Abstract
Objectives
To determine whether nonselective preoperative carotid artery ultrasound screening alters management of patients scheduled for coronary artery bypass grafting (CABG), and whether such screening affects neurologic outcomes.
Methods
From March 2011 to September 2013, preoperative carotid artery ultrasound screening was performed on 1236 of 1382 patients (89%) scheduled to undergo CABG. Carotid artery stenosis (CAS) was classified as none or mild (any type 0%–59% stenosis), moderate (unilateral 60%-79% stenosis), or severe (bilateral 60%-79% stenosis or unilateral 80%–100% stenosis).
Results
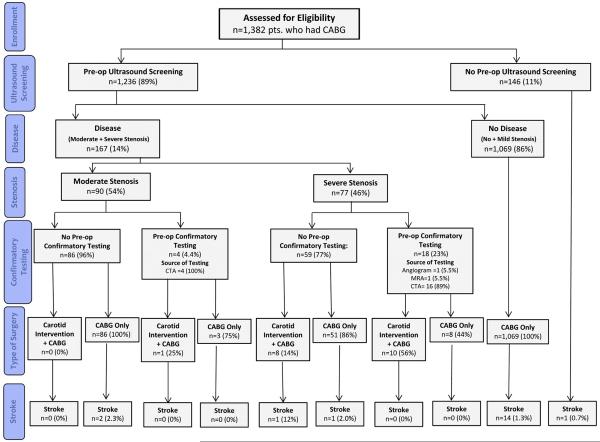
A total of 1069 (86%) had<moderate; 90 (7.3%) had moderate; and 77 (6.2%) had severe CAS. Of those with moderate CAS, 4 (4.4%) had preoperative confirmatory testing, and 1 (1.1%) underwent combined CABG + carotid endarterectomy (CEA); 11 (12%) had off-pump surgery. Of those with severe CAS, 18 (23%) had confirmatory testing, and 18 (23%) underwent combined CABG + CEA; 6 (7.8%) had off-pump surgery. Stroke occurred in 14 of 1069 (1.3%) patients with <moderate CAS; 2 of 90 (2.2%) of those with moderate CAS; and 2 of 77 (2.6%) of those with severe CAS (P = .3). In patients with ≥moderate CAS, 1 of 19 (5.3%) undergoing CABG + CEA and 3 of 148 (2.0%) undergoing CABG alone experienced stroke (P = .4). In patients with moderate CAS, stroke occurred in 1 of 11 (9.1%) off-pump and 1 of 79 (1.3%) on-pump patients (P = .2). In patients with severe CAS, stroke occurred in 1 of 6 (17%) off-pump and 1 of 71 (1.4%) on-pump patients (P = .15).
Conclusions
Routine preoperative carotid artery evaluation altered the management of a minority of patients undergoing CABG; this did not translate into perioperative stroke risk. Hence, a more targeted approach for preoperative carotid artery evaluation should be adopted.
Keywords: carotid stenosis, carotid endarterectomy, ultrasound screening, coronary artery bypass grafting
Stroke is a devastating complication of coronary artery bypass grafting (CABG)1 that is associated with substantial morbidity, mortality, and costs for both patients and healthcare systems. With the expectation of reducing the occurrence of perioperative stroke, some groups routinely screen patients before CABG to identify carotid artery disease that they believe requires revascularization before or during CABG.2–7 In 2011, we implemented a quality improvement protocol to reduce the occurrence of strokes, which included universal carotid artery screening. The purposes of this study were to determine whether this quality improvement protocol (1) altered the management of patients scheduled to undergo isolated CABG, and (2) affected neurologic outcomes.
