Abstract
Objective:
This study aimed to assess the effect of sensory stimulation on patient MRI experience and to assess whether sensory stimulation has a significant effect on MR image quality.
Methods:
A case-control study was conducted over 4 months, involving patients undergoing MRI brain, cervical spine, breast and prostate. The study involved 106 patients, 64 cases and 42 controls. Cases underwent sensory stimulation during the scan in the form of a scented cotton pad placed in the scanner near their head and/or calming bird noises were played over headphones. Post-scan, participants completed a questionnaire regarding their experience of MRI. Scanning radiographers completed a questionnaire regarding patient tolerance of the scan. All studies were evaluated by two radiologists for the presence of movement artefact.
Results:
39% of cases and 38% of controls reported anxiety in the days preceding MRI. 6.2% of cases required coaching during image acquisition, while 9.7% of controls required coaching. 4.7% of cases and 4.8% controls required sequence repetition owing to movement artefact. Mean patient experience score (as graded by the patient) for controls was 1.74 ± 0.63 standard deviation (SD) and for cases, it was 1.67 ± 0.60 SD. (Lower assigned scores equated to a better experience). Mean patient experience score based on comments on a 5-point scale as graded by two observers was 2.81 ± 0.70 SD for controls, 2.42 + 0.94 SD for sound intervention and 2.46 ± 1.01 SD for scent intervention. Mean motion artefact score graded by the two radiologists was 1.13 ± 0.53 SD for controls and 1.08 ± 0.36 SD for cases. (A lower score equated to less movement artefact). We demonstrated a trend towards a relaxing experience in those patients undergoing MRI for the first time who underwent sensory intervention. Participant positive ratings of the smell pleasantness were associated with a reduced likelihood of experiencing anxiety (p = 0.13). Results were not statistically significant.
Conclusion:
This study demonstrated a subjectively improved experience of MRI for some patients with the intervention of sound and smell. The study failed to show a significant decrease in patient movement during MRI investigations. This may relate to the small study size and a low level of patient movement in the case group.
Advances in knowledge:
Sound and olfactory sensory environment interventions at MRI can improve the patient experience. These low-cost interventions are well tolerated, may improve acceptance of MRI in patients with anxiety and offer a competitive advantage to imaging centres.
INTRODUCTION
Patient anxiety at the time of MRI can lead to an unfavourable patient experience and decreased scan quality owing to movement artefact or the early cessation of imagine acquisition at patient request. Anxiety at the time of MRI can manifest as a feeling of apprehension, panic or claustrophobia. Between 1 and 15% of all patients scheduled for MRI suffer from claustrophobia and cannot be imaged or require sedation to complete the scan.1,2 Anxiety at MRI has been shown to effect females more than males, may predate the day of MRI and can be influenced by prior personal imaging experience or the anecdotal experiences of others.3–5 Diagnostic centres invest considerable capital expenditure on acquiring up-to-date technology. However, even the most up-to-date scanners remain subject to motion artefacts. An unfavourable MR experience may lead to the requirement for sedation at the time of future MRI, or even in patient refusal to undergo MRI at a future date.1,3 It is important, therefore, to employ all measures that can lead to a positive patient experience and optimize image quality.
It has been shown that effective communication before and during the scan can effectively reduce patient anxiety.6 Other techniques are employed with varying effects, including patient education, drug therapy and cognitive–behavioural intervention.7
Some manufacturers have introduced effective environmental measures at the time of scanning, such as noise reduction technology.2 Other environmental interventions have included the use of ambient lighting or backlit nature images/photographs in the scan room or waiting areas which aim to reduce patient anxiety and improve acceptance of MRI. If beneficial, these environmental measures could give a competitive advantage to centres employing these techniques. However, to date, there are little data available on the effects of these environmental interventions.
This study looks at the effect of introducing two environmental factors, a specific pre-recorded sound series (or soundscape) and a scent intervention consisting of application of a specific essential oil to a surface close to the patient in the MRI scanner. We analyzed the potential benefits of these sensory design interventions, including improved patient experience; increased scan quality as assessed by patient motion-induced image artefacts; and lower rates of subdiagnostic studies. A single type of sound and scent intervention was chosen by a collaborating industry partner Condiment Junkie Limited, London, UK. This company has extensive experience working with the advertising industry, particularly in using sound interventions to evoke a psychological response. The interventions used are simple to activate and are felt to be more portable and less costly than most other environmental interventions used elsewhere.
