | 1244776 | 4.6 |
| 2 | 58185 | 1.5 | 104860 | 1.6 | 225179 | 1.8 | 536685 | 2.0 |
| 3 | 14416 | 0.4 | 27676 | 0.4 | 65046 | 0.5 | 167782 | 0.6 |
| 4 | 3772 | 0.1 | 7836 | 0.1 | 20422 | 0.2 | 56646 | 0.2 |
| ≥5 | 6126 | 0.2 | 12950 | 0.2 | 33576 | 0.3 | 100105 | 0.4 |
Discharge weights were used to produce national estimates at the population level, and weighted frequency was rounded to integers. All comparisons were significant with P <0.001, except for discharge year (P=0.54).
Table 2. Comorbid risk factors by annualized delivery volume.
| 50-500 | 501-1000 | 1001-2000 | >2000 | All patients | |
|---|---|---|---|---|---|
| Risk factors | Prevalence rate per 100,000 deliveries | ||||
|
| |||||
| Pulmonary hypertension** | 5.4 | 7.7 | 10.8 | 16.9 | 13.2 |
| Placenta previa** | 174.6 | 199.4 | 234.9 | 260.7 | 239.3 |
| Sickle cell disease/thalassemias** | 49.4 | 67.2 | 106.0 | 145.8 | 117.7 |
| Gestational hypertension | 3062.4 | 2996.8 | 2820.7 | 2889.0 | 2899.8 |
| Mild or unspecified preeclampsia** | 2609.5 | 2272.1 | 2469.2 | 2677.3 | 2565.8 |
| Severe preeclampsia or eclampsia** | 621.1 | 737.4 | 961.6 | 1318.6 | 1096.3 |
| Chronic renal disease* | 186.6 | 168.4 | 178.0 | 192.0 | 184.9 |
| Chronic hypertension** | 1094.4 | 1159.4 | 1386.1 | 1676.1 | 1488.4 |
| Chronic ischemic heart disease* | 11.3 | 6.4 | 9.2 | 13.8 | 11.4 |
| Congenital heart disease** | 40.3 | 44.1 | 58.4 | 71.8 | 62.3 |
| Systemic lupus erythematosus** | 38.0 | 51.7 | 71.5 | 109.5 | 86.6 |
| Human immunodeficiency virus** | 30.9 | 51.1 | 98.7 | 146.0 | 112.4 |
| Multiple gestation** | 932.5 | 1127.9 | 1465.8 | 1940.9 | 1633.5 |
| Drug abuse* | 244.0 | 247.7 | 278.2 | 209.0 | 234.3 |
| Alcohol abuse* | 94.2 | 99.3 | 96.8 | 102.4 | 99.9 |
| Cardiac valvular disease** | 337.1 | 505.5 | 595.4 | 742.2 | 641.7 |
| Chronic congestive heart failure* | 0.2 | 0.1 | 0.5 | 0.7 | 0.5 |
| Asthma** | 1414.9 | 1661.6 | 1963.6 | 2369.9 | 2098.0 |
| Preexisting diabetes** | 531.4 | 620.8 | 744.7 | 925.6 | 808.4 |
| Previous cesarean delivery** | 14237.2 | 14173.5 | 14517.6 | 14958.1 | 14685.9 |
Discharge weights were used to produce national estimates at the population level.
Statistically significant comparisons across volume categories are denoted by
P <0.05 and
P <0.001.
Prevalence of severe morbidity rose significantly over the course of the study period from 471.2 cases per 100,000 deliveries in 1998 to 751.5 per 100,000 in 2010, an increase of 59.5% (Table 3). Delivery at high volume hospitals was associated with higher risk for severe morbidity (618.6 per 100,000 deliveries), compared to moderate, low, and very low volume centers (incidence rates of 542.1, 443.7, 476.4 cases per 100,000 deliveries respectively). Risk was also higher for women older than 34 compared to younger women, for black women compared to other racial and ethnic groups, and in the South compared to other geographic regions. A high score on the obstetric comorbidity index was associated with increased risk for severe morbidity; for example, a score of 0 was associated with an incidence rate of 0.4% of severe morbidity whereas a score of ≥5 was associated with an incidence of 5.7% risk of severe morbidity. The prevalence rate of individual severe morbidity diagnoses stratified by hospital volume is presented in the Appendix.
Table 3. Factors associated with severe morbidity and failure to rescue.
