Abstract
Objective:
To assess the image quality of mammograms in females with an implanted medical device (IMD), to evaluate pain and anxiety during mammography in these females and to investigate the experience of radiographers.
Methods:
Image quality was evaluated by two radiographers and one radiologist in the images of females with an IMD participating in the Dutch screening programme (clients). Pain and anxiety were scored using a Numeric Rating Scale in both clients visiting a screening organization and patients from the Isala Hospital, Zwolle. Experience of screening radiographers was collected with a questionnaire.
Results:
Images of the breast with IMD showed reduced contrast in craniocaudal (CC) and mediolateral–oblique (MLO) views [by both the radiographers and radiologist (range: 11–29%)], less projected breast tissue [only radiographers; CC lateral side: 25.5%, 95% confidence interval (CI): 18.7–32.2] and reduced projection of the pectoral muscle (only radiographers; MLO width pectoral muscle: 31.5%, 95% CI: 24.4–38.7). Clients experienced more pain and anxiety during mammography in the breast with IMD compared to the breast without IMD in the breast (pain difference CC: 0.48 ± 0.16, p = 0.003; pain difference MLO: 0.46 ± 0.16, p = 0.004; anxiety difference 1.30 ± 0.22; p < 0.001). Patients experienced more pain (1.05 ± 0.12; p < 0.001) and anxiety (1.22 ± 0.15; p < 0.001) after placement of IMD. Radiographers are more cautious, more anxious and use less compression during mammography of breasts with IMD.
Conclusion:
Image quality in a breast with an IMD could be improved by projecting more breast tissue on the mammogram, thereby including (part of) the IMD between the paddles, if required. In addition, radiographers should pay sufficient attention to reducing discomfort both before and during the screening examination.
Advances in knowledge:
Little is known about the quality of mammography in females with an IMD or how these females and radiographers experience the screening examination. The results of our study showed that having an IMD could result in a suboptimal mammogram and increased discomfort.
INTRODUCTION
One of the requirements for a successful breast cancer screening programme is optimal quality of the mammograms. The mammogram must comply with the highest standards regarding technical image quality criteria.1,2 This also applies to females with an implanted medical device (IMD) located in the breast, such as an implantable cardioverter defibrillator (ICD), pacemaker, heart rhythm monitor or port-a-cath. The presence of an IMD may lead to lower image quality of the mammogram. In the scientific literature, little is known about mammography in females with an IMD. Roelke et al3 report that part of the mammogram was obscured in 12% of the females with a pacemaker. To our knowledge, this is the only study that has reported on the mammographic image quality in females with an IMD.
Besides the presence of the IMD, other factors also influence image quality. Compression of the breast is essential for reducing the radiation dose, preventing motion artefacts, obtaining flattened breast tissue with a homogeneous tissue thickness to improve the dynamic range of luminance and for improving visibility by spreading structures in the breast.1,4 We hypothesize that radiographers find mammographic examination in females with IMD more difficult, as it may be necessary to compress (part of) the area where the device is located. To our knowledge, no guideline or recommendation on performing a mammographic examination in females with an IMD is available for radiographers. We also hypothesize that females with an IMD find the examination more uncomfortable and frightening when compression is exerted on the breast. This may lead to less compression force in the breast with IMD, resulting in lower image quality of the mammograms.4
The purpose of this study was to assess image quality during screening mammography in the breast with IMD (hereafter: IMD + breast). We also evaluated the pain and anxiety of females with an IMD during mammography and the experience of the radiographers performing the mammograms.
METHODS AND MATERIALS
Study population
The Dutch screening programme biennially invites females aged 50–75 years and is regionally executed by five screening organizations.5 To assess image quality, we collected mammograms and data from the digital imaging and communications in medicine (DICOM) header (compression force and breast thickness) from clients with an IMD (ICD, pacemaker, heart rhythm monitor or port-a-cath) who participated in the screening programme in the period May–June 2013 (hereafter: clients). Four of the five screening organizations participated: East, North, South, South-West. The standard screening procedure was used for all participants. All mammograms were taken with Hologic Selenia® and Dimensions® (Hologic Inc., Danbury, CT). Each screening examination consisted of a mediolateral–oblique (MLO) and craniocaudal (CC) view of both breasts. The target force for all compressions was between 12 and 20 daN, but radiographers were allowed to cease compression if the females expressed severe pain. In addition, females with an IMD who were under surveillance at the Isala Hospital in Zwolle (Netherlands) and aged 50–75 years (target age group for screening) were asked to complete a questionnaire about their experience with mammography (hereafter: patients). This latter group potentially includes females who chose not to participate in the screening.
