Abstract
Purpose: To explore which socio-demographic, clinical, and other factors are associated with reduced perceived access to physiotherapy among people with low back disorders. Methods: A cross-sectional study design was used to evaluate perceived access to physiotherapy services in a convenience sample of 111 people with low back disorders presenting to a spinal triage service. Participants were asked whether they felt that they had reduced access to physiotherapy as a result of cost, wait time, or location. Bivariate and multivariate logistic regression were used to explore the association between perceived access to physiotherapy and a range of socio-demographic, clinical, and other factors. Results: Overall reduced perceived access to physiotherapy was reported by 27.9% of the sample; 13.5% reported reduced access resulting from cost, 9.9% from wait time, and 10.8% from location. A variety of socio-demographic and clinical variables were found to be associated with reduced perceived access, including the presence of other health conditions, rural residence, and no prior physiotherapy use. Conclusion: Perceived access to physiotherapy among people with low back disorders may be associated with a diverse range of factors. Further research is required to determine the relationship between these variables and actual use of physiotherapy services.
Key Words : health services accessibility, low back pain, survey
Abstract
Objectif : explorer quels facteurs sociodémographiques, cliniques et autres sont associés à la perception d'un accès limité à la physiothérapie chez les personnes souffrant de troubles lombaires. Méthodes : une étude transversale a été menée pour évaluer l'accès perçu aux services de physiothérapie au sein d'un échantillon de commodité formé de 111 patients lombalgiques s'étant présentés dans une clinique de triage. On a demandé aux participants s'ils croyaient que leur accès à la physiothérapie était limité en raison du coût des services, du temps d'attente avant de les obtenir ou encore de l'endroit où ils étaient offerts. Des analyses de régression logistique bivariée et multivariée ont été réalisées pour examiner les liens entre l'accès perçu à la physiothérapie et une gamme de facteurs sociodémographiques, cliniques et autres. Résultats : globalement, 27,9% des participants ont déclaré percevoir qu'ils avaient un accès limité à la physiothérapie; 13,5% ont attribué cet accès limité au coût des services, 9,9% au temps d'attente et 10,8% à l'emplacement. La perception d'accès limité s'est avérée associée à diverses variables sociodémographiques et cliniques telles que la présence d'autres problèmes de santé, un domicile rural ou l'absence d'antécédents en physiothérapie. Conclusions : la perception de l'accès à la physiothérapie chez les personnes souffrant de troubles lombaires peut être associée à une vaste gamme de facteurs. D'autres travaux de recherche seront nécessaires afin de déterminer la relation entre ces variables et l'utilisation réelle des services de physiothérapie.
Mots clés : accessibilité des services de santé, douleur lombaire, physiothérapeutes
Low back pain (LBP) is a prevalent and costly public health issue, and it is one of the leading causes of morbidity worldwide.1 Approximately 22% of Canadians report having chronic back problems.2 Canadians living with chronic health conditions, such as chronic back disorders, are more likely than people without chronic health conditions to report facing barriers to accessing health care services.3 Although people with persistent LBP can use a variety of health care services, their perceived access to these services affects how they actually use them.4
The accessibility of health care services is a key component of high-quality health care. Prior research has examined access to and use of health care providers; however, this work has not provided insight into the reasons why a patient chooses or is able to access a particular health care service.5–7 Access and use are not synonymous because an individual may need to overcome barriers that limit his or her access to a particular service to use it.8 In addition, the health care needs of an individual do not necessarily reflect access to particular services, nor do health care needs consistently correlate with patterns of health care use.9
Wait time is identified by Canadians as an important measure of access to health care, and it is cited as the most prominent barrier among those who experience difficulties obtaining care.10 For example, wait times of up to a year or more were reported by publicly funded Saskatchewan physiotherapists.11 Cost is also a contributor to decreased perceived access to private physiotherapy services, particularly among people whose only health insurance is funded by their province or territory.12 Proximity to health care services is also an important indicator of perceived access, and for this reason, there can be substantial differences in access between urban and rural communities.13
The objective of this study was to determine which socio-demographic, clinical, and other factors are associated with reduced perceived access to physiotherapy services as a result of cost, wait time, or location among people with low back disorders who were referred to a spinal triage service.
