Abstract
Objective:
This study aimed to assess the types of vertebral segments at the thoracolumbar junction, as they relate to the most caudal ribs, to evaluate the reliability of this assessment using axial CT with curved planar reformatting (CPR) images, to describe the morphologic characteristics of a thoracolumbar transitional vertebra (TLTV), to introduce a new classification system for the TLTV and to evaluate the reliability of the classification system using axial CT with CPR images.
Methods:
This was a retrospective review of 744 consecutive patients who underwent spine CT imaging that included the thoracolumbar junction. Two radiologists (Readers 1 and 2) independently evaluated the axial CT with CPR images for all cases (n = 744). Each radiologist differentiated the vertebral segments at the thoracolumbar junction as TLTV or non-TLTV (thoracic segment or lumbar segment). In addition, each radiologist classified the 94 patients with the TLTV using a novel classification system. Interobserver agreement between the two radiologists regarding the differentiation of vertebral segments at the thoracolumbar junction was analysed with kappa statistics. Similarly, intra- and interobserver agreement regarding TLTV classification was analysed with kappa statistics.
Results:
Interobserver agreement between the two readers with respect to the differentiation of vertebral segments at the thoracolumbar junction via axial CT with CPR images was nearly perfect (κ-value: 0.959). Interobserver agreement between the two readers with respect to TLTV classification using axial CT with CPR images was nearly perfect (κ-value: 0.846). In addition, intraobserver agreement for Reader 1 was also nearly perfect (κ-value: 0.877).
Conclusion:
Morphologic analysis of the thoracolumbar junction may help accurate spinal enumeration.
Advances in knowledge:
Consideration of various variants at the thoracolumbar junction should help radiologists and clinicians to interpret the morphology of the thoracolumbar junction. This may facilitate communication with the referring clinician, thereby reducing the error in spinal enumeration.
INTRODUCTION
In the typical method of spinal enumeration,1–6 the last thoracic vertebra is defined by counting down from the second cervical vertebra (C2) or the first thoracic vertebra (T1) under the assumption that there are 12 thoracic vertebra. However, this method may be prone to error because the number and distribution of thoracic and lumbar segments exhibit considerable variation, even though the cervical spine has a relatively stable morphology and a fixed vertebral count of seven.3,7–10 In addition, acquisition of whole-body spine radiographs, MR scans or CT scans are needed for this method. Nonetheless, this method remains widely used.1,2,4–6 Wigh et al suggested that the true nature of lower vertebral segmentation can be established by using images that include the thoracolumbar junction.11,12 In such images, hypoplastic true ribs can be differentiated from large transverse processes, thereby allowing correct identification of the L1 vertebral body.11,12 Farshad-Amacker et al1 also proposed that ribs or rib equivalents are more reliable for numbering the lumbar vertebra. Several studies have labelled the rib-bearing vertebra as the thoracic vertebra.8,13,14 However, these studies did not establish definite criteria by which ribs can be differentiated from rib equivalents8,14 (Table 1). Without classifying bones as either ribs or rib equivalents, any vertebra showing an attached bone is considered to be a thoracic vertebra.13
Table 1.
Comparison of enumeration methods
| System of enumeration | Advantages | Disadvantages |
|---|---|---|
| Counting down from the second cervical vertebra (C2) or the first thoracic vertebra (T1) under the assumption that there are 12 thoracic vertebra1–6 | • Counting the number of presacral segments | • Prone to error because the number and distribution of thoracic and lumbar segments exhibit significant variation (e.g. 22, 23 or 25 presacral segments, 13 rib-bearing thoracic vertebra with 4 lumbar-type vertebra, 11 rib-bearing thoracic vertebra with 6 lumbar-type vertebra) • Acquisition of whole-body spine radiographs, MR scans or CT scans are needed. If no such images have been acquired, the patient must be recontacted |
| Labelling the rib-bearing vertebra as the thoracic vertebra8,13,14 | • Possible without whole spine images • Allows segmentation of the lumbar and thoracic vertebra |
• Lack of definite criteria by which ribs can be differentiated from rib equivalents (until the current study) |
| Differentiation of vertebral segments at the thoracolumbar junction as the TLTV or non-TLTV (thoracic or lumbar) segments through definitive criteria for differentiating the most caudal ribs | • Possible without whole spine images, by using the axial spine CT image with a CPR image. The patient's axial chest, abdomen CT or spine MR image can also be used for morphologic evaluation, except for the length of bone • Allows segmentation of the lumbar and thoracic vertebra |
• Requires an axial image that shows the relationship between the vertebra and most caudal ribs |
CPR, curved planar reformatting; TLTV, thoracolumbar transitional vertebra.