| Severe Morbidity | Failure to Rescue | |||
|---|---|---|---|---|
|
| ||||
| Total cases (n) | 284883 | 2795 | ||
|
| ||||
| Cases | Per 100,000 deliveries | Cases | Per 100,000 cases severe morbidity | |
| Annualized delivery volume*# | ||||
| 50-500 | 19033 | 476. 4 | 117 | 617.2 |
| 501-1000 | 29633 | 443.7 | 267 | 902.5 |
| 1001-2000 | 68952 | 542.1 | 812 | 1177.1 |
| >2000 | 167265 | 618.6 | 1598 | 955.4 |
| Age*# | ||||
| <20 | 16918 | 459.0 | 124 | 730.2 |
| 20-24 | 59964 | 468.4 | 506 | 843.4 |
| 25-29 | 74110 | 520.0 | 614 | 828.9 |
| 30-34 | 74735 | 609.3 | 722 | 966.3 |
| ≥35 | 59156 | 796.3 | 828 | 1400.5 |
| Year*# | ||||
| 1998 | 16258 | 471.2 | 249 | 1534.2 |
| 1999 | 17400 | 484.8 | 252 | 1445.9 |
| 2000 | 17086 | 447.7 | 243 | 1421.6 |
| 2001 | 17469 | 466.3 | 185 | 1060.7 |
| 2002 | 19375 | 495.3 | 243 | 1254.9 |
| 2003 | 20968 | 545.1 | 218 | 1041.8 |
| 2004 | 22207 | 555.8 | 198 | 893.6 |
| 2005 | 22445 | 560.3 | 232 | 1032.1 |
| 2006 | 23015 | 567.1 | 155 | 671.4 |
| 2007 | 25555 | 591.1 | 161 | 628.6 |
| 2008 | 28071 | 696.3 | 189 | 675.0 |
| 2009 | 27167 | 687.6 | 225 | 829.4 |
| 2010 | 27868 | 751.5 | 243 | 873.4 |
| Household income*# | ||||
| Lowest quartile | 62113 | 658.8 | 647 | 1041.4 |
| Second quartile | 67755 | 557.8 | 859 | 1267.7 |
| Third quartile | 67966 | 536.5 | 622 | 915.2 |
| Highest quartile | 80337 | 525.8 | 608 | 756.9 |
| Unknown | 6713 | 736.5 | 58 | 868.6 |
| Insurance status*# | ||||
| Medicare | 2994 | 1228.1 | 51 | 1705.9 |
| Medicaid | 117111 | 608.7 | 1405 | 1199.7 |
| Private | 145154 | 523.4 | 1096 | 755.1 |
| Self pay | 10409 | 597.6 | 137 | 1318.8 |
| Other | 8501 | 625.1 | 101 | 1182.7 |
| Unknown | 714 | 629.2 | --a | 680.0 |
| Race*# | ||||
| White | 108811 | 525.2 | 769 | 707.0 |
| Black | 42329 | 848.9 | 717 | 1694.6 |
| Hispanic | 41874 | 487.1 | 510 | 1217.9 |
| Other/unknown | 91869 | 569.5 | 798 | 868.2 |
| Hospital bed size* | ||||
| Small | 26552 | 482.4 | 188 | 706.9 |
| Medium | 72886 | 542.9 | 764 | 1048.7 |
| Large | 184305 | 588.5 | 1832 | 994.0 |
| Unknown | 1141 | 614.0 | --a | 855.0 |
| Hospital Location* | ||||
| Rural | 27450 | 451.2 | 194 | 706.2 |
| Urban | 256293 | 580.3 | 2591 | 1011.0 |
| Unknown | 1141 | 614.0 | --a | 855.0 |
| Hospital Region*# | ||||
| Northeast | 51134 | 598.8 | 438 | 856.3 |
| Midwest | 56423 | 516.2 | 435 | 771.2 |
| South | 117162 | 630.9 | 1245 | 1062.6 |
| West | 60164 | 485.4 | 677 | 1124.5 |
| Hospital Teaching*# | ||||
| Non-teaching | 126091 | 473.9 | 1097 | 870.0 |
| Teaching | 154252 | 675.8 | 1610 | 1043.7 |
| Unknown | 4541 | 453.9 | 87 | 1915.6 |
| Hospital Owner* | ||||
| Government | 15900 | 478.0 | 182 | 1146.0 |
| Private non-profit | 51259 | 489.5 | 434 | 846.7 |
| Private investor | 24036 | 480.4 | 267 | 1109.5 |
| Unknown/other | 193689 | 612.3 | 1911 | 986.6 |
| Comorbidity Index*# | ||||
| 0 | 114715 | 353.9 | 783 | 682.5 |
| 1 | 57800 | 527.2 | 446 | 771.9 |
| 2 | 40022 | 883.9 | 469 | 1170.8 |
| 3 | 19219 | 1426.6 | 270 | 1406.6 |
| 4 | 10519 | 2415.9 | 161 | 1532.0 |
| >=5 | 42608 | 5692.1 | 665 | 1561.0 |
Severe morbidity cases were defined by ≥1 acute organ injury diagnosis. Failure to rescue was defined as death in the setting of any acute organ injury diagnosis. Discharge weights were used to produce national estimates at the population level, and weighted frequencies were rounded to integers.
Cell size ≤10 are not presented as per data usage agreement.
P <0.05 for severe morbidity;
P <0.05 for failure to rescue.
Failure to rescue occurred in 1.0% of women with severe morbidity cases: 2795 deaths amongst 284,883 cases of severe morbidity. The unadjusted risk for failure to rescue was lowest in very low volume hospitals (0.6%) and highest in moderate volume hospitals (1.2%). Other factors associated with increased risk for failure to rescue include maternal age ≥35 (failure to rescue rate of 1.5%), black race (1.7%), and obstetric comorbidity index score of ≥5 (1.6%). Failure to rescue was highest in 1998 at the start of the study period (1.5%) and decreased to 0.6% in 2007 before rising to 0.9% in 2010.
