Abstract
Introduction
We evaluated a synergistic epidemic (syndemic) of substance use, mental illness, and familial conflict non-negotiation among HIV-positive injection drug users (IDU).
Method
Baseline BEACON study data was utilized. Latent class analyses identified syndemic classes. These classes were regressed on sex, viral suppression, and acute care non-utilization. Females were hypothesized to have higher syndemic burden, and worse health outcomes than males.
Results
Nine percent of participants had high substance use/mental illness prevalence (Class 4); 23% had moderate levels of all factors (Class 3); 25% had high mental illness (Class 2); 43% had moderate substance use/mental illness (Class 1; N=331). Compared to Classes 1–3, Class 4 was mostly female (p<.05), less likely to achieve viral suppression, and more likely to utilize acute care (p<.05).
Discussion
Interventions should target African-American IDU females to improve their risk of negative medical outcomes. Findings support comprehensive syndemic approaches to HIV interventions, rather than singular treatment methods.
Keywords: HIV, injection drug use, viral suppression, health disparities, Syndemic Theory, African-Americans, health services research
INTRODUCTION
Thirty-five years into the HIV pandemic, advancements have been made in the availability of antiretroviral therapy (ART), reduction of AIDS-related mortality, and awareness of HIV risk among at-risk groups such as persons who inject drugs (PWID). During the same period, the public’s perceptions and demographic characteristics of people living with HIV/AIDS (PLHIV) have also changed (Towner, 2008; Centers for Disease Control and Prevention [CDC], 2012). Because HIV is no longer a death sentence, many PLHIV are aging well into older adulthood, albeit with more co-morbidities than their non-PLHIV counterparts (CDC, 2012; Havlik et al., 2011). Common HIV co-morbidities, irrespective of age, include viral Hepatitis and tuberculosis, which may complicate the treatment of HIV with ART, due to issues such as multi-drug resistance (CDC, 2012). Regardless of biologic or behavioral origin, factors which co-present with HIV, and interact in etiology and prognosis comprise a syndemic (Kaaya et al., 2013; Singer, 1996; Singer & Clair, 2003; Singer, 2009).
Syndemic Theory and HIV-related disparities
Syndemic Theory refers to two or more co-morbid conditions, which interact synergistically, and collectively increase disease burden in a given population (Singer, 1996; Singer & Clair, 2003). These health-related problems cluster together either by person, place, or time, overlap, and therefore must be controlled and addressed collectively (Milstein, 2001; Singer & Clair, 2003). Singer (1996) first proposed the ‘SAVA’ syndemic, referring to concurrent and mutually reinforcing substance abuse, violence, and HIV infection among low-income and racial/ethnic minorities. Ostrach and Singer (2012) posit that women are particularly vulnerable to syndemic health threats, due to socio-political environmental factors and multiple pathways of risk. In support of this view, Illangasekare et al (2013) found that compared to women who with no SAVA Syndemic factors, women who had experienced all three factors were significantly more likely to report depressive symptoms. Meyer et al (2011) reviewed 45 studies related to the SAVA Syndemic, and found that the SAVA Syndemic was associated with increased engagement in HIV-risk behaviors, mental illness, and lower rates of HIV medical adherence.
Similarly, Marcus (2014) posited that physical health, abuse, mental illness, loss, instability, and substance use are a syndemic worsening the health of homeless women, whom are predominantly of color. Freudenberg et al (2006) also posited a syndemic, consisting of tuberculosis, HIV infection, and homicide, and affecting predominantly men and women of color over the span of decades in New York City. Related syndemics have also been identified in Hispanic/Latino men and women. Mendenhall (2013) posited the presence of a syndemic among Mexican immigrant women, comprised of violence, immigration-related stress, depression, diabetes, and abuse. Gonzalez-Guarda et al (2010) demonstrated that Hispanic/Latino-American men are disproportionately affected by substance abuse, perpetration of intimate partner violence, and HIV risk. A follow up study found a similar syndemic present in Hispanic/Latina-American women, with the additional burden of depressive symptoms, intimate partner violence victimization, and socioeconomic disadvantage (Gonzalez-Guarda et al., 2011). Horner and Nassiri (2013) posit another syndemic may be present among Hispanic/Latinos, comprised of neighborhood effects, malnutrition, and HIV/AIDS risk.
Several commonalities exist among the various HIV-related syndemics. First, nearly all of the syndemics that have been investigated posit that substance use and violence predict increased HIV risk, and primarily occur in low-income and racial/ethnic minority populations (Senn et al., 2010). Next, among women and men who have sex with men especially, mental illness is a common syndemic factor (Meyer et al., 2011). Moreover, the majority of syndemic models that have been investigated conceptualize women as having greater risk of factors precipitating HIV infection than men – including higher prevalence of intimate partner violence victimization, mental illnesses, and socioeconomic disadvantange. However, very few studies have focused on tertiary prevention of HIV-related burden, in lieu of HIV-related risk and primary HIV prevention. To our knowledge, however, no syndemic models have been theorized and tested among a disadvantaged, predominantly African-American PWID PLHIV population.
A new framework – The SUMIC Syndemic and African-American PLHIV
Disparities in HIV-related outcomes due to race and sex are well documented, such that African-Americans and women bear the largest burden of HIV and negative HIV medical outcomes (CDC, 2012). Syndemic Theory helps to describe those most vulnerable to these disparities. The ‘SUMIC’ Syndemic (i.e. Substance Use, Mental Illness, and Familial Conflict non-negotiation), places African-Americans, and particularly African-American women, at high risk of death and/or disability related to HIV/AIDS in the United States. First, persons who inject drugs are at increased risk of HIV infection compared to non-users, as injection drug use is a more efficient route of HIV transmission than unprotected sex (CDC, 2012).
Mental illness often co-occurs with substance use, both of which may predict increased risk of negative HIV outcomes (Kaaya et al., 2013; Senn & Carey, 2008; Wyatt, 2002; Zierler & Krieger, 1997). Consequently, many substance users report having been diagnosed and treated for depression, schizophrenia, manic depressive disorder, and other serious mental illness (Senn & Carey, 2008; Latkin et al., 2002; Johnson et al., 2008). Finally, familial conflict non-negotiation may be common among those living with HIV and syndemic factors such as substance use and mental illness. Familial conflict refers to any overt disagreement between family members related by any means, which may be acute or chronic, and may be directly or indirectly related to the HIV-infected individual and their care. (Semple, 1992; Rolland, 1994).
