The aging population has led to increasing number of patients with spinal deformities. Such deformities can be congenital, idiopathic, or inflammatory in origin and can be functionally and psychologically debilitating. Osteotomies could be lifesaving procedures for some severe deformities. Currently, various osteotomy techniques have been applied to treat spinal deformities. The goals of surgery are to obtain a satisfactory balance in both the sagittal and coronal planes, create a solid fusion with a balanced spine, relieve pain, and prevent further deformity.[1]
To achieve an optimal profile, surgical correction requires careful planning.[2] Preoperative clinical and radiographic evaluations are necessary.[3] Anteroposterior and lateral full-length spinal radiographs, supine bending, and three-dimensional reconstruction imaging can demonstrate the flexibility and severity of the deformity. The surgeon must consider the global spinopelvic alignment during surgical planning. According to Smith et al.,[4] the ideal sagittal alignment is sagittal vertical axis <50 mm, pelvic tilt <25°, and pelvic incidence–lumbar lordosis <10°. The patient's chief complaint, neurological status, medical comorbidities, and the predicted natural course of the deformity are the other main factors of the preoperative plan.[1] Selecting the appropriate level is also critical to the success of an osteotomy. Osteotomies are typically performed in the region of the relative kyphosis and maximal deformity, which can be in the cervical, thoracic, or lumbar spine.[5] Determining which osteotomy is most appropriate is critically important because no single type of surgery works for all deformities.
Smith-Peterson osteotomy (SPO) is described as an opening wedge osteotomy with a hinge at the posterior aspect of the disc space. This technique involves the resection of posterior elements, including bilateral facet joints, part of the lamina, and the posterior ligaments at the osteotomy site. Deformity correction during this procedure is achieved by shortening the posterior column and lengthening the anterior column by opening a disc through manual extension [Figure 1a]. The Ponte osteotomy (PO) as a modified technique advanced the SPO one step further removing both superior and inferior facets, the posterior ligaments, and more as indicated for Scheuermann's kyphosis and adolescent idiopathic scoliosis.[6]
Figure 1.
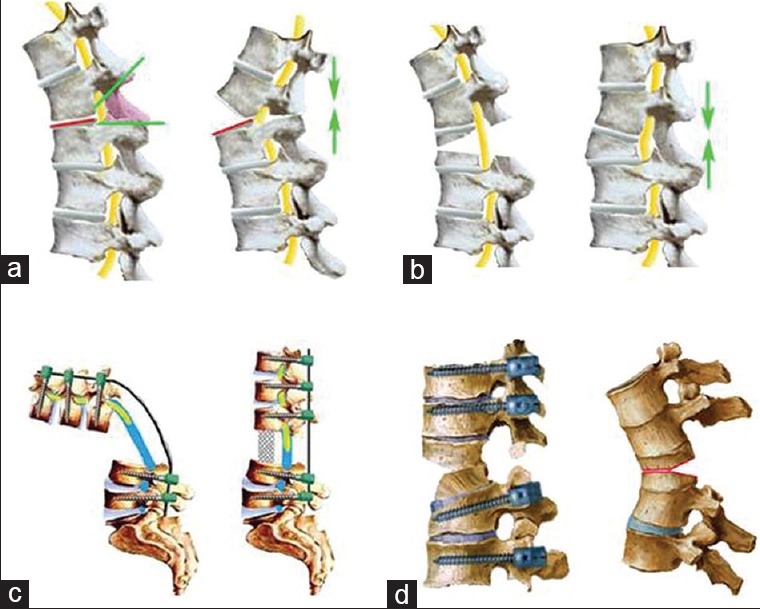
Spine osteotomy techniques. (a) Smith-Peterson osteotomy. (b) Pedicle subtraction osteotomy. (c) Vertebral column resection. (d) “Y”-shaped vertebral column decancellation.
Of note, classical SPO is limited to 10°–15° as the expected range resulting from a single-segment osteotomy with 1 cm resection through a disc that is mobile and of adequate height. Moreover, SPO has a potential loss of correction. Zhu et al.[7] compared the SPO and pedicle subtraction osteotomy (PSO) methods in ankylosing spondylitis (AS) patients and concluded that the mean loss of correction of >5° occurred in four cases (21.1%) in the SPO group and five cases (16.1%) in the PSO group. SPO and PO are mainly used for cases of long, rounded, smooth kyphosis, such as Scheuermann's and idiopathic kyphosis, especially with a previous fusion and malunion. Minor kyphosis deformities <30° are also candidates for SPO. Clinically, SPO is a relatively simple procedure that offers stable fixation and deformity correction with less bleeding, less operative time, and fewer complications. The potential complications caused by SPO include paraplegia from spinal kinking, cauda equina compression, and abdominal vessel injury from stretching of the anterior column. Some surgeons have modified SPO into a more posterior column resection and anterior osteoclasis and have achieved over 30° of correction at one level.[8] It should be noted that SPO is susceptible to sagittal translation of the spinal column, which can cause cord compromise.