The aim of this study was to demonstrate whether the use of a sensory design in the context of routine MRI scans can deliver an improvement in overall patient experience and an improvement in scan quality.
METHODS AND MATERIALS
Participants
This is a multicentre prospective case-control study of patient experience and image quality as a result of an environmental intervention.
Ethics committee approval was secured (institutional ethics approval number: 1/378/1670). The study involved 106 patients overall, 64 cases and 42 controls, recruited over a 4-month period (February–May 2015). Imaging studies were performed at two MRI centres n = 93 (Centre 1) and n = 13 (Centre 2), respectively (Table 1).
Table 1.
Patient characteristics
| Study Points | Casea | Control | Total |
|---|---|---|---|
| Sex | |||
| Male | 20 | 13 | 33 |
| Female | 44 | 29 | 73 |
| Age (years) | 23–92, median 49 | 24–89, median 50 | |
64 cases in total, 13 of these cases received sound intervention alone, 51 cases received both sound and scent intervention.
In the case group, there were 44 females and 20 males, ranging in age from 23 to 92 years, with median age of 49 years. In the control group, there were 29 females and 13 males, ranging in age from 24 to 89 years, with median age of 50 years.
The study population included both inpatients and outpatients capable of giving consent and undergoing MRI of the brain, breast, prostate or cervical spine. Exclusion criteria included patients requiring sedation (as determined prior to the scan), patients incapable of informed consent, patients who were pregnant, those under 18 years of age and those with a history of hypersensitivity to essential oils. Exclusion criteria also included emergency imaging referrals, i.e. those presenting acutely unwell and requiring urgent imaging. These patients were excluded as any anxiety they felt regarding MRI may have been exacerbated by their clinical status.
Protocol
Patients falling within the study criterion were approached by an MRI specialist radiographer prior to imaging.
An information leaflet explaining the study was given to each patient. If patients were willing to participate, they signed a consent form at the time of the standard safety questionnaire prior to MRI.
All patients from Centre 1 were randomly assigned to one of two groups (case or control) by the flip of a coin. All patients from Centre 2 were assigned to the case group. Group 1 underwent sensory stimulation (case) while Group 2 did not (control). All patients selected for intervention in imaging Centre 1 received both the sound and scent intervention contemporaneously. All patients in Centre 2 received the sound intervention only.
For those case patients receiving sound intervention, a relaxing soundscape was played at the time of MRI. The soundscape was delivered via the existing sound system using non-metallic earphones. The sound consisted of natural sounds designed to evoke open spaces; in this study, a “Birdsong” was used. The same soundscape was used for all patients.
For those case patients also undergoing scent intervention, they were exposed to a pure natural lavender scent. The scent was delivered via a pad imbued with the scent oil and then placed near the patient head. The oil used was a European Community quality standard-approved essential oil at 100% concentration in order to mitigate any possible contamination. The same scent was used for all patients.
Following the scan, all patients completed a questionnaire examining their subjective experience of the scan. Case patients also completed questions regarding their subjective experience of the sensory intervention. The questionnaire for all patients required a numerical scale grading their experience. All patients were asked to comment on their overall experience and the cases were also asked to comment on their experience of the sensory intervention. If they had received both sound and scent intervention, they were asked to comment on each one separately (Table 2). Patients individually graded their experience of the MRI study in terms of anxiety based on a 4-point numeric scale (1 = relaxing, 2 = equivocal, 3 = tolerable anxiety and 4 = intolerable). Patient experience was further graded based on comments on the questionnaire and was scored on a 5-point scale by two observers, with differences resolved by consensus. Case patient comments were graded separately for the sound intervention, scent intervention and overall experience. Grading scale was as follows: 1 = very positive experience, 2 = positive experience, 3 = equivocal experience or no comment, 4 = negative experience and 5 = very negative experience.
Table 2.
