Abstract
Purpose: To investigate the interrater reliability of inter-rectus distance (IRD) measured from ultrasound images acquired at rest and during a head-lift task in parous women and to establish the standard error of measurement (SEM) and minimal detectable change (MDC) between two raters. Methods: Two physiotherapists independently acquired ultrasound images of the anterior abdominal wall from 17 parous women and measured IRD at four locations along the linea alba: at the superior border of the umbilicus, at 3 cm and 5 cm above the superior border of the umbilicus, and at 3 cm below the inferior border of the umbilicus. The interrater reliability of the IRD measurements was determined using intra-class correlation coefficients (ICCs). Bland-Altman analyses were used to detect bias between the raters, and SEM and MDC values were established for each measurement site. Results: When the two raters performed their own image acquisition and processing, ICCs(3,5) ranged from 0.72 to 0.91 at rest and from 0.63 to 0.96 during head lift, depending on the anatomical measurement site. Bland-Altman analyses revealed no systematic bias between the raters. SEM values ranged from 0.23 cm to 0.71 cm, and MDC values ranged from 0.64 cm to 1.97 cm. Conclusion: When using ultrasound imaging to measure IRD in women, it is acceptable for different therapists to compare IRDs between patients and within patients over time if IRD is measured above or below the umbilicus. Interrater reliability of IRD measurement is poorest at the level of the superior border of the umbilicus.
Key Words : abdominal muscles, reproducibility of results, ultrasonography
Abstract
Objectif : examiner la fiabilité interévaluateurs de la mesure de la distance entre les deux faisceaux du grand droit, au repos et en contraction, à partir d'échographies prises chez des femmes qui ont eu un enfant, et établir l'erreur type de mesure (ETM) et le changement minimal détectable (CMD) entre deux évaluateurs. Méthodes : deux physiothérapeutes ont obtenu indépendamment des échographies de la paroi abdominale antérieure de 17 femmes et mesuré la distance sur quatre sites le long de la ligne blanche : au bord supérieur de l'ombilic, à 3 cm et à 5 cm au-dessus du bord supérieur de l'ombilic et 3 cm sous le bord inférieur de l'ombilic. La fiabilité interévaluateurs des mesures a été déterminée à l'aide de coefficients de corrélation intraclasse (CCI). Des analyses Bland-Altman ont été réalisées afin de détecter le biais entre les évaluateurs et les valeurs ETM et CMD ont été calculées pour chaque site de mesure. Résultats : lorsque les deux évaluateurs ont obtenu et traité eux-mêmes les images, les CCI(3,5) allaient de 0,72 à 0,91 au repos et de 0,63 à 0,96 en contraction, selon le site de mesure. Les analyses Bland-Altman n'ont révélé aucun biais systématique entre les évaluateurs. Les valeurs ETM allaient de 0,23 cm à 0,71 cm, les valeurs CMD de 0,64 cm à 1,97 cm. Conclusion : lorsqu'on mesure la distance entre les faisceaux du grand droit à partir d'échographies, il est acceptable pour différents thérapeutes de comparer la distance entre patients et au fil du temps pour un même patient si la distance est mesurée au-dessus ou en dessous de l'ombilic. La fiabilité interévaluateurs de la mesure est la plus faible au niveau du bord supérieur du nombril.
Mots clés : échographie, muscles abdominaux, reproductibilité des résultats
Introduction
Inter-rectus distance (IRD) is defined as the width of the linea alba between the connective tissue sheaths surrounding the paired rectus abdominis muscles; it normally ranges between 1.0 and 2.2 cm at rest, depending on the anatomical measurement site.1,2 Increased IRD is the hallmark of diastasis recti, a condition primarily associated with pregnancy in which there is a visible and palpable separation between the two heads of the rectus abdominis. Reliable and valid measures of IRD are of interest because it has been suggested that abnormal IRD and slackening of the linea alba3–6 may contribute to lumbopelvic dysfunction4–8 and urogynecological complaints such as pelvic organ prolapse, urinary incontinence, and fecal incontinence.9,10
IRD is often measured under two conditions: at rest (with the abdominal muscles relaxed) and during abdominal muscle activation,11–13 using a task such as a head lift. These measurements can be used to detect and quantify changes in IRD in patients over time, both naturally occurring1 and in response to physiotherapeutic interventions.14–18 Furthermore, the narrowing or widening of the linea alba during activity (i.e., change in IRD from rest) is thought to provide insight into its functional capacity to transmit forces generated by the muscles of the lateral abdominal wall3 and has been suggested as a means of determining the appropriateness of certain interventions.3,12
Ultrasound imaging (USI) has been named the gold standard for non-invasive IRD assessment.19 IRD measurements using USI are reportedly valid compared with intra-operative surgical compass measurements when imaging is performed at or above the level of the umbilicus.20 USI has also reportedly produced consistent IRD measurements between sessions when performed by the same operator.11,21 In addition, USI is more responsive to changes in IRD than palpation,22 the traditional method of assessing IRD.