Ethical approval: Formal institutional review board approval was waived by Isala Hospital. However, according to good research practice, all clients and patients participating in this study signed written informed consent.
Client image quality assessment
Image quality of the image of the IMD+ breast compared to the IMD− breast was evaluated by two experienced radiographers by consensus (13 and 14 years' experience) and by one experienced radiologist (over 20 years' experience), based on the ‘Criteria positioning Technique mammography’ of the Dutch Reference Centre for Screening (LRCB). The radiographers scored the following criteria: nipple less in profile, reduced spread of the fibroglandular tissue, reduced projection on the image in comparison with the previous examination, reduced amount of tissue at lateral, medial or chest wall side, reduced width of the pectoral muscle, reduced depth of the pectoral muscle, inframammary angle is less displayed, more skin folds are displayed in the inframammary angle and bucky is set lower.2
In addition to the criteria described in the previous paragraph, all observers scored IMD + image for both the CC and MLO views with “yes” or “no” on the following criteria: visibility of the IMD, black area around the device, blurred image and reduced contrast. If the IMD was visible on the image, the location was indicated. For the CC view, the locations were defined as: behind the nipple, lateral, medial and at the chest wall side. For the MLO view, the locations were: entirely overlying the pectoral muscle, lateral, low axilla and behind the nipple. In addition, the radiographers scored the IMD + image as “yes” or “no” based on the criteria shown in Table 1 in comparison with the image of the breast without IMD (hereafter: IMD − breast). Finally, the entire mammogram was evaluated on the following criteria by all observers: the mammogram is assessable “completely” or “partly”; a retake is necessary “yes, an additional other view”, “yes, retake” or “no”; and mammogram image quality is “adequate” or “inadequate”. For the criterion “a retake is necessary”, a mammogram was classified as “yes, retake” when the image quality was not sufficient according to the “Criteria positioning technique mammography” of the LRCB; a mammogram was classified as “yes, an additional other view” when image quality is sufficient according to the LRCB criteria, but the radiographer decides that an additional view will provide more information. All observers used the same workstation, i.e. a Hologic Securview diagnostic workstation with 5-MP monitors (Hologic Inc., Danbury, CT).
Table 1.
Results of the image quality assessment of craniocaudal (CC) and mediolateral–oblique (MLO) views by radiographers and radiologist for the implanted medical device (IMD) + breast
| Criteria | CC view (n = 165) (radiographers) |
CC view (n = 165) (radiologist) |
MLO view (n = 165) (radiographers) |
MLO view (n = 165) (radiologist) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | |
| Blurred image | 9 | 5.5 | 2.0–9.0 | 23 | 13.9 | 8.6–19.3 | 31 | 18.8 | 12.8–24.8 | 46 | 27.9 | 21.0–34.8 |
| Reduced contrasta | 18 | 10.9 | 6.1–15.7 | 30 | 18.2 | 12.2–24.1 | 32 | 19.4 | 13.3–25.5 | 48 | 29.1 | 22.1–36.1 |
| Nipple less in profilea | 10 | 6.1 | 2.4–9.7 | 10 | 6.1 | 2.4–9.7 | ||||||
| Reduced spread of the fibroglandular tissuea | 5 | 3.0 | 0.4–5.7 | 15 | 9.1 | 4.7–13.5 | ||||||
| Reduced projection on the image in comparison with previous examinationb | 51 | 32.5 | 25.1–39.9 | 52 | 32.1 | 24.8–39.4 | ||||||
| Reduced amount of tissuea | ||||||||||||
| Lateral side | 42 | 25.5 | 18.7–32.2 | |||||||||
| Medial side | 15 | 9.1 | 4.7–13.5 | |||||||||
| Chest wall side | 25 | 15.2 | 9.6–20.7 | |||||||||
| Reduced width of the pectoral musclea | 52 | 31.5 | 24.4–38.7 | |||||||||
| Reduced depth of the pectoral musclea | 40 | 24.2 | 17.6–30.9 | |||||||||
| Inframammary angle is less displayeda | 20 | 12.1 | 7.1–17.2 | |||||||||
| More skinfolds are displayed in inframammary anglea | 34 | 20.6 | 14.4–26.8 | |||||||||
| Bucky is set lowera | 26 | 15.8 | 10.1–21.4 | |||||||||
CI, confidence interval.