Questions for patients
| Have you ever undergone an MRI scan before? |
| Were you anxious about the scan over the preceding days/weeks? If so, what were you anxious about? |
| Were you able to remain in the scanner to completion of the scan? |
| Do you think you moved during the scan? |
| What was your overall experience of the scan: (Numerical scale) 1 = relaxing, 2 = equivocal, 3 = caused tolerable anxiety and 4 = intolerable |
| Did you experience any adverse effects as a result of the scented oil, such as allergy or nasal irritation? |
| Please provide an overall comment relating to the scan, the sound intervention and the scent intervention |
The radiographer completed a separate questionnaire examining patient behaviour, the need for sequence repetition due to patient movement and the need for coaching during the scan (Table 3). Coaching was defined as an active interaction between the MRI radiographer and the patient during image acquisition in order to allay patient anxiety.
Table 3.
Questions for radiographers
| Did the patient have sensory stimulation during image acquisition? If so, was it sound and smell intervention or sound alone? |
| What was the length of image acquisition in minutes? |
| Did a sequence have to be repeated owing to poor image quality secondary to movement? |
| Did the patient require coaching during image acquisition owing to anxiety/movement? |
| Was there a delay in image acquisition owing to patient anxiety? |
Images were analyzed for the presence of movement artefact by two radiologists (ES and MOC). Motion artefact at MRI is typically greatest in slower sequences such as T2 or fluid-attenuated inversion-recovery sequences.8 Therefore, in order to evaluate for movement artefact, axial T2 imaging was chosen to standardize assessment, as this sequence was performed as part of all of the MRI studies used in the study. Motion artefact was graded on a 4-point scale: 1 = no motion, 2 = minimal motion, 3 = moderate motion interfering with image interpretation and 4 = severe motion limiting image interpretation. Each reviewer graded the scans as to whether it was of diagnostic quality or not (yes/no) and whether scan sequences would need to be repeated or not (yes/no). All differences were resolved by consensus.
Data analysis
Mean values with standard deviations were calculated for the patient-graded experience score and also for the scores calculated based on patient comments.
Subgroup analysis of controls vs patients undergoing both sound and scent interventions at the same time was performed. This included analysis of the effect of the interventions on patients who had not previously undergone MRI examination. Comparisons were also made between case and control groups matched for the type of MRI procedure performed for those patients undergoing MRI brain and breast MRI (N = 54 and N = 42, respectively), as the number of patients undergoing prostate and cervical spine MRI was considered too low to be of significance (N = 8 and N = 2, respectively). Comparison of patient experience grading on the 4-point scale was also matched for gender.
In order to investigate the role of sounds and smells during the MRI scan relative to independent variables, a binomial logistic regression was conducted. The dependent variables were whether the participants moved during the scan and whether they experienced claustrophobia or anxiety. The independent variables included as predictors in the regression model were: age, sex, acquisition time, whether a patient had had an MRI before, the rating of smell and sound (as per the comment section on the questionnaire) and whether a patient found the smells and sounds relaxing. This analysis was performed on participants who had both sound and scent interventions at the same time. Again, those who underwent sound intervention alone (n = 13) were not analyzed.
RESULTS
Types of MRI performed in the case and control groups are listed in Table 4. In the case group, 51 patients had a sound and scent intervention at the same time. 13 patients had a sound intervention only and all 13 of these patients underwent MRI brain. No patient reported an adverse reaction to the sound or scent intervention.
Table 4.
MRI study type
| Study | Case | Control | Total |
|---|---|---|---|
| MRI brain | 37 | 17 | 54 |
| MRI cervical spine | 0 | 2 | 2 |
| MRI prostate | 5 | 3 | 8 |
| MRI breast | 22 | 20 | 42 |
| Mean acquisition time (min) | 27.5 | 30.5 |
Mean image acquisition time was 30.5 min for patients in the control group and 27.5 min for patients in the case group.
No patient required sedation during the scan in either the case or control groups. All patients in the control group completed the full series of planned MRI sequences. 1 (1.5%) patient in the case group undergoing brain MRI in Centre 2 with sound intervention only was unable to complete the full series of sequences. However, the sequences obtained were regarded as being sufficient to answer the clinical question for which the scan was requested.
22 (55%) patients in the control group and 40 (62.5%) patients in the case group had had an MRI before.
16 (38%) patients in the control group and 25 (39%) patients in the case group reported anxiety about the scan in the days preceding MRI.
2 (4.8%) patients in the control group and 3 (4.7%) patients in the case group needed to have a sequence repeated owing to movement.
