Abstract
Objectives
Surgical simulation is an increasingly important method to facilitate the acquiring of surgical skills. Simulation can be helpful in developing hip fracture fixation skills because it is a common procedure for which performance can be objectively assessed (i.e., the tip-apex distance). The procedure requires fluoroscopic guidance to drill a wire along an osseous trajectory to a precise position within bone. The objective of this study was to assess the construct validity for a novel radiation-free simulator designed to teach wire navigation skills in hip fracture fixation.
Methods
Novices (N=30) with limited to no surgical experience in hip fracture fixation and experienced surgeons (N=10) participated. Participants drilled a guide wire in the center-center position of a synthetic femoral head in a hip fracture simulator, using electromagnetic sensors to track the guide wire position. Sensor data were gathered to generate fluoroscopic-like images of the hip and guide wire. Simulator performance of novice and experienced participants was compared to measure construct validity.
Results
The simulator was able to discriminate the accuracy in guide wire position between novices and experienced surgeons. Experienced surgeons achieved a more accurate tip-apex distance than novices (13 vs 23 mm, respectively, p=0.009). The magnitude of improvement on successive simulator attempts was dependent on level of expertise; tip-apex distance improved significantly in the novice group, while it was unchanged in the experienced group.
Conclusions
This hybrid reality, radiation-free hip fracture simulator, which combines real-world objects with computer-generated imagery demonstrates construct validity by distinguishing the performance of novices and experienced surgeons. There is a differential effect depending on level of experience, and it could be used as an effective training tool in novice surgeons.
Keywords: Surgical Simulation, hip fracture, hybrid reality
Introduction
Hip fractures are a common orthopaedic problem in the United States, with an incidence of 957.3 per 100,000 for women and 414.4 per 100,000 for men between 1986 and 2005.1 The most common operative treatment involves using either cannulated screws, sliding hip screw fixation, or cephalomedullary nail. A fundamental skill required in performing these surgeries is the accurate placement of a guide wire in the femoral head.
Wire navigation is defined as the ability to deliver a wire from a specific starting point to a target end point under fluoroscopic guidance. This skill requires both an anatomical knowledge for interpreting the imagery and the manual dexterity for using instruments to advance the wire. Trainees currently learn fluoroscopic-guided wire navigation via the apprenticeship training model where a more experienced surgeon guides the trainee through the procedure on actual patients. Concerns involving patient safety, prolonged surgical time, and other limitations with in-vivo training make surgical simulation an appealing alternative for training of junior surgeons.2
The most common, current orthopaedic surgical simulation approaches to this problem use either cadaveric or synthetic models, coupled with drills, implants, C-arm fluoroscopy, and other typical OR equipment.2 Although this paradigm facilitates hands-on practice, it requires hazardous radiation exposure as well as access to costly radiation equipment and personnel, which may be prohibitive in some settings. The limitation posed by this existing training paradigm may potentially be overcome with a radiation-free simulator that uses sensors to track wire position within a synthetic proximal femur model. Such a simulator incorporates the beneficial radiation-free aspects of a computer-based model, while offering the same direct tactile feedback of a benchtop model.
The purpose of this study was to introduce a potentially widely applicable, radiation-free simulator and quantify its construct validity by measuring differences in the performance of novices and experienced orthopaedic surgeons using the simulator. A secondary goal was to demonstrate improvement in performance on the simulator with repeated practice in novice learners.
Materials and Methods
Subjects
After institutional review board approval, forty participants with varying levels of surgical experience participated in the study. The participants were classified into two groups. The novice group consisted of subjects with minimal to no surgical experience, and the experienced group consisted of subjects with orthopaedic surgical experience. The novice group included six first-year post-graduate (PGY-1) orthopaedic residents and twenty-four undergraduate engineering students. The experiment was performed six months into residency training for the PGY-1 residents, and it was assumed that they had limited to no surgical experience with hip fracture at this time interval. At our institution, PGY-1 residents spend six months on an orthopaedic surgery rotation, and of these six months, active participation in the operating room is limited. The experienced group included one PGY-3 orthopaedic resident, four PGY-4 orthopaedic residents, and five faculty surgeons who take general call.
