Abstract
Background:
There is conflicting evidence as to whether the femoral head should be preserved or replaced in elderly patients with displaced intracapsular femoral neck fractures. In this article, we performed a systematic review and meta-analysis to compare the short- and long-term effectiveness of arthroplasty (AR) and internal fixation (IF).
Methods:
PubMed, Embase, and the Cochrane Library were searched systematically up to January 2016. All randomized controlled trials directly comparing the effectiveness of AR and IF for displaced intracapsular fracture were retrieved with no limitation on language or publication year.
Results:
In total, eight prospective randomized studies involving 2206 patients were included. The results of our study showed that patients in the AR group reported significantly lower complication (risk ratio: 0.56, 95% confidence interval [CI] = 0.38–0.80), re-operation (risk ratio: 0.17, 95% CI = 0.13–0.22), revision rates (risk ratio: 0.11, 95% CI: 0.08–0.16), and better function compared with their IF counterparts, and they were less likely to suffer postoperative pain. No statistically significant differences for the rates of mortality, infection, and/or deep vein thrombosis between AR and IF were found.
Conclusions:
Based on our analysis, we recommend that AR should be used as the primary treatment for displaced intracapsular femoral neck fractures in the elderly. However, IF may be appropriate for those who are very frail.
Keywords: Arthroplasty, Internal Fixation, Femoral Neck Fracture
Introduction
Femoral neck fractures are one of the most common orthopedic injuries in the elderly.[1,2,3,4] About 1.6 million individuals suffer from femoral neck fractures every year, of which more than 50% are intracapsular fractures.[5,6] According to several epidemiological studies, the incidence of femoral neck fracture will continue to increase, with an estimated incidence of 6.26 million in 2050.[6,7,8]
A displaced intracapsular femoral neck fracture is associated with a high incidence of nonunion and femoral head necrosis, as well as a significant mortality and disability.[9,10]
Although most femoral neck fractures in young, active patients are treated using reduction with internal fixation (IF),[11] there is conflicting evidence regarding the choice of surgical treatment for elderly patients with displaced intracapsular femoral neck fractures. Indeed, it has frequently been termed “the unsolved fracture.”[2,4,9]
Currently, this type of fracture is typically managed by arthroplasty (AR) or IF.[1,4] IF, including screw and plate fixation, has been reported to cause minor damage to soft tissue and to have shorter operation times and less intraoperative blood loss when compared with AR.[12,13,14] However, IF is also related to high morbidity of nonunion and femoral head avascular necrosis (with reported incidences of 20–35%, and 5–30%, respectively).[14] AR, including hemiarthroplasty (HA) and total hip arthroplasty (THA), entails replacing the femoral head with an artificial hip joint, which avoids the risk of nonunion or femoral head necrosis. The reported advantages of AR also include a low re-operation rate and early functional recovery.[14,15,16] However, AR involves more extensive soft tissue damage and a high risk of aseptic loosening.[1,10,14] Several short-to-intermediate term studies and the most recent systematic review indicated that AR may have an advantage over IF in terms of functional outcomes and re-operation rate.[9,17] However, to our knowledge, to date, very few systematic review or meta-analysis regarding long-term (>10 years postsurgery) results of AR and IF has been published. Thus, the supposed long-term superiority in the outcome of AR has not yet been clearly demonstrated.
We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) for the following purposes: (1) To investigate and compare the short- (<5 years) and long-term (>10 years) clinical effectiveness of AR and IF in elderly patients with displaced intracapsular femoral neck fractures, including the rates of complications, mortality, and revision and postoperative functional scores and (2) to do subgroup analysis of THA and HA with IF for further comparison.
Methods
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University, School of Medicine, and followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines[18] and the methods established in the Cochrane Handbook for Systematic Reviews of Interventions (version 5.0.2).
Literature search
Three independent investigators (Chen-Yi Ye, An Liu, and Ming-Yuan Xu) searched electronic databases (PubMed, the Cochrane Library, and Embase) with no language restriction through January 2016. The following Medical Subject Headings or key words were used: “femoral neck fracture” or “intracapsular” or “intraarticular” or “cervical” or “subcapital” and “arthroplasty” or “joint replacement” or “total hip arthroplasty” or “THA” or “total joint replacement” or “TJR” or “hemiarthroplasty” or “HA” and “internal fixation” or “IF” or “plate” or “screw.” We also manually searched reference lists for additional studies. The Clinical Trial Registry, the Current Controlled Trials databases, and the National Institutes of Health were also searched for unpublished trials and for those in progress.
Inclusion criteria
Two independent reviewers (Chen-Yi Ye and An Liu) screened manuscript titles and abstracts and identified articles that met the following eligibility criteria: (1) Randomized controlled design, (2) direct comparison of the AR and IF techniques reporting clinical outcomes, (3) enrollment of elderly individuals (≥60 years) with an acute displaced intracapsular femoral neck fracture (Garden III and IV classification), and (4) a minimum follow-up of 12 months. We excluded (1) articles that did not satisfy the inclusion criteria, (2) animal studies, cadaver studies, letters, abstracts, case reports, reviews, conference proceedings; (3) studies with no comparative data provided, and (4) studies with follow-up <1 year.
Data extraction
Three reviewers (Chen-Yi Ye, An Liu, and Ming-Yuan Xu) independently obtained relevant data and assessed accuracy. The following information was extracted from each study: family name of the first author, year of publication, study design, patient demographics (age, gender, interventions, and sample size), length of follow-up, complication rate, mortality rate, revision rate, and postoperative functional scores. We also attempted to contact the corresponding authors to verify the accuracy of the data, as well as to obtain any further data for the analysis.