4 (9.5%) patients in the control group and 4 (6.2%) patients in the case group required coaching during image acquisition.
Mean patient experience score (as graded by the patient) in the control group was 1.74 ± 0.63 standard deviation (SD) and in the case group, it was 1.67 ± 0.60 SD. As in Table 2, scores were graded 1–4, from relaxing (score = 1) to intolerable (score = 4).
Mean patient experience score based on comments on a 5-point scale as graded by two observers was 2.81 ± 0.70 SD in the control group, 2.42 + 0.94 SD for sound intervention and 2.46 ± 1.01 SD for scent intervention.
Mean motion artefact score graded by the two radiologists was 1.13 ± 0.53 SD in the control group and 1.08 ± 0.36 SD in the case group (values indicated from 1 = no motion to 4 = severe motion). Review by the same two radiologists graded scans as diagnostic quality in all control studies and in 63 out of 64 cases. (1 of the 64 study patients undergoing breast MRI was not graded, as diagnostic quality based on image degradation secondary to marked background enhancement was unrelated to patient movement or anxiety.) No patient required repeat imaging (Table 5).
Table 5.
Results
| Study Points | Case (n = 64) | Control (n = 41) |
|---|---|---|
| Prior MRI | 40 (62.5%) | 22 (53%) |
| Anxiety preceding MRI | 25 (39%) | 16 (39%) |
| Required sequence repeated | 3 (4.7%) | 2 (4.8%) |
| Required coaching | 4 (6.2%) | 4 (9.7%) |
| Patient experiencea (subjective) | Mean: 1.67 ± 0.60 SD, median: 2 | Mean: 1.74 ± 0.63 SD, median: 3 |
| Patient experienceb (objective) | Mean: 2.42 ± 0.94 SD, median: 4 (sound intervention) Mean: 2.46 ± 1.01 SD, median: 4 (scent intervention) |
Mean: 2.81 ± 0.70 SD, median: 3 |
| Motion artefactc | 1.08 ± 0.36 SD | 1.13 ± 0.53 SD |
SD, standard deviation.
Patients individually graded their experience of the MRI study in terms of anxiety or claustrophobia based on a 4-point numeric scale (1 = relaxing, 2 = equivocal, 3 = tolerable anxiety and 4 = intolerable).
Patient experience was further graded based on comments on the patient questionnaire and was scored on a 5-point scale by two observers. Grading scale was: 1 = very positive experience, 2 = positive experience, 3 = normal experience or no comment, 4 = negative experience and 5 = very negative experience.
Motion artefact was graded on a 4-point scale: 1 = no motion, 2 = minimal motion, 3 = moderate motion interfering with image interpretation and 4 = severe motion limiting image interpretation.
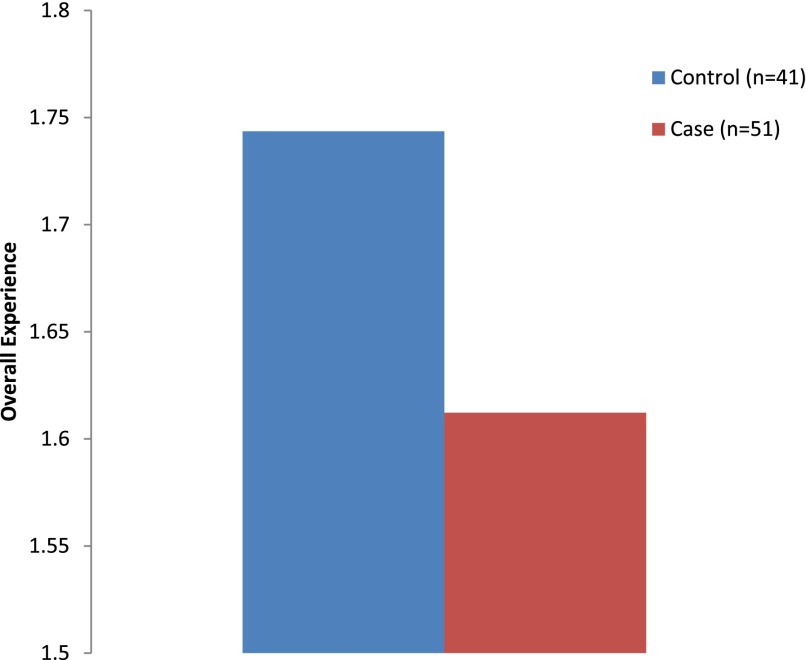
Figure 1 outlines a summary of comparison of 41 controls (1 patient was excluded for incomplete data) with 51 cases (those patients who underwent both sound and scent intervention), indicating that patients found the experience of MRI more relaxing with the presence of sensory intervention.