Hybrid Reality Wire-Navigation Hip Fracture Simulator
The simulator used in this study mimics the task of drilling a guide wire from the lateral cortex to the femoral head with the aid of fluoroscopy. Unlike existing hip fracture simulators, the simulator does not use a mouse or a haptic feedback device for wire positioning and input. Instead, the simulator utilizes hybrid reality by blending real-world objects, such as a real drill and surrogate femur, with computer-generated fluoroscopic imagery. This technique aims to closely replicate the sensation of drilling in the operating room while retaining the benefit of a radiation-free training environment.
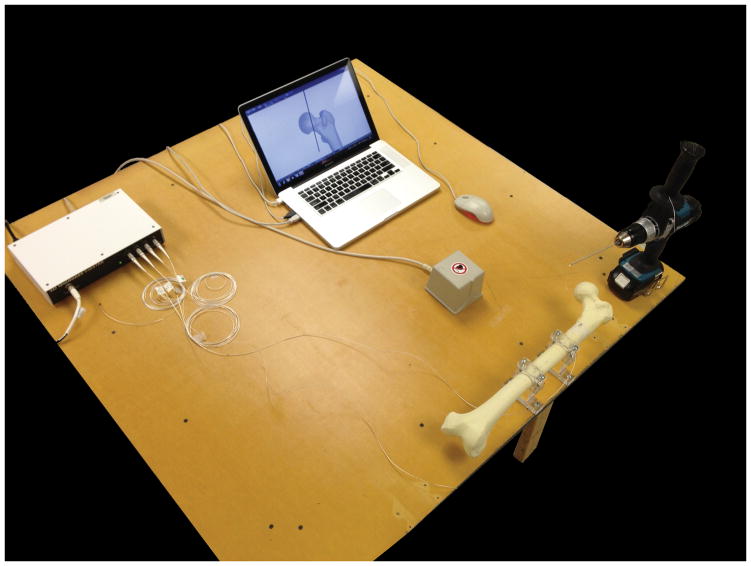
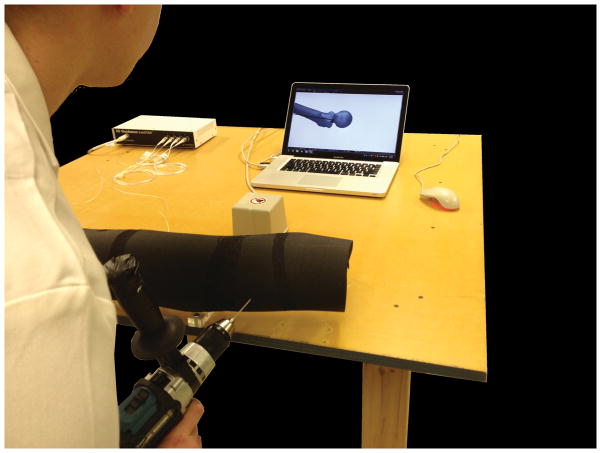
The simulator consists of four main components: a personal computer, a battery-powered drill, a synthetic femur (Sawbones Part No. 1129), and an electromagnetic tracking sensor (Ascension 3D Guidance trakSTAR™) (Figure 1). The electromagnetic sensors are attached to both the bone and an extension off the drill, which enables six degrees of freedom motion tracking (Figure 2). Foam padding is used to conceal the artificial bone to mimic the overlying soft tissue (Figure 3). Using the spatial data from the electromagnetic sensors, the computer generates dimensionally accurate virtual fluoroscopic images of both the guide wire and the synthetic femur (Figure 4). Two standard views are available in the simulator: the anteroposterior (AP) view and lateral view.
Figure 1.