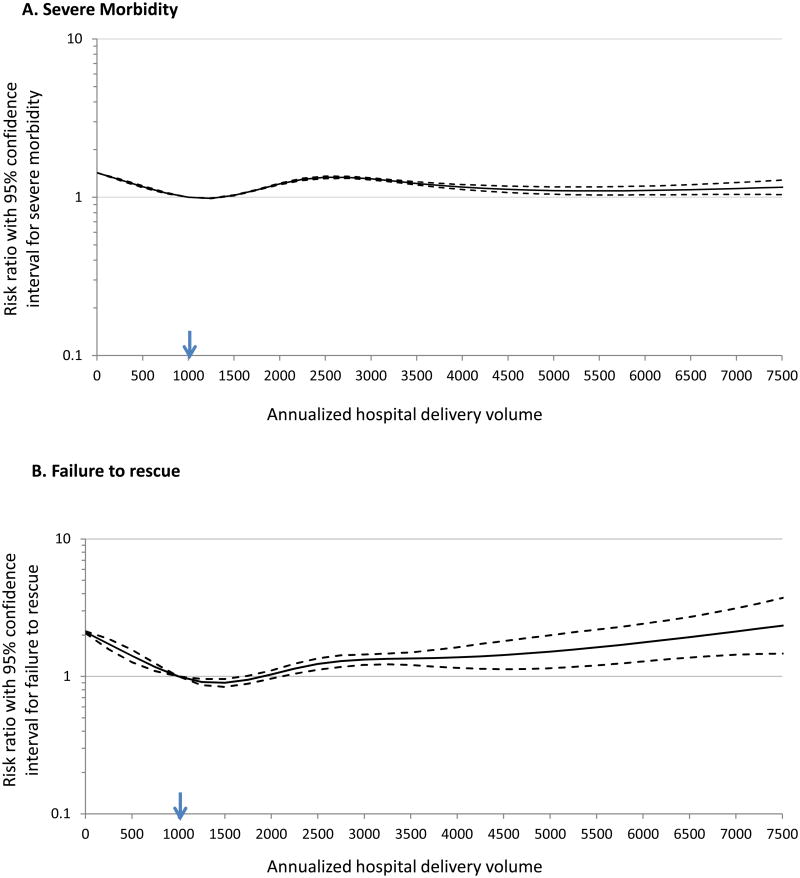
The adjusted model for severe morbidity based on hospital volume is presented in Figure 1A. With annualized delivery volume of 1000 as the reference, risk for severe morbidity was increased at delivery volume of 50 (risk ratio (RR) 1.40, 95% confidence interval (CI) 1.39-1.40). Risk then decreased to a nadir at an annualized volume of approximately 1250 (RR=0.98, 95%CI 0.98 – 0.99), and then rose again as volume increased with a peak RR at annualized volume of 2500 (RR=1.34, 95%CI 1.31-1.36) before decreasing again. Other factors associated with increased risk for severe morbidity included year of delivery, with risk generally increasing as the study period progressed, and higher score based on the obstetric comorbidity index (RR 1.56, 95% CI 1.56-1.56) (Table 4). Analysis of AIC demonstrates that the most important factors in severe morbidity risk were (i) patient-level comorbidity as measured by the comorbidity index, and (ii) hospital random effects as captured by the mixed model. The role of annualized delivery volume within the model was minor (Table 5).
Figure 1. Adjusted models for severe morbidity and failure to rescue, Legend.
Legend: The regression models for severe morbidity and maternal death used 5-piece restricted cubic splines with knot locations at 377, 1252, 2170, 3437, and 7163; while the 5-piece restricted cubic spine model for failure to rescue used knot locations at 432, 1478, 2378, 3600, and 7433. The models were adjusted for demographic factors, hospital factors, and comorbid maternal risk. Delivery volume of 1000 was used as reference (arrow). The dotted lines demonstrate the 95% confidence interval at each volume.
Table 4. Mixed effects spline regression models (risk ratio with 95% confidence interval) for severe morbidity and failure to rescue.
| Severe Morbidity Model | Failure to Rescue model | |
|---|---|---|
| Annualized delivery volume | See figure 1-a | See figure 1-b |
| Age | ||
| <20 | 0.98 (0.96-0.99) | 0.81 (0.67-0.99) |
| 20-24 | 1.00 (Referent) | |
| 25-29 | 1.14 (1.13-1.16) | 1.15 (1.02-1.29)) |
| 30-34 | 1.32 (1.30-1.33) | 1.34 (1.19-1.52) |
| ≥35 | 0.89 (0.88-0.90) | 1.75 (1.55-1.98) |
| Year | ||
| 1998 | 1.00 (Referent) | 1.00 (Referent) |
| 1999 | 1.05 (1.02-1.07) | 1.36 (1.06-1.73) |
| 2000 | 1.02 (0.99-1.05) | 1.16 (0.89-1.50) |
| 2001 | 1.06 (1.04-1.09) | 1.07 (0.82-1.40) |
| 2002 | 1.11 (1.08-1.14) | 1.09 (0.85-1.40) |
| 2003 | 1.11 (1.08-1.14) | 0.91 (0.71-1.18) |
| 2004 | 1.13 (1.10-1.16) | 0.79 (0.61-1.01) |
| 2005 | 1.11 (1.08-1.14) | 0.93 (0.72-1.20) |
| 2006 | 1.19 (1.16-1.22) | 0.58 (0.44-0.76) |
| 2007 | 1.14 (1.12-1.17) | 0.57 (0.43-0.74) |
| 2008 | 1.33 (1.29-1.36) | 0.73 (0.56-0.94) |
| 2009 | 1.32 (1.29-1.36) | 0.81 (0.63-1.05) |
| 2010 | 1.28 (1.25-1.32) | 0.81 (0.63-1.05) |
| Household income | ||
| Lowest quartile | 1.00 (Referent) | 1.00 (Referent) |
| Second quartile | 1.02 (1.01-1.03) | 1.21 (1.08-1.36) |
| Third quartile | 1.00 (0.99-1.01) | 0.93 (0.81-1.06) |
| Highest quartile | 0.96 (0.95-0.97) | 0.89 (0.77-1.04) |
| Unknown | 1.02 (0.99-1.05) | 1.08 (0.79-1.47) |
| Insurance status | ||
| Medicare | 1.62 (1.56-1.68) | 1.20 (0.83-1.72) |
| Medicaid | 1.17 (1.16-1.18) | 1.34 (1.21-1.47) |
| Private | 1.00 (Referent) | 1.00 (Referent) |
| Self pay | 1.09 (1.07-1.12) | 1.43 (1.17-1.73) |
| Other | 1.20 (1.17-1.22) | 1.48 (1.19-1.85) |
| Unknown | 1.22 (1.13-1.32) | 0.78 (0.31-1.96) |
| Race | ||
| White | 1.00 (Referent) | 1.00 (Referent) |
| Black | 1.19 (1.18-1.21) | 1.77 (1.56-2.00) |
| Hispanic | 0.90 (0.88-0.91) | 1.34 (1.17-1.54) |
| Other/unknown | 1.15 (1.13-1.16) | 1.10 (0.96-1.27) |
| Hospital bed size | ||
| Small (<400) | 1.00 (Referent) | 1.00 (Referent) |
| Medium (400-600) | 1.03 (1.00-1.07) | 1.25 (0.89-1.76) |