Methods
Study design, participants, and variables
This study was a cross-sectional secondary analysis of baseline data from a prospective evaluation of a physiotherapy-led spinal triage service in a private practice setting.14 People are referred to the triage service from primary care providers or from the surgeons associated with it. A regular physiotherapy assessment fee is charged, but it is waived for people who indicate that they do not have the ability to pay. The inclusion criteria were as follows: referral to the triage service primarily with low-back–related complaints, aged 18–80 years, and providing informed consent. The exclusion criteria were receipt of third-party-payer funding (e.g., worker's compensation) for back-related complaints; primarily neck (cervical spine) or mid-back (thoracic spine) complaints; and language, reading, or comprehension barriers that would impede them from adequately completing the paperwork for the study.
Participants first completed a paper-based survey, then underwent a triage assessment performed by a physiotherapist. The physiotherapist also completed a clinical classification tool that, in addition to the survey, established baseline measures. Information gathered from participants at intake included demographic information, general health status, comorbidities, location of symptoms, pain severity, perceived function, and quality of life. Further details regarding the measurement tools can be found elsewhere.14 Participants were also asked whether they thought that physiotherapy services were “available and accessible” (yes–no response) and whether they thought that physiotherapy services were not accessible because of cost, wait time, or location. It took approximately 20–30 minutes for participants to complete their paperwork.
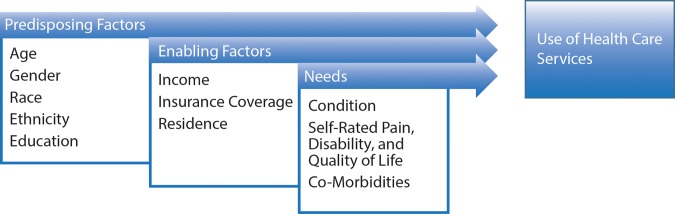
The Aday and Andersen15 model of health care access was used as a guiding framework to identify potential predisposing factors, enabling factors, and needs associated with decreased perceived access to physiotherapy. According to this model (see Figure 1), access includes “[all of the] dimensions which describe the potential and actual entry of a given population group to the health care delivery system.”15(p.5–6) We also included other variables, such as recommendations arising from the triage assessment, that we thought were relevant to our study's objective but that were not directly captured by this model.
Figure 1.
Aday and Andersen model for understanding access to health services.
Analysis
Multivariate logistic regression was used to explore which variables were associated with reduced perceived access to physiotherapy services as a result of cost, wait time, or rural location. The model-building process began with a bivariate analysis exploring the association of socio-demographic, clinical, and other variables using either χ2 or Fisher's exact tests, where appropriate. Any variable that had a p<0.25 from the bivariate analysis was considered to be a candidate for the multivariate models. Correlation between independent variables selected by the bivariate analysis was evaluated using the Spearman correlation coefficient. For any independent variables that were correlated (r>0.5), only the most significant variable (according to the bivariate analysis) was used in the multivariate models. The remaining dependent variables were evaluated with logistic regression, using a backward, step-wise selection procedure, with p values of 0.10 to exit the model and 0.05 to enter it. The final results are presented as crude odds ratios (ORs) and adjusted ORs with 95% CIs. The University of Saskatchewan Research Ethics Board approved this study, and statistical analysis was carried out using PASW Statistics for Mac version 18.0 (SPSS Inc., Chicago, IL).