METHODS
Patients
From March 2011 to September 2013, nonselective carotid artery ultrasound screening was performed prospectively on 1236 of 1382 (89%) patients scheduled to undergo isolated CABG at Cleveland Clinic. Preoperative, operative, and postoperative variables were retrieved from the Cardiovascular Information Registry, a database populated concurrently with patient care information. Medical records of all patients who were recorded as having carotid artery stenosis, identified on screening ultrasound, were reviewed to identify any change in perioperative management that occurred on that basis. Medical and imaging records of patients experiencing an adverse neurologic event were reviewed. The average age of screened patients was 65 ± 10 years, and 75% were male, with no statistically significant differences between those who were, versus were not, screened (Table 1). Data used in this study were approved for use in this quality improvement project by the Cleveland Clinic Institutional Review Board.
TABLE 1.
Patient characteristics stratified by degree of preoperative carotid stenosis
| No stenosis or mild stenosis (n = 1069) |
Moderate stenosis (n = 90) |
Severe stenosis (n = 77) |
|||||
|---|---|---|---|---|---|---|---|
| Characteristic | n* | No. (%) or mean ± SD | n* | No. (%) or mean ± SD | n* | No. (%) or mean ± SD | P value |
| Demographics | |||||||
| Age (y) | 1068 | 64 ± 10 | 90 | 69 ± 9.9 | 77 | 69 ± 8.7 | <.0001 |
| Gender, female | 1068 | 240 (22) | 90 | 37 (41) | 77 | 30 (39) | <.0001 |
| Height (cm) | 1068 | 173 ± 9.6 | 90 | 170 ± 11 | 77 | 170 ± 9.8 | .004 |
| Body mass index (kg/m2) | 1068 | 30 ± 5.8 | 90 | 28 ± 5.6 | 77 | 29 ± 5.6 | .003 |
| NYHA functional class | 841 | 74 | 68 | .09 | |||
| I | 113 (13) | 9 (12) | 7 (10) | ||||
| II | 375 (45) | 28 (38) | 22 (32) | ||||
| III | 260 (31) | 28 (38) | 24 (35) | ||||
| IV | 93 (11) | 9 (12) | 15 (22) | ||||
| Cardiac comorbidities | |||||||
| LVEF (%) | 1049 | 51 ± 11 | 89 | 53 ± 11 | 77 | 50 ± 12 | .4 |
| No. of coronary artery systems diseased (≥50% stenosis) | 1066 | 90 | 77 | .16 | |||
| 1 | 62 (5.8) | 5 (5.6) | 0 (0) | ||||
| 2 | 206 (19) | 13 (14) | 13 (17) | ||||
| 3 | 798 (75) | 72 (80) | 64 (83) | ||||
| Left main disease | 1065 | 283 (27) | 90 | 27 (30) | 77 | 28 (36) | .15 |
| Heart failure | 1068 | 277 (26) | 90 | 29 (32) | 77 | 32 (42) | .007 |
| Noncardiac comorbidities | |||||||
| Peripheral arterial disease | 1068 | 197 (18) | 90 | 40 (44) | 77 | 42 (55) | <.0001 |
| Prior stroke | 1068 | 81 (7.6) | 90 | 10 (11) | 77 | 12 (16) | .03 |
| Hypertension | 1068 | 998 (93) | 90 | 86 (96) | 77 | 73 (95) | .7 |
| Diabetes mellitus, pharmacologically treated | 1068 | 479 (45) | 90 | 47 (52) | 77 | 43 (56) | .08 |
| COPD | 1068 | 228 (21) | 90 | 18 (20) | 77 | 24 (31) | .12 |
| History of smoking | 1068 | 228 (21) | 90 | 23 (26) | 77 | 27 (35) | .02 |
| Creatinine (mg/dL) | 1062 | 0.97 (0.77, 1.3) | 90 | 1.0 (0.71, 1.5) | 77 | 1.1 (0.79, 1.8) | .003 |
| Blood urea nitrogen (mg/dL) | 1062 | 20 ± 8.8 | 90 | 22 ± 11 | 77 | 23 ± 10 | .05 |
| Bilirubin (mg/dL) | 1028 | 0.52 ± 0.31 | 89 | 0.45 ± 0.26 | 74 | 0.49 ± 0.29 | .05 |
| Total cholesterol (mg/dL) | 939 | 159 ± 46 | 77 | 170 ± 45 | 66 | 162 ± 54 | .10 |
| Triglycerides (mg/dL) | 939 | 144 ± 110 | 77 | 143 ± 128 | 66 | 136 ± 69 | .6 |
| Hematocrit (%) | 1066 | 40 ± 5.6 | 90 | 37 ± 5.3 | 77 | 37 ± 6.3 | <.0001 |
Values are mean ± SD, or No. (%), unless otherwise indicated (creatinine is given as median [15th, 85th percentiles]). NYHA, New York Heart Association; LVEF, left ventricular ejection fraction; COPD, chronic obstructive pulmonary disease.