Quality assessment
Two investigators (Chen-Yi Ye and An Liu) independently assessed the quality of the methodological data included in the studies based on the 12-item scale.[19] The 12-item scale comprised the following: adequately randomized, allocation concealed, patient blinded, outcome assessor blinded, care provider blinded, similar baseline, similar timing, similar or avoided cofactors, patient compliance, avoided selective reporting, acceptable dropout rate, and intention-to-treat analysis. Divergences were evaluated using kappa test, and consensus was obtained by discussion with the corresponding author (Rong-Xin He).
Statistical analysis
RevMan software (version 5.3; The Nordic Cochrane Centre, Copenhagen, Denmark) was used to pool the data. STATA 11.0 software (Stata Corp., College Station, TX, USA) was used to evaluate publication bias. P ≤ 0.05 was considered statistically significant. Relative risk (RR) and 95% confidence intervals (CIs) were calculated as summary statistics for dichotomous outcomes, while weighted mean differences (WMDs) or standardized mean differences (SMDs) with 95% CIs were calculated for continuous data.[20] Chi-square test on N − 1 degrees of freedom was used to evaluate statistical heterogeneity, with significance set at 0.05. I2 (I2 = [(Q − df)/Q] × 100%) was used to evaluate the percentage of the variability in effect estimates according to the heterogeneity. I2 values of 25%, 50%, and 75% were considered to indicate low, medium, and high heterogeneity, respectively.[21] If no statistical heterogeneity was detected (I2 < 50%), a fixed-effects model was used; otherwise, we used a random-effects model. If substantial heterogeneity across studies (I2 > 50%) was detected, post hoc sensitivity analysis was performed by omitting the outlier studies to determine the sources of heterogeneity. Begg's rank correlation test and Egger's regression test were used to assess publication bias.
Results
Literature search
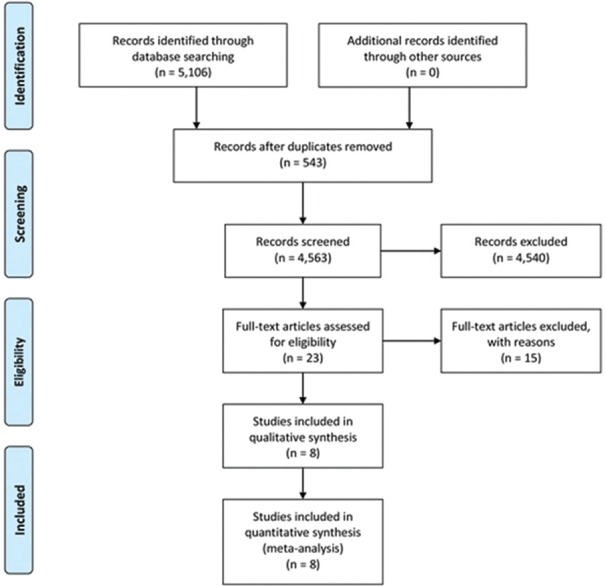
In total, the search identified 5106 candidate publications; however, 5083 were excluded due to duplications, nonrelevance, or because they were not RCTs. After assessing the 23 potentially relevant articles, eight RCTs involving 2206 patients met the inclusion criteria.[22,23,24,25,26,27,28,29] The primary reasons for exclusion were as follows: six were review articles,[11,30,31,32,33,34] six reported data that did not pertain to intracapsular hip fractures,[3,15,35,36,37,38] one was a correspondence letter,[39] and two studies were excluded because they were not RCTs.[40,41] Details of the selection process are shown in Figure 1. The weighted kappa for the agreement on eligibility between the reviewers was 0.88 (95% CI [0.83–0.94]).
Figure 1.
A Preferred Reporting Items for Systematic Reviews and Meta-analyses flowchart illustrated the selection of studies included in our systematic review.
Study characteristics
The characteristics and quality assessment results of the eight RCTs are summarized in Tables 1 and 2. Five studies compared HA with IF,[23,24,26,27,29] two studies compared both THA and HA with IF,[22,25] and one study compared THA and IF.[28] The mean length of follow-up ranged from 1 to 17 years. In total, 2206 patients were included in the analysis: 435 males and 1771 females aged from 62 to 103 years. Of these, 1184 patients received AR and 1022 patients received IF.
Table 1.
Methodological quality of the included studies based on the 12-item scoring system
| Study | Randomized adequately* | Allocation concealed | Patient blinded | Care provider blinded | Outcome assessor blinded | Acceptable dropout rate† | ITT analysis‡ | Avoided selective reporting | Similar baseline | Similar or avoided cofactor | Patient compliance§ | Similar timing | Quality|| |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ravikumar and Marsh, 2000[22] | Yes | Yes | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | High |
| Davison et al., 2001[23] | Yes | Yes | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | High |
| Parker et al., 2002[24] | Yes | Yes | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Unclear | Yes | Yes | Yes | Moderate |
| Keating et al., 2006[25] | Yes | Yes | Unclear | Unclear | Yes | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | High |
| Frihagen et al., 2007[26] | Yes | Yes | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Unclear | Moderate |
| Parker et al., 2010[27] | Yes | Yes | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | High |
| Chammout et al., 2012[28] | Yes | No | No | No | No | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | Moderate |
| Parker, 2015[29] | Yes | Yes | Unclear | Yes | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | High |
*Only if the method of sequence made was explicitly introduced could get a “yes;” sequence generated by “dates of admission” or “patients’ number” receives a “no;” †Dropout rate <20% could get a “yes,” otherwise “no;” ‡ITT: Intention-to-treat, only if all randomized participants were analyzed in the group they were allocated to could receive a “yes;” §More than 75% of the patients wore respective devices for at least 3 weeks means “yes,” otherwise “no;” ||“Yes” items >7 means “high”; “Yes” items more than 4 but no more than 7 means ‘‘Moderate’’; ‘Yes” items <4 means ‘‘Low’’.
