Abstract
Pancreatic ductal adenocarcinoma is a highly aggressive tumor with an overall 5-year survival rate of less than 5%. Prognosis and treatment depend on whether the tumor is resectable or not, which mostly depends on how quickly the diagnosis is made. Chemotherapy and radiotherapy can be both used in cases of non-resectable pancreatic cancer. In cases of pancreatic neoplasm that is locally advanced, non-resectable, but non-metastatic, it is possible to apply percutaneous treatments that are able to induce tumor cytoreduction. The aim of this article will be to describe the multiple currently available treatment techniques (radiofrequency ablation, microwave ablation, cryoablation, and irreversible electroporation), their results, and their possible complications, with the aid of a literature review.
Keywords: Irreversible electroporation, Pancreatic cancer, Pancreatic adenocarcinoma, Percutaneous treatment, Ablation treatment, Microwave ablation, Cryoablation, Radiofrequency ablation
Core tip: Pancreatic ductal adenocarcinoma is a highly aggressive tumor with a prognosis and treatment that depend on whether the tumor is resectable or not, which mostly depends on how quickly the diagnosis is made. In cases of non-metastatic pancreatic neoplasm that is locally advanced, it is possible to apply percutaneous treatments that are able to induce tumor cytoreduction. This article aims to expose the technical procedures, results, and complications of the multiple treatment techniques that are currently available.
INTRODUCTION
Pancreatic ductal adenocarcinoma is the most common primary malignancy of the pancreas and is the most frequent exocrine pancreatic neoplasm, representing 80% of malignant pancreatic tumors[1-4].
Treatment and prognosis of pancreatic ductal adenocarcinoma depend on tumor resectability, which is usually linked with how quickly the diagnosis was made[5,6]. In almost 95% of cases, pancreatic ductal adenocarcinoma is diagnosed at an advanced stage[1], with locally advanced or metastatic disease in 40% of cases[2,6,7].
The majority of pancreatic tumors that undergo percutaneous treatment are ductal adenocarcinomas[8-11].
CLINICAL INDICATIONS
The majority of percutaneous treatment procedures, regardless of whether they involve either thermal or non-thermal ablative surgery, are dedicated to ductal adenocarcinoma[8-11] if it is locally advanced and unresectable, but not metastatic; a required indication for percutaneous treatment of ductal adenocarcinoma is therefore a locally advanced unresectable tumor, without the presence of metastases. Although tumor resectability is an absolute exclusion criterion, since complete surgical resection is the only potentially curative treatment for this tumor, only about 20% of patients present with resectable disease at the time of diagnosis. The presence of distant metastases is another exclusion criterion, and includes ascites that can be an indirect sign of peritoneal carcinomatosis[4]. It is therefore mandatory that a pathologically proved diagnosis and the correct tumor staging are obtained before percutaneous procedures.
Chemotherapy is the treatment of choice in unresectable pancreatic adenocarcinoma. Nowadays, new treatments such as radiofrequency ablation (RFA), microwave ablation (MWA), cryoablation, and irreversible electroporation (IRE) can be considered, together with chemotherapy, in multimodal therapeutic approaches for unresectable pancreatic adenocarcinoma that is locally advanced and without metastases. The palliative therapeutic effects of these treatments are intuitively linked to the development of intralesional necrosis, cytolysis, and cells death, with a resulting neoplastic mass cytoreduction[12]; some studies have explained some of the argumentations on post-ablation amplification of tumor-induced immune response[13]. These treatments can be associated with chemotherapy and could be included in a combined therapeutic plan that is tailored for each individual case[4].
TECHNIQUES AND RESULTS
There are currently many techniques for treating pancreatic ductal adenocarcinoma that is locally advanced and without metastases. These different techniques can be divided in two main groups: the thermal ablative group, which uses thermal energy, and the non-thermal ablative group, which uses energy-making direct damage to neoplastic cells that is unmediated by any thermal effect. All of these techniques can be performed in a surgery room with laparotomy or laparoscopy approaches, or they can be performed via percutaneous or endoscopic approaches, which are less invasive.
RFA
RFA causes coagulative necrosis and tissue damage via the generation of high local temperatures produced by high frequency alternating current application. RFA is currently used in many solid organs malignancies, such as hepatocellular carcinoma, thyroid neoplasms, breast and prostate tumors, and pancreatic neoplasms; it has a very important role in the treatment of hepatocellular carcinoma and has become a standard therapy[14,15].
RFA of pancreatic cancer can be guided by ultrasound both percutaneously and with endoscopic ultrasound or intraoperatively by intraoperative ultrasound; the latter is usually required in instances of biliary and gastric bypass for pancreatic head tumors[4,16,17].
The ablation procedure is performed under local anesthesia with patient sedation in both percutaneous and endoscopic approaches. In addition to the mandatory confirmation of the malignant nature of the lesion by pathological analysis before commencing treatment, it is also extremely important to carry out precise staging of the tumor.
The percutaneous approach can be more safely considered for the ablation of pancreatic tumors located in the body, as the complicated anatomy of the pancreatic head region makes the percutaneous RFA procedure more difficult and dangerous in this region. However, the pancreatic head can be treated with RFA via the endoscopic approach. RFA is performed with a needle that has to be inserted completely inside the lesion. The most efficient approach, needle choice, and opening degree of the electrodes are usually influenced by tumor shape and size.
There are currently two main types of needle: those with expandable electrodes (Figure 1) and those with single electrodes (Figure 2). In the former, the expandable electrodes can be opened from the top (Figure 1A) or the back of the needle (Figure 1B), with these two needle types each being used in different way. With electrodes opened from the top, the needle tip has to be stopped immediately before the lesion and then up to nine electrodes have to be opened up and widened into the lesion. This type of needle can be used to treat small tumors because it can be opened at different degrees in relation to the size of the requested ablation area; unfortunately, however, the flexibility of electrodes can be a disadvantage in the treatment of very hard lesions. With needles where the electrodes open from back, the electrodes, usually four, are opened up at about 2 cm behind the tip and moved towards the outside so that the needle, for correct positioning, has to pass completely through the tumor; the presence of the central needle for at least 2 cm within the mass assures that the electrodes are inside the neoplastic tissue. This type of needle crosses throughout the mass with stiffer electrodes, guaranteeing excellent stability inside the tumor even in the presence of hard tumors. However, the needle’s requirement to be introduced throughout the lesion for at least 2 cm can have disadvantages related to tumor location and dimensions.
Figure 1.
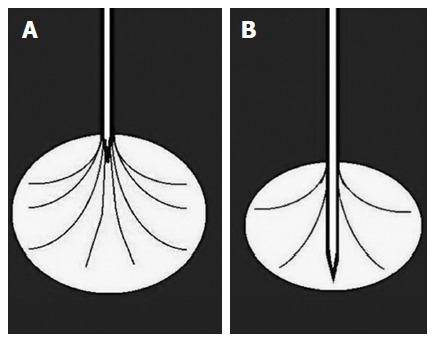
Needle with expandable electrodes. Electrodes can be opened within the lesion from the top (A) or from the back (B) of the needle.
Figure 2.
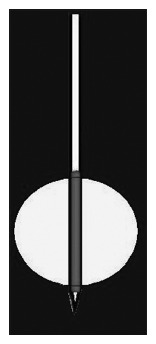
Needle with single electrode. Single electrode of the needle within the lesion.
Both types of expandable needle are used to produce a spherical/ovoid necrotic area, with a mean diameter ranging from 2 to 5/6 cm depending on the needle and electrode degree opening.
On the other hand, when using needles with a single incorporated electrode, the length of the area to be treated depends on the uncovered portion of the electrode, with measurement of the treated area depending on both the length of the uncovered portion and the time of ablation. This type of needle usually produces a cylindrical necrotic area ranging from 1 to 3 cm, depending on the extension of the uncovered metallic portion of the needle.
