Abstract
Background:
Arthroscopic partial meniscectomy (APM) combined with physical therapy (PT) have yielded pain relief similar to that provided by PT alone in randomized trials of subjects with a degenerative meniscal tear. However, many patients randomized to PT received APM before assessment of the primary outcome. We sought to identify factors associated with crossing over to APM and to compare pain relief between patients who had crossed over to APM and those who had been randomized to APM.
Methods:
We used data from the MeTeOR (Meniscal Tear in Osteoarthritis Research) Trial of APM with PT versus PT alone in subjects ≥45 years old who had mild-to-moderate osteoarthritis and a degenerative meniscal tear. We assessed independent predictors of crossover to APM among those randomized to PT. We also compared pain relief at 6 months among those randomized to PT who crossed over to APM, those who did not cross over, and those originally randomized to APM.
Results:
One hundred and sixty-four subjects were randomized to and received APM and 177 were randomized to PT, of whom 48 (27%) crossed over to receive APM in the first 140 days after randomization. In multivariate analyses, factors associated with a higher likelihood of crossing over to APM among those who had originally been randomized to PT included a baseline Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Pain Score of ≥40 (risk ratio [RR] = 1.99; 95% confidence interval [CI] = 1.00, 3.93) and symptom duration of <1 year (RR = 1.74; 95% CI = 0.98, 3.08). Eighty-one percent of subjects who crossed over to APM and 82% of those randomized to APM had an improvement of ≥10 points in their pain score at 6 months, as did 73% of those who were randomized to and received only PT.
Conclusions:
Subjects who crossed over to APM had presented with a shorter symptom duration and greater baseline pain than those who did not cross over from PT. Subjects who crossed over had rates of surgical success similar to those of the patients who had been randomized to surgery. Our findings also suggest that an initial course of rigorous PT prior to APM may not compromise surgical outcome.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
Degenerative meniscal tears are a common clinical problem that presents management challenges. Symptomatic, radiographically apparent knee osteoarthritis affects over 10 million adults in the U.S.1, and up to 80% of individuals with knee osteoarthritis have imaging evidence of a meniscal tear2. More than 350,000 arthroscopic partial meniscectomies (APMs) are performed annually in the U.S., and thousands more are done worldwide, to treat meniscal tears presumed to be symptomatic in individuals with concomitant knee osteoarthritis3.
The efficacy of APM in patients with osteoarthritis and a meniscal tear was examined in 4 recent randomized controlled trials that compared APM with a standardized physical therapy (PT) regimen. Three of the trials did not demonstrate a statistically significant or clinically important difference in symptomatic outcomes between subjects randomized to APM with PT and those randomized to PT alone4-7. One trial documented a statistically significant and clinically meaningful advantage for surgery4. However, these trials are difficult to interpret because up to one-third of subjects randomized to the PT arm crossed over and had APM before assessment of the primary outcome4-6 (Table I).
TABLE I.
Proportion of Subjects Randomized to Nonoperative Therapy Who Crossed Over to Surgery and Proportion Randomized to Surgery Who Did Not Receive Surgery in Randomized Trials of Orthopaedic Surgical Interventions
| Condition/Surgery | Duration of Follow-up (yr) | Crossover from Nonoperative to Surgery* | Randomized to Surgery but Failed to Receive Surgery† |
| Meniscal tear/APM | |||
| Herrlin et al., 20135 | 2 | 13/49, 27% | 0/47, 0% |
| Katz et al., 20136 (>2-yr follow-up) | 1 | 64/177, 36% | 10/174, 6% |
| Yim et al., 20137 | 2 | 1/54, 2% | 0/54, 0% |
| Gauffin et al., 20144 | 2 | 16/75, 21% | 9/75, 12% |
| ACL tear/ACL reconstruction surgery: Frobell et al., 201024 | 2 | 23/59, 39% | 1/62, 2% |
| Lumbar spinal stenosis/standard posterior decompressive laminectomy | |||
| Weinstein et al., 201022 | 2 | 65/151, 43% | 46/138, 33% |
| Delitto et al., 201521 | 2 | 47/82, 57% | 2/87, 2% |
| Lumbar degenerative spondylolisthesis/standard posterior decompressive laminectomy with or without fusion: Weinstein et al., 200923 | 2 | 71/145, 49% | 58/159, 36% |
| Lumbar disc herniation/surgery: Lurie et al., 201420 | 2 | 110/256, 43% | 104/245, 42% |
Number randomized to nonoperative treatment/number crossed over, percent crossed over.
Number randomized to surgery/number failed to receive surgery, percent failed to receive surgery.
The trial findings raise 2 questions that are the focus of this paper. First, what factors identify patients who are likely to cross over from nonoperative therapy to APM? If trial investigators could identify these patients, they might attempt interventions to reduce the likelihood of early crossover, since crossovers complicate the interpretation of randomized trials. There is little published information on predictors of crossover to surgery in this setting or, more generally, on predictors of the outcome of nonoperative therapy for a degenerative meniscal tear. Rimington et al. found that men with a degenerative meniscal tear were more likely to undergo surgical treatment compared with women with such a tear8. Additionally, smaller tears have been shown to do well with conservative treatment, with fewer people with such tears requiring surgical intervention9.
Second, how successful is APM in relieving symptoms among patients who were randomized to PT and later crossed over to surgery as compared with patients originally randomized to APM? If those who crossed over to surgery did not do as well as those who had surgery at the outset, clinicians would be concerned that delay may compromise outcome. We address these questions using data from the MeTeOR (Meniscal Tear in Osteoarthritis Research) Trial.
Materials and Methods
Setting and Design
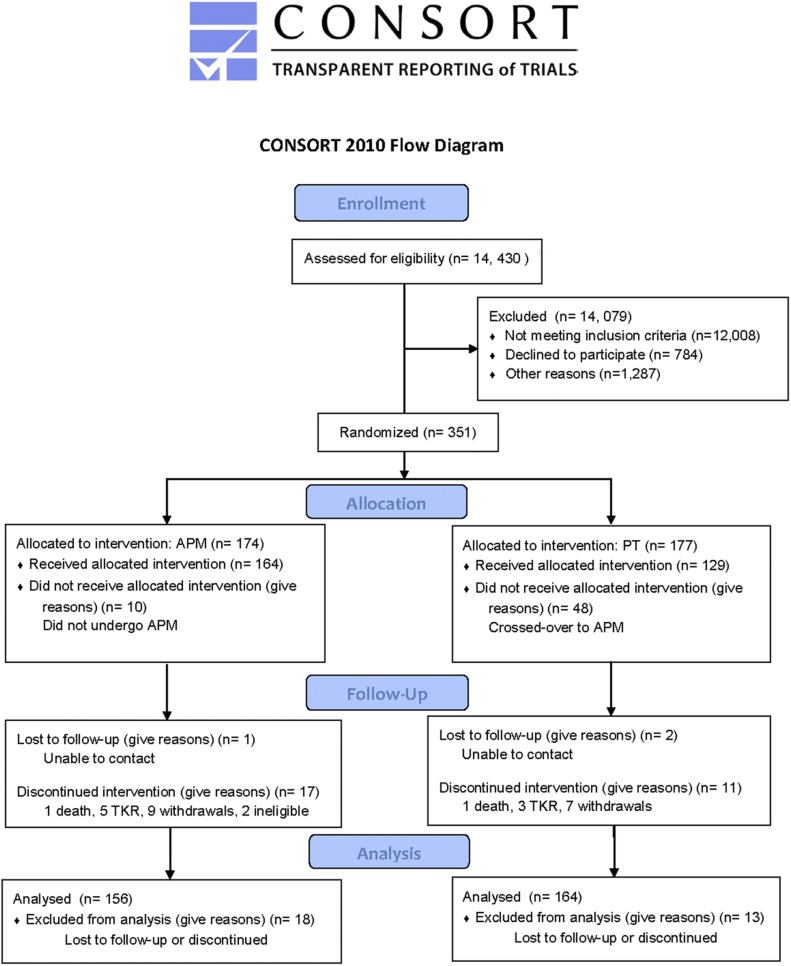
MeTeOR (ClinicalTrials.gov NCT00597012) is a 7-center randomized controlled trial of APM versus nonoperative therapy in subjects ≥45 years old with knee symptoms, a meniscal tear, and degenerative cartilage changes (including focal or diffuse cartilage defects) documented on radiographs and/or magnetic resonance imaging (MRI) studies. Subjects with Kellgren-Lawrence Grade-4 changes (>50% joint space narrowing) were excluded. Details of the study design, subject selection and enrollment, randomization, and outcome assessment have been reported previously6,10. Briefly, eligible subjects were randomized to receive either APM with a standardized PT regimen or the PT regimen alone without surgery. The details of the PT protocol was provided in Supplementary Materials attached to the original article on the trial6, and enrollment and follow-up in the parent trial are shown in Figure 1 of that study and the present study. Of the eligible subjects, 26% agreed to enroll in the study and were randomized. Neither the subjects nor the surgeons were blinded to treatment assignment. The trial was powered to detect an 8-point difference in the primary outcome (Western Ontario and McMaster Universities Osteoarthritis Index [WOMAC] Pain Score11) at 6 months.
Fig. 1.
Consort diagram for parent MeTeOR trial. TKR = total knee replacement.
Baseline Variables
Baseline variables were ascertained prior to randomization with self-report questionnaires and with a physical examination performed by a trained research assistant. These variables included age, sex, body mass index (BMI), duration of symptoms prior to enrollment, preoperative level of pain and functional status (measured with the WOMAC11 and Knee injury and Osteoarthritis Outcome Score [KOOS])12, mechanical symptoms, mental health status (measured with the 5-item Mental Health Inventory13), Kellgren-Lawrence radiographic grade, and several physical examination variables including passive knee flexion and extension, strength (measured with a handheld goniometer), muscle lengths, static knee alignment, and the result of the timed “up and go” test14-17.
Follow-up Protocol
Subjects completed questionnaires at the time of the 6-month follow-up after randomization. In this analysis, we examined baseline and 6-month data. We chose 6 months as the time to assess the primary outcome in order to capture the response to treatment, which is generally apparent at 6 months, while minimizing the potential for the pain score to reflect new problems in other lower-extremity joints or from another disease process in the index knee. The questionnaires included the WOMAC Pain and Function Scales and the KOOS Pain, Symptom, and Activity of Daily Living Scale. Study staff also called subjects every 2 weeks for the first 3 months after randomization to ascertain whether those assigned to surgery had undergone APM and whether those randomized to PT had crossed over and undergone APM.
Crossover Status
Subjects were permitted to see their orthopaedic surgeons throughout the study. If the subject and surgeon wished to proceed with surgery, the subject could cross over and undergo APM. At each follow-up call, study staff asked subjects whether they were continuing the original treatments or had crossed over to APM. Subjects were also asked about crossover each time that they completed a questionnaire. In these analyses, we included crossovers occurring in the first 140 days so that subjects would have at least 40 days to recover from surgery before the 6-month outcome assessment. Subjects randomized to surgery who did not ultimately undergo APM (6% of those randomized to surgery) were excluded from this analysis.
Statistical Analysis
We used generalized linear models with a binary outcome (crossover or not) to assess potential predictors of crossover to APM among those originally randomized to PT. We used a log link function to estimate risk ratios (RRs) rather than odds ratios (which take on more extreme values than RRs when used to assess a frequent outcome such as crossover). Potential predictors included duration of symptoms (dichotomized at 1 year), age, sex, BMI, preoperative level of pain and functional status, mechanical symptoms (as assessed with a 5-item inventory summed to a 0 to 100-point scale, in which 100 points is most severe, and dichotomized at 25 points), mental health status, Kellgren-Lawrence radiographic grade, and several physical examination variables as noted above. We considered variables with bivariate associations with crossover at p < 0.20 for inclusion in the multivariate model. We then manually eliminated variables that did not contribute meaningfully to arrive at a parsimonious model. We also compared the likelihood of achieving a ≥10-point improvement in the KOOS Pain Score (considered a clinically important improvement18) between those randomized to PT who crossed over to APM and those originally randomized to APM. Finally, to complement the analysis of the binary primary outcome—achieving a ≥10-point improvement—we also examined the difference between these 2 groups regarding the absolute improvement in the KOOS Pain Score (a continuous outcome).
Results
Features of Study Sample
Of the 351 subjects enrolled in the MeTeOR Trial, 174 were randomized to APM, of whom 164 received surgery, generally within 3 weeks after randomization. One hundred and seventy-seven were randomized to PT, of whom 48 (27%) crossed over to receive APM in the first 140 days after randomization. Another 16 crossed over between 140 days and 24 months. Of those randomized to PT, 59% were female and 64% were <60 years old; 76% had Kellgren-Lawrence Grade-0, 1, or 2 radiographic changes and 24% had Grade 3. Sixty-four percent of the subjects randomized to PT had a WOMAC Pain Score of ≥40 at baseline (on a scale of 0 to 100), indicating a moderately high level of knee pain.
Factors Associated with Crossover (Table II)
TABLE II.
Factors Associated with Crossover from Nonoperative to Surgical Therapy in MeTeOR Trial
| Crossover (No. [%])* |
Risk Ratio (95% CI) |
|||
| Factor | No | Yes | Bivariate Analysis | Multivariate Analysis |
| Sex | 1.28 (0.78, 2.11) | |||
| Male | 49 (74%) | 17 (26%) | ||
| Female | 63 (67%) | 31 (33%) | ||
| Age | 1.18 (0.73, 1.91) | |||
| <60 yr | 74 (72%) | 29 (28%) | ||
| ≥60 yr | 38 (67%) | 19 (33%) | ||
| Baseline pain (WOMAC) | 1.90 (1.05, 3.42) | 1.99 (1.00, 3.93) | ||
| <40 points | 46 (81%) | 11 (19%) | ||
| ≥40 points | 64 (63%) | 37 (37%) | ||
| Baseline function (WOMAC) | 1.32 (0.79, 2.21) | |||
| <37 points | 51 (74%) | 18 (26%) | ||
| ≥37 points | 44 (66%) | 23 (34%) | ||
| Mechanical symptoms (on 0 to 100-point scale) | 1.20 (0.72, 1.99) | |||
| <25 points | 56 (68%) | 26 (32%) | ||
| ≥25 points | 50 (74%) | 18 (26%) | ||
| BMI | 1.16 (0.68, 1.96) | |||
| <30 kg/m2 | 52 (67%) | 26 (33%) | ||
| ≥30 kg/m2 | 37 (71%) | 15 (29%) | ||
| Symptom duration | 1.65 (0.97, 2.83) | 1.74 (0.98, 3.08) | ||
| <1 yr | 48 (77%) | 14 (23%) | ||
| ≥1 yr | 52 (63%) | 31 (37%) | ||
| No. of comorbidities | 1.00 (0.82, 1.23) | |||
| 0-1 | 60 (71%) | 25 (29%) | ||
| ≥2 | 52 (70%) | 22 (30%) | ||
| Kellgren-Lawrence grade | 1.03 (0.55, 1.95) | |||
| <3 | 74 (72%) | 29 (28%) | ||
| 3 | 24 (73%) | 9 (27%) | ||
| Mental Health Index-5 item | 1.03 (0.64, 1.67) | |||
| <85 points | 56 (71%) | 23 (29%) | ||
| ≥85 points | 56 (70%) | 24 (30%) | ||
| Index foot planus | 1.45 (0.87, 2.43) | |||
| No | 85 (74%) | 30 (26%) | ||
| Yes | 23 (62%) | 14 (38%) | ||
| Knee flexion | 1.32 (0.81, 2.14) | |||
| <120° | 35 (65%) | 19 (35%) | ||
| ≥120° | 74 (73%) | 27 (27%) | ||
| Flexion contracture | 1.69 (0.83, 3.44) | |||
| <3° | 80 (67%) | 39 (33%) | ||
| ≥3° | 29 (81%) | 7 (19%) | ||
| Hamstring strength | 1.80 (0.97, 3.34) | |||
| <30 lb (<13.6 kg) | 42 (81%) | 10 (19%) | ||
| ≥30 lb (≥13.6 kg) | 66 (65%) | 35 (35%) | ||
| Swelling | 1.59 (0.78, 3.23) | |||
| No | 27 (79%) | 7 (21%) | ||
| Yes | 82 (67%) | 40 (33%) | ||
Totals across cells differ for the different factors because of missing data.
The data did not provide evidence that demographic factors, including age, sex, and BMI, were associated with crossing over to surgery among patients randomized to PT. Similarly, we did not observe evidence that meniscal symptoms (either aggregated or separated as intermittent locking or catching), medical comorbidities, or mental health were associated with crossover from PT to APM. Several physical examination factors, including varus and valgus knee alignment and quadriceps and hamstring muscle lengths, were also not associated with crossover status. In the bivariate analyses, a duration of symptoms of <1 year was associated with crossover (RR = 1.65; 95% confidence interval [CI] = 0.97, 2.83), as was a baseline WOMAC Pain Score of ≥40 (RR = 1.90; 95% CI = 1.05, 3.42). Subjects with hamstring strength of <30 lb (13.6 kg) (RR = 1.80; 95% CI = 0.97, 3.34), those with normal knee extension (RR = 1.69; 95% CI = 0.83, 3.44), and those with swelling (RR = 1.59; 95% CI = 0.78, 3.23) were also somewhat more likely to cross over to APM, although the associations did not reach significance.
In multivariate analyses, factors associated with a higher likelihood of crossing over to APM among those randomized to PT included a baseline WOMAC Pain Score of ≥40 (RR = 1.99; 95% CI = 1.00, 3.93) and a symptom duration of <1 year (RR = 1.74; 95% CI = 0.98, 3.08). With these variables included in the model, none of the other factors (e.g., hamstring strength, knee extension, or swelling) made a significant contribution.
We performed sensitivity analyses to examine the effects of different specifications of potential predictors of crossover. For example, we dichotomized the Kellgren-Lawrence grade at 0 and 1 versus 2 and 3. The newly dichotomized variable was not associated with crossover (RR = 1.29; 95% CI = 0.75, 2.20, for Grades 0 and 1 versus 2 and 3).
Association Between Crossover Status and Outcome of Surgery
The proportion of subjects who achieved a ≥10-point improvement in KOOS Pain Score was 82% in the group randomized to APM, 73% in the group randomized to PT who did not later cross over to APM, and 81% of the subjects who crossed over to APM. In multivariate analyses, those who crossed over to APM had a virtually identical likelihood of achieving a ≥10-point improvement in the KOOS Pain Score as subjects originally randomized to APM (RR = 0.95; 95% CI = 0.64, 1.41), after adjustment for baseline pain and duration of symptoms. The 2 groups also had similar absolute improvements in the KOOS Pain Score over 6 months. Subjects randomized to APM had an average improvement of 24.5 points (standard error [SE] = 1.5 points) and those randomized to PT who crossed over to APM had an average improvement of 27.1 points (SE = 2.8 points); the difference between the 2 groups averaged 2.7 points (SE = 3.2 points; p = 0.41).
Discussion
In this study, we examined factors associated with crossover from PT to APM and we compared the outcome, in terms of relief of symptoms, of APM between subjects randomized to APM and those who crossed over from PT to APM. The findings suggest that patients assigned to PT who are most likely to cross over to APM are those with a more acute and painful presentation, characterized by a short duration of symptoms and higher pain scores. The findings also suggest that patients who cross over to APM are as likely to experience improvement in pain scores as those originally randomized to APM.
In several trials comparing APM and nonoperative therapy for subjects with knee pain, a meniscal tear, and osteoarthritis, up to one-third of the patients assigned to nonoperative therapy crossed over to receive APM over the course of follow-up4-6 (Table I). These crossovers complicate interpretation of these trials, as subjects analyzed in the nonoperative arm actually underwent the surgical intervention but had to be included in the group to which they had been randomized in an intention-to-treat analysis. Substantial crossover from nonoperative to operative therapy has also been reported in trials of total knee replacement versus PT19; spine surgery versus usual care for lumbar disc protrusion20, lumbar spinal stenosis21,22, and degenerative spondylolisthesis23; and treatment of anterior cruciate ligament (ACL) tears24 (Table I). The authors of several prior trials comparing surgery and nonoperative therapy examined factors associated with crossover from nonoperative to surgical arms. Delitto et al. showed that lower educational status and greater baseline pain were associated with a higher risk of crossover in their trial comparing surgery and PT for lumbar spinal stenosis21. The SPORT (Spine Patient Outcomes Research Trial) investigators reported that subjects who crossed over from nonoperative therapy to surgery in a trial of surgery for lumbar disc protrusion, spinal stenosis, and degenerative spondylolisthesis had been more bothered by their symptoms and had expressed a greater preference for surgery at baseline compared with those who did not cross over23,25,26. Rimington et al. found that men with a degenerative meniscal tear were more likely than women with such a tear to undergo surgical treatment8. Also, smaller tears appear to be associated with greater success of conservative treatment9.
Our finding that subjects with greater pain at baseline were more likely to cross over to surgery is consistent with the prior findings described above. On the question of whether subjects who cross over to APM have outcomes similar to those of individuals originally randomized to surgery, our findings mirror those of Herrlin et al., who noted that the 13 patients who crossed over from their PT arm to their APM group had the same levels of improvement at the 6-month follow-up evaluation as those who had been randomized to APM5. Delitto et al. also noted that subjects randomized to decompressive surgery for spinal stenosis and those randomized to nonoperative therapy who later crossed over to surgery had similar outcomes21.
Several limitations of our study should be noted. In the MeTeOR Trial, only 26% of eligible subjects chose to participate, potentially limiting external validity6. Furthermore, the sample size was modest, with 48 subjects experiencing the outcome of interest—crossover to APM in the first 140 days after randomization to PT. In addition, because subjects were not randomized to either cross over or not cross over, our comparison of surgical results between those randomized to surgery and those who crossed over from PT to surgery is vulnerable to confounding. We addressed this issue with multivariate analysis and noted that the nearly identical outcomes between those randomized to APM and those who crossed over to APM persisted after adjustment with the factors available to us. We were not able to use MRI measures, activity level, or meniscal tear type as predictors of crossover, and we did not have objective measures of outcome. We also did not have information regarding patient preferences for surgery at baseline enrollment.
The strengths of this study include the prospective design, multicenter setting, and extensive array of baseline questionnaire and physical examination data.
These findings have implications for research and practice. From a research standpoint, crossovers complicate interpretation of clinical trials. Our findings suggest that crossovers are difficult to predict, as reflected by the modest risk ratios associated with the risk factors that we identified. However, the factors that we identified point toward a combination of characteristics placing a subject at risk for crossover: severe pain and a relatively short symptom duration. Investigators may wish to make special efforts to keep these subjects in nonoperative therapy. As indicated above, prior research has also documented higher crossover rates for subjects with greater baseline pain22,23,25,26. From a clinical standpoint, our data suggest that the outcome of surgery is probably similar between patients who undergo surgery earlier and those who do so after crossing over from PT. These findings underscore the emerging treatment recommendation in this clinical setting to try a PT regimen before opting for APM27. Finally, the similarity of the outcomes among subjects randomized to APM, those who crossed over to APM from PT, and those randomized to PT who did not cross over underscores the important role that patient preferences should play as patients and their clinicians discuss treatments for degenerative meniscal tears.
Footnotes
Investigation performed at Brigham and Women’s Hospital, Boston, Massachusetts; Cleveland Clinic, Garfield Heights, Ohio; Hospital for Special Surgery, New York, NY; Mayo Clinic, St. Paul, Minnesota; Vanderbilt University, Nashville, Tennessee; and Washington University, St. Louis, Missouri
Disclosure: This study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), which had no role in the design, execution, analysis, or reporting of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work.
References
- 1.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008. January;58(1):26-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, Einhorn TA, Felson DT. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003. January;85(1):4-9. [DOI] [PubMed] [Google Scholar]
- 3.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report. 2009. January 28;11:1-25. [PubMed] [Google Scholar]
- 4.Gauffin H, Tagesson S, Meunier A, Magnusson H, Kvist J. Knee arthroscopic surgery is beneficial to middle-aged patients with meniscal symptoms: a prospective, randomised, single-blinded study. Osteoarthritis Cartilage. 2014. November;22(11):1808-16. Epub 2014 Jul 30. [DOI] [PubMed] [Google Scholar]
- 5.Herrlin SV, Wange PO, Lapidus G, Hållander M, Werner S, Weidenhielm L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surg Sports Traumatol Arthrosc. 2013. February;21(2):358-64. Epub 2012 Mar 23. [DOI] [PubMed] [Google Scholar]
- 6.Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL, Donnell-Fink LA, Guermazi A, Haas AK, Jones MH, Levy BA, Mandl LA, Martin SD, Marx RG, Miniaci A, Matava MJ, Palmisano J, Reinke EK, Richardson BE, Rome BN, Safran-Norton CE, Skoniecki DJ, Solomon DH, Smith MV, Spindler KP, Stuart MJ, Wright J, Wright RW, Losina E. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013. May 2;368(18):1675-84. Epub 2013 Mar 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yim JH, Seon JK, Song EK, Choi JI, Kim MC, Lee KB, Seo HY. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013. July;41(7):1565-70. Epub 2013 May 23. [DOI] [PubMed] [Google Scholar]
- 8.Rimington T, Mallik K, Evans D, Mroczek K, Reider B. A prospective study of the nonoperative treatment of degenerative meniscus tears. Orthopedics. 2009. August;32(8). [DOI] [PubMed] [Google Scholar]
- 9.Weiss CB, Lundberg M, Hamberg P, DeHaven KE, Gillquist J. Non-operative treatment of meniscal tears. J Bone Joint Surg Am. 1989. July;71(6):811-22. [PubMed] [Google Scholar]
- 10.Katz JN, Chaisson CE, Cole B, Guermazi A, Hunter DJ, Jones M, Levy BA, Mandl LA, Martin S, Marx RG, Safran-Norton C, Roemer FW, Skoniecki D, Solomon DH, Spindler KP, Wright J, Wright RW, Losina E. The MeTeOR trial (Meniscal Tear in Osteoarthritis Research): rationale and design features. Contemp Clin Trials. 2012. November;33(6):1189-96. Epub 2012 Sep 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988. December;15(12):1833-40. [PubMed] [Google Scholar]
- 12.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998. August;28(2):88-96. [DOI] [PubMed] [Google Scholar]
- 13.Berwick DM, Murphy JM, Goldman PA, Ware JE Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991. February;29(2):169-76. [DOI] [PubMed] [Google Scholar]
- 14.Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA. Muscles: testing and function with posture and pain. Philadelphia: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 15.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991. February;39(2):142-8. [DOI] [PubMed] [Google Scholar]
- 16.Reinking MF, Bockrath-Pugliese K, Worrell T, Kegerreis RL, Miller-Sayers K, Farr J. Assessment of quadriceps muscle performance by hand-held, isometric, and isokinetic dynamometry in patients with knee dysfunction. J Orthop Sports Phys Ther. 1996. September;24(3):154-9. [DOI] [PubMed] [Google Scholar]
- 17.Schaubert KL, Bohannon RW. Reliability and validity of three strength measures obtained from community-dwelling elderly persons. J Strength Cond Res. 2005. August;19(3):717-20. [DOI] [PubMed] [Google Scholar]
- 18.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64 Epub 2003 Nov 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, Rasmussen S. A randomized, controlled trial of total knee replacement. N Engl J Med. 2015. October 22;373(17):1597-606. [DOI] [PubMed] [Google Scholar]
- 20.Lurie JD, Tosteson TD, Tosteson AN, Zhao W, Morgan TS, Abdu WA, Herkowitz H, Weinstein JN. Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial. Spine (Phila Pa 1976). 2014. January 1;39(1):3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Delitto A, Piva SR, Moore CG, Fritz JM, Wisniewski SR, Josbeno DA, Fye M, Welch WC. Surgery versus nonsurgical treatment of lumbar spinal stenosis: a randomized trial. Ann Intern Med. 2015. April 7;162(7):465-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weinstein JN, Tosteson TD, Lurie JD, Tosteson A, Blood E, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976). 2010. June 15;35(14):1329-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson AN, Birkmeyer N, Herkowitz H, Longley M, Lenke L, Emery S, Hu SS. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. Four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009. June;91(6):1295-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010. July 22;363(4):331-42. [DOI] [PubMed] [Google Scholar]
- 25.Weinstein JN, Lurie JD, Tosteson TD, Tosteson AN, Blood EA, Abdu WA, Herkowitz H, Hilibrand A, Albert T, Fischgrund J. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2008. December 1;33(25):2789-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H; SPORT Investigators. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008. February 21;358(8):794-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buchbinder R. Meniscectomy in patients with knee osteoarthritis and a meniscal tear? N Engl J Med. 2013. May 2;368(18):1740-1. Epub 2013 Mar 18. [DOI] [PubMed] [Google Scholar]