Abstract
Purpose: To investigate Ontario physiotherapists' knowledge and use of, and attitudes toward, non-steroidal anti-inflammatory drugs (NSAIDs) to identify whether there is a need for physiotherapists to receive education specific to NSAIDs. Method: An existing survey instrument was modified and tested by five Ontario physiotherapists. The final version was distributed electronically to approximately 4,400 Ontario Physiotherapy Association members as a self-administered online questionnaire. Results: A total of 294 physiotherapists responded to the survey (response rate=6.7%). Respondents demonstrated variability in their knowledge of NSAID contraindications, side effects, and drug interactions. Most respondents (62.6%) were incorrect or unsure about where and how to obtain most NSAIDs, and most demonstrated incorrect or uncertain knowledge of the relevant legislation. Despite this lack of knowledge, 50% of respondents recommend NSAIDs to their patients. Conclusions: Many Ontario physiotherapists who participated in this survey recommend NSAIDs to their patients despite having a variable understanding of the legislation and medication-related factors. A lack of thorough knowledge of risks and contraindications has implications for patient safety. Physiotherapists who incorporate medications into their practice should access comprehensive information on appropriate NSAID use and should inform themselves about legislative restrictions to ensure that associated treatment is provided in a manner that is evidence based, safe, and in keeping with regulatory boundaries.
Key Words : legislation, non-steroidal anti-inflammatory agents, patient safety, survey
Abstract
Objectif : enquêter sur les connaissances et l'usage de médicaments anti-inflammatoires non stéroïdiens par les physiothérapeutes de l'Ontario, ainsi que leurs opinions à l'égard de ceux-ci, afin de déterminer si les physiothérapeutes devraient recevoir une formation spécifique sur les anti-inflammatoires. Méthodes : un instrument de sondage existant a été modifié et mis à l'essai par cinq physiothérapeutes ontariens. La version finale a été distribuée électroniquement à environ 4 400 membres de la Ontario Physiotherapy Association. Résultats : 294 physiothérapeutes ont répondu au sondage (taux de réponse=6,7%). Un niveau de connaissance variable a été observé chez les répondants quant aux contre-indications, aux effets secondaires et aux interactions médicamenteuses des anti-inflammatoires. La majorité des répondants (62,6%) avaient une connaissance erronée ou incertaine du mode d'obtention de la plupart des anti-inflammatoires, et la plupart avaient une connaissance erronée ou incertaine des lois régissant leur usage. Malgré ce manque de connaissance, 50% des répondants recommandent des anti-inflammatoires à leurs patients. Conclusions : les physiothérapeutes ontariens qui ont participé au sondage sont nombreux à recommander des anti-inflammatoires à leurs patients malgré un niveau de connaissance variable des lois applicables et de certains facteurs liés aux médicaments. Un manque de connaissance des risques et des contre-indications a des répercussions sur la sécurité des patients. Les physiothérapeutes qui intègrent la médicamentation dans leur pratique devraient se renseigner en profondeur sur l'usage des anti-inflammatoires et les restrictions législatives afin de s'assurer que le traitement associé est dispensé en toute sécurité et conformément aux données probantes et aux lois.
Mots clés : anti-inflammatoires non stéroïdiens, législation, physiothérapeute, sécurité des patients
Canadian physiotherapists are primary-contact health professionals, and many of them work with patients with musculoskeletal conditions or injuries who use non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs are one of the most commonly prescribed medications in the world and are the most frequently encountered drug agents in physiotherapy practice.1 Approximately 29% of Canadians use prescription NSAIDs, and many more use NSAIDs in their over-the-counter (OTC) form.2 Physiotherapists are often asked to recommend medications or advise on their use,3 and they may do so as part of an overall physiotherapy treatment plan to manage pain and control inflammation.
NSAIDs are not without their risks, however, and their use has been associated with adverse effects in healthy individuals and those with risk factors. Risks of oral NSAIDs include central nervous system (CNS) effects, such as headache and dizziness; cardiovascular events, such as myocardial infarction (MI) and ischemia; gastrointestinal (GI) and renal complications, including GI bleeding, ulcers, and renal failure; and allergic reactions.1,4 Risks of topical NSAIDs are relatively low because of their low drug concentration; however, adverse reactions still occur, including cutaneous and gastric irritation, asthma, and renal impairments.5 Although information is lacking about NSAID-related deaths in Canada, a study from Spain has suggested that 15.3 deaths per 100,000 NSAID users can be attributed to NSAID use.6 Further research has suggested that 16,500 NSAID-related deaths occur among patients with rheumatoid arthritis or osteoarthritis every year in the United States.7 Research has also suggested that chronic NSAID use increases the risk of death from bleeding or perforated gastroduodenal ulcers; one systematic review concluded that, on average, 1 in 1,200 patients taking NSAIDs for at least 2 months will die from gastroduodenal complications who would not otherwise have died.8 Tramèr and colleagues extrapolated from this to estimate that approximately 2,000 deaths each year occur in the United Kingdom alone. Even short-term use of NSAIDs has been associated with an increased risk of death and recurrent MI in patients who have already experienced an MI.9
Although OTC NSAIDs are usually used at a lower dose than prescription NSAIDs and are intended to be used for shorter periods, no medicine is without risk to the user. Furthermore, physiotherapists who provide NSAID advice or use NSAIDs with patients may be at risk of medico-legal action should a safety incident occur.
To date, we can find no evidence in the literature of any investigation into Canadian physiotherapists' knowledge or use of NSAIDs in practice. In other countries, studies have revealed the need for physiotherapists to be educated in the medication's mechanism of action, dosage, adverse effects, risk factors, and contraindications.3,10–16 In Canada, the legislation governing physiotherapists varies among provinces. For this reason, we conducted an Ontario-specific study to investigate knowledge and use of, and attitudes toward, NSAIDs in physiotherapy practice and identify whether there is a need for Ontario physiotherapists to receive education specifically about NSAIDs.
To be consistent with other research findings,14 we hypothesized that physiotherapists who recommend NSAIDs would demonstrate greater knowledge of NSAIDs than those who do not recommend NSAIDs. We further hypothesized that physiotherapists who recommend NSAIDs would report sufficient knowledge to do so safely and would demonstrate greater knowledge of the relevant legislation.
