Abstract
Objective. This is a review of spiritually based interventions (eg, mindfulness-based stress reduction) that utilized psychoneuroimmunological (PNI) outcome measures in breast cancer survivors. Specifically, this review sought to examine the evidence regarding relationships between spiritually based interventions, psychosocial-spiritual outcomes, and biomarker outcomes in breast cancer survivors. Methods. A systematic search of 9 online databases was conducted for articles of original research, peer-reviewed, randomized and nonrandomized control trials from 2005-2015. Data were extracted in order to answer selected questions regarding relationships between psychosocial-spiritual and physiological measures utilized in spiritually based interventions. Implications for future spiritually based interventions in breast cancer survivorship are discussed. Results. Twenty-two articles were reviewed. Cortisol was the most common PNI biomarker outcome studied. Compared with control groups, intervention groups demonstrated positive mental health outcomes and improved or stable neuroendocrine-immune profiles, although limitations exist. Design methods have improved with regard to increased use of comparison groups compared with previous reviews. There are few spiritually based interventions that specifically measure religious or spiritual constructs. Similarly, there are few existing studies that utilize standardized religious or spiritual measures with PNI outcome measures. Findings suggest that a body of knowledge now exists in support of interventions with mindfulness-breathing-stretching components; furthermore, these interventions appear to offer potential improvement or stabilization of neuroendocrine-immune activity in breast cancer survivors compared to control groups. Conclusion. From a PNI perspective, future spiritually based interventions should include standardized measures of religiousness and spirituality in order to understand relationships between and among religiousness, spirituality, and neuroendocrine-immune outcomes. Future research should now focus on determining the minimum dose and duration needed to improve or stabilize neuroendocrine-immune function, as well as diverse setting needs, including home-based practice for survivors who are too ill to travel to group sessions or lack economic resources.
Keywords: breast cancer, interventions, oncology, psychoneuroimmunology, religious, review, spirituality
Introduction
Despite the vast amount of research that has been conducted in breast cancer, the extended survivorship trajectory for breast cancer survivors remains unpredictable and complicated by breast cancer recurrence or treatment-related physical effects (ie, secondary lymphedema).1 The incidence of secondary lymphedema in breast cancer survivors ranges from 6% to 94% and is associated with a lifetime risk.2 Because of these posttreatment late effects, as many as 30% of breast cancer survivors have reported physical function decline, poorer mental health, social difficulties, and a poorer quality of life.3-5 When considering interventions appropriate for symptom management in breast cancer survivorship, it is recognized that breast cancer survivors are now an aging population with multifaceted problems beyond physiological symptoms, including economic, psychosocial, and spiritual stress.6-8
According to Pew Forum Research data, 92% of Americans believe in God or a higher power and 56% report religion is very important in their lives.9 Previous research has shown that older adults rely on religious practices (ie, prayer) while seeking treatment for chronic symptoms.10 To cope with chronic physical and psychological symptoms, studies have shown that 80% to 90% of breast cancer survivors report using spiritually based complementary and alternative medicine (CAM) therapies (eg, mindfulness, meditation, yoga, Tai Chi, Qigong, guided imagery, and affirmations) to manage long-term breast cancer treatment–related symptoms.11-15
Religious coping has shown an association with spiritual growth, better mental health, and positive outcomes following stressful life events.16,17 Studies of chronically ill populations, including breast cancer survivors, have reported that religious and spiritual factors (eg, relationship with God/higher power, prayer, and congregational/social support) are used for comfort and coping with cancer survivorship experiences.10,18,19 In the past 10 years, a number of CAM interventions have been conducted in breast cancer populations to examine changes in psychological and physiological outcomes in those receiving the interventions.20,21 Although many of these CAM interventions (eg, mindfulness-based interventions and Qigong) had a spiritual component, the relationships between the spiritual basis of these interventions and health outcomes have remained unclear. Moreover, previous data suggest that religious and spiritual variables influence mental health outcomes; however, a gap exists in the psychoneuroimmunological (PNI) research regarding the evidence linking religious and spiritual variables and physiological health outcomes.
The purpose of this article is to review PNI-based interventions for health outcomes associated with religious and spiritually based interventions in breast cancer survivors. Despite numerous CAM interventions reported in the breast cancer literature, there remain few reported findings regarding the relationships between religious and spiritual variables and neuroimmune function changes associated with these religious and spiritual interventions. This article is divided into 2 sections: (1) An overview of the relationships between and among religious and spiritual variables related to health outcomes and (2) a systematic review of spiritually based interventions with PNI health outcomes in breast cancer survivors.
Literature Review
Religious and Spiritual Variables Related to Health
Many terms have been used to describe spirituality for health research purposes including meaning, purpose in life, the mystical, the numinous, hope, value, optimism, emotional connectedness, transcendence, gratitude, and forgiveness.22-24 Religious and spirituality researchers have conceptualized spirituality based on their own cultural and philosophical traditions that may have either a religious or a secular basis.25,26 Consequently, the constructs of religiousness and spirituality have been difficult to clarify for health research purposes due to the lack of agreement among contemporary researchers who have viewed the 2 constructs as complex with overlapping aspects (i.e. searching for the sacred).27-29
In general, religion refers to denomination affiliation, religious identity, public religious practice (eg, attendance and group prayer) and specific beliefs in religious tenets (eg, afterlife).22,30 Religious practices are culturally based practices such as prayer, church attendance, meditation, or reading religious texts. Spirituality is viewed as a subjective experience of the sacred and refers to an emotional connectedness or relationship with God or the transcendent beyond the self.31-33 Additionally, recent data suggest that spirituality may be a dimension of personality.23,24
Self-transcendence refers to the ability to stand outside one’s immediate sense of time and place to view life from a larger perspective.24,34 Spiritual self-transcendence is further characterized by recognition that a synchronicity to life exists and fosters a sense of commitment to helping others.35 Three common themes have been represented in the literature regarding spirituality: a relationship with the transcendent and to others, the existence of a higher being, and an appreciation for the greater world.36
Although it has been generally agreed that religion and spirituality are separate constructs, the literature discusses these two constructs as interchangeable; furthermore, religious and spiritual variables have often been denoted as “RS.” Extending from this trend, religious and spirituality research now reflects measures with religious and spiritual construct overlap. It is recognized that there remains a lack of a “gold standard” definition providing separation of religious and spiritual constructs for health care research purposes.25,37 Therefore, for purposes of this discussion and where appropriate, religious and spiritual variables will hereafter be denoted as “RS.”
Spiritual Experiences, Religious Practices, and Congregational Support
Findings from a recent factor analysis of religious measures, spiritual measures, and health outcomes suggested that 3 dimensions represent the religious and spiritual variables related to health outcomes: spiritual experiences (ie, emotional connectedness to the transcendent), religious practices (ie, behaviors), and congregational support (ie, social support).27 Moreover, religious and spiritual dimensions are viewed as separate constructs that can be distinguished as positive and negative (eg, loving God/higher power vs a punishing God/higher power and positive/negative congregational support).27,38,39 Positive spiritual experiences are associated with better physical health in individuals with chronic disabilities, and negative spiritual experiences are associated with worse health. Among religious and spiritual variables, forgiveness appears to be a greater predictor of health outcomes.23
RS Variables and Health Outcomes in Breast Cancer
Observation of breast cancer survivors (n = 763) over 10 years demonstrated that although a diagnosis of cancer was associated with a sense of vulnerability, there was a positive change in survivor participants’ worldview and perceptions of life’s meaning that persisted even 10 years postdiagnosis.40 A growing consensus in the literature has suggested that the presence of a spiritual dimension is an indicator of positive adaptation to cancer treatment and coping with cancer.41,42 Data have also shown that social isolation among women with newly diagnosed breast cancer was associated with higher mortality risk.43 Breast cancer survivors who reported positive perceptions of social support (eg, emotional reassurance, personal assistance, and advice) also demonstrated positive immune system benefits and decreased psychological distress.44,45
Data from breast cancer populations have suggested that increased stress correlates with decreased immune function (ie, natural killer [NK] cell activity and T cell response), resulting in a decreased ability to destroy cancerous tumors.46 Data have also shown that emotional distress experienced by breast cancer survivors correlated with impaired NK cell and cytokine function and further suggested that emotional distress negatively influenced the immune profile of breast cancer survivor participants.47 Pilot data from mindfulness-based interventions have shown that mindfulness exerted a positive influence on NK cell cytotoxicity, cytokine function,48-50 and cortisol patterns.49,51-54 These relationships between psychosocial and RS (eg, mindfulness) variables and health outcomes in populations with immune dysregulation (ie, breast cancer) are consistent with a psychoneuroimmunological (PNI) model of health.
The PNI Model of Health
The PNI model of health seeks to explain causal relationships between and among stress, brain function (ie, mind/thoughts), psycho-social-behavioral components (eg, spirituality), and physiological components (ie, neuroendocrine-immune system interactions).55-57 As stress influences perceptions, the resulting thought processes are then communicated from the brain to the immune system via neuroendocrine and hormonal pathways. The subsequent adaptive immune system response then manifests as a psychological or physiological symptom (ie, mental or physical illness) or health maintenance (ie, wellness).58,59
Psychoneuroimmunological research has established that neuroendocrine-immune function can be studied through measures of biomarker levels obtained in saliva and serum specimens. The 2 primary neuroendocrine-immune pathways associated with stress are the sympathoadrenomedullary (SAM) axis, which includes the sympathetic nervous system (SNS); and the hypothalamic-pituitary-adrenocortical axis (HPAA).60 Chronic stress results in dysregulation of both axes.61 During acute stress the SAM axis activates the SNS to release norepinephrine which induces a “fight or flight” response.62 The HPAA responds by releasing endocrine-based glucocorticoids, primarily in the form of cortisol hormone.63 Repeated activation of the HPAA system results in increased allostatic load and has been shown to cause chronic immunosuppression associated with negative health outcomes.61,64,65 In chronically ill populations, suppressed immune function associated with long-term stress is further associated with increased susceptibility to illness, delayed wound healing, and prolonged recovery from illness.66 After prolonged HPAA vigilance, elevated cortisol activity becomes detrimental, as it becomes immunosuppressive and ultimately contributes to persistent immune dysregulation.58,67
Mindfulness-Based Interventions and Moving Meditations as Spiritually Based Interventions
Among the most commonly reported psychosocial interventions in breast cancer research literature, mindfulness-based interventions (eg, mindfulness-based stress reduction [MBSR] and mindfulness-based cognitive therapies [MBCT]) have become prolific as adjunct treatments for post–cancer treatment–related symptoms.68,69 Traditional forms of MBSR stem from the contemplative, spiritually based Buddhist philosophy, which promotes the development of a nonjudgmental, accepting, and patient worldview and teaches relaxation through focused awareness on breathing.48 MBSR and MBCT interventions use meditation and gentle Yoga stretching to “maintain awareness moment by moment, disengaging oneself from strong attachment to beliefs, thoughts or emotions, and thereby developing a greater sense of emotional balance or well-being.”70(p1350) Similarly, there are other movement-meditative-breathing interventions (eg, Qigong and Tai Chi) that include encourage mindfulness and self-awareness. Since spiritual self-transcendence involves viewing life from a larger perspective beyond the self, mindfulness and meditation practices facilitate spiritual change.24 From this perspective, interventions that encourage mindfulness, meditation, and self-awareness through breath work and movement are viewed as facilitating spiritual transformation.