Familial conflict may be particularly problematic for PLHIV who benefit from open communication with relatives who are often their caregivers. HIV diagnosis represents a chronic stressor, which may then trigger substance use, mental illness, and/or familial conflict (Semple et al., 1997; Zea et al., 2005; Li et al., 2012; Romero-Diaz et al., 2005). If left unresolved, or non-negotiated, familial conflict may have implications for reduced adherence to medical regimens, and use of health services (Rolland, 1994). However, few studies have examined the construct of familial conflict non-negotiation to inform tertiary prevention of HIV health complications (Minze et al., 2010; Sanders-Phillips, 2002; Jones, Beach, Forehand, & Foster, 2003).
Purpose
The dearth of theoretically-informed, tertiary HIV prevention programs geared towards African-Americans is a gap in the literature (Johnson et al., 2008; Gielen et al., 2005; Tobin et al., 2011; McDaid & Hart, 2010). To date, only three studies have applied Syndemic Theory to assess the effects of syndemic factors on HIV medical outcomes (Sullivan et al., 2015; Blashill et al., 2014; Mizuno et al., 2014). Blashill et al (2014) found that syndemic effects of factors including childhood abuse, current violence, and alcohol or substance abuse were associated with lower ART adherence. Additionally, both Mizuno et al (2014) and Sullivan et al (2015) found that persons with more syndemic problems were less likely to be virally suppressed than those with less syndemic problems. However, assessment of Syndemic Theory in a sample of all African-American HIV-positive persons with a history of substance use has not been conducted to our knowledge. Also, unlike these studies, the present analyses utilized latent class analyses, which has been applied in several previous investigations of Syndemic Theory (Bastard et al., 2011; Ahn et al., 2008; Collins & Lanza, 2010). Therefore, the purpose of this study was to examine the presence and correlates of a potential latent syndemic in a cohort of African-American PLHIV. Specifically, study aims were to: (a) assess active substance use, mental illness, and familial conflict non-negotiation as a potential latent syndemic; and (b) examine syndemic patterns as a function of HIV medical outcomes and sex.
Previous research suggests that, compared to African-American men, African-American women have higher rates of mental illness, and lower rates of access to HIV care (Buseh & Stevens, 2008; Gullette et al., 2010). In regards to our second study aim, we hypothesized that: 1) women comprise the individuals with the highest prevalence of the proposed SUMIC Syndemic; and 2) individuals with higher syndemic burden would have poorer HIV medical outcomes than individuals with lower syndemic burden. The proposed syndemic and study were unique in examining tertiary prevention of HIV medical outcomes, rather than primary prevention of HIV infection among African-Americans, to improve HIV health outcomes.
METHODS
Procedure
Data were from the baseline survey of the Being Active and Connected (BEACON) study, which examined psychosocial factors associated with health outcomes and well-being among disadvantaged PLHIV. Study participants all resided in Baltimore City, and were individuals who were living with HIV, and also had a history of injection drug use. Inclusion criteria were: (a) age of 18 years or older; (b) documented HIV seropositive status; (c) current or former injection drug use; (d) current use of ART regimen defined as use in the prior 30 days; and (e) willingness to invite a supportive partner to the study. All participants completed baseline and were invited to complete follow-up assessments. Serum viral load, CD4 count data, and toxicology tests were conducted at baseline and 6-month visits for all participants. All other data were self-report measures. Participants were recruited via street outreach, community sampling, and targeted strategies. The Johns Hopkins Bloomberg School of Public Health Institutional Review Board approved the study.
Measures
Dependent variable
SUMIC Syndemic latent class membership was the outcome of interest. Latent class analyses (LCA) were conducted to identify unique patterns of behavioral risk. Therefore, the SUMIC Syndemic latent classes were participants’ most likely membership classes, based on posterior probability of self-reporting of items referring to active substance use, mental illness diagnoses, and familial conflict non-negotiation (Ahn et al., 2008; Collins & Lanza, 2010). Active substance use was made up of six items referring to illicit drug use, coded as reported use of opiates, marijuana, heroin, cocaine or crack, hallucinogens, and/or non-prescribed prescription drugs use in the past month. Each item was binary (coded 0 = no use and 1 = use in past 30 days). Mental illness was made up of five items, coded as reporting having ever been diagnosed by a doctor with depression, bipolar disorder, anxiety or post-traumatic stress disorder (PTSD), schizophrenia, and/or any other psychiatric condition. Each item was binary (coded 0 = not diagnosed and 1 = ever diagnosed). Familial conflict non-negotiation was made up of three items, reporting whether current family members rarely discuss problems, problem-solve together, and/or show caring for one another. Each item was binary, where 0 = no conflict, and 1 = frequent conflict. Familial conflict non-negotiation questions were based on the Conflict Tactics Scale, to assesses intra-family aggression and conflict resolution (Straus, 1979).
Independent variables
HIV medical outcomes were defined as level of acute care non-utilization and HIV viral suppression. Acute care non-utilization was measured via a cumulative score of access to health care services and level of engagement in HIV medical services. This definition is based on The HIV Cost and Service Utilization Study (HCSUS), which defines optimal service utilization as prompt engagement in HIV care after diagnosis, minimization of acute care, and successful ART adherence (Fremont et al., 2007). All participants in this study had access to HIV primary care and ART; therefore non-utilization of acute care and viral suppression were outcomes of interest.
Respondents reported numeric responses to the following: “In the past 6 months, how many times have you gone to an emergency room (ER) for your health care?”, and “In the past 6 months, how many times were you admitted to a hospital, that means that you stayed there overnight?” Responses were summed and dichotomized at the median, where 0 = 1 or more ER visits and/or overnight hospitalizations in the last 6 months and 1 = 0 ER visits or overnight hospitalizations in the last 6 months (MacCallum et al., 2002). In the present study, participants were nearly all insured and enrolled in care, and therefore should have had less reason to access acute care services. Therefore, while informed by the HCSUS study, the outcome of interest was non-utilization of acute care services, as opposed to other types of healthcare utilization.
HIV viral suppression was defined as a viral load of 40 copies per milliliter (mL) or less, as measured by the Roche Cobas Amplicor viral load assay (Schumacher et al., 2007). A dichotomous variable of viral suppression was constructed, where 0 = detectable viral load (greater than 40 copies/mL) and 1 = undetectable viral load (UVL), or viral suppression (less than 40 copies/mL). Finally, sex was a binary variable included in survey questionnaires, coded as 1= Males, and 2 = Females. Viral suppression is an accepted biomarker proxy of adherence, and was assessed in a population of drug-using African-American PLHIV, who traditionally have lower rates of both adherence and viral suppression than other racial groups (CDC, 2012).