Given the interest in IRD and linea alba function in postpartum patient populations and the increasing accessibility of USI as this technology becomes more affordable,23 it is likely that USI will be adopted by physiotherapists as a clinical tool and that IRD, change in IRD during functional tasks, or both will be adopted as one or more clinical outcome measures. Although it has already been demonstrated that, using USI, a single rater (physiotherapist) can reliably measure IRD from one day to another,11,21 the interrater reliability of IRD measured using USI has not been studied. Interrater reliability has important implications for clinical practice because the physiotherapist providing care to a particular patient may change over time, in either temporary (leaves, illnesses, scheduling difficulties) or more permanent (resignation, transfer of care) situations.
Thus, the purposes of this study were (1) to investigate the interrater reliability of IRD, measured at rest and during a head-lift task at four anatomical locations along the linea alba when two separate raters independently performed their own image acquisition and image processing and (2) to establish the standard error of measurement (SEM) and minimal detectable change (MDC) of IRD measurements between the raters using the same measurement sites and test conditions.
Methods
This study was approved by the Queen's University Health Sciences Research Ethics Board (REH-559–13), and all volunteers provided written informed consent before participating. We recruited participants within the Kingston, Ontario, community using flyers and word of mouth. The appropriate sample size for this study was estimated to be 11, using the recommendations from Walter and collegues24 when proposing to perform reliability analyses using intra-class correlation coefficients (ICCs). The underlying assumptions of the sample size calculation included a minimum acceptable reliability coefficient (ICC) of 0.70,25 an expected ICC of 0.90 based on intra-rater reliability studies,11,21 five repetitions of the task, and standard type I (α=0.05) and type II (β=0.20) error rates. We recruited 17 participants to compensate for potential unusable data resulting from poor image quality or unanticipated technical problems.
Participants
Parous women aged between 18 and 60 years were recruited. There were only two exclusion criteria: persistent neck pain within 3 months of volunteering and low back pain that prevented potential participants from lying on their backs for 1 hour. These exclusion criteria were put in place to ensure that all participants would be able to perform the study tasks without pain or difficulty, thus maximizing the consistency of task performance.
Ultrasound imaging system specifications
For all imaging, we used a GE Voluson i system (GE Healthcare, Chalfont St. Giles, UK) interfaced with a two-dimensional, high-frequency (3–10 MHz) linear transducer in B-mode. Anonymized images were exported to a local database for off-line processing.
Rater qualifications
Both raters were physiotherapists who had received training from a national expert in ultrasound system operation as well as in image optimization, acquisition, and processing (this was a structured course consisting of 16 hours covering both theory and practice, although it did not specifically cover IRD measurement). Rater 1 developed the specific methodology for the IRD measurement described in the Procedure section on the basis of performing more than 100 USI evaluations specific to IRD visualization in her regular clinical practice, which focused on women's health issues. Before beginning to collect data for this study, Rater 2 received approximately 10 hours of hands-on training from Rater 1 to standardize the imaging technique and the selection of landmarks for measuring IRD.