The hybrid reality hip fracture simulator consists of a synthetic femur model (shown here without exterior foam padding) that is mounted onto a table, electromagnetic tracking sensors that are positioned on the femur and a hand-powered drill, and a laptop that displays simulated fluoroscopic images. Reproduced from Thomas et al, “The Validity and Reliability of a Hybrid Reality Simulator for Wire Navigation in Orthopaedic Surgery,” IEEE Transactions on Human-Machine Systems, by ScholarOne, Inc.
Figure 2.

The electromagnetic sensors are attached to both the synthetic bone and an extension off the drill, which enables six degrees of freedom motion tracking.
Figure 3.
The resident is demonstrating use of the simulator, which is concealed with foam padding to mimic soft tissue.
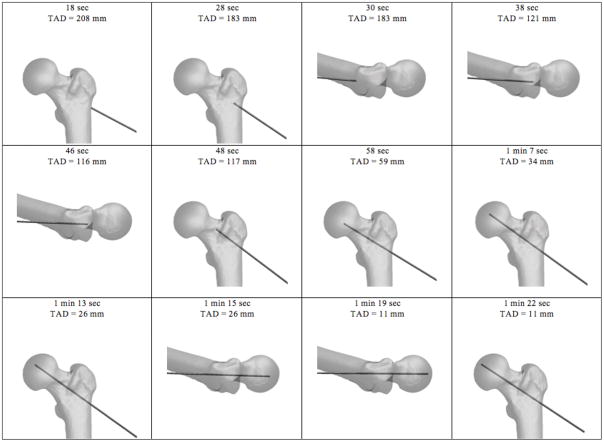
Figure 4.
Computer software utilizes positional data from the electromagnetic sensors to generate AP and lateral fluoroscopic images of the proximal femur and guide pin position. Progress in the simulation is shown going from upper left to right. Time stamp and tip-apex distance measures, which are not shown during the simulation, are included for reference.
Prior to beginning the trial, the participant is given written instructions about the exercise. The instructions explain that the objective is to place the wire in the center-center position of the femoral head. Performance outcomes measured include tip-apex distance (TAD), time to complete the task, and number of virtual fluoroscopic images. An angled guide, which is commonly utilized in hip screw surgery, is not incorporated in the simulator as the goal of the simulator is to target basic concepts of fluoroscopic-wire navigation, not to necessarily replicate all the steps of a hip screw surgery. Participants are instructed that the starting location is proximal to the lesser trochanter. The target is the center-center location without penetrating intra-articularly, while achieving a TAD less than 25 mm. The TAD is defined for the participants as the sum of the distance from the apex of the femoral head to the tip of the wire on the AP view and on the lateral view.
Each participant is allowed to manipulate the drill in the simulator environment to familiarize himself or herself with the simulator components and generated fluoroscopy for up to 10 minutes. The undergraduate engineering students are given a tutorial trial with instructions on proper placement of the wire. The participant directs the position, angle, and force of the drill to drive a guide wire from the center of the lateral cortex to the center of the femoral head. The participant can verify the position of the wire at any time via the computer generated fluoroscopic images, thereby mimicking the intraoperative use of a C-arm. The simulation continues until the participant is satisfied with the position of the guide wire. After the end of a trial, an interactive 3D model of the proximal femur appears with the final position of the guide wire. In addition to the visual model, the simulator saves each virtual fluoroscopic image that is requested and records the TAD and the total duration of the trial. After task completion, trainees are allowed to review the 3D model and analyze the collected data to increase learning through immediate feedback.
Construct Validity
Construct validity is the degree to which a test measures the underlying concepts that are being assessed.3 To demonstrate construct validity, the simulator should distinguish between participants of varying skill. To assess construct validity, both the novice and experienced groups in our study completed three consecutive trials on the simulator. Performance metrics analyzed included TAD, time to completion, and the total number of virtual fluoroscopic images used. Statistical analysis included t-test and chi-squared analysis to compare results of novices and experienced surgeons, and subgroups within the novice and experienced groups. An analysis of variance model was utilized to analyze changes in performance across the three simulator trials.