In comparison with the IMD − breast.
CC view: 157 prior images available; MLO view: 162 prior images available.
In addition to the image quality evaluation, compression force and breast thickness were extracted from the DICOM header for each examination.
Experiences of clients, patients and radiographers
During the screening examination, pain was assessed using a Numerical Rating Scale (NRS) directly after each compression. The NRS is an 11-point scale from “no pain” to “severe pain” and is considered as a valid instrument for measuring pain.6 In addition, we assessed client anxiety using the NRS after the radiographer explained the mammographic examination and before visual inspection. Females were asked about anxiety for compression of both breasts separately. Furthermore, clients were asked to complete a short questionnaire about possible complaints or problems with the IMD after mammography.
The patients with IMD under surveillance at the Isala Hospital were asked to complete a retrospective questionnaire. They were asked to score pain and anxiety during mammography using an NRS before and after placement of the IMD. They were also asked whether they had any doubts about participation in the screening programme because of the IMD and whether they ever had complaints/problems with the IMD after mammography.
All radiographers (n = 440) working in the four participating screening organizations were asked to complete an online questionnaire about their experience during mammography of an IMD + breast. They scored 10 statements as “never”, “sometimes”, “most of the times” and “always” (Table 2).
Table 2.
Results of the statements scored by the radiographers (n = 161)
| Statements | Never % (n) | Sometimes % (n) | Often % (n) | Always % (n) | p-value |
|---|---|---|---|---|---|
| I experience mammography in females with medical device the same as in females without medical device | 30.4 (49) | 37.9 (61) | 29.1 (47) | 2.5 (4) | <0.001 |
| During mammography, I am more cautious with females with medical device than females without medical device | 0.0 (0) | 14.9 (24) | 16.1 (26) | 68.9 (111) | <0.001 |
| It is more frightening to compress a breast with medical device than a breast without medical device | 17.4 (28) | 42.9 (69) | 22.4 (36) | 17.4 (28) | <0.001 |
| I use less compression during mammography of a breast with medical device than without medical device | 1.2 (2) | 30.4 (49) | 35.4 (57) | 32.9 (53) | <0.001 |
| I am afraid to damage the medical device during mammography | 32.9 (53) | 42.9 (69) | 17.4 (28) | 6.8 (11) | <0.001 |
| I change the positioning technique in females with medical device in comparison with females without medical device | 6.2 (10) | 59.0 (95) | 26.1 (42) | 8.7 (14) | <0.001 |
| During mammography in females with medical device, I am more tolerant in assessing the positioning technique than in females without medical device | 8.1 (13) | 49.1 (79) | 34.2 (55) | 8.7 (14) | <0.001 |
| The quality of the mammogram is not always optimal because of the presence of the medical device. If this is the case, I make an additional image | 11.2 (18) | 64.0 (103) | 21.7 (35) | 3.1 (5) | <0.001 |
Statistical analysis
Descriptive statistics (percentages) were used to assess the image quality for the IMD + breast and to describe radiographer experience. A one-sample t-test was used to calculate the 95% confidence interval (CI) for the image quality criteria. Location subanalysis was performed using a χ2 test. The mean difference of compression force and breast thickness between IMD + breast and IMD − breast was compared using a paired t-test. Pain and anxiety scores were compared using the Wilcoxon signed-ranks test. Results are shown as means with standard error of the mean. All analyses were performed using SPSS® v. 20 (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL). The significance level was set at p < 0.05.
RESULTS
In total, 176 clients with a medical device visited one of the screening organizations during the 7-week inclusion period. 9 clients did not give informed consent and were excluded, resulting in 167 clients participating in the study. Furthermore, the questionnaire was completed by 362 of the 588 patients at the Isala Hospital, a response rate of 61.6%. Of these 362 patients, 44 patients did not sign informed consent, resulting in 318 patients being included in this study. The mean ages of the client and patient group was 64.2 ± 0.5 years and 66.1 ± 0.3 years, respectively. In the client group, 51.5% of patients had a pacemaker, 23.4% of patients had an ICD, 13.2% of patients had a reveal, 6.6% of patients had a port-a-cath and 5.4% of patients had other types of IMDs. In the patient group, 35.8% of patients had a pacemaker, 48.7% of patients had an ICD, 10.4% of patients had a reveal and 3.1% of patients had other types of IMDs. Finally, 161 (37%) of 440 radiographers completed the questionnaire about their experience with mammography in females with an IMD.