As previously stated, needle choice and the opening degree of the electrodes are usually influenced by tumor shape and size. For example it is better to use an expendable electrode needle to treat rounded lesions, while single electrode needles are preferred for ovoid lesions. The latter is also preferable in cases of very small lesions with particularly difficult access, as a needle with a lower caliper would be better in that particular situation[4].
With ultrasound it is possible to guide the ablation technique, both during the orientation of the needle and during the opening of the electrodes inside the tumor, which are both echoic. Usually the needle tip and electrodes must be kept almost 5 mm from sensitive structures such as peripancreatic vessels, as previously reported[4,18-20].
The correct needle positioning and electrode opening are followed by a procedure parameter setting that varies depending on the system used, although the procedure normally lasts from 5 to 10 min.
The power provided to the system directly influences the temperature reached and indirectly affects the treated volume of the lesion. In some cases and with some systems, it is possible to evaluate the tissue impedance that increases with necrosis growth during the procedure. The system shows the temperature at the electrode tip, which includes needles with multiple electrodes, thereby assuring a more uniform distribution of temperature in the treated lesion. Choosing the correct temperature is very important for both treatment aims and to prevent irreparable damage. As a result of the protein denaturation that starts at 50-60 °C, higher temperatures reached during RFA lead to more homogeneous coagulative necrosis, but the use of very high temperatures (usually more than 105 °C) increases the risk of complications without any favorable effects. For this reason, it is better to apply middle range temperatures (mean 90 °C) to avoid complications during RFA ablation of a pancreatic mass. Several studies have confirmed that reducing RFA temperature to about 90 °C led to minimal complications related to the procedure[14,16,21].
The capacity of RFA to successfully treat a tumor is in part limited by two primary characteristics linked to this heating mechanism. The first characteristic is that heating tissue with the electric current used in this process is a self-limiting process, as the desiccation, water vapor, and charring created during the RFA process gradually increase the tissue impedance that limits additional current application and limits temperatures that can be reached in the ablation area. The other characteristic is that heat transfer is moderately slow in most tissues and can differ according to local tissue environment, perfusion, and ventilation[22-24].
In a recently published paper by our institute[8], a percutaneous approach with a single tip needle with a single incorporated electrode and an exposable uncovered portion of the electrode of 17-gauge was used. In this paper, a relatively short burst of the needle is used with power set at low values (30 W) at the beginning of the procedure in order to obtain a progressive low development of coagulative necrosis and thereby allowing for intratumoral heat propagation. With respect to the uncovered portion of the needle, double necrotic volume can be obtain with this techniques thanks to intralesional passive conduction (e.g., exposure of 1.5 cm can provide necrosis of more than 3 cm). This technique is reported to be particularly safe because the heat is conducted inside the neoplastic mass and not outside, which lacks conductive neoplastic tissue. This so-called “thermal diffusivity effect” is strictly related to heat neoplastic conductibility and leads to a necrotic area morphology that is quite perfectly modelled inside each single treated lesion (Figure 1). In this study, we applied a mean radiofrequency application time for every single passage of 3 min 13 s (range: from 30 s to 10 min), with 18 patients having proved unresectable pancreatic ductal adenocarcinoma that was locally advanced without metastases and were subsequently treated with percutaneous RFA. In 16 (93%) of the 18 patients, technical success of the procedure was obtained that was proven via a CT scan. Furthermore, one month after the treatment, a decreased blood value in CA 19.9 marker was observed in 40% of the treated patients.
Ultrasound makes possible to monitor the procedure in real-time, watching the lesion progressively becomes hyperechoic due to the gas produced inside, confirming the thermal effect obtained in the tumor, and monitoring the integrity of the sensitive surrounding structures[4,25].
Carrafiello et al[26] treated with a percutaneous RFA patient with pancreatic metastasis from renal cell carcinoma localized in the body-tail using a percutaneous approach under fluoro-CT guidance with deep sedation of the patient. They utilized a 19-gauge needle electrode (Invatec Miras RC, Brescia, Italy) that usually generates up to 3 cm diameter predetermined zones of necrosis. The RFA procedure lasted 8 min and 35 s and reached temperatures between 80 and 100 °C. Although the patient reported abdominal pain, amylase serum increase, and a little peripancreatic fluid collection as complications, the result of the treatment was that he was free of symptoms without recurrence in the follow-up of 12 mo.
Limmer et al[27], with a CT-guided RFA, ablated an insulinoma localized in the body-tail of a patient under general anesthesia. A 16 G-cooled tip single RFA needle with 3 cm active tip was stepwise advanced into the tumor until the needle tip had reached the center of the tumor. The ablation cycle last 18 min, with the last 3 min without cooling and a maximum energy delivery that ranged from 70 to 130 W. The patient had a minimal peripancreatic inflammatory reaction and was then free of symptoms in 1.5 mo of follow-up.
Wu et al[28] treated, without complications, a gastrinoma in the pancreatic tail of a patient with percutaneous transplenic RFA combined with radioactive 125I seed implantation. The patient was free of symptoms without recurrence in 20 mo of follow-up.
Singh et al[29] treated a patient with ductal adenocarcinoma via a CT guided percutaneous approach (the other 10 patients included in the study were treated with the surgical approach), putting the needle in the center of the tumor, and applying approximately 4200 W of energy to the tumor using a saline perfused needle with the aim of producing a necrosis of 3 cm. Partial necrosis (up to 3 cm) of the tumor was achieved in all cases. One patient died 1 mo after RFA due to massive myocardial infarction. Survival of remaining 10 patients ranged between 9 to 36 mo, with 8 patients receiving post-RFA chemotherapy. The authors concluded that RFA is a safe and feasible technique for tumor cytoreduction, but did not specify if the treated patients developed complications such as mild abdominal pain, transient ascites, self-limiting pleural effusion, or asymptomatic pseudocyst. Furthermore, they did not specify the follow-up length or medial survival.
Rossi et al[30] treated 8 patients under local anesthesia (7 with percutaneous RFA and 1 with endoscopic RFA) with neuroendocrine tumors (6 in the head and 2 in the body-tail; 5 with non-functional neuroendocrine tumors, 2 with insulinomas, and 1 with gastrinoma). The 19-gauge single-spiral electrode was inserted under US guidance, with the tip in the center of the tumor. The RF generator was activated to deliver 20 to 50 W for 6 to 12 min. This maneuver was repeated 1 to 4 times, depending on the tumor size. Although the same technique was used with the 17-gauge triple-spiral electrodes, a single 60-degree rotation of the shaft was sufficient to ensure full circumference ablation of the tumor. Three patients developed acute pancreatitis with fluid collections. After a median follow-up of 34 mo, all treated patients were alive and in good condition. The authors concluded that RFA is a feasible, safe, and effective option for patients with small pancreatic neuroendocrine tumors who cannot or do not wish to undergo surgical resection. A short summary of these studies is shown in Table 1.
Table 1.
Summary of studies concerning radiofrequency ablation
| Authors | Number of patients | Lesion type | Location | Treatment type | Approach | Needle | Mean treatment duration | Conclusion |
| D’Onofrio et al[8] | 18 | Pancreatic ductal adenocarcinoma | Head | Radiofrequency ablation | Percutaneous with US | 17 G | 3 min and 13 s | High success rate, with 40% of cases showing CA 19.9 reduction |
| Carrafiello et al[26] | 1 | Pancreatic metastases from renal cell | Body-tail | Radiofrequency ablation | Percutaneous with CT | 19 G | 8 min and 35 s | RFA is feasible for |
| metastatic lesions at body-tail | ||||||||
| Limmer et al[27] | 1 | Insulinoma | Body-tail | Radiofrequency ablation | Percutaneous with CT | 16 G | 18 min | RFA proved to be a clinically successful |
| procedure | ||||||||
| Wu et al[28] | 1 | Gastrinoma | Tail | Radiofrequency ablation | Percutaneous transplenic with CT | - | - | Percutaneous transplenic RFA is feasible |
| Singh et al[29] | 11 | Pancreatic ductal adenocarcinoma | - | Radiofrequency ablation | 1 percutaneous with CT + 10 laparoscopic | - | - | RFA is a safe and feasible technique of tumor cytoreduction |
| Rossi et al[30] | 8 | Pancreatic neuroendocrine tumors | Head and body-tail | Radiofrequency ablation | Percutaneous with CT | 17 and 19 G | 9 min | RFA is a feasible, safe, and effective option |
US: Ultrasound; CT: Computed tomography; RFA: Radiofrequency ablation.