Although researchers outside Canada have not found an association between physiotherapists' years of experience and practice behaviour, we hypothesized that those with greater experience would be more likely to recommend NSAIDs than would novice physiotherapists. We further hypothesized that physiotherapists in private practice would be more likely to recommend NSAIDs than those in other practice settings because NSAID use is prevalent in the orthopaedic outpatient population.17
Methods
The Queen's University Health Sciences Research Ethics Board granted approval for the study.
Survey instrument
Grimmer and colleagues'10 questionnaire, used by researchers investigating physiotherapists' knowledge and use of medications in other countries,11–16 was adapted for this study and was tested for face, content, and construct validity by a team of five physiotherapists using an iterative process. Team members were asked to comment on usability, omissions, and ease of completion, and their feedback resulted in changes to question wording, other content, and layout. Questions were designed to identify respondents' knowledge, including where and how to obtain NSAIDs, conditions for which NSAIDs are appropriate, common adverse reactions to NSAIDs, drugs with which NSAIDs interact, and conditions for which NSAIDs may be contraindicated. Questions also addressed knowledge of the relevant legislation, use of NSAIDs in practice, and attitudes toward NSAIDs. Questions about the legislation were reviewed by a representative of the College of Physiotherapists of Ontario (CPO), the provincial regulatory body, and on the basis of this feedback, changes were made to the wording and content of our survey to reduce potential misinterpretation by respondents (see Appendix 1). The survey was mounted as a self-administered questionnaire using FluidSurveys (Fluidware, Ottawa, ON).
Participants
The invitation to participate was sent to all members of the Ontario Physiotherapy Association (OPA), the professional association representing Ontario physiotherapists, in April 2014 using the Canadian Physiotherapy Association's email platform. At that time, the convenience population represented approximately 4,400 physiotherapists.18
Inclusion criteria restricted participation to physiotherapists in active practice who had access to a computer and email. Physiotherapists who self-identified as eligible and interested in participating were asked to access the survey using a hyperlink included in the invitation.
Data analysis
Descriptive statistics were used to analyze the data. The frequency of response to each question, as a percentage of the total number of responses, was analyzed and described by count and proportion. Where respondents could list multiple responses, and when analyzing open-ended textual responses, the principal investigator categorized the responses and analyzed the data as a percentage of the total number of responses.
When inferential statistical analysis was warranted, cell counts were examined. If any cell count was 5 or less, categories were collapsed until either there were no cell counts of 5 or less or the table was reduced to a 2×2 table; in practice, this always led to 2×2 tables, which were analyzed with Fisher's exact tests to examine significance. When all cell counts were more than 5, χ2 was used to examine proportions. Alpha was set at 0.05 to accept or reject the null hypotheses regarding differences in proportion among categories of responses, except when we set them lower to account for multiple comparisons (see Results). All statistical analyses were conducted using algorithms in Microsoft Excel, except Fisher's exact tests, which were calculated using an online calculator.19
Results
Response to survey and subject demographics
A total of 294 physiotherapists responded to at least one question on the survey, representing a 6.7% response rate. More than half of those who initiated the survey (57.8%) completed all questions, with the remaining physiotherapists responding to at least one survey question. Most respondents had more than 15 years of experience (61.9%) and held a bachelor's degree as their entry-level physiotherapy qualification (63.3%).
Non-steroidal anti-inflammatory drug use
Fifty percent of respondents who completed all survey questions (n=140 of 280) reported recommending NSAIDs to their patients. Of those, 88.3% and 79.3% recommend OTC oral and topical NSAIDs, respectively, and 19.3% and 13.8% recommend prescription oral and topical NSAIDs, respectively.
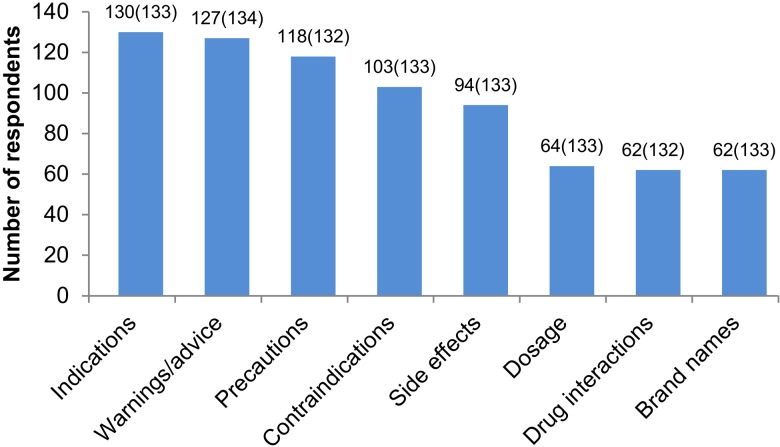
Most respondents who recommend NSAIDs reported that they commonly advise their patients to consult a pharmacist (91.7%) or general or medical practitioner (87.2%). Many also provide warnings or advice as well as information on indications, precautions, contraindications, and side effects. Less commonly, they reported discussing dosage, drug interactions, and brand names (see Figure 1). Of the respondents who recommend NSAIDs, 75.2% reported that they record these discussions in a patient's clinical record.
Figure 1.
Information included in NSAID discussions.
Note: The numbers above the bars indicate the number of respondents who answered yes to including this topic when discussing NSAIDs with patients, followed in parentheses by the total sample size for each question.
NSAIDs=non-steroidal anti-inflammatory drugs.
NSAID knowledge
Respondents demonstrated variable knowledge of where and how to obtain NSAIDs. Only 2.8% (n=3 of 107) of respondents who recommend NSAIDs correctly identified the point of access for all 10 NSAIDs listed. This percentage was not significantly different from that of the respondents who do not recommend NSAIDs; of those, 0.9% answered correctly (n=1 of 112, p=0.36). Most respondents who recommend NSAIDs (63.6%, n=68 of 107) were incorrect about, or did not know at all, where or how to obtain 5 or more NSAIDs, with 4.7% (n=5 of 107) incorrect or unsure of where or how to obtain all 10. Note that results are based on 10 NSAIDs rather than the 13 listed in the survey because 2 of the NSAIDs were identified by drug names not commonly available in Canada, and a third is commonly available in both OTC and prescription forms. Of the 10 NSAIDs considered, 4 require a doctor's prescription (celecoxib [Celebrex], diclofenac [Voltaren] tablets, ketorolac [Toradol], and meloxicam [Mobicox]), and the remainder can be accessed at retail locations without a pharmacy.
Respondents were asked to list conditions for which NSAIDs are appropriate, conditions for which NSAIDs may be contraindicated, common adverse reactions to oral and topical NSAIDs, and drugs with which NSAIDs interact. Most respondents who recommend NSAIDs were able to list at least one correct response for all categories, and many respondents who do not recommend NSAIDs were also able to do so (see Table 1).