Accurate spinal enumeration is necessary to establish the correct level in spinal surgery. In some cases, spine surgeries are performed on unintended levels because of various spinal variants.9,15,16 In contrast to the lumbosacral transitional vertebra, very little is known about the thoracolumbar transitional vertebra (TLTV). Indeed, the precise definition of the vertebra is still debated.
Direct visualization of the thoracolumbar junction would be helpful for evaluating the morphologic characteristics of this region. CT with curved planar reformatting (CPR) imaging is an appropriate modality for evaluating bone structure at this junction and for measuring the length of the curves of various bones, including rib bones.17 Therefore, the purpose of this study was to classify the vertebral segments at the thoracolumbar junction as either TLTV or non-TLTV (i.e. thoracic or lumbar segment) according to the most caudal ribs. We also aimed to evaluate the reliability of this approach using axial CT with CPR images, to describe the morphologic characteristics of the TLTV, to introduce a new classification system for the TLTV and to evaluate the reliability of the classification system using axial CT with CPR images.
METHODS AND MATERIALS
Case selection
This study was a retrospective review of 744 consecutive patients who underwent CT of the spine, including the thoracolumbar junction, for back pain between January 2012 and December 2014. Our institutional review board approved this study, and the requirement for informed consent was waived.
Spine CT
All CT examinations were performed on a dual-source CT scanner (Somatom® Definition® Flash; Siemens Healthcare, Erlangen, Germany) equipped with two X-ray tubes. All spine scans were acquired by using an identical protocol (detector collimation, 128 × 0.6 mm; pitch, 0.7; gantry rotation time, 0.5 s) with combined modulation (CARE Dose 4D®). Standard-of-care spine CT imaging was performed at 275 quality reference mAs. Images were reconstructed with 1-mm section thickness and 0.7-mm reconstruction increments.
Definition and nomenclature of ribs
A rib is defined as a separated bone that articulates with the facet at the body or pedicle of the vertebra.12,18 The pedicle is one of the paired parts that connects the lamina to the vertebral body.19 In this study, the anterior and posterior borders of the pedicle were defined as the posterior margin of the vertebral body and the anterior margin of the lamina, respectively.19 However, the anterior margin of the lamina has not been clearly defined in the anatomic literature and, thus, is somewhat ambiguous. The lamina has been defined as the flattened posterior portion of the vertebral arch from which the spinous process extends.20 Based on this definition, the anterior margin of the lamina was defined as the point at which the concavity turns into a straight line at the posterior portion of the vertebral arch.
Farshad-Amacker et al1 proposed that most caudal ribs can be classified into one of four types: normal rib, hypoplastic rib (short rib), unfused transverse process (accessory ossification centre) and mixed type. However, the nomenclature for the most caudal ribs is often confusing. Several reports have used different terms when referring to the most caudal ribs.1,7,8,12,21 For example, short ribs (as we refer to them in the present study) have been referred to as hypoplastic ribs, diminutive ribs and rudimentary ribs.1,12,13 A short rib has been defined as a separated bone <3.8 cm in length that articulates with the facet at the pedicle of the vertebra, as described by Wigh et al.12 In addition, the vertebral body was included in the location of the articular facet for the rib heads in this study. Although the articular facets for the rib heads at the lower thoracic vertebral segments are usually located on pedicles,18 we have observed that they are sometimes located at the vertebral bodies. This observation is based on years of reading spine CT images in our division. A short rib was thus defined as a separated bone, 3.8 cm in length, that articulates with the facet at the pedicle or the vertebral body in our study. Similar to the short rib, the accessory ossification centre has also been given several names, including the lumbar rib and the unfused transverse process.1,12,22 The term “accessory ossification centre” is preferred because this structure is generally bullous and several centimeters long.12 Therefore, we used this term in the present study. Accessory ossification centres refer to additional bones that can be elongated and rib shaped; these bones articulate with shortened lumbar costal processes or are linearly adjacent to the processes, thereby obscuring the observation of this joint as a true joint.12 An accessory ossification centre was defined as a structure articulating with a shortened lumbar costal process or as a structure that was linearly adjacent to such processes in this study. Accessory ossification centres were not further subtyped in our study. As mentioned above, although Farshad-Amacker et al1 reported four types of caudal ribs, they also noted the difficulty in differentiating most caudal ribs and did not propose definite definitions for them. Therefore, a separated bone that did not meet the criteria for a short rib, a normal rib (>3.8 cm length rib) or an accessory ossification centre at the thoracolumbar junction was defined as a mixed-type rib in this study. Its morphologic appearance included a separated bone articulating with the facet placed on both the pedicle and transverse process.