Table 2.
Study characteristics and details of interventions of the included studies
| Studies | Study design | Age | Gender male/female | Number of patients | Interventions | Follow-up (years) | Prostheses | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AR | IF | AR | IF | AR | IF | AR | IF | ||||
| Ravikumar and Marsh 2000[22] | RCT | 81.55 ± 3.36 | 79.73 ± 2.49 | 27/244 | 180 | 91 | HA/THA | Screw/plate | 13 | HA: Austin Moore/THA: Howse II | Sliding compression screw plate |
| Davisonet al., 2001[23] | RCT | 75.48 ± 1.61 | 73 ± 1.75 | 67/213 | 187 | 93 | HA | Screw/plate | 5 | Thompson HA/Monk bipolar HA | Sliding compression screw plate |
| Parkeret al., 2002[24] | RCT | 82.4 ± 7.5 | 82.2 ± 8 | 91/364 | 229 | 226 | HA | Screw | 3 | Austin Moore | AO cancellous screws |
| Keatinget al., 2006[25] | RCT | 75.32 ± 6.62 | 74.68 ± 6.74 | 81/286 | 180 | 187 | HA/THA | Screw/plate | 2 | NA | NA |
| Frihagenet al., 2007[26] | RCT | 82.5 ± 7.32 | 83.2 ± 7.65 | 57/165 | 110 | 112 | HA | Screw | 2 | Charnley–Hastings bipolar HA | Olmed screw |
| Parkeret al., 2010[27] | RCT | 82.4 ± 7.5 | 82.2 ± 8 | 91/364 | 229 | 226 | HA | Screw | 11 | Austin Moore | AO cancellous screws (Stratec Ltd.) |
| Chammoutet al., 2012[28] | RCT | 78 ± 6.25 | 79 ± 6 | 21/79 | 43 | 57 | THA | Screw | 17 | Bi-metric | Olmed screw |
| Parker, 2015[29] | RCT | 81.2 ± 6.5 | 81.5 ± 8 | 0/56 | 26 | 30 | HA | Screw/plate | 1 | Exeter trauma stem | Targon femoral plate |
AR: Arthroplasty; IF: Internal fixation; THA: Total hip arthroplasty; HA: Hemiarthroplasty; NA: Not applicable; RCT: Randomized controlled trial.
Outcome measures
The pooled results are shown in Table 3.
Table 3.
The statistical comparison in outcomes between AR and IF
| Outcomes | Studies (n) | Participants | Event (n/N) | Mean (95% CI) | I2 (%) | P | |
|---|---|---|---|---|---|---|---|
| AR | IF | ||||||
| Total mortality rate - RR | 6 | 1826 | 587/954 | 501/872 | 1.02 (0.96, 1.08) | 25 | 0.63 |
| Mortality rate within 1 year | 5 | 1284 | 167/732 | 126/552 | 1.06 (0.86, 1.30) | 0 | 0.58 |
| Mortality rate within 2 years | 4 | 1324 | 221/706 | 180/618 | 1.15 (0.98, 1.34) | 0 | 0.08 |
| Mortality rate >10 years | 2 | 726 | 362/409 | 290/317 | 0.97 (0.90, 1.06) | 59 | 0.52 |
| Total re-operation rate - RR | 6 | 1738 | 63/864 | 378/874 | 0.17 (0.13, 0.22) | 10 | <0.00001 |
| Re-operation rate within 1 year | 2 | 336 | 3/213 | 28/123 | 0.07 (0.02, 0.22) | 0 | <0.00001 |
| Re-operation rate within 2 years | 3 | 869 | 28/477 | 138/392 | 0.19 (0.13, 0.27) | 0 | <0.00001 |
| Re-operation rate >10 years | 2 | 371 | 39/223 | 67/148 | 0.44 (0.31, 0.62) | 0 | <0.00001 |
| Total revision rate - RR | 7 | 1838 | 33/907 | 314/931 | 0.11 (0.08, 0.16) | 35 | <0.00001 |
| Revision rate within 1 year | 2 | 327 | 16/206 | 31/121 | 0.29 (0.16, 0.52) | 30 | <0.00001 |
| Revision rate within 2 years | 2 | 502 | 5/297 | 39/205 | 0.08 (0.03, 0.21) | 0 | <0.00001 |
| Revision rate >10 years | 2 | 555 | 16/272 | 112/283 | 0.15 (0.09, 0.25) | 8 | <0.00001 |
| Total complication rate - RR | 5 | 1415 | 177/742 | 294/673 | 0.56 (0.38, 0.80) | 76 | <0.01 |
| Total patients with pain - RR | 4 | 776 | 53/423 | 105/353 | 0.31 (0.23, 0.41) | 30 | <0.00001 |
| Patients with pain within 1 year | 2 | 551 | 97/409 | 69/317 | 0.50 (0.07, 3.55) | 0 | 0.16 |
| Patients with pain within 2 years | 3 | 869 | 23/339 | 39/338 | 0.70 (0.37, 1.34) | 0 | <0.05 |
| Patients with pain >10 years | 2 | 371 | 47/223 | 73/148 | 0.83 (0.32, 2.17) | 38 | <0.00001 |
| Infection rate - RR | 6 | 1598 | 36/832 | 30/766 | 1.06 (0.66, 1.71) | 15 | 0.81 |
| Infection rate within 1 year | 2 | 551 | 1/367 | 1/184 | 0.50 (0.07, 3.55) | 0 | 0.49 |
| Infection rate within 2 years | 3 | 869 | 14/477 | 20/392 | 0.70 (0.37, 1.34) | 0 | 0.28 |
| Infection rate >10 years | 2 | 371 | 10/223 | 7/148 | 0.83 (0.32, 2.17) | 0 | 0.7 |