Procedure
Each of the two raters acquired images from all participants' anterior abdominal walls; the order of the raters was randomized to ensure that no systematic bias was introduced. Participants were positioned in supine, with their head resting on one pillow. The rater who performed the first set of USI assessments marked four locations along a participant's abdomen using a black skin marker: at the superior border of the umbilicus, 3 cm above the superior border of the umbilicus, 5 cm above the superior border of the umbilicus, and 3 cm below the inferior border of the umbilicus. These marks remained in place for the duration of the data collection session to ensure that both raters acquired images at the same anatomical sites. Each rater captured five ultrasound images at each of these four locations along the linea alba under two conditions: with the abdominal muscles relaxed and during a head lift to activate the rectus abdominis. When performing a head lift, the participant was instructed to keep her neck in line with her spine and to gently lift her head off the pillow so that her head was still touching, but no longer supported by, the pillow. The raters performed visual inspection to ensure that the head-lift task was performed consistently while the data were being collected. In situations in which the investigator was unable to visualize the entire width of the linea alba using the USI approach described here, she inserted an acoustic standoff pad (ATS Laboratories, Bridgeport, CT; 2 cm or 4 cm thick, as required) between the skin surface and the transducer (with ultrasound gel above and below the pad); this increased the field of view so that the borders of the linea alba could be delineated.
Data processing
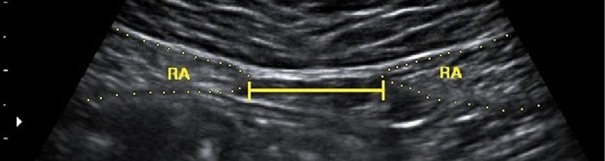
IRD was measured off-line, using ImageJ (National Institutes of Health, Bethesda, MD), from the static, two-dimensional ultrasound images captured at each of the four anatomical locations and during both rest and the head-lift task. Each rater processed the images she had captured and remained blinded to the other rater's IRD measurements while the data were being processed. IRD was determined by measuring the calibrated length of a straight line connecting the medial borders of the hyperechoic fascia surrounding the hypoechoic rectus abdominis heads bilaterally (see Figure 1). The mean IRD was calculated from the five images recorded at each location and under each condition, and these mean values were used in the statistical analyses. When a rater was unable to measure IRD from all five images captured at a particular anatomical location under a particular condition, and as long as there were at least two images of sufficient quality to measure IRD, the average IRD of the usable images was used in the statistical analyses.
Figure 1.
Example of image processing to measure inter-rectus distance.
Note: RA represents the rectus abdominis muscles, with fascia indicated by dotted lines, and the solid line represents the inter-rectus distance.
Data analyses
We performed our statistical analyses using IBM SPSS Statistics version 22 (IBM Corp., Armonk, NY). Data were first tested for normality by visually inspecting histograms and probability–probability plots, and they were confirmed using the Kolmogorov–Smirnov test with a Lilliefors significance correction. Separate analyses were performed for each surface anatomical measurement site and for each condition (rest and head lift).
Interrater reliability was determined by calculating ICCs (see Equation 1) with 95% CIs. Because the raters were fixed, Model 3 according to Shrout and Fleiss26 was chosen. Bland-Altman plots were used to assess the systematic bias between the raters. Bias was said to exist if the 95% CIs around the mean difference between the raters did not include zero.
| (1) |
, where k represents the number of trials (i.e., 5) that were performed for each task, BMS is the between-subject mean square, and EMS is the error mean square.26
The SEM (see Equation 2) was calculated to determine the typical error associated with IRD measurement from ultrasound images captured and processed by two separate raters.
| (2) |
, where SStotal represents the overall variance in the model and n represents the total number of participants.27
The MDC (see Equation 3) was calculated to determine the minimal change in IRD necessary to be certain that a real change had occurred when two different raters performed the USI assessment and IRD measurement.27
| (3) |
.
Currier's recommendations were then used to classify reliability, where a reliability coefficient (i.e., ICC) of 0.69 or less indicated poor reliability; between 0.70 and 0.79, fair reliability; between 0.80 and 0.89, good reliability; and 0.90 or more indicated excellent or high reliability.25
Results
Seventeen parous women aged between 28 and 50 years (mean 38 y, [SD 8]) participated in the study. The average BMI for the sample was 26.4 kg/m2 (SD 7.3). Average participant height was 163.1 cm (SD 5.5). Average parity was 2 children (SD 1), and the average length of time since most recent delivery was 7 years (range 6 mo–25 y).