PSO, a closing-wedging osteotomy, is a three-column osteotomy. During this procedure, posterior elements and a V-shaped bony wedge of the vertebral body are resected and the middle column is shortened without lengthening the anterior column [Figure 1b]. Compared with SPO, PSO is classified as a higher-grade osteotomy and is technically more demanding.[9] On average, classical PSO can achieve approximately 30°–40° of lordosis at each level which it is performed.[10] Many modifications of this closing-wedge osteotomy have been described. Chen et al.[11] removed the bone and the upper disc through the pedicle and this technique was performed as a safe and reliable surgical option in 13 patients with failed short-segment pedicle instrumentation after thoracolumbar fracture. Zhang et al.[12] also achieved satisfactory results using modified PSO to treat Kümmell disease with neurologic deficits. One-level modified PSO can obtain a maximum correction angle of 60° by removing more of the lamina and upper and/or lower end plate.[13] In recent years, PSO has become a more popular choice for correcting spinal deformity. Short angular deformity, severe global positive sagittal imbalance >6 cm, and concomitant coronal deformity are often candidates for PSO. Examples include posttraumatic kyphotic collapse, degenerative scoliosis, postinfectious kyphosis, and AS. This technique requires the dissection of more structures, theoretically leading to a longer operation time, more blood loss, and a higher risk of neural deficits. Stability of the spinal column may be lost abruptly during the process of closing the osteotomy space. Sagittal translation sometimes occurs during asymmetric osteotomy or cantilever maneuvers and can cause catastrophic dura impingement.
Another three-column osteotomy is the bone-disc-bone osteotomy (BDBO), which aims to resect the disc with its adjacent endplate(s). During this procedure, a wedge osteotomy that includes the disc endplate(s) with or without the pedicle(s) is performed. The correction rates range from 35° to 60°. Kose et al.[14] reported that BDBO was performed at the C7-T1 level to correct an extension deformity of the cervical spine in patients with muscular dystrophy who presented clinically with debilitating hyperlordosis; the procedure resulted in significant acute clinical and radiological improvement.
Vertebral column resection (VCR), the most powerful tool for spinal deformity correction,[15] is defined as the resection of more vertebral segments, including the spinous process and lamina, pedicles, vertebral body, and the discs above and below the vertebral body [Figure 1c]. VCR is useful for treating patients with severe and fixed trunk translation, and it has been described for the treatment of spinal column tumors, spondyloptosis, congenital kyphosis, and hemivertebral excision.[16] Because this procedure is extremely technically demanding and has considerable potential for complications, Suk et al.[17] referred to it as a “formidable last resort technique for the most tenacious spinal deformities.”
Overall complication rate has been reported to range widely by different authors. Major and minor complications of VCR are subdivided into neurological and nonneurological complications, respectively. During posterior reconstruction, the spine is highly unstable; consequently, neurological deficits are not uncommon secondary to vertebral subluxation, dural bucking, or compression of the spinal cord.[1] In addition to neural injury, pneumothorax, fixation failure, and postoperative pulmonary complications are also relatively common injuries.[18]
As a combination of several osteotomy techniques, “Y”-shaped vertebral column decancellation (VCD) is a new spinal osteotomy that incorporates the eggshell technique, SPO, PSO, and VCR.[19] The procedure is a “Y”-type osteotomy rather than a “V”-type osteotomy. It is characterized by controlled anterior column opening, posterior column closing, and middle column preservation as the hinge. The key points of the “Y”-shaped VCD technique are to remove a relatively small amount of the posterior half of the osteotomy column and preserve as much as possible of the middle column as the hinge, which serves as the correction “leverage” to provide greater stability and better fusion during the correction procedure. Opening the anterior column results in a larger correction angle and decreases the need to shorten the posterior column, which reduces the risk of sagittal translation and neurological sequelae. Furthermore, osteoclasis of the anterior cortex is more suitable for correcting rigid deformities [Figure 1d].
Patients with congenital kyphoscoliosis or severe sagittal angular kyphosis, such as Pott's deformity, have ideal indications for the “Y”-shaped VCD osteotomy.[20] If the required correction of a round angular deformity is much larger than 40°, a “Y”-shaped VCD is also an option. In fact, “Y”-shaped VCD is useful for most deformities other than L5 spondyloptosis and spinal tumors. The “Y”-shaped VCD technique creates an osteotomy gap with a “Y” shape rather than a “V” shape, which preserves the middle vertebral column. According to Denis three-column theory, the middle column is the most important supporting structure.