Relaxation and Visualization Therapy
Relaxation and visualization therapy (RVT) involves the induction of a relaxation using mental imagery of a desired object or outcome and includes progressive muscle relaxation, continued guided imagery, meditation, and deep breathing.71 RVT involves imagery of peaceful scenery and focused sensory awareness on individual muscle groups. RVT has been reported to improve quality of life, mood, reduced social conformity, and enhanced emotional expression.72,73
Guided Imagery
Similar to RVT, guided imagery utilizes progressive relaxation of muscle groups combined with focused breathing techniques intended to calm the mind and prepare it for guided imagery.74 Guided imagery is a consciousness-focused practice intended to increase awareness with a relaxed, open mind for the purpose of confronting a specific concern or issue. Guided imagery is viewed as a way to allow patients to participate in their own healing and has been reportedly used for healing, symptom management, promotion of positive health behaviors, and making positive life changes. Guided imagery also includes aspects involving the “unconscious mind” including intuition, emotions, feelings, memories, values, beliefs, perceptions, and goals.75
Tai Chi
In Western culture, Tai Chi is a moving meditation or a form of low-level exercise, which involves a sequence of fluid, graceful movements, focused breathing, posturing movement, and consciousness directed at relaxation.76,77 However, for some traditions, Tai Chi is a Chinese martial art, a Shamanic religious ritual, an exercise, and a relaxation technique that has been in existence for at least 5000 years.76 The practice of Tai Chi is meant to increase the participant’s mind-body connection through the awareness of the body’s energy and potential for self-healing, resulting in self-empowerment. The meanings of the Tai Chi movements and philosophy are conveyed using the 5 elements (ie, fire, earth, minerals, water, and wood) and seasons of the year to represent (spiritual) transformation.77
Yoga
Yoga is an ancient Eastern traditional mind-body practice.78 Yoga is also considered a moving meditation and consists of breathing exercises, postures, relaxation, and meditation.79 Yoga encourages increased self-awareness and relaxation and has been observed to alter the stress response associated with thoughts and emotions, subsequently reducing psychological distress.79
Qigong
Qigong, also a 5000 year-old Chinese mind-body tradition, conceptualizes health as the result of unimpeded flow of “qi” (ie, energy, spirit or life force) through “gong” (ie, achievement).80,81 The focus of Qigong is the prevention and healing of diseases by harmonizing the mind, body, and spirit.82 Specifically, 4 main components are involved in the stimulation and manipulation of the qi: consciousness, mindful focus on the body, breathing techniques, and specific movements.83 Unlike other moving meditations, Qigong can be practiced internally or externally. In external Qigong practice, a Qigong master may facilitate the clearing of qi blockages or balancing of qi for an individual.83
Given the preceding definitions, mindfulness-based interventions, RVT, guided imagery, Tai Chi, yoga, and Qigong all suggest common themes of mindfulness, self-awareness, and self-transcendence (ie, viewing life from a larger perspective beyond the self).24 Therefore, because these practices involve themes of spirituality and spiritual transformation, they were included in this review and are referred to as spiritually based interventions.
Summary of Previous Spiritually Based Interventions and Health Outcomes
MBSR Interventions and Health Outcomes
Early pilot studies demonstrated that MBSR improves mindfulness,84-86 stress,50,87 mood, and psychological distress.49,84,88 MBSR has been shown to decrease depression and anxiety,89-91 and rumination among breast cancer survivors.92,93 Data have shown that MBSR improved sleep quality,54,85 reduced fatigue,21,54 improved quality of life,52,92 and improved perceptions of life being more meaningful.94 Although 2 studies have reported MBSR improves perceptions of spiritual growth in breast cancer survivors,94,95 few studies have examined relationships between mindfulness-based practices and RS constructs (ie, positive and negative spiritual experiences, congregational support, and religious practices).
A previous meta-analysis and review revealed that the majority of early MBSR studies utilized exploratory, pilot designs, with small samples, varied intervention design, and lacked information regarding intervention therapy protocols.96,97 A more recent meta-analysis of MBSR studies (n = 9) with psychological measures in breast cancer survivors reported that MBSR interventions had a moderate to large effect (d = 0.76) on mental health outcomes.98 In a narrative review of MBSR interventions (n = 43) with PNI measures in heterogeneous cancer populations, Carlson69 noted that strong level 1 evidence offered support that MBSR improved anxiety, quality of life, depression, stress, spiritual growth, and well-being in cancer populations. Moreover, quantitative findings suggested MBSR improved PNI biomarker levels in cancer survivors (ie, decreased inflammatory cytokines and cortisol levels), but relationships remain unclear and the overall evidence was weak.69
Subnis et al99 conducted a systematic review of randomized control trials (RCTs), nonrandomized control trials (non-RCTs), and pretest/posttest designs (n = 24) among heterogeneous cancer populations who received cognitive-behavioral interventions or spiritually based interventions (eg, MBSR, yoga) and the associated PNI-based outcome measures. Analyses revealed that most of the psychosocial measures were measures of negative psychological states, with mood as the most common psychosocial measure of interest (11 of 24 studies) and cortisol as the most common biomarker of interest (11 of 24 studies). Moreover, effectiveness of interventions on PNI outcomes among cancer patients could not be determined due to lack of longitudinal designs, small sample sizes, wide variation in intervention protocols, and lack of adherence data. Finally, the review by Subnis et al99 was one of the first to address the lack of biomarker measures representing the SAM (ie, SNS) response to stress. The majority of PNI studies to date have investigated only the HPAA by using cortisol as a proxy measure of chronic stress.
Qigong and Tai Chi Interventions
In a systematic review of 23 studies (RCT and non-RCT), Chan et al100 reported that Qigong had a statistically significant effect on quality of life, symptom improvement, improved fatigue, improved well-being, and improved immune function. However, the overall quality of studies was ranked as poor in methodology, with 3 studies rated “A” and 9 studies rated as “B” (based on Oxford Centre for Evidence-Based Medicine’s levels of evidence).100,101 Moreover, half of the studies were not peer-reviewed and had numerous methodological flaws, including small sample sizes, lack of randomization designs, and disparities in intervention protocols (eg, duration, dose).100
In a meta-analysis by Zeng et al,102 Qigong (n = 5) and Tai Chi (n = 8) intervention data showed that Qigong did not have a statistically significant effect on depression or anxiety; however, it was associated with improved fatigue (P = .04) and improved quality of life (P = .008). Additionally, both Qigong and Tai Chi intervention data demonstrated reduction of cortisol levels (P < .05) and offered limited, but supportive, data suggesting positive associations with improved C-reactive protein and cytokine function. Zeng et al102 also found limitations in intervention designs and methodologies, as well as limited ability to pool data from multiple studies due to lack of heterogeneity between trials.
Specific RS Interventions
In a meta-analysis of RCTs and non-RCTs, Oh and Kim103 examined interventions (n = 14), including protocol descriptions of religious interventions, spiritual nursing care, spiritual counseling, spiritually focused meditation, and meaning-centered psychotherapy, in heterogeneous cancer patients (n = 889). Analyses of RS intervention data revealed significant effects on spiritual well-being (d = −0.48), meaning of life (d = −0.58), depression (d = −0.62), and anxiety (d = −0.82), as well as supported associations between RS interventions and improved mental health outcomes. However, findings and conclusions were limited by a lack of physiological measures, overlap of religious and spiritual constructs, heterogeneous samples, and varied intervention protocols.103
Gaps in the Literature
Breast cancer survivors report perceived therapeutic benefits from using mindfulness-based (ie, spiritual) practices (ie, MBSR and yoga) to cope with posttreatment sequela, although there has been limited empirical evidence to support how spiritual practices influence physiological outcomes. A major gap in current PNI research is the limitations regarding the evidence linking objective measures of neuroendocrine-immune function (eg, biomarkers) to self-report measures of stress and RS variables (eg, religious and spiritual beliefs). The purpose of this review is to address the following questions:
What psychosocial and RS measures have been used in spiritually based interventions in breast cancer survivors; and what were the associated mental health outcomes?
What PNI outcome measures have been used in spiritually based interventions in breast cancer survivors, and what were the associated physiological biomarker outcomes?
What is the evidence regarding the relationships between and among spiritually based interventions, psychosocial-spiritual outcomes, and PNI-based outcomes in breast cancer survivors?
What are the implications for future research studies regarding spiritually based interventions, measures of RS, and PNI-based outcome measures?
Methods
Articles from 2005 through 2015 were retrieved from the following databases: PubMed, Medline, PsycInfo, PsycArticles, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Academic Search Complete, American Theological Library Association (ATLA) Religion, Educational Resources Information Center (ERIC), and Google Scholar. Additionally, a hand search of peer-reviewed journals with a PNI focus (eg, Brain, Behavior, and Immunity [BBI], Psychoneuroendocrinology, and Psycho-Oncology), an ancestry search of references from selected articles, and a personal library search were done.
Keywords
The keywords search was developed from 6 main categories with related subcategories noted in parentheses: (1) spirituality (spiritual, spirituality, spiritual beliefs, spiritual practices), (2) religious (religious, religion, religiosity, religiousness, religious beliefs, religious practices), (3) cancer (neoplasm, oncology, breast, lymphedema), (4) stress, (5) intervention (spiritual, psychosocial, spiritual healing, spiritual therapies, faith healing, CAM, psychological therapy/therapies, spiritual coping, mind-body-therapies, Qigong, group therapy, mindfulness, and (6) PNI-based measures (biomarkers, immune function, immune system, leukocyte, lymphocyte, cytokines, natural killer cell, interferon-gamma, interleukin, tumor necrosis factor- alpha, cortisol, salivary alpha-amylase, neuroendocrine, neuroimmune, hormonal, and inflammatory/inflammation).