Results
Description of study sample
During the 8-month study intake period, 198 people were assessed by the spinal triage service. Of these, 142 people met the inclusion criteria, and 27 chose not to participate. This left 115 participants, 111 of whom completed the question about perceived access to physiotherapy. Thus, the overall response rate among those people who were eligible was 78.2% (111/142). The mean age of participants was 51.7 years (range 20–79 y), and 48.6% of the sample was female. Participants had a mean symptom duration of 139 months (11.6 y), ranging from 1 to 480 months (40 y). A description of selected demographic, health, and triage recommendations can be found in Table 1. A full description of the characteristics of the study sample can be found elsewhere.14
Table 1.
Selected Characteristics of Study Sample
| Variable | No. (%) of respondents (n=111) |
|---|---|
| Age <50 y | 51 (45.9) |
| Female | 54 (48.6) |
| Education: completed grade 12 or less | 50 (45.0) |
| Annual household income <$30,000 | 18* (17.1) |
| Rural residence | 73 (65.8) |
| Not working as a result of LBP | 21 (18.9) |
| LBP “caused by work” | 41 (36.9) |
| Past physiotherapy treatment of LBP | 63 (56.8) |
| Other health problems | |
| Bone, muscle, or joint problems | 70 (63.1) |
| Headaches | 42 (37.8) |
| Stomach or digestive problems | 29 (26.1) |
| Lung or breathing problems | 16 (14.4) |
| Two or more health problems (other than LBP) | 66 (59.5) |
| Triage recommendations | |
| Physiotherapy | 63 (56.8) |
| Diagnostic imaging | 30 (27.0) |
| Review by surgeon | 17 (15.3) |
Six respondents chose not to answer this question.
LBP=low back pain.
Perceived access to physiotherapy services
Overall, 27.9% (31/111) of respondents reported reduced perceived access to physiotherapy services. Among all participants, cost was the main reason (13.5%; 15/111), followed by location (10.8%; 12/111) and wait time (9.9%; 11/111). Table 2 summarizes the results of the multivariate analyses for perceived access to physiotherapy care, and it presents both unadjusted and adjusted ORs, along with 95% CIs. The bivariate results of the variables included in the multivariate analyses can be found in Appendix 1.
Table 2.
Crude and Adjusted Estimates for Reduced Perceived Access to Physiotherapy Care
| Odds ratio |
||||
|---|---|---|---|---|
| Variable | Unadjusted | 95% CI | Adjusted | 95% CI |
| Covariates of reduced perceived access as a result of wait time | ||||
| Presence of lung and breathing problems | 6.742 | 1.762, 25.801 | 27.200 | 3.764, 195.543 |
| Presence of other bone and joint problems | 2.877 | 0.590, 14.024 | 5.524 | 0.900, 33.903 |
| No previous physiotherapy treatment of LBP | 1.028 | 0.282, 3.748 | 8.276 | 1.388, 49.331 |
| Diagnostic imaging recommended | 3.800 | 1.065, 13.564 | 8.469 | 1.628, 44.047 |
| Covariates of reduced perceived access as a result of location | ||||
| Presence of lung and breathing problems | 8.900 | 2.409, 32.990 | 71.798 | 5.791, 890.212 |
| Full- or part-time paid employment status | 5.254 | 0.650, 42.476 | 16.305 | 0.797, 333.578 |
| Prior use of prescription medication for back pain | 3.286E8 | 0.000* | 4.211E8 | 0.000* |
| Rural residence | 6.565 | 0.814, 52.926 | 8.198E8 | 0.000* |
| Review by surgeon recommended | 1.317 | 0.326, 5.317 | 55.483 | 1.844, 1,669.555 |
| Covariates of reduced perceived access as a result of cost | ||||
| Age ≥50 y | 2.638 | 0.785, 8.866 | 4.773E51 | 0.000* |
| Annual income <$30,000 | 20.500 | 5.610, 74.916 | 2.372E51 | 0.000* |
| Current smoker | 2.857 | 0.807, 7.956 | 7.307E50 | 0.000* |
| Not married | 9.294 | 2.815, 30.691 | 1.245E77 | 0.000* |
| Obese | 2.286 | 0.388, 5.690 | 7.708E25 | 0.000* |
| LBP caused by work | 3.00 | 0.982, 9.165 | 2.679 | 0.000* |
| Presence of lung and breathing problems | 2.545 | 0.698, 9.288 | 1.310E64 | 0.000* |
| Presence of other bone and joint problems | 2.621 | 0.693, 9.905 | 8.742E12 | 0.000* |
| No urgent referral to surgeon | 3.029E8 | 0.000* | 3.871E52 | 0.000* |
| No follow-up recommended | 1.19E10 | 0.000* | 2.430E53 | 0.000* |
| Other management recommended | 11.273 | 2.226, 57.085 | 2.014 E79 | 0.000* |
Note: ORs significant at 0.05 level appear in bold.