| Deep vein thrombosis rate - RR | 4 | 1100 | 7/545 | 12/555 | 0.64 (0.27, 1.51) | 0 | 0.31 |
| Harris score within 1 year - WMD | 2 | 589 | NA/290 | NA/299 | 6.93 (4.33, 9.53) | 0 | <0.00001 |
| Harris score within 2 years - WMD | 2 | 589 | NA/290 | NA/299 | 3.60 (0.73, 6.47) | 0 | <0.05 |
| Operation time - WMD | 3 | 878 | NA/435 | NA/443 | 19.66 (15.44, 23.87) | 58 | <0.00001 |
| Blood loss - SMD | 2 | 677 | NA/339 | NA/338 | 1.87 (1.69, 2.05) | 0 | <0.00001 |
| Hospital stay -WMD | 3 | 558 | NA/323 | NA/235 | 1.09 (0.46, 1.73) | 25 | <0.01 |
AR: Arthroplasty; IF: Internal fixation; RR: Risk ratio; SMD: Standardized mean difference; WMD: Weighted mean difference; NA: Not applicable; CI: Confidence interval.
Mortality of 30 days, 3−6 months, and up to 1, 2, and 10 years
No statistically significant difference was found regarding mortality between AR and IF at 30 days and 3−6 months postoperatively (RR = 1.27, 95% CI = 0.74−2.17; P = 0.38 and RR = 1.21, 95% CI = 0.88−1.65; P = 0.25, respectively). In addition, there was also no statistically significant difference between groups in 1 or 2 years postoperatively (RR = 1.06, 95% CI = 0.86−1.30; P = 0.58 and RR = 1.15, 95% CI = 0.98−1.34; P = 0.08, respectively). No evidence of significant heterogeneity (I2 = 0) was observed within any subgroup, except a low heterogeneity (I2 = 59%) regarding the mortality rate of >10 years postoperatively. However, due to the limited number of available studies (n = 2), a sensitivity analysis was not possible.
Re-operation
The incidence of re-operations (including revision surgery, drainage of infected implants, fixation of periprosthetic fractures, removal of implants, reduction of dislocation, and excision AR) was reported in six studies (1738 patients, 441 events). These studies included 864 ARs and 874 IFs (re-operation events occurred in 63 and 378 cases, respectively). The pooled RR for re-operation after AR compared with IF was 0.17 (95% CI = 0.13−0.22; P < 0.00001, I2 = 10%). The re-operation rate following AR was significantly lower than for IF at 1, 2, and >10 years postoperatively (P < 0.00001). No evidence of heterogeneity was observed (I2 = 0%).
Revision
The total revision rates in the AR and IF groups were 33/907 and 314/931, respectively. The pooled RR for revision after AR versus IF was 0.11 (95% CI = 0.08–0.16; P < 0.0001, I2 = 35%). AR was associated with significantly lower revision rates than IF at 1, 2, and >10 years postoperatively (P < 0.00001). No evidence of significant heterogeneity was observed (I2 < 50%).
Complications
Details of complications are shown in Table 3. AR was associated with significantly fewer total complications (fixation failure, femoral head necrosis, nonunion, dislocation, and perioperative complications, including deep wound infection, deep venous thrombosis (DVT), myocardial infarction, pulmonary embolism, and stroke) than IF (RR = 0.56; 95% CI = 0.38−0.80; P < 0.01, I2 = 76%). No significant difference in infection or DVT rates was found (P > 0.05, I2 = 0). A sensitivity analysis was performed for the results of total complication rates, which yielded similar results to those obtained when all studies were analyzed simultaneously.
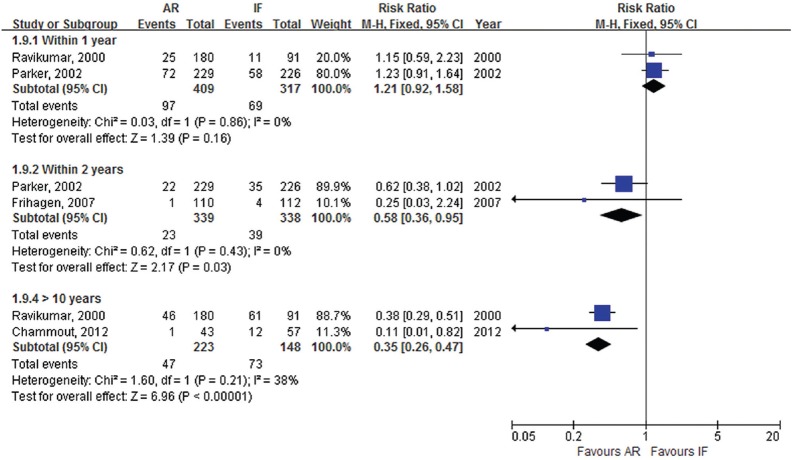
Pain
Pain was reported in four studies (776 patients, 158 events). Pain was more frequent in patients treated with IF (105/353, 29.7%) than those treated with AR (53/423, 12.5%) (RR = 0.31; 95% CI = 0.23−0.41; P < 0.00001, I2 = 30%). Subgroup analysis regarding the length of follow-up showed no statistically significant difference between AR and IF in 1 year postoperatively. However, patients treated with AR group had significantly less pain than those receiving IF at 2 and >10 years after the operation (P < 0.05). Heterogeneity was not significant (I2 < 50%) [Figure 2].