As we know, most of the kyphotic deformities result from AS and Pott's deformity in China. Almost 100 patients with AS or Pott's deformity received surgical treatment at our hospital and we preferred this effective spinal osteotomy of “Y”-shaped VCD. It offers a safe and reliable way to achieve good results, including realignment of the deformed spine, decompression of neurological elements, and improved neurological function. In experienced hands, these results can be achieved with an acceptable complication rate when compared with other procedures of a similar magnitude. Each osteotomy technique has its unique characteristics and advantages, and balance is the ultimate goal in deformity correction. In recent years, global balance in the spine and major joints has attracted an increasing attention. The range of motion of the hip and knee and spine alignment influence one another. Gebhart et al.[21] suggested that hip function is closely related to spinal symptoms. When selecting a surgical strategy for correcting a spinal deformity, the function of the hip and knee should be taken into consideration.
Over the past decades, osteotomies ranging from smaller facetectomies to major three-column resections have been widely used in clinical practice. Of note, using osteotomies for correcting spinal deformity involves skill not only in the operating setting, but also in a detailed patient-specific plan prior to operation. We believe that multicenter collaboration will provide more evidence-based guidelines for the complex clinical scenarios in the future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang
References
- 1.Enercan M, Ozturk C, Kahraman S, Sarier M, Hamzaoglu A, Alanay A. Osteotomies/spinal column resections in adult deformity. Eur Spine J. 2013;22(Suppl 2):S254–64. doi: 10.1007/s00586-012-2313-0. doi: 10.1007/s00586-012-2313-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang X, Zhang Z, Wang J, Lu M, Hu W, Wang Y, et al. Vertebral column decancellation: A new spinal osteotomy technique for correcting rigid thoracolumbar kyphosis in patients with ankylosing spondylitis. Bone Joint J. 2016;98-B:672–8. doi: 10.1302/0301-620X.98B5.35726. doi: 10.1302/0301-620X.98B5.35726. [DOI] [PubMed] [Google Scholar]
- 3.Wu XB, Wang JQ, Zhao CP, Sun X, Shi Y, Zhang ZA, et al. Printed three-dimensional anatomic templates for virtual preoperative planning before reconstruction of old pelvic injuries: Initial results. Chin Med J. 2015;128:477–82. doi: 10.4103/0366-6999.151088. doi: 10.4103/0366-6999.151088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP, et al. Change in classification grade by the SRS-schwab adult spinal deformity classification predicts impact on health-related quality of life measures: Prospective analysis of operative and nonoperative treatment. Spine (Phila Pa 1976) 2013;38:1663–71. doi: 10.1097/BRS.0b013e31829ec563. doi: 10.1097/BRS.0b013e31829ec563. [DOI] [PubMed] [Google Scholar]
- 5.Sansur CA, Fu KM, Oskouian RJ, Jr, Jagannathan J, Kuntz C, 4th, Shaffrey CI. Surgical management of global sagittal deformity in ankylosing spondylitis. Neurosurg Focus. 2008;24:E8. doi: 10.3171/FOC/2008/24/1/E8. doi: 10.3171/FOC/2008/24/1/E8. [DOI] [PubMed] [Google Scholar]
- 6.Pizones J, Sánchez-Mariscal F, Zúñiga L, Izquierdo E. Ponte osteotomies to treat major thoracic adolescent idiopathic scoliosis curves allow more effective corrective maneuvers. Eur Spine J. 2015;24:1540–6. doi: 10.1007/s00586-014-3749-1. doi: 10.1007/s00586-014-3749-1. [DOI] [PubMed] [Google Scholar]
- 7.Zhu Z, Wang X, Qian B, Wang B, Yu Y, Zhao Q, et al. Loss of correction in the treatment of thoracolumbar kyphosis secondary to ankylosing spondylitis: A comparison between Smith-Petersen osteotomies and pedicle subtraction osteotomy. J Spinal Disord Tech. 2012;25:383–90. doi: 10.1097/BSD.0b013e318224b199. doi: 10.1097/BSD.0b013e318224b199. [DOI] [PubMed] [Google Scholar]