Data analyses
First, univariate statistics were calculated among the entire sample of participants (N=383). Relevant summary statistics were generated for: (a) demographic variables: sex, age, race, educational attainment, and monthly income; (b) substance use, mental illness, and familial conflict non-negotiation items; and (c) HIV medical outcomes (viral suppression and acute care non-utilization). Next, factor analyses were conducted to assess the factor structure and internal reliability of the items for each SUMIC Syndemic factor. A latent one-factor structure of the 6 binary active substance use items yielded acceptable fit (Chi-square [χ2] = 11.37; Degrees of freedom [df] = 9; Root Mean Square Error of Approximation [RMSEA] = 0.03; Comparative Fit Index [CFI] = 1.00; Rasch, 1980). A latent one-factor structure of the 5 binary mental illness items yielded acceptable fit (χ2 = 2.41; df = 5; RMSEA = 0.00; CFI = 1.00; Rasch, 1980).
Factor analyses were conducted to account for a latent one-factor structure of the 3 binary familial conflict non-negotiation items, which yielded acceptable fit (χ2 = 0.00; df = 0; RMSEA = 0.00; CFI = 1.00; Rasch, 1980). Third, LCA was used as a data reduction technique by which to categorize individuals into their most likely class membership along the spectrum of the SUMIC Syndemic (non-observable latent variable, based on the latent conditions of active substance use, mental illness, and familial conflict non-negotiation; Bastard et al., 2011; Ahn et al., 2008; Collins & Lanza, 2010). Fourth, the syndemic classes were regressed on the three relevant correlates: sex, viral suppression (UVL), and acute care non-utilization (ACN).
Comparisons were made about class membership as a function of sex and HIV medical outcomes (i.e. UVL and ACN). Odds ratios were analyzed as an acceptable approximation of relative risk, given that the LCA outcome of interest, SUMIC Syndemic Class 4 was rare (less than 10%; McNutt et al., 2003). LCA were run with solutions ranging from two classes to six classes with African-American Participants only (N=351). Analyses were conducted on complete cases only, due to acceptable missingness (less than 10%; Bennett, 2001). Both theory and fit statistics were utilized to select the best model for the data, including Akaike’s Information Criteria (AIC; Akaike, 1973). Descriptive analyses were run among in Stata Version 11.2 SE (StataCorp, 2009), and all latent factor analyses and LCA were run using MPlus Version 7.0 (Muthén & Muthén, 2011).
RESULTS
Descriptive statistics
Table 1 reports demographic characteristics of all participants (N=383). Participants were predominantly African-American (91.6%), male (61.4%), and earned a monthly income between $500 to $999 (57.2%). Most participants had attended high school and/or had earned a high school diploma or GED (39.2% and 37.9%, respectively), and also had a history of ever being in jail or prison (84.1%). Half of the participants achieved acute care non-utilization (50.9%). Two-thirds achieved viral suppression (65.8%). Mean age was 48.2 years. Among African-American participants cocaine/crack (33.7%) and heroin (20.8%) were the substances most frequently used (N=351; Table 2). Depression (59.5%) and bipolar disorder (33.1%) were the most common mental illness diagnoses. The most frequent familial conflict non-negotiations were families rarely or never talking about problems (29.9%), and rarely or never problem-solving (28.2%). Present LCA yielded a four-class solution, with low AIC, Bayesian Information Criteria, and high Entropy, along with theoretical meaningfulness (Akaike, 1973; Table 5).
Table 1.
Demographic characteristics of all participants (N=383)
| Demographic Characteristic | Total N(%) or Mean (SD) |
|
|---|---|---|
| Race | ||
| African-American/Black | 351 | (91.6) |
| White | 27 | (7.0) |
| Other | 5 | (1.4) |
| Education | ||
| 8th grade or less | 26 | (6.8) |
| Some high school | 150 | (39.2) |
| High school diploma/GED | 145 | (37.9) |
| Some college/tech school | 45 | (11.7) |
| College degree | 10 | (2.6) |
| Any graduate training | 7 | (1.8) |
| Monthly income | ||
| $0–$499 | 87 | (22.7) |
| $500–$999 | 219 | (57.2) |
| $1000+ | 77 | (20.1) |
| Relationship status | ||
| Married | 36 | (9.4) |
| In a committed relationship | 97 | (25.3) |
| Separated | 28 | (7.3) |
| Divorced | 33 | (8.6) |
| Widowed | 15 | (3.9) |
| Single | 174 | (45.5) |
| Usual healthcare provider | ||
| Medical clinic at a hospital | 270 | (70.5) |
| Med clinic not at a hospital | 108 | (28.2) |
| Hospital emergency room | 1 | (0.3) |
| Some other type of place | 4 | (1.0) |
| Physical functioning | ||
| Low | 135 | (35.2) |
| Medium | 116 | (30.3) |
| High | 132 | (34.5) |
| Acute care non-utilization | ||
| Suboptimal | 188 | (49.1) |
| Optimal | 195 | (50.9) |
| Viral suppression | ||
| Detectable viral load | 131 | (34.2) |
| Undetectable viral load | 252 | (65.8) |
| Ever been in jail/prison | ||
| Yes | 322 | (84.1) |
| No | 61 | (15.9) |
| Sex | ||
| Males | 235 | (61.4) |
| Females | 148 | (38.6) |
| Age (years) | 48.2 | (6.3) |
Table 2.
SUMIC Syndemic frequencies among African-Americans (N=351)
| Syndemic Factor and Indicators | Total (N=351) | |
|---|---|---|
| Active substance use | ||
| Opiates in last 30 days | 52 | (14.8) |
| Marijuana in last 30 days | 56 | (16.0) |
| Heroin in last 30 days | 73 | (20.8) |
| Cocaine or crack in last 30 days | 117 | (33.3) |
| Hallucinogens in last 30 days | 3 | (0.9) |
| Prescription drugs in last 30 days | 17 | (4.8) |
| Most frequently co-occuring substances used | ||
| Heroin/cocaine in last 30 days | 63 | (17.9) |
| Marijuana/cocaine in last 30 days | 39 | (11.1) |
| Marijuana/heroin in last 30 days | 25 | (7.1) |
| Mental illness | ||
| Diagnosed with depression | 209 | (59.5) |
| Diagnosed with bipolar disorder | 116 | (33.1) |
| Diagnosed with anxiety or PTSD | 89 | (25.4) |
| Diagnosed with schizophrenia | 34 | (9.7) |
| Diagnosed with other psychiatric illness | 18 | (5.2) |
| Most frequently co-occuring mental illnesses | ||
| Diagnosed with depression/bipolar disorder | 109 | (31.1) |
| Diagnosed with depression/anxiety or PTSD | 81 | (23.1) |
| Familial conflict non-negotiation | ||
| Family rarely/never talks about problems | 105 | (29.9) |
| Family rarely/never problem solves together | 99 | (28.2) |
| Family rarely/never shows caring for each other | 29 | (8.3) |
| Most frequently co-occuring familial conflict non-resolution | ||
| Family rarely/never talk/problems solves together | 80 | (22.8) |
Table 5.
