Abstract
Intracranial metastasis of prostate cancer is rarely seen, and there are few studies in this regard in the literature. Most of these studies in the literature comprise the metastasis of prostate cancer to the sphenoid sinus, and metastasis to the frontal and ethmoid sinus is a much rare entity. Association of visual symptoms, epistaxis, headache, and hematuria may indicate a urologic malignancy in terms of the origin of the primary tumor. This study was aimed to present the prostate cancer case of a 73-year-old patient whose paranasal sinus tomograms revealed the presence of frontal and ethmoid sinus metastasis.
Keywords: Metastasis, paranasal sinus, prostatic adenocarcinoma
Introduction
Prostate adenocarcinoma, which is frequently seen in the elderly male population and is one of the leading causes of death, spreads through local invasion and lymphatic and vascular channels.[1,2] While bony tissue and visceral organs are frequent sites of metastasis intracranial metastasis of prostate adenocarcinoma is not widespread.[1] Metastasis of primary prostate adenocarcinoma to paranasal sinuses, and especially to frontal and ethmoid sinuses, is a rarely encountered case.[3,4] The diagnosis of prostate cancer is made during histopathological examination of transrectal ultrasonography-guided biopsies carried out because of increase in PSA levels. An intravesical mass was observed on urinary system ultrasonograms of our patient who had macroscopic hematuria, and dysuria. The mass, which had been treated with transurethral resection, was detected to be a prostate carcinoma after a histopathological examination was carried on.
Case presentation
A 73- year-old male patient applied to the outpatient clinic of ophthalmology due to a swelling in his right eye and headache ongoing for 3 months. On examination, exophthalmos in the right eye, limitation in looking up and to the right, and diplopia were determined. Thereupon, orbital Magnetic Resonance Imaging (MRI) and paranasal sinus Computed Tomography (CT) revealed a mass lesion causing destruction in the frontal sinus, frontal ethmoid cells, and orbital and frontal sinus posterior wall, and a dural involvement in the frontobasal site, and also destructing brain tissue (Figure 1).
Figure 1 a–d.
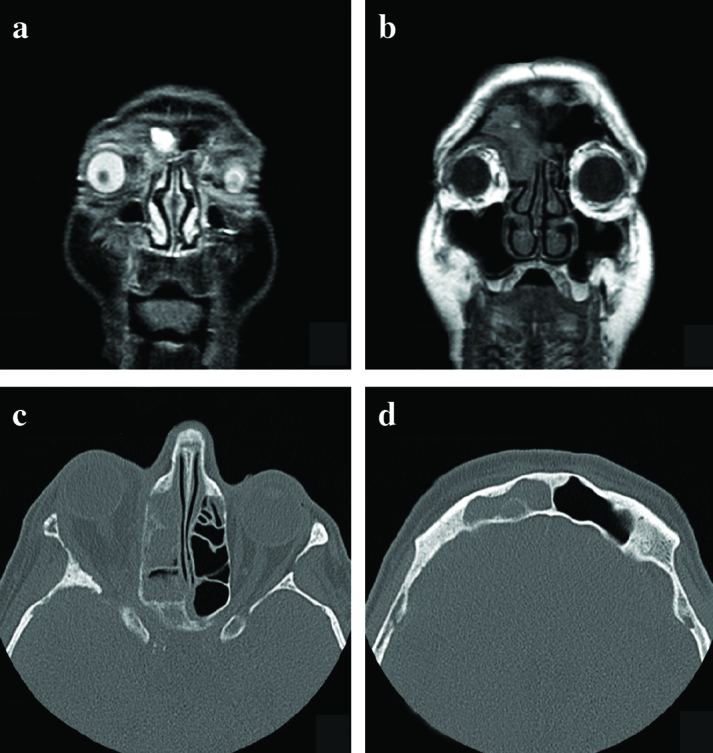
(a) Orbital MRI; Exophthalmos on the right eye and right frontoethmoidal sinus involvement are seen. (b) MR Imaging showing involvement of the frontal, ethmoid sinus. (c, d) Paranasal sinus tomography showing frontoethmoidal sinus involvement
Hereupon, biopsies were taken from right frontal recess, ethmoid cells and lesions in the uncinate process under local anesthesia by the otorhinolaryngology clinic after his informed consent was obtained. Since the patient had hematuria and difficulty in urinating at the same time, his urologic evaluation was conducted in our outpatient clinic. The patient whose serum total PSA level was determined as 20.4 ng/dL, underwent a digital rectal examination which demonstrated diffusely indurated prostate. The urinary system ultrasonography of the patient, who complained about intermittent hematuria revealed a mass causing grade 3 hydronephrosis in the right kidney and ureteral obstruction adjacent to the right lateral wall of the bladder. Then the patient underwent cystoscopy under general anesthesia after his informed consent was obtained. Transurethral resection (TUR) was performed on solid tumoral tissues originating from the prostate which extended to the right lateral wall of the bladder involving the right ureter orifice. Intraoperatively, right ureter orifice could not be separated and the circulation of methylene blue instilled through the right percutaneous nephrostomy to the bladder could not be observed. In consequence of the histopathological examination of the biopsies taken from the paranasal sinuses and TUR material, prostate adenocarcinoma, with a Gleason score of 4+5, was determined to be the primary focus for metastasis to the frontoethmoidal sinus and uncinate process (Figures 2, 3). Any other metastasis was not detected on the whole body bone scintigraphy of the patient diagnosed with stage 4 prostate cancer, and the patient was started on maximal androgen blockade treatment.
Figure 2.
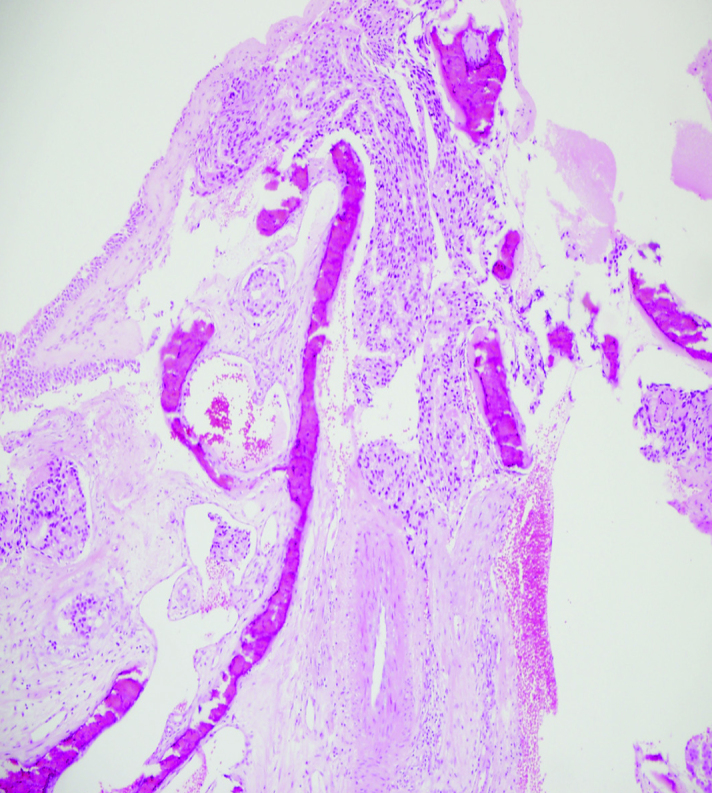
Prostatic adenocarcinoma metastasis is seen under paranasal sinus mucosa (HE ×200)
Figure 3.