MWA
Microwave radiation indicates electromagnetic spectrum frequencies ranging from 900 to 2450 MHz that lie between infrared radiation and radio waves. Electromagnetic microwaves heat material by agitating water particles in the surrounding substance, producing friction, heat, and inducing cellular death via coagulation necrosis[31] in a manner nearly identical to that observed in RFA[22]. In some cases, the mechanism of microwave heating may have advantages. Polar molecules (primarily water) continuously realign with the oscillating microwave field, effectively increasing kinetic energy and tissue temperature. Unlike electric currents, microwaves spread throughout biological tissues, including those with a high impedance to electric current[22,32], thereby allowing microwaves to incessantly generate heat in a larger volume of tissue around the antenna[22,33]. Microwave energy can therefore produce faster, hotter, and larger ablation areas in multiple tissues than radiofrequency current, as well as requiring fewer applicators and effective ablative margins, making it easier to obtain.
Systems that can create microwave energy are mainly divided into three types: first-generation systems that lack active antenna cooling and are limited to low power and short durations; second-generation systems with antenna cooling but limited generator power; and third-generation systems with incorporated antenna cooling and high-power generators. Each system is characterized by different combinations of antennae diameter, frequency, generated power, and power loss between the generator and applicator tip. Due to all of these features, system performance can vary a great deal, so it is therefore very important to understand that ablation zone shapes and sizes are created by different time and power associations with a particular system; MWA area volume depends on power applied, design, number of antennae, orientation of antennae, and microwave frequency.
Microwave antenna type affects the size and shape of the ablation area, with many described antennae controlling energy transfer[22,34,35]. Some antennae create an elongated ablation area of up to 6 cm called triaxial antennae, which can burn skin or other structures adjacent to the treated organ; newer antennae, such as modified triaxial antennae or dual slot antennae, therefore create more rounded and forward-weighted heating to treat smaller tumors[22,36,37]. Multiple antennae can be used together to create a larger and more confluent ablation area inside the tumor[22,38,39].
Microwaves systems also differ according to their created frequency, with the best heating typically occurring within 1 cm of the antenna. The potential advantages of MWA over RFA include faster ablations (usually 2-8 min with high-powered systems), higher temperatures without the disadvantages related to electric impedance, less sensitivity to different tissue types, and the ability to create much larger ablation zones if needed[22,32,35,40-42].
Both this ablation technique and radiofrequency ablation can be performed via various different approaches, including percutaneous, endoscopic, laparoscopic, and open surgical methods. Although conscious sedation of the patient is employed in the percutaneous and endoscopic approaches, the other methods use general anesthesia instead. The lesion targeted for treatment is first localized with the computed tomographic guide, although the ultrasound guide is preferred if possible, and then the best suited treatment approach is selected[31]. The tumor is then hit with a thin microwave antenna (14-15-gauge), which is in turn connected to the microwave generator with a coaxial cable and an electromagnetic microwave is released from the exposed, non-insulated portion of the antenna. Each generator is capable of producing 60 W of power at a frequency of 915 MHz. Temperatures reached inside the tumor can be measured with a separately placed thermocouple. MWA can be used in different organs, such as the liver, kidneys, lung, adrenal glands, pancreas, and bone[31,43-46].
The only paper in the literature dedicated to percutaneous MWA is that by Carrafiello et al[47], where 5 patients were treated percutaneously with ductal adenocarcinoma; 2 of the cases suffered from mild pancreatitis, 1 suffered from a pseudocyst, and 1 had pseudoaneurysm of the gastroduodenal artery. In all patients, MW ablation was performed under moderate sedation. The path of the antenna was carefully evaluated on the basis of a preliminary US examination, and was chosen in such a way that the vessels, stomach, and bowel were far from the antenna. The most important evaluation involves prediction of the ablation area on the basis of the antenna position. The end of the antenna features a tip such that the use of an antenna with a 37 mm radiating section results in an ablation zone with a diameter of 37 mm (7 mm on the back of the tip and 30 mm ahead of it), while the use of an antenna with a 20 mm radiating section results in an ablation zone with a diameter of 20 mm (ahead of the tip). The technical success rate was 100%, due to correct positioning of antennae. Improvement in the quality of life was observed in all patients, with none requiring repeat treatment during 9 mo follow-up. The authors concluded that patients had an improved quality of life after treatment, and that MWA appears to be feasible in the palliative treatment of cephalic pancreatic tumors, albeit with precise patient selection owing to the high risk of visceral injury. A short summary concerning this study is shown in Table 2.
Table 2.
Summary of study concerning microwave ablation
| Authors | Number of patients | Lesion | Location | Treatment type | Approach | Needle | Mean treatment duration | Conclusion |
| Carrafiello et al[47] | 5 | Pancreatic ductal adenocarcinoma | Head | Microwave ablation | Percutaneous with US | - | - | Microwave ablation appears to be feasible in palliative treatment |
Cryoablation
In the cryoablation technique, cell death is due to cold temperatures. The death mechanism in this situation differs from that under high temperatures, owing to both intracellular and extracellular ice formation during the freezing process that can result in cellular death; ice formation location and the mechanism of cell death changes with the freezing rate and final tissue temperature. Rapid freezing assists the formation of intracellular ice crystals, which result in cell death due to direct damage to the cell membrane and organelles[22,48]. On the other hand, slow freezing favors extracellular ice crystal formation, with a change of osmolality within the extracellular space consequently leading to cell dehydration and cell death[22,49]. Apoptosis induced by freezing contributes to this process, although this is a role that is poorly understood[22,50]. However, breakdown of the cell membrane with the release of intracellular contents causes cell death. Although the temperature necessary to cause necrosis depends on the cell type and the thermal history of the tissue where the lesion is, the estimated temperature is from -35 °C to -20 °C[22,51,52].
During the process of cryoablation, an “ice ball” is created inside the treated area that is predictive of the ablation area. One of the greatest advantages of this technique is that this expanding ball is extremely well-visualized under ultrasound, CT, and MRI, thereby allowing for more precise monitoring of the ablation area than during heat-based techniques[22].
Systems that generate cryoablation take advantage of the Joule-Thomson theory of expanding gases within a needle-like cryoprobe: argon moves from an internal feed line into an internal expansion chamber, producing a heat sink near the antenna tip that cools the probe to temperatures of -160 °C or less. The heat transfer from the tissue into the cryoprobe is governed by passive thermal diffusion, so cryoablation devices provide no zone of direct or active cooling, thereby differing from RFA or MWA devices, with the result being that the surface area of the cryoprobe limits cooling efficiency; smaller diameters of cryoprobe are usually linked with lower cooling capacity and smaller ablation zones, making the use of several cryoprobes to treat the majority of the tumors indispensable in clinical practice, with high ablation times (usually mean 25-30 min) that are longer than the average times found in microwave or RFA procedures[22].
Furthermore, after the procedure there is a rapid release of cellular debris into the systemic circulation due to ablation area reperfusion, thereby sometimes causing systemic complications, such as cryoshock, that are rare with heat-based ablation[22,53].
The cryoablation technique can be performed percutaneously with ultrasound or a computed tomography guide, although it is most commonly performed intraoperatively under ultrasound guidance. As previously stated, lesions smaller than 3 cm can be treated with a single, centrally-placed probe, although larger tumors require multiple probes or sequential treatments. At 160 °C, the tumor is cooled and the ultrasound guide can monitor the created ice ball inside the entire lesion without compromising local structures. After ice ball creation, the tissue has to slowly thaw to 0 °C, and then a second cycle of freezing is performed after any necessary repositioning of the cryoprobes. As with the RFA technique, it is better to have safety margins of at least 5 mm from major structures[14].