Patients with data available.
Carotid Artery Screening
Most of the carotid duplex ultrasound examinations (92%) were performed in the Non-Invasive Vascular Laboratory of Cleveland Clinic, a facility accredited by the Intersocietal Accreditation Commission (www.intersocietal.org) in extracranial cerebrovascular testing. Studies were performed by registered vascular technologists using a standardized scanning protocol, and interpreted by vascular medicine specialists and vascular surgeons certified in vascular interpretation. Duplex ultrasound examination findings and results were entered into an electronic database at the time of interpretation. The median interval from screening ultrasound to CABG was 4 days, with 90% performed within 16 days. Each internal carotid artery was graded and categorized according to the severity of stenosis, based on standardized laboratory diagnostic criteria,8 including internal carotid artery peak systolic and end-diastolic velocities and presence of atherosclerotic plaque.
Results of the carotid artery ultrasound were classified as follows: no stenosis or mild stenosis (any type <60%, including categories 0%–19%, 20%–39%, and 40%–59%); moderate stenosis (unilateral, 60%-79% stenosis of either internal carotid artery); or severe stenosis (bilateral 60%-79% stenosis; unilateral or bilateral 80%–99% stenosis, or 100% occlusion). For patients who underwent preoperative carotid duplex ultrasound outside Cleveland Clinic (1%) or in the radiology department at Cleveland Clinic (7%), available study examination imaging or report of ultrasound velocity findings were used by a single investigator (H.K.) to grade the severity of carotid stenosis, using the standardized diagnostic criteria of the Cleveland Clinic Non-Invasive Vascular Laboratory.
Endpoints
Perioperative stroke was defined as any new focal or global neurologic deficit lasting >24 hours that could not be explained by another medical process. This included persistent neurologic deficit for >72 hours, and reversible ischemic neurologic deficit and recovery within 72 hours; excluded was transient ischemic attack with recovery within 24 hours. Temporal onset of stroke was classified as intraoperative if the neurologic deficit was present when the patient awoke from anesthesia, and postoperative if the deficit developed after the patient emerged from anesthesia.
Statistical Analysis
All analyses were performed using SAS, version 9.2 software (SAS Institute, Cary, NC). Continuous variables are summarized as mean ± SD, or as equivalent 15th, 50th (median), and 85th percentiles when the distribution of values is skewed. Categoric data are summarized by frequencies and percentages.
RESULTS
Screening Results
Among the 1236 patients who had preoperative carotid ultrasound screening, 1069 (86%) had no stenosis or mild stenosis, 90 (7.3%) had moderate stenosis, and 77 (6.2%) had severe stenosis (Figure 1). Patients with no stenosis or mild stenosis were younger than patients with moderate or severe stenosis. More of the patients with moderate or severe stenosis were women, and had heart failure, peripheral arterial disease, and a history of stroke and smoking (Table 1). Of those with moderate stenosis, most lesions were unilateral, equally distributed on the right (50%) and left sides (50%; Table 2). Ten (11%) of these patients had a history of stroke. Of those with severe stenosis, it was most commonly bilateral (48%; Table 3). Twelve (16%) of these patients had a history of stroke.