Inclusion Criteria
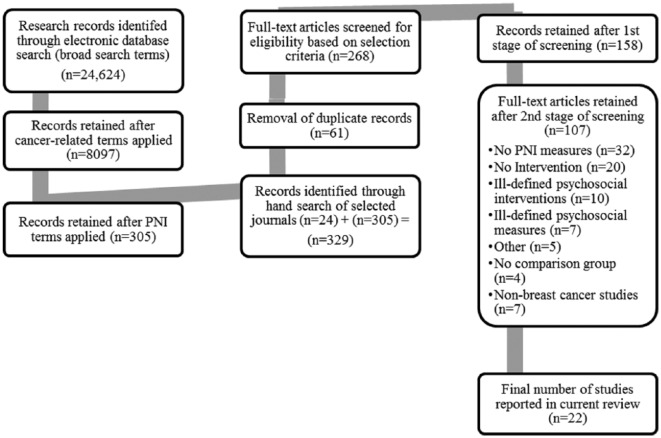
The inclusion criteria included the following: original research in peer-reviewed journals, full-text available online, clearly stated descriptions of samples and methodology, randomized control trials (RCTs), nonrandomized control trials (non-RCTs), human subjects, adults, and articles available in English. The initial search yielded 268 articles. Articles were further screened in several stages. First, titles of articles and abstracts were evaluated based on the inclusion criteria, which resulted in the selection of 158 articles. Next, selected articles were further evaluated by reading the full-text which resulted in 107 articles. Finally, articles were excluded for the following reasons: lack of PNI-based measures (n = 32), lack of RS-based PNI interventions (n = 20), poorly defined or highly customized psychosocial interventions (ie, difficult to replicate based on information provided (n = 10), lack of standardized psychosocial measures (ie, subjective measures) (n = 7), small sample size (n < 10) (n = 3), healthy participant sample (n = 2), and lack of a comparison group (n = 4).
Article Selection
Figure 1 provides a flowchart of the identification, screening, and article selection process, which resulted in 22 articles original articles with RS interventions in breast cancer survivors. Article data selected for extraction and summary included (1) first author and year of publication, (2) study design, (3) cancer stage, (4) sample size of intervention and control groups, (5) type and description of interventions, (6) psychosocial measure data, (7) RS measure data, (8) PNI measures, and (9) conclusion of findings.
Figure 1.
Flowchart of article identification, screening, and selection process.
Results and Discussion
Studies reviewed included RCTs (n = 19) and non-RCTs (n = 3). The majority of studies were from the United States (n = 12), followed by Canada (n = 3), India (n = 2), China (n = 1), Brazil (n = 1), Taiwan (n = 1), Sweden (n = 1), and the United Kingdom (n = 1). Participant sample sizes in the research studies ranged from 28 to 271 participants. RS interventions were a majority MBSR (n = 8), followed by yoga (n = 5), cognitive based stress management (CBSM) (n = 2), guided imagery (n = 2), relaxation visualization therapy (RVT) (n = 1), mindfulness-based cancer recovery (MBCR) (n = 1), Qigong (n = 1), Tai Chi/spiritual growth group (n = 1), and body-mind-spirit (n = 1). Interventions were described as lasting from 5 to 37 weeks in duration. The majority of research designs used a single intervention group with a wait list or usual care control group (n = 13). All studies utilized physiological measures, with cortisol being the most common biomarker measure (n = 12; 54.5%).
Question 1: What psychosocial and RS measures have been used in spiritually based interventions in breast cancer survivors; and what were the associated health outcomes?
The majority of studies (n = 20) included standardized, self-report psychosocial measures, with an average of 3 to 4 psychosocial instruments administered per study. The most common self-report psychosocial measures included depression (n = 8), stress (n = 7), quality of life (n = 7), anxiety (n = 6), fatigue (n = 5), mindfulness (n = 4), and mood (n = 2). Importantly, only 1 study examined specific RS measures: spiritual growth (ie, meaning of life).104 Because many of the studies reviewed have psychosocial (subjective) and PNI (objective) outcomes, the findings are separated and presented in 2 tables to illustrate the relationships between subjective and objective variables. Table 1 provides a brief summary of the statistically significant psychosocial-spiritual findings associated with each spiritually based intervention, while Table 2 focuses on the respective PNI outcomes associated with each spiritually based intervention. Both Tables 1 and 2 utilize upward- or downward-pointing arrows, respectively, to illustrate the reported direct or inverse relationships between the variables. Additionally, the number of studies in this review are noted in Tables 1 and 2 by their corresponding order of presentation in Table 3 where highlights of the reviewed studies are provided.
Table 1.
Spiritually Based Interventions and Psychosocial-Spiritual Outcomes in Breast Cancer Survivors.
| Study Number (See Table 3) | Spiritually Based Interventions | Psychosocial-Spiritual Outcomes (↓ or ↑)a |
|---|---|---|
| 1,4, 6, 8, 15, 18 | CBSM, MBSR, Qigong, RVT, Yoga | ↓ Depression |
| 1, 4, 6, 8, 12 | CBSM, MBSR, RVT, Yoga | ↓ Anxiety |
| 2, 4, 14, 15, 18, 19, 20 | MBCR, MBSR, Qigong, Yoga | ↑ Quality of life/vitality/vigor |
| 4 | Yoga | ↓ Distress |
| 4, 17 | MBSR, Yoga | ↓ Symptoms |
| 2 | MBSR | ↑ Coping |
| 5, 7 | CBSM | ↑ Relaxation |
| 1, 6, 8, 12, 14, 18 | CBSM, MBCR, MBSR,RVT, Yoga | ↓ Stress |
| 16 | Tai Chi | ↑ Stress |
| 9, 12, 13 | MBSR | ↑ Mindfulness |
| 11 | BMS | ↑ Spiritual growth/spiritual well-being |
| 13 | MBSR | ↓ Rumination |
| 14 | MBCR | ↑ Social support |
| 15, 17, 18, 19, 20 | MBSR, Qigong, Stretching, Yoga | ↓ Fatigue |
| 9, 14 | MBCR, MBSR | ↑ Mood |
| 17 | MBSR | ↑ Cognitive function (postchemotherapy) |
Abbreviations: CBSM, cognitive-based stress management; MBCR, mindfulness-based cancer recovery; MBSR, mindfulness-based stress reduction; RVT, relaxation visualization therapy; BMS, body-mind-spirit.
↓ indicates decreased and ↑ indicates increased.
Table 2.
RS Interventions and Biomarker Outcomes in Breast Cancer Survivors.
| Study Number (See Table 3) | RS Intervention | Biomarker Outcomes (↓, ↑, or Stable)a |
|---|---|---|
| 18 | Yoga | ↓ Interleukin (IL)-1 |
| 7, 20 | GI, Yoga | ↓ IL-1β |
| 3, 6 | GI, CBSM | ↑ (IL)-2 |
| 2, 17 | MBSR | ↓ IL-4 |
| 6 | CBSM | ↑ IL-4 |
| 2, 20 | MBSR, Yoga | ↓ IL-6 |
| 2 | MBSR | ↓ IL-10 |
| 2, 3, 7 | GI, MBSR | ↑Natural killer (NK) cell activity |
| 4 | Yoga | ↓ Immunoglobulin A (IgA) |
| 4 | Yoga | ↑ CD56 % |
| 2, 5, 6, 8, 9b, 11, 14, 19 | BMS, CBSM, MBCR, MBSR,Yoga | ↓ Cortisol |
| 1, 12, 15, 18 | MBSR, Qigong, RVT, Yoga | Stable or no change in cortisol |
| 18, 20 | Yoga | Stable or ↓ tumor necrosis factor–α (TNF-α) |
| 9, 13 | MBSR | ↓ Blood pressure |
| 9 | MBSR | ↓ Pulse |
| 9 | MBSR | ↓ Respirations |
| 2, 6, 10, 17 | CBSM, MBSR | ↑ Lymphocyte subsets; T cells, Th1/Th2 |
| 7, 17 | GI, MBSR | ↑ CD4+/CD8+ |
| 2, 6, 17 | CBSM, MBSR | ↑ Interferon-γ (IFN-γ) |
| 21, 22 | MBSR | Stable (preserved) telomere length |
| 17 | MBSR | Stable/no change in CD4+ T lymphocytes |
| 17 | MBSR | Stable/no change CD3+ subsets (T1/T2) |
Abbreviations: RS, religious and spiritual; GI, guided imagery; CBSM, cognitive-based stress management; MBSR, mindfulness-based stress reduction; BMS, body-mind-spirit; RVT, relaxation/visualization therapy; MBCR, mindfulness-based cancer recovery.
↓ indicates decreased and ↑ indicates increased.
Decreased cortisol not sustained at 1 month follow-up.
Table 3.
RS Interventions With PNI Measures in Breast Cancer Survivors.