In 21 of the 680 images acquired by Rater 2 (i.e., 3%), IRD could not be measured because the images were not sufficiently clear. These unusable images were found in seven participants' data. For four of those seven participants, only one of the images was not usable. For one participant, Rater 2 was unable to measure IRD from any of the images captured below the umbilicus; thus, that participant's data were excluded from the statistical analyses for that anatomical location. Rater 1 was able to measure IRD from all of her captured images.
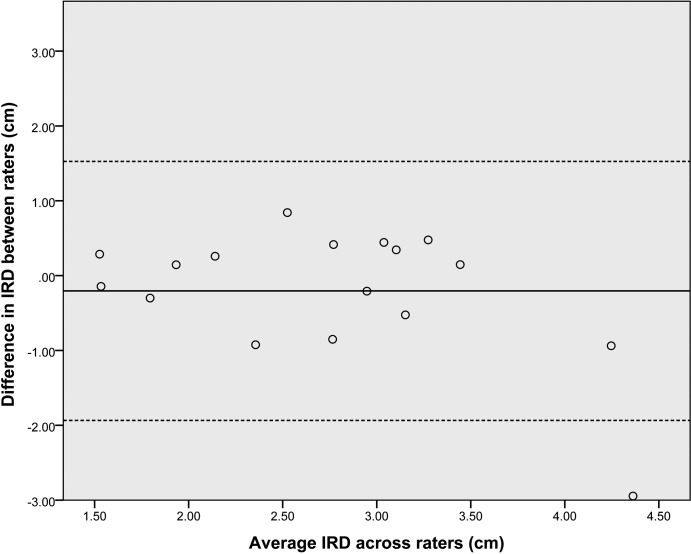
IRD values captured at rest, D(135)=0.049, p=0.20, and during head lift, D(135)=0.061, p=0.20, were normally distributed. Mean IRD values for images captured by each rater are shown in Table 1, and the associated interrater ICC, SEM, and MDC values are displayed in Table 2. Using Bland-Altman analyses, all 95% CIs around the mean difference between the raters included zero; thus, no systematic bias between the raters was found at any measurement site across both tasks. A sample Bland-Altman plot constructed from IRD measurements from both raters at the superior border of the umbilicus at rest is displayed in Figure 2.
Table 1.
Inter-Rectus Distance Measurements Obtained by Each Rater at Four Anatomical Locations at Rest and During Head Lift
| Anatomical measurement site and condition |
Sample size |
Mean (SD) IRD, cm |
|
|---|---|---|---|
| Rater 1 | Rater 2 | ||
| 5ASU | |||
| At rest | 17 | 1.81 (0.85) | 2.24 (0.88) |
| Head lift | 17 | 1.78 (0.84) | 1.97 (0.81) |
| 3ASU | |||
| At rest | 17 | 2.12 (0.83) | 2.39 (0.66) |
| Head lift | 17 | 2.22 (0.88) | 2.08 (0.55) |
| SBU | |||
| At rest | 17 | 2.86 (1.12) | 2.66 (0.73) |
| Head lift | 17 | 2.73 (0.85) | 2.24 (0.65) |
| 3BIU | |||
| At rest | 16 | 1.40 (0.90) | 1.55 (0.76) |
| Head lift | 16 | 1.09 (0.76) | 1.14 (0.58) |
Note: The sample size was reduced to n=16 for measurements made below the umbilicus; Rater 2 was unable to measure IRD from one set of images because the image quality was poor.
IRD=inter-rectus distance; 5ASU=5 cm above the superior border of the umbilicus; 3ASU=3 cm above the superior border of the umbilicus; SBU=superior border of the umbilicus; 3BIU=3 cm below the inferior border of the umbilicus.
Table 2.