Definition of thoracolumbar transitional vertebra or non-thoracolumbar transitional vertebra
A thoracic vertebra is identified by the presence of paired ribs that are 3.8 cm or more in length and originate from the facet at the pedicle (or the body of the vertebra). By contrast, a lumbar vertebra is defined as a vertebra without articulating ribs, the absence of facets for a rib on the pedicle (or the body of the vertebra), with fused transverse processes.12
Different definitions of the TLTV have been proposed.1,7,8,12 Wigh et al12 suggested that the TLTV includes segments with a short rib, <3.8 cm in length or with an accessory ossification centre. However, Thawait et al7 defined the TLTV as the presence of hypoplastic ribs <3.8 cm in length on the lowest rib-bearing segment. Carrino et al8 defined the TLTV as a vertebra with one side showing a rib and the contralateral side showing a transverse process. However, these studies are not sufficient to explain the various morphologies of the TLTV. Moreover, no definitive criteria have been proposed by which the TLTV can be accurately classified. A transitional vertebra is defined as one with characteristics of the corresponding superior and inferior segments,12 whereas the TLTV is defined as a vertebra with partially retained features of the thoracic and lumbar segments at the thoracolumbar junction.7,12 In the current study, any segment that did not meet the above-mentioned criteria for thoracic or lumbar vertebra in the thoracolumbar junction was considered a TLTV.
Establishment of thoracolumbar transitional vertebra classification
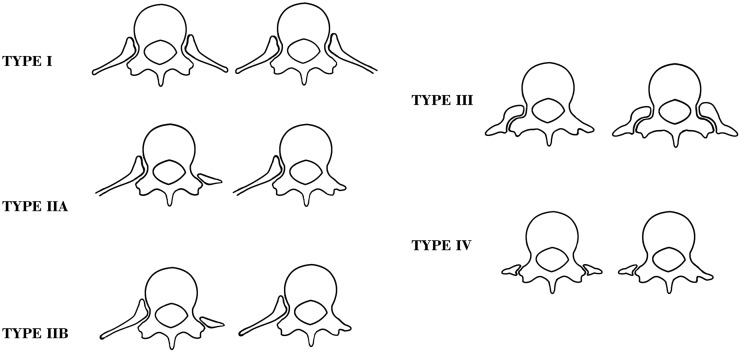
Since no definite criteria for identifying the TLTV have yet been established, classification was based on observations made in our division over years of reading spine CT images and previous literature.1,7,8,12 After several meetings with two radiologists, we developed a classification system for the TLTV as observed on axial CT with CPR images. Five types (Types I, IIA, IIB, III and IV) were identified according to the length of the separated bones, the presence or absence of a facet at the pedicle (or body) of the vertebra and the presence or absence of articulation with separated bones (Figure 1). Type I includes paired ribs with more than one short rib; Type IIA, a 3.8-cm or longer rib on one side and an accessory ossification centre or transverse process on the contralateral side; Type IIB, a short rib on one side and an accessory ossification centre or transverse process on the contralateral side; Type III, a unilateral or bilateral mixed type rib; and Type IV, a unilateral or bilateral accessory ossification centre.
Figure 1.
Schematic illustration of thoracolumbar transitional vertebra (TLTV) classification using axial CT with curved planar reformatting images. Type I includes paired ribs with more than one short rib; Type IIA, a 3.8-cm or longer rib on one side and an accessory ossification centre or transverse process on the contralateral side; Type IIB, a short rib on one side and an accessory ossification centre or transverse process on the contralateral side; Type III, a unilateral or bilateral mixed type rib; and Type IV, a unilateral or bilateral accessory ossification centre.