| No. | Study (First Author, Year) | Design | Cancer Stage | Intervention Group (IG) (n) vs Control Group (CG) (n) | Intervention Duration | Psychosocial and RS Measures | Objective (PNI) Measures | Key Health Outcomes |
|---|---|---|---|---|---|---|---|---|
| 1 | Nunes (2007)71 | RCT | I-II | Relaxation/visualization (IG) (RVT)* (n = 20) vs CG: Assessment only* (n = 14) *All participants undergoing concurrent radiotherapy |
24 consecutive days, 30-min sessions | Stress, Anxiety, Depression (ISSL, STAI, BAI, BDI) | Cortisol | RVT improved depression and anxiety scores (P < .05). Change in anxiety negatively correlated with cortisol (r = −0.38). RVT had no effect on cortisol levels |
| 2 | Witek-Janusek (2008)105 | Non-RCT | 0-II | MBSR (IG) (n = 38) vs CG: Assessment only (n = 28) |
8 weeks; 150 min/wk | Quality of Life, Coping, Mindfulness (QOLI-cv3, JCS, MAAS) | Lymphocytes, NKCA, Cytokines (Interleukin [IL])-2, IL-4, IL-6, IL-10, and interferon-gamma (IFN-γ), cortisol | MBSR group had lower levels of NKCA, IL-4, IL-6, IFN-γ (all P < .04) compared with CG. cortisol was lower in MBSR group (P = .002) than CG. No effect on mindfulness (P > .05). Treatment group reestablished positive immune function while control group had continued immune dysregulation |
| 3 | Lengacher (2008)74 | RCT | 0-II | Guided imagery (IG) (n = 15) vs Usual care CG (n = 13) |
6-7 weeks (2-3 weeks preop through 4 weeks postop) | None | Natural killer (NK) cells, cytokine (IL-2) | Guided imagery positively influenced NK cell cytotoxicity after IL-2 activation at 4 weeks postoperative compared with CG (P < .05) |
| 4 | Rao (2008)79 | RCT | II-III | Yoga (IG) (n = 33) vs Supportive therapy and exercise CG (n = 36) |
4 weeks | (Anxiety, Depression, Function) (STAI, BDI, FLIC) |
T-lymphocyte subsets, CD4%, CD8%, NK cells, and immunoglobulin (IgA, IgG, IgM) | Yoga group demonstrated decreased anxiety (P = .04), depression (P = .01), decreased symptom severity (P = .01), decreased distress (P < .01) and improved QOL (P = .01) compared with CG. Less immune dysfunction was observed in yoga group (decreased CD56%, P = .02) and (decreased IgA, P = .001) compared with CG |
| 5 | Phillips (2008)106 | RCT | 0-III | CBSM (IG) (n = 65) vs 1-day education CG (n = 63) |
10 weeks; repeat measures over 12 months | Current Status (MOCS-Relaxation) | Cortisol | Greater reductions in cortisol levels across 12 months in CBSM compared with CG, although effect was small (d = 0.20). |
| 6 | Antoni (2009)107 | RCT | 0-III | CBSM (IG) (n = 65) vs Usual care CG: 1-day education (n = 63) |
10 weeks | Stress, Anxiety & Depression, & Negative Mood (IES, HADS, ABS) |
Cortisol, lymphocyte subsets, cytokines (IL-2, IFN-γ, IL-4) | CBSM had improved cortisol patterns (P < .01), improved IL-2 (P < .05), and improved IFN-γ (P < .01) function compared with CG during the first 6 months. Results suggest CBSM group may have experienced a buffering effect of adjuvant therapy compared with the CG. Improved trends observed in psychosocial measures; however, no significant effects observed between changes in psychosocial measures and biomarker measures |
| 7 | Eremin (2009)72 | RCT | II-IV | Relaxation and guided imagery (IG) (n = 40) vs Standard care CG (n = 40) |
37 weeks | None | T-cell subsets and lymphokine activated killer cells, B lymphocytes and monocytes; cytokines IL-1beta (1β), IL-2, IL-4 and IL- 6 and TNF-α | At 8 weeks, significant correlations observed between imaging ratings and natural killer cell activity (r = 0.319, P = .02). Relaxation frequency (r = 0.308, P = .018) and imagery ratings (r = 0.308, P = .019) correlated significantly with blood IL-1β, CD4+, and CD8+ levels. |
| 8 | Vadiraja (2009)108 | RCT | I-III | Yoga (IG) (n = 44)* vs Supportive therapy CG* (n = 44) *All participants undergoing concurrent radiotherapy |
6 weeks (3) 1-hour sessions per week |
Anxiety & Depression, Stress (HADS, PSS) |
Cortisol | Positive correlations between decreased AM cortisol levels and decreased anxiety (Cohen’s f = 0.31), depression (f = 0.31), and stress (f = 0.36) in yoga group compared with CG |
| 9 | Matchim (2010)109 | Non-RCT | 0-II | MBSR (IG) (n = 15) vs Wait list CG (n = 17) |
8 weeks 90 min/wk Repeat measures at 1 month |
Mood, Stress, Mindfulness (POMS, C-SOSI, FFMQ) | Salivary cortisol, blood pressure (BP), pulse, and respirations | Increased mindfulness decreased BP, pulse, and respirations observed in MBSR compared with CG (P = .05 to P = .001). Initial decrease in AM cortisol within MBSR group was statistically significant (P < .05), but was not sustained at 1-month follow-up |
| 10 | Lengacher (2013)50 | RCT | 0-III | MBSR (IG) (n = 42) vs Usual care CG (n = 40) |
6 weeks 2 h/wk Repeat measures at 12 weeks |
None | Lymphocyte subsets, T helper 1 and 2 cells (Th1/Th2), NK cells, IFN-γ, IL-4 | Positive associations between all immune subset recoveries in MBSR group compared with CG. Women who received MBSR had T cells more readily activated by the mitogen phytohemagglutinin and an increase in the Th1/Th2 ratio (P = .002). MBSR associated with a more rapid return to normal immune function compared with CG, particularly in early posttreatment recovery periods |
| 11 | Hsiao (2012)104 | RCT | 0-III | Body-mind-spirit (BMS) (IG) (n = 26) vs Education CG (n = 22) |
8 weeks 2 h/wk Repeat measures at 5 and 8 months |
Depression Meaning in Life (Purpose, Search) (BDI, MLQ-P, MLQ-S) |
Cortisol | At 5 months, BMS was related to greater spiritual growth (search for meaning in life) (P < .01). At 8 months, the BMS group demonstrated healthier cortisol patterns compared with CG (P < .05). |
| 12 | Branstrom (2012; 2013)110,111 | RCT | Data not provided | MBSR (IG) (n = 32) vs Wait list CG (n = 39) |
8 weeks 2 h/wk Repeat measures at 3 and 6 months |
Stress, Anxiety & Depression, Mood, Coping; Mindfulness (PSS, HADS, IES-R, PSOM, CSES, FFMQ) |
Cortisol | MBSR associated with lower stress (P = .06), lower anxiety (P = .09), and increased mindfulness (P < .01). Although not quite significant (r = −0.38, P = .06) a trend was observed that MBSR demonstrated a moderate effect on awakening cortisol levels and was sustained at 6-month follow-up. Nonsignificant effects between stress and cortisol (P = .06) were observed |
| 13 | Campbell (2012)92 | NonRCT | Data not provided | MBSR (IG) (n = 19) vs Wait list CG (n = 16) |
8 weeks 90 min/wk |
Mindfulness, Rumination (MAAS, RRQ-rs) | Blood pressure (BP) | MBSR may improve mindfulness, moderate effect between decreased rumination and decrease systolic BP (r = 0.35), no main effects observed |
| 14 | Carlson (2013)68 | RCT | 0-IV | MBCR (IG) (n = 113) vs Supportive emotional therapy (SET) (IG) (n = 104) vs Usual care CG: 1-day stress management seminar (n = 54) |
8 weeks 90 min/wk |
Mood, Stress, Quality of Life, Social Support (POMS-TMD, C-SOSI, FACT-B, FACT-G, MOS-SSS) |
Cortisol | Cortisol patterns were stable over time in both SET (P = .003) and MBCR (P = .014) groups relative to the CG, who had more flattened cortisol slopes. Women in MBCR improved more over time on stress symptoms compared with both SET (P = .009) and control (P = .023) groups. Greater improvements in MBCR group in quality of life compared with SET (P = .006) and CG (P = .005); and in social support compared with the SET (P = .012) |
| 15 | Chen (2013)112 | RCT | 0-III | Qigong (IG) (n = 49)* vs Wait list CG (n = 47)* *Participants currently undergoing radiotherapy |
5 weeks 40 min/wk with 1- and 3-month repeat measures |
Depression, Fatigue, Quality of Life, Sleep Disturbance (CES-D, BFI, FACT-G, PSQI) |
Cortisol | Qigong group reported less depression over time than women in CG (P = .05). Women who had elevated depressive symptoms at the start of radiotherapy reported less fatigue (P < .01) and better overall quality of life (P < .05) in the Qigong group compared with the CG. No significant changes observed in cortisol slopes |
| 16 | Robins (2013)77 | RCT | I-IIIa | (n = 109)* (no further data) Tai Chi (IG) vs Spiritual growth group (IG) vs Usual care CG *Concurrent chemotherapy |
10 weeks 90 min/wk Repeat measures at 1 week, 4.5 months, 6 months |
Stress, Quality of Life, Depression (IES, FACT-B, CES-D) |
Cytokine panel (IL-1β, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL-12, IL-13, IL-17, TNF-α) | Interesting patterns in biomarkers observed; however, no statistically significant effects observed between intervention and control groups while currently receiving chemotherapy |
| 17 | Reich (2014)113 | RCT | 0-III | MBSR (IG) (n = 17) vs Usual care/wait list CG (n = 24) |
6 weeks 2 hs/wk Measures at baseline and 6 weeks |
Symptoms (MDASI) |
Lymphocyte subsets, mitogen-stimulated subsets, cytokines | After 6 weeks, multiple baseline biomarkers were significantly positively improvement in GI symptoms (P = .035) and fatigue (P = .035) in MBSR group. Regression modeling identified B-lymphocytes and IFN-γ as the strongest predictors of gastrointestinal symptom improvement (P < .01). CD4+, CD8+ were predictive of strongest predictor of cognitive/ psychological improvement (P = .02). Lymphocytes and IL-4 were strongest predictors of fatigue improvement (P < .01) |
| 18 | Bower (2012; 2014)78,114 | RCT | 0-II | Iyengar yoga (IG) (n = 14) vs Usual care CG (n = 15) |
12 weeks 90 min, twice weekly Repeat measures at baseline, 12 weeks, and 24 weeks |
Fatigue, Depression, Sleep, Stress, Vigor (FSI, BDI-II, PSQI, PSS, MSFI) |
Cortisol, tumor necrosis factor-alpha (TNF-α), IL-1, IL-6, CRP | Decreased fatigue in yoga group from baseline to posttreatment and sustained at 3-month follow-up compared to CG (P = .032). Yoga group had significant increases in vigor compared with CG (P = .011). Both groups had positive changes in depressive symptoms and perceived stress (P < .05). Yoga group showed improved immune biomarker functioning compared with controls (P < .05). Tumor necrosis factor patterns remained stable in yoga group, while CG levels increased (P = 0.28). Similar trend observed with IL-1, but nonsignificant (P = .16). No significant changes in CRP, IL-6 or diurnal cortisol patterns |
| 19 | Chandwani (2014)115 | RCT | 0-III | Yoga (IG) (n = 53)* vs Stretching (IG) (n = 56)* vs Wait list CG (n = 54)* *Concurrently undergoing radiotherapy |
6 weeks Up to 180 min/wk Repeat measures at 1, 3, and 6 months postintervention |
Quality of Life, Fatigue, Depression, Sleep (MO-SF 36, BFI, CES-D, PSQI) |
Cortisol | Yoga group demonstrated greater increases in physical component scale scores compared with CG at 1 and 3 months after radiotherapy (P = .01 and P = .01, respectively). At 1, 3, and 6 months, the yoga group had greater increases in physical functioning compared with both stretching and CG (P < .05), with stretching and CG differences at only 3 months (P < .02). Yoga and stretching groups had reduced fatigue (P < .05) at radiotherapy completion. No group differences for mental health and sleep quality. Cortisol slope was steepest for the yoga group compared with the stretching and CG at the end (P = .023 and P = .008, respectively) and 1 month after radiotherapy completed (P = .05 and P = .04, respectively) |