Results
Performance on the simulator was compared between the novice and experienced groups. The average TAD of the experienced group (12.7±3.9 mm) was significantly less than the corresponding average TAD of the novice group (23±11.7 mm, p=0.009) (Table 1). The experienced group also significantly outperformed the novice group in TAD for the final trial (p=0.037). The average time to completion and number of virtual fluoroscopic images used were not statistically different between the two groups (Table 1). Sixty-seven percent of novices achieved an average TAD less than 25 mm across all three trials, compared to one hundred percent of experienced surgeons (chi-squared 4.44, p=0.035). The average TAD of the novice group decreased with each successive trial (p=0.021), while it did not change for the experienced group (p=0.59) (Table 1). The average time for the novice and experienced groups decreased significantly with repetition during successive trials (p=0.023, p=0.013, respectively). The average number of virtual fluoroscopic images decreased with repetition during successive trials for the experienced group (p=0.083), but not for the novice group (p=0.96) (Table 1).
Table 1.
Performance on simulator in novice and experienced groups for each trial and averaged across all three trials.
| Novice | Experienced | p-value | |
|---|---|---|---|
| Tip-apex distance (mm) | |||
| Trial 1 | 29.1±20.9 | 12.4±4.7 | 0.017* |
| Trial 2 | 22.0±12.4 | 14.2±6.9 | 0.069 |
| Trial 3 | 18.2±9.2 | 11.5±6.3 | 0.037* |
| Average | 23.1±11.7 | 12.7±3.9 | 0.009* |
| p-value | 0.021* | 0.59 | |
|
| |||
| Time (s) | |||
| Trial 1 | 180.9±64.5 | 205.9±90.3 | 0.34 |
| Trial 2 | 147.8±72.7 | 129.0±43.3 | 0.45 |
| Trial 3 | 133.7±63.3 | 121.9±52.1 | 0.60 |
| Average | 154.1±56.7 | 152.4±49.3 | 0.93 |
| p-value | 0.023* | 0.013* | |
|
| |||
| Number of fluoro shots | |||
| Trial 1 | 25.1±11.4 | 38.8±19.8 | 0.010* |
| Trial 2 | 24.0±15.2 | 26.4±12.4 | 0.66 |
| Trial 3 | 24.3±16.2 | 23.6±13.2 | 0.90 |
| Average | 24.5±12.7 | 29.6±12.3 | 0.27 |
| p-value | 0.96 | 0.083 | |
Values demonstrate mean ± SD.
p<0.05
Subgroup analysis of the novice group demonstrated no significant difference in average TAD across all three trials between the PGY-1 residents (21.5±7.1mm) and engineering students (23.5±12.7mm, p=0.71). There was no significant difference in number of fluoroscopic shots (33±13.8 vs 22.4±11.7, p=0.06), while there was significant variation in time (196±71.7s vs 143.7±48.6s, p=0.04) between the PGY-1 residents and engineering students, respectively. Comparison of the senior residents and attending surgeons demonstrated no difference in average TAD (12.4±2.5mm vs 13.1±5.9, respectively, p=0.82), number of fluoroscopic shots (29.3±12.1mm vs 30±14.5, respectively, p=0.94), and time (158.1±59.7 vs 143.75±34.5, respectively, p=0.68).
Discussion
The goals of this study were to introduce a hybrid reality, radiation-free hip fracture simulator for wire navigation training and to compare the performance of subjects, with varying surgical experience, on the simulator. The simulator discriminated novice and experienced groups based on TAD, providing preliminary evidence that the simulator is a viable method for training. Less experienced subjects displayed a significantly greater improvement in TAD compared to a more experienced group during repeated trials on the simulator, suggesting greater benefit from repeated practice in this group.
