Abstract
Objective
The purpose of this study is to determine whether individuals with neck pain who demonstrate centralisation of symptoms have more favourable outcome than individuals who do not demonstrate centralisation.
Methods
Eleven subjects with neck pain were evaluated and treated by two physical therapists certified in Mechanical Diagnosis and Therapy (MDT). Eleven physical therapy patients underwent a routine initial evaluation and were treated 2–3 times per week using MDT principles and other physical therapy interventions. The Neck Disability Index (NDI) tool was administered at the initial examination, approximately 2 weeks following the initial examination, each subsequent re-evaluation, and at discharge from the study to measure changes in functional outcomes for each subject. Patients continued with treatments until they were discharged or removed from the study. Four subjects were referred back to their physician by treating physical therapist secondary to non-centralisation (NC) and worsening of symptoms.
Results
Of the 11 subjects, six demonstrated centralisation (CEN) and five demonstrated NC. At initial evaluation, the average NDI score for the CEN group was 51.0 (SD ± 19.4) and 56.4 (SD ± 17.6) for the NC group. For the CEN group, the average change in NDI score between initial evaluation and discharge was 41.2 (SD ± 13.2 and 12.2 (SD ± 13.0) for the NC group. The correlation coefficient of CEN and change in NDI score was 0.772 and was statistically significant (P = 0.005).
Conclusions
In this limited sample, people with neck pain demonstrated more favourable outcomes when the CEN phenomenon was observed. Future research on CEN should be investigated with a larger sample size and with a greater number of clinicians trained in the MDT approach.
Keywords: Centralisation, MDT, Cervical radiculopathy, NDI
Introduction
Individuals with neck pain constitute the second largest outpatient population in physical therapy.1 Approximately 50–70% of the population has experienced neck pain in the past 6 months.2,3 Influencing factors of neck pain may include poor posture, muscle sprains, injuries resulting from sporting or occupational activities, or psychological factors such as anxiety or depression.4,5
Neck pain commonly arises insidiously and is generally multifactorial in nature.6 Individuals experiencing radiating pain typically describe peripheral symptoms that are felt in the upper extremity. Cervical radiculopathy is the clinical description of pain and neurological symptoms of nerve root origin. Individuals who demonstrate cervical radiculopathy present with intermittent or constant peripheralisation of symptoms.
Currently, a variety of treatments are used to decrease pain and increase function, but few studies demonstrate which interventions promote the best functional outcomes for individuals with neck pain.7–9 A common principle of treatment used by physical therapists for management of spinal pain is Mechanical Diagnosis and Therapy (MDT).7 According to the patient's response to repeated end range spinal loading movements, MDT classifies patients into three syndromes: dysfunction, derangement or postural syndrome.10 The most prevalent classification is the derangement syndrome, defined as an internal articular displacement that causes a disturbance in the joint and produces pain.11 Symptomatic and mechanical changes may occur with therapeutic loading strategies. Performance of movements that reduce the internal articular displacement can result in a decrease, abolition or centralisation (CEN) of symptoms as well as improvement in range of motion and function. Directional preference is the phenomenon of preference for postures and/or movements that decreases, abolishes or centralises symptoms and/or improves a limited motion.12 The patient's directional preference guides the prescription of specific exercises for treatment. Centralisation, a form of directional preference, is characterised by spinal pain and referred symptoms that are progressively abolished in a distal to proximal direction in response to therapeutic loading strategies.13 Additionally, patients can exhibit non-centralisation (NC) in which the symptoms remain at the distal segment and the symptoms do not move with therapeutic loading strategies. Improvement of function is assessed through the phenomenon of ‘CEN’ of symptoms as reported by the patient.7
The hypothesis for this study was that the CEN as observed in patients would be associated with more favourable functional outcomes as compared to the outcomes of these patients who do not demonstrate centralisation (NC). Centralisation as seen in patients with low back pain (LBP) has been found to be an excellent predictor of a favourable outcome.12–18 Although Edmond et al. found individuals with neck pain who presented with CEN or a directional preference demonstrated improvements in functional outcomes,14 the research is limited. Therefore, the purpose of this study is to determine the relationship between CEN and outcome in people with neck pain and peripheral symptoms who are treated in physical therapy according to the MDT approach.
Methods
Study design
The design of this study is a retrospective chart review with the raters blinded to the subjects participating in the study. The dependent variables were the scores from the Neck Disability Index (NDI) and whether individuals demonstrated CEN or NC. Independent variables included the treating physical therapists and treatment time.
Subjects
The subjects included 11 physical therapy patients who presented with neck pain and were evaluated and treated at a physical therapist owned private practice and a hospital-based outpatient facility in western New York State. This study was approved by the institutional review boards for protection of human subjects at the Catholic Health System of Buffalo, NY, and Daemen College.
Inclusion criteria
Participating patients were included if they presented with the following: (1) they were at least 18 years of age, (2) they were currently experiencing neck pain at the time of the physical therapy referral or (3) they presented with neck pain and presented with symptoms indicating cervical radiculopathy.
Exclusion criteria
Patients were excluded from the study if they presented with any of the following – pregnancy, history of spinal surgery, a progressive disease process, psychological illness – and were experiencing symptoms relative to cervical instability and/or vertebrobasilar insufficiency. Also, excluded were individuals who were unable to understand English or if they were engaged in litigation related to their neck pain.
Physical therapists
Physical therapy examinations and interventions were performed by two physical therapists, one of whom is diplomaed in MDT and the other is certified in MDT. Clare et al. found reliability among physical therapists with these levels of training in classifying patients with the MDT system.3,10 Research also indicates that clinicians with a MDT certification or diplomacy are reliable at detecting CEN.3,18–21
Outcomes instrument
Neck pain can be assessed using a variety of different standardised outcomes, and the NDI is a widely utilised, researched and validated instrument for assessing disability in patients with neck pain.22 Other questionnaires are limited in peer-reviewed research supporting their reliability, validity, consistency and/or responsiveness.2,22–28
The NDI is a self-rated questionnaire with moderate test–retest reliability, and the NDI measures improvement in neck pain and overall patient function.24 Evidence supports the NDI as an efficient and valid tool.2,22–25,28 Macdermid et al.22 noted that questions regarding the reliability of the NDI stem from a failure to consider acute versus chronic status.
The NDI contains seven items related to activities of daily living, two items related to pain and one item related to the ability to read (concentration). Scoring ranges from 0, representing no disability, to a maximum score of 50 (0–100% disability). The minimal detectable change (MDC), a noticeable change in patient symptoms, varies22,29–31 but Macdermid et al.,22 through a systematic review, determined that MDC should be a five-point change (or 10% disability) to be clinically relevant.
Physical examination
Prior to physical examination, individuals signed an informed consent form to agree to participate in the study. Once subjects agreed to participate in the study, each subject filled out the NDI prior to the initial physical therapy exam.
The initial examination followed MDT principles and included, but was not limited to the following: a history and testing of active, repeated end range and passive movements, as well as neurological testing and special tests. During the subjective interview, a past/present medical history was gathered to determine if the individual currently presented with any pathologies such as recent spinal surgery or a progressive disease process that would exclude the patient from participating. Following the history, the physical therapist conducted the physical portion examination. The physical examination also included special tests to rule out vertebrobasilar insufficiency and cervical instability. A home exercise programme that included but was not limited to therapeutic loading strategies and postural correction were given to each subject based on their symptomatic response. Patients who did not demonstrate CEN at the initial examination were assessed for CEN at each subsequent visit.
Intervention
Following the initial evaluation, patients returned to the clinic for physical therapy intervention as determined by their individualised plan of care (average two visits per week). Physical Therapy sessions included any/all of the following: postural correction, therapeutic loading exercises, thrust and non-thrust manipulation as determined by the patient's mechanical response. Direction of movement and force progression were determined by patient's symptomatic response and MDT principles. At the beginning of each session, subjects were reassessed and asked to note changes in pain. At the end of each session, subjects were mechanically reassessed and asked to note changes in their pain prior to leaving. The NDI questionnaires were administered at the initial examination, approximately 2 weeks following the initial examination, each subsequent re-evaluation and at discharge.
Subjects continued therapy until they were discharged by the clinician or were referred back to their physician due to worsening of symptoms, thereby concluding their participation in the study.
Data analysis
Data related to change in NDI score and whether or not a subject presented with CEN were analysed using Statistical Package for the Social Sciences 19 (SPSS). Descriptive statistics were used to calculate mean and standard deviation for initial NDI scores (Table 1) and change in NDI score between evaluation and discharge (Table 2).
Table 1.
Initial NDI Score among the CEN and NC groups
| Group | N | Mean | Std. deviation |
|---|---|---|---|
| NC | 5 | 56.4 | 17.6 |
| CEN | 6 | 51.0 | 19.4 |
Note: NC: non-centralisation; CEN: centralisation; N: number of subjects; NDI: Neck Disability Index; Mean in %.
Table 2.
Change in NDI Score between CEN and NC groups
| Group | N | Mean | Std. deviation |
|---|---|---|---|
| NC | 5 | 12.2 | 13.0 |
| CEN | 6 | 41.2 | 13.2 |
Note: NC: non-centralisation; CEN: centralisation; N: number of subjects; NDI: Neck Disability Index; Mean in %.
A point bi-serial correlation, or a Pearson correlation in SPSS, was calculated to test for associations between change in NDI score and CEN/NC (Table 3). NDI scores were collected and are presented in % disability rather than raw score.
Table 3.
Correlation between change in NDI Score and CEN and NC groups
| Pearson correlation | 0.772** |
|---|---|
| Sig. (2-tailed) | 0.005 |
| N | 11 |
NDI: Neck Disability Index; CEN: centralization; NC: non-centralisation.
Correlation is significant at the 0.01 level (2-tailed).
Results
Eleven subjects consented to participate and completed the study from three physical therapy clinics in western New York. Out of the 11 subjects, six subjects presented with CEN and five subjects presented with NC.
At initial evaluation, the average NDI score for the CEN group was 51.0 (SD ± 19.4) and 56.4 (SD ± 17.6) for the NC group.
Table 1 depicts mean and standard deviation for initial NDI scores. For the CEN group, the average change in NDI score between initial evaluation and discharge was 41.2 (SD ± 13.2) and 12.2 (SD ± 13.0) for the NC group. Table 2 depicts change in NDI score between evaluation and discharge, and Fig. 1 further analyses the difference in change of NDI score between groups, depicting each subject as a data point according to their respective group. The correlation coefficient of CEN and change in NDI score was 0.772 and was statistically significant (P = 0.005). Table 3 depicts the correlation coefficient.
Figure 1.
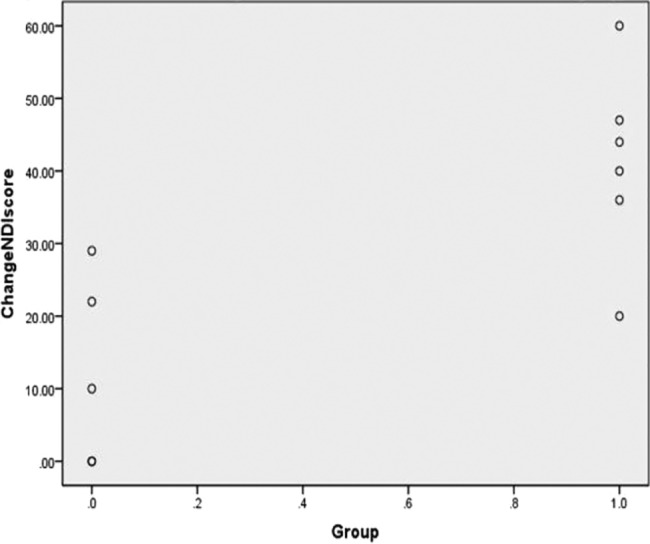
Difference in change of NDI score between the non-centralisation (NC) and centralisation (CEN) groups. Note: 0: NC; 1: CEN; NDI: Neck Disability Index.
Discussion
Sterling et al.32 found that higher initial NDI scores indicated a poor outcome 6 months following injury. While our study did not compare the initial score ranges of our participants, this research by Sterling et al.32 provides a generalised expectation for a NDI score and a patient's prognosis. This patient group also involved victims of whiplash injuries, while we examined patients with or without cervical radiculopathy. Fritz et al.33 focussed on patients with cervical radiculopathy, who had improved NDI scores at 4 weeks, with continued improvement at 6 and 12 months post-treatment. Our study did not include follow-up assessments with the NDI to track improvement. Although traction was added to general exercises in the Fritz et al.33 study, which was not part of our study, a correlation can be made to continued improvement in NDI scores when substantial initial improvement was present. In addition to initial improvements having better results, patient prognosis also is improved based on patient belief. Bishop et al.34 found improved NDI score with manipulation when the patient believed that manipulation would help. Manipulation was included in our study if the clinician believed it was necessary after a progression of forces. The research by Bishop et al.34 demonstrates that if a patient fits inclusion criteria and believes that they will improve with this treatment, manipulation should be incorporated but will not be as effective if the patient is reluctant or pessimistic about manipulation.
Three studies examined the effects of spinal manipulation alone compared to spinal manipulation and another intervention. Spinal thrust manipulation is included in the MDT system of force progression and was included in our study for both groups if the clinician believed it was necessary. Bronfort et al.35 determined that spinal manipulation and strengthening is more beneficial than spinal manipulation alone, and Boyles et al.36 determined no significant difference with the addition of cervical thrust manipulation to manual therapy in comparison to manual therapy alone. Masaracchio et al.37 determined that thoracic spine thrust manipulation with cervical spine mobilisation and interventions is more beneficial than cervical spine non-thrust mobilisation. In addition, subjects in the above studies, who were treated with multiple interventions rather than one intervention (e.g. manipulation alone), were associated with better outcomes. In our study, subjects received McKenzie principles.
Moffett et al.7 compared McKenzie to a cognitive behavioural approach to physical therapy, while Kjellman and Oberg8 compared a control group, a general exercise group (consisting of range of motion, strengthening and endurance exercises) and a McKenzie group. Individuals treated with McKenzie have a higher satisfaction7 and required fewer additional healthcare visits7,8; in addition, individuals presented with a greater short-term reduction in pain intensity.7 However, the subjects in the McKenzie group were not classified as demonstrating DP and/or CEN. Werneke et al.13 classified subjects according to their symptom presentation and determined that NC was associated with worse discharge pain for patients with cervical impairments but was not associated with functional outcomes. Our study determined that the NC group had worse functional outcomes than the CEN group. Similarly, Edmond et al.14 examined functional and pain outcomes of individuals treated with McKenzie and determined that CEN and/or DP groups obtained better improvements in functional outcomes than NC; however, different assessment tools were used to determine functional outcomes and our study examined the functional outcomes of individuals presenting with either CEN or NC.
Limitations/Future Research
There were several limitations in this study that should be considered when interpreting our results. It is a retrospective chart review; therefore, all confounding variables were not evaluated because they were not recorded by the examiners at the time of the study. Also, data were collected at three clinics in the same geographic area, which presents a risk for selection bias. Additionally, the length of the informed consent (eight pages) subjects were required to read and sign prior to the study significantly limited the number of willing participants and should be condensed for future research.
Despite these limitations, our study provides sufficient evidence for considering CEN as a key indicator for better functional outcomes for individuals who present with mechanical neck pain. Boissonnault and Badke1 determined individuals whose symptom duration are greater than 6 months demonstrate significantly less functional improvement;1 therefore, future research should focus on examining the chronicity of symptoms in relation to CEN and functional outcomes. Other considerations may include: gender, age, severity of injury and type of disc derangement to determine if these factors play a significant role in improving functional outcomes for individuals with mechanical neck pain.
Conclusion
This study found that CEN was correlated with better outcomes compared to NC. Therefore, in this limited sample, subjects with neck pain who demonstrated CEN were more likely to attain better functional outcomes than subjects who do not demonstrate CEN.
Disclaimer Statements
Contributors Terrence Rose, Joshua Butler, Nicholas Salinas, Ryan Stolfus, Tanisha Wheatley: data collection and writing. Ronald Schenk: data collection, writing and study design.
Funding None.
Conflicts of interest There were no conflicts of interest in the conduction of this study.
Ethics approval Approval for this study was received by the Catholic Health System of Buffalo Human Subjects committee and the Daemen College Human Subjects Research Review committee.
References
- 1.Boissonnault WG, Badke M. Influence of acuity on physical therapy outcomes for patients with cervical disorder. Arch Phys Med Rehabil. 2008;89:81–6. [DOI] [PubMed] [Google Scholar]
- 2.Young BA, Walker MJ, Strunce JB, Boyles RE, Whitman JM, Childs JD. Responsiveness of the Neck Disability Index in patients with mechanical neck disorders. Spine J. 2009;9:802–8. [DOI] [PubMed] [Google Scholar]
- 3.Dionne CP, Bybee RF, Tomaka J. Inter-rater reliability of McKenzie assessment in patients with neck pain. Physiother. 2006;92:75–82. [Google Scholar]
- 4.Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334:527–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarig-Bahat H. Evidence for exercise therapy in mechanical neck disorders. Man Ther. 2003;8:10–20. [DOI] [PubMed] [Google Scholar]
- 6.Heintz MM, Hegedus EJ. Multimodal management of mechanical neck pain using a treatment based classification system. J Man Manip Ther. 2008;16(4):217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moffett JK, Jackson DA, Gardiner ED, Torgerson DJ, Coulton S, Eaton S, et al. Randomized trial of two physiotherapy interventions for primary care neck and back pain patients: ‘McKenzie’ vs brief physiotherapy pain management. Rheumatology. 2006;45:1514–21. [DOI] [PubMed] [Google Scholar]
- 8.Kjellman G, Oberg B. A randomized clinical trial comparing general exercise, McKenzie treatment and a control group in patients with neck pain. J Rehabil Med. 2002;34:183–90. [DOI] [PubMed] [Google Scholar]
- 9.Ylinen J, Kautiainen H, Wiren K, Hakkinen A. Stretching exercises vs manual therapy in treatment of chronic neck pain: a randomized, controlled cross-over trial. J Rehabil Med. 2007;39:126–32. [DOI] [PubMed] [Google Scholar]
- 10.Clare HA, Adams R, Maher CG. Reliability of McKenzie classification of patients with cervical or lumbar pain. J Manip Physiol Ther. 2005;28:122–7. [DOI] [PubMed] [Google Scholar]
- 11.McKenzie R, May S. The cervical and thoracic spine mechanical diagnosis and therapy. New Zealand: Spinal Publications; 2006. [Google Scholar]
- 12.May S, Aina A. Centralization and directional preference: a systematic review. Man Ther. 2012;7:497–506. [DOI] [PubMed] [Google Scholar]
- 13.Werneke MW, Hart DL, Resnik L, Stratford PW, Reyes A. Centralization: prevalence and effect on treatment outcomes using a standardized operational definition and measurement method. J Orthop Sports Phys Ther. 2008;38(3):116–26. [DOI] [PubMed] [Google Scholar]
- 14.Edmond SL, Cutrone G, Werneke M, Ward J, Grigsby D, Weinberg J, et al. Association between centralization and directional preference and functional and pain outcomes in patients with neck pain. J Orthop Sports Phys Ther. 2014;44(2):68–75. [DOI] [PubMed] [Google Scholar]
- 15.Werneke M, Hart DL, Cook D. A descriptive study of the centralization phenomenon. Spine. 1999;24(7):676–83. [DOI] [PubMed] [Google Scholar]
- 16.May S, Gardiner E, Young S, Klaber-Moffet J. Predictor variables for a positive long term functional outcome in patients with acute and chronic neck and back pain treated with a McKenzie approach: a secondary analysis. J Man Manip Ther. 2008;16(3):155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Werneke M, Hart DL. Discriminant validity and relative precision for classifying patients with nonspecific neck and back pain by anatomic pain patterns. Spine. 2003;28(2):161–6. [DOI] [PubMed] [Google Scholar]
- 18.Aina A, May S, Clare H. The centralization phenomenon of spinal symptoms – a systematic review. Man Ther. 2004;9:134–43. [DOI] [PubMed] [Google Scholar]
- 19.Fritz JM, Delitt Fritz JM, Delitto A, Vignovic M, Busse RG. Interrater reliability of judgements of the centralization phenomenon and status change during movement testing in patients with low back pain. Arch Phys Med Rehabil. 2000;81:57–61. [DOI] [PubMed] [Google Scholar]
- 20.Kilby J, Stigant M, Roberts A. The reliability of back pain assessment by physiotherapists, using a ‘McKenzie algorithm’. Physiother. 1990;76:579–83. [Google Scholar]
- 21.Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P, Videman T, Alen M. Interexaminer reliability of low back pain assessment using the McKenzie method. Spine. 2002;27:E207–14. [DOI] [PubMed] [Google Scholar]
- 22.Macdermid JC, Walton DM, Avery S, Blanchard A, Etruw E, Mcalpine C, et al. Measurement properties of the Neck Disability Index: a systematic review. J Orthop Sports Phys Ther. 2009;39(5):400–32. [DOI] [PubMed] [Google Scholar]
- 23.Vernon H. The Neck Disability Index: state-of-the-art. J Manip Physiol Ther. 2008;31:491–502. [DOI] [PubMed] [Google Scholar]
- 24.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and numeric pain rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69–74. [DOI] [PubMed] [Google Scholar]
- 25.Schellingerhout JM, Verhagen AP, Heymans MW, Koes BW, de Vet HC, Terwee CB. Measurement properties of disease-specific questionnaires in patients with neck pain: a systematic review. Qual Life Res. 2012;21:659–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pietrobon R, Coeytaux RR, Carey TS, Richardson WJ, DeVellis RF. Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine. 2002;27:515–22. [DOI] [PubMed] [Google Scholar]
- 27.Resnick DN. Subjective outcome assessments for cervical spine pathology: a narrative review. J Chiro Med. 2005;4:113–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Young IA, Cleland JA, Michener LA, Brown C. Reliability, construct validity, and responsiveness of the Neck Disability Index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am J Phys Med Rehabil. 2010;89:831–9. [DOI] [PubMed] [Google Scholar]
- 29.Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine. 2006;31:598–602. [DOI] [PubMed] [Google Scholar]
- 30.Vos CJ, Verhagen AP, Koes BW. Reliability and responsiveness of the Dutch version of the Neck Disability Index in patients with acute neck pain in general practice. Eur Spine J. 2006;15:1729–36. [DOI] [PubMed] [Google Scholar]
- 31.Fritz JM, Brennan GP. Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain. Phys Ther. 2007;87:513–24. [DOI] [PubMed] [Google Scholar]
- 32.Sterling M, Jull G, Kenardy J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Int Assoc Study Pain. 2006;122:102–8. [DOI] [PubMed] [Google Scholar]
- 33.Fritz JM, Thackeray A, Brennan GP, Childs JD. Exercise only, exercise with mechanical traction, or exercise with over-door traction for patients with cervical radiculopathy, with or without consideration of status on a previously described subgrouping rule: a randomized control trial. J Orthop Sports Phys Ther. 2014;44(2):45–56. [DOI] [PubMed] [Google Scholar]
- 34.Bishop MD, Mintken P, Bialosky JE, Cleland JA. Patient expectations of benefit from interventions for neck pain and resulting influence on outcomes. J Orthop Sports Phys Ther. 2013;43(7):457–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine. 2001;26(7):788–99. [DOI] [PubMed] [Google Scholar]
- 36.Boyles RE, Walker MJ, Young BA, Strunce JB, Wainner RS. The addition of cervical thrust manipulations to a manual physical therapy approach in patients treated for mechanical neck pain: a secondary analysis. J Orthop Sports Phys Ther. 2010;40(3):133–40. [DOI] [PubMed] [Google Scholar]
- 37.Masaracchio M, Cleland J, Hellman M, Hagins M. Short-term combined effects of thoracic spine thrust manipulation and cervical spine nonthrust manipulation in individuals with mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2013;43(3):118–27. [DOI] [PubMed] [Google Scholar]