| Large (>600) | 1.14 (1.10-1.18) | 1.66 (1.15-2.39) |
| Hospital Location | ||
| Rural | 1.00 (Referent) | 1.00 (Referent) |
| Urban | 1.08 (1.03-1.13) | 1.11 (0.65-1.90) |
| Hospital Region | ||
| Northeast | 1.00 (Referent) | 1.00 (Referent) |
| Midwest | 0.88 (0.80-0.96) | 0.79 (0.37-1.72) |
| South | 1.23 (1.12-1.35) | 2.18 (1.03-4.58) |
| West | 1.01 (0.91-1.11) | 2.19 (1.01-4.77) |
| Hospital Teaching | ||
| Non-teaching | 1.00 (Referent) | 1.00 (Referent) |
| Teaching | 0.96 (0.92-0.99) | 0.99 (0.67-1.46) |
| Unknown | 0.90 (0.86-0.95) | 2.18 (1.40-3.39) |
| Hospital Owner | ||
| Government | 1.00 (Referent) | |
| Private non-profit | 1.03 (0.98-1.08) | 1.00 (Referent) 0.58 (0.34-0.98) |
| Private investor | 0.95 (0.89-1.01) | 0.71 (0.39-1.31) |
| Unknown/other | 1.17 (1.11-1.24) | 1.11 (0.60-2.04) |
| Comorbidity Index | 1.56 (1.56-1.56) | 1.07 (1.05-1.09) |
For severe morbidity, annualized delivery volume was modeled based on a 5-piece restricted cubic spline transformation with knot locations at 377, 1252, 2170, 3437, and 7163. For failure to rescue annualized delivery volume was modeled based on a 5-piece restricted cubic spline transformation with knot locations at 432, 1478, 2378, 3600, and 7433.
Table 5. Importance of variables in multivariable spline regression models.
| Omitted Covariates | Rank | AIC | Difference of AIC | -2(Log Likelihood) | LRT | df | P-value |
|---|---|---|---|---|---|---|---|
| Severe Morbidity Model | |||||||
| Full model | 3207536.0 | 3207442.0 | |||||
| Comorbidity Index | 1 | 3359890.7 | 152354.7 | 3359798.7 | 152356.7 | 1 | <0.0001 |
| Hospital | 2 | 3279247.0 | 71711.0 | 3279157.0 | 71715.0 | 1 | <0.0001 |
| Age | 3 | 3213189.0 | 5653.0 | 3213103.0 | 5661.0 | 4 | <0.0001 |
| Race | 4 | 3209238.9 | 1702.9 | 3209150.9 | 1708.9 | 3 | <0.0001 |
| Insurance status | 5 | 3209068.8 | 1532.8 | 3208984.8 | 1542.8 | 5 | <0.0001 |
| Year | 6 | 3208904.8 | 1368.8 | 3208834.8 | 1392.8 | 12 | <0.0001 |
| Household income | 7 | 3207615.2 | 79.2 | 3207529.2 | 87.2 | 4 | <0.0001 |
| Hospital bed size | 8 | 3207613.0 | 77.0 | 3207523.0 | 81.0 | 2 | <0.0001 |
| Hospital Region | 9 | 3207597.6 | 61.6 | 3207509.6 | 67.6 | 3 | <0.0001 |
| Hospital Ownership | 10 | 3207586.3 | 50.3 | 3207498.3 | 56.3 | 3 | <0.0001 |
| Annualized delivery volume | 11 | 3207583.9 | 47.9 | 3207497.9 | 55.9 | 4 | <0.0001 |
| Hospital Teaching | 12 | 3207551.8 | 15.8 | 3207461.8 | 19.8 | 2 | <0.0001 |
| Hospital Location | 13 | 3207542.0 | 6.0 | 3207450.0 | 8.0 | 1 | 0.005 |
|
| |||||||
| Failure to Rescue Model | |||||||
|
| |||||||
| Full model | 26401.5 | 26307.5 | |||||
| Hospital | 1 | 29990.5 | 3589.0 | 29900.5 | 3593.0 | 1 | <0.0001 |
| Age | 2 | 26512.5 | 111.0 | 26426.5 | 119.0 | 4 | <0.0001 |
| Race | 3 | 26482.8 | 81.3 | 26394.8 | 87.3 | 3 | <0.0001 |
| Year | 4 | 26474.1 | 72.6 | 26404.1 | 96.6 | 12 | <0.0001 |
| Comorbidity Index | 5 | 26459.9 | 58.4 | 26367.9 | 60.4 | 1 | 0.0002 |
| Insurance status | 6 | 26431.0 | 29.5 | 26347.0 | 39.5 | 5 | <0.0001 |
| Household income | 7 | 26420.6 | 19.1 | 26334.6 | 27.1 | 4 | <0.0001 |
| Hospital Teaching | 8 | 26412.1 | 10.6 | 26322.1 | 14.6 | 2 | 0.0007 |
| Hospital bed size | 9 | 26407.3 | 5.8 | 26317.3 | 9.8 | 2 | 0.007 |
| Annualized delivery volume | 10 | 26405.0 | 3.5 | 26319.0 | 11.5 | 4 | 0.02 |
| Hospital Region | 11 | 26404.7 | 3.2 | 26316.7 | 9.2 | 3 | 0.03 |
| Hospital Ownership | 12 | 26401.5 | 0.0 | 26313.5 | 6.0 | 3 | 0.11 |
| Hospital Location | 13 | 26399.5 | -2.0 | 26307.5 | 0.0 | 1 | 1 |
AIC, Alkaike information criterion. LRT, likelihood ratio test. The LRT compares the full model (including all variables) with a reduced model omitting 1 variable at a time. AIC was calculated as minus twice log likelihood plus 2 degrees of freedom. The higher the AIC, the greater importance of the omitted variable.