Interrater Reliability of Inter-Rectus Distance Measurement
| Anatomical measurement site and condition |
Sample size |
Measurement (cm) |
||
|---|---|---|---|---|
| ICC(3,k) (95% CI) | SEM | MDC | ||
| 5ASU | ||||
| At rest | 17 | 0.91 (0.086, 0.98) | 0.38 | 1.06 |
| Head lift | 17 | 0.96 (0.83, 0.99) | 0.23 | 0.64 |
| 3ASU | ||||
| At rest | 17 | 0.82 (0.61, 0.96) | 0.37 | 1.03 |
| Head lift | 17 | 0.87 (0.65, 0.95) | 0.38 | 1.04 |
| SBU | ||||
| At rest | 17 | 0.72 (0.24, 0.90) | 0.71 | 1.97 |
| Head lift | 17 | 0.63 (0.017, 0.87) | 0.68 | 1.89 |
| 3BIU | ||||
| At rest | 16 | 0.85 (0.58, 0.95) | 0.46 | 1.29 |
| Head lift | 16 | 0.74 (0.23, 0.91) | 0.50 | 1.38 |
Note: The sample size was reduced to n=16 for measurements made below the umbilicus; Rater 2 was unable to measure inter-rectus distance from one set of images because the image quality was poor.
ICC=intra-class correlation coefficient; 95% CI=95% CI around the ICC; SEM=standard error of measurement; MDC=minimal detectable change; 5ASU=5 cm above the superior border of the umbilicus; 3ASU=3 cm above the superior border of the umbilicus; SBU=superior border of the umbilicus; 3BIU=3 cm below the inferior border of the umbilicus.
Figure 2.
Bland-Altman plot using inter-rectus measurement from both raters at the superior border of the umbilicus at rest.
Note: The solid horizontal line is the average difference between raters, and the dotted lines represent the 95% CI around the mean.
IRD=inter-rectus distance.
Discussion
When classifying reliability according to Currier's25 recommendations, interrater reliability of IRD measured using USI above the umbilicus was good to excellent; at the umbilicus, poor to fair; and below the umbilicus, fair to good. On the basis of this classification scheme, it appears that raters are more likely to achieve acceptable consistency when acquiring and processing images above or below the umbilicus. At the superior border of the umbilicus, however, it may be inappropriate to compare IRD among or within patients (i.e., to measure changes in IRD over time or in response to intervention) if different therapists perform the assessment each time. Changes in IRD of less than 2 cm at this level cannot be considered to reflect true changes outside of the measurement error. The MDC is better at measurement sites above (between 0.64 and 1.06 cm) and below (between 1.29 and 1.38 cm) the umbilicus.
We found the greatest measurement error at the superior border of the umbilicus; this is not consistent with what was expected, based on other psychometric studies. Mendes and colleagues20 reported inaccuracies in IRD measurement below the umbilicus compared with intra-operative surgical compass measurement and stated that this result was likely due to a loss of posterior rectus sheath definition (required for IRD landmark visualization) at this level compared with sites at or above the umbilicus.20,28 Consistent with this finding, we had previously found that the measurement error from one day to another was greatest when using USI to measure IRD below the umbilicus compared with sites at or above the umbilicus; this may have been attributable to greater difficulty in visualizing the rectus sheath at this level.21 It is unclear why IRD measurement between the raters was inconsistent at the superior border of the umbilicus. At this level, the posterior rectus sheath is well defined,20,28 and the thickness of the linea alba is similar to its thickness above the umbilicus.28 In our sample, IRD was widest at the superior border of the umbilicus; however, the investigators did not report any increased difficulty in landmark visualization at this site compared with other levels.
Potential sources of interrater error include variations in image acquisition technique and/or variations in image processing. Inconsistencies in image acquisition may be the result of variations in probe location or probe pressure used by the raters.29 In this study, inconsistencies in probe location between the raters were unlikely because both raters used the same marks on the skin surface to ensure that they were acquiring images at the same anatomical locations. Although not explicitly investigated, too much pressure may deform the abdominal wall and the linea alba, and too little pressure will not allow for adequate contact with the skin surface, thus decreasing the ability to visualize the underlying structures. It is possible that the two raters in this study used different amounts of pressure at the superior border of the umbilicus, resulting in inconsistent IRD values at this level. Processing ultrasound images to measure IRD requires a rater to choose the appropriate landmarks that denote the medial borders of the rectus abdominis muscles bilaterally. Although Rater 1 trained Rater 2 on landmark identification and IRD measurement, it is possible that inconsistencies in landmark identification contributed to variable results between the raters; still, it is not clear why this may have occurred to a larger extent at the superior border of the umbilicus than at the other sites.