Client image quality assessment
Results of the image quality assessment of the mammograms are presented in Table 1 (CC and MLO views). Mammograms of 165 clients were evaluated by the observers. Prior images were available for 157 CC views and for 162 MLO views. The assessment of the image quality of the CC view by radiographers showed reduced contrast in 10.9% of IMD + breasts (95% CI: 6.1–15.7), less projection in comparison with a previous image in 30.9% (95% CI: 23.8–38.0) and less projection of the lateral (25.5%; 95% CI: 18.7–32.2), medial (9.1%; 95% CI: 4.7–13.5) and chest wall side (15.2%; 95% CI: 9.6–20.7). The radiologist scored 13.9% (95% CI: 8.6–19.3) of the IMD + CC views as blurred and 18.2% (95% CI: 12.2–24.1) of the IMD + CC views as reduced contrast. The highest scores in the radiographer assessment of the IMD + MLO views were a reduced width of the pectoral muscle (31.5%; 95% CI: 24.4–38.7), a reduced depth of the pectoral muscle (24.2%; 95% CI: 17.6–30.9) and more skinfolds at the inframammary angle (20.6%; 95% CI: 14.4–26.8). In addition, the radiologist scored 27.9% (95% CI: 21.0–34.8) of the IMD + MLO views as blurred and 29.1% (95% CI: 22.1–36.1) IMD + MLO views as reduced contrast.
Location subanalysis
In total, 40 (24.2%) IMDs were visible in the CC view and 128 (77.6%) IMDs in the MLO view. If a device was visible, there was a black area around the device in 90% of the images. When the IMD was visible in the CC view, a higher proportion of the images was blurred (radiographers: 12.5 vs 3.2%, p = 0.024; radiologist: 30.0 vs 8.8%, p = 0.001) and the contrast was reduced (radiographers: 42.5 vs 0.8%, p ≤ 0.001; radiologist: 50.0 vs 8.0%, p ≤ 0.001) compared with the images where the medical device (MD) was not visible. In the MLO view, more images scored better on the following criteria evaluated by the radiographers when the MD was visible than when the MD was not visible: reduced width and depth of the pectoral muscle (width 23.1 vs 59.5%, p ≤ 0.001; depth 19.5 vs 40.5%; p = 0.009), and the bucky was set lower (10.9 vs 32.4%; p = 0.002).
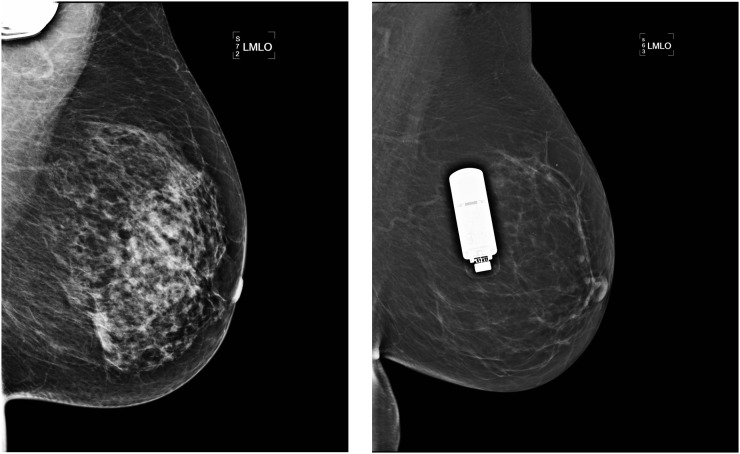
In the CC view, most IMDs were imaged at the medial side (52.5%) and chest wall side (37.5%). In the MLO view, most IMDs were imaged entirely in the pectoralis (31.3%) and lateral (55.5%). As can be seen in Figure 1, the contrast was reduced when the device was imaged in the centre of the mammogram; however, it was less affected when the device was imaged in the corner of the mammogram or entirely in the pectoralis. The radiographers scored a blurred image in 5% of the images when the IMD was entirely in the pectoralis compared with 27.3% when the IMD was not/partly in the pectoralis (p = 0.004); contrast was reduced in 2.5% of images when the IMD was entirely in the pectoralis compared with 33.0% of images when the IMD was not/partly in the pectoralis (p ≤ 0.001). The radiologist scored a blurred image in 15.0% of images when the IMD was entirely in the pectoralis compared with 37.5% of images when the IMD was not/partly in the pectoralis (p = 0.010).