The adjusted model for failure to rescue based on hospital volume is presented in Figure 1B. As with the severe morbidity model, results are presented as smoothed lines with risk ratios and 95% confidence intervals. With annualized delivery volume of 1000 as the reference, hospital volume of 50 was associated with a doubling of the risk for failure to rescue (RR 2.02 (95%CI 1.95-2.08). Risk decreased to a nadir at an annualized volume of approximately 1500 (RR 0.90, 95%CI 0.84-0.96) and then rose, with risk significantly increased at annualized volume of 2250 (RR=1.14, 95% CI 1.05-1.24). Other factors associated with increased failure to rescue included black race (RR 1.77, 95% CI 1.56-2.00) and Medicaid insurance (RR 1.34, 95% CI 1.21-1.47). Comorbidity index was associated with a modestly increased likelihood of increased risk of failure to rescue (RR 1.07, 95% CI 1.05-1.09). Review of the AIC demonstrates that variable hospital-level effects in the mixed model were the most important factor in the failure to rescue model. The role of annualized hospital volume was relatively small (Table 5).
Discussion
In this large, nationally representative sample of delivery hospitalizations, low delivery volume was found to be associated with increased risk for both failure to rescue and severe maternal morbidity. However, the relative importance of hospital volume in both models was small. These findings suggest that other factors, in particular characteristics of individual centers, may be most important in determining outcomes. While the NIS is limited in assessing individual hospital factors, possible hospital characteristics associated with reduced risk for failure to rescue at moderate versus low and very low volume centers may include availability of consultants, the medical and nursing culture, staffing, and effective use of safety protocols to reduce risk.
A possible explanation for our findings at low volume hospitals may have to do with the specific leading causes of maternal mortality: hemorrhage, venous thromboembolism, hypertensive diseases of pregnancy, and cardiac and non-cardiac medical conditions.2,32,33 While complicated medical and cardiac patients may benefit from sub-specialty care in a tertiary medical center (and in fact patients with particularly high-risk medical conditions in this cohort were much more likely to deliver at high-volume centers), strategies to reduce risk from hemorrhage, hypertension, and venous thromboembolism are relatively straightforward and implementable and require only modest utilization of resources.34-37 For example, postpartum hemorrhage has been identified as a frequently preventable cause of maternal death.38 Timely recognition, an organized response, availability of a massive transfusion protocol, and appropriate treatment may reduce risk for death from this complication.36 Institutional readiness based on implementing strategies that anticipate and optimize management of postpartum hemorrhage may be more important in avoiding failure to rescue from hemorrhage than volume of the complication experienced within a center. Major national efforts to reduce maternal mortality such as the United Kingdom's Confidential Enquiries into Maternal Death utilize both epidemiologic surveillance data as well as comprehensive mortality case reviews in fashioning recommendations to improve outcomes.33 This analysis supports this approach, in that determination of optimal hospital-level practices may be critically important in improving care.
An unexpected finding from our analysis was that risk for failure to rescue increased as obstetrical volume increased for high volume hospitals. The causes of this finding are unclear. Specifically, it is unclear why modest changes in volume for high volume hospitals were associated with significantly increased risk compared to medium volume hospitals. It is possible that unmeasured confounding may be a factor in that we are not fully able to control for comorbid risk using administrative data; 39,40 accurate use of secondary diagnoses may be tied to reimbursement and some risk factors such as obesity that are demonstrated to be highly associated with maternal mortality in case reviews33 are poorly coded. While tools to estimate comorbidity are routinely used to account for comorbid risk in population-based studies,41 the degree to which secondary ICD-9 codes are included may be driven by reimbursement policies.42 Another possibility is a greater degree of care variation in larger centers; administrative, nursing, and provider resources may be allocated differently across high volume centers with implications for clinical care. These findings support the need for future research to determine whether adjusted risk for failure to rescue is in fact higher at high volume centers and, if so, what hospital level practices are associated with best outcomes for patients experiencing severe morbidity.
In determining adjusted risk based on hospital delivery volume, we avoided use of categorical volume variables43 and presented a regression model that did not assume a linear relationship between hospital volume and severe morbidity or failure to rescue. Indeed, we found that hospital volume demonstrated non-linear effects on the outcomes that modeling volume as a categorical variable may have masked the true effects. Furthermore, our model identified the highest risk for failure to rescue at the very lowest volume centers, suggesting that optimizing management in this setting may be an important component in improving maternal safety.