Upper limit of 95% CI cannot be calculated.
LBP=low back pain.
On the basis of the bivariate analyses, the following independent variables were included in the regression models when reduced perceived access to physiotherapy services as a result of wait time was the dependent variable: presence of lung and breathing problems, presence of other bone and joint problems, no previous physiotherapy treatment of LBP, and diagnostic imaging recommended by the spinal triage assessor. All variables except the presence of other bone and joint problems were statistically significant in the final adjusted, multivariate model.
On the basis of the bivariate analyses, the following independent variables were included in the regression models when reduced perceived access to physiotherapy services as a result of location was the dependent variable: the presence of lung and breathing problems, having full- or part-time paid employment, prior use of prescription medication for back pain, living in a rural location, and having a triage recommendation for review by a surgeon. Only the presence of lung and breathing problems and having a triage recommendation for review by a surgeon were significant in the final model.
On the basis of the bivariate analyses, the following independent variables were included in the regression models when reduced perceived access to physiotherapy services as a result of cost was the dependent variable: being age 50 years or older; having an annual income less than $30,000; being a current smoker, unmarried, or obese; having LBP that was thought to be caused by work; the presence of lung and breathing problems; the presence of other bone and joint problems; no urgent referral to a surgeon; no further follow-up recommended; and whether management other than physiotherapy or surgeon review was recommended. None of these variables were significant in the final model.
Discussion
We investigated a variety of factors—age, income, smoking history, marital status, BMI, residence, presence of comorbidities, aspects of previous medical management, and spinal triage management recommendations—and their association with reduced perceived access to physiotherapy services as a result of cost, wait time, or location. These factors can be linked with the predisposing, enabling, and need categories described in the Aday and Andersen15 model for accessing health care (see Figure 1). Only the presence of lung and breathing problems and different spinal triage recommendations were significant in the final multivariate, adjusted models for wait time and location; no variables were significant in the final models for cost.
Predisposing factors are traits of an individual that will lead him or her to seek services. The presence of lung and breathing problems was statistically associated with reduced perceived access as a result of wait time and location. Having other chronic health conditions or comorbidities, such as lung and breathing problems, is linked to reduced access.16 People with additional comorbidities may have reduced functional capacity, making it difficult to physically access services. For people with multiple health conditions, timing and scheduling of appointments may also become a barrier because they may need to have appointments with numerous health care providers to address a wider range of health care needs.
Contrary to our results, previous research has shown that obesity17 and not being married7 are predictors of reduced health care utilization. Although increased age is known to be associated with an increased likelihood of having a chronic health condition, age was not a significant predictor of reduced perceived access in our study.
Enabling factors are environmental factors that may either assist or act as barriers to patients accessing care. Living in a rural area, having full- or part-time paid employment, having an annual income of less than $30,000, and having LBP caused by work were identified in the bivariate analysis as potential variables associated with reduced perceived access; however, none were significant in the final models. These findings are surprising given prior research and what we hypothesize may be environmental factors or barriers to people accessing physiotherapy services. A growing body of literature has demonstrated inequity in access to health care services as a result of geographical or location factors among rural residents.13
Reduced perceived access as a result of cost may be amplified if there is limited access to, or availability of, publicly funded physiotherapy services. Furthermore, employment status may be linked to reduced access because of the travel time required to access physiotherapy services or difficulty scheduling appointments around work hours. Participants who reported that their LBP was caused by work may have financial barriers to accessing care because they have been laid off and have lost their employment income. Inability to work as a result of back pain may also reduce self-efficacy and act as a psychosocial barrier to access.