Figure 1.
Left: a good-quality mediolateral–oblique (MLO) view with the implanted medical device (IMD) in the corner of the mammogram; right: decreased contrast in the MLO view owing to interference by the IMD in the centre of the mammogram.
Assessing the mammogram
The mammogram scored “partly assessable” in 64.1% of the images by the radiographers and in 55.7% of the images by the radiologist. This shows that in more than half of the mammograms, a part of the image was not assessable because either the IMD obscured a part of the image or image quality was not good enough. The radiographers scored the positioning technique insufficient in 31.7% of the images and indicated that a retake was necessary in 35.3% of the images. The radiologist required a retake in only 3.0% of the images.
Compression force and breast thickness
The results of the compression force and breast thickness are shown in Table 3. For the CC view, the compression force was 3.4 ± 0.3 daN lower in the IMD + breast than that in the IMD − breast (8.6 ± 0.3; 12.0 ± 0.2, respectively; p < 0.001). For the MLO view, the compression force was 4.2 ± 0.3 daN lower in the IMD + breast than that in the IMD − breast (8.9 ± 0.3; 13.0 ± 0.3, respectively; p < 0.001). In some cases (CC n = 19; MLO n = 14), the compression force was even <4.5 daN, showing a decaNewton of 0.0 in the DICOM header. This low compression force could result in an inadequate image quality because of incorrect image processing.
Table 3.
Results of compression force, breast thickness and pain and anxiety with implanted medical device (IMD) vs without IMD
| Clients | n | IMD (mean ± SEM) | Without IMD (mean ± SEM) | Difference IMD vs without IMD (mean ± SEM) | p-value |
|---|---|---|---|---|---|
| Compression force (daN) | |||||
| CC view | 163 | 8.6 ± 0.3 | 12.0 ± 0.2 | 3.4 ± 0.3 | <0.001 |
| MLO view | 163 | 8.9 ± 0.3 | 13.0 ± 0.3 | 4.2 ± 0.3 | <0.001 |
| Breast thickness (mm) | |||||
| CC view | 163 | 59.8 ± 1.0 | 58.1 ± 0.9 | 1.8 ± 0.4 | <0.001 |
| MLO view | 163 | 65.2 ± 1.1 | 60.0 ± 0.9 | 5.3 ± 0.5 | <0.001 |
| Pain experience in clients (NRS scale) | |||||
| CC view | 153 | 3.05 ± 0.22 | 2.57 ± 0.19 | 0.48 ± 0.16 | 0.003 |
| MLO view | 151 | 3.38 ± 0.21 | 2.92 ± 0.20 | 0.46 ± 0.16 | 0.004 |
| Anxiety in clients (NRS scale) | 156 | 2.48 ± 0.23 | 1.18 ± 0.14 | 1.30 ± 0.22 | <0.001 |
| Patients | n | After placement (mean ± SEM) | Before placement (mean ± SEM) | Difference after vs before placement (mean ± SEM) | p-value |
|---|---|---|---|---|---|
| Pain in patients (NRS scale) | 202 | 5.40 ± 0.19 | 4.35 ± 0.18 | 1.05 ± 0.12 | <0.001 |
| Anxiety in patients (NRS scale) | 206 | 3.40 ± 0.23 | 2.18 ± 0.18 | 1.22 ± 0.15 | <0.001 |
CC, craniocaudal; MLO, mediolateral–oblique; NRS, Numeric Rating Scale; SEM, standard error of the mean.
For the CC view, breast thickness was increased by 1.8 ± 0.4 mm in the IMD + breast compared with the IMD − breast (59.8 ± 1.0; 58.1 ± 0.9, respectively; p < 0.001). For the MLO view, breast thickness was increased by 5.3 ± 0.5 mm in the IMD + breast compared with the IMD − breast (65.2 ± 1.1; 60.0 ± 0.9, respectively; p < 0.001).