Table 1.
Physiotherapists' Knowledge of NSAIDs
| No. (%) of respondents |
|||
|---|---|---|---|
| Findings | Recommend NSAIDs |
Do not recommend NSAIDs |
Total |
| Conditions for which NSAIDs may be indicated (n=178) | |||
| All correct | 79 (84.0) | 64 (76.2) | 143 (80.3) |
| Partially correct | 15 (16.0) | 7 (8.3) | 22 (12.4) |
| Don't know/did not respond | 0 (0.0) | 13 (15.5) | 13 (7.3) |
| Conditions for which NSAIDs may be contraindicated (n=176) | |||
| All correct | 61 (65.6) | 35 (42.2) | 96 (54.5) |
| Partially correct | 18 (19.4) | 23 (27.7) | 41 (23.3) |
| Don't know/did not respond | 14 (15.1) | 25 (30.1) | 39 (22.2) |
| Adverse reactions to oral NSAIDs (n=175) | |||
| All correct | 78 (84.8) | 55 (66.3) | 133 (76.0) |
| Partially correct | 2 (2.2) | 1 (1.2) | 3 (1.7) |
| Don't know/did not respond | 12 (13.0) | 27 (32.5) | 39 (22.3) |
| Adverse reactions to topical NSAIDs (n=175) | |||
| All correct | 63 (68.5) | 44 (53.0) | 107 (61.1) |
| Partially correct | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Don't know/did not respond | 29 (31.5) | 39 (47.0) | 68 (38.9) |
| Drugs with which NSAIDs may interact (n=176) | |||
| All correct | 34 (36.2) | 14 (17.1) | 48 (27.3) |
| Partially correct | 31 (33.0) | 19 (23. 1) | 50 (28.4) |
| Don't know/did not respond | 29 (30.8) | 49 (59.8) | 78 (44.3) |
Note: Percentages may total more than 100 because of rounding.
NSAIDs=non-steroidal anti-inflammatory drugs.
When respondents were asked to list three conditions for which NSAIDs were appropriate, the most common correct responses were inflammation (31.8%), minor musculoskeletal trauma (20.5%), arthritis (19.5%), and pain (17%); when asked to list three conditions for which NSAID use may be contraindicated, the most common correct responses were ulcers (17.9%), GI conditions (12.2%), kidney disorders (9.5%), defects of coagulation (9.5%), and cardiovascular conditions (9.2%). The majority of respondents who recommend NSAIDs demonstrated good knowledge in these areas; 84.0% (n=79 of 94) correctly identified three conditions for which NSAIDs are indicated, and 65.6% (n=61 of 93) correctly identified three conditions for which NSAID use may be contraindicated. The corresponding values for respondents who do not recommend NSAIDs were 76.2% (n=64 of 84) and 42.2% (n=35 of 83), respectively (see Table 1). When we analyzed responses to the question about indications, “all correct” was collapsed into “partially correct” for the Fisher's exact test because respondents who recommend NSAIDs may recommend them for only one condition. The 2×2 table for the Fisher's exact test about indications was therefore composed of [94 (i.e., 79+15), 0, 71 (i.e., 64+7), 13] (see Table 1, top section) to determine whether respondents who recommend NSAIDs were more likely to be knowledgeable about conditions for which NSAIDs may be indicated; the resulting p value was less than 0.001. When we analyzed responses to the question about contraindicated conditions, “partially correct” was collapsed into “don't know/did not respond” because, to be safe, physiotherapists should know all common contraindicated conditions. For the 2×2 table of [61, 32 (i.e., 18+14), 35, 48 (i.e., 23+25)] (see Table 1, second section), the p value was 0.002. Thus, respondents who recommend NSAIDs, although not perfect in their knowledge, were significantly more likely to be correct than respondents who do not recommend NSAIDs.
When respondents were asked to list adverse reactions to NSAIDs, the most common correctly reported adverse reactions to oral NSAIDs were GI disturbances (53.5%), ulcers or GI bleeds (15.4%), and cardiovascular reactions (7.5%), and the most common correctly reported adverse reaction to topical NSAIDs was skin reaction (78.9%). Many respondents who recommend NSAIDs correctly identified one or more adverse reaction to NSAIDs; 98.8% of responses listed for oral NSAIDs and 100% of responses listed for topical NSAIDs were correct. Among respondents who recommend NSAIDs, 84.8% (n=78 of 92) answered entirely correctly for oral NSAIDs, and 68.5% (n=63 of 92) did so for topical NSAIDs. The corresponding values for respondents who do not recommend NSAIDs were 66.3% (n=55 of 83) and 53.0% (n=44 of 83; see Table 1). For statistical analysis, “partially correct” was collapsed into “don't know/did not respond.” For both data sets, respondents who recommend NSAIDs were significantly more likely to demonstrate correct knowledge than respondents who do not (oral NSAIDs, p=0.005; topical NSAIDs, p=0.044).
When respondents were asked to identify three drugs with which NSAIDs interact, the most common correct responses were anti-coagulants (34.5%), anti-hypertensives (27.4%), other NSAIDs (13.4%), and aspirin (7.5%). Respondents' knowledge in this area was limited; only 36.2% (n=34 of 94) of respondents who recommend NSAIDs were able to correctly identify three drugs with which NSAIDs may interact. Among respondents who do not recommend NSAIDs, only 17.1% (n=14 of 82) were able to do the same (see Table 1). For statistical analysis, “partially correct” was collapsed into “don't know/did not respond,” and the resulting Fisher's exact test p value was 0.006. Thus, although knowledge of drug interactions is far from perfect among respondents who recommend NSAIDs, it was significantly better than among those who do not.
Slightly fewer than half of respondents (42.6%, n=75 of 176) reported being made aware of adverse reactions to NSAIDs by at least one of their patients. The most common adverse reactions reported were GI disturbances, including stomach pain and nausea (64.0%), GI bleeds or ulcers (21.3%), and cardiovascular complications, including increased blood pressure and MI (14.7%). Only 15.7% of respondents reported having updated their NSAID knowledge in the past year. An additional 50.5% had updated their knowledge in the past 1–5 years.