Need factors are traits of an individual that will precipitate him or her to seek services. Prior use of prescription medication for LBP may indicate that an individual is relying on pharmacological aids because either he or she, or a primary care provider, perceives that other services are unavailable, although further investigation is needed to explore whether this is indeed the case. Relative severity of need can have an impact on people's perception of access by affecting the number of services they require and how motivated they are to seek care.18,19
Other factors of note that are not directly linked to the Aday and Andersen15 model arose from recommendations made in the triage assessment itself. A few variables associated with reduced perceived physiotherapy access stemmed from the triage service: management other than physiotherapy being recommended, recommendation of diagnostic imaging, and recommendation for review by a surgeon. A recommendation of diagnostic imaging was associated with reduced perceived access as a result of wait time. A recommendation by the spinal triage assessor for review by a surgeon or an urgent referral to a surgeon was associated with reduced perceived access as a result of location. The association between these factors and perceived access may be influenced by the participants' knowledge of availability of services and actual prior access to physiotherapy, specialist services, or both. Knowledge and availability of physiotherapy services may have affected the types of referrals made by the spinal triage physiotherapist.
There are many limitations to our study. This convenience sample of people referred to a spinal triage service may not represent a typical person who presents with low back complaints in a primary care setting.20 Further bias may have been introduced by restricting the sample to only those who had adequate reading and comprehension skills to complete the paperwork for the study. The cross-sectional design precludes us from determining causal relationships among variables. Furthermore, the lack of statistical significance of most of the covariates in the adjusted models suggests that a larger sample size, with possibly less variability, is needed to fully explore the contribution of each variable to perceived access.
The sample size was further reduced when we examined certain variables with missing data (e.g., household income). Also, despite the large range of variables considered in the analysis and the use of the Aday and Andersen15 model as a guiding framework, important key variables, such as ethnicity, that are potentially associated with reduced physiotherapy access, were not included in our study. Also of interest is determining the impact of location, cost, and wait time among people and groups who have the greatest potential need for physiotherapy services, thus helping to ensure more equitable access. Relating perceived access to health care services to actual accessibility or use of these services will assist policymakers to develop strategies that increase the appropriate distribution and availability of physiotherapy services.
Conclusion
Perceived access to physiotherapy may be affected by cost, wait time, and location. Among this sample of people with chronic low back disorders referred to a private spinal triage service, cost was the most common reason for reduced perceived access. Reduced perceived access may be associated with the presence of predisposing, enabling, and need factors of an individual or with health service characteristics, such as spinal triage recommendations in this population. These results provide insight into the variables affecting perceived access and may be useful for guiding future research aimed at improving equitable access to physiotherapy services.
Key Messages
What is already known on this topic
Equitable access to health care means that services are available wherever and whenever a person needs them. Realized access is actual use of services, whereas potential access is linked to an individual's perception of access as well as other contextual and environmental factors. Much of the health services research to date has focused on use of services; however, perceived access is an important factor influencing patterns of use and equity of access to care, and it has been studied very little to date. Uncovering factors relating to perceived barriers may help improve equitable access to physiotherapy services.
What this study adds
Cost was the most common reason for reduced perceived access in this sample of people referred to a privately delivered spinal triage service. A variety of predisposing, enabling, and need factors are associated with reduced perceived access to physiotherapy services as a result of wait time and location among people with low back disorders. However, this study did not identify any statistically significant variables associated with reduced perceived access resulting from cost. The results of this exploratory study may have implications for further research evaluating the effect of perceived access on use of physiotherapy services as well as investigating strategies to improve equitable access to services.