Fluoroscopic-guided wire navigation is a necessary skill in fracture fixation that presents a steep learning curve for learners. The surgeon must rely on tactile feedback and visual cues to accurately place a wire in 3D space, relying upon 2D imagery. Fluoroscopy poses a radiation risk for the patient and the surgeon, therefore minimizing exposure by taking only pertinent shots is important.4
Surgical simulation provides a controlled environment for trainees to practice independently or with supervision. Skills assessment and feedback are important and valuable parts of simulation training.2, 5, 6 Simulation in orthopaedic trauma has traditionally consisted of benchtop models that involve placing implants on cadaveric or synthetic bone models.7 Technological advancements have facilitated the introduction of computer-based simulators into the field of orthopaedics, greatly expanding the opportunities for surgical skills training. There are several simulators that target hip fracture surgery. The BoneDoc DHS simulator (Auckland, New Zealand) is a computer-based dynamic-hip screw simulator that has shown good face validity and construct validity.8, 9 TraumaVision (Simulutions, Burnsville, MN) is a haptic-based simulator that utilizes a handheld haptic device to act as a driver, and produces fluoroscopic-like images of the hip using computer technology.10 Computer navigation, which provides concurrent augmented feedback during surgery, has been advocated to be an important surgical training tool in arthroplasty, and potentially in hip fracture surgery as well.11, 12, 13 Participants who trained with computer navigation took fewer attempts to position screws in the hip and used less fluoroscopy time than those trained with fluoroscopy.11
The present simulator is conceptually similar to computer navigation, but it does not require fluoroscopy to initially register the sensors, making it entirely radiation-free. Further, the simulator does not rely upon the availability of an expensive surgical navigation system. In this study, we have demonstrated that a hybrid reality, wire navigation simulator differentiates novices from more experienced surgeons on a variable (TAD) that has been demonstrated to be clinically relevant. The novice group had a larger absolute TAD, and lower percentage of TAD less than 25 mm, compared to the experienced group. We acknowledge that the simulator exercise tested both the participant’s cognitive understanding and technical skill of achieving an acceptable TAD. It is plausible that the participant’s lack of conceptual understanding of TAD, despite the written and verbal instructions, may have confounded his or her ability to technically execute the task. More repetition beyond three trials may also be necessary to demonstrate a better learning curve.
It was further demonstrated that the magnitude and type of improvement on the simulator was dependent on level of expertise. In our experiment design, we placed equal emphasis on TAD, time, and number of fluoroscopic images. The experienced group started with a lower TAD, at the expense of taking more time and fluoroscopic images on the first try. With each trial, the number of images and time decreased while TAD remained constant. The novice group, on the other hand, started with a larger TAD and took longer to complete the first trial, which decreased significantly by the third trial. This suggests that the experienced surgeons were already proficient at achieving a TAD less than 25 mm (accuracy), and the simulator simply helped to improve efficiency (less time and fluoroscopic images). The novice subjects had an improvement in their accuracy and efficiency with each successive trial. In addition, number of fluoroscopic images did not change for the novice group, suggesting that three trials may not be enough to demonstrate efficiency with fluoroscopy. Both accuracy and efficiency are important and interrelated in evaluation of surgical skills. Future experiments may need to focus on separating these two elements.
We acknowledge that the two groups were not homogeneous in composition - this was a byproduct of confronting an inherent challenge of performing a study limited to residents and surgeons with a certain level of surgical experience at one institution. Comparison of the subgroups within the novice and experienced groups demonstrated that there was no significant difference between the PGY-1 residents and engineering students, and senior residents and faculty surgeons, with the exception of time. The engineering students were faster than the PGY-1 residents, and as fast as the attending surgeons in completing the task. Perhaps the engineering students’ lack of medical knowledge and clinical experience led them to exercise less caution than the PGY-1 residents.
In conclusion, wire navigation in orthopaedics is a fundamental skill that requires both an understanding of fluoroscopy and visual-spatial dexterity. Teaching this multi-faceted skill by means of a hip fracture simulator is appealing because hip fractures are common and most training occurs on actual patients over several years. We have demonstrated that our hybrid-reality, radiation-free, hip fracture simulator can discriminate novice and experienced surgeons. The data further suggests that trainees with limited surgical experience will benefit most from this simulator. Future investigations comparing different types of simulators will be important to determine which is most useful and cost-effective, and to demonstrate that simulation improves performance of trainees in the actual operating room.