Image analysis
For the thoracolumbar junction evaluation, two radiologists (Readers 1 and 2) independently evaluated the axial CT with CPR images for all cases (n = 744). Each radiologist assessed the types of vertebral segments at the thoracolumbar junction by classifying each vertebral segment at the thoracolumbar junction as TLTV or non-TLTV (a thoracic or lumbar segment). To ensure accurate measurement of bone length, the desired curves were defined along the ribs in all cases and each radiologist independently measured the lengths of the ribs on the CPR images (Figure 2). Rib length was measured by drawing a line at the midpoint of the rib width from the proximal head of the rib to the distal body. The length of this line was considered to be the length of the rib. Each reader was blinded to the results of the other reader. In cases of TLTV disagreement, a third radiologist (Reader 3) made a final decision.
Figure 2.
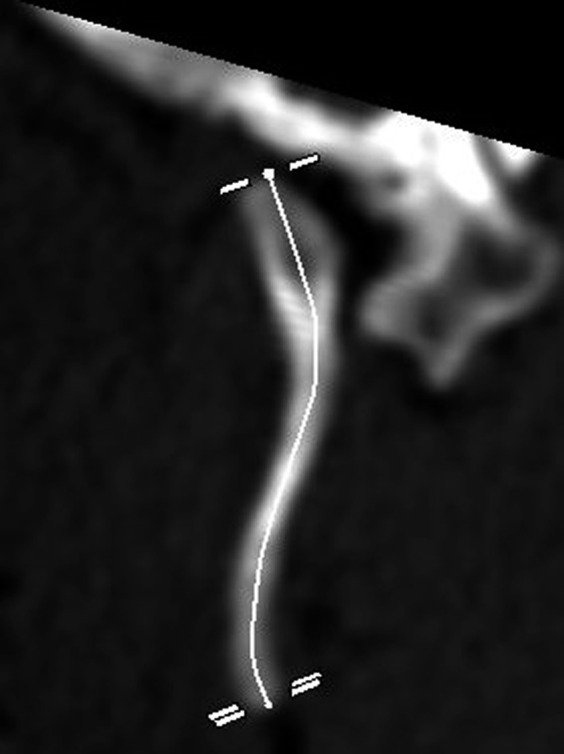
Curved planar reformatting images of a rib.
Next, two radiologists independently evaluated the axial CT findings and CPR images of each patient with TLTV. Each radiologist assessed the TLTV type using the new classification system described above. Although accessory ossification centres sometimes resemble fracture fragments, these anomalies are radiologically different from fractures because they show smooth and round borders.22 Each reader was blinded to the results of the other reader. Reader 1 also evaluated the TLTV axial CT and CPR images after more than 2 months in order to assess intraobserver agreement. All examinations were reviewed in a random order to avoid bias.
Statistical analysis
Interobserver agreement between the two radiologists with respect to the differentiation of vertebral segments at the thoracolumbar junction was analysed using kappa statistics. Interobserver agreement between the two radiologists and intraobserver agreement (Reader 1) regarding TLTV classification were also analysed using kappa statistics. The κ- values were categorized as slight (0–0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80) or nearly perfect (0.81–1.00) agreement.23
RESULTS
The average patient age was 45.9 years (range, 11–95 years). In total, 490 males (65.9%) and 254 females (34.1%) were included in the study. In seven cases, the two readers reached different results regarding the differentiation of the vertebral segment type at the thoracolumbar junction. All of these cases (n = 7) included paired ribs originating from the facet at the pedicle (or the vertebral body). The rib lengths in these seven cases were also discrepant between the two readers. Therefore, a third radiologist (Reader 3) made a final decision by independently measuring the rib length. Finally, all seven cases were regarded as non-TLTV (thoracic segment), since the length of the rib was >3.8 cm. In total, 94 patients had TLTV, a frequency of 12.6% (94/744). The average age of the patients with TLTV was 43 years (range, 18–95 years); these patients included 61 males (64.9%) and 33 females (35.1%) (Table 2). The TLTV was classified into five types (I, IIA, IIB, III or IV) according to the CT scans and CPR images (Figures 3–7). The TLTV types for each reader are presented in Table 3. The TLTV types in order of decreasing frequency were as follows: Type IV, Type I, Type II, and Type III.
Table 2.