Appendix 1: Bivariate Analysis Summary
Reduced perceived access to physiotherapy as a result of wait time
| No. (%) of respondents |
|||
|---|---|---|---|
| Variable | Not accessible (n=11) |
Accessible (n=100) |
p-value |
| Lung and breathing problems | 5 (45.5) | 11 (11.0) | 0.002 |
| Other bone and joint problems | 9 (81.8) | 61 (61.0) | 0.21 |
| No previous physiotherapy treatment of LBP | 8 (72.7) | 40 (40.0) | 0.054 |
| No diagnostic imaging recommended | 6 (54.5) | 24 (24.0) | 0.030 |
Reduced perceived access to physiotherapy as a result of location
| No. (%) of respondents |
|||
|---|---|---|---|
| Variable | Not accessible (n=12) |
Accessible (n=99) |
p-value |
| Lung and breathing problems | 6 (50.0) | 10 (10.1) | <0.001 |
| Full- or part-time employment status | 11 (91.7) | 67 (67.7) | 0.11 |
| Previous use of prescription medication for LBP | 12 (100.0) | 59 (59.6) | 0.004 |
| Review by surgeon recommended | 2 (16.7) | 4 (4.0) | 0.13 |
| Rural residence | 12 (100.0) | 71 (71.7) | 0.035 |
Reduced perceived access to physiotherapy as a result of cost
| No. (%) of respondents |
|||
|---|---|---|---|
| Variable | Not accessible (n=15) |
Accessible (n=96) |
p-value |
| Age ≥50 | 11 (73.3) | 49 (51.0) | 0.16 |
| Income <$30,000 per year | 10 (66.7) | 8 (8.9)* | <0.001 |
| Current smoker | 6 (40.0) | 20 (20.8) | 0.10 |
| Not married | 10 (66.7) | 17 (17.7) | <0.001 |
| Obese | 8 (53.3) | 32 (33.3) | 0.13 |
| LBP caused by work | 9 (60.0) | 32 (33.3) | 0.047 |
| Presence of lung and breathing problems | 4 (26.7) | 12 (12.5) | 0.23 |
| Presence of other bone and joint problems | 12 (80.0) | 58 (60.4) | 0.17 |
| No urgent surgeon referral recommended | 15 (100.0) | 80 (83.3) | 0.12 |
| No follow-up recommended | 13 (86.7) | 96 (100.0) | 0.017 |
| Other management recommended | 4 (26.7) | 3 (3.1) | 0.006 |
Six respondents chose not to answer this question.
References
- 1. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–96. http://dx.doi.org/10.1016/S0140-6736(12)61729-2. Medline:23245607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bath B, Trask C, McCrosky J, et al. A biopsychosocial profile of adult Canadians with and without chronic back disorders: a population-based analysis of the 2009-2010 Canadian Community Health Surveys. BioMed Res Int. 2014;2014:919621 http://dx.doi.org/10.1155/2014/919621. Medline:24971357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ronksley PE, Sanmartin C, Quan H, et al. Association between perceived unmet health care needs and risk of adverse health outcomes among patients with chronic medical conditions. Open Med. 2013;7(1):e21–30. Medline:23687534 [PMC free article] [PubMed] [Google Scholar]
- 4. Chevan J, Riddle DL. Factors associated with care seeking from physicians, physical therapists, or chiropractors by persons with spinal pain: a population-based study. J Orthop Sports Phys Ther. 2011;41(7):467–76. http://dx.doi.org/10.2519/jospt.2011.3637. Medline:21654096 [DOI] [PubMed] [Google Scholar]
- 5. Lim K-L, Jacobs P, Klarenbach S. A population-based analysis of healthcare utilization of persons with back disorders: results from the Canadian Community Health Survey 2000-2001. Spine. 2006;31(2):212–8. http://dx.doi.org/10.1097/01.brs.0000194773.10461.9f. Medline:16418643 [DOI] [PubMed] [Google Scholar]