To determine whether the interrater reliability was more affected by inconsistencies in image acquisition or image processing, a secondary analysis was performed on images acquired at the superior border of the umbilicus. We selected this imaging site because it demonstrated the greatest measurement variability between the raters. Rater 1 processed (i.e., measured IRD on) all images captured at the superior border of the umbilicus by Rater 2. The ICC, SEM, and MDC were calculated again and were improved relative to the values obtained when Rater 2 measured her own images. This improvement was evidenced by higher ICC values both at rest (ICC[3,5]=0.96, 95% CI: 0.90, 0.99) and during head lift (ICC[3,5]=0.89, 95% CI: 0.70, 0.96). The SEMs (0.30 cm at rest, 0.44 cm during head lift) and MDCs (0.83 cm at rest, 1.22 cm during head lift) improved accordingly. This finding suggests that lower interrater reliability at the superior border of the umbilicus may result, in part, from inconsistencies in image processing. Thus, interrater reliability may be improved if the same rater processes all ultrasound images, whether or not he or she acquired them. If IRD measured from USI is to become a clinical outcome measure, it appears that the images should be retained and, if the therapist changes, the new therapist should re-measure the IRD from the initial visit and use this measurement as a basis for comparison on repeat visits.
The intra-rater reliability of IRD measured from one day to another at, above, and below the umbilicus using USI, at rest and during abdominal muscle activation, has been reported in other studies, and the ICCs have been reported to be excellent; all have been above 0.93.11,21 Although our study showed that interrater reliability is acceptable when IRD is measured at most anatomical locations along the anterior abdominal wall, it is not as good as when the rater is kept consistent. In fact, the interrater SEM and MDC values reported here are twice as great as the SEM and MDC values reported when the same rater was used21 (e.g., 5 cm above the superior border of the umbilicus at rest: intrarater MDC=0.29 cm, interrater MDC=1.06 cm). On the basis of these values, measuring changes in IRD over time when the assessing physiotherapist changes may not be adequately reliable, depending on the magnitude of the change expected. For example, the IRD in women in the early postpartum period may be between 4 and 11.5 cm.1,18 IRD has been reported to reduce by 2–9 cm in response to natural recovery or physiotherapeutic intervention.1,18 In such cases, one would be able to detect changes in IRD over time even if the physiotherapist changed. In contrast, it may not be possible to detect changes in IRD in women whose baseline IRD is within 1 cm of normative values. In these situations, IRD measurement using USI is of little value unless the rater is kept constant or, at a minimum, the same rater processes all ultrasound images.
Rater 2 was not able to measure IRD from all of the images she captured, whereas Rater 1 had no unusable images. Given that Rater 1 had more experience with IRD visualization and measurement than Rater 2, clinical experience with the specific imaging technique, including practice in both image acquisition and processing, may play a role in the ability of a physiotherapist to consistently image and measure IRD using USI. Future studies should investigate the impact of hands-on experience on the consistency of IRD measurement.
Limitations
Both raters had more experience with musculoskeletal USI than most physiotherapists currently have. Furthermore, Rater 2 received approximately 10 hours of hands-on training from Rater 1 on IRD measurement. Thus, results generated from this study may not be generalizable to all physiotherapists, but they are generalizable to those who have taken a postgraduate course in USI, who have accumulated some experience with USI of the linea alba, and who have received some training specific to IRD measurement.
Conclusion
Interrater reliability of IRD measurement in parous women using USI when separate raters perform image acquisition and processing is acceptable when they image above the umbilicus or below the umbilicus, but poorest when they image at the level of the superior border of the umbilicus. Thus, it may not be appropriate to compare IRD measured at this level among patients or within patients over time if different therapists have performed the USI protocol and if the observed differences are less than 2 cm. In these situations, it is recommended that images be saved and that the same therapist measure IRD on the images captured at each time point to improve measurement consistency and better detect any changes.
Key Messages
What is already known on this topic
When using ultrasound imaging (USI) to measure inter-rectus distance (IRD) at the level of the umbilicus as well as at levels above and below the umbilicus, high reproducibility is possible from one day to another if the same rater is used; however, IRD measured below the umbilicus has been shown to be inaccurate.