Acknowledgments
Source of Funding: This project was funded (in part) by a National Board of Medical Examiners® (NBME®) Edward J. Stemmler, MD Medical Education Research Fund grant. Grants from the Orthopaedic Research and Education Foundation, OMeGA Medical Grants, and the Orthopaedic Trauma Association provided additional support.
This project was supported by grant number R18HS022077 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
The authors would like to thank Mr. Brian Westerlind for his support during the experiment.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
IRB Approval: This project meets the regulatory requirements for the protection of human subjects.
Presented in part at the AOA CORD Meeting in Denver, CO, June 2013.
Bibliography
- 1.Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atesok K, Mabrey JD, Jazrawi LM, et al. Surgical simulation in orthopaedic skills training. The Journal of the American Academy of Orthopaedic Surgeons. 2012;20:410–422. doi: 10.5435/JAAOS-20-07-410. [DOI] [PubMed] [Google Scholar]
- 3.Michelson JD. Simulation in orthopaedic education: an overview of theory and practice. J Bone Joint Surg Am. 2006;88:1405–1411. doi: 10.2106/JBJS.F.00027. [DOI] [PubMed] [Google Scholar]
- 4.Giordano BD, Grauer JN, Miller CP, et al. Radiation exposure issues in orthopaedics. J Bone Joint Surg Am. 2011;93:e69, 61–10. doi: 10.2106/JBJS.J.01328. [DOI] [PubMed] [Google Scholar]
- 5.Schaefer JJ, 3rd, Vanderbilt AA, Cason CL, et al. Literature review: instructional design and pedagogy science in healthcare simulation. Simul Health. 2011;6(Suppl):S30–41. doi: 10.1097/SIH.0b013e31822237b4. [DOI] [PubMed] [Google Scholar]
- 6.Michelson JD. Simulation in orthopaedic education: an overview of theory and practice. J Bone Joint Surg Am. 2006;88:1405–1411. doi: 10.2106/JBJS.F.00027. [DOI] [PubMed] [Google Scholar]
- 7.Leong JJ, Leff DR, Das A, et al. Validation of orthopaedic bench models for trauma surgery. J Bone Joint Surg Br. 2008;90:958–965. doi: 10.1302/0301-620X.90B7.20230. [DOI] [PubMed] [Google Scholar]
- 8.Blyth P, Stott NS, Anderson IA. Virtual reality assessment of technical skill using the Bonedoc DHS simulator. Injury. 2008;39:1127–1133. doi: 10.1016/j.injury.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Blyth P, Stott NS, Anderson IA. A simulation-based training system for hip fracture fixation for use within the hospital environment. Injury. 2007;38:1197–1203. doi: 10.1016/j.injury.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 10.Froelich JM, Milbrandt JC, Novicoff WM, et al. Surgical simulators and hip fractures: a role in residency training? J Surg Educ. 2011;68:298–302. doi: 10.1016/j.jsurg.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 11.Nousiainen MT, Omoto DM, Zingg PO, et al. Training femoral neck screw insertion skills to surgical trainees: computer-assisted surgery versus conventional fluoroscopic technique. J Orthop Trauma. 2013;27:87–92. doi: 10.1097/BOT.0b013e3182604b49. [DOI] [PubMed] [Google Scholar]
- 12.Gofton W, Dubrowski A, Tabloie F, et al. The effect of computer navigation on trainee learning of surgical skills. J Bone Joint Surg Am. 2007;89:2819–2827. doi: 10.2106/JBJS.F.01502. [DOI] [PubMed] [Google Scholar]
- 13.DiGioia AM, 3rd, Blendea S, Jaramaz B. Computer-assisted orthopaedic surgery: minimally invasive hip and knee reconstruction. Orthop Clin North Am. 2004;35:183–189. doi: 10.1016/S0030-5898(03)00133-0. [DOI] [PubMed] [Google Scholar]