Several other findings from our study are of general public health significance. First, severe morbidity continued to rise throughout the study period. Therefore, given the increase in severe morbidity, the absolute number of deaths from failure to rescue did not decrease in proportion to the decreased rate of failure to rescue. To reduce the absolute number of failure to rescue deaths, a reduction in risk for severe morbidity in addition to improving management of complications may be required. Second, our analysis adds insight into well-documented health disparities in severe maternal morbidity and mortality.44 Not only were severe morbidity rates higher among black women, but failure-to-rescue rates were higher as well, suggesting that management of severe morbidity may play a role in mortality disparities. Third, higher comorbid risk as classified by the obstetric comorbidity index utilized in this analysis was associated with much higher risk for severe morbidity but only modestly increased the risk of failure to rescue. As demonstrated in the results, patients with a comorbidity score of ≥5 were more than 16 times as likely to develop severe morbidity than those with a score of 0 whereas risk for failure to rescue was approximately 2.3 times higher for the high comorbidity score group. In short, our findings suggest that risk for mortality with patients with high co-morbidity may be more associated with development of a complication rather than failure to rescue, relative to patients with less comorbid risk.
In interpreting this study, proper interpretation of the concept of failure to rescue in an obstetrical context is important. Differences in failure to rescue risk noted across varying hospital volumes do not necessarily signify that care was inadequate; this analysis cannot determine causally what was responsible for increased risk at high and low volume centers. A variety of factors including staffing, clinical practices, available resources, administrative factors, consultative services, and ancillary services may all be related to outcomes for specific morbidities at hospitals with varying delivery volumes. Furthermore, in studies evaluating failure to rescue in the setting of high-risk surgical procedures such as pancreatectomy and esophosagectomy,45 a relatively small set of specific complications are responsible for mortality in comparison to the diverse and heterogeneous diagnoses representing organ failure in this study.
In considering the results of this study, there are important limitations to consider. First, is the role of hospital transfers: While the NIS dataset allowed exclusion of patients transferred in from other centers, we were not able to determine outcomes of outgoing transfers. This methodological limitation may bias the study towards making outcomes at low volume hospitals, which may be more likely to transfer out critically ill patients who then die, appear better than they are. For very low volume hospitals the magnitude of increased risk for failure to rescue may be underestimated. Second, while we used mean hospital volume over the study period it is possible that year-to-year variation could have affected study outcomes. While we could have restricted our analysis to hospitals with delivery volumes within consistent ranges throughout the study period, or classified hospitals within volume categories on a year-by-year basis, we elected to use mean volumes to ensure a large a study population as possible (given the rarity of maternal death), evaluate volume continuously, and have the study design be as clearly interpretable as possible. A third limitation in our analysis is that the NIS offers a relatively limited set of variables characterizing individual hospitals. While we evaluated obstetric volume and such factors as geographic region and teaching status, it is possible that that other unmeasured structural, administrative, and staffing factors could be strongly associated with risk for failure to rescue. A fourth limitation is that administrative data is collected with the primary purpose of administration and billing and is not collected for research purposes. While analysis of administrative data can be a cost-effective and time-efficient means of evaluating research hypotheses, prospective clinical data, while costlier and more time-intensive to collect, may yield data for valid for research purposes. Of particular concern in our study is that variation in reporting of outcomes including severe morbidity diagnoses may affect the calculation of failure to rescue diagnoses. Specifically, there are no means of assessing ascertainment trends. With this limitation noted, the interpretation of rising maternal morbidity diagnoses in the NIS in the context of well defined increased comorbid risk has been interpreted by leading organizations such as the Centers for Disease Control and Prevention within the context pf other surveillance mechanisms as representing true increases in the maternal burden of severe morbidity.2-4,15,38 A fifth limitation of this analysis is that without performing chart reviews, we are unable to include certain factors in the analysis. For example, we elected not to include mode of delivery, given that the role of this variable in the pathway of the outcomes that we were assessing may vary on a case-by-case basis. Depending on the individual clinical scenario, the mode of delivery: (i) could be the result of severe morbidity, (ii) could be causal or increase risk for severe morbidity, or (iii) could be representative of severity of morbidity. Finally, for many patients with significant medical comorbidities, the probability of an optimal maternal outcome may be affected by pre-conceptional and prenatal care, factors that this analysis was also unable to evaluate.
In summary, analysis of this large, nationally representative sample of delivery hospitalizations found that while low and high delivery volumes were associated with increased maternal risk, the relative importance of hospital volume was small, and center-level effects were the most important factor associated with maternal outcomes. Risk for failure to rescue may be driven more by hospital-level factors other than the volume of deliveries performed on an annual basis.
Acknowledgments
Dr. Friedman is supported by a career development award (1K08HD082287-01A1) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health.
Appendix Table 1
National estimates for severe morbidity by annualized delivery volume categories.
| 50-500 | 501-1000 | 1001-2000 | >2000 | All patients | |
|---|---|---|---|---|---|
| Acute organ injury | Per 100,000 deliveries | ||||
|
| |||||
| Acute heart failure** | 35.1 | 34.1 | 44.7 | 51.6 | 46.3 |
| Acute liver disease | 79.8 | 78.8 | 92.3 | 91.8 | 89.3 |
| Acute myocardial infarction* | 0.9 | 1.0 | 2.0 | 2.0 | 1.8 |
| Acute renal failure** | 12.7 | 17.0 | 30.9 | 38.5 | 31.7 |
| Acute respiratory failure** | 23.9 | 34.4 | 42.8 | 53.2 | 45.8 |
| Disseminated intravascular coagulation** | 153.0 | 174.9 | 211.8 | 250.9 | 223.5 |
| Coma* | 0.4 | 0.5 | 1.1 | 1.5 | 1.2 |
| Delirium | 5.0 | 4.7 | 6.6 | 5.4 | 5.6 |
| Puerperal cerebrovascular disorders** | 20.2 | 23.5 | 31.4 | 33.7 | 30.7 |
| Pulmonary edema** | 14.9 | 17.4 | 28.1 | 52.3 | 38.7 |
| Pulmonary embolism* | 18.7 | 15.6 | 18.6 | 20.6 | 19.3 |
| Sepsis* | 124.5 | 63.4 | 68.4 | 74.4 | 75.1 |
| Shock** | 18.3 | 17.8 | 20.1 | 24.5 | 22.0 |
| Status asthmaticus** | 4.2 | 5.2 | 7.2 | 7.9 | 7.1 |
| Status epilepticus | 0.6 | 1.0 | 1.0 | 0.9 | 0.9 |
Discharge weight was used to produce national estimates at population level. Statistically significant comparisons are denoted by
P <0.05 and
P <0.001. Discharge weight was used to produce national estimates at population level.