What this study adds
This study is the first to investigate the interrater reliability of IRD measurement using USI. Our results suggest that interrater reliability is acceptable when IRD is measured above or below the umbilicus, but poor when measured at the level of the umbilicus. Reliability improves when the same rater measures all images acquired by different physiotherapists. Depending on the anatomical measurement site, it may not be appropriate to compare IRD among patients or within the same patient over time if different therapists have performed the USI and measurement, a common situation in physiotherapy clinics. Reliability may improve if images have been stored and the new therapist can reprocess the stored images along with the new images to detect changes over time.
References
- 1. Coldron Y, Stokes MJ, Newham DJ, et al. Postpartum characteristics of rectus abdominis on ultrasound imaging. Man Ther. 2008;13(2):112–21. http://dx.doi.org/10.1016/j.math.2006.10.001. Medline:17208034 [DOI] [PubMed] [Google Scholar]
- 2. Beer GM, Schuster A, Seifert B, et al. The normal width of the linea alba in nulliparous women. Clin Anat. 2009;22(6):706–11. http://dx.doi.org/10.1002/ca.20836. Medline:19637295 [DOI] [PubMed] [Google Scholar]
- 3. Lee DG, Hodges P. New perspectives from the Integrated Systems Model for Treating Women with Pelvic Girdle Pain, Urinary Incontinence, Pelvic Organ Prolapse, and Diastasis Rectus Abdominis. Presentation at: The Associated Charter of Physiotherapists in Women's Health Conference; 2013 Sep; Bristol, England http://dianelee.ca/courses-conference-presentations.php [Google Scholar]
- 4. Lee DG, Lee LJ, McLaughlin L. Stability, continence and breathing: the role of fascia following pregnancy and delivery. J Bodyw Mov Ther. 2008;12(4):333–48. http://dx.doi.org/10.1016/j.jbmt.2008.05.003. Medline:19083692 [DOI] [PubMed] [Google Scholar]
- 5. Toranto IR. The relief of low back pain with the WARP abdominoplasty: a preliminary report. Plast Reconstr Surg. 1990;85(4):545–55. http://dx.doi.org/10.1097/00006534-199004000-00009. Medline:2138335 [DOI] [PubMed] [Google Scholar]
- 6. Oneal RM, Mulka JP, Shapiro P, et al. Wide abdominal rectus plication abdominoplasty for the treatment of chronic intractable low back pain. Plast Reconstr Surg. 2011;127(1):225–31. http://dx.doi.org/10.1097/PRS.0b013e3181fad2f7. Medline:21200216 [DOI] [PubMed] [Google Scholar]
- 7. Parker M, Millar LA, Dugan SA. Diastasis rectus abdominis and lumbo-pelvic pain and dysfunction - are they related? J Womens Health Phys Therap. 2009;33(2):15–22. http://dx.doi.org/10.1097/01274882-200933020-00003 [Google Scholar]
- 8. Toranto IR. Resolution of back pain with the wide abdominal rectus plication abdominoplasty. Plast Reconstr Surg. 1988;81(5):777–9. http://dx.doi.org/10.1097/00006534-198805000-00024. Medline:2966414 [DOI] [PubMed] [Google Scholar]
- 9. Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(3):321–8. http://dx.doi.org/10.1007/s00192-006-0143-5. Medline:16868659 [DOI] [PubMed] [Google Scholar]
- 10. Turan V, Colluoglu C, Turkyilmaz E, et al. Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekol Pol. 2011;82(11):817–21. Medline:22384613 [PubMed] [Google Scholar]
- 11. Mota P, Pascoal AG, Sancho F, et al. Test-retest and intrarater reliability of 2-dimensional ultrasound measurements of distance between rectus abdominis in women. J Orthop Sports Phys Ther. 2012;42(11):940–6. http://dx.doi.org/10.2519/jospt.2012.4115. Medline:22810966 [DOI] [PubMed] [Google Scholar]
- 12. Pascoal AG, Dionisio S, Cordeiro F, et al. Inter-rectus distance in postpartum women can be reduced by isometric contraction of the abdominal muscles: a preliminary case-control study. Physiotherapy. 2014;100(4):344–8. http://dx.doi.org/10.1016/j.physio.2013.11.006. Medline:24559692 [DOI] [PubMed] [Google Scholar]