Latent class analysis fit statistics
| Number of Latent Classes | Akaike Information Criteria | Bayesian Information Criteria | Entropy |
|---|---|---|---|
| 2 | 4096.8 | 4220.4 | 0.75 |
| 3 | 3951.2 | 4144.3 | 0.83 |
| 4 | 3858.8 | 4121.4 | 0.85 |
| 5 | 3810.5 | 4142.5 | 0.84 |
| 6 | 3797.9 | 4199.4 | 0.90 |
Class 1: Moderate Substance use/Mental illness
Class 1 (Moderate SU/MI) individuals had moderate prevalence of substance use and mental illness (43% of the sample; Table 3). Individuals in this class were the only to report hallucinogens use (2.1%), and moderate rates of cocaine use (33.4%), and heroin (20.6%). Class 1 individuals were least likely of all class members to report a mental illness diagnosis, though nearly 30% had a depression diagnosis (p<.01). These individuals were least likely to endorse experiencing familial conflict non-negotiation, such that only 6.6% endorsed rarely or never talking about problems with their families (p<.01). Thus, Class 1 (Moderate SU/MI) has the lowest burden of the SUMIC Syndemic, and were the sample majority. Similarly to Table 3, Figure 1 reports the SUMIC Syndemic classes, where the Y-axis is the probability of reporting ‘yes’ for each syndemic item.
Table 3.
Probability of SUMIC factors by latent class among African-American Indexes (N=351)
| C1: (43%) Moderate SU/MI |
C2: (25%) High MI |
C3: (23%) Moderate SU/MI/C |
C4: (9%) High SU/MI |
|
|---|---|---|---|---|
| Active substance use | ||||
| Opiates in last 30 days | 13.8*** | 08.1ǂ | 17.3*** | 33.1*** |
| Marijuana in last 30 days | 14.2*** | 03.0 | 21.8*** | 47.9*** |
| Heroin in last 30 days | 20.6*** | 01.9 | 23.6*** | 71.3*** |
| Cocaine or crack in last 30 days | 33.4*** | 04.2 | 41.4*** | 100 |
| Hallucinogens in last 30 days | 02.1ǂ | – | – | – |
| Prescription drugs in last 30 days | 04.0* | – | 04.0ǂ | 25.5** |
| Mental illness | ||||
| Diagnosed with depression | 27.0** | 92.5*** | 64.8*** | 95.2*** |
| Diagnosed with bipolar disorder | – | 68.6*** | 33.5*** | 75.6*** |
| Diagnosed with anxiety or PTSD | 03.6 | 43.0*** | 29.4*** | 61.2*** |
| Diagnosed with schizophrenia | – | 13.5** | 09.6** | 42.6*** |
| Diagnosed with other psychiatric illness | 01.9 | 07.6* | 07.4* | 06.7 |
| Familial conflict non-negotiation | ||||
| Family rarely/never talks about problems | 06.6** | 12.4* | 93.9*** | 25.4* |
| Family rarely/never problem solves together | 04.3ǂ | 05.9 | 95.9*** | 31.2** |
| Family rarely/never shows caring | – | 03.0 | 28.6*** | 09.7 |
marginally significant p<.10,
p<.05,
p<.01,
p<.001
Figure 1.
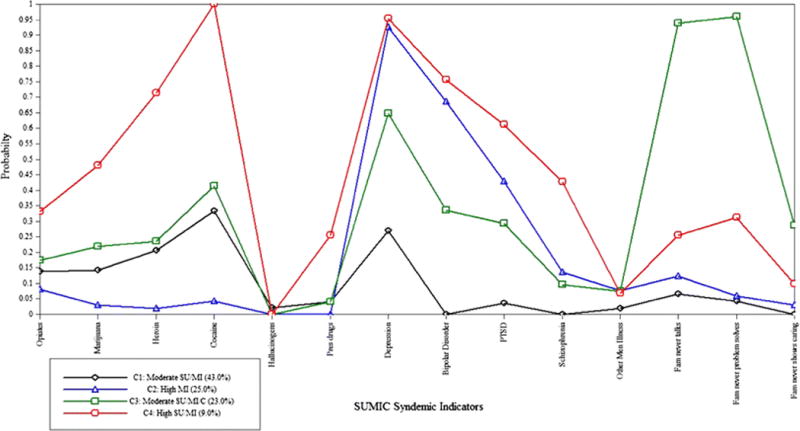
Four-class latent class analysis of SUMIC Syndemic factors among African-American participants (N=351)
Class 2: High Mental illness
Class 2 (High MI) individuals had very high prevalence of mental illness (25% of sample population; Table 3). These individuals reported the second highest rates of depression diagnoses (92.5%; p<.001) and the second-highest rates of anxiety/PTSD diagnoses (43%; p<.01). Additionally, over two-thirds of Class 2 individuals had been diagnosed with bipolar disorder (68.6%; p<.001). The most commonly used substance in this class was opiates (8.1%). They also had the second lowest rates of familial conflict non-negotiation (12.4%; p<.05). This class had the lowest prevalence of active substance use and familial conflict non-negotiation; thus Class 2 (High MI) had lower SUMIC Syndemic burden than both Classes 3 and 4 (Table 3 and Figure 1).
Class 3: Moderate Substance use and Mental illness/High Familial conflict non-negotiation
Class 3 individuals had moderate to high prevalence of all SUMIC Syndemic factors (23% of sample; Table 3). These individuals reported the second-highest rates of active cocaine use (41.4%), marijuana use (21.8%), and heroin use (23.6%) out of all 4 classes. Nearly two-thirds of Class 3 (Moderate SU/MI/C) individuals had a depression diagnosis (p<.001), and one-third had a bipolar disorder diagnosis (p<.001). These individuals reported the highest rates of familial conflict non-negotiation, where over 93% of individuals reported that their families rarely or never talk about problems and rarely or never problem solves together (93.9% and 95.9%, respectively; p<.001; Figure 1).
Class 4: High Substance use/High Mental illness
Class 4 (High SU/MI) individuals had the highest substance use and mental illness prevalence (9% of the sample; Table 3). These individuals were most likely to report active cocaine use (100%), marijuana use (47.9%), and heroin use (71.3%) out of all participants. One-quarter of Class 4 individuals reported active prescription drug use, as compared to 4% in the other classes (p<.01). These individuals also had the highest rates of all mental illness diagnoses including depression (95.2%), bipolar disorder (75.6%), and anxiety/PTSD (61.2%). Class 4 (High SU/MI) individuals had the highest rates of active substance use and mental illness, and the second-highest rates of familial conflict non-negotiation; thus they comprise the class with the highest SUMIC Syndemic health burden (Figure 1).