Figure 2.
Relative risk and 95% confidence interval for the number of patients with moderate-to-severe pain.
Functional scores
Functional scores were reported in two studies including 589 patients. The pooled WMDs of mean Harris hip score for AR versus IF was 6.93 (95% CI = 4.33−9.53; P < 0.00001, I2 = 0) and 3.60 (95% CI = 0.73−6.47; P < 0.05, I2 = 0) at 1 and 2 years after the operation, respectively. Patients treated with AR appear to have had better postoperative function than those treated with IF.
Other data
IF was associated with significantly shorter operation times (WMD, 19.66; 95% CI = 15.44–23.87; P < 0.00001, I2 = 58%), less blood loss (SMD, 1.87, 95% CI = 1.69–2.05; P < 0.00001, I2 = 0%), and fewer in-hospital days (WMD, 1.09; 95% CI = 0.46–1.73; P < 0.01, I2 = 25%) when compared with AR. No statistically significant difference was found between AR and IF.
Subgroup analyses
Results of subgroup analyses of the statistical comparison in outcomes between HA, THA, and IF are shown in Table 4. Both HA and THA were superior to IF in terms of re-operation, revision, and pain, whereas IF was associated with significantly shorter operation times, hospital stays, and less blood loss. No statistically significant difference in mortality, infection, or deep vein thrombosis rates was found.
Table 4.
Subgroup analysis of the statistical comparison in outcomes between HA, THA, and IF
| Outcomes | Studies | Participants | Event | Mean (95% CI) | I2 (%) | P | |
|---|---|---|---|---|---|---|---|
| AR | IF | ||||||
| Subgroup analysis between HA and IF | |||||||
| Total mortality rate -RR | 6 | 1697 | 478/892 | 428/805 | 1.06 (0.99, 1.14) | 15 | 0.11 |
| Total re-operation rate - RR | 6 | 1600 | 57/795 | 351/805 | 0.16 (0.13, 0.21) | 15 | <0.00001 |
| Total revision rate - RR | 6 | 1695 | 29/892 | 266/803 | 0.10 (0.07, 0.15) | 0 | <0.00001 |
| Total complications - RR | 4 | 1088 | 117/431 | 191/435 | 0.55 (0.37, 0.82) | 36 | <0.01 |
| Total patients with pain - RR | 3 | 859 | 62/430 | 89/429 | 0.69 (0.54, 0.89) | 0 | <0.01 |
| Infection rate - RR | 5 | 1506 | 30/797 | 24/709 | 1.23 (0.73, 2.08) | 27 | 0.44 |
| Deep vein thrombosis - RR | 4 | 962 | 3/476 | 9/486 | 0.45 (0.15, 1.33) | 0 | 0.15 |
| Harris hip score within 2 years - WMD | 2 | 434 | NA/212 | NA/222 | 3.21 (−0.12, 6.53) | 0 | 0.06 |
| Operation time - WMD | 2 | 285 | NA/137 | NA/148 | 0.59 (0.11, 1.08) | 62 | <0.05 |
| Blood loss - SMD | 2 | 677 | NA/339 | NA/338 | 1.87 (1.69, 2.05) | 0 | <0.00001 |
| Hospital stay - WMD | 3 | 558 | NA/323 | NA/235 | 1.09 (0.46, 1.73) | 25 | <0.01 |
| Subgroup analysis between THA and IF - RR | |||||||
| Total mortality rate | 2 | 318 | 78/158 | 91/160 | 0.87 (0.76, 1.01) | 0 | 0.06 |
| Total re-operation rate | 3 | 418 | 23/201 | 94/217 | 0.28 (0.19, 0.42) | 17 | <0.00001 |
| Total revision rate | 3 | 418 | 10/201 | 78/217 | 0.15 (0.08, 0.27) | 45 | <0.00001 |
| Total complications | 3 | 418 | 33/158 | 35/160 | 0.72 (0.38, 1.35) | 0 | 0.81 |
| Total patients with pain | 2 | 280 | 6/132 | 73/148 | 0.09 (0.04, 0.19) | 0 | <0.00001 |
| Infection rate | 3 | 418 | 6/201 | 11/217 | 0.59 (0.23, 1.54) | 0 | 0.28 |
HA: Hemiarthroplasty; THA: Total hip arthroplasty; AR: Arthroplasty; IF: Internal fixation;RR: Risk ratio; SMD: Standardized mean difference; WMD: Weighted mean difference; NA: Not applicable; CI: Confidence interval.
Publication bias
No substantial asymmetry was identified using Begg's rank correlation test (Z = 0.75, P = 0.452) or Egger's regression test (t = 0.17, P = 0.874).