Demographic characteristics of study patients
| Characteristic | Value |
|---|---|
| Total 744 patients | |
| Age (years) (range) | 45.9 (11–95) |
| Male patients, no. (%) | 490 (65.9) |
| Female patients, no. (%) | 254 (34.1) |
| TLTV, no. (%) | 94 (12.6) |
| 94 patients with TLTV | |
| Age (years) (range) | 43 (18–95) |
| Male patients, no. (%) | 61 (64.9) |
| Female patients, no. (%) | 33 (35.1) |
no., number; TLTV, thoracolumbar transitional vertebra.
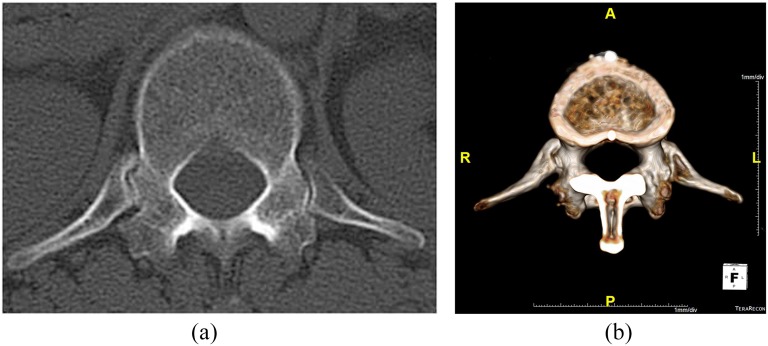
Figure 3.
A 52-year-old female with Type I thoracolumbar transitional vertebra. (a) Bilateral short ribs on an axial CT scan. (b) Reformatted volume-rendered image from the axial CT images of the thoracolumbar junction.
Figure 7.
A 29-year-old female with Type IV thoracolumbar transitional vertebra. (a) Bilateral accessory ossification centres on the axial CT scan. (b) Reformatted volume-rendered image from the axial CT images of the thoracolumbar junction.
Table 3.
Thoracolumbar transitional vertebra (TLTV) classification for each reader
| TLTV type | Reader 1 | Reader 2 | Reader 1 after more than 2 months |
|---|---|---|---|
| Type I | 18 | 20 | 16 |
| Type IIA | 2 | 2 | 2 |
| Type IIB | 10 | 10 | 13 |
| Type III | 10 | 10 | 9 |
| Type IV | 54 | 52 | 54 |
Data are numbers of patients.
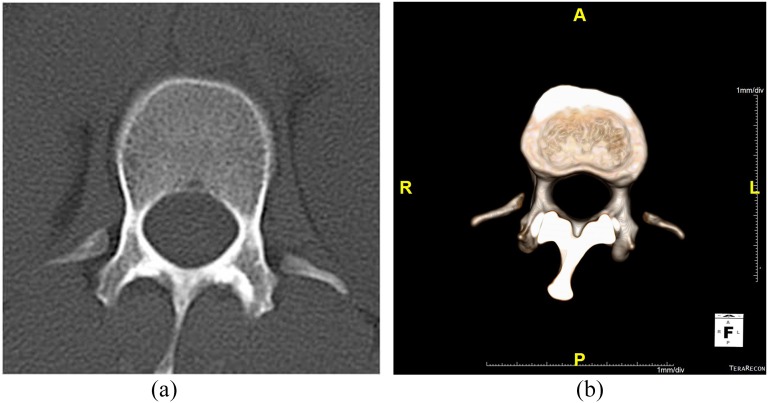
Figure 4.
A 51-year-old female with Type IIA thoracolumbar transitional vertebra. (a) Axial CT scan of a long rib measuring >3.8 cm on the right side and with an accessory ossification centre on the left side. (b) Reformatted volume-rendered image from the axial CT images of the thoracolumbar junction.
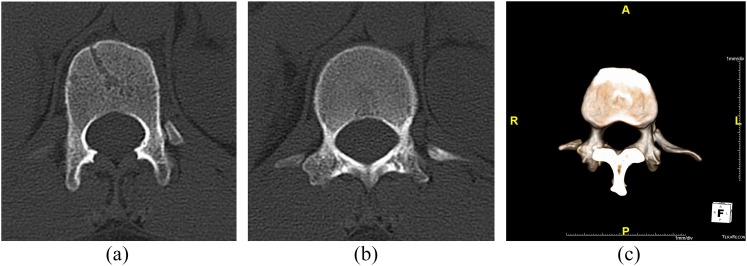
Figure 5.