Latent class logistic regression results
Table 4 reports latent class regression odds ratios, where SUMIC Syndemic class membership was regressed on viral suppression (UVL), acute care non-utilization (ACN), and sex among African-American participants (N=351). Compared to the class with the highest SUMIC Syndemic burden (Class 4), individuals with the lowest SUMIC Syndemic burden (Class 1) had 80% fewer odds of being female (Odds Ratio [OR] = 0.21; 95% Confidence Interval [95% CI] = 0.01, 0.61). Class 1 (Moderate SU/MI) individuals were 5 times as likely as Class 4 individuals to have not used acute care services in the past 6 months (OR = 5.03; 95% CI = 1.38, 18.39). Females were more likely to be in Class 4 than males, and less likely to be in Class 1. Therefore, females were more likely to have highest SUMIC Syndemic burden, and to have utilized acute care services.
Table 4.
Odds ratios of SUMIC latent class regression among African-American participants (N=351)a
| Class 1: Moderate SU/MI | Class 2: High MI | Class 3: Moderate SUMIC | ||||
|---|---|---|---|---|---|---|
| Variable | ORb | CIc | OR | CI | OR | CI |
|
Sex (Ref: Males) |
0.21** | (0.01, 0.61) | 0.46 | (0.12, 1.77) | 0.21** | (0.01, 0.67) |
|
Viral suppression (Ref:>40 copies/mL) |
2.26 | (0.73, 6.99) | 4.60** | (1.48, 14.29) | 4.68* | (1.26, 17.36) |
|
Acute care non-utilization (Ref: 1 or more ED admissions/hospitalizations in the past 6 months) |
5.03* | (1.38, 18.39) | 2.40 | (0.70, 8.30) | 6.56* | (1.80, 23.78) |
p<.05,
p<.01,
p<.001
Reference group: Class 4 (High SU/MI)
OR = Unadjusted Odds Ratio
CI = 95% Confidence Interval
Compared to Class 4, individuals with high mental illness only (Class 2) had 4.6 times the odds of UVL (95% CI = 1.48, 14.29). Individuals in Classes 1 (Moderate SU/MI) and 4 were more likely to have detectable viral load than to have achieved UVL. In contrast, individuals in Classes 2 and 3 were mostly virally suppressed. Individuals in Classes 1 and 3 (Moderate SU/MI/C) were more likely to achieved acute care non-utilization, which is preferable among a sample of insured individuals with primary care access. Compared to Class 4, individuals with moderate rates of all SUMIC Syndemic factors (Class 3) had between 4 to 6 times greater odds of viral suppresion and non-utilization of acute care. This class was also significantly more likely to be male.
Hypothesis testing
Study results suggest that females were less likely to achieve viral suppression and more likely to utilize acute care than males. As an exemplar, Class 2 (High MI) and 4 (High SU/MI) individuals were more likely to use acute care services in the prior 6 months, as compared to the other classes. Post-hoc analyses indicated both of these classes were predominantly female – 51% of Class 2 were female, and 69% of Class 4 (High SU/MI). Moreover, Class 4 was comprised of individuals with the highest syndemic burden. Therefore, for our first study hypothesis was supported. Also, we hypothesized that individuals with higher syndemic burden would have poorer HIV medical outcomes than individuals with lower syndemic burden. Individuals in Class 4 were less likely to have achieved viral suppression and acute care non-utilization than all other classes – thereby supporting our second hypothesis. While not statistically significant, post-hoc analyses also revealed that African-American females were less likely than African American males to achieve viral suppression (67.1% vs. 65.9%, respectively) and more likely to utilize acute care services (53.9% vs. 48.5%, respectively).
DISCUSSION
Our study results suggest that, among disadvantaged African-American PLHIV, active substance use, mental illness, and familial conflict non-negotiation may be contributing to poor HIV medical outcomes, particularly among African-American females. This is logical, given that extant research suggests that these factors are both common predecessors of HIV infection and frequent outcomes after HIV diagnosis (Kaaya et al., 2013; Senn & Carey, 2008; Wyatt, 2002; Zierler & Krieger, 1997; Johnson et al., 2008; Zea et al., 2005; Li et al., 2012). Furthermore, our results suggest that these factors lend themselves well to application of Syndemic Theory. Our latent class analyses (LCA) reveal that the ‘SUMIC’ Syndemic (Substance Use, Mental Illness, and Familial Conflict non-negotiation) approach yielded four distinct classes of behavioral risk patterns within the study population (Table 3 and Figure 1), each with differential distribution of the aforementioned factors.
Several previous investigations of syndemic classes have utilized LCA as a meaningful way to classify subtypes of individuals based on their unique behavioral patterns of HIV risk, to inform treatment interventions (Keiser et al., 2012; Noor et al., 2014; Brinkley-Rubinstein & Craven, 2014; Halkitis et al., 2012; Konda et al., 2011). In the present LCA model, the largest syndemic class, Class 1, also had the lowest syndemic burden of moderate mental illness (43%; N=351). The majority of PLHIV in this study, therefore, had low rates of mental illness and were older in age, both of which correlate with viral suppression (Nicholas et al., 2014; CDC, 2012).
As mentioned, study results provided support for both study hypotheses; first, that females report poorer HIV medical outcomes, and second, that individuals with higher syndemic burden would report poorer HIV medical outcomes than individuals with less syndemic burden. Moreover, latent class regression analyses indicated that all three classes with lower syndemic burden had higher odds of both viral suppression and acute care non-utilization compared to Class 4 (High SU/MI; Table 3). These results suggest that interventions to improve HIV medical outcomes among African-American PLHIV should target African-American women, as they are more likely than men to suffer from concurrent and mutually reinforcing SUMIC Syndemic factors and low adherence (Towner, 2008; CDC, 2012; Prejean et al., 2011).
Classes 2 (High MI) and Class 3 (Moderate SU/MI/C) were individuals with moderate SUMIC Syndemic burden (N=351). Nearly 80% of individuals in both classes had achieved viral suppression; however, only 38% of Class 2 individuals, and 64% of Class 3 individuals achieved acute care non-utilization. Therefore, these syndemic factors do not have similar effects on viral suppression and acute services non-utilization. Also, higher prevalence of mental illness and substance use, regardless of familial conflict non-resolution level, is associated with increased acute services utilization.