| 20 | Kiecolt-Glaser (2014)116 | RCT | 0-IIIa | Yoga (IG) (n = 100) vs Wait list CG (n = 100) |
12 weeks 90 min/twice weekly Repeat measures at 3 months postintervention |
Fatigue, Quality of Life, Depression, Sleep, Activity, Diet (MFSI-SF, MO SF-36, CES-D, PQSI, CHAMPS, FFQ) |
Cytokines (IL-1β, IL-6, TNF-α) | At posttreatment, fatigue was not lower in yoga compared with CG (P > .05) but vitality was higher (P = .01). At 3 months posttreatment, fatigue was lower in the yoga group (P = .002), vitality was higher (P = .01), and IL-6 (P = .027), TNF-α (P = .027), and IL-1 (P = .037) were lower for yoga group compared with CG. No group differences in depression at either time points (P > .20). Frequency of yoga practice showed a stronger association with fatigue and vitality, but not depression; greater changes associated with more frequent practice. At 3 months posttreatment, increased yoga practice was associated with decreased IL-6 (P = .01) and IL-1 (P = .03), but not TNF-α production (P > .05) |
| 21 | Lengacher (2014)117 | RCT | 0-III | MBSR (IG) (n = 74) vs Usual care (n = 68) |
6 weeks intervention Repeat measures at 12 weeks |
Recurrence Concerns, Mindfulness, Stress, Anxiety, Depression (CARS,CAMS, PSS, STAI, CES-D) |
Telomere length, telomere activity | Telomere activity (TA) increased steadily over 12 weeks in MBSR group (17%) compared with minimal increase in CG (approximately 3%, P < .01). No effects observed on Telomere length (P = .92). MBSR appears to increase TA in peripheral blood mononuclear cells. TA was not associated with change in mindfulness, stress, anxiety, or fear of recurrence |
| 22 | Carlson (2015)118 | RCT | I-III | MBCR (IG) (n = 53) vs Supportive emotional therapy group (SET) (IG) (n = 49) vs Usual care (n = 26) (1-day seminar) |
8 weeks 90 min/wk plus 6-hour, 1-day retreat 12 weeks 90 min/wk 1-day, 6-hour, stress management seminar |
Mood, Stress (POMS, C-SOSI) |
Telomere length | No correlations between measures of mood (P = .80) and stress (P = .24) and changes in telomere length between MBCR and SET groups and the CG (P = .28), or across the 2 intervention conditions (P = .31) and (P = .55). Telomere length in the MBCR and SET groups remained preserved (positive outcome) while a decrease among the CG was significant (P = .04) |
Abbreviations: RS, religious and spiritual; PNI, psychoneuroimmunological; RCT, randomized control trial group; IG, intervention group; CRP, C-reactive protein; CG, control group; RVT, relaxation and visualization therapy; ISSL, Inventory of Stress Symptoms Lipp; STAI, State-Trait Anxiety Inventory; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; non-RCT, nonrandomized control trial group; MBSR, mindfulness-based stress reduction; QOLI-v3, Quality of Life Index Cancer Version 3, JCS, Jaloweic Coping Scale; MAAS, Mindfulness Attention Awareness Scale; FLIC, Functional Living Index of Cancer; MOCS-R, Measure of Current Status–Relaxation; IES, Impact of Events Scale; HADS, Hospital Anxiety and Depression Scale; ABS, Affects Balance Scale; PSS, Perceived Stress Scale; POMS, Profile of Mood States; C-SOSI, Calgary Symptoms of Stress Inventory; FFMQ, Five Facet Mindfulness Questionnaire; MDASI, MD Anderson Symptom Inventory; MLQ-P, Meaning in Life Questionnaire, Presence; MLQ-S, Meaning in Life Questionnaire; IES-R, Impact of Events Scale–Revised; PSOM, Positive State of Mind; CSES, Coping Self-Efficacy Scale; RRQ-rs, Rumination Reflection Questionnaire—revised; MBCR, mindfulness-based cancer recovery; POMS-TMD, Profile of Mood States–Total Mood Disturbance; FACT-B, Functional Assessment of Cancer Therapy–Breast; FACT-G, Functional Assessment of Cancer Therapy–General; MOS-SSS, Medical Outcomes Study–Social Support Survey; SOSI, Symptoms of Stress Inventory; NK, natural killer; IFN-γ, interferon-gamma; IL, interleukin; DHEA, dehydroepiandrosterone sulfate; FACIT-G, Functional Assessment of Cancer Illness Therapy–General; CES-D, Center for Epidemiological Studies–Depression Scale; BFI, Brief Fatigue Inventory; PSQI, Pittsburg Sleep Quality Index; FSI, Fatigue Symptom Inventory; BDI-II, Beck Depression Inventory–II; MFSI, Multidimensional Fatigue Symptom Inventory; MO SF-36, Medical Outcomes Short-Form 36; CHAMPS, Community Healthy Activities Model Program for Seniors; FFQ, Food Frequency Questionnaire; CARS, Concerns About Recurrence Scale; CAMS, Cognitive and Affective Mindfulness Scale–Revised.
The majority of spiritually based intervention studies demonstrated positive changes in one or more of the psychosocial-spiritual outcome measures examined. The most common positive psychosocial outcomes associated with spiritually based interventions were observed in measures of quality of life, depression, stress, anxiety, fatigue, and mood. The exception was a study by Robins et al77 in which measures of stress at study conclusion demonstrated an overall decrease in perceived stress among Tai Chi, spiritual intervention, and control groups compared with preintervention measures, however, the Tai Chi group continued to report more perceived stress compared to those in the spiritual intervention group and control group at postintervention. Of note, all participants, including the control group, were receiving adjuvant chemotherapy. Robins et al77 suggested that greater perceived stress among the Tai Chi participants may have indicated psychological distress that occurred due to increased self-awareness or “centering” secondary to the interventions. Moreover, the authors noted that although Tai Chi encourages mindfulness, an unintended initial effect of increased mindfulness may be temporary depression-like symptoms (ie, psychological distress) that occur during stressful life events (eg, post–cancer chemotherapy treatment sequela). Additionally, Robins et al77 noted that psychological distress may have been secondary to chemotherapy sequela (eg, fatigue) and/or secondary to learning Tai Chi movement; however, these potential confounders were not measured. Finally, 2 studies examined relationships between mindfulness-based interventions, psychosocial measures (eg, mood and stress), and telomere variables; however, the psychosocial relationships very small and were not statistically significant.117,118
Question 2: What PNI outcome measures have been used in spiritually based interventions in breast cancer survivors; and what were the associated physiological biomarker outcomes?
Table 2 provides an overview of the spiritually based intervention studies with PNI-based biomarker outcomes. In this review, cortisol is the most commonly studied biomarker outcome studied in the spiritually based interventions. An interesting finding was that among the cortisol studies reviewed, 8 studies reported positive changes in cortisol activity (ie, decreased levels or healthier diurnal slope patterns compared to control groups), while 4 studies reported “no change” or “stable” cortisol levels compared with control groups. These can be somewhat mixed findings to interpret, as “no change” in cortisol levels is occasionally noted in studies in which elevated levels of cortisol are observed in the control group. These findings suggested that in some instances, “no change” or “stable” cortisol levels after a spiritually based intervention may reflect a positive buffering effect associated with the intervention. Additionally, some cortisol studies reported significant changes immediately postintervention, but not sustained at 1-month,109 3-month,110 and 6-month follow-up.111
Two biomarkers of emerging PNI interest, telomere length and telomere activity are noteworthy for this discussion. Recent data suggest that shorter telomere length is associated with poorer outcomes in chronic lymphocytic leukemia populations119 and may be predictive or poor prognosis in cancer patients.120 In this review, Carlson et al118 reported that MBSR appeared to preserve telomere length in breast cancer survivors in the intervention group, while telomere length in the control group was shortened. Interestingly, Lengacher et al117 did not report preserved telomere length among MBSR breast cancer survivor participants; instead, their study demonstrated that those receiving the MBSR intervention had increased telomerase activity. Of note, duration of these MBSR interventions ranged from 6 to 8 weeks. These studies offer significant direction to PNI research as both provide early data regarding the potential relationship between mindfulness-based interventions and telomere length/telomere activity in breast cancer populations. Although more empirical data are required, these studies are some of the first studies to report observations between spiritually based practices and physiological outcomes.
Overall, a wide variety of neuroendocrine-immune biomarker measures represented in the studies were observed in this review. Positive and negative associations between the spiritually based interventions and PNI outcome variables for the intervention studies were examined and these relationships are depicted in Table 2 with upward- or downward-pointing arrows. Moreover, the studies reporting these associations in Table 2 are linked with their corresponding study number as presented in Table 3. Among studies reviewed, MBSR interventions have been the most utilized spiritually based interventions in breast cancer survivors. MBSR is associated with improved inflammatory cytokine activity, improved lymphocyte function, improved or stabilization of cortisol levels, and increased or preservation of telomere activity. Moreover, interventions similar to MBSR, including CBSM, MBCR, and yoga all demonstrated similar influences on cytokine function, lymphocyte production, and improved or stabilized cortisol activity. While the remaining interventions, including Qigong, body-mind-spirit, and relaxation visualization therapy showed preservation or improved cortisol function in breast cancer survivors, there are few of these studies to date and conclusions are limited. Findings suggest that in general, spiritually based interventions are associated with improved neuroendocrine-immune function, particularly cortisol and cytokine activity.
Question 3: What is the evidence regarding the relationships between spiritually based interventions, psychosocial-spiritual outcomes, and PNI-based outcomes in breast cancer survivors?
Details of each reviewed intervention study are provided in Table 3, including designs, sample sizes, intervention and control group descriptions, psychosocial-spiritual measures, PNI measures, and the statistical significance of the outcome variables. The comparison of findings is challenging due to the wide variation in intervention duration and the wide range of psychosocial measures, as well as variation in PNI measures outcomes. However, there is a growing body of evidence to suggest a positive pattern is emerging between spiritually based interventions and physiological health outcomes. The majority of studies in this review report positive psychosocial and mindfulness-spiritual outcomes, as well as positive biomarker outcomes across differing spiritually based interventions.