Client pain and anxiety
Table 3 shows that a total of 153 clients scored pain experience for both breasts for the CC view and 151 clients for the MLO view. For the CC view, 31.4% clients scored a higher and 14.4% clients a lower pain score during compression of the IMD + breast. The mean pain score for the CC view of the IMD + breast was 3.05 ± 0.22 and for the IMD − breast, it was 2.57 ± 0.19, resulting in a pain difference of 0.48 ± 0.16 (p = 0.003). For the MLO view, 33.1% of clients scored a higher and 19.2% of clients a lower pain score during compression of the IMD + breast. The mean pain score for the IMD + breast was 3.38 ± 0.21 and for the IMD − breast, it was 2.92 ± 0.20, resulting in a pain difference of 0.46 ± 0.16 (p = 0.004).
In total, 156 clients scored anxiety for both breasts. Of these, 34.0% of clients experienced more anxiety and 2.6% of clients experienced less anxiety during mammography of the IMD + breast. The mean anxiety score with IMD was 2.48 ± 0.23 and without IMD, it was 1.18 ± 0.14, resulting in a difference of 1.30 ± 0.22 (p < 0.001).
Six clients visited the cardiologist because of complaints following mammography; one client visited because she still had pain after 2 months, one client was very anxious and one client visited because the lead had come loose (it is unknown whether this was due to the mammography). The other three clients gave no reason for their visit.
Patient pain and anxiety
In total, 202 patients scored pain retrospectively during the screening examination before and after placement of IMD. Of these, 42.2% patients scored a higher and 5.4% patients a lower pain score after placement. The mean pain score after placement was 5.40 ± 0.19 and before placement, it was 4.35 ± 0.18, leading to a difference of 1.05 ± 0.12 (p < 0.001).
Of the 206 patients who scored anxiety before and after placement of IMD, 35.4% patients scored a higher and 1.5% patients a lower anxiety score after placement. The mean anxiety score after placement was 3.40 ± 0.23 and before placement, it was 2.18 ± 0.18, resulting in a difference of 1.22 ± 0.15 (p < 0.001).
Of the patients, 21.1% patients answered the question whether they had doubts about participating in the screening programme affirmatively. The main reasons mentioned included fear of damage to the device, more tension before screening and lack of knowledge to make a decision about participation. 2 (0.6%) patients visited the cardiologist or pacemaker technician because the lead had come loose and 1 (0.3%) patient visited because the device was moved following mammography. Whether these cases are related to mammography is not clear.
Experience of radiographers
Table 2 shows that most radiographers experience screening of females with IMD differently to those without IMD. They are more cautious (68.9% always), more anxious (38.8% often or always) and use less compression (68.3% often or always). In addition, 59.0% of the radiographers sometimes change the positioning technique; 26.1% radiographers do this often and 8.7% radiographers always. If the quality of the mammogram is not optimal because of the IMD, 11.2% of the radiographers do not take an additional image.
DISCUSSION
The results of this first study on the quality of mammography screening in females with an IMD showed that image quality (i.e. positioning technique) is compromised and that both females and radiographers are influenced by the presence of the IMD. The IMD + images are often blurred, have reduced contrast and reduced projected breast tissue. This can partly be explained by the presence of the IMD, but also by the lower applied compression force. Radiographers are more cautious and anxious during compression of an IMD + breast, presumably driven by the increased pain and anxiety in females with IMD or their own concerns about damaging the device.
The results showed reduced projected breast tissue on the MLO view if the IMD was not visible on the image compared with when the device was visible; in many cases, radiographers tried to avoid compression of the device, thereby omitting the device from the image. On balance, the overall positioning technique could have been improved by imaging as much of the breast tissue as possible, thereby including the IMD. Image quality is improved when the device is located completely in the pectoralis or in the upper corner of the IMD + image compared with the images where the IMD is located elsewhere. Assessment of the mammogram is more difficult when the device is located in the middle of the breast because of interference between the device and image acquisition. Because of the absence of follow-up information about cancer detection, it was not possible to estimate the influence of the reduced projected breast tissue on breast cancer detection. However, the retroglandular area represents a clinically relevant part of the breast for the detection of cancer and we believe that including this part on the mammogram leads to improved breast cancer detection.7,8