Xu et al[9] enrolled 49 patients with locally advanced pancreatic cancer (12 with liver metastases) that underwent cryosurgery (36 treated percutaneously and 13 treated intraoperatively) combined with 125I seed implantation. The procedure was performed under local anesthesia and under the guidance of ultrasound or CT. Cryoprobe insertion was often carried out via the retroperitoneal approach based on the location of the tumor. Generally, 2 or 3 mm cryoprobes were used, with 2 to 3 probes being used for tumors larger than 3 cm in size (mean tumor size ranged from 2.2-7.1 cm). For liver metastases, simultaneous cryosurgery was performed using additional cryoprobes inserted through the right intercostal space. The procedure consisted of a double cycle of freeze/thaw procedure with an argon gas-based cryosurgical unit (EndoCare, Inc., CA, United States). Each cryoprobe was cooled to -160 °C and the resulting ice ball was monitored with ultrasound until the frozen region encompassed the entire mass of the tumor with a safety margin of at least 0.5 cm. The tissue was then allowed to slowly thaw to 0 °C. A second cycle of freezing/thawing was performed after repositioning the cryoprobes, which were then removed. Of the 36 percutaneously treated patients, 17 received a second course of cryosurgery and 3 underwent a third. The conclusions were that cryosurgery, which is far less invasive than conventional pancreatic resection and associated with a low rate of adverse effects, should be the treatment of choice for patients with locally advanced pancreatic cancer. Furthermore, 125I seed implantation can destroy the residual surviving cancer cells after cryosurgery via a complementary effect that combines both modalities. Complete response was observed in 20.4% of patients, partial response in 38.8% of patients, stable disease in 30.6% of patients, and progressive disease in 10.2% (5/49) of patients during a median follow-up of 18 mo (range of 5-40 mo), with a median survival duration of 16.2 mo.
Li et al[54] used percutaneous cryosurgery to treat 2 neuroendocrine tumors in 2 patients with MEN-1 syndrome. The first insulinoma was treated under CT guidance, where three 1.7 mm diameter cryoprobes were inserted into the tumor localized in the pancreatic tail, with 100% argon applied for 10 min. The target zone was covered by an ice ball and the cycle was repeated. The second lesion was located in the pancreatic head and preventively treated with transarterial embolization, due to its dimensions, followed by cryosurgery under ultrasound guidance. Four 2 mm diameter cryoprobes were placed into the pancreatic head tumor, frozen for 15 min and then rewarmed. All probes were extracted by 3 cm and frozen for a further 15 min. A reduction of blood glucose levels and necrosis were found under CT studies, with improvement in patient quality of life being found in the 3 mo follow-up.
Niu et al[55] treated 67 patients (31 with cryoimmunotherapy and 36 with cryotherapy) with ductal adenocarcinoma. Complications included abdominal distension, nausea, increased amylase serum levels, ascites, abdominal bleeding, fever, a mild decrease in blood platelet count, and an increase of fasting blood glucose levels. The obtained results showed a decreased pain score and a median overall survival that was higher after multiple cryoablations than after a single attempt. A short summary concerning these studies is shown in Table 3.
Table 3.
Summary of studies concerning cryosurgery
| Authors | Number of patients | Lesion | Location | Treatment type | Approach | Needle | Mean treatment duration | Conclusion |
| Xu et al[9] | 49 | Pancreatic ductal adenocarcinoma | - | Cryosurgery | 36 percutaneous with US or CT + 13 intraoperative | 2 or 3 mm | - | Cryosurgery is associated with a low rate of adverse effects |
| Li et al[54] | 2 | Neuroendocrine tumors | Head and tail | Cryosurgery | Percutaneous with US and CT | 1.7 mm and 2 mm | 10 and 15 min | Percutaneous cryosurgery is minimally invasive and |
| has advantages compared with conventional surgery | ||||||||
| Niu et al[55] | 67 | Pancreatic ductal adenocarcinoma | - | Cryosurgery | Percutaneous with US and CT | 1.7 mm | - | Cryoimmunotherapy significantly increased overall survival in metastatic |
| pancreatic cancer |
US: Ultrasound; CT: Computed tomography.
IRE
IRE is a non-thermal technique that can be used in the treatment of locally advanced non-metastatic pancreatic adenocarcinoma by inducing cell death. The ablative effect, with its consequential cell death, is based upon the use of a short high-voltage electric current. The application of these short high-voltage electric pulses, guided by one or more monopolar electrodes placed within the lesion, causes irreversible permeabilization of lipid membranes, leading to the disruption of cellular homeostasis and the switching on of apoptotic pathways, thereby resulting in the cell death of neoplastic cells[56-63]. IRE can be performed both during surgery and percutaneously.
This emerging non-thermal ablative technique uses electrodes placed within the targeted lesion in order to deliver up to 3 kV of direct current, thereby inducing the formation of nanoscale pores within the cell membrane, irreversibly damaging the cell homeostatic mechanism, and causing apoptosis[14].
One of the positive features of IRE that separates it from RFA is the ability to preserve surrounding structures, such as the underlying tissue and the vital surrounding structures such as nerves or vessels[56,64-66]. This ability of IRE of preserve vessels could be a very important aspect for evaluation in cases of tumors that encase major peripancreatic vessels.
However, this treatment is not a “pure” non-thermal technique, as it could cause partial cellular damage in a thermal manner and, in some conditions of high intensity, the current applied can produce coagulative necrosis similar to those produced by thermal techniques such as RFA or MWA[56,67]. Other studies have concluded that IRE does not produce significant thermal energy, at least when using settings most commonly applied in clinical treatment, but it has been shown that the presence of a metallic stent could increase the risk of producing thermal injuries, due to metal conductivity[56,68]. This aspect is therefore fundamental to keep in mind when treating patients who are carrying a biliary metallic stent for jaundice palliation.
The planning of IRE treatment has extreme importance. Several tools can be used to help select the best treatment plan and, as shown in some papers, can also accurately describe the procedure under ideal settings in cases of pancreatic tumor treatment[56,69,70].
One of the greatest restrictions of IRE is the need for general anesthesia with complete muscular paralysis[71]. Bagla et al[72] described a case report of percutaneous ablation of a pancreatic cancer in the body-tail, planned and performed as two ablative sessions in order to avoid the need for more than six probes to be placed at once. The treatment was performed with four 15 cm monopolar probes (NanoKnife; AngioDynamics, Latham, New York, United States) placed into the central and lateral aspects of the tumor under ultrasound guidance in a square configuration, with an average spacing of 1.8 cm. CT imaging with contrast medium was then performed to evaluate needle position relative to vessels and measure inter-probe distance. A 22-gauge spinal needle (Becton Dickinson, Franklin Lakes, New Jersey) was placed under US guidance into the gastrohepatic space to perform hydrodissection with sterile water. The treatment had no complications and patients suffered no recurrence upon a 6 mo follow-up. The authors concluded that percutaneous IRE showed promise as a feasible and potentially safe method for local tumor control in patients with surgically unresectable disease.
Martin et al[73] described 27 pancreatic cancer patients (15 in the head and 12 in the body-tail), of whom 26 were treated with surgical IRE and 1 with percutaneous IRE. IRE was performed via the NanoKnife system (AngioDynamics, Latham, New York, United States). Two monopolar probes with 2 cm spacing delivered electroporation defect of approximately 3.5 cm axial, 2.5 cm anterior-posterior, and 2.5 cm cranial-caudal. This electroporation defect was achieved through a maximum of 1.5 cm exposure, 1500 volts/cm, and with 100 microsecond wavelength. No specific complications occurred to the percutaneously-treated patient among hematologic disorders, ileus, bile leak, portal vein thrombosis, deep venous thrombosis, pulmonary infections, renal failure, ascites, and wound infection. The authors concluded that IRE ablation of locally advanced pancreatic adenocarcinoma is safe and feasible as a primary local treatment in unresectable locally advanced disease.