While the immune system response to spiritually based interventions during chemotherapy and/or radiotherapy was not an initial question for the review, it was observed that five spiritually based intervention studies were conducted while participants were concurrently undergoing chemotherapy or radiotherapy for breast cancer treatment. These interventions included RVT, yoga, Qigong, Tai Chi/spiritual growth, and yoga/stretching. It was observed that yoga interventions report a limited, but positive, trend on immune function during chemotherapy and radiotherapy treatments.108,115 While comparison is limited due to differing designs and treatments, both yoga interventions utilized the same intervention dose and duration (6 weeks, 180 min/wk) and utilized cortisol measures in breast cancer participants with stage III or lower.
Question 4: What are the implications for future research studies regarding spiritually based interventions, measures of RS, and PNI outcome measures?
Although interventions with a spiritual basis were the primary focus of this review, only one breast cancer study reported utilization of actual RS measures. Hsiao et al104 reported an association between an 8-week body-mind-spirit intervention, spiritual growth, and healthier cortisol patterns among breast cancer participants, compared with the control group (P < .05). While there were no other breast cancer body-mind-spirit intervention studies for comparison in this review, a similar study in patients with chronic depression and anxiety reported no association between prayers and cortisol levels.121 These findings contrast with those reported by Bormann et al,122 who did find an association between prayer and decreased cortisol levels in HIV-positive individuals. There are few studies examining specific RS measures and associated PNI biomarker outcomes in breast cancer survivorship; therefore, the nature of these relationships remain unclear.
Table 3 provides the differences in the spiritually based interventions, including duration and dosing protocols (ie, frequency of practice). Similar to findings by Subnis et al,99 little has been reported regarding intervention practice adherence. Additionally, it should be noted that spiritually based interventions with fewer weeks of duration have shown positive benefits similar to those with longer durations. This is important because intervention designs need to consider examination of the minimum dose and duration required to achieve a positive effect on immune function. Furthermore, these interventions add a degree of burden to chronically ill participants who may not feel well enough to leave home and travel to a group setting. Future intervention design should consider modifying spiritually based interventions for use in personal (ie, home-based) settings.
Previously, spiritually based interventions with PNI measures were of exploratory design, cross-sectional, and lacking a comparison arm. This review found that studies reviewed were generally more rigorous in approach than previous studies as a growing number of interventions (n = 6) were greater than 10 weeks in duration and the majority performed repeat measures ranging from 3 to 24 months postintervention. Moreover, it was feasible to find a number of studies with comparison groups (22 RCTs/non-RCTs) that satisfactorily met review criteria, allowing a more comprehensive examination of findings than earlier reviews that lacked comparison groups.
Findings from this review are consistent with other reviews that found spiritually based interventions exerted a positive influence on psychological health, particularly on symptoms of depression, anxiety, mood, stress, and perceptions of quality of life. However, previous reviews have been mixed on the extent to which spiritually based interventions influence PNI outcome measures. This review revealed a positive pattern between spiritually based interventions and a number of PNI biomarker outcomes, suggesting that spiritually based interventions offer positive mental and physiological health benefits. For breast cancer survivors, these studies suggested that engaging in spiritually based practices may improve or stabilize the immune profile dysregulation that occurs with breast cancer.
Future questions to be answered based on these findings include the following: which components of the interventions are most influential on outcomes (eg, mindfulness, breathing, stretching); and, are all components necessary to achieve the immune profile benefits? Additionally, what could the minimum dose (eg, frequency and length of practice) and duration (eg, weeks, months, or lifetime) be for achieving and sustaining neuroendocrine-immune benefits? Moreover, which spiritually based interventions are most predictive of biomarker outcomes?
Limitations
This review found that spiritually based interventions utilized disease-specific variables (ie, treatment-type, stage) for study inclusion criteria. However, this design does not allow for individual differences in psychosocial-spiritual variables (eg, perceptions of distress, spiritual beliefs, coping skills, and lifestyle behavior patterns). For these reasons, and as Carlson69 indicated previously, recruitment of a study population based on disease characteristics rather than psychosocial-spiritual considerations may result in unintended participant stress and impede measurement of the intervention’s therapeutic value.
Similar to previous reviews, there remains a continued need for larger sample sizes and the inclusion of study power calculations. The direction of future spiritually based intervention design needs to standardize methods for intervention dosing, frequency, and duration of treatment. This review observed an increase in the numbers of study designs with randomization and longitudinal measures. However, because of the relative “newness” of spiritually based interventions in health care research, a variety of methods and study protocols exist between these interventions. Subsequently, these study methods and protocols vary in the reporting of details, resulting in a lack of guidance for prospective researchers wishing to reproduce intervention findings. A recent National Institutes of Health123 mandate for grant submissions highlights the need for reporting detailed study protocols and statistical computation methods in order to facilitate scientific validation of study findings.
Finally, this review did not utilize a standard measure of study quality as this was beyond the focus of the review. Additionally, rigor of study randomization and blinding practices were not examined. However, screening and selection of intervention studies reviewed were limited to studies with comparison groups; and the majority of studies reviewed were randomized control trials.
Conclusion
This review found a positive pattern of relationships between spiritually based interventions, mental health outcomes, and neuroendocrine-immune function in breast cancer survivors. However, there were limited and uncertain benefits regarding the impact of spiritually based interventions on neuroendocrine-immune function among individuals receiving chemotherapy and/or radiotherapy. There is a growing body of evidence supporting relationships between RS self-report measures and mental health outcomes; however, RS self-report measures were rarely utilized when psychosocial-spiritual and PNI outcome measures (ie, biomarkers) were examined. Specifically, the trend in PNI intervention studies has been to measure a wide variety of psychosocial variables, with minimal measures of specific RS variables. Therefore, future research must clarify how best to address the issue regarding overlap of RS constructs in order for intervention outcomes to be more meaningful.
Additional biomarker studies are needed with specific and standardized measures of RS in order to understand the relationships between RS variables and PNI health outcomes. Similarly, future studies should examine which biomarkers offer the most utility in predicting breast cancer survivorship outcomes including biomarkers associated with the risk of post–breast cancer treatment late effects. Future psychosocial-spiritual healthcare research might consider intervention designs that personalize treatment based on psychosocial-spiritual needs, as well as diverse participant setting considerations. Additionally, research that can inform on the minimum necessary spiritual-intervention dose and duration will serve to reduce survivors’ burden in managing post-breast cancer treatment-related symptoms. Finally, intervention designs will need to consider home-based delivery options, which remain important for survivors who are too ill to travel, have a preference for private/individual practice settings, or lack economic resources for traveling and transportation for group interventions.
Acknowledgments
The authors would like to acknowledge the Mizzou Advantage Fund, the University of Missouri Interdisciplinary Center on Aging: Research Enrichment and Dissemination (READ) program, and Sigma Theta Tau International–Alpha Iota Chapter for Jennifer Hulett’s doctoral research program support.
Footnotes
Authors’ Note: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, The University of Utah, or the University of Missouri.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported (in part) by the National Institute of Nursing Research of the National Institutes of Health under Award Number T32NR013456.
References
- 1. Battaglini C, Dennehy C, Groff D, Kirk D, Anton P. Complementary therapies in the management of cancer treatment-related symptoms: the individualized prescriptive exercise intervention approach. Med Sportiva. 2006;10(2):49-57. [Google Scholar]
- 2. Armer JM, Stewart BR. Post-breast cancer lymphedema: incidence increases from 12 to 30 to 60 months. Lymphology. 2010;43:118-127. [PMC free article] [PubMed] [Google Scholar]
- 3. Clough-Gorr KM, Ganz PA, Silliman RA. Older breast cancer survivors: factors associated with self-reported symptoms of persistent lymphedema over 7 years of follow-up. Breast J. 2010;16:147-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Foster C, Wright D, Hill H, Hopkinson J, Roffe L. Psychosocial implications of living 5 years or more following a cancer diagnosis: a systematic review of the research evidence. Eur J Cancer Care (Engl). 2009;18(3):223-247. [DOI] [PubMed] [Google Scholar]
- 5. Fu MR, Rosedale M. Breast cancer survivors’ experiences of lymphedema-related symptoms. J Pain Symptom Manage. 2009;38:849-859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Armer JM, Stewart BR, Wanchai A, Lasinski BB, Smith KM, Cormier JN. Rehabilitation concepts among aging survivors living with and at risk for lymphedema: a framework for assessment, enhancing strengths, and minimizing vulnerability. Top Geriatr Rehabil. 2012;28:260-268. [Google Scholar]
- 7. Feinstein M, Liu K, Ning H, Fitchett G, Lloyd-Jones DM. Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: the multi-ethnic study of atherosclerosis. Circulation. 2010;121:659-666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Howlader N, Noone A, Krapcho M, et al., eds. SEER Cancer Statistics Review, 1975-2011. Bethesda, MD: National Cancer Institute; 2014. [Google Scholar]
- 9. Pew Center for Center. Pew Research Religion and Public Life Project. Religious beliefs and practices. 2008; http://religions.pewforum.org/reports#. Accessed February 16, 2015.