Footnotes
Financial Disclosure: The authors did not report any potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–74. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 2.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstetrics and gynecology. 2015;125:5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 3.Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998 to 2005. Obstetrics and gynecology. 2010;116:1302–9. doi: 10.1097/AOG.0b013e3181fdfb11. [DOI] [PubMed] [Google Scholar]
- 4.D'Alton ME, Bonanno CA, Berkowitz RL, et al. Putting the “M” back in maternal-fetal medicine. American journal of obstetrics and gynecology. 2013;208:442–8. doi: 10.1016/j.ajog.2012.11.041. [DOI] [PubMed] [Google Scholar]
- 5.Simpson KR. An overview of distribution of births in United States hospitals in 2008 with implications for small volume perinatal units in rural hospitals. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN / NAACOG. 2011;40:432–9. doi: 10.1111/j.1552-6909.2011.01262.x. [DOI] [PubMed] [Google Scholar]
- 6.Thabut G, Christie JD, Kremers WK, Fournier M, Halpern SD. Survival differences following lung transplantation among US transplant centers. Jama. 2010;304:53–60. doi: 10.1001/jama.2010.885. [DOI] [PubMed] [Google Scholar]
- 7.Kramer MS, Berg C, Abenhaim H, et al. Incidence, risk factors, and temporal trends in severe postpartum hemorrhage. American journal of obstetrics and gynecology. 2013;209:449 e1–7. doi: 10.1016/j.ajog.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Schrag D, Cramer LD, Bach PB, Cohen AM, Warren JL, Begg CB. Influence of hospital procedure volume on outcomes following surgery for colon cancer. Jama. 2000;284:3028–35. doi: 10.1001/jama.284.23.3028. [DOI] [PubMed] [Google Scholar]
- 9.Simunovic M, To T, Baxter N, et al. Hospital procedure volume and teaching status do not influence treatment and outcome measures of rectal cancer surgery in a large general population. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2000;4:324–30. doi: 10.1016/s1091-255x(00)80083-9. [DOI] [PubMed] [Google Scholar]
- 10.Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstetrics and gynecology. 2013;122:233–41. doi: 10.1097/AOG.0b013e318299a6cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuklina EV, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Maternal and child health journal. 2008;12:469–77. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- 12.Snowden JM, Cheng YW, Kontgis CP, Caughey AB. The association between hospital obstetric volume and perinatal outcomes in California. American journal of obstetrics and gynecology. 2012;207:478 e1–7. doi: 10.1016/j.ajog.2012.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Panchal S, Arria AM, Harris AP. Intensive care utilization during hospital admission for delivery: prevalence, risk factors, and outcomes in a statewide population. Anesthesiology. 2000;92:1537–44. doi: 10.1097/00000542-200006000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Selo-Ojeme DO, Omosaiye M, Battacharjee P, Kadir RA. Risk factors for obstetric admissions to the intensive care unit in a tertiary hospital: a case-control study. Archives of gynecology and obstetrics. 2005;272:207–10. doi: 10.1007/s00404-004-0695-x. [DOI] [PubMed] [Google Scholar]
- 15.Callaghan WM, Mackay AP, Berg CJ. Identification of severe maternal morbidity during delivery hospitalizations, United States, 1991-2003. American journal of obstetrics and gynecology. 2008;199:133 e1–8. doi: 10.1016/j.ajog.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 16.Bateman BT, Mhyre JM, Hernandez-Diaz S, et al. Development of a comorbidity index for use in obstetric patients. Obstetrics and gynecology. 2013;122:957–65. doi: 10.1097/AOG.0b013e3182a603bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madan I, Puri I, Jain NJ, Grotegut C, Nelson D, Dandolu V. Characteristics of obstetric intensive care unit admissions in New Jersey. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2009;22:785–90. doi: 10.3109/14767050902874097. [DOI] [PubMed] [Google Scholar]
- 18.Al-Suleiman SA, Qutub HO, Rahman J, Rahman MS. Obstetric admissions to the intensive care unit: a 12-year review. Archives of gynecology and obstetrics. 2006;274:4–8. doi: 10.1007/s00404-004-0721-z. [DOI] [PubMed] [Google Scholar]
- 19.Ferreira EC, Costa ML, Cecatti JG, et al. Robson ten group classification system applied to women with severe maternal morbidity. Birth. 2015;42:38–47. doi: 10.1111/birt.12155. [DOI] [PubMed] [Google Scholar]