- 13. Sancho F, Pascoal AG, Mota P. An ultrasound study on the effect of exercise on postpartum women inter-rectus abdominis distance. J Biomech. 2012;45(Suppl 1):S493 http://dx.doi.org/10.1016/S0021-9290(12)70494-3 [Google Scholar]
- 14. Acharry N, Kutty RK. Abdominal exercise with bracing, a therapeutic efficacy in reducing diastasis-recti among postpartal females. Int J Physiotherapy Res. 2015;3(2):999–1005. http://dx.doi.org/10.16965/ijpr.2015.122 [Google Scholar]
- 15. Awad M, Morsy M, Mohamed M, et al. Efficacy of Tupler technique on reducing post natal diastasis recti: a controlled study. Brit J Appl Sci Technol. 2016;12(1):1–8. http://dx.doi.org/10.9734/BJAST/2016/17876 [Google Scholar]
- 16. Banerjee A, Mahalakshmi V, Baranitharan R. Effect of antenatal exercise program with and without abdominal strengthening exercises on diastasis rectus abdominis—a post partum follow up. Indian J Physiotherapy Occ Ther. 2013;7(4):123 http://dx.doi.org/10.5958/j.0973-5674.7.4.134 [Google Scholar]
- 17. Chiarello CM, Falzone L, McCaslin K, et al. The effects of an exercise program on diastasis recti abdominis in pregnant women. J Womens Health Phys Therap. 2005;29(1):11–6. http://dx.doi.org/10.1097/01274882-200529010-00003 [Google Scholar]
- 18. Litos K. Progressive therapeutic exercise program for successful treatment of a postpartum woman with a severe diastasis recti abdominis. J Womens Health Phys Therap. 2014;38(2):58–73. http://dx.doi.org/10.1097/JWH.0000000000000013 [Google Scholar]
- 19. Benjamin DR, van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014;100(1):1–8. http://dx.doi.org/10.1016/j.physio.2013.08.005. Medline:24268942 [DOI] [PubMed] [Google Scholar]
- 20. Mendes DA, Nahas FX, Veiga DF, et al. Ultrasonography for measuring rectus abdominis muscles diastasis. Acta Cir Bras. 2007;22(3):182–6. http://dx.doi.org/10.1590/S0102-86502007000300005. Medline:17546290 [DOI] [PubMed] [Google Scholar]
- 21. Keshwani N, McLean L. Ultrasound imaging in postpartum women with diastasis recti: intrarater between-session reliability. J Orthop Sports Phys Ther. 2015;45(9):713–8. http://dx.doi.org/10.2519/jospt.2015.5879. Medline:26161625 [DOI] [PubMed] [Google Scholar]
- 22. Mota P, Pascoal AG, Sancho F, et al. Reliability of the inter-rectus distance measured by palpation. Comparison of palpation and ultrasound measurements. Man Ther. 2013;18(4):294–8. http://dx.doi.org/10.1016/j.math.2012.10.013. Medline:23298825 [DOI] [PubMed] [Google Scholar]
- 23. Szabo T. Diagnostic ultrasound imaging: inside out. 2nd ed. Waltham (MA): Elsevier; 2014. [Google Scholar]
- 24. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101–10. http://dx.doi.org/10.1002/(SICI)1097-0258(19980115)17:1<101::AID-SIM727>3.0.CO;2-E. Medline:9463853 [DOI] [PubMed] [Google Scholar]
- 25. Currier D. Elements of research in physical therapy. 3rd ed. Baltimore: Williams & Williams; 1990. [Google Scholar]
- 26. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–8. http://dx.doi.org/10.1037/0033-2909.86.2.420. Medline:18839484 [DOI] [PubMed] [Google Scholar]
- 27. Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–40. Medline:15705040 [DOI] [PubMed] [Google Scholar]
- 28. Axer H, Keyserlingk DG, Prescher A. Collagen fibers in linea alba and rectus sheaths. I. General scheme and morphological aspects. J Surg Res. 2001;96(1):127–34. http://dx.doi.org/10.1006/jsre.2000.6070. Medline:11181006 [DOI] [PubMed] [Google Scholar]
- 29. Whittaker J. Ultrasound imaging for rehabilitation of the lumbopelvic region. A clinical approach. Philadelphia: Elsevier; 2007. [Google Scholar]