Discussion
In the absence of a new study of the long-term efficacy for AR and IF, we conducted this systematic review and meta-analysis of eight RCTs, trying to provide updated evidence by comparing the short- and long-term clinical effectiveness of AR and IF for elderly patients with displaced intracapsular femoral neck fractures. The pooled results of long-term follow-up suggest that relative to IF, AR leads to lower total rates of re-operation, revision, and major method-related complications, without increasing the mortality. Moreover, patients treated with AR seemed to suffer less persistent pain and possibly have better postoperative function than those receiving IF.
The most recent previous systematic review about IF versus AR for adults with intracapsular proximal femoral fractures[9] showed that IF was associated with less operative trauma but had an increased risk of re-operation (40% vs. 11%; RR = 3.22, 95% CI = 2.31–4.47). This study also found that IF has a significantly shorter length of operation, less intraoperative blood loss, and less incidence of deep wound infection than AR. No significant difference regarding hospital stay or mortality was observed.[9] However, due to the limited number of available studies, comparisons regarding long-term re-operation rates, revision rates, and patients with persistent pain between AR and IF were not made. Because AR was not widely used in the 1990s for femoral neck fractures, we excluded RCTs published before 2000. Moreover, we included all RCTs with long-term follow-up (>10 years)[22,27,28] and all RCTs focusing only on elderly patients. Similar results to the previous study were found regarding short-term mortality, re-operation, incidence of persistent pain, and perioperative parameters, including the length of operation and intraoperative blood loss. However, our study indicated the long-term superiority of AR in terms of re-operation, revision, and the incidence of persistent pain. No significant difference regarding infection rate was observed.
The long-term re-operation rate is one of the most important parameters for evaluating AR and IF. It is difficult to pool data regarding re-operation because of the varied definitions across studies. To manage this, we subdivided re-operations into two categories: total re-operation rates and revision rates. The large number of patients requiring a second operation is of concern. Re-operation rates between 30% and 50% have been reported after IF for displaced intracapsular femoral neck fractures.[14,42] The previous review article indicated that IF was associated with an increased risk of re-operation when compared with AR (40% vs. 11%).[9] In this study, similar results for IF were observed (43.2%), while the observed re-operation rate in the AR group was lower (7.3%). Our study showed that AR might not only lead to fewer long-term re-operations but also fewer revisions than IF. However, some of these patients had more than one re-operation, and the times of re-operations were often not reported. Moreover, as noted by Parker,[29] the application of newer implants in IF may be associated with a reduction in the revision rate. More RCTs directly comparing different IF implants are needed in the future, with both short- and long-term follow-ups.
The long-term pain rate was significantly higher for IF group than AR. By conducting a subgroup analysis, we found that this difference existed at 2 and >10 years postoperatively while no statistically significant difference was observed in the 1st year after the primary surgery. The reasons, we suggest, may be largely related to the high incidence of avascular necrosis, nonunion, and mechanical failure of implants following IF.[22,23,24,25,26,27,28,29] Attempting to minimize the influence of different descriptions of pain across studies, the analyses only documented the number of patients with persistent pain; results based on different scoring systems were not pooled.
Although IF was favored in terms of perioperative parameters, there was no significant difference between AR and IF with respect to mortality at any follow-up time point, consistent with the results of Parker and Gurusamy.[9] The reason, we suggest, may be the study population; we included only elderly patients, with a mean age of >70 years, meaning that most of the patients (1088 of 1826 patients in six studies, 59.58%) were lost because of natural death. For the same reason, comparison of long-term mortality rates is of little value.[17]
With respect to total complications, including fixation failure, femoral head necrosis, nonunion, dislocation, and perioperative complications, the present study indicated a lower total complication rate following AR than IF. The avoided risk of nonunion or femoral head necrosis and the reported low re-operation rate of AR may contribute to this.[14,15,16] However, the subgroup analysis revealed that this difference was specific to THA versus IF. Further well-designed RCTs of high quality are needed.
The pooled data for the Harris hip score at 1 and 2 years after surgery showed that AR may increase the chances of early functional recovery. The Harris hip score difference between AR and IF in the present study was 3.6 points at 2 years postoperatively, which is less than the minimal clinically important difference of 4 points,[43] suggesting AR might not be preferential to IF in terms of overall functional recovery.
We acknowledge that our study has several limitations. The limitations include: (1) The limited number of RCTs comparing AR with IF with long-term follow-up. Our systematic review and meta-analysis included eight RCTs; three reported results with a follow-up of >10 years. Future RCTs with large samples and long-term follow-up are still needed, (2) the wide range of implants used both for IF and AR may increase bias. However, this variety of usage is likely to continue in clinical practice. Future studies based on different types of prostheses would be of interest, (3) information on cost-effectiveness and long-term function was not available, (4) some caution is needed when considering the results of this study because of the age and the underlying diseases of the included patients, which may influence the results such as infection rate or deep vein thrombosis rates. Future comprehensive analyses regarding the optimal treatment for displaced intracapsular femoral neck fractures are still needed. Despite these limitations, the study does provide useful insights into the long-term effectiveness of AR and IF for displaced intracapsular femoral neck fractures in the elderly.
In conclusion, based on our analysis, we recommend that AR should be used as the primary treatment for displaced intracapsular femoral neck fractures in the elderly. However, IF may be appropriate for those who are very frail.