A 31-year-old female with Type IIB thoracolumbar transitional vertebra. (a, b) A short rib on the left side and an accessory ossification centre on the right side on an axial CT scan. (c) Reformatted volume-rendered image from the axial CT images of the thoracolumbar junction.
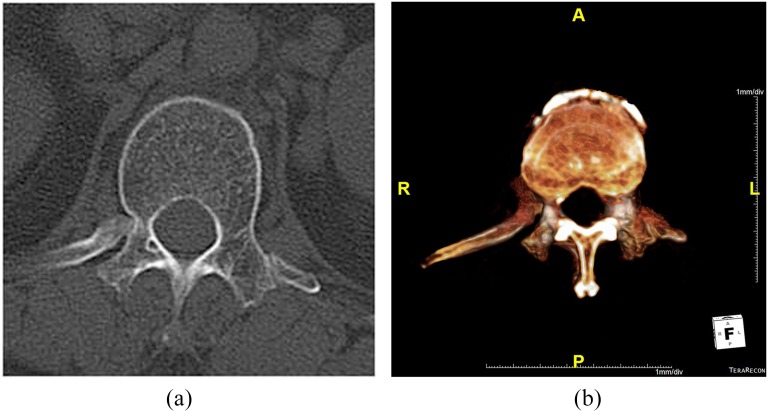
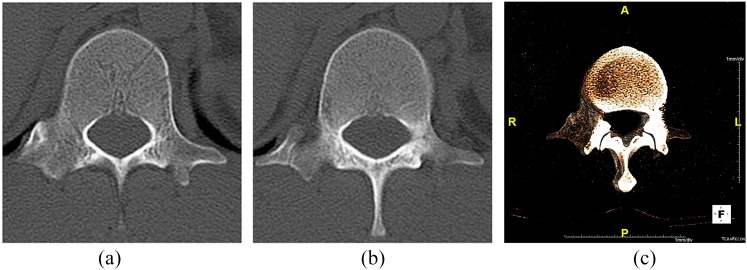
Figure 6.
A 35-year-old male with Type III thoracolumbar transitional vertebra. (a, b) A mixed-type rib on the right side of the axial CT scan image. (c) Reformatted volume-rendered image from the axial CT images of the thoracolumbar junction.
Interobserver agreement between the two readers regarding the differentiation of the vertebral segment type at the thoracolumbar junction on CT images with CPR was nearly perfect (κ-value: 0.959). Interobserver agreement between the two readers regarding TLTV classification on CT images with CPR was also nearly perfect (κ-value: 0.846). Intraobserver agreement for Reader 1 was also nearly perfect (κ-value: 0.877).
DISCUSSION
We proposed definitive criteria for differentiating the most caudal ribs. These criteria involved measuring the lengths of the separated bones, evaluating the presence or absence of a facet at the pedicle (or body), and determining the presence of articulation with the separated bones. Here, we showed that this method was highly reliable in determining which vertebral segments at the thoracolumbar junction were TLTV and which were non-TLTV (thoracic or lumbar) segments. If TLTV was present, the next caudal vertebral segment could be considered the first lumbar vertebral segment. This method may help the numbering of lumbar vertebra on axial CT scans with CPR images. An advantage of this method is that it does not require additional modalities and/or images, such as whole body spinal radiographs, MRI, or CT (Table 1).
We analysed the morphologic characteristics of the TLTV and identified a set of criteria, based on axial CT and CPR images, by which the TLTV can be classified. Our TLTV classification system showed high intra- and interobserver agreement. We anticipate that our classification system will help establish a standard definition of the TLTV. The consideration of various variants at the thoracolumbar junction should help radiologists and clinicians to interpret the morphology of the thoracolumbar junction. Moreover, increased awareness of TLTV morphology may reduce errors in spinal enumeration.
In this study, the frequency of TLTV was 12.6% (94 of 744). By contrast, Carrino et al8 reported TLTV in 4.1% (6 of 147) of patients. Carrino et al defined the TLTV as a vertebra with one side showing a rib and the contralateral side showing a transverse process. Thus, only those vertebra classified as Type IIA and IIB in our classification system would have been defined as the TLTV by the criteria of Carrino et al. This difference may explain why TLTV frequency varied between the two studies.