While few studies have examined Syndemic Theory among African-American PLHIV, there are some similarities between our results and previous investigations. First, congruent with most previous syndemic models, the present sample was low-income racial minorities, with high rates of substance use and mental illness (Senn et al., 2010). Next, the only other studies to date which have investigated similar medical outcomes among PLHIV also found that higher syndemic burden was associated with lower ART adherence and viral suppression (Mizuno et al., 2014; Blashill et al., 2014; Sullivan et al., 2015). Our results suggest that Class 4 (High SU/MI) individuals, with the highest SUMIC Syndemic burden were mostly women (Table 4). Similarly, Illangasekare et al (2013) found that women with syndemic substance use, violence, and HIV-seropositivity had seven times the risk of depression as women with no syndemic factors, suggesting high disadvantage due to syndemic risk among women. The present study found that women fared worse than men in terms of prevalence of mental illness and SUMIC Syndemic burden, as well as odds of achieving viral suppression, and acute care non-utilization.
Interventions to improve HIV medical outcomes in this population should promote use of usual healthcare providers, which 70% of study participants reported having access to. In such a setting, providers could utilize standardized screening questions to systematically assess syndemic burden, and make appropriate referrals to linkage to care. Finally, the study results suggest that interventions to improved HIV medical outcomes among African-American PLHIV within the SUMIC Syndemic must address mental illness, as all 4 classes of Syndemic individuals reported at least moderate depression (range: 27% to 95.2%) and bipolar disorder (range: 33.5% to 75.6%), among other diagnoses.
This is congruent with extant literature, given that rates of depression among PLHIV are estimated as twice that of the general public (Kaaya et al., 2013). However, unlike previous models, the present study is the first to apply Syndemic Theory to tertiary HIV prevention outcomes among only African-American participants in a sample of persons who are HIV-positive, and all of whom have a history of injection drug use.
Limitations
There are several limitations to consider in this study. First, the median time since HIV diagnosis was ten years, and participants were nearly all African-American, middle-aged, current or former persons who inject drugs, with access to regular healthcare and ART. Therefore, these population characteristics limit the generalizability of our findings beyond other similar populations. Second, as reported in Table 4, several logistic regression odds ratios had large confidence intervals, suggesting that the sample size may have been insufficient to detect all statistically significant findings. Third, while the use of acute care non-utilization builds on the prior HCSUS study definition (Fremont et al., 2007), reasons for acute care non-utilization in the sample were unknown and therefore use may not be problematic if sicker individuals were utilizing these services more. Fourth, most of the data were self-report, which suggests underreporting may have been a factor. Additionally, data were cross-sectional, while study constructs such as adherence may change over time. Finally, there is controversy about the causal associations (temporality) of syndemic factors. However, from a treatment perspective, presence of SUMIC syndemic factors may hold more precedence than temporality.
Conclusions
Despite these limitations, this study is the first to theorize and test the SUMIC Syndemic among a cohort of African-American PLHIV, and only the third to apply Syndemic Theory to HIV medical outcomes (Blashill et al., 2014; Mizuno et al., 2014). This study builds upon previous research in Syndemic Theory (Milstein, 2001; Singer & Clair, 2003; Senn et al., 2010; Stall et al., 2003), and contributes a new framework for conceptualizing HIV disparities to promote tertiary HIV prevention. Moreover, results substantiate comprehensive treatment of syndemic factors among African-American PLHIV (Senn et al., 2010).
While the SUMIC Syndemic is non sex-specific, interventions must consider sex differences in outcomes such as viral suppression and acute care non-utilization, such that women may have unique contextual factors which reduce their likelihood of viral suppression and positive HIV-related medical outcomes. These factors may include less financial resources and more homelessness, lower perceived social support, and competing priorities that interfere with medical adherence, such as having an HIV-positive significant other for whom they provide care (Blank, 2014; Edwards, 2006; Knowlton et al., 2011). Therefore, future research should consider homelessness and syndemic factors in HIV medical outcomes among PWID PLHIV.
Results suggest that structural competence training with healthcare providers may increase their understanding of how syndemic factors impact patient outcomes, and may be exacerbated by structural factors such as institutional racism or drug use stigmatization (Metzl & Hansen, 2014). Also, structural HIV interventions should be evaluated. While the Affordable Care Act has increased insurance coverage of mental health and substance use disorder services, advocacy is needed for the prioritization of women’s set-aside federal research funding, which has been inconsistent since its creation in 1984 (Tracy & Martin, 2007). Finally, familial conflict non-negotiation was a common health threat experienced by the study population. Future interventions in this population should consider family ecosystems therapy and communication skills building to improve HIV medical outcomes (Mitrani et al., 2012).
These comprehensive approaches, coupled with sex-specific and culturally-appropriate interventions, may reduce stigmatization of substance use, barriers to HIV-related care, and mental illness treatments, to ultimately improve HIV health outcomes in this population.
Acknowledgments
This study was supported by grants from the National Institutes of Health (R01 DA019413 and R01 NR14050-01). This research was also supported by the Johns Hopkins Center for AIDS Research (1P30AI094189).
Footnotes
Conflicts of interest: None
References
- Ahn J, McCombs JS, Jung C, Croudace TJ, McDonnell D, Ascher-Svanum H, Edgell ET, Shi L. Classifying patients by antipsychotic adherence patterns using latent class analysis: characteristics of nonadherent groups in the California Medicaid (Medi-Cal) program. Value in Health. 2008;11(1):48–56. doi: 10.1111/j.1524-4733.2007.00214.x. [DOI] [PubMed] [Google Scholar]
- Akaike H. Second International Symposium on Information Theory. Budapest, Hungary: 1973. Information theory and an extension of the maximum likelihood principle. [Google Scholar]
- Bastard M, Koita FM, Laniece I, Taverne B, Desclaux A, Ecochard R, Sow PS, Delaporte E, Etard JF. Revisiting long-term adherence to HAART in Senegal using latent class analysis. Journal of Acquired Immune Deficiency Syndrome. 2011;57(1):55–61. doi: 10.1097/QAI.0b013e318211b43b. [DOI] [PubMed] [Google Scholar]
- Bennett DA. How can I deal with missing data in my study? Australian and New Zealand Journal of Public Health. 2001;25:464–69. [PubMed] [Google Scholar]
- Blank MB. Homelessness, Mental Illness, Substance Abuse, and HIV: An Insidious Syndemic. HIV/AIDS Research & Treatment Open Journal. 2014;1(1):e001–4. [Google Scholar]
- Blashill AJ, Bedoya CA, Mayer KH, O’Cleirigh C, Pinkston MM, Remmert JE, Mimiaga MJ, Safren SA. Psychosocial Syndemics are Additively Associated with Worse ART Adherence in HIV-Infected Individuals. AIDS & Behavior. 2014;19(6):981–6. doi: 10.1007/s10461-014-0925-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinkley-Rubinstein L, Craven K. A Latent Class Analysis of Stigmatizing Attitudes and Knowledge of HIV Risk among Youth in South Africa. PLOS ONE. 2014;9(2):e89915. doi: 10.1371/journal.pone.0089915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buseh AG, Stevens PE. Constrained But Not Determined by Stigma: Resistance by African-American Women Living with HIV. Women & Health. 2008;44(3):1–18. doi: 10.1300/J013v44n03_01. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] HIV in the United States: The Stages of Care, 2012. 2012 Retrieved September 17, 2014, from http://www.cdc.gov/nchhstp/newsroom/docs/2012/Stages-of-CareFactSheet-508.pdf.
- Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. New York, NY: Wiley Publishing; 2010. [Google Scholar]
- Fremont A, Young A, Chinman M, Pantoja P, Morton SC, Koegel P, Sullivan JG, Kanouse DE. Differences in HIV Care Between Patients with and Without Severe Mental Illness. Psychiatric Services. 2007;58(5):681–8. doi: 10.1176/ps.2007.58.5.681. [DOI] [PubMed] [Google Scholar]
- Freudenberg N, Fahs M, Galea S, Greenberg A. The impact of New York City’s 1975 fiscal crisis on the tuberculosis, HIV, and homicide syndemic. American Journal of Public Health. 2006;96(3):424–34. doi: 10.2105/AJPH.2005.063511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen AC, McDonnell KA, O’Campo PJ, Burke JG. Suicide risk and mental health indicators: Do they differ by abuse and HIV status? Women’s Health Issues. 2005;15:89–95. doi: 10.1016/j.whi.2004.12.004. [DOI] [PubMed] [Google Scholar]
- González-Guarda RM, McCabe BE, Florom-Smith A, Cianelli R, Peragallo N. Substance Abuse, Violence, HIV, and Depression An Underlying Syndemic Factor Among Latinas. Nursing Research. 2011;60(3):182–9. doi: 10.1097/NNR.0b013e318216d5f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Guarda RM, Ortega J, Vasquez EP, De Santis J. La mancha negra: Substance abuse, violence, and sexual risks among Hispanic males. Western Journal of Nursing Research. 2010;32(1):128–48. doi: 10.1177/0193945909343594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gullette DL, Wright PB, Booth BM, Stewart KE. Stages of Change, Decisional Balance, and Self-Efficacy in Condom Use Among Rural African-American Stimulant Users. Journal of Associated Nurses AIDS Care. 2010;20(6):428–41. doi: 10.1016/j.jana.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Moeller RW, Siconolfi DE, Storholm ED, Solomon TM, Bub KL. Measurement model exploring a syndemic in emerging adult gay and bisexual men. AIDS & Behavior. 2013;17(2):662–73. doi: 10.1007/s10461-012-0273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Kupprat SA, Hampton MB, Perez-Figueroa R, Kingdon M, Eddy JA, Ompad DC. Evidence for a Syndemic in Aging HIV-positive Gay, Bisexual, and Other MSM: Implications for a Holistic Approach to Prevention and Healthcare. Natural Resource Modeling. 2012;36(2):1–21. doi: 10.1111/napa.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havlik RJ, Brennan M, Karpiak SE. Comorbidities and depression in older adults with HIV. Sexual Health. 2011;8:551–9. doi: 10.1071/SH11017. [DOI] [PubMed] [Google Scholar]
- Horner P, Nassiri R. Social Cultural Stressors in Dominican Republic HIV/AIDS Prevention and Treatment. Journal of AIDS & Clinical Research. 2013;4(242):1–6. [Google Scholar]
- Illangasekare S, Burke J, Chander G, Gielen A. The syndemic effects of intimate partner violence, HIV/AIDS, and substance abuse on depression among low-income urban women. Journal of Urban Health. 2013;90(5):934–7. doi: 10.1007/s11524-013-9797-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, Malow R, McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database of Systematic Reviews. 2008;3:CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- Jones DJ, Beach SR, Forehand R, Foster SE. Self-Reported Health in HIV-Positive African-American Women: The Role of Family Stress and Depressive Symptoms. Journal of Behavioral Medicine. 2003;26(6):577–99. doi: 10.1023/a:1026205919801. [DOI] [PubMed] [Google Scholar]
- Kaaya S, Eustache E, Lapidos-Salaiz I, Musisi S, Psaros C, Wissow L. Grand Challenges: Improving HIV Treatment Outcomes by Integrating Interventions for Co-Morbid Mental Illness. PLOS Medicine. 2013;5(10):e1001447. doi: 10.1371/journal.pmed.1001447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keiser O, Spycher B, Rauch A, Calmy A, Cavassini M, Glass TR, Nicca D, Ledergerber B, Egger M, Swiss HIV Cohort Study Outcomes of Antiretroviral Therapy in the Swiss HIV Cohort Study: Latent Class Analysis. AIDS & Behavior. 2012;16:245–55. doi: 10.1007/s10461-011-9971-5. [DOI] [PubMed] [Google Scholar]
- Konda KA, Celentano DD, Kegeles S, Coates TJ, Caceres CF, NIMH Collaborative HIV/STD Prevention Trial Group Latent Class Analysis of Sexual Risk Patterns Among Esquineros (Street Corner Men) a Group of Heterosexually Identified, Socially Marginalized Men in Urban Coastal Peru. AIDS & Behavior. 2011;15:862–8. doi: 10.1007/s10461-010-9772-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related behaviors among urban disadvantaged drug users. Social Science & Medicine. 2002;56:465–76. doi: 10.1016/s0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- Li L, Ji G, Ding Y, Tian J, Lee A. Perceived burden in adherence of antiretroviral treatment in rural China. AIDS Care. 2012;24(4):502–8. doi: 10.1080/09540121.2011.613912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the Practice of Dichotomization of Quantitative Variables. Psychological Methods. 2002;7(1):19–40. doi: 10.1037/1082-989x.7.1.19. [DOI] [PubMed] [Google Scholar]
- Marcus R. Women’s Discourse on the Homeless Experience: It’s About Love and Loss. 2014 Retrieved June 9, 2015 from http://digitalcommons.uconn.edu.