Knowledge of legislation
Most respondents, both those who recommend NSAIDs and those who do not, demonstrated incorrect or uncertain knowledge of the legislation, particularly the legislation governing advice and recommendation, sale, and use and administration of NSAIDs (see Table 2). The only category in which most respondents demonstrated correct knowledge was dispensing; this is the preparation and giving out of a medication to a patient, an act overseen by provincial pharmacy regulators.
Table 2.
Physiotherapists' Knowledge of Legislation Regarding NSAIDs
| No. (%) of respondents |
|||
|---|---|---|---|
| Legislation allows |
Legislation does not allow |
Don't know | |
| Physiotherapists to advise on/recommend | |||
| OTC NSAIDs* | 71 (32.3)† | 97 (44.1) | 52 (23.6) |
| Prescription NSAIDs* | 9 (4.1)† | 185 (84.1) | 26 (11.8) |
| Physiotherapists to dispense | |||
| Oral OTC NSAIDs* | 3 (1.4) | 195 (88.6)† | 22 (10.0) |
| Oral prescription NSAIDs* | 0 (0.0) | 205 (93.2)† | 15 (6.8) |
| Topical OTC NSAIDs* | 23 (10.5) | 158 (71.8)† | 39 (17.7) |
| Topical prescription NSAIDs‡ | 4 (1.8) | 192 (87.7)† | 23 (10.5) |
| Physiotherapists to sell | |||
| Oral OTC NSAIDs* | 2 (0.9)† | 190 (86.4) | 28 (12.7) |
| Oral prescription NSAIDs‡ | 0 (0.0) | 199 (90.9)† | 20 (9.1) |
| Topical OTC NSAIDs§ | 18 (8.3)† | 155 (71.1) | 45 (20.6) |
| Topical prescription NSAIDs‡ | 3 (1.4) | 186 (84.9)† | 30 (13.7) |
| Physiotherapists to administer/use in treatment | |||
| Oral OTC NSAIDs* | 3 (1.4)† | 191 (86.8) | 26 (11.8) |
| Oral prescription NSAIDs‡ | 2 (0.9)† | 199 (90.9) | 18 (8.2) |
| Topical OTC NSAIDs* | 59 (26.8)† | 114 (51.8) | 47 (21.4) |
| Topical prescription NSAIDs* | 49 (22.3)† | 137 (62.3) | 34 (15.5) |
n=220.
Correct response.
n=219.
n=218.
OTC=over the counter; NSAIDs=non-steroidal anti-inflammatory drugs.
Because we also had data regarding whether respondents recommend NSAIDs, we were interested to compare their reported actions on recommending with their knowledge of the legislation on this point. Of the 71 respondents who answered that the legislation allows physiotherapists to recommend OTC NSAIDs, 51 reported recommending OTC NSAIDs to their patients, and 20 did not. Of the 149 respondents who answered either that the legislation does not permit such action or that they did not know, 56 reported recommending OTC NSAIDs to their patients, and 93 did not. The difference in proportion was highly significant (Fisher's exact test p<0.001), indicating that although only 51 of the 107 (47.7%) respondents who recommend OTC NSAIDs correctly thought that the legislation allows it, this number is significantly higher than the 20 of 113 (17.7%) respondents who do not recommend OTC NSAIDs who were correct about the legislation. The corresponding analysis for prescription NSAIDs showed that 6.5% (n=7 of 107) of respondents who recommend NSAIDs correctly thought that the legislation allows it, and 1.8% (n=2 of 113) of respondents who do not recommend NSAIDs thought the same thing; the difference in percentages was not statistically significant.
Attitudes toward NSAIDs
Respondents were asked whether they believe that physiotherapists should be able to prescribe NSAIDs, an activity prohibited by the legislation governing Ontario physiotherapists. A slight majority (51.2%) did not believe that physiotherapists should be able to prescribe NSAIDs; however, 31.8% were in favour of a legislative change to allow physiotherapists to do so. The remainder of respondents did not express an opinion.
Respondents were also asked whether their current knowledge was sufficient to safely advise on the use of NSAIDs. Most respondents (82.9%) reported that their current knowledge was insufficient to safely advise on the use of prescription NSAIDs, and 50% reported insufficient knowledge to safely advise on the use of OTC NSAIDs.
When asked to summarize their attitudes toward NSAIDs in physiotherapy practice, 63.1% expressed support for NSAID use, including recommendation, use as an adjunct to treatment, and prescription. Typical comments were as follows:
NSAIDs may be a useful adjunct to conservative management of many conditions. It would be nice to be able to make recommendations where indicated without having to refer patients back to their doctor or pharmacist.
Physiotherapists should be able to advise on and prescribe medications to treat conditions which are within the physiotherapy scope of practice to treat.
A minority (12.1%) were against NSAIDs in practice, with many respondents citing lack of knowledge or training. Others responded that NSAIDs were not a physiotherapist's responsibility. Typical comments included the following:
Not our field. There are doctors and pharmacists that have studied the subject and should be the ones giving advice.
We do not possess sufficient knowledge and should remain drugless practitioners.
Due to the potentially serious side effects and possible drug interactions, I do not feel that we have the proper medical/pharmaceutical background to give advice on NSAIDs.
Multiple respondents highlighted the need for further education (28.2%; 42 of 149) or regulatory oversight (6%) to incorporate NSAIDs into practice.
Respondents were asked to identify who should take responsibility for providing NSAID information to physiotherapists. Multiple answers were provided; these are listed in Table 3.
Table 3.
Whose Responsibility Is It to Provide NSAID Information to Physiotherapists?
| Information source | No. (%) of respondents (n=170) |
|---|---|
| Academic institutions | 121 (71.2) |
| Physiotherapists should seek it themselves | 112 (65.9) |
| Physiotherapy regulatory colleges | 91 (53.5) |
| Physiotherapy conferences | 81 (47.6) |
| Canadian Physiotherapy Association | 80 (47.1) |
| Local pharmacists | 47 (27.6) |
| General practitioners (i.e., medical practitioners, physicians) | 31 (18.2) |
| Drug companies | 26 (15.3) |
| Other | 18 (10.6) |
Associations between practice behaviour and practitioner features
We examined whether there was any relationship between demographic variables, including years of experience, practice setting, and practice behaviour. No statistically significant relationship was found in a χ2 analysis between practice behaviour (recommending or not recommending NSAIDs) and years of experience. When examining whether practice setting was associated with practice behaviour, several frequency counts were less than 5, rendering a χ2 invalid. Therefore, counts for respondents in each setting were compared against total counts for respondents in all other settings in a series of six 2×2 tables, evaluated with Fisher's exact tests. To reduce the chances of a type I error, only ps<0.0083 (0.05/6) were considered significant. Respondents working in a hospital inpatient setting were significantly less likely than others to recommend NSAIDs (p=0.007), and physiotherapists working in private practice were significantly more likely (p=0.006) than others to recommend NSAIDs.