A lower compression force may lead to increased breast thickness and decreased image quality.4 The thickness differences between the IMD + breasts and IMD − breasts were small. It is possible that increases in thickness in the IMD + breast, resulting from reduced compression force, may have been offset by non-inclusion of the pectoral muscle. On the other hand, a higher compression force increases discomfort.9 In our study, females experienced more pain and were more anxious during mammography of the IMD + breast. It should be noted that general pain scores in our study were low and the difference in pain scores between breasts was small, although statistically significant. This may have been a result of reduced compression force being used on the IMD+ breast, offsetting any increase in pain caused by the presence of the IMD. Previous personal experience, anxiety and insufficient attention given by the radiographer are related to the pain experienced during mammography.10–12 High pain scores may even lead to the decision to stop participating in the programme.13 Therefore, it is important for radiographers to explain the procedure well and reassure females before and during mammography.14,15
Of the patients, 20% patients had doubts about participating in the screening programme because of the IMD. Some females also contacted their cardiologist to ask whether it was possible to perform mammography with an IMD. This indicates that it is important to provide females with an IMD sufficient information about participation in the screening programme. Based on the low number of problems noted in this study, we do not believe that mammography presents a high risk of damaging the IMD and it is not clear whether the problems noted were related to mammography. In the literature, we found one case report that describes damage to a pacemaker after performing mammography.16 Another study about long-term follow-up of submammary pacemakers and ICDs in females reported that most females in their study had no problem with mammography after their implant.17
To learn more about the maximum pressure allowed during mammography in females with an IMD to avoid damaging the IMD, we contacted the Netherlands Heart Rhythm Association (NHRA) (committee of the Netherlands Society of Cardiology) and several medical device manufacturers. The responses of the NHRA and IMD manufacturers to our question about the maximum pressure allowed were not straightforward. The LRCB advises compressing the IMD + breast very carefully, if possible with a minimum of 5 daN because of possibly incorrect image processing under 5 daN. Following the advice of the NHRA, we recommend that females with a subcutaneous ICD not participate in the screening programme.
A limitation of this study is that the pain and anxiety scores of the patients were collected retrospectively, while the scores of the clients were collected prospectively. It is possible that anxiety was heightened for the IMD + breast by explanation of the study. Owing to the time interval between the actual mammography examination and the pain and anxiety assessment, recall bias can influence the validity of these results in patients.18 However, both pain and anxiety scores (and the difference between the breasts) in patients point in the same direction as the client scores. The advantage of including the patient group was that we also received feedback from females who did not participate in the screening programme. Another limitation of the study was the response rate on the questionnaire of the radiographers (37%). However, we used this questionnaire only as a first inventory to receive input from radiographers.
In the results, we noted some differences in the evaluation of image quality between the radiographers and radiologist, e.g. the number of required retakes. The radiographers were more focused on the optimal positioning technique, while the radiologist was more focused on whether the images were sufficient for diagnostic evaluation.
In summary, interference by the IMD, a lower applied compression force and suboptimal positioning technique all lead to reduced image quality in mammography. Females with IMD are more anxious and find mammography more painful. Radiographers are more careful during compression of the IMD + breast. To help radiographers improve the image quality and reduce discomfort in females with IMD, LRCB developed a set of best practice recommendations for a mammographic examination in females with IMD (available from: www.lrcb.nl). In addition, radiographers should pay sufficient attention to reducing discomfort both before and during the screening.
Acknowledgments
ACKNOWLEDGMENTS
Firstly, the authors wish to thank the females who participated in the study. Furthermore, the authors wish to thank Irene de Lange, Caro Sluijter, Jacqueline Visser, Peter Paul Delnoy and Esther Meindersma for their contribution to this study. In addition, the authors thank the Isala Zwolle and the screening organizations (Foundation of Population Screening East, Foundation of Population Screening North, Foundation of Population Screening South and Foundation of Population Screening South-West) for their co-operation and for providing the data.
Contributor Information
Ellen Paap, Email: e.paap@lrcb.nl.
Marloes Witjes, Email: marloes.witjes@radboudumc.nl.
Cary van Landsveld-Verhoeven, Email: c.vanlandsveld-verhoeven@lrcb.nl.
Ruud M Pijnappel, Email: r.pijnappel@lrcb.nl.
Angela H E M Maas, Email: angela.maas@radboudumc.nl.
Mireille J M Broeders, Email: mireille.broeders@radboudumc.nl.