- 6. Ritzwoller DP, Crounse L, Shetterly S, et al. The association of comorbidities, utilization and costs for patients identified with low back pain. BMC Musculoskelet Disord. 2006;7(1):72 http://dx.doi.org/10.1186/1471-2474-7-72. Medline:16982001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Walker BF, Muller R, Grant WD. Low back pain in Australian adults. Health provider utilization and care seeking. J Manipulative Physiol Ther. 2004;27(5):327–35. http://dx.doi.org/10.1016/j.jmpt.2004.04.006. Medline:15195040 [DOI] [PubMed] [Google Scholar]
- 8. Thorpe JM, Thorpe CT, Kennelty KA, et al. Patterns of perceived barriers to medical care in older adults: a latent class analysis. BMC Health Serv Res. 2011;11(1):181 http://dx.doi.org/10.1186/1472-6963-11-181. Medline:21812953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Allin S, Grignon M, Le Grand J. Subjective unmet need and utilization of health care services in Canada: what are the equity implications? Soc Sci Med. 2010;70(3):465–72. http://dx.doi.org/10.1016/j.socscimed.2009.10.027. Medline:19914759 [DOI] [PubMed] [Google Scholar]
- 10. Carrière G, Sanmartin C. Waiting time for medical specialist consultations in Canada, 2007. Health Rep. 2010;21(2):7–14. Medline:20632519 [PubMed] [Google Scholar]
- 11. Health Sciences Association of Saskatchewan. Market supplement adjudication physical therapists [Internet]. Saskatoon and Regina: The Association; 2012. [cited 2015 Mar 18]. Available from: http://www.hsas.ca/assets/market-supplement-report-physical-therapist-september-26-2012.pdf [Google Scholar]
- 12. Bath B, Janzen B. Patient and referring health care provider satisfaction with a physiotherapy spinal triage assessment service. J Multidiscip Healthc. 2012;5:1–15. Medline:22328826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sibley LM, Weiner JP. An evaluation of access to health care services along the rural-urban continuum in Canada. BMC Health Serv Res. 2011;11(1):20 http://dx.doi.org/10.1186/1472-6963-11-20. Medline:21281470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bath B, Lovo Grona S. Biopsychosocial predictors of short-term success among people with low back pain referred to a physiotherapy spinal triage service. J Pain Res. 2015;2015(8):189–202. http://dx.doi.org/10.2147/JPR.S81485. Medline:25960675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aday LA, Andersen RM. Equity of access to medical care: a conceptual and empirical overview. Med Care. 1981;19(12):4–27. http://dx.doi.org/10.1097/00005650-198112001-00004 [PubMed] [Google Scholar]
- 16. Wilson K, Rosenberg MW. Accessibility and the Canadian health care system: squaring perceptions and realities. Health Policy. 2004;67(2):137–48. http://dx.doi.org/10.1016/S0168-8510(03)00101-5. Medline:14720632 [DOI] [PubMed] [Google Scholar]
- 17. IJzelenberg W, Burdorf A. Impact of musculoskeletal co-morbidity of neck and upper extremities on healthcare utilisation and sickness absence for low back pain. Occup Environ Med. 2004;61(10):806–10. http://dx.doi.org/10.1136/oem.2003.011635. Medline:15377765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thomas JW, Penchansky R. Relating satisfaction with access to utilization of services. Med Care. 1984;22(6):553–68. http://dx.doi.org/10.1097/00005650-198406000-00006. Medline:6738145 [DOI] [PubMed] [Google Scholar]
- 19. Mielenz TJ, Carey TS, Dyrek DA, et al. Physical therapy utilization by patients with acute low back pain. Phys Ther. 1997;77(10):1040–51. Medline:9327819 [DOI] [PubMed] [Google Scholar]
- 20. Bath B, Pahwa P. A physiotherapy triage assessment service for people with low back disorders: evaluation of short-term outcomes. Patient Relat Outcome Meas. 2012;3:9–19. http://dx.doi.org/10.2147/PROM.S31657. Medline:22915980 [DOI] [PMC free article] [PubMed] [Google Scholar]