- 20.Metcalfe A, Lix L, Johnson JA, et al. Validation of an obstetric comorbidity index in an external population. BJOG : an international journal of obstetrics and gynaecology. 2015 doi: 10.1111/1471-0528.13254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sadler LC, Austin DM, Masson VL, et al. Review of contributory factors in maternity admissions to intensive care at a New Zealand tertiary hospital. American journal of obstetrics and gynecology. 2013;209:549 e1–7. doi: 10.1016/j.ajog.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 22.Nair M, Kurinczuk JJ, Brocklehurst P, Sellers S, Lewis G, Knight M. Factors associated with maternal death from direct pregnancy complications: a UK national case-control study. BJOG : an international journal of obstetrics and gynaecology. 2015;122:653–62. doi: 10.1111/1471-0528.13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nair M, Knight M, Kurinczuk JJ. Risk factors and newborn outcomes associated with maternal deaths in the UK from 2009 to 2013: a national case-control study. BJOG : an international journal of obstetrics and gynaecology. 2016 doi: 10.1111/1471-0528.13978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright JD, Ananth CV, Ojalvo L, et al. Failure to rescue after major gynecologic surgery. American journal of obstetrics and gynecology. 2013;209:420 e1–8. doi: 10.1016/j.ajog.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Annals of surgery. 2009;250:1029–34. doi: 10.1097/sla.0b013e3181bef697. [DOI] [PubMed] [Google Scholar]
- 26.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. The New England journal of medicine. 2009;361:1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 27.Pasquali SK, He X, Jacobs JP, Jacobs ML, O'Brien SM, Gaynor JW. Evaluation of failure to rescue as a quality metric in pediatric heart surgery: an analysis of the STS Congenital Heart Surgery Database. The Annals of thoracic surgery. 2012;94:573–9. doi: 10.1016/j.athoracsur.2012.03.065. discussion 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Snowden JM, Cheng YW, Emeis CL, Caughey AB. The impact of hospital obstetric volume on maternal outcomes in term, non-low-birthweight pregnancies. American journal of obstetrics and gynecology. 2015;212:380 e1–9. doi: 10.1016/j.ajog.2014.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Janakiraman V, Lazar J, Joynt KE, Jha AK. Hospital volume, provider volume, and complications after childbirth in U.S. hospitals. Obstetrics and gynecology. 2011;118:521–7. doi: 10.1097/AOG.0b013e31822a65e4. [DOI] [PubMed] [Google Scholar]
- 30.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 31.Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29:1037–57. doi: 10.1002/sim.3841. [DOI] [PubMed] [Google Scholar]
- 32.Cantwell R, Clutton-Brock T, Cooper G, et al. Saving Mothers' Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG : an international journal of obstetrics and gynaecology. 2011;118(Suppl 1):1–203. doi: 10.1111/j.1471-0528.2010.02847.x. [DOI] [PubMed] [Google Scholar]
- 33.Knight M, Tuffnell D, Kenyon S, Shakespeare J, Gray R, Kurinczuk JJ, editors. on behalf of MBRRACE-UK. Saving Lives, Improving Mothers' Care - Surveillance of maternal deaths in the UK 2011-13 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009-13. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2015. [Google Scholar]
- 34.Clark SL, Belfort MA, Dildy GA, Herbst MA, Meyers JA, Hankins GD. Maternal death in the 21st century: causes, prevention, and relationship to cesarean delivery. American journal of obstetrics and gynecology. 2008;199:36 e1–5. doi: 10.1016/j.ajog.2008.03.007. discussion 91-2 e7-11. [DOI] [PubMed] [Google Scholar]
- 35.Clark SL, Christmas JT, Frye DR, Meyers JA, Perlin JB. Maternal mortality in the United States: predictability and the impact of protocols on fatal postcesarean pulmonary embolism and hypertension-related intracranial hemorrhage. American journal of obstetrics and gynecology. 2014;211:32 e1–9. doi: 10.1016/j.ajog.2014.03.031. [DOI] [PubMed] [Google Scholar]
- 36.Main EK, Goffman D, Scavone BM, et al. National Partnership for Maternal Safety: Consensus Bundle on Obstetric Hemorrhage. Obstetrics and gynecology. 2015;126:155–62. doi: 10.1097/AOG.0000000000000869. [DOI] [PubMed] [Google Scholar]
- 37.Clark SL, Hankins GD. Preventing maternal death: 10 clinical diamonds. Obstetrics and gynecology. 2012;119:360–4. doi: 10.1097/AOG.0b013e3182411907. [DOI] [PubMed] [Google Scholar]
- 38.Berg CJ, Harper MA, Atkinson SM, et al. Preventability of pregnancy-related deaths: results of a state-wide review. Obstetrics and gynecology. 2005;106:1228–34. doi: 10.1097/01.AOG.0000187894.71913.e8. [DOI] [PubMed] [Google Scholar]
- 39.Deeks JJ, Dinnes J, D'Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess. 2003;7:iii–x. 1–173. doi: 10.3310/hta7270. [DOI] [PubMed] [Google Scholar]
- 40.Zhan C, Miller MR. Administrative data based patient safety research: a critical review. Qual Saf Health Care. 2003;12(Suppl 2):ii58–63. doi: 10.1136/qhc.12.suppl_2.ii58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Sarrazin MS, Rosenthal GE. Finding pure and simple truths with administrative data. Jama. 2012;307:1433–5. doi: 10.1001/jama.2012.404. [DOI] [PubMed] [Google Scholar]
- 43.Livingston EH, Cao J. Procedure volume as a predictor of surgical outcomes. Jama. 2010;304:95–7. doi: 10.1001/jama.2010.905. [DOI] [PubMed] [Google Scholar]
- 44.Creanga AA, Bateman BT, Kuklina EV, Callaghan WM. Racial and ethnic disparities in severe maternal morbidity: a multistate analysis, 2008-2010. American journal of obstetrics and gynecology. 2014;210:435 e1–8. doi: 10.1016/j.ajog.2013.11.039. [DOI] [PubMed] [Google Scholar]
- 45.Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Medical care. 2011;49:1076–81. doi: 10.1097/MLR.0b013e3182329b97. [DOI] [PubMed] [Google Scholar]