In a 2012 paper, Narayanan et al[10] treated 14 cases of ductal adenocarcinoma (6 in the head, 1 in uncinated process, and 7 in body-tail) using the NanoKnife IRE device (AngioDynamics, Latham, New York, United States). The IRE was set up to produce 70-microsecond high-voltage (1500-3000 V) direct current (25-45 A) electrical pulses. Unipolar electrodes were more commonly used, and the maximum separation between the electrodes was 2.2 cm. No tissue separation maneuvers were used to protect structures adjacent to the IRE electrodes. The electrodes were advanced percutaneously under CT guidance. Bipolar probes were positioned within and around the tumor, and current was applied when CT had confirmed adequate position. The generator was programmed to stop delivery and recharge if the current flow exceeded 48 A. Pull-back was performed if the target treatment zone was greater than 2 cm, and treatment was repeated to cover the entire target. As the only complications encountered were 1 case of pancreatitis and 1 case of pneumothorax during anesthesia, the authors concluded that percutaneous IRE for pancreatic adenocarcinoma is feasible and safe. 1 patient was retreated owing to local disease progression after 7 mo. Due to downstaging, two patients had to receive surgery. The median event-free survival after the IRE procedure was 6.7. The 6 mo overall survival was 70%.
Månsson et al[11] included 24 patients in their study who had locally advanced pancreatic cancer (19 in the head and 5 in the body-tail), prior chemotherapy and/or radiochemotherapy, and underwent percutaneous IRE. NanoKnife IRE equipment from AngioDynamics (Latham, New York, United States) was used. In all patients, the ultrasound-guided needle placement outlined the tumor, with a needle also placed in the center of the tumor when the tumor diameter exceeded 2.0 cm. The electrical parameters were calculated by the machine in order to compensate for any error in the assessment of needle distance. Six needles were used in twenty patients, four needles in two patients, and three needles in the remaining two patients. The active needle length was 1.5 cm in all cases. A minimum of 90 pulses was delivered between each adequate needle pair, which was defined as the distance between the needles not exceeding 2.5 cm. After completion of the treatment cycles in the deep portions of the tumors, the needles were pulled back 1.5 cm and another treatment with the same parameters was performed in the superficial portion of the tumor. In 11 patients, IRE-related complications were observed (infections and thrombosis), of which 3 were serious. There was no IRE-related mortality. Recurrence occurred in 9 patients. The overall survival was 17.9 mo. The authors concluded that percutaneous IRE after chemotherapy/radiochemotherapy appears reasonably safe and shows promising results with regards to efficacy. A short summary of the results is given in Table 4.
Table 4.
Summary of studies concerning irreversible ablation
| Authors | Number of patients | Lesion | Location | Treatment type | Approach | Needle | Mean treatment duration | Conclusion |
| Bagla et al[72] | 1 | Pancreatic ductal adenocarcinoma | Body-tail | Irreversible electroporation | Percutaneous with US and CT | 22 G | - | Percutaneous IRE showed promise as a feasible and potentially safe method for unresectable tumor |
| Martin et al[73] | 27 | Pancreatic ductal adenocarcinoma | 15 head + 12 body-tail | Irreversible electroporation | 1 percutaneous + 26 surgical | - | - | IRE ablation is safe and feasible as a primary local treatment in unresectable locally advanced disease |
| Narayanan et al[10] | 14 | Pancreatic ductal adenocarcinoma | 6 head + 1 uncinated process + 7 body-tail | Irreversible electroporation | Percutaneous with CT | - | - | Percutaneous IRE in pancreatic adenocarcinoma is feasible and safe |
| Månsson et al[11] | 24 | Pancreatic ductal adenocarcinoma | 19 head + 5 body-tail | Irreversible electroporation | Percutaneous with US | - | - | Percutaneous IRE is reasonably safe and shows promising results for efficacy |
US: Ultrasound; CT: Computed tomography; IRE: Irreversible electroporation.
POST-OPERATIVE IMAGING AND COMPLICATIONS
The goal of all these treatments is to reduce tumor volume via cytoreduction. In the case of pancreatic treatment, since ductal adenocarcinoma is significantly hypovascular, detection of the created necrotic area with respect to residual viable tumor tissue can be very difficult. A very important difference between RFA of the pancreas and that of the liver is that, in the treatment of pancreatic tumors, the presence of residual viable tumor at the periphery of the treated area is almost always an intrinsic aspect of the procedure, as the necrotic area must be included in the tumor. Additionally, in other thermal ablative procedures, such as MWA and cryoablation, the ablated area has to be kept inside the tumor in order to avoid complications due to thermal energy outside the pancreatic parenchyma. The most important difference among all thermal procedures and IRE is that is possible with IRE to create necrosis throughout the tumor, as opposed to merely inside it, thereby hypothetically destroying all the cells within the lesion in order to eliminate viable tissue borders outside the induced necrosis.
To evaluate the resulting ablated area, dynamic examination after contrast agent injection is usually performed from one month after the procedure, as it is able to detect the intratumoral necrotic area produced by thermal ablation treatment. In our experience, patients treated with percutaneous RFA for pancreatic adenocarcinoma should undergo a CT scan one day after the procedure in order to completely exclude the presence of some complications. If no complications are present, patients should undergo another CT scan one month after the previous scan as part of routine follow-up. If the ablated area results under dynamic CT scan are slightly hyperdense at the basal scan, then they are obviously avascular throughout the dynamic phases, thereby maintaining the same basal density. In particular, while the arterial and venous phases are very important in highlighting vascular complications such as pseudoaneurysms and venous thrombosis, the late phase is vital for showing the ablated area as being better delineated from the enhanced adjacent tissue (Figure 3). The late phase is therefore best for measuring the ablated area.
Figure 3.
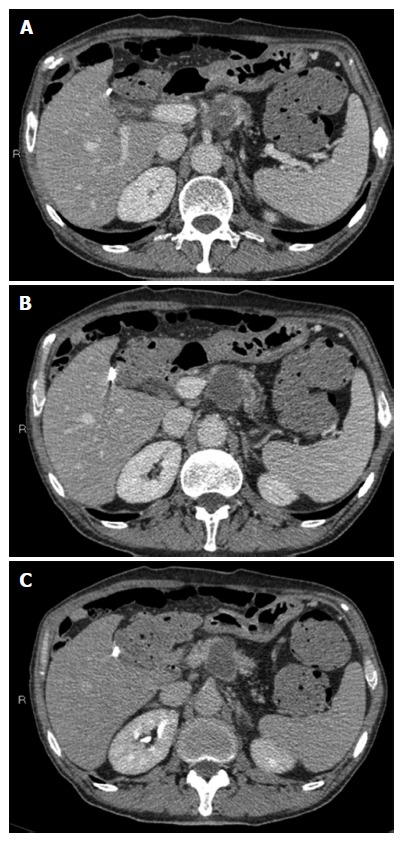
Radiofrequency ablation of pancreatic cancer. Computed tomography (CT) scan in the portal phase (A, B) shows the markedly hypodense necrotic avascular area modelled within the tumor. CT scan in the late phase (C) shows the ablated area as being better delineated from the enhanced adjacent tissue.
Tumor reduction greatly increases the possibility of an improved quality of life and life expectancy, as is possible to reduce the pain caused by pancreatic tumors by causing necrosis within it. Causing cytoreduction also makes it possible to reduce the possibility of rapid disease progression[4,14,54,74-78]. Furthermore, these procedures of creating necrosis inside the tumor can reduce tumor markers and induce an immune response towards the tumor, thereby releasing factors from the tumor that are able to stimulate the immune response and activate host anti-tumor immunity in order to control micrometastases and generate tumor resistance[8,12]. More studies are necessary in order to assess the ability of these treatments to improve life expectancy, as there are currently few in the literature.
Percutaneous pancreatic cancer treatment causes minor complications, including abdominal pain, nausea, fever, skin burn, and fluid collection, as well as major complications such as a comprised splenic vein, portal vein thrombosis, digestive or abdominal bleeding, duodenal perforation, pancreatic fistula, infection, severe pancreatitis, and death.