Figure 1.
Comparison of case and control “Overall Experience” score: the cases included are those participants who received both the scent and sound intervention. As Table 4 demonstrates, cases found the experience more relaxing [mean (standard deviation): 1.61 (0.61) vs 1.74 (0.063)], as indicated by their lower scores. Independent samples t-test showed that this failed to reach statistical significance (t90 = 0.987, p = 0.326).
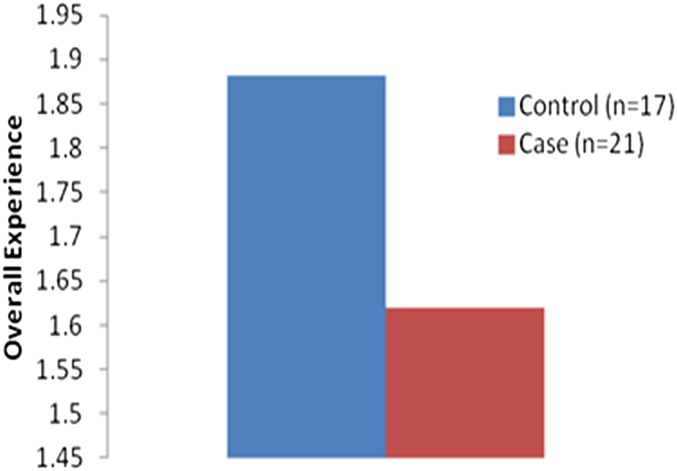
Figure 2 outlines a case vs control comparison of the grading of experience in those who had not had an MRI before, demonstrating a stronger trend to a relaxing experience in those patients who underwent sensory intervention.
Figure 2.
A comparison of overall patient experience in those who had not had an MRI before is demonstrating that cases (n = 21) found the experience more relaxing than controls (n = 17) [mean (standard deviation): 1.61 (0.58) vs 1.88 (0.60)]. Independent samples t-test showed a stronger trend towards significance, but this failed to reach statistical significance (t36 = 1.36, p = 0.183).
Subgroup analysis of patients who underwent sensory (both scent and sound) intervention during brain MRI showed a trend towards a positive experience, although without statistical significance. Cases (n = 24) had a mean score of 1.58 ± 0.65 SD vs controls (n = 15) having a mean score of 1.80 ± 0.68 SD, (t37 = 0.994, p = 0.327).
Analysis of the subgroup of patients undergoing breast MRI showed no difference between cases and controls in patient-graded experience on a 4-point scale (p = 0.57). However, note was made that a number of individual patient subjective comments in the breast MRI case group were very strongly positive.
There were no significant differences in patient-graded experience when comparing female cases and controls or male cases and controls (p > 0.04).
DISCUSSION
Many years of research have brought MRI technology to the level of complexity it has reached today.9 However, patient anxiety often remains an obstacle to optimization of this technology. Patients with poor MRI experience may refuse future MRI or request sedation for future MRI, leading to increased cost, increased scan time and the potential for increased morbidity.1,3
It has been shown that effective communication before and during the scan can reduce anxiety. Tazegul et al6 demonstrated a higher post-scan serum cortisol in patients in the control group who received no communication during MRI vs patients in the case group who received communication every 2 min during their scan. Törnqvist et al4 have shown that increased information about the MRI scanning procedure and expected experiences during the scan may decrease motion artefacts.
While the benefits of education and effective communication on patient anxiety levels are well documented, there are very limited data on the effects of sensory interventions on patient anxiety and experience of MRI in the literature. There is, however, a growing body of research exploring the effects of “sedative music” on pain, stress and anxiety in healthcare settings.
Knight and Rickard10 previously studied the effect of sedative music on physiological stress as well as subjective anxiety. Measures of subjective anxiety as well as tracking changes in systolic blood pressure and heart rate in response to stressors were examined. It was found that the presence of sedative music prevented stress-related increases across all three measurements.