REFERENCES
- 1.Perry N, Broeders M, de Wolf C, Tornberg S, Holland R, von Karsa L. European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition—summary document. Ann Oncol 2008; 19: 614–22. doi: 10.1093/annonc/mdm481 [DOI] [PubMed] [Google Scholar]
- 2.Van Landsveld-Verhoeven C. The right focus: manual on mammography positioning technique. Nijmegen, Netherlands: Landelijk Referentiecentrum voor Bevolkingsonderzoek (LRCB), National Expert and Training Centre for Breast Cancer Screening; 2013. [Google Scholar]
- 3.Roelke M, Rubinstein VJ, Kamath S, Krauser D, Ngarmukos T, Parsonnet V. Pacemaker interference with screening mammography. Pacing Clin Electrophysiol 1999; 22: 1106–7. doi: 10.1111/j.1540-8159.1999.tb00581.x [DOI] [PubMed] [Google Scholar]
- 4.Poulos A, McLean D, Rickard M, Heard R. Breast compression in mammography: how much is enough? Australas Radiol 2003; 47: 121–6. doi: 10.1046/j.0004-8461.2003.01139.x [DOI] [PubMed] [Google Scholar]
- 5.National Evaluation Team for Breast cancer screening (NETB). National evaluation of breast cancer screening in the Netherlands 1990–2011/2012. Rotterdam, Netherlands: Department of Public Health: Erasmus MC, University Medical Center Rotterdam; 2014. [Google Scholar]
- 6.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs 2005; 14: 798–804. doi: 10.1111/j.1365-2702.2005.01121.x [DOI] [PubMed] [Google Scholar]
- 7.Brown M, Eccles C, Wallis MG. Geographical distribution of breast cancers on the mammogram: an interval cancer database. Br J Radiol 2001; 74: 317–22. doi: 10.1259/bjr.74.880.740317 [DOI] [PubMed] [Google Scholar]
- 8.Tabar L, Dean PB. Tabar's forbidden zones. Teaching atlas of mammography. 2nd edn. New York, NY: Thieme Inc.; 1985. pp. 5–14. [Google Scholar]
- 9.de Groot JE, Branderhorst W, Grimbergen CA, den Heeten GJ, Broeders MJ. Towards personalized compression in mammography: a comparison study between pressure- and force-standardization. Eur J Radiol 2015; 84: 384–91. doi: 10.1016/j.ejrad.2014.12.005 [DOI] [PubMed] [Google Scholar]
- 10.de Groot JE, Broeders MJ, Grimbergen CA, den Heeten GJ. Pain-preventing strategies in mammography: an observational study of simultaneously recorded pain and breast mechanics throughout the entire breast compression cycle. BMC Womens Health 2015; 15: 26. doi: 10.1186/s12905-015-0185-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keefe FJ, Hauck ER, Egert J, Rimer B, Kornguth P. Mammography pain and discomfort: a cognitive-behavioral perspective. Pain 1994; 56: 247–60. doi: 10.1016/0304-3959(94)90163-5 [DOI] [PubMed] [Google Scholar]
- 12.Keemers-Gels ME, Groenendijk RP, van den Heuvel JH, Boetes C, Peer PG, Wobbes TH. Pain experienced by women attending breast cancer screening. Breast Cancer Res Treat 2000; 60: 235–40. doi: 10.1023/A:1006457520996 [DOI] [PubMed] [Google Scholar]
- 13.Whelehan P, Evans A, Wells M, Macgillivray S. The effect of mammography pain on repeat participation in breast cancer screening: a systematic review. Breast 2013; 22: 389–94. doi: 10.1016/j.breast.2013.03.003 [DOI] [PubMed] [Google Scholar]
- 14.Bakker DA, Lightfoot NE, Steggles S, Jackson C. The experience and satisfaction of women attending breast cancer screening. Oncol Nurs Forum 1998; 25: 115–21. [PubMed] [Google Scholar]
- 15.Miller D, Livingstone V, Herbison P. Interventions for relieving the pain and discomfort of screening mammography. Cochrane Database Syst Rev 2008; 1: CD002942. doi: 10.1002/14651858.CD002942.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherman MM. Damage to pacemaker lead during mammography. N Engl J Med 2005; 353: 1865. doi: 10.1056/NEJM200510273531725 [DOI] [PubMed] [Google Scholar]
- 17.Giudici MC, Carlson JI, Krupa RK, Meierbachtol CJ, Vanwhy KJ. Submammary pacemakers and ICDs in women: long-term follow-up and patient satisfaction. Pacing Clin Electrophysiol 2010; 33: 1373–5. doi: 10.1111/j.1540-8159.2010.02871.x [DOI] [PubMed] [Google Scholar]
- 18.Rothman K. Epidemiology: an introduction. 2nd edn. Oxford, UK: Oxford University Press; 2012. [Google Scholar]