- McDaid LM, Hart G. Sexual risk behaviour for transmission of HIV in men who have sex with men: recent findings and potential interventions. Current Opinion in HIV & AIDS. 2010;5(4):311–15. doi: 10.1097/COH.0b013e32833a0b86. [DOI] [PubMed] [Google Scholar]
- McNutt L, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. American Journal of Epidemiology. 2003;157:940–3. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- Mendenhall E. Syndemic Suffering: Social Distress, Depression, and Diabetes among Mexican Immigrant Women. Walnut Creek, CA: Left Coast Press; 2013. [Google Scholar]
- Metzl JM, Hansen H. Structural competency: Theorizing a new medical engagement with stigma and inequality. Social Science & Medicine. 2014;103:126–33. doi: 10.1016/j.socscimed.2013.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. Journal of Women’s Health. 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milstein B. Introduction to the Syndemics Prevention Network. 2001 Retrieved September 14, 2014 from http://www.cdc.gov/syndemics/
- Minze LC, McDonald R, Rosentraub EL, Jouriles EN. Making sense of family conflict: intimate partner violence and preschoolers’ externalizing problems. Journal of Family Psychology. 2010;24(1):5–11. doi: 10.1037/a0018071. [DOI] [PubMed] [Google Scholar]
- Mizuno Y, Purcell DW, Knowlton AR, Wilkinson JD, Gourevitch MN, Knight KR. Syndemic Vulnerability, Sexual and Injection Risk Behaviors, and HIV Continuum of Care Outcomes in HIV-Positive Injection Drug Users. AIDS & Behavior, (Epub) 2014 doi: 10.1007/s10461-014-0890-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitrani VB, McCabe BE, Burns MJ, Feaster DJ. Family mechanisms of structural ecosystems therapy for HIV-seropositive women in drug recovery. Health Psychology. 2012;31(5):591–600. doi: 10.1037/a0028672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 2011. [Google Scholar]
- Nicholas PK, Willard S, Thompson C, Dawson-Rose C, Corless IB, Wantland DJ, Sefcik EF, Nokes KM, Kirksey KM, Hamilton MJ, Holzemer WL, Portillo CJ, Mendez MR, Robinson LM, Rosa M, Human SP, Cuca Y, Huang E, Maryland M, Arudo J, Eller LS, Stanton MA, Driscoll M, Voss JG, Moezzi S. Engagement with Care, Substance Use, and Adherence to Therapy in HIV/AIDS. AIDS Research & Treatment. 2014;2014:1–7. doi: 10.1155/2014/675739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noor SWB, Ross MW, Lai D, Risser JM. Use of Latent Class Analysis Approach to Describe Drug and Sexual HIV Risk Patterns among Injection Drug Users in Houston, Texas. AIDS & Behavior. 2014;18:S276–83. doi: 10.1007/s10461-014-0713-3. [DOI] [PubMed] [Google Scholar]
- Ostrach B, Singer M. At Special Risk: Biopolitical Vulnerability and HIV Syndemics Among Women. Health Sociology Review. 2012;21(3):258–71. [Google Scholar]
- Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, Lin LS, An Q, Mermin J, Lansky A, Hall HI, HIV Incidence Surveillance Group Estimated HIV Incidence in the United States, 2006–2009. PLOS ONE. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasch G. Probabilistic models for Some Intelligence and Attainment tests. Chicago, IL: University of Chicago Press; 1980. [Google Scholar]
- Rolland JS. Families, illness and disability. New York: Basic Books; 1994. [Google Scholar]
- Schumacher WE, Frick M, Kauselmann V, Maier-Hoyle R, van der Vliet R, Babiel R. Fully automated quantification of human immunodeficiency virus (HIV) type 1 RNA in human plasma by the COBAS AmpliPrep/COBAS Taqman system. Journal of Clinical Virology. 2007;38:304–12. doi: 10.1016/j.jcv.2006.12.022. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Temoshok LR, Straits-Tröster K, Atkinson JH, Koch W, Grant I. Family Conflict and Depressive Symptoms: A Study of HIV-Seropositive Men. AIDS & Behavior. 1997;1(1):53–60. [Google Scholar]
- Semple SJ. Conflict in Alzheimer’s caregiving families: Its dimensions and consequences. The Gerontologist. 1992;32:648–55. doi: 10.1093/geront/32.5.648. [DOI] [PubMed] [Google Scholar]
- Senn TE, Carey MP. HIV, STD, and Sexual Risk Reduction for Individuals with a Severe Mental Illness: Review of the Intervention Literature. Current Psychiatry Review. 2008;4(2):87–100. doi: 10.2174/157340008784529313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn T, Carey M, Variable P. The intersection of violence, substance use, negative affect, and STDs: Testing of a syndemic pattern among patients attending an urban STD clinic. Journal of the National Medical Association. 2010;102(7):614–20. doi: 10.1016/s0027-9684(15)30639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M. A Dose of Drugs, a Touch of Violence, a Case of AIDS: Conceptualizing the SAVA Syndemic. Free Inquiry in Creative Sociology. 1996;24(2):99–110. [Google Scholar]
- Singer M. Introduction to Syndemics: A Critical Systems Approach to Public and Community Health. San Francisco, CA: Jossey-Bass Books; 2009. [Google Scholar]
- Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Medical Anthropology Quarterly. 2003;17(4):423–41. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- Singer M, Romero-Daza N. A notable connection between substance abuse, violence, and AIDS: initial findings from research in the Puerto Rican community of Hartford. Hartford, CT: Hispanic Health Council; 1997. [Google Scholar]
- Stall R, Mills TC, Williamson J. Association of cooccurring psychosocial health problems and increased vulnerability to HIV & AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93:939–42. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software, Rel 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- Straus MA. Measuring intra family conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage & the Family. 1979;41(1):75–88. [Google Scholar]
- Sullivan KA, Messer LC, Quinlivan EB. Substance Abuse, Violence, and HIV/AIDS (SAVA) Syndemic Effects on Viral Suppression Among HIV Positive Women of Color. AIDS Patient Care and STDs. 2015;29(S1):S42–8. doi: 10.1089/apc.2014.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Kuramoto SJ, Davey-Rothwell MA, Latkin CA. The STEP into Action study: a peer-based, personal risk network-focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction. 2011;106(2):366–75. doi: 10.1111/j.1360-0443.2010.03146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towner WJ. The Changing Face of HIV Infection. Permanente Journal. 2008;12(4):60–4. doi: 10.7812/tpp/08-023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy EM, Martin TC. Children’s roles in the social networks of women in substance abuse treatment. Journal of Substance Abuse Treatment. 2007;32(1):81–8. doi: 10.1016/j.jsat.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Wyatt GE. Does a history of trauma contribute to HIV risk for women of color? Implications for prevention and policy. American Journal of Public Health. 2002;92(4):660–5. doi: 10.2105/ajph.92.4.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zea M, Reisen C, Poppen P, Bianchi F, Echeverry J. Disclosure of HIV status and psychological well-being among Latino gay and bisexual men. AIDS & Behavior. 2005;9(1):15–26. doi: 10.1007/s10461-005-1678-z. [DOI] [PubMed] [Google Scholar]
- Zierler S, Krieger N. Reframing Women’s Risk: Social Inequalities and HIV Infection. Annual Review of Public Health. 1997;18:401–36. doi: 10.1146/annurev.publhealth.18.1.401. [DOI] [PubMed] [Google Scholar]