- 8.Liu H, Yang C, Zheng Z, Ding W, Wang J, Wang H, et al. Comparison of Smith-Petersen osteotomy and pedicle subtraction osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis: A systematic review and meta-analysis. Spine (Phila Pa 1976) 2015;40:570–9. doi: 10.1097/BRS.0000000000000815. doi: 10.1097/BRS.0000000000000815. [DOI] [PubMed] [Google Scholar]
- 9.Diebo B, Liu S, Lafage V, Schwab F. Osteotomies in the treatment of spinal deformities: Indications, classification, and surgical planning. Eur J Orthop Surg Traumatol. 2014;24(Suppl 1):S11–20. doi: 10.1007/s00590-014-1471-7. doi: 10.1007/s00590-014-1471-7. [DOI] [PubMed] [Google Scholar]
- 10.Jaffray D, Becker V, Eisenstein S. Closing wedge osteotomy with transpedicular fixation in ankylosing spondylitis. Clin Orthop Relat Res. 1992;(279):122–6. doi: 10.1097/00003086-199206000-00014. [PubMed] [Google Scholar]
- 11.Chen F, Kang Y, Li H, Lv G, Lu C, Li J, et al. Modified pedicle subtraction osteotomy as a salvage method for failed short-segment pedicle instrumentation in the treatment of thoracolumbar fracture. Clin Spine Surg. 2016;29:E120–6. doi: 10.1097/BSD.0000000000000093. doi: 10.1097/BSD.0000000000000093. [DOI] [PubMed] [Google Scholar]
- 12.Zhang X, Hu W, Yu J, Wang Z, Wang Y. An effective treatment option for kummell disease with neurological deficits: Modified transpedicular subtraction and disc osteotomy combined with long-segment fixation. Spine. 2016;41:E923–30. doi: 10.1097/BRS.0000000000001467. doi: 10.1097/BRS.0000000000001467. [DOI] [PubMed] [Google Scholar]
- 13.Xi YM, Pan M, Wang ZJ, Zhang GQ, Shan R, Liu YJ, et al. Correction of post-traumatic thoracolumbar kyphosis using pedicle subtraction osteotomy. Eur J Orthop Surg Traumatol. 2013;23(Suppl 1):S59–66. doi: 10.1007/s00590-013-1168-3. doi: 10.1007/s00590-013-1168-3. [DOI] [PubMed] [Google Scholar]
- 14.Kose KC, Caliskan I, Bal E, Inanmaz ME, Isik C. C7-T1 anterior closing wedge bone-disc-bone osteotomy for the treatment of cervical hyperlordosis in muscular dystrophy: A new technique for correction of a rare deformity. Spine (Phila Pa 1976) 2014;39:E1066–72. doi: 10.1097/BRS.0000000000000433. doi: 10.1097/BRS.0000000000000433. [DOI] [PubMed] [Google Scholar]
- 15.Screening for Idiopathic Scoliosis in Adolescents. Pediatrics. 2016;137 doi: 10.1542/peds.2016-0065. pii: E20160065. doi: 10.1542/peds.2016-0065. [DOI] [PubMed] [Google Scholar]
- 16.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31(19 Suppl):S171–8. doi: 10.1097/01.brs.0000231963.72810.38. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 17.Suk SI, Chung ER, Lee SM, Lee JH, Kim SS, Kim JH. Posterior vertebral column resection in fixed lumbosacral deformity. Spine (Phila Pa 1976) 2005;30:E703–10. doi: 10.1097/01.brs.0000188190.90034.be. doi: 10.1097/01.brs.0000188190.90034.be. [DOI] [PubMed] [Google Scholar]
- 18.Baron EM, Albert TJ. Medical complications of surgical treatment of adult spinal deformity and how to avoid them. Spine (Phila Pa 1976) 2006;31(19 Suppl):S106–18. doi: 10.1097/01.brs.0000232713.69342.df. doi: 10.1097/01.brs.0000232713.69342.df. [DOI] [PubMed] [Google Scholar]
- 19.Alexander RE, Davidson DD, Lopez-Beltran A, Montironi R, MacLennan GT, Compérat E, et al. Human papillomavirus is not an etiologic agent of urothelial inverted papillomas. Am J Surg Pathol. 2013;37:1223–8. doi: 10.1097/PAS.0b013e3182863fc1. doi: 10.1097/PAS.0b013e3182863fc1. [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Zhang Y, Zhang X, Wang Z, Mao K, Chen C, et al. Posterior-only multilevel modified vertebral column resection for extremely severe Pott's kyphotic deformity. Eur Spine J. 2009;18:1436–41. doi: 10.1007/s00586-009-1067-9. doi: 10.1007/s00586-009-1067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gebhart JJ, Weinberg DS, Conry KT, Morris WZ, Sasala LM, Liu RW. Hip-Spine syndrome: Is there an association between markers for cam deformity and osteoarthritis of the lumbar spine? Arthroscopy. 2016 doi: 10.1016/j.arthro.2016.04.025. pii:S0749-806330199-2. [Epub ahead of print] doi: 10.1016/j.arthro.2016.04.025. [DOI] [PubMed] [Google Scholar]