FIGURE 1.
Diagram of study flow showing carotid artery ultrasound screening, its results, interventions, and endpoints. pts., Patients; CABG, coronary artery bypass grafting; Pre-op, preoperative; CTA, computed tomography angiography; MRA, magnetic resonance angiography.
TABLE 2.
Right and left coronary artery stenosis severity in patients with moderate stenosis
| Right stenosis (% range) | Left stenosis (% range) | No. (%) |
|---|---|---|
| 0–19 | 60–79 | 4 (4.4) |
| 20–39 | 60–79 | 25 (28) |
| 40–59 | 60–79 | 16 (18) |
| 60–79 | 0–19 | 2 (2.2) |
| 60–79 | 20–39 | 16 (18) |
| 60–79 | 40–59 | 27 (30) |
TABLE 3.
Right and left coronary artery stenosis severity in patients with severe stenosis
| Stenosis type | No. (%) |
|---|---|
| Bilateral, 60%–79% | 36 (47) |
| Occluded unilateral | 20 (26) |
| Unilateral, 80%–99% | 15 (19) |
| ICA occlusion and contralateral, 80%–99% | 3 (3.9) |
| CCA occluded | 1 (1.3) |
| Bilateral, 80%–99% | 1 (1.3) |
| CCA occlusion and contralateral, 80%–99% | 1 (1.3) |
ICA, Internal carotid artery; CCA, common carotid artery.
Management
Of those with moderate carotid artery stenosis, 4 (4.4%) had preoperative confirmatory testing (computed tomography angiography), and only 1 (1.1%) underwent combined CABG and carotid endarterectomy (CABG + CEA). The latter patient had no history of stroke and was found to have severe carotid stenosis on confirmatory testing. Of those with severe stenosis, 18 (23%) had confirmatory testing (computed tomography angiography = 16, magnetic resonance angiography = 1, angiogram = 1), and 18 (23%) underwent CABG + CEA. Of the 18 undergoing CABG + CEA, 3 had a history of stroke; CABG + CEA was performed under the same anesthesia, with carotid endarterectomy performed first, and the wound left open. Afterward, coronary surgery was performed, followed by closure of chest and neck wounds. No patient in the study underwent carotid stenting or staged CEA followed by CABG. Off-pump surgery was performed in 75 (7.0%) patients who had no stenosis or mild stenosis, 11 (12%) who had moderate stenosis, and 6 (7.8%) who had severe stenosis.
Stroke
By stenosis severity
Stroke occurred in 19 of 1382 (1.4%) patients: 14 of 1069 (1.3%) of those with no stenosis or mild carotid artery stenosis; 2 of 90 (2.2%) of those with moderate stenosis; 2 of 77 (2.6%) of those with severe stenosis (P = .3); and 1 in a patient who was not screened.
By management
In patients with moderate stenosis, 2 of 89 (2.2%) strokes occurred in those undergoing isolated CABG, and no stroke occurred in the 1 patient who underwent CABG + CEA. For both patients who had a stroke, neither had had a prior stroke, and the stroke was bilateral hemispheric; 1 patient had been managed with cardiopulmonary bypass, and the other was an off-pump case.
In patients with severe stenosis, 1 of 59 (1.7%) strokes that were ipsilateral to the carotid artery stenosis occurred in a patient undergoing isolated CABG; and 1 of 18 (5.5%) strokes that were contralateral to the carotid stenosis occurred in patients undergoing CABG + CEA. Therefore, in patients with moderate or severe stenosis, 1 of 19 (5.3%) undergoing CABG + CEA and 3 of 148 (2.0%) undergoing isolated CABG experienced stroke (P = .4).