The effect of sedative music on pain and anxiety in patients following open-heart surgery has also been studied. It was found that those patients who received 30 min of sedative music during post-operative chair-based resting experienced significantly less anxiety, pain sensation and pain distress than those who did not.11
Nilsson12 conducted a systematic review of 42 randomized controlled trials of the effects of music interventions in perioperative settings. Music intervention had positive effects on reducing patient anxiety and pain in approximately half of the reviewed studies.
Relative to sound, there is a scarcity of peer-reviewed academic studies on the use of scent to reduce anxiety and promote relaxation in a medical setting. However, aromatherapy has long been used as a form of alternative medicine. While aromatherapy is defined as the treatment or prevention of disease by use of essential oils, other wide-ranging purported benefits have been described, including pain and anxiety reduction, and enhancement of energy and short-term memory. Two basic theories are put forward to explain the alleged effects. The first, and less empirically supported, is that the oils have a direct pharmacological effect on the body. The other more likely mechanism is that aromas influence the brain, particularly the limbic system, via the closely connected olfactory system, and this in turn regulates the bodily experience of emotion.13
Braden et al13 performed an experiment to explore the ability of the essential oil lavandin to reduce pre-operative anxiety in patients undergoing surgery. Controlling for baseline anxiety and pain, it was found that patients exposed to the scent of lavandin experienced significantly lower anxiety. Kim et al14 observed a similar effect using lavender oil, which was found to reduce stress, bispectral index values and pain upon needle insertion in patients.
In this study, the sensory interventions, in particular the scent intervention, subjectively reduced patient anxiety, although this reduction in anxiety did not reach statistical significance, possibly owing to the low power of the study. In particular, it is worth noting that there was a trend towards a positive MRI experience in patients who received sensory intervention and who were undergoing MRI for the first time. This may indicate that this particular patient cohort may be more likely to undergo repeat MRI at a future date than if they had had a poorer first-time experience.
A limited number of patients had significant motion artefacts during the study in both the control and study groups. We did not identify a patient characteristic that significantly predicted whether the participants moved or experienced anxiety. However, it is important to note that only 3 out of the 51 participants with sensory intervention moved, which limits the model to predict movement.
The study was confounded by the fact that most patients did not experience significant anxiety or movement artefacts and, most likely, even without the smells and sounds, would not have had any problems during the scan. Therefore, it is difficult to establish whether the sounds and smells reduced anxiety when baseline levels of these factors were low to start with. Subgroup analysis revealed a mild (although not statistically significant) relationship between finding the scent intervention relaxing and a reduction in anxiety. It is possible that if a larger sample size was used, or if patients with known anxiety were studied directly, this effect may become more pronounced.
In terms of experimental design of future studies, it would be favourable to use a randomized control trial approach in participants who are known to experience difficulties during MRI scans. This, however, would lead to a longer study period and likely lower patient numbers, as the number of patients who experience anxiety and claustrophobia that limits imaging is relatively small (based on this study).
Patient experience is important in terms of psychological morbidity, including overall morale and mood. Positive patient experience may be a discriminator that is useful in a competitive market place for imaging centres. We propose that these low-cost interventions could be used routinely in all patients with a history of anxiety or for those who have had a poor experience of MRI previously and could be offered as part of a “menu” at the time of MRI, much like way that the option of radio or a personal music CD is currently offered.
CONCLUSION
This study demonstrated a subjectively improved experience of MRI for some patients with the intervention of sound and smell. The addition of these low-cost and simple interventions is likely to improve patient acceptance of MRI investigations and could offer a competitive advantage to imaging centres. The study failed to show a significant decrease in patient movement during MRI investigations. This may relate to the small study size and a low level of patient movement in the study group.
Sound and olfactory sensory environment interventions at MRI can improve the patient experience. These low-cost interventions are well tolerated, may improve acceptance of MRI in patients with anxiety and offer a competitive advantage to imaging centres.
Acknowledgments
ACKNOWLEDGMENTS
Olfactory study materials and data analysis were provided by Condiment Junkie Limited.
Contributor Information
Emma Stanley, Email: estanley@mater.ie.