Wigh et al12 proposed that segments with short ribs at the thoracolumbar junction can be considered the thoracic-type TLTV, whereas segments with accessory ossification centres can be considered the lumbar-type TLTV. It may be possible to achieve a consensus through discussion or additional studies that Type I vertebra is thoracic-type TLTV and Type IV vertebra is lumbar-type TLTV. However, Types II and III vertebra are not easily grouped into thoracic vs lumbar types.
Our study had several limitations. First, a relatively small number of cases with thoracolumbar transitional vertebra were evaluated. Therefore, future studies with larger sample sizes are necessary. Second, most patients in our study complained of pain, so our study might have been affected by selection bias. In addition, we did not assess the relationship between pain and TLTV morphology on CT images. As a third limitation, the TLTV classification was based mainly on the length of the separated bones and the presence or absence of facet joint articulation with the separated bones at the pedicle (or the body) of the vertebra. The morphology of the vertebral body, spinal canal, transverse process and the direction of the articular facet were not categorized. However, these features are not likely to be helpful for categorizing the TLTV using objective standards because of the morphological complexity and different directions of the vertebra. The fourth limitation is that rib length measurements are prone to error. Although we used CPR images to reduce error, the images may still have led to inaccuracies in rib length measurement. Furthermore, the frequency of Type IV was high in our study because we did not restrict accessory ossification centres to a given morphology. Accessory ossification centres have been reported to be occasionally elongated and rib shaped.12 However, no definitive criteria for the accessory ossification centres that are elongated and rib shaped have yet been established. Therefore, we classified all accessory ossification centres as Type IV in our TLTV classification system.
CONCLUSION
We differentiated the most caudal ribs by measuring the lengths of the separated bones, evaluating the presence or absence of a facet at the pedicle (or body) and assessing the presence of articulation with the separated bones. Using this method, we differentiated vertebral segments (TLTV or non-TLTV) at the thoracolumbar junction. We also proposed new morphologic characteristics for the TLTV and outlined a novel TLTV classification scheme. Morphologic analysis of the thoracolumbar junction may facilitate communication with the referring clinician, thereby reducing the error in spinal enumeration.
Acknowledgments
ACKNOWLEDGMENTS
The authors acknowledge the contribution of Su Jin Hwang to the illustrations.
Contributor Information
Se K Park, Email: cordialsk@hanmail.net.
Jung G Park, Email: cibertim@naver.com.
Beom S Kim, Email: zxczxc@gmail.net.
Jin D Huh, Email: jdhuh@dreamwiz.com.
Hee Kang, Email: soinvain@naver.com.
Funding
Our study was supported by a grant from Kosin University College of Medicine (2015).
REFERENCES
- 1.Farshad-Amacker NA, Aichmair A, Herzog RJ, Farshad M. Merits of different anatomical landmarks for correct numbering of the lumbar vertebrae in lumbosacral transitional anomalies. Eur Spine J 2015; 24: 600–8. doi: 10.1007/s00586-014-3573-7 [DOI] [PubMed] [Google Scholar]
- 2.Farshad-Amacker NA, Lurie B, Herzog RJ, Farshad M. Is the iliolumbar ligament a reliable identifier of the L5 vertebra in lumbosacral transitional anomalies? Eur Radiol 2014; 24: 2623–30. doi: 10.1007/s00330-014-3277-8 [DOI] [PubMed] [Google Scholar]
- 3.Akbar JJ, Weiss KL, Saafir MA, Weiss JL. Rapid MRI detection of vertebral numeric variation. AJR Am J Roentgenol 2010; 195: 465–6. doi: 10.2214/AJR.09.3997 [DOI] [PubMed] [Google Scholar]
- 4.Peh WC, Siu TH, Chan JH. Determining the lumbar vertebral segments on magnetic resonance imaging. Spine (Phila Pa 1976) 1999; 24: 1852–5. doi: 10.1097/00007632-199909010-00017 [DOI] [PubMed] [Google Scholar]