In patients who had no stenosis or mild stenosis, stroke occurred in 1 of 75 (1.3%) undergoing off-pump surgery and 13 of 994 (1.3%) undergoing on-pump surgery (P = .9). In patients with moderate stenosis, stroke occurred in 1 of 11 (9.1%) undergoing off-pump surgery and 1 of 79 (1.3%) undergoing on-pump surgery (P = .2). In patients with severe stenosis, stroke occurred in 1 of 6 (17%) undergoing off-pump surgery and 1 of 71 (1.4%) undergoing on-pump surgery (P = .15).
By timing and location
Of the 14 strokes that occurred in patients with no stenosis or mild stenosis, 3 were intraoperative, and 11 occurred postoperatively between days 1 and 13; stroke was bilateral in 8 patients (Table 4). Of the 2 strokes that occurred in patients who had moderate stenosis, 1 was intraoperative, and the other occurred postoperatively, on day 3; stroke was bilateral hemispheric in both. Of the 2 strokes that occurred in patients who had severe stenosis, 1 occurred on postoperative day 2 and the other on postoperative day 4; stroke was unilateral in both.
TABLE 4.
Perioperative stroke location and carotid artery disease
| Carotid stenosis | Right (% range) | Left (% range) | No. of patients | Stroke location | Postoperative day |
|---|---|---|---|---|---|
| No screening | — | — | 1 | Left | 6 |
| No stenosis or mild stenosis | |||||
| 0–19 | 0–19 | 1 | Bilateral | 1 | |
| 20–39 | 20–39 | 7 | Bilateral | 1 | |
| Bilateral | 13 | ||||
| Right | 6 | ||||
| Left | 1 | ||||
| Left | 2 | ||||
| Left | 5 | ||||
| Left | 11 | ||||
| 20–39 | 40–59 | 3 | Bilateral | Upon awakening | |
| Bilateral | 3 | ||||
| Right | Upon awakening | ||||
| 40–59 | 20–39 | 2 | Bilateral | Upon awakening | |
| Bilateral | 3 | ||||
| 40–59 | 40–59 | 1 | Bilateral | 4 | |
| Moderate stenosis | |||||
| 60–79 | 40–59 | 2 | Bilateral | Upon awakening | |
| Bilateral | 3 | ||||
| Severe stenosis | |||||
| 20–39 | 80–99 | 1 | Right | 4 | |
| 100 (occluded) | 20–39 | 1 | Right | 2 |
DISCUSSION
Principal Findings
Routine, nonselective carotid artery ultrasound screening in our institution altered the management of only a minority of the patients who were found to have moderate or severe carotid artery stenosis. The minority of these went on to confirmatory testing and carotid revascularization. Patients with moderate or severe carotid artery disease did, in fact, experience more perioperative strokes. However, CEA did not seem to prevent these. The choice of performing CABG either on- or off-pump did not seem to be influenced by the severity of carotid artery stenosis, and the occurrence of stroke was similar in patients undergoing either type of surgery, with mild, moderate, or severe stenosis. The laterality of the stroke in the 3 patients who had moderate or severe stenosis and underwent CABG alone was ipsilateral to the carotid stenosis in only 1 patient, making the cause of perioperative stroke in the other 2 patients unlikely to be related to carotid disease.
Findings in Context
Other studies have reported findings similar to ours. Fukuda and colleagues3 found that nonselective carotid artery ultrasound screening resulted in carotid revascularization in only 11 of 308 (4%) patients. In their study, 2 strokes occurred: 1 in a patient with >50% stenosis who underwent combined CABG + CEA, and 1 in a patient who had no stenosis or mild stenosis. No strokes occurred in the 33 patients with >50% stenosis who did not undergo carotid revascularization. Salehiomran and colleagues2 performed routine screening of 1604 patients that led to carotid revascularization in only 5. In their study, no patients who had significant carotid stenosis (>60%) had a stroke, whereas 22 strokes occurred in patients who did not have significant carotid stenosis. In addition, studies have shown that the risk of stroke in patients with carotid disease is low,9–11 and carotid stenosis has no direct causal relationship with ipsilateral stroke.10
Because patients with significant carotid stenosis are likely to have an atherosclerotic aorta, off-pump surgery should be considered, to avoid aortic manipulation. However, in our study, carotid stenosis did not influence the surgeon's choice of performing CABG on-pump versus off-pump, and off-pump surgery did not reduce stroke risk.
Several other strategies can be considered as a means to reduce the occurrence of stroke in patients undergoing CABG, including intraoperative epiaortic scanning and monitoring of blood pressure throughout the procedure. We recommend performing intraoperative epiaortic scanning in all patients undergoing CABG to identify those in whom aortic manipulation should be avoided. In patients with severe carotid stenosis, avoiding extremes of blood pressure is important, because hypotension can cause cerebral ischemia, and hypertension can cause plaque rupture. Off-pump surgery can be considered for patients who have severe carotid stenosis, to avoid hypotension, which may occur during use of cardiopulmonary bypass. Present-day carotid screening focuses on decreasing the occurrence of intraoperative stroke via use of these techniques; however, it does not appear to do so. We know from this study and our previous one1 that most strokes occur postoperatively, not intraoperatively. Therefore, postoperative antiplatelet therapy should be considered for patients undergoing CABG, because most postoperative strokes result from thromboembolic events.
Routine Versus Selective Screening
Based on the results of this study, we have changed our approach from use of routine screening to use of selective screening for carotid stenosis in CABG patients. We now screen only those patients who have a history of stroke or of transient ischemic attack, bruit, left main disease, previous CEA or stenting, amaurosis fugax, or new-onset extremity weakness.
Studies have shown that selective screening in certain high-risk patients can detect ≥50% carotid stenosis with 100% sensitivity.12 These high-risk patients include women and those with a history of diabetes, hypertension, peripheral arterial disease, carotid disease, stroke, left main coronary disease, and smoking. Durand and colleagues5 conducted a study to determine which of 2 approaches—selective or nonselective preoperative carotid screening—is most clinically efficacious. They found that selective screening using a risk-profiling algorithm based on patients being aged >65 years, having carotid bruit on exam, and having a history of stroke would have reduced the screening load by 40%, with a negligible effect on either surgical management or stroke. Given these findings and the findings of our study, a more targeted approach for preoperative carotid artery evaluation seems reasonable. Additionally, guidelines recommend screening in selected patients only.9,13–17
Limitations
The association of surgical intervention with stroke risk was determined observationally and may be confounded by unmeasured covariables. In addition, because the occurrence of stroke was low, the study was underpowered to detect significant differences. Further, carotid revascularization can be performed using staged or synchronous CEA or carotid artery stenting; however, patients in this study underwent only synchronous CABG and CEA. No one underwent carotid stenting or staged CEA followed by CABG. Because individual surgeons have interpreted the available data differently, some have performed combined CABG + CEA for important carotid stenosis, and others have not. In general, the rationale for making either decision was not documented in the medical record.
Classification of the timing of stroke occurrence is somewhat arbitrary and sometimes challenging in the setting of anesthesia use, as well as postoperative delirium and other complications. Additionally, we were unable to determine whether each stroke was embolic, thrombotic, or hypoperfusive in etiology. Finally, these results are from a single academic medical center and may not be generalizable.
CONCLUSIONS
Nonselective preoperative carotid artery screening altered the management of a minority of patients undergoing CABG. These changes did not translate into a decrease in perioperative stroke risk. Given this observation, carotid artery disease might be only a surrogate marker of patients' diffuse atherosclerotic burden. The most compelling evidence from this study emerges from the stroke patterns observed—many more postoperative than intraoperative events, approximately equal numbers of bilateral versus unilateral events, and an absence of correlation between unilateral events and laterality of carotid disease when it was present. This information strongly suggests that the incremental benefit of carotid screening, even if present, is likely to be small. Hence, in patients undergoing CABG, a more targeted approach for preoperative carotid artery evaluation should be adopted.
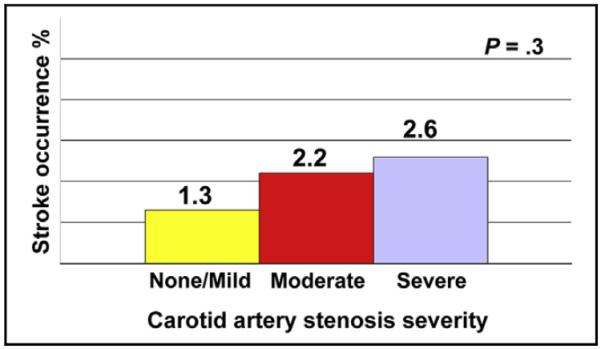
Stroke occurrence by severity of carotid artery stenosis in patients undergoing coronary artery bypass grafting.
Acknowledgments
This study was supported in part by the Sheikh Hamdan bin Rashid Al Maktoum Distinguished Chair in Thoracic and Cardiovascular Surgery, held by J.F.S.; the Kenneth Gee and Paula Shaw, PhD, Chair in Heart Research, held by E.H.B.; and the Gus P. Karos Registry Fund. The individuals for whom these funding sources are named played no role in the collection of data or analysis and interpretation of the data, and had no right to approve or disapprove publication of the finished article.
Abbreviations and Acronyms
- CABG
coronary artery bypass grafting
- CEA
carotid endarterectomy
Footnotes
Central Message Routine, as opposed to selective, preoperative carotid artery ultrasound screening before coronary artery bypass grafting is of questionable value.
Perspective Routine preoperative carotid artery evaluation altered the management of a minority of patients undergoing CABG. These changes in management did not decrease the prevalence of perioperative stroke. Hence, in patients undergoing CABG, a more targeted approach for preoperative carotid artery evaluation should be adopted.
Read at the 95th Annual Meeting of The American Association for Thoracic Surgery, Seattle, Washington, April 25–29, 2015.
Conflict of Interest Statement Authors have nothing to disclose with regard to commercial support.
You can watch a Webcast of this AATS meeting presentation by going to: http://webcast.aats.org/2015/Video/Tuesday/04-28-15_4E_1615_Masabni.mp4.
References
- 1.Tarakji KG, Sabik JF, III, Bhudia SK, Batizy LH, Blackstone EH. Temporal onset, risk factors, and outcomes associated with stroke after coronary artery bypass grafting. JAMA. 2011;305:381–90. doi: 10.1001/jama.2011.37. [DOI] [PubMed] [Google Scholar]
- 2.Salehiomran A, Shirani S, Karimi A, Ahmadi H, Marzban M, Movahedi N, et al. Screening of carotid artery stenosis in coronary artery bypass grafting patients. J Tehran Heart Cent. 2010;5:25–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Fukuda I, Gomi S, Watanabe K, Seita J. Carotid and aortic screening for coronary artery bypass grafting. Ann Thorac Surg. 2000;70:2034–9. doi: 10.1016/s0003-4975(00)02132-9. [DOI] [PubMed] [Google Scholar]
- 4.Anastasiadis K, Karamitsos TD, Velissaris I, Makrygiannakis K, Kiskinis D. Preoperative screening and management of carotid artery disease in patients undergoing cardiac surgery. Perfusion. 2009;24:257–62. doi: 10.1177/0267659109347404. [DOI] [PubMed] [Google Scholar]
- 5.Durand DJ, Perler BA, Roseborough GS, Grega MA, Borowicz LM, Jr, Baumgartner WA, et al. Mandatory versus selective preoperative carotid screening: a retrospective analysis. Ann Thorac Surg. 2004;78:159–66. doi: 10.1016/j.athoracsur.2004.02.024. discussion 166. [DOI] [PubMed] [Google Scholar]
- 6.Shirani S, Boroumand MA, Abbasi SH, Maghsoodi N, Shakiba M, Karimi A, et al. Preoperative carotid artery screening in patients undergoing coronary artery bypass graft surgery. Arch Med Res. 2006;37:987–90. doi: 10.1016/j.arcmed.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Lee EJ, Choi KH, Ryu JS, Jeon SB, Lee SW, Park SW, et al. Stroke risk after coronary artery bypass graft surgery and extent of cerebral artery atherosclerosis. J Am Coll Cardiol. 2011;57:1811–8. doi: 10.1016/j.jacc.2010.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Olin JW, Fonseca C, Childs MB, Piedmonte MR, Hertzer NR, Young JR. The natural history of asymptomatic moderate internal carotid artery stenosis by duplex ultrasound. Vasc Med. 1998;3:101–8. doi: 10.1177/1358836X9800300203. [DOI] [PubMed] [Google Scholar]
- 9.Masabni K, Raza S, Blackstone EH, Gornik HL, Sabik JF. Does preoperative carotid stenosis screening reduce perioperative stroke in patients undergoing coronary artery bypass grafting? J Thorac Cardiovasc Surg. 2015;149:1253–60. doi: 10.1016/j.jtcvs.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Y, Walicki D, Mathiesen C, Jenny D, Li Q, Isayev Y, et al. Strokes after cardiac surgery and relationship to carotid stenosis. Arch Neurol. 2009;66:1091–6. doi: 10.1001/archneurol.2009.114. [DOI] [PubMed] [Google Scholar]
- 11.Ghosh J, Murray D, Khwaja N, Murphy MO, Walker MG. The influence of asymptomatic significant carotid disease on mortality and morbidity in patients undergoing coronary artery bypass surgery. Eur J Vasc Endovasc Surg. 2005;29:88–90. doi: 10.1016/j.ejvs.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Sheiman RG, Janne d'Othee B. Screening carotid sonography before elective coronary artery bypass graft surgery: Who needs it. AJR Am J Roentgenol. 2007;188:W475–9. doi: 10.2214/AJR.06.1024. [DOI] [PubMed] [Google Scholar]
- 13.Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with The American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. Executive summary. J Am Coll Cardiol. 2011;58:2584–614. doi: 10.1016/j.jacc.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 14.The Society of Thoracic Surgeons [Accessed September 4, 2013];Five things physicians and patients should question. Choosing Wisely. An initiative of the ABIM Foundation. Available at: http://www.choosingwisely.org/doctor-patient-lists/the-society-of-thoracic-surgeons/
- 15.Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. J Am Coll Cardiol. 2011;57:1002–44. doi: 10.1016/j.jacc.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 16.Mohler ER, III, Gornik HL, Gerhard-Herman M, Misra S, Olin JW, Zierler RE, et al. ACCF/ACR/AIUM/ASE/ASN/ICAVL/SCAI/SCCT/SIR/SVM/SVS/SVU [corrected] 2012 appropriate use criteria for peripheral vascular ultrasound and physiological testing part I: arterial ultrasound and physiological testing: a report of the American College of Cardiology Foundation appropriate use criteria task force, American College of Radiology, American Institute of Ultrasound in Medicine, American Society of Echocardiography, American Society of Nephrology, Intersocietal Commission for the Accreditation of Vascular Laboratories, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Interventional Radiology, Society for Vascular Medicine, Society for Vascular Surgery, [corrected] and Society for Vascular Ultrasound. [corrected] J Am Coll Cardiol. 2012;60:242–76. doi: 10.1016/j.jacc.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qureshi AI, Alexandrov AV, Tegeler CH, Hobson RW, II, Dennis Baker J, Hopkins LN. Guidelines for screening of extracranial carotid artery disease: a statement for healthcare professionals from the multidisciplinary practice guidelines committee of the American Society of Neuroimaging; cosponsored by the Society of Vascular and Interventional Neurology. J Neuroimag. 2007;17:19–47. doi: 10.1111/j.1552-6569.2006.00085.x. [DOI] [PubMed] [Google Scholar]