- 10. Bearon LB, Koenig H.G. Religious cognitions and use of prayer in health and illness. Gerontologist. 1990;30:249-253. [DOI] [PubMed] [Google Scholar]
- 11. Altschuler A, Rosenbaum E, Gordon P, Canales S, Avins A. Audio recordings of mindfulness-based stress reduction training to improve cancer patients’ mood and quality of life—a pilot feasibility study. Support Care Cancer. 2012;20:1291-1297. [DOI] [PubMed] [Google Scholar]
- 12. Fouladbakhsh J, Stommel M. Gender, symptom experience, and use of complementary and alternative medicine practices among cancer survivors in the U.S. cancer population. Oncol Nurs Forum. 2010;37:E7-E15. [DOI] [PubMed] [Google Scholar]
- 13. Lengacher CA, Bennett MP, Kip KE, et al. Frequency of use of complementary and alternative medicine in women with breast cancer. Oncol Nurs Forum. 2002;29:1445-1452. [DOI] [PubMed] [Google Scholar]
- 14. Wyatt G, Sikorskii A, Wills CE, An HS. Complementary and alternative medicine: use, spending, and quality of life in early stage breast cancer. Nurs Res. 2010;59:58-66. [DOI] [PubMed] [Google Scholar]
- 15. Yates JS, Mustian KM, Morrow GR, et al. Prevalence of complementary and alternative medicine use in cancer patients during treatment. Support Care Cancer. 2005;13:806-811. [DOI] [PubMed] [Google Scholar]
- 16. Pargament KI. The Psychology of Religion and Coping: Theory, Research, Practice. New York, NY: Guilford Press; 1997. [Google Scholar]
- 17. Ano GG, Vasconcelles EB. Religious coping and psychological adjustment to stress: a meta-analysis. J Clin Psychol. 2005;61:461-480. [DOI] [PubMed] [Google Scholar]
- 18. Hulett JM, Armer JM, Stewart BR, Wanchai A. Perspectives of the breast cancer survivorship continuum: diagnosis through 30 months post-treatment. J Pers Med. 2015;5:174-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gall TL, Cornblat MW. Breast cancer survivors give voice: a qualitative analysis of spiritual factors in long-term adjustment. Psychooncology. 2002;11:524-535. [DOI] [PubMed] [Google Scholar]
- 20. McCain NL, Gray DP, Elswick RK, Jr, et al. A randomized clinical trial of alternative stress management interventions in persons with HIV infection. J Consult Clin Psychol. 2008;76:431-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lengacher CA, Johnson-Mallard V, Post-White J, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology. 2009;18:1261-1272. [DOI] [PubMed] [Google Scholar]
- 22. Aldwin CM, Park CL, Jeong Y-J, Nath R. Differing pathways between religiousness, spirituality, and health: a self-regulation perspective. Psychol Relig Spiritual. 2014;6:9. [Google Scholar]
- 23. Johnstone B, Yoon DP, Cohen D, et al. Relationships among spirituality, religious practices, personality factors, and health for five different faith traditions. J Relig Health. 2012;51:1017-1041. [DOI] [PubMed] [Google Scholar]
- 24. Piedmont RL, Ciarrochi JW, Dy-Liacco GS, Williams JEG. The empirical and conceptual value of the spiritual transcendence and religious involvement scales for personality research. Psychol Relig Spiritual. 2009;1:162-179. [Google Scholar]
- 25. Reinert KG, Koenig HG. Re-examining definitions of spirituality in nursing research. J Adv Nurs. 2013;69:2622-2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hsiao YC, Chien LY, Wu LY, Chiang CM, Huang SY. Spiritual health, clinical practice stress, depressive tendency and health-promoting behaviours among nursing students. J Adv Nurs. 2010;66:1612-1622. [DOI] [PubMed] [Google Scholar]
- 27. Johnstone B, Yoon DP, Franklin KL, Schopp L, Hinkebein J. Re-conceptualizing the factor structure of the Brief Multidimensional Measure of Religiousness/Spirituality. J Relig Health. 2009;48:146-163. [DOI] [PubMed] [Google Scholar]
- 28. Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality. Implications for physical and mental health research. Am Psychol. 2003;58:64-74. [DOI] [PubMed] [Google Scholar]
- 29. Miller WR, Thoresen CE. Spirituality, religion, and health. An emerging research field. Am Psychol. 2003;58:24-35. [DOI] [PubMed] [Google Scholar]
- 30. Fetzer Institute/National Institute on Aging Working Group. Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research: A Report of the Fetzer Institute/National Institute on Aging Working Group. Kalamazoo, MI: Fetzer Institute; 1999. [Google Scholar]
- 31. Emmons RA, Paloutzian RF. The psychology of religion. Annu Rev Psychol. 2003;54:377-402. [DOI] [PubMed] [Google Scholar]
- 32. Johnstone B, Glass BA. Support for a neuropsychological model of spirituality in persons with traumatic brain injury. Zygon. 2008;43:861-874. [Google Scholar]
- 33. Rose S. Is the term “spirituality” a word that everyone uses, but nobody knows what anyone means by it? J Contemp Relig. 2001;16:193-207. [Google Scholar]
- 34. Johnstone B, Bodling A, Cohen D, Christ SE, Wegrzyn A. Right parietal lobe-related “selflessness” as the neuropsychological basis of spiritual transcendence. Int J Psychol Relig. 2012;22:267-284. [Google Scholar]
- 35. Piedmont RL. Does spirituality represent the sixth factor of personality? Spiritual transcendence and the five-factor model. J Pers. 1999;67:985-1013. [Google Scholar]
- 36. White ML, Peters R, Schim SM. Spirituality and spiritual self-care: expanding self-care deficit nursing theory. Nurs Sci Q. 2011;24:48-56. [DOI] [PubMed] [Google Scholar]
- 37. Koenig H, King D, Carson VB. Handbook of Religion and Health. Oxford, England: Oxford University Press; 2012. [Google Scholar]
- 38. Bodling A, Heneghan M, Walsh JC, Yoon DP, Johnstone B. The Brief Multidimensional Measure of Religiousness/Spirituality with an Irish sample: a factor analysis. Int J Ther Rehabil. 2013;20:72-78. [Google Scholar]
- 39. Cohen D, Yoon DP, Johnstone B. Differentiating the impact of spiritual experiences, religious practices, and congregational support on the mental health of individuals with heterogeneous medical disorders. Int J Psychol Relig. 2009;19:121-138. [Google Scholar]
- 40. Bower J, Meyerowitz B, Bernaards C, Rowland J, Ganz P, Desmond K. Perceptions of positive meaning and vulnerability following breast cancer: predictors and outcomes among long-term breast cancer survivors. Ann Behav Med. 2005;29:236-245. [DOI] [PubMed] [Google Scholar]
- 41. Stefanek M, McDonald PG, Hess SA. Religion, spirituality and cancer: current status and methodological challenges. Psychooncology. 2005;14:450-463. [DOI] [PubMed] [Google Scholar]
- 42. Vespa A, Jacobsen PB, Spazzafumo L, Balducci L. Evaluation of intrapsychic factors, coping styles, and spirituality of patients affected by tumors. Psychooncology. 2011;20:5-11. [DOI] [PubMed] [Google Scholar]
- 43. Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006;24:1105-1111. [DOI] [PubMed] [Google Scholar]
- 44. Lutgendorf SK, Sood AK, Anderson B, et al. Social support, psychological distress, and natural killer cell activity in ovarian cancer. J Clin Oncol. 2005;23:7105-7113. [DOI] [PubMed] [Google Scholar]
- 45. Powell ND, Tarr AJ, Sheridan JF. Psychosocial stress and inflammation in cancer. Brain Behav Immun. 2013;30(suppl):S41-S47. [DOI] [PubMed] [Google Scholar]
- 46. Andersen BL, Farrar WB, Golden-Kreutz D, et al. Stress and immune responses after surgical treatment for regional breast cancer. J Natl Cancer Inst. 1998;90:30-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Witek-Janusek L, Gabram S, Mathews HL. Psychologic stress, reduced NK cell activity, and cytokine dysregulation in women experiencing diagnostic breast biopsy. Psychoneuroendocrinology. 2007;32:22-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65:571-581. [DOI] [PubMed] [Google Scholar]
- 49. Carlson LE, Speca M, Faris P, Patel KD. One year pre–post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21:1038-1049. [DOI] [PubMed] [Google Scholar]
- 50. Lengacher CA, Kip KE, Post-White J, et al. Lymphocyte recovery after breast cancer treatment and mindfulness-based stress reduction (MBSR) therapy. Biol Res Nurs. 2013;15:37-47. [DOI] [PubMed] [Google Scholar]
- 51. Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448-474. [DOI] [PubMed] [Google Scholar]
- 52. Loizzo J, Charlson M, Peterson J. A program in contemplative self-healing: stress, allostasis, and learning in the Indo-Tibetan tradition. Ann N Y Acad Sci. 2009;1172:123-147. [DOI] [PubMed] [Google Scholar]
- 53. Matousek RH, Pruessner JC, Dobkin PL. Changes in the cortisol awakening response (CAR) following participation in mindfulness-based stress reduction in women who completed treatment for breast cancer. Complement Ther Clin Pract. 2011;17:65-70. [DOI] [PubMed] [Google Scholar]
- 54. Lengacher CA, Kip KE, Barta M, et al. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J Holist Nurs. 2012;30:170-185. [DOI] [PubMed] [Google Scholar]
- 55. Ader R, Cohen N. Behaviorally conditioned immunosuppression. Psychosom Med. 1975;37:333-340. [DOI] [PubMed] [Google Scholar]
- 56. Zeller JM, McCain NL, Swanson B. Psychoneuroimmunology: an emerging framework for nursing research. J Adv Nurs. 1996;23:657-664. [DOI] [PubMed] [Google Scholar]
- 57. Ray O. How the mind hurts and heals the body. Am Psychol. 2004;59:29-40. [DOI] [PubMed] [Google Scholar]
- 58. Ader R. Psychoneuroimmunology. Curr Dir Psychol Sci. 2001;10:94-98. [Google Scholar]
- 59. Lutgendorf SK, Costanzo ES. Psychoneuroimmunology and health psychology: an integrative model. Brain Behav Immun. 2003;17:225-232. [DOI] [PubMed] [Google Scholar]
- 60. Besedovsky H, Del Rey A, Sorkin E. Immune-neuroendocrine interactions. J Immunol. 1985;135(2 suppl):750s-754s. [PubMed] [Google Scholar]
- 61. Chrousos GP, Gold PW. The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA. 1992;267:1244-1252. Erratum in: JAMA. 1992;268:200 [PubMed] [Google Scholar]
- 62. Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21:55-89. [DOI] [PubMed] [Google Scholar]
- 63. Hellhammer DH, Wüst S, Kudielka BM. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology. 2009;34:163-171. [DOI] [PubMed] [Google Scholar]
- 64. McEwen BS. Mood disorders and allostatic load. Biol Psychiatry. 2003;54:200-207. [DOI] [PubMed] [Google Scholar]
- 65. Sephton SE, Sapolsky RM, Kraemer HC, Spiegel D. Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst. 2000;92:994-1000. [DOI] [PubMed] [Google Scholar]
- 66. Glaser R, Rabin B, Chesney M, Cohen S, Natelson B. Stress-induced immunomodulation: implications for infectious diseases? JAMA. 1999;281:2268-2270. [DOI] [PubMed] [Google Scholar]
- 67. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171-179. [DOI] [PubMed] [Google Scholar]
- 68. Carlson LE, Doll R, Stephen J, et al. Randomized controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer (Mindset). J Clin Oncol. 2013;31:3119-3126. Erratum in: J Clin Oncol. 2014;32:3686-3687. [DOI] [PubMed] [Google Scholar]
- 69. Carlson LE. Mindfulness-based interventions for physical conditions: a narrative review evaluating levels of evidence. ISRN Psychiatry. 2012;2012:651583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300:1350-1352. [DOI] [PubMed] [Google Scholar]
- 71. Nunes DFT, Rodriguez AL, da Silva Hoffmann F, et al. Relaxation and guided imagery program in patients with breast cancer undergoing radiotherapy is not associated with neuroimmunomodulatory effects. J Psychosom Res. 2007;63:647-655. [DOI] [PubMed] [Google Scholar]
- 72. Eremin O, Walker MB, Simpson E, et al. Immuno-modulatory effects of relaxation training and guided imagery in women with locally advanced breast cancer undergoing multimodality therapy: a randomised controlled trial. Breast. 2009;18:17-25. [DOI] [PubMed] [Google Scholar]
- 73. Walker LG, Walker MB, Ogston K, et al. Psychological, clinical and pathological effects of relaxation training and guided imagery during primary chemotherapy. Br J Cancer. 1999;80:262-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lengacher CA, Bennett MP, Gonzalez L, et al. Immune responses to guided imagery during breast cancer treatment. Biol Res Nurs. 2008;9:205-214. [DOI] [PubMed] [Google Scholar]
- 75. Academy for Guided Imagery. How guided imagery works. Mechanisms of action according to basic principles of interactive guided imagerySM 2015. http://acadgi.com/abouttheacademy/FAQs/index.html. Accessed February 10, 2016.
- 76. Chen K-M, Snyder M. A research-based use of Tai Chi/movement therapy as a nursing intervention. J Holist Nurs. 1999;17:267-279. [DOI] [PubMed] [Google Scholar]
- 77. Robins JL, McCain NL, Elswick RK, Jr, Walter JM, Gray DP, Tuck I. Psychoneuroimmunology-based stress management during adjuvant chemotherapy for early breast cancer. Evid Based Complement Alternat Med. 2013;2013:372908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bower JE, Greendale G, Crosswell AD, et al. Yoga reduces inflammatory signaling in fatigued breast cancer survivors: a randomized controlled trial. Psychoneuroendocrinology. 2014;43:20-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Rao RM, Nagendra HR, Raghuram N, et al. Influence of yoga on mood states, distress, quality of life and immune outcomes in early stage breast cancer patients undergoing surgery. Int J Yoga. 2008;1:11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Oh B, Butow P, Mullan B, et al. A critical review of the effects of medical Qigong on quality of life, immune function, and survival in cancer patients. Integr Cancer Ther. 2012;11:101-110. [DOI] [PubMed] [Google Scholar]
- 81. Chen K, Yeung R. Exploratory studies of Qigong therapy for cancer in China. Integr Cancer Ther. 2002;1:345-370. [DOI] [PubMed] [Google Scholar]
- 82. Oh B, Butow P, Mullan B, et al. Impact of medical Qigong on quality of life, fatigue, mood and inflammation in cancer patients: a randomized controlled trial. Ann Oncol. 2010;21:608-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Cohen L, Chen Z, Arun B, et al. External QiGong therapy for women with breast cancer prior to surgery. Integr Cancer Ther. 2010;9:348-353. [DOI] [PubMed] [Google Scholar]
- 84. Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822-848. [DOI] [PubMed] [Google Scholar]
- 85. Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12:278-285. [DOI] [PubMed] [Google Scholar]
- 86. Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR). Psychooncology. 2010;19:1004-1009. [DOI] [PubMed] [Google Scholar]
- 87. Ott MJ, Norris RL, Bauer-Wu SM. Mindfulness meditation for oncology patients: a discussion and critical review. Integr Cancer Ther. 2006;5:98-108. [DOI] [PubMed] [Google Scholar]
- 88. Altschuler A, Rosenbaum E, Gordon P, Canales S, Avins AL. Audio recordings of mindfulness-based stress reduction training to improve cancer patients’ mood and quality of life—a pilot feasibility study. Support Care Cancer. 2012;20:1291-1297. [DOI] [PubMed] [Google Scholar]
- 89. Monti DA, Peterson C, Kunkel EJ, et al. A randomized, controlled trial of mindfulness-based art therapy (MBAT) for women with cancer. Psychooncology. 2006;15:363-373. [DOI] [PubMed] [Google Scholar]
- 90. Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. 2006;62:373-386. [DOI] [PubMed] [Google Scholar]
- 91. Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62:613-622. [DOI] [PubMed] [Google Scholar]
- 92. Campbell TS, Labelle LE, Bacon SL, Faris P, Carlson LE. Impact of mindfulness-based stress reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: a waitlist-controlled study. J Behav Med. 2012;35:262-271. [DOI] [PubMed] [Google Scholar]
- 93. Shapiro SL, Brown KW, Biegel GM. Teaching self-care to caregivers: effects of mindfulness-based stress reduction on the mental health of therapists in training. Train Educ Prof Psychol. 2007;1:105-115. [Google Scholar]
- 94. Dobkin PL. Mindfulness-based stress reduction: What processes are at work? Complement Ther Clin Pract. 2008;14:8-16. [DOI] [PubMed] [Google Scholar]
- 95. Garland SN, Carlson LE, Cook S, Lansdell L, Speca M. A non-randomized comparison of mindfulness-based stress reduction and healing arts programs for facilitating post-traumatic growth and spirituality in cancer outpatients. Support Care Cancer. 2007;15:949-961. [DOI] [PubMed] [Google Scholar]
- 96. Ledesma D, Kumano H. Mindfulness-based stress reduction and cancer: a meta-analysis. Psychooncology. 2009;18:571-579. [DOI] [PubMed] [Google Scholar]
- 97. Matchim Y, Armer JM, Stewart BR. Mindfulness-based stress reduction among breast cancer survivors: a literature review and discussion. Oncol Nurs Forum. 2011;38:E61-E71. [DOI] [PubMed] [Google Scholar]
- 98. Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: a meta-analysis. Psychooncology. 2013;22:1457-1465. [DOI] [PubMed] [Google Scholar]
- 99. Subnis UB, Starkweather AR, McCain NL, Brown RF. Psychosocial therapies for patients with cancer: a current review of interventions using psychoneuroimmunology-based outcome measures. Integr Cancer Ther. 2013;13:85-104. [DOI] [PubMed] [Google Scholar]
- 100. Chan CL, Wang CW, Ho RT, et al. A systematic review of the effectiveness of Qigong exercise in supportive cancer care. Support Care Cancer. 2012;20:1121-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Center for Evidence-based Medicine. Center for evidenced-based medicine (CEBM) levels of evidence. 2009; http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/. Accessed March 12, 2015.
- 102. Zeng Y, Luo T, Xie H, Huang M, Cheng AS. Health benefits of Qigong or Tai Chi for cancer patients: a systematic review and meta-analyses. Complement Ther Med. 2014;22:173-186. [DOI] [PubMed] [Google Scholar]
- 103. Oh PJ, Kim SH. The effects of spiritual interventions in patients with cancer: a meta-analysis. Oncol Nurs Forum. 2014;41:E290-E301. [DOI] [PubMed] [Google Scholar]
- 104. Hsiao F, Jow G, Kuo W, et al. The effects of psychotherapy on psychological well-being and diurnal cortisol patterns in breast cancer survivors. Psychother Psychosom. 2012;81:173-182. [DOI] [PubMed] [Google Scholar]
- 105. Witek-Janusek L, Albuquerque K, Chroniak KR, Chroniak C, Durazo-Arvizu R, Mathews HL. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav Immun. 2008;22:969-981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Phillips KM, Antoni MH, Lechner SC, et al. Stress management intervention reduces serum cortisol and increases relaxation during treatment for nonmetastatic breast cancer. Psychosom Med. 2008;70:1044-1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Antoni MH, Lechner S, Diaz A, et al. Cognitive behavioral stress management effects on psychosocial and physiological adaptation in women undergoing treatment for breast cancer. Brain Behav Immun. 2009;23:580-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Vadiraja H, Raghavendra RM, Nagarathna R, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Integr Cancer Ther. 2009;8:37-46. [DOI] [PubMed] [Google Scholar]
- 109. Matchim Y, Armer JM, Stewart BR. Effects of mindfulness-based stress reduction (MBSR) on health among breast cancer survivors. West J Nurs Res. 2010;33:996-1016. [DOI] [PubMed] [Google Scholar]
- 110. Bränström R, Kvillemo P, Moskowitz JT. A randomized study of the effects of mindfulness training on psychological well-being and symptoms of stress in patients treated for cancer at 6-month follow-up. Int J Behav Med. 2012;19:535-542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Bränström R, Kvillemo P, Åkerstedt T. Effects of mindfulness training on levels of cortisol in cancer patients. Psychosomatics. 2013;54:158-164. [DOI] [PubMed] [Google Scholar]
- 112. Chen Z, Meng Z, Milbury K, et al. Qigong improves quality of life in women undergoing radiotherapy for breast cancer. Cancer. 2013;119:1690-1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Reich RR, Lengacher CA, Kip KE, et al. Baseline immune biomarkers as predictors of MBSR (BC) treatment success in off-treatment breast cancer patients. Biol Res Nurs. 2014;16:429-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Bower JE, Garet D, Sternlieb B, et al. Yoga for persistent fatigue in breast cancer survivors. Cancer. 2012;118:3766-3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Chandwani KD, Perkins G, Nagendra HR, et al. Randomized, controlled trial of yoga in women with breast cancer undergoing radiotherapy. J Clin Oncol. 2014;32:1058-1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Kiecolt-Glaser JK, Bennett JM, Andridge R, et al. Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2014;32:1040-1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Lengacher CA, Reich RR, Kip KE, et al. Influence of mindfulness-based stress reduction (MBSR) on telomerase activity in women with breast cancer (BC). Biol Res Nurs. 2014;16:438-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Carlson LE, Beattie TL, Giese-Davis J, et al. Mindfulness-based cancer recovery and supportive-expressive therapy maintain telomere length relative to controls in distressed breast cancer survivors. Cancer. 2015;121:476-484. [DOI] [PubMed] [Google Scholar]
- 119. Rossi D, Lobetti Bodoni C, Genuardi E, et al. Telomere length is an independent predictor of survival, treatment requirement and Richter’s syndrome transformation in chronic lymphocytic leukemia. Leukemia. 2009;23:1062-1072. [DOI] [PubMed] [Google Scholar]
- 120. Bisoffi M, Heaphy CM, Griffith JK. Telomeres: Prognostic markers for solid tumors. Int J Cancer. 2006;119:2255-2260. [DOI] [PubMed] [Google Scholar]
- 121. Boelens PA, Reeves RR, Replogle WH, Koenig HG. A randomized trial of the effect of prayer on depression and anxiety. Int J Psychiatry Med. 2009;39:377-392. [DOI] [PubMed] [Google Scholar]
- 122. Bormann JE, Aschbacher K, Wetherell JL, Roesch S, Redwine L. Effects of faith/assurance on cortisol levels are enhanced by a spiritual mantram intervention in adults with HIV: a randomized trial. J Psychosom Res. 2009;66:161-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. National Institute of Health. Grants and funding: rigor and reproducibility. 2015. http://grants.nih.gov/reproducibility/index.htm. Accessed February 10, 2016.