In our experience of 18 cases of pancreatic adenocarcinoma treated with percutaneous RFA, none of the patients developed intra- or post-procedural complications[8].
CONCLUSION
Currently, ablation procedures are combined with chemotherapy for the treatment of pancreatic cancer. The percutaneous approach is one of the reported possible routes to guarantee minimal invasiveness.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: There is no conflict of interest for any of the authors.
Peer-review started: June 27, 2016
First decision: September 5, 2016
Article in press: October 19, 2016
P- Reviewer: Kleeff J S- Editor: Yu J L- Editor: Rutherford A E- Editor: Zhang FF
References
- 1.Schima W, Ba-Ssalamah A, Kölblinger C, Kulinna-Cosentini C, Puespoek A, Götzinger P. Pancreatic adenocarcinoma. Eur Radiol. 2007;17:638–649. doi: 10.1007/s00330-006-0435-7. [DOI] [PubMed] [Google Scholar]
- 2.Cubilla AL, Fitzgerald PJ. Tumors of the exocrine pancreas. In: Atlas of Tumor Pathology., editor. 2nd series, fascicle 19. Washington, DC: Armed Forces Institute of Pathology; 1984. pp. 98–108. [Google Scholar]
- 3.O’Connor TP, Wade TP, Sunwoo YC, Reimers HJ, Palmer DC, Silverberg AB, Johnson FE. Small cell undifferentiated carcinoma of the pancreas. Report of a patient with tumor marker studies. Cancer. 1992;70:1514–1519. doi: 10.1002/1097-0142(19920915)70:6<1514::aid-cncr2820700612>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 4.D’Onofrio M, Barbi E, Girelli R, Martone E, Gallotti A, Salvia R, Martini PT, Bassi C, Pederzoli P, Pozzi Mucelli R. Radiofrequency ablation of locally advanced pancreatic adenocarcinoma: an overview. World J Gastroenterol. 2010;16:3478–3483. doi: 10.3748/wjg.v16.i28.3478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Stasio GD, Mansi L. Mirko D’Onofrio, Paola Capelli and Paolo Pederzoli (Eds) Imaging and Pathology of Pancreatic Neoplasms. A Pictorial Atlas : Springer-Verlag Italia, 2015 ISBN 978-88-470-5677-0. Eur J Nucl Med Mol Imaging. 2016;43:1568. [Google Scholar]
- 6.Sahani DV, Shah ZK, Catalano OA, Boland GW, Brugge WR. Radiology of pancreatic adenocarcinoma: current status of imaging. J Gastroenterol Hepatol. 2008;23:23–33. doi: 10.1111/j.1440-1746.2007.05117.x. [DOI] [PubMed] [Google Scholar]
- 7.Hermanek P. Staging of exocrine pancreatic carcinoma. Eur J Surg Oncol. 1991;17:167–172. [PubMed] [Google Scholar]
- 8.D’Onofrio M, Crosara S, De Robertis R, Butturini G, Salvia R, Paiella S, Bassi C, Pozzi Mucelli R. Percutaneous Radiofrequency Ablation of Unresectable Locally Advanced Pancreatic Cancer: Preliminary Results. Technol Cancer Res Treat. 2016 doi: 10.1177/1533034616649292. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu KC, Niu LZ, Hu YZ, He WB, He YS, Li YF, Zuo JS. A pilot study on combination of cryosurgery and (125)iodine seed implantation for treatment of locally advanced pancreatic cancer. World J Gastroenterol. 2008;14:1603–1611. doi: 10.3748/wjg.14.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Narayanan G, Hosein PJ, Arora G, Barbery KJ, Froud T, Livingstone AS, Franceschi D, Rocha Lima CM, Yrizarry J. Percutaneous irreversible electroporation for downstaging and control of unresectable pancreatic adenocarcinoma. J Vasc Interv Radiol. 2012;23:1613–1621. doi: 10.1016/j.jvir.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 11.Månsson C, Brahmstaedt R, Nilsson A, Nygren P, Karlson BM. Percutaneous irreversible electroporation for treatment of locally advanced pancreatic cancer following chemotherapy or radiochemotherapy. Eur J Surg Oncol. 2016;42:1401–1406. doi: 10.1016/j.ejso.2016.01.024. [DOI] [PubMed] [Google Scholar]
- 12.D’Onofrio M, Barbi E, Girelli R, Tinazzi Martini P, De Robertis R, Ciaravino V, Salvia R, Butturini G, Frigerio I, Milazzo T, et al. Variation of tumoral marker after radiofrequency ablation of pancreatic adenocarcinoma. J Gastrointest Oncol. 2016;7:213–220. doi: 10.3978/j.issn.2078-6891.2015.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dromi SA, Walsh MP, Herby S, Traughber B, Xie J, Sharma KV, Sekhar KP, Luk A, Liewehr DJ, Dreher MR, et al. Radiofrequency ablation induces antigen-presenting cell infiltration and amplification of weak tumor-induced immunity. Radiology. 2009;251:58–66. doi: 10.1148/radiol.2511072175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keane MG, Bramis K, Pereira SP, Fusai GK. Systematic review of novel ablative methods in locally advanced pancreatic cancer. World J Gastroenterol. 2014;20:2267–2278. doi: 10.3748/wjg.v20.i9.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19:329–338. doi: 10.1055/s-2007-1007122. [DOI] [PubMed] [Google Scholar]
- 16.Girelli R, Frigerio I, Salvia R, Barbi E, Tinazzi Martini P, Bassi C. Feasibility and safety of radiofrequency ablation for locally advanced pancreatic cancer. Br J Surg. 2010;97:220–225. doi: 10.1002/bjs.6800. [DOI] [PubMed] [Google Scholar]
- 17.Siriwardena AK. Radiofrequency ablation for locally advanced cancer of the pancreas. JOP. 2006;7:1–4. [PubMed] [Google Scholar]
- 18.Wu Y, Tang Z, Fang H, Gao S, Chen J, Wang Y, Yan H. High operative risk of cool-tip radiofrequency ablation for unresectable pancreatic head cancer. J Surg Oncol. 2006;94:392–395. doi: 10.1002/jso.20580. [DOI] [PubMed] [Google Scholar]
- 19.Ng KK, Lam CM, Poon RT. Portal vein thrombosis after radiofrequency ablation for recurrent hepatocellular carcinoma. Asian J Surg. 2013;26:50–54. doi: 10.1016/S1015-9584(09)60218-9. [DOI] [PubMed] [Google Scholar]
- 20.Ng KK, Lam CM, Poon RT, Shek TW, Fan ST, Wong J. Delayed portal vein thrombosis after experimental radiofrequency ablation near the main portal vein. Br J Surg. 2004;91:632–639. doi: 10.1002/bjs.4500. [DOI] [PubMed] [Google Scholar]
- 21.Date RS, McMahon RF, Siriwardena AK. Radiofrequency ablation of the pancreas. I: Definition of optimal thermal kinetic parameters and the effect of simulated portal venous circulation in an ex-vivo porcine model. JOP. 2005;6:581–587. [PubMed] [Google Scholar]
- 22.Hinshaw JL, Lubner MG, Ziemlewicz TJ, Lee FT, Brace CL. Percutaneous tumor ablation tools: microwave, radiofrequency, or cryoablation--what should you use and why? Radiographics. 2014;34:1344–1362. doi: 10.1148/rg.345140054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed M, Liu Z, Humphries S, Goldberg SN. Computer modeling of the combined effects of perfusion, electrical conductivity, and thermal conductivity on tissue heating patterns in radiofrequency tumor ablation. Int J Hyperthermia. 2008;24:577–588. doi: 10.1080/02656730802192661. [DOI] [PubMed] [Google Scholar]