Financial support and sponsorship
This work was supported by the grant from the National Natural Science Foundation of China (No. 81572124).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang and Li-Min Chen
References
- 1.Parker MJ, Pryor GA. Internal fixation or arthroplasty for displaced cervical hip fractures in the elderly: A randomised controlled trial of 208 patients. Acta Orthop Scand. 2000;71:440–6. doi: 10.1080/000164700317381090. doi: 10.1080/000164700317381090. [DOI] [PubMed] [Google Scholar]
- 2.Singer BR, McLauchlan GJ, Robinson CM, Christie J. Epidemiology of fractures in 15,000 adults: The influence of age and gender. J Bone Joint Surg Br. 1998;80:243–8. doi: 10.1302/0301-620x.80b2.7762. [DOI] [PubMed] [Google Scholar]
- 3.Rogmark C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg Br. 2002;84:183–8. doi: 10.1302/0301-620x.84b2.11923. doi: http://dx.doi.org/10.1302/0301-620X.84B2.11923. [DOI] [PubMed] [Google Scholar]
- 4.Parker MJ. The management of intracapsular fractures of the proximal femur. J Bone Joint Surg Br. 2000;82:937–41. doi: 10.1302/0301-620x.82b7.11595. doi: http://dx.doi.org/10.1302/0301-620X.82B7.11595. [DOI] [PubMed] [Google Scholar]
- 5.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–33. doi: 10.1007/s00198-006-0172-4. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 6.Lofthus CM, Osnes EK, Falch JA, Kaastad TS, Kristiansen IS, Nordsletten L, et al. Epidemiology of hip fractures in Oslo, Norway. Bone. 2001;29:413–8. doi: 10.1016/s8756-3282(01)00603-2. [DOI] [PubMed] [Google Scholar]
- 7.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–7. doi: 10.1016/S0140-6736(02)08657-9. doi: 10.1016/s0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 8.Riggs BL, Melton LJ., 3rd The worldwide problem of osteoporosis: Insights afforded by epidemiology. Bone. 1995;17(5 Suppl):505S–11S. doi: 10.1016/8756-3282(95)00258-4. doi: http://dx.doi.org/10.1016/8756-3282(95)00258-4. [DOI] [PubMed] [Google Scholar]
- 9.Parker MJ, Gurusamy K. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev. 2006;(4):CD001708. doi: 10.1002/14651858.CD001708.pub2. doi: 10.1002/14651858.CD001708.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993;75:797–8. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 11.Damany DS, Parker MJ, Chojnowski A. Complications after intracapsular hip fractures in young adults. A meta-analysis of 18 published studies involving 564 fractures. Injury. 2005;36:131–41. doi: 10.1016/j.injury.2004.05.023. doi: 10.1016/j.injury.2004.05.023. [DOI] [PubMed] [Google Scholar]
- 12.Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Joint Surg Am. 2005;87:1680–8. doi: 10.2106/JBJS.D.02655. doi: 10.2106/jbjs.d.02655. [DOI] [PubMed] [Google Scholar]
- 13.van Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ. Hip fracture in elderly patients: Outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res. 2001;(390):232–43. doi: http://dx.doi.org/10.1097/00003086-200109000-00027. [PubMed] [Google Scholar]
- 14.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76:15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Johansson T, Jacobsson SA, Ivarsson I, Knutsson A, Wahlström O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: A prospective randomized study of 100 hips. Acta Orthop Scand. 2000;71:597–602. doi: 10.1080/000164700317362235. doi: 10.1080/000164700317362235. [DOI] [PubMed] [Google Scholar]
- 16.Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P, 3rd, Obremskey W, Koval KJ, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003;85-A:1673–81. doi: 10.2106/00004623-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: A meta-analysis of 14 randomized studies with 2,289 patients. Acta Orthop. 2006;77:359–67. doi: 10.1080/17453670610046262. doi: 10.1080/17453670610046262. [DOI] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Furlan AD, Pennick V, Bombardier C, van Tulder M. 2009 updated method guidelines for systematic reviews in the cochrane back review group. Spine (Phila Pa 1976) 2009;34:1929–41. doi: 10.1097/BRS.0b013e3181b1c99f. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 20.Walter SD, Yao X. Effect sizes can be calculated for studies reporting ranges for outcome variables in systematic reviews. J Clin Epidemiol. 2007;60:849–52. doi: 10.1016/j.jclinepi.2006.11.003. doi: 10.1016/j.jclinepi.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur-13 year results of a prospective randomised study. Injury. 2000;31:793–7. doi: 10.1016/s0020-1383(00)00125-x. [DOI] [PubMed] [Google Scholar]
- 23.Davison JN, Calder SJ, Anderson GH, Ward G, Jagger C, Harper WM, et al. Treatment for displaced intracapsular fracture of the proximal femur. A prospective, randomised trial in patients aged 65 to 79 years. J Bone Joint Surg Br. 2001;83:206–12. doi: 10.1302/0301-620x.83b2.11128. [DOI] [PubMed] [Google Scholar]
- 24.Parker MJ, Khan RJ, Crawford J, Pryor GA. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures in the elderly. A randomised trial of 455 patients. J Bone Joint Surg Br. 2002;84:1150–5. doi: 10.1302/0301-620x.84b8.13522. doi: http://dx.doi.org/10.1302/0301-620X.84B8.13522. [DOI] [PubMed] [Google Scholar]