We also examined the association between a physiotherapist's recommendation practice and his or her belief that he or she is sufficiently knowledgeable to recommend OTC NSAIDs safely; 170 respondents answered both questions. Surprisingly, fewer than two-thirds of respondents who reported recommending OTC NSAIDs (58.2%; n=53 of 91) answered yes to the question of whether their knowledge was sufficient to do so. However, this was significantly higher than the percentage of respondents who do not recommend OTC NSAIDs and who answered yes to this question (21.5%; n=17 of 79, Fisher's exact test, p<0.001). Nevertheless, physiotherapists are self-regulated professionals who are expected by their regulatory college and the public to practise in a safe manner. As such, one would expect all physiotherapists who recommend NSAIDs to report that they have sufficient knowledge to do so safely. Therefore, a Fisher's exact test was conducted, comparing a distribution of theoretical public safety, wherein all physiotherapists who recommend NSAIDs would also believe that their knowledge is sufficient to advise patients on the safe use of OTC NSAIDs. The resulting p value was highly significant (<0.001), indicating that the proportion is significantly lower than one would expect if physiotherapists were behaving competently.
Discussion
This study identified that many Ontario physiotherapists who participated in this survey do not have comprehensive knowledge about commonly used NSAIDs. Consistent with previous findings, respondents who recommend NSAIDs were more likely to demonstrate correct knowledge about appropriate NSAID use than those who do not recommend NSAIDs.13 However, even in this subset of respondents, knowledge was inconsistent. Although those who recommend NSAIDs demonstrated good knowledge of indications and conditions for which NSAIDs may be contraindicated, knowledge in all other areas was variable.
Although respondents who recommend NSAIDs were able to accurately list adverse reactions to NSAIDs, the majority (81.5%) demonstrated knowledge of oral NSAIDs that was limited to GI issues, ulcers, or bleeding. Few (26.1%) demonstrated knowledge of cardiovascular, CNS, allergic, or renal complications. This is consistent with previous findings.10,13,16 It is also consistent with research related to patient education by physicians and pharmacists, which found that most patients who were prescribed NSAIDs reported higher rates of counselling on GI risk and comparatively lower rates of counselling on heart attack risk.20
Most respondents who recommend NSAIDs identified skin reactions as an adverse reaction to topical NSAIDs (65.2%); however, only 6.5% demonstrated knowledge of GI disturbance, ulcers, or bleeding, and even fewer demonstrated knowledge of cardiovascular reactions (2.2%). Side effects of oral and topical NSAIDs are almost identical;4 thus, one would expect respondents to have identified the same adverse reactions for both. However, not only did fewer physiotherapists respond when asked about side effects of topical NSAIDs, but also very few of them were able to identify issues other than skin reactions. This is consistent with previous research, which found that respondents listed rashes, itching, and burns as the most common risks associated with use of topical medications.15
Respondents who recommend NSAIDs were more confident in their ability to recommend NSAIDs safely than those who do not recommend NSAIDs. This finding may reflect the self-regulated nature of the profession, whereby physiotherapists work within their legislated scope of practice, considering their own knowledge, skills, and abilities and respecting patient safety. However, many respondents who recommend NSAIDs (41.7%; 38 of 91) continue to do so despite being uncertain of the sufficiency of their knowledge or reporting that their knowledge is insufficient. This is consistent with previous findings.10,16
In addition, more than half of the respondents who recommend NSAIDs are doing so despite being unsure of the legislative constraints (27.1%) or in the belief that the legislation prohibits physiotherapists from recommending NSAIDs (25.2%). Previous studies have also identified a need for physiotherapists to be educated about the relevant legislation.10,15,16
Although Ontario legislation does not prohibit recommending OTC NSAIDs, only half of the respondents recommend NSAIDs to their patients. This result suggests that their recommendation practice is somewhat more conservative than that of physiotherapists in other countries, where studies have identified that between 55% and 100% of respondents recommend NSAIDs.10,11,13
Most respondents who recommend NSAIDs also tend to advise their patients to consult a pharmacist or medical practitioner, both appropriately positioned to provide advice about medication. Thus, although a physiotherapist may not identify all issues of concern with respect to NSAID use, a patient who elects to follow up with a pharmacist or medical practitioner before using NSAIDs should be relatively safe from adverse consequences or should know what to do should they occur.
However, recommending that a patient consult a pharmacist or medical practitioner does not safeguard a physiotherapist from possible medico-legal liability issues. As primary-contact health care professionals, physiotherapists are often asked by their patients to comment on medication.3 NSAIDs, particularly OTC NSAIDs, may be viewed as a relatively safe category of medication to discuss because they are so commonly used and available. Patients may not have access to other practitioners, such as pharmacists or medical practitioners, or they may elect to rely solely on physiotherapists' counsel because they view them as duly qualified professionals with expertise in this area.10 Furthermore, although previous studies have identified incidence ranging from 0%16 to 80%10 for physiotherapists' knowledge of their patients having had adverse reactions to NSAIDs, almost half of the respondents to this survey reported being aware that at least one of their patients had experienced an adverse reaction to NSAIDs.
Previous studies have not identified3 or investigated10–16 a connection between practice setting and behaviour with respect to physiotherapists recommending NSAIDs. However, this study indicates that respondent physiotherapists working in a hospital inpatient setting are less likely, and those in private practice more likely, than others to recommend NSAIDs. This may be because patients seen in private practice commonly seek treatment of conditions for which NSAID use is indicated (e.g., minor musculoskeletal trauma or a condition with associated pain or inflammation). It may also reflect the direct-access nature of the patient–practitioner interaction, whereby the private practice physiotherapist may be the patient's primary or sole caregiver and may thus be the patient's main source of medical information. Patients in hospital, however, may have greater access to additional health care providers, including physicians, nurses, and pharmacists.
Although half of the respondents to this survey recommend NSAIDs, not all record their discussions in the patient's clinical record. This is comparable to the finding of Grimmer and colleagues10 that 65% of respondents recorded NSAID discussions in patient notes. Full and accurate documentation is essential to facilitate appropriate legal defence should a claim be made against a physiotherapist.21 To enhance patient safety, and from a legal perspective, it is perhaps desirable that physiotherapists be discouraged from giving advice to patients on NSAID use unless they are certain that their knowledge is adequate and they are prepared to document these discussions appropriately in patient records.