- 24.Liu Z, Ahmed M, Weinstein Y, Yi M, Mahajan RL, Goldberg SN. Characterization of the RF ablation-induced “oven effect”: the importance of background tissue thermal conductivity on tissue heating. Int J Hyperthermia. 2006;22:327–342. doi: 10.1080/02656730600609122. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD, Dupuy DE, Gervais DA, Gillams AR, Kane RA, Lee FT, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2009;20:S377–S390. doi: 10.1016/j.jvir.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Carrafiello G, Laganà D, Recaldini C, Dionigi G, Boni L, Bacuzzi A, Fugazzola C. Radiofrequency ablation of a pancreatic metastasis from renal cell carcinoma: case report. Surg Laparosc Endosc Percutan Tech. 2008;18:64–66. doi: 10.1097/SLE.0b013e3181592a13. [DOI] [PubMed] [Google Scholar]
- 27.Limmer S, Huppert PE, Juette V, Lenhart A, Welte M, Wietholtz H. Radiofrequency ablation of solitary pancreatic insulinoma in a patient with episodes of severe hypoglycemia. Eur J Gastroenterol Hepatol. 2009;21:1097–1101. doi: 10.1097/meg.0b013e328323d70e. [DOI] [PubMed] [Google Scholar]
- 28.Wu PH, Pan CC, Huang ZL, Li W, Zhao M, Zhou ZW. Percutaneous radiofrequency ablation approach through the spleen: initial case report for pancreatic tail gastrinoma. Chin J Cancer. 2010;29:836–841. doi: 10.5732/cjc.009.10755. [DOI] [PubMed] [Google Scholar]
- 29.Singh V, Varshney S, Sewkani A. Radiofrequency ablation of unresectable pancreatic carcinoma: 10-year experience from single centre. Pancreatology. 2011;11 Suppl 1:1–80. [Google Scholar]
- 30.Rossi S, Viera FT, Ghittoni G, Cobianchi L, Rosa LL, Siciliani L, Bortolotto C, Veronese L, Vercelli A, Gallotti A, et al. Radiofrequency ablation of pancreatic neuroendocrine tumors: a pilot study of feasibility, efficacy, and safety. Pancreas. 2014;43:938–945. doi: 10.1097/MPA.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 31.Simon CJ, Dupuy DE, Mayo-Smith WW. Microwave ablation: principles and applications. Radiographics. 2005;25 Suppl 1:S69–S83. doi: 10.1148/rg.25si055501. [DOI] [PubMed] [Google Scholar]
- 32.Brace CL. Radiofrequency and microwave ablation of the liver, lung, kidney, and bone: what are the differences? Curr Probl Diagn Radiol. 2009;38:135–143. doi: 10.1067/j.cpradiol.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andreano A, Brace CL. A comparison of direct heating during radiofrequency and microwave ablation in ex vivo liver. Cardiovasc Intervent Radiol. 2013;36:505–511. doi: 10.1007/s00270-012-0405-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bertram JM, Yang D, Converse MC, Webster JG, Mahvi DM. A review of coaxial-based interstitial antennas for hepatic microwave ablation. Crit Rev Biomed Eng. 2006;34:187–213. doi: 10.1615/critrevbiomedeng.v34.i3.10. [DOI] [PubMed] [Google Scholar]
- 35.Brace CL. Microwave tissue ablation: biophysics, technology, and applications. Crit Rev Biomed Eng. 2010;38:65–78. doi: 10.1615/critrevbiomedeng.v38.i1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang Y, Sun Y, Feng L, Gao Y, Ni X, Liang P. Internally cooled antenna for microwave ablation: results in ex vivo and in vivo porcine livers. Eur J Radiol. 2008;67:357–361. doi: 10.1016/j.ejrad.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 37.Brace CL. Dual-slot antennas for microwave tissue heating: parametric design analysis and experimental validation. Med Phys. 2011;38:4232–4240. doi: 10.1118/1.3601019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laeseke PF, Lee FT, van der Weide DW, Brace CL. Multiple-Antenna Microwave Ablation: Spatially Distributing Power Improves Thermal Profiles and Reduces Invasiveness. J Interv Oncol. 2009;2:65–72. [PMC free article] [PubMed] [Google Scholar]
- 39.Oshima F, Yamakado K, Nakatsuka A, Takaki H, Makita M, Takeda K. Simultaneous microwave ablation using multiple antennas in explanted bovine livers: relationship between ablative zone and antenna. Radiat Med. 2008;26:408–414. doi: 10.1007/s11604-008-0251-x. [DOI] [PubMed] [Google Scholar]
- 40.Lubner MG, Brace CL, Hinshaw JL, Lee FT. Microwave tumor ablation: mechanism of action, clinical results, and devices. J Vasc Interv Radiol. 2010;21:S192–S203. doi: 10.1016/j.jvir.2010.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Knavel EM, Hinshaw JL, Lubner MG, Andreano A, Warner TF, Lee FT, Brace CL. High-powered gas-cooled microwave ablation: shaft cooling creates an effective stick function without altering the ablation zone. AJR Am J Roentgenol. 2012;198:W260–W265. doi: 10.2214/AJR.11.6503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li X, Zhang L, Fan W, Zhao M, Wang L, Tang T, Jiang H, Zhang J, Liu Y. Comparison of microwave ablation and multipolar radiofrequency ablation, both using a pair of internally cooled interstitial applicators: results in ex vivo porcine livers. Int J Hyperthermia. 2011;27:240–248. doi: 10.3109/02656736.2010.536967. [DOI] [PubMed] [Google Scholar]
- 43.Carrafiello G, Laganà D, Mangini M, Fontana F, Dionigi G, Boni L, Rovera F, Cuffari S, Fugazzola C. Microwave tumors ablation: principles, clinical applications and review of preliminary experiences. Int J Surg. 2008;6 Suppl 1:S65–S69. doi: 10.1016/j.ijsu.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 44.Shibata T, Iimuro Y, Yamamoto Y, Maetani Y, Ametani F, Itoh K, Konishi J. Small hepatocellular carcinoma: comparison of radio-frequency ablation and percutaneous microwave coagulation therapy. Radiology. 2002;223:331–337. doi: 10.1148/radiol.2232010775. [DOI] [PubMed] [Google Scholar]
- 45.Seki T, Tamai T, Nakagawa T, Imamura M, Nishimura A, Yamashiki N, Ikeda K, Inoue K. Combination therapy with transcatheter arterial chemoembolization and percutaneous microwave coagulation therapy for hepatocellular carcinoma. Cancer. 2000;89:1245–1251. [PubMed] [Google Scholar]
- 46.Lu MD, Chen JW, Xie XY, Liu L, Huang XQ, Liang LJ, Huang JF. Hepatocellular carcinoma: US-guided percutaneous microwave coagulation therapy. Radiology. 2001;221:167–172. doi: 10.1148/radiol.2211001783. [DOI] [PubMed] [Google Scholar]
- 47.Carrafiello G, Ierardi AM, Fontana F, Petrillo M, Floridi C, Lucchina N, Cuffari S, Dionigi G, Rotondo A, Fugazzola C. Microwave ablation of pancreatic head cancer: safety and efficacy. J Vasc Interv Radiol. 2013;24:1513–1520. doi: 10.1016/j.jvir.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 48.Rui J, Tatsutani KN, Dahiya R, Rubinsky B. Effect of thermal variables on human breast cancer in cryosurgery. Breast Cancer Res Treat. 1999;53:185–192. doi: 10.1023/a:1006182618414. [DOI] [PubMed] [Google Scholar]
- 49.Hoffmann NE, Bischof JC. The cryobiology of cryosurgical injury. Urology. 2002;60 Suppl 1:S40–S49. doi: 10.1016/s0090-4295(02)01683-7. [DOI] [PubMed] [Google Scholar]
- 50.Gage AA, Baust J. Mechanisms of tissue injury in cryosurgery. Cryobiology. 1998;37:171–186. doi: 10.1006/cryo.1998.2115. [DOI] [PubMed] [Google Scholar]
- 51.Rubinsky B. Cryosurgery. Annu Rev Biomed Eng. 2000;2:157–187. doi: 10.1146/annurev.bioeng.2.1.157. [DOI] [PubMed] [Google Scholar]
- 52.Rubinsky B, Lee CY, Bastacky J, Onik G. The process of freezing and the mechanism of damage during hepatic cryosurgery. Cryobiology. 1990;27:85–97. doi: 10.1016/0011-2240(90)90055-9. [DOI] [PubMed] [Google Scholar]
- 53.Chapman WC, Debelak JP, Wright Pinson C, Washington MK, Atkinson JB, Venkatakrishnan A, Blackwell TS, Christman JW. Hepatic cryoablation, but not radiofrequency ablation, results in lung inflammation. Ann Surg. 2000;231:752–761. doi: 10.1097/00000658-200005000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li J, Zhang C, Chen J, Yao F, Zeng J, Huang L, Yang X, Liu W, Chen F, Xu K, et al. Two case reports of pilot percutaneous cryosurgery in familial multiple endocrine neoplasia type 1. Pancreas. 2013;42:353–357. doi: 10.1097/MPA.0b013e318258f233. [DOI] [PubMed] [Google Scholar]
- 55.Niu L, Chen J, He L, Liao M, Yuan Y, Zeng J, Li J, Zuo J, Xu K. Combination treatment with comprehensive cryoablation and immunotherapy in metastatic pancreatic cancer. Pancreas. 2013;42:1143–1149. doi: 10.1097/MPA.0b013e3182965dde. [DOI] [PubMed] [Google Scholar]
- 56.Paiella S, Salvia R, Ramera M, Girelli R, Frigerio I, Giardino A, Allegrini V, Bassi C. Local Ablative Strategies for Ductal Pancreatic Cancer (Radiofrequency Ablation, Irreversible Electroporation): A Review. Gastroenterol Res Pract. 2016;2016:4508376. doi: 10.1155/2016/4508376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rubinsky B, Onik G, Mikus P. Irreversible electroporation: a new ablation modality--clinical implications. Technol Cancer Res Treat. 2007;6:37–48. doi: 10.1177/153303460700600106. [DOI] [PubMed] [Google Scholar]
- 58.Davalos RV, MirLM, Rubinsky B. Tissue ablation with irreversible electroporation. Ann Biom Enge. 2005;33:223–231. doi: 10.1007/s10439-005-8981-8. [DOI] [PubMed] [Google Scholar]
- 59.Al-Sakere B, André F, Bernat C, Connault E, Opolon P, Davalos RV, Rubinsky B, Mir LM. Tumor ablation with irreversible electroporation. PLoS One. 2007;2:e1135. doi: 10.1371/journal.pone.0001135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang Z, Li W, Procissi D, Tyler P, Omary RA, Larson AC. Rapid dramatic alterations to the tumor microstructure in pancreatic cancer following irreversible electroporation ablation. Nanomedicine (Lond) 2014;9:1181–1192. doi: 10.2217/nnm.13.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee EW, Wong D, Prikhodko SV, Perez A, Tran C, Loh CT, Kee ST. Electron microscopic demonstration and evaluation of irreversible electroporation-induced nanopores on hepatocyte membranes. J Vasc Interv Radiol. 2012;23:107–113. doi: 10.1016/j.jvir.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 62.Yarmush ML, Golberg A, Serša G, Kotnik T, Miklavčič D. Electroporation-based technologies for medicine: principles, applications, and challenges. Annu Rev Biomed Eng. 2014;16:295–320. doi: 10.1146/annurev-bioeng-071813-104622. [DOI] [PubMed] [Google Scholar]
- 63.Golberg A, Yarmush ML. Nonthermal irreversible electroporation: fundamentals, applications, and challenges. IEEE Trans Biomed Eng. 2013;60:707–714. doi: 10.1109/TBME.2013.2238672. [DOI] [PubMed] [Google Scholar]
- 64.Maor E, Ivorra A, Leor J, Rubinsky B. Irreversible electroporation attenuates neointimal formation after angioplasty. IEEE Trans Biomed Eng. 2008;55:2268–2274. doi: 10.1109/TBME.2008.923909. [DOI] [PubMed] [Google Scholar]
- 65.Maor E, Ivorra A, Rubinsky B. Intravascular irreversible electroporation: theoretical and experimental feasibility study. IEEE Engin Med Biol Society. 2008:2051–2054. doi: 10.1109/IEMBS.2008.4649595. [DOI] [PubMed] [Google Scholar]
- 66.Schoellnast H, Monette S, Ezell PC, Deodhar A, Maybody M, Erinjeri JP, Stubblefield MD, Single GW, Hamilton WC, Solomon SB. Acute and subacute effects of irreversible electroporation on nerves: experimental study in a pig model. Radiology. 2011;260:421–427. doi: 10.1148/radiol.11103505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Faroja M, Ahmed M, Appelbaum L, Ben-David E, Moussa M, Sosna J, Nissenbaum I, Goldberg SN. Irreversible electroporation ablation: is all the damage nonthermal? Radiology. 2013;266:462–470. doi: 10.1148/radiol.12120609. [DOI] [PubMed] [Google Scholar]
- 68.Dunki-Jacobs EM, Philips P, Martin RC. Evaluation of thermal injury to liver, pancreas and kidney during irreversible electroporation in an in vivo experimental model. Br J Surg. 2014;101:1113–1121. doi: 10.1002/bjs.9536. [DOI] [PubMed] [Google Scholar]
- 69.Martin RC. Irreversible electroporation of locally advanced pancreatic head adenocarcinoma. J Gastrointest Surg. 2013;17:1850–1856. doi: 10.1007/s11605-013-2309-z. [DOI] [PubMed] [Google Scholar]
- 70.Martin RC, Philips P, Ellis S, Hayes D, Bagla S. Irreversible electroporation of unresectable soft tissue tumors with vascular invasion: effective palliation. BMC Cancer. 2014;14:540. doi: 10.1186/1471-2407-14-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thomson KR, Kavnoudias H, Neal RE. Introduction to Irreversible Electroporation--Principles and Techniques. Tech Vasc Interv Radiol. 2015;18:128–134. doi: 10.1053/j.tvir.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 72.Bagla S, Papadouris D. Percutaneous irreversible electroporation of surgically unresectable pancreatic cancer: a case report. J Vasc Interv Radiol. 2012;23:142–145. doi: 10.1016/j.jvir.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 73.Martin RC, McFarland K, Ellis S, Velanovich V. Irreversible electroporation therapy in the management of locally advanced pancreatic adenocarcinoma. J Am Coll Surg. 2012;215:361–369. doi: 10.1016/j.jamcollsurg.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 74.Linecker M, Pfammatter T, Kambakamba P, DeOliveira ML. Ablation Strategies for Locally Advanced Pancreatic Cancer. Dig Surg. 2016;33:351–359. doi: 10.1159/000445021. [DOI] [PubMed] [Google Scholar]
- 75.Weiss MJ, Wolfgang CL. Irreversible electroporation: a novel pancreatic cancer therapy. Curr Probl Cancer. 2013;37:262–265. doi: 10.1016/j.currproblcancer.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 76.Niu L, He L, Zhou L, Mu F, Wu B, Li H, Yang Z, Zuo J, Xu K. Percutaneous ultrasonography and computed tomography guided pancreatic cryoablation: feasibility and safety assessment. Cryobiology. 2012;65:301–307. doi: 10.1016/j.cryobiol.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 77.Spiliotis JD, Datsis AC, Michalopoulos NV, Kekelos SP, Vaxevanidou A, Rogdakis AG, Christopoulou AN. Radiofrequency ablation combined with palliative surgery may prolong survival of patients with advanced cancer of the pancreas. Langenbecks Arch Surg. 2007;392:55–60. doi: 10.1007/s00423-006-0098-5. [DOI] [PubMed] [Google Scholar]
- 78.Rombouts SJ, Vogel JA, van Santvoort HC, van Lienden KP, van Hillegersberg R, Busch OR, Besselink MG, Molenaar IQ. Systematic review of innovative ablative therapies for the treatment of locally advanced pancreatic cancer. Br J Surg. 2015;102:182–193. doi: 10.1002/bjs.9716. [DOI] [PubMed] [Google Scholar]