Andrea Cradock, Email: andrea.cradock@ucd.ie.
James Bisset, Email: jbisset@materprivate.ie.
Ciara McEntee, Email: mcenteec@mater.ie.
Martin J O'Connell, Email: oconnellm@mater.ie.
CONFLICTS OF INTEREST
Condiment Junkie Limited was not involved in the presentation of data findings or the writing of this article.
REFERENCES
- 1.Enders J, Zimmermann E, Rief M, Martus P, Klingebiel R, Asbach P, et al. Reduction of claustrophobia during magnetic resonance imaging: methods and design of the “CLAUSTRO” randomized controlled trial. BMC Med Imaging 2011; 11: 4. doi: 10.1186/1471-2342-11-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dewey M, Schink T, Dewey CF. Claustrophobia during magnetic resonance imaging: cohort study in over 55,000 patients. J Magn Reson Imaging 2007; 26: 1322–7. doi: 10.1002/jmri.21147 [DOI] [PubMed] [Google Scholar]
- 3.Murphy KJ, Brunberg JA. Adult claustrophobia, anxiety and sedation in MRI. Magn Reson Imaging 1997; 15: 51–4. doi: 10.1016/S0730-725X(96)00351-7 [DOI] [PubMed] [Google Scholar]
- 4.Törnqvist E, Månsson A, Larsson EM, Hallström I. Impact of extended written information on patient anxiety and image motion artifacts during magnetic resonance imaging. Acta Radiol 2006; 47: 474–80. [DOI] [PubMed] [Google Scholar]
- 5.MacKenzie R, Sims C, Owens RG, Dixon AK. Patients' perceptions of magnetic resonance imaging. Clin Radiol 1995; 50: 137–43. doi: 10.1016/S0009-9260(05)83042-9 [DOI] [PubMed] [Google Scholar]
- 6.Tazegul G, Etcioglu E, Yildiz F, Yildiz R, Tuney D. Can MRI related patient anxiety be prevented? Magn Reson Imaging 2015; 33: 180–3. doi: 10.1016/j.mri.2014.08.024 [DOI] [PubMed] [Google Scholar]
- 7.Melendez JC, McCrank E. Anxiety-related reactions associated with magnetic resonance imaging examinations. JAMA 1993; 270: 745–7. [DOI] [PubMed] [Google Scholar]
- 8.Krupa K, Bekiesinska-Figatowska M. Artifacts in magnetic resonance imaging. Pol J Radiol 2015; 80: 93–106. doi: 10.12659/PJR.892628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fuchs VR, Sox HC, Jr. Physicians' views of the relative importance of thirty medical innovations. Health Aff (Millwood) 2001; 20: 30–42. doi: 10.1377/hlthaff.20.5.30 [DOI] [PubMed] [Google Scholar]
- 10.Knight WE, Rickard NS. Relaxing music prevents stress-induced increases in subjective anxiety, systolic blood pressure, and heart rate in healthy males and females. J Music Ther 2001; 38: 254–72. doi: 10.1093/jmt/38.4.254 [DOI] [PubMed] [Google Scholar]
- 11.Voss JA, Good M, Yates B, Baun MM, Thompson A, Hertzog M. Sedative music reduces anxiety and pain during chair rest after open-heart surgery. Pain 2004; 112: 197–203. doi: 10.1016/j.pain.2004.08.020 [DOI] [PubMed] [Google Scholar]
- 12.Nilsson U. The anxiety- and pain-reducing effects of music interventions: a systematic review. AORN J 2008; 87: 780–807. doi: 10.1016/j.aorn.2007.09.013 [DOI] [PubMed] [Google Scholar]
- 13.Braden R, Reichow S, Halm MA. The use of the essential oil lavandin to reduce preoperative anxiety in surgical patients. J Perianesth Nurs 2009; 24: 348–55. doi: 10.1016/j.jopan.2009.10.002 [DOI] [PubMed] [Google Scholar]
- 14.Kim S, Kim HJ, Yeo JS, Hong SJ, Lee JM, Jeon Y. The effect of lavender oil on stress, bispectral index values, and needle insertion pain in volunteers. J Altern Complement Med 2011; 17: 823–6. doi: 10.1089/acm.2010.0644 [DOI] [PubMed] [Google Scholar]