- 5.Hahn PY, Strobel JJ, Hahn FJ. Verification of lumbosacral segments on MR images: identification of transitional vertebrae. Radiology 1992; 182: 580–1. doi: 10.1148/radiology.182.2.1732988 [DOI] [PubMed] [Google Scholar]
- 6.Tureli D, Ekinci G, Baltacioglu F. Is any landmark reliable in vertebral enumeration? A study of 3.0-Tesla lumbar MRI comparing skeletal, neural, and vascular markers. Clin Imaging 2014; 38: 792–6. doi: 10.1016/j.clinimag.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 7.Thawait GK, Chhabra A, Carrino JA. Spine segmentation and enumeration and normal variants. Radiol Clin North Am 2012; 50: 587–98. doi: 10.1016/j.rcl.2012.04.003 [DOI] [PubMed] [Google Scholar]
- 8.Carrino JA, Campbell PD, Jr, Lin DC, Morrison WB, Schweitzer ME, Flanders AE, et al. Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology 2011; 259: 196–202. doi: 10.1148/radiol.11081511 [DOI] [PubMed] [Google Scholar]
- 9.Hanson EH, Mishra RK, Chang DS, Perkins TG, Bonifield DR, Tandy RD, et al. Sagittal whole-spine magnetic resonance imaging in 750 consecutive outpatients: accurate determination of the number of lumbar vertebral bodies. J Neurosurg Spine 2010; 12: 47–55. doi: 10.3171/2009.7.SPINE09326 [DOI] [PubMed] [Google Scholar]
- 10.Kier EL. Some developmental and evolutionary aspects of the lumbosacral spine. Gouaze ASG, ed. Berlin: Springer Berlin Heidelberg; 1988. [Google Scholar]
- 11.Hughes RJ, Saifuddin A. Imaging of lumbosacral transitional vertebrae. Clin Radiol 2004; 59: 984–91. doi: 10.1016/j.crad.2004.02.019 [DOI] [PubMed] [Google Scholar]
- 12.Wigh RE. The thoracolumbar and lumbosacral transitional junctions. Spine (Phila Pa 1976) 1980; 5: 215–22. doi: 10.1097/00007632-198005000-00003 [DOI] [PubMed] [Google Scholar]
- 13.Sekharappa V, Amritanand R, Krishnan V, David KS. Lumbosacral transition vertebra: prevalence and its significance. Asian Spine J 2014; 8: 51–8. doi: 10.4184/asj.2014.8.1.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg 2007; 73: 687–95. [PubMed] [Google Scholar]
- 15.Wigh RE. Phylogeny and the herniated disc. South Med J 1979; 72: 1138–43. doi: 10.1097/00007611-197909000-00017 [DOI] [PubMed] [Google Scholar]
- 16.Malanga GA, Cooke PM. Segmental anomaly leading to wrong level disc surgery in cauda equina syndrome. Pain Physician 2004; 7: 107–10. [PubMed] [Google Scholar]
- 17.Cody DD. AAPM/RSNA physics tutorial for residents: topics in CT. Image processing in CT. Radiographics 2002; 22: 1255–68. doi: 10.1148/radiographics.22.5.g02se041255 [DOI] [PubMed] [Google Scholar]
- 18.Wikipedia C. Thoracic vertebra. Wikipedia, the free encyclopedia; 2015 [updated 26 October 2015; cited 18 November 2015]; Available from: https://en.wikipedia.org/w/index.php?title=Thoracic_vertebrae&oldid=687547926 [Google Scholar]
- 19.Miller-Keane and Marie T. O'Toole MT. Miller-Keane Encyclopedia & Dictionary of Medicine, Nursing & Allied health—revised reprint. 7th edn. Philadelphia, PA. WB Saunders; 2003. Available from: http;//medical-dictionary.thefreedictionary.com/pedicle [Google Scholar]
- 20.Dictionary.com. Lamina of vertebral arch. The American Heritage® Stedman's Medical Dictionary. Houghton Mifflin Company. 2015 [cited 17 November 2015]; Available from: http://dictionary.reference.com/browse/lamina-of-vertebral-arch [Google Scholar]
- 21.Singer KP, Breidahl PD. Accessory ossification centres at the thoracolumbar junction. Surg Radiol Anat 1990; 12: 53–8. doi: 10.1007/BF02094126 [DOI] [PubMed] [Google Scholar]
- 22.Mellado JM, Larrosa R, Martin J, Yanguas N, Solanas S, Cozcolluela MR. MDCT of variations and anomalies of the neural arch and its processes: part 2–articular processes, transverse processes, and high cervical spine. AJR Am J Roentgenol 2011; 197: W114–21. doi: 10.2214/AJR.10.5811 [DOI] [PubMed] [Google Scholar]
- 23.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74. doi: 10.2307/2529310 [DOI] [PubMed] [Google Scholar]