- 25.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88:249–60. doi: 10.2106/JBJS.E.00215. doi: 10.2106/jbjs.e.00215. [DOI] [PubMed] [Google Scholar]
- 26.Frihagen F, Nordsletten L, Madsen JE. Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: Randomised controlled trial. BMJ. 2007;335:1251–4. doi: 10.1136/bmj.39399.456551.25. doi: 10.1136/bmj.39399.456551.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parker MJ, Pryor G, Gurusamy K. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures: A long-term follow-up of a randomised trial. Injury. 2010;41:370–3. doi: 10.1016/j.injury.2009.10.003. doi: 10.1016/j.injury.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Chammout GK, Mukka SS, Carlsson T, Neander GF, Stark AW, Skoldenberg OG. Total hip replacement versus open reduction and internal fixation of displaced femoral neck fractures: A randomized long-term follow-up study. J Bone Joint Surg Am. 2012;94:1921–8. doi: 10.2106/JBJS.K.01615. doi: 10.2106/jbjs.k.01615. [DOI] [PubMed] [Google Scholar]
- 29.Parker MJ. Hemiarthroplasty versus internal fixation for displaced intracapsular fractures of the hip in elderly men: A pilot randomised trial. Bone Joint J. 2015;97-B:992–6. doi: 10.1302/0301-620X.97B7.35524. doi: 10.1302/0301-620x. 97b7.35524. [DOI] [PubMed] [Google Scholar]
- 30.Goh SK, Samuel M, Su DH, Chan ES, Yeo SJ. Meta-analysis comparing total hip arthroplasty with hemiarthroplasty in the treatment of displaced neck of femur fracture. J Arthroplasty. 2009;24:400–6. doi: 10.1016/j.arth.2007.12.009. doi: 10.1016/j.arth.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 31.Dai Z, Li Y, Jiang D. Meta-analysis comparing arthroplasty with internal fixation for displaced femoral neck fracture in the elderly. J Surg Res. 2011;165:68–74. doi: 10.1016/j.jss.2009.03.029. doi: 10.1016/j.jss.2009.03.029. [DOI] [PubMed] [Google Scholar]
- 32.Zi-Sheng A, You-Shui G, Zhi-Zhen J, Ting Y, Chang-Qing Z. Hemiarthroplasty vs primary total hip arthroplasty for displaced fractures of the femoral neck in the elderly: A meta-analysis. J Arthroplasty. 2012;27:583–90. doi: 10.1016/j.arth.2011.07.009. doi: 10.1016/j.arth.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 33.Carroll C, Stevenson M, Scope A, Evans P, Buckley S. Hemiarthroplasty and total hip arthroplasty for treating primary intracapsular fracture of the hip: A systematic review and cost-effectiveness analysis. Health Technol Assess. 2011;15:1–74. doi: 10.3310/hta15360. doi: 10.3310/hta15360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: Systematic review. BMJ. 2010;340:c2332. doi: 10.1136/bmj.c2332. doi: 10.1136/bmj.c2332. [DOI] [PubMed] [Google Scholar]
- 35.Tidermark J, Ponzer S, Svensson O, Söderqvist A, Törnkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg Br. 2003;85:380–8. doi: 10.1302/0301-620x.85b3.13609. doi: http://dx.doi.org/10.1302/0301-620X.85B3.13609. [DOI] [PubMed] [Google Scholar]
- 36.Rödén M, Schön M, Fredin H. Treatment of displaced femoral neck fractures: A randomized minimum 5-year follow-up study of screws and bipolar hemiprostheses in 100 patients. Acta Orthop Scand. 2003;74:42–4. doi: 10.1080/00016470310013635. doi: 10.1080/00016470310013635. [DOI] [PubMed] [Google Scholar]
- 37.Bjørgul K, Reikerås O. Hemiarthroplasty in worst cases is better than internal fixation in best cases of displaced femoral neck fractures: A prospective study of 683 patients treated with hemiarthroplasty or internal fixation. Acta Orthop. 2006;77:368–74. doi: 10.1080/17453670610046271. doi: 10.1080/17453670610046271. [DOI] [PubMed] [Google Scholar]
- 38.Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Displaced femoral neck fracture: Comparison of primary total hip replacement with secondary replacement after failed internal fixation: A 2-year follow-up of 84 patients. Acta Orthop. 2006;77:638–43. doi: 10.1080/17453670610012728. doi: 10.1080/17453670610012728. [DOI] [PubMed] [Google Scholar]
- 39.Beaulé PE. Early lesions of the labrum and acetabular cartilage in osteonecrosis of the femoral head. J Bone Joint Surg Br. 2003;85:462. doi: 10.1302/0301-620x.85b3.14199. [DOI] [PubMed] [Google Scholar]
- 40.Wani IH, Sharma S, Latoo I, Salaria AQ, Farooq M, Jan M. Primary total hip arthroplasty versus internal fixation in displaced fracture of femoral neck in sexa- and septuagenarians. J Orthop Traumatol. 2014;15:209–14. doi: 10.1007/s10195-013-0278-3. doi: 10.1007/s10195-013-0278-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Talboys R, Pickup L, Chojnowski A. The management of intracapsular hip fractures in the young elderly internal fixation or total hip replacement? Acta Orthop Belg. 2012;78:41–8. [PubMed] [Google Scholar]
- 42.Parker MJ, Raghavan R, Gurusamy K. Incidence of fracture-healing complications after femoral neck fractures. Clin Orthop Relat Res. 2007;458:175–9. doi: 10.1097/BLO.0b013e3180325a42. doi: 10.1097/BLO.0b013e3180325a42. [DOI] [PubMed] [Google Scholar]
- 43.Bech NH, Kodde IF, Dusseldorp F, Druyts PA, Jansen SP, Haverkamp D. Hip arthroscopy in obese, a successful combination? J Hip Preserv Surg. 2015;3:37–42. doi: 10.1093/jhps/hnv076. doi: 10.1093/jhps/hnv076. [DOI] [PMC free article] [PubMed] [Google Scholar]