Limitations
Limitations to this study include representativeness, generalizability, and the survey instrument itself. The survey was a modification of a previously validated and published questionnaire and was pilot tested with physiotherapists representing a variety of practice settings. However, there is always the possibility that some questions remained ambiguous or were misinterpreted, particularly those concerning the relevant legislation. Questions about the legislation were reviewed by a CPO representative, and the activities they described were phrased to align with terms used in the Ontario legislation and in documentation available from the Canadian Alliance of Physiotherapy Regulators. Despite these efforts, the high number of respondents who answered incorrectly or indicated that they did not know the correct response for one or more questions suggests that certain questions may have been misinterpreted. Furthermore, several survey questions, including those about recommendation practice and information included in NSAID discussions, required the respondent to self-report practice behaviour. A discrepancy between self-reported and actual practice behaviour may influence the validity of conclusions drawn from self-reported responses.
The length of the survey and complexity of the questions may have been an impediment because just fewer than half of those who initiated the survey withdrew. An overall response rate of 6.7%, with a 3.9% response rate for fully completed surveys, was achieved. Previous studies have achieved more robust response rates; however, the number of respondents to this study is consistent with other research in the field.10,13–16
Selection bias was introduced by targeting members of OPA, who represent approximately 60% of all registered physiotherapists in Ontario. Physiotherapists who are members of their professional association may differ from non-member physiotherapists in a variety of ways, including their commitment to professional development and clinical best practices. In addition, the survey was sent only to those with accurate email addresses. Because most registered physiotherapists in Ontario are OPA members and much of the communication between OPA and its members is conducted electronically, the impact of this bias is expected to be minimal.
The respondents self-selected when choosing to complete the questionnaire, and as a result, they may have had a particular interest in this topic. Thus, the results must be interpreted with caution because the respondents may not represent the knowledge, behaviour, and attitudes of the general Ontario physiotherapist population or that in other jurisdictions. Moreover, if the sample had been larger and random rather than self-selected, it would have been valid to construct CIs around the proportions; this would have provided greater interpretability of the results.
Despite these limitations, however, the respondents to this survey represent a wide range of experience and all major areas of clinical practice in Ontario. We believe that the survey sample provides insight into the needs of physiotherapists in a range of practice settings. Furthermore, there was a very even split between respondents who do and do not recommend NSAIDs, allowing statistical analysis of both groups.
The responses provided information on issues that should be addressed in educational and professional development programmes, including education on medication-related factors and legislation. The respondents indicated that this information should be made available by academic institutions, regulatory bodies, conferences, and the professional association, among others. Thus, this study suggests a need for these organizations to offer regular publications, educational presentations, and practice updates on the appropriate use of NSAIDs, including strategies to communicate the appropriate knowledge to influence practice and effect optimal patient care and outcomes.
This research was limited by sample size; therefore, it is recommended that a similar study be replicated in Ontario, with a larger, more representative sample to allow the results to be better generalized. Because this research provided information only on Ontario physiotherapy practice, it is also recommended that similar research be undertaken to identify the knowledge and practice patterns of physiotherapists throughout the rest of Canada as well as educational requirements on the best use of NSAIDs.
Conclusion
Many Ontario physiotherapists who responded to this survey provide advice about NSAIDs to their patients. Almost half of the respondents who recommend NSAIDs are doing so despite being uncertain of the sufficiency of their knowledge or reporting that their knowledge is insufficient. According to the principle of self-regulation, physiotherapists are expected to practise within the sphere of their competence; as a result, this finding has implications for professional practice. Given that most of those surveyed also demonstrated a variable understanding of the legislation and medication-related factors, this study identified a need for physiotherapists to be educated in these areas. Physiotherapists treating patients who may inquire about NSAIDs should access and incorporate into their practice up-to-date and comprehensive information on appropriate NSAID use, particularly side effects, contraindications, and drug interactions. Physiotherapists should also inform themselves about legislative restrictions with respect to medications and should recognize the importance of keeping comprehensive patient records. These efforts should assist those physiotherapists who incorporate medications into their practice to do so in a manner that is evidence based, safe, and in keeping with regulatory boundaries.
Key Messages
What is already known on this topic
Researchers in several countries have identified that many physiotherapists lack comprehensive knowledge about NSAIDs, and many also believe that their knowledge is insufficient to safely advise on or recommend NSAIDs. However, patients are asking questions about medications, and physiotherapists are frequently responding. A lack of thorough knowledge of the risks and contraindications has implications for patient safety.
What this study adds
To our knowledge, this is the first study to evaluate Canadian physiotherapists' current knowledge and use of, and attitudes toward, NSAIDs. The results suggest that many Ontario physiotherapists who participated in this survey recommend NSAIDs to their patients, despite having a variable understanding of the legislation and medication-related factors. Our study adds to and complements previous reports on physiotherapists' knowledge of and behaviour regarding NSAIDs.
Appendix 1: Word Version of Online Survey
OTC NSAIDs in practice
Over-the-counter non-steroidal anti-inflammatory drugs in practice: a survey of Ontario physiotherapists' knowledge, use and attitudes
Demographics
Please select the appropriate response
Question 1
Where is your primary place of employment?
-
□
Hospital inpatients
-
□
Private practice
-
□
Hospital outpatients
-
□
Visiting agency/business or home care
-
□
Long-term care facility/Seniors residence/Retirement home
-
□
Other (please specify) ________________
Question 2
How many years of experience do you have as a physiotherapist?
-
□
<1–5
-
□
6–10
-
□
11–15
-
□
16–20
-
□
21–25
-
□
26+
Question 3
What is your entry-level physiotherapy qualification?
-
□
Diploma
-
□
Bachelor's degree
-
□
Master's degree
-
□
Doctoral degree
Question 4
Did your entry-level physiotherapy program include education on non-steroidal anti-inflammatory drugs (NSAIDs)?
-
□
Yes
-
□
No
-
□
Don't recall
Question 5
When did you last update your knowledge of NSAIDs?
-
□
Never (branches to “Current Practice”)
-
□
1–5 years
-
□
5–10 years
-
□
<1 year
-
□
>10 years
Question 6
Did you actively seek out this information?
-
□
Yes
-
□
No
Question 7
How did you obtain this information?
(Please select as many as you require)
-
□
Via another physiotherapist
-
□
Journal (academic) article(s)
-
□
Direct from drug companies
-
□
General medical practitioner
-
□
Via the College of Physiotherapists of Ontario
-
□
Local pharmacist
-
□
Via Canadian Physiotherapy Association
-
□
Compendium of Pharmaceuticals and Specialties (CPS)
-
□
Academic institution (e.g.: university)
-
□
Advertising campaign
-
□
Via Health Canada
-
□
Alliance of Physiotherapy Regulators
-
□
Via Internet search
-
□
Other, please specify… ____________
Current Practice
Question 1
Does your practice/place of employment have a policy regarding physiotherapists recommending NSAIDs to patients?
-
□
Yes
-
□
No
-
□
Don't know
If Yes – Do you follow this policy?
-
□
Yes
-
□
No
If No or Don't know – Do you think such a policy would be beneficial?
-
□
Yes
-
□
No
-
□
Don't know
Question 2
Do you recommend NSAIDs to your patients?
-
□
Yes
-
□
No (If no, branches to Question 7)
If Yes – select as many as are appropriate to your practice
-
□
Over-the-counter oral medication
-
□
Over-the-counter topical medication
-
□
Prescription oral medication
-
□
Prescription topical medication
Question 3
Do your recommendations on the use of NSAIDs include? (select as many as are appropriate)
Warnings/advice Yes □ No □
Indications Yes □ No □
Precautions Yes □ No □
Contraindications Yes □ No □
Drug interactions Yes □ No □
Potential side effects Yes □ No □
Dosage Yes □ No □
Brand names Yes □ No □
Question 4
When recommending NSAIDs do you advise your patients to:
Consult a pharmacist
Yes □ No □
Consult a GP or other medical practitioner
Yes □ No □
Question 5
Which NSAIDs do you usually recommend?
___________________________________________________
Question 6
Do you record any discussions on medications in your clinical records?
Yes □ No □
Question 7
Which of the following sources have you used in the past 6 months to find out about NSAIDs? (Please select as many as you require)
-
□
Current CPS
-
□
Drug company information
-
□
Drug company studies
-
□
Internet sources on drugs
-
□
Medical practitioner
-
□
Pharmacists
-
□
Research papers
-
□
Instructions on packets
-
□
Other, please specify… _______________
-
□
None
Current Knowledge
Question 1
Where are the following medications obtained? (Please select the most appropriate option for each product)
| Retail locations WITHOUT A PHARMACY (e.g., corner store) |
OVER THE COUNTER at retail locations WITH PHARMACY (e.g., Walmart) or PHARMACY |
VIA PHARMACIST at retail locations WITH PHARMACY (e.g., Walmart) or PHARMACY |
Doctor's prescription |
Don't know | |
|---|---|---|---|---|---|
| Indocid | □ | □ | □ | □ | □ |
| Aspirin | □ | □ | □ | □ | □ |
| Voltaren Gel | □ | □ | □ | □ | □ |
| Celebrex | □ | □ | □ | □ | □ |
| Advil | □ | □ | □ | □ | □ |
| Voltaren tablets | □ | □ | □ | □ | □ |
| Ansaid | □ | □ | □ | □ | □ |
| Toradol | □ | □ | □ | □ | □ |
| Anacin | □ | □ | □ | □ | □ |
| Motrin | □ | □ | □ | □ | □ |
| Mobicox | □ | □ | □ | □ | □ |
| Aleve | □ | □ | □ | □ | □ |
| Robaxisal | □ | □ | □ | □ | □ |
Question 2
List the risks that you know are associated with the use of oral NSAIDs:
___________________________________________________
Question 3
List the risks that you know are associated with the use of topical NSAIDs:
___________________________________________________
Question 4
Ontario legislation allows: (Please select the appropriate response)
Physiotherapists to advise on / recommend:
OTC NSAIDs
Yes □ No □ Don't know
Prescription NSAIDs
Yes □ No □ Don't know
Physiotherapists to dispense (i.e.: to prepare and give out):
Oral OTC NSAIDs
Yes □ No □ Don't know
Oral prescription NSAIDs
Yes □ No □ Don't know
Topical OTC NSAIDs
Yes □ No □ Don't know
Topical prescription NSAIDs
Yes □ No □ Don't know
Physiotherapists to sell:
Oral OTC NSAIDs
Yes □ No □ Don't know
Oral prescription NSAIDs
Yes □ No □ Don't know
Topical OTC NSAIDs
Yes □ No □ Don't know
Topical prescription NSAIDs
Yes □ No □ Don't know
Physiotherapists to administer/use the following in patient treatment:
Oral OTC NSAIDs
Yes □ No □ Don't know
Oral prescription NSAIDs
Yes □ No □ Don't know
Topical OTC NSAIDs
Yes □ No □ Don't know
Topical prescription NSAIDs
Yes □ No □ Don't know
Physiotherapists to prescribe NSAIDs
Yes □ No □ Don't know
Question 5
List three conditions for which NSAIDs are appropriate as part of management
1. ______________________________________________
2. ______________________________________________
3. ______________________________________________
Question 6
List three common drugs with which NSAIDs interact
1. ______________________________________________
2. ______________________________________________
3. ______________________________________________
Question 7
List three conditions for which NSAIDs may be contraindicated
1. ______________________________________________
2. ______________________________________________
3. ______________________________________________
Question 8
List common adverse reactions to oral NSAIDs:
__________________________________________________
Question 9
List common adverse reactions to topical NSAIDs:
__________________________________________________
Question 10
Do you know of any of your patients having had adverse reactions to NSAIDs?
Yes □ No □
If Yes – briefly describe:
__________________________________________________
Your views on NSAIDs
Question 1
Do you believe that:
Physiotherapists should be able to prescribe NSAIDs
Yes □ No □ Don't know
Your current knowledge is sufficient to allow you to advise patients on safe use of OTC NSAIDs?
Yes □ No □ Don't know
Your current knowledge is sufficient to allow you to advise patients on safe use of prescription NSAIDs?
Yes □ No □ Don't know
Question 2
Whose responsibility do you think it is to provide information on NSAIDs to physiotherapists? (Select as many as you wish)
-
□
Physiotherapists should seek it themselves
-
□
Drug companies
-
□
Physiotherapy Regulatory Colleges
-
□
Canadian Physiotherapy Association
-
□
Local pharmacists
-
□
General practitioners
-
□
Academic institutions (e.g.: School of Physiotherapy/Pharmacy in a university)
-
□
Physiotherapy conferences
-
□
Other, please specify… ______________
Question 3
Could you summarize your attitude toward the place of NSAIDs in physiotherapist practice?
__________________________________________________
Thank you for taking the time to complete this questionnaire.
References
- 1. Biederman RE. Pharmacology in rehabilitation: nonsteroidal anti-inflammatory agents. J Orthop Sports Phys Ther. 2005;35(6):356–67. http://dx.doi.org/10.2519/jospt.2005.35.6.356. Medline:16001907 [DOI] [PubMed] [Google Scholar]
- 2. Rostom A, Moayyedi P, Hunt R; Canadian Association of Gastroenterology Consensus Group. Canadian consensus guidelines on long-term nonsteroidal anti-inflammatory drug therapy and the need for gastroprotection: benefits versus risks. Aliment Pharmacol Ther. 2009;29(5):481–96. http://dx.doi.org/10.1111/j.1365-2036.2008.03905.x. Medline:19053986 [DOI] [PubMed] [Google Scholar]
- 3. Lansbury G, Sullivan G. Advising clients about prescription medications: a survey of physiotherapy practice in Australia. Physiotherapy. 2002;88(1):18–24. http://dx.doi.org/10.1016/S0031-9406(05)60525-1 [Google Scholar]
- 4. Risser A, Donovan D, Heintzman J, et al. . NSAID prescribing precautions. Am Fam Physician. 2009;80(12):1371–8. Medline:20000300 [PubMed] [Google Scholar]
- 5. Vaile JH, Davis P. Topical NSAIDs for musculoskeletal conditions: a review of the literature. Drugs. 1998;56(5):783–99. http://dx.doi.org/10.2165/00003495-199856050-00004. Medline:9829153 [DOI] [PubMed] [Google Scholar]
- 6. Lanas A, Perez-Aisa MA, Feu F, et al. ; Investigators of the Asociación Española de Gastroenterología (AEG). A nationwide study of mortality associated with hospital admission due to severe gastrointestinal events and those associated with nonsteroidal antiinflammatory drug use. Am J Gastroenterol. 2005;100(8):1685–93. http://dx.doi.org/10.1111/j.1572-0241.2005.41833.x. Medline:16086703 [DOI] [PubMed] [Google Scholar]
- 7. Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999;340(24):1888–99. http://dx.doi.org/10.1056/NEJM199906173402407. Medline:10369853 [DOI] [PubMed] [Google Scholar]
- 8. Tramèr MR, Moore RA, Reynolds DJM, et al. . Quantitative estimation of rare adverse events which follow a biological progression: a new model applied to chronic NSAID use. Pain. 2000;85(1–2):169–82. http://dx.doi.org/10.1016/S0304-3959(99)00267-5. Medline:10692616 [DOI] [PubMed] [Google Scholar]
- 9. Schjerning Olsen AM, Fosbøl EL, Lindhardsen J, et al. . Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study. Circulation. 2011;123(20):2226–35. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.004671. Medline:21555710 [DOI] [PubMed] [Google Scholar]
- 10. Grimmer K, Kumar S, Gilbert A, et al. . Non-steroidal anti-inflammatory drugs (NSAIDs): physiotherapists' use, knowledge and attitudes. Aust J Physiother. 2002;48(2):82–92. http://dx.doi.org/10.1016/S0004-9514(14)60202-6. Medline:12047206 [DOI] [PubMed] [Google Scholar]
- 11. Unger M, Lochner R. Pharmacology practice and South African physiotherapists—part one. South African J Physiother. 2005;61(3):21–7 [Google Scholar]
- 12. Unger M, Lochner R. Pharmacology practice and South African physiotherapists—part two a needs analysis. South African J Physiother. 2006;62(2):18–22 [Google Scholar]
- 13. Braund R, Abbott JH. Recommending NSAIDs and paracetamol: A survey of New Zealand physiotherapists' knowledge and behaviours. Physiother Res Int. 2011;16(1):43–9. http://dx.doi.org/10.1002/pri.472. Medline:21110412 [DOI] [PubMed] [Google Scholar]
- 14. Braund R, Abbott JH. Nonsteroidal antiinflammatory drugs (NSAIDs) and paracetamol for acute musculoskeletal injuries: physiotherapists' understanding of which is safer, more effective, and when to initiate treatment. Physiother Theory Pract. 2011;27(7):482–91. http://dx.doi.org/10.3109/09593985.2010.527430. Medline:21548816 [DOI] [PubMed] [Google Scholar]
- 15. Onigbinde AT, Olaogun MOB, Iroghue K. An evaluation of the knowledge level of Nigerian physiotherapists on topical pharmacotherapy. Hong Kong Physiother J. 2012;30(1):36–42. http://dx.doi.org/10.1016/j.hkpj.2011.11.003 [Google Scholar]
- 16. Coelho-de-Souza LN, Gomes ST, Abdon AP, et al. [Physical therapists understanding and attitudes toward non-steroidal anti-inflammatory drugs]. Revista Dor. 2013;14(1):44–7. Portuguese http://dx.doi.org/10.1590/S1806-00132013000100011 [Google Scholar]
- 17. Boissonnault WG. Prevalence of comorbid conditions, surgeries, and medication use in a physical therapy outpatient population: a multicentered study. J Orthop Sports Phys Ther. 1999;29(9):506–19, discussion 520–5. http://dx.doi.org/10.2519/jospt.1999.29.9.506. Medline:10518293 [DOI] [PubMed] [Google Scholar]
- 18. Green M. (BMS Canada Risk Services Ltd.). Conversation with: R. Lipson (Canadian Physiotherapy Association). 2014. July 10
- 19. GraphPad Software Inc. QuickPad 2x2 contingency tables. La Jolla (CA): GraphPad Software Inc.; 2016. [cited 2015 Aug 20] Available from: http://graphpad.com/quickcalcs/contingency1/ [Google Scholar]
- 20. Schmitt MR, Miller MJ, Harrison DL, et al. . Communicating non-steroidal anti-inflammatory drug risks: verbal counseling, written medicine information, and patients' risk awareness. Patient Educ Couns. 2011;83(3):391–7. http://dx.doi.org/10.1016/j.pec.2010.10.032. Medline:21129892 [DOI] [PubMed] [Google Scholar]
- 21. Canadian Physiotherapy Association. Occupational risk. Ottawa: The Association; 2012. [cited 2014 Aug 15]. Available from: http://physiotherapy.ca/Practice-Resources/Resources/Resources/Risk-Management-Resource-1 [Google Scholar]