Abstract
Background and Aims:
Critical incident reporting helps to identify errors and formulate preventive strategies. Many countries have existing national reporting systems. Such a system is yet to be established in India. We aimed to study the incidence of critical events in the paediatric operation theatre (OT) of our institute.
Methods:
We conducted a prospective observational study of all children receiving anaesthesia in paediatric OT over a period of 1 year. They were monitored intraoperatively as well as postoperatively, and critical incidents were noted in terms of date and time of incident, location (OT/post-anaesthesia care unit, clinical category, age of patient, degree of patient harm resulting from the incident, description of what happened and duration of surgery. Percentage incidence of critical events was calculated.
Results:
A total of 1206 children received an anaesthetic during the study. Incidence of critical events was 8.9% (108). Airway and respiratory events were the maximum recorded accounting for 60 (55%) incidents. There were 43 cases of oxygen desaturation out of which 21 were attributable to laryngospasm. Cardiovascular events were 12 (11.1%). Medication-related incidents were 4 (3.8%). Severe harm was reported in ten incidents, and 1 death was reported. A few uncommon incidents like change in voice following use of a cuffed endotracheal tube and post-operative acute renal failure requiring haemodialysis were noted.
Conclusion:
Incidence of critical incidents was almost one for every ten patients, and the audit helped us establish policy guidelines in our institution.
Keywords: Anaesthesia, critical incidents, paediatric
INTRODUCTION
Patient safety is the cornerstone of good patient care. This is especially important in the operating room setup. The perioperative care of children is even more challenging resulting in set up of specialised paediatric care centres with professionals trained to cater to this patient population. Reporting of critical incidents and near misses is an established method of improving patient safety.[1] It provides insights into the system and plays a key role in learning from problems.[2] It allows lessons to be learnt, helps in implementing change and prevents similar incidents from occurring in future.[3] Most countries adopt a National Reporting system for identifying critical incidents, for example, Australian Incident Monitoring System (AIMS), United Kingdom (UK) National Reporting and Learning Systems (NRLS). However, in India, we do not have established reporting systems. Most of the previous studies of critical incident reporting are based on analysis of records.[1,4] We noted that in these studies, data were inadequate due to misclassification and lack of reporting.[5,6,7]
There are various international publications relating to analysis of incidents relevant to paediatric anaesthesia.[8,9,10] There are no such studies exclusive to the paediatric population in the Indian context. A previous Indian study on critical incident reporting in anaesthesia reported maximum incidents in 0-10 year age group compared to the adult population and attributed this to anatomical and physiological differences in this age group.[11]
Hence, we proposed to prospectively identify and analyse perioperative critical incidents relating to paediatric anaesthesia in our paediatric operation theatre (OT) to increase the accuracy and validity of reporting. The purpose of this study was to formulate a reporting system in our department which would help us to make recommendations for future practice and thus improve patient safety. Our primary objective was to study the incidence of critical events, and secondary objectives were to categorise them into the degree of harm they caused and to study their association with respect to the age of the child.
METHODS
We conducted a prospective observational study in paediatric surgery OT of a tertiary level teaching hospital. After obtaining Institutional Ethics Committee approval and waiver of parental consent, all children up to 15 years of age of either sex receiving an anaesthetic in the paediatric OT over a period of 1 year were included in the study. From previous year's records, the incidence of critical events in paediatric OT was 5%. Hence, to get sufficient sample for analysis and to draw valid inference, it was decided to carry out the study over a period of 1 year. Children having pre-operative cardiovascular compromise (hypotension, hypertension, arrhythmias) were excluded from cardiovascular adverse events. Hypotension was considered as systolic blood pressure (SBP) <5th percentile for age. Hypertension was considered as SBP >95th percentile for age. Those having pre-operative desaturation/hypercarbia (e.g., congenital diaphragmatic hernia [CDH], tracheoesophageal fistula) were excluded from respiratory adverse events. Oxygen saturation <94% was considered as desaturation and end-tidal carbon dioxide (ETCO2) >50 mm Hg was considered as hypercarbia. For laparoscopies ETCO2 values <60 mm Hg was not considered as a critical incident.
Surgeries included were thoracic, abdominal, genitourinary procedures, neurosurgeries and miscellaneous paediatric surgeries such as circumcision, examination and dressing under general anaesthesia, lymph node biopsy. Cardiac and ear nose throat (ENT) surgeries were not included as they are performed at other locations in our hospital. Participants were recruited on the day of surgery at the time of entry into the pre-operative area of OT. Pre-anaesthetic check (PAC) form was scrutinised by the consultant and child was reassessed. These children were then monitored intraoperatively by the same consultant as well as postoperatively in the post-anaesthesia care unit (PACU) by the 3rd year resident posted there for a period of 2 h. Standard American Society of Anesthesiologists recommended monitoring was used. This included an electrocardiogram and pulse rate on cardioscope, pulse oximetry, ETCO2, blood pressure and temperature. A critical incident register was created for the purpose of this study where incidents were noted down as and when they occurred, by the anaesthesiologist delivering the anaesthetic or observing the child in PACU.
A paediatric critical incident was defined as an event adversely affecting, or potentially affecting, the perioperative anaesthetic management of a patient aged 15 years or under.[1]
Degree of harm was assigned according to the definitions of incident severity used by NRLS as follows:[1] (a) no harm-no harm. (b) Low harm-any unexpected or unintended incident that required extra observation or minor treatment and caused minimal harm. (c) Moderate harm-any unexpected or unintended incident that resulted in further treatment, possible surgical intervention, cancelling of treatment or transfer to another area, and which caused short-term harm. (d) Severe harm-any unexpected or unintended incident that caused permanent or long-term harm and (e) death-any unexpected or unintended event that caused death.
The following observations were noted in the critical incident register: Date and time of incident, surgery posted for, location of incident (OT or PACU), clinical category of the incident, age of patient, degree of patient harm resulting from incident, description of what happened and duration of surgery.
The UK, NRLS has its own categorization systems for critical incidents.[1] We used the same system for classifying events in our OT. These were: (1) Assessment, (2) documentation, (3) medical device/equipment, (4) medication, (5) airway, (6) cardiovascular, (7) regional anaesthesia, (8) organisation and communication and (9) miscellaneous. A checklist was prepared and attached in the anaesthesia register and used as a reference for classifying critical incidents.
Critical incidents that occurred were treated as per the standard operating protocol of our OT and PACU.
Data were pooled and analysed by the principal and co-investigators from a secondary database prepared on Microsoft Office Excel® 2007 Spreadsheet and percentage incidence of critical events was calculated.
RESULTS
During the study of 1 year, 1206 children received an anaesthetic out of which 105 (8.70%) were neonates, 227 (18.8%) were infants, 317 (26.2%) were toddlers and 557 (46.1%) were older children. The incidence of critical events was 108/1206 (8.9%) in all age groups with almost similar incidence in each of the four groups [Figure 1]. Duration of surgery varied depending on the type of cases. 52 (48.14%) critical incidents were noted in short duration surgeries which lasted <2 h, 49 (45.37%) incidents occurred in surgeries lasting 2–6 h and 4 (0.03%) incidents occurred in surgeries lasting >6 h. There was no relation between the occurrence of critical events and duration of surgery.
Figure 1.
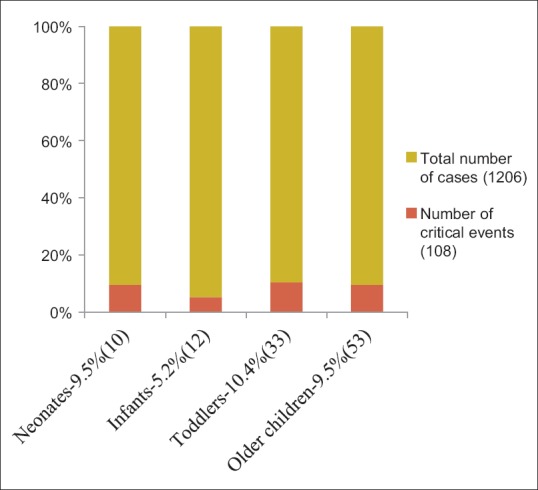
Incidence of critical events in different age groups (Percentage incidence reported on y axis. Incidence is reported as percentage [number of children] in each group on x axis)
Clinical Assessment accounted for 4 (3.7%) incidents. In a 3-year-old child posted for laparoscopic inguinal hernia repair, cardiac murmur was missed in the PAC done by the senior resident. This was detected on the morning of surgery by the consultant and the child was referred for echocardiography. In two children, surgery was cancelled as haematological investigations were not done. In a 5-year-old posted for muscle biopsy, pre-operative echocardiography was not available. The child developed ventricular premature contractions (VPC's) intraoperatively and needed additional observation postoperatively.
Documentation of events accounted for 2 (1.8%) incidents. There was one case where investigations of one child were interchanged in the file of another child. In another case, checklist was not read prior to induction. Antibiotic was not administered prior to incision in this case and was given at the end of the procedure.
There were two equipment-related incidents (2.7%). Anaesthesia machine and monitor suddenly shut down due to failure of battery backup as the mains had not been connected. In one case while switching over from closed to Jackson Rees's circuit at the end of the case, circuit connector could not be found. The patient was put back on closed circuit till it was retrieved below the surgical drapes.
Four (3.8%) incidents were medication related errors. Two were related to drug administration while two were adverse drug reactions. Intravenous (IV) atropine was administered instead of IV atracurium at induction. This was related to look alike syringe labelling (ATRO for atropine; 1 ml diluted to 5 ml and ATRA for atracurium prepared as a diluted solution in 5 ml syringe) and was noticed at the time of intubation when the patient was not relaxed. A 2-year-old boy developed chest rigidity following premedication with IV fentanyl. A 9-year-old boy developed hypotension, bronchospasm and desaturation following administration of gelofusine®. A 4-year-old girl developed adverse drug reaction (urticaria) along the hand over the IV line following administration of IV atracurium.
Airway and respiratory critical events were the maximum recorded and accounted for 60 (55.5%) incidents. There were 43 cases of oxygen desaturation out of which 21 were attributable to laryngospasm [Table 1]. This was related to the use of supraglottic airway devices (SGD) in 73% cases of laryngospasm. The SGD size was appropriately selected for weight of the child. We attributed this high incidence of SGD related laryngospasm to lighter plane of anaesthesia towards the end of surgery. In 12 cases, securing the airway was difficult. Out of these, four were neonatal intubations where the call for help was late which led to desaturation and bradycardia. Five children had difficult mask ventilation at induction. Six children required urgent reintubation post operatively, out of which three were Down's syndrome babies with associated hypothyroidism. 63% airway events were noted at recovery. Out of the total critical events reported 108 (8.9%); 9 out of 10 (90%) neonates, 10 out of 12 (83%) infants, 23 out of 33 (69%) toddlers and 18 out of 53 (33%) older children had airway-related events [Figure 2]. Thus the incidence of airway-related events decreased with increasing age.
Table 1.
Distribution of respiratory and airway critical incidents
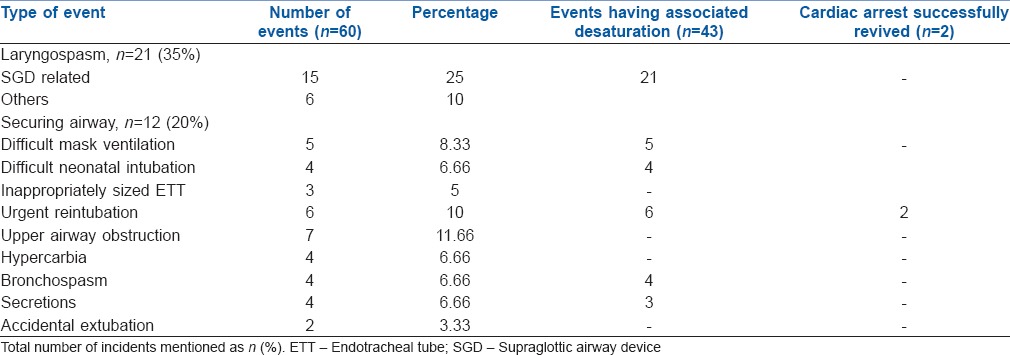
Figure 2.
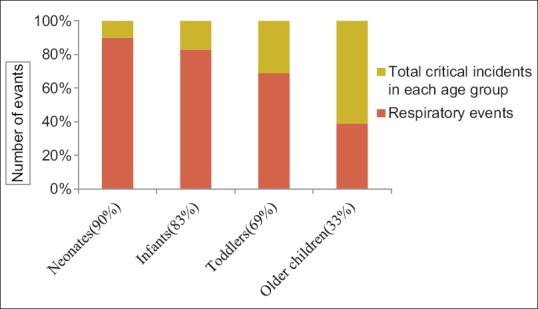
Percentage incidence of respiratory events with respect to age (different age groups represented on x axis with percentage incidence of respiratory events in each age group mentioned in brackets)
Cardiovascular events accounted for 12 (11.1%) of incidents. A 7-year-old child posted for anterior sagittal anorectoplasty developed atrial premature complexes during maintenance of anaesthesia which later on progressed to VPC's and then ventricular bigeminy. There were three incidences of bradycardia during recovery from anaesthesia. All three babies had Down's syndrome with hypothyroidism. There were four accidental carotid punctures during central venous catheterisation (CVC). All were by landmark technique. We recorded four cardiac arrests. The first was an 11-year-old girl posted for mediastinal mass excision. Accidental inferior vena cava injury during surgical manipulations resulted in massive haemorrhagic shock which progressed to cardiac arrest. Despite all attempts at resuscitation, the patient could not be revived. There were two bradycardia related cardiorespiratory arrests. Both children were hypothyroid and developed respiratory arrest in PACU which progressed to bradycardia necessitating resuscitation. A 3-day-old male child undergoing CDH repair developed sudden intraoperative bradycardia and cardiac arrest and was successfully resuscitated.
Five (4.6%) critical incidents were related to regional anaesthesia. There were four instances of accidental epidural catheter removal in PACU despite tunnelling and one case of dural puncture while instituting lumbar epidural anaesthesia.
One (0.9%) incident was recorded in organisation and communication events. A 4-year-old male child posted for herniotomy was fed milk on the morning of surgery despite pre-operative fasting orders. Case was postponed resulting in moderate harm.
Seventeen (15.7%) incidents were categorised as miscellaneous. There were three cases of accidental IV disconnection below the surgical drapes resulting in spillage of blood. Four children developed IV extravasation leading to a swollen and edematous limb and fever in PACU. There was one case of accidental CVC dislodgement while shifting a child from OT to PACU resulting in surgical emphysema over the neck. A 5-month-old female child undergoing colostomy developed cautery burn over caudal region. An 8-year-old female child underwent exploratory laparotomy with a 5.5 mm ID cuffed endotracheal tube in place for 5 h without cuff pressure monitoring. She did not vocalise for 2 days postoperatively. After speech therapy, she started vocalising on the fifth post-operative day. A 13-year-old female diagnosed as congenital adrenal hyperplasia underwent feminising genitoplasty. The child developed post-operative anuria and acute renal failure and eventually needed haemodialysis.
DISCUSSION
Reporting of critical incidents helps to gain insight into potential disasters. Critical incident analysis was first introduced by Flanagan in 1954 and was used in aviation.[12] In healthcare, Australia was the first country to set up AIMS on a national level in 1987.[13] It is currently in the form of an online database where anaesthesiologists report on an anonymous and voluntary basis any unintended incident which reduced or could have reduced the safety margin for a patient. Later, similar online reporting systems were set up in Switzerland and Germany.[2] This reporting enabled practitioners to investigate factors causing catastrophes and recommend changes.
In this prospective observational study, we analysed the critical incidents occurring over a 1 year period in the paediatric OT of a tertiary level teaching hospital. A total of 108 critical incidents were reported during this duration. Four incidents resulted in no harm, 29 in low harm, 64 in moderate harm, 10 in severe harm and 1 resulted in death [Figure 3]. Airway and respiratory events were the most predominant (55.5%). 70% of these events were noted in neonates, infants and toddlers while the rest were in older children. Incidents were more in the beginning of each month (46.29% of incidents occurred in the 1st week of each month). This was attributed to the monthly change in the anaesthesia resident team. 33 incidents were near misses (no harm/low harm). This entity has been described in previous critical incident reporting where the potential for harm is identified before any grave harm actually occurs.[14] The early pickup of near misses in these 33 incidents was important as they prevented a future mishap from occurring or reaching a point of no return.
Figure 3.
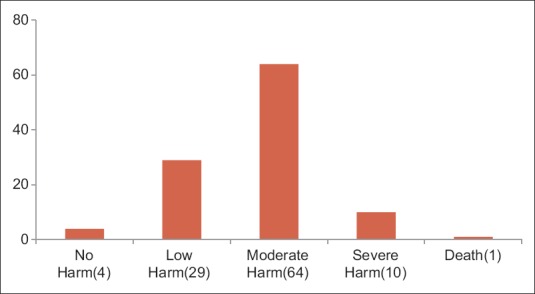
Degree of patient harm recorded (number of patients in each group mentioned in brackets)
The more serious incidents (arrest events and severe harm) led to combined surgical and anaesthesia team meets to stimulate discussions and analyse what went wrong and what could be done to prevent such events from occurring in future. This led us to formulate policy guidelines based on the results of our audit. We started briefing the new anaesthesia resident team in the beginning of each month. A protocol book was prepared for this purpose.
We reiterate the use of pre-operative check list and have it ready for every case to document consent, site and side of surgery, nil by mouth status, allergies, availability of equipment and instruments, anaesthesia machine and airway equipment check, antibiotic administration and anticipated critical events.
Based on the results of this study, we made a few recommendations for our practice. All preterm babies (<34 weeks) to be preferably extubated in PACU. Colour coding of drugs was started with use of red labels for muscle relaxants. We recommend extra care in fixation of epidural catheters. Nurses and parents should be educated about care especially during positioning, changing clothes, physiotherapy and mobilisation. We reinforce difficult airway society guidelines where the call for help should be early, after the first failed intubation and further intubation attempts should be taken over by an experienced anaesthesiologist. IV lines should be kept accessible below the surgical drapes to facilitate regular checks for disconnection. We came up with a policy of vigilance with Down's syndrome and hypothyroid babies especially in the post-operative period. We reinforce the use of cuff pressure monitoring while using cuffed endotracheal tubes especially for prolonged surgeries. CVC placement should be preferably done under ultrasound guidance. We urge anaesthesia and critical care departments to create a work attitude which encourages reporting and avoids blame. Critical incident reporting should be introduced in all anaesthesia departments as part of quality assurance programs to ensure improved patient care.[11]
There were a few limitations to this study. Fewer incidents were recorded during emergency hours. This was attributed to a change in the anaesthesia resident team who were not aware of the study or not compliant with recording events. The data were self-reported due to lack of automated anaesthesia recording systems which could have resulted in under reporting. ENT surgeries were not included. Airway-related incidences could have been still higher if they would have been included in this study.
CONCLUSION
Critical incident reporting provides an opportunity to increase perioperative safety of children. The anaesthesiologists should be encouraged to report critical incidents as a part of their routine clinical practice. Hospitals and anaesthesiology societies should set up hospital and national critical incident monitoring system.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.MacLennan AI, Smith AF. An analysis of critical incidents relevant to pediatric anesthesia reported to the UK National Reporting and Learning System, 2006-2008. Paediatr Anaesth. 2011;21:841–7. doi: 10.1111/j.1460-9592.2010.03421.x. [DOI] [PubMed] [Google Scholar]
- 2.Wan S, Siow YN, Lee SM, Ng A. Audits and critical incident reporting in paediatric anaesthesia: Lessons from 75,331 anaesthetics. Singapore Med J. 2013;54:69–74. doi: 10.11622/smedj.2013027. [DOI] [PubMed] [Google Scholar]
- 3.Smith AF, Mahajan RP. National critical incident reporting: Improving patient safety. Br J Anaesth. 2009;103:623–5. doi: 10.1093/bja/aep273. [DOI] [PubMed] [Google Scholar]
- 4.Marcus R. Human factors in pediatric anesthesia incidents. Paediatr Anaesth. 2006;16:242–50. doi: 10.1111/j.1460-9592.2005.01771.x. [DOI] [PubMed] [Google Scholar]
- 5.Leape LL. Error in medicine. JAMA. 1994;272:1851–7. [PubMed] [Google Scholar]
- 6.Taylor JA, Brownstein D, Christakis DA, Blackburn S, Strandjord TP, Klein EJ, et al. Use of incident reports by physicians and nurses to document medical errors in pediatric patients. Pediatrics. 2004;114:729–35. doi: 10.1542/peds.2003-1124-L. [DOI] [PubMed] [Google Scholar]
- 7.Vincent C, Stanhope N, Crowley-Murphy M. Reasons for not reporting adverse incidents: An empirical study. J Eval Clin Pract. 1999;5:13–21. doi: 10.1046/j.1365-2753.1999.00147.x. [DOI] [PubMed] [Google Scholar]
- 8.Tay CL, Tan GM, Ng SB. Critical incidents in paediatric anaesthesia: An audit of 10 000 anaesthetics in Singapore. Paediatr Anaesth. 2001;11:711–8. doi: 10.1046/j.1460-9592.2001.00767.x. [DOI] [PubMed] [Google Scholar]
- 9.Murat I, Constant I, Maud’huy H. Perioperative anaesthetic morbidity in children: A database of 24,165 anaesthetics over a 30-month period. Paediatr Anaesth. 2004;14:158–66. doi: 10.1111/j.1460-9592.2004.01167.x. [DOI] [PubMed] [Google Scholar]
- 10.Cohen MM, Cameron CB, Duncan PG. Pediatric anesthesia morbidity and mortality in the perioperative period. Anesth Analg. 1990;70:160–7. doi: 10.1213/00000539-199002000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Gupta S, Naithani U, Brajesh SK, Pathania VS, Gupta A. Critical incident reporting in anaesthesia: A prospective internal audit. Indian J Anaesth. 2009;53:425–33. [PMC free article] [PubMed] [Google Scholar]
- 12.Flanagan JC. The critical incident technique. Psychol Bull. 1954;51:327–58. doi: 10.1037/h0061470. [DOI] [PubMed] [Google Scholar]
- 13.Spigelman AD, Swan J. Review of the Australian incident monitoring system. ANZ J Surg. 2005;75:657–61. doi: 10.1111/j.1445-2197.2005.03482.x. [DOI] [PubMed] [Google Scholar]
- 14.Boëlle PY, Garnerin P, Sicard JF, Clergue F, Bonnet F. Voluntary reporting system in anaesthesia: Is there a link between undesirable and critical events? Qual Health Care. 2000;9:203–9. doi: 10.1136/qhc.9.4.203. [DOI] [PMC free article] [PubMed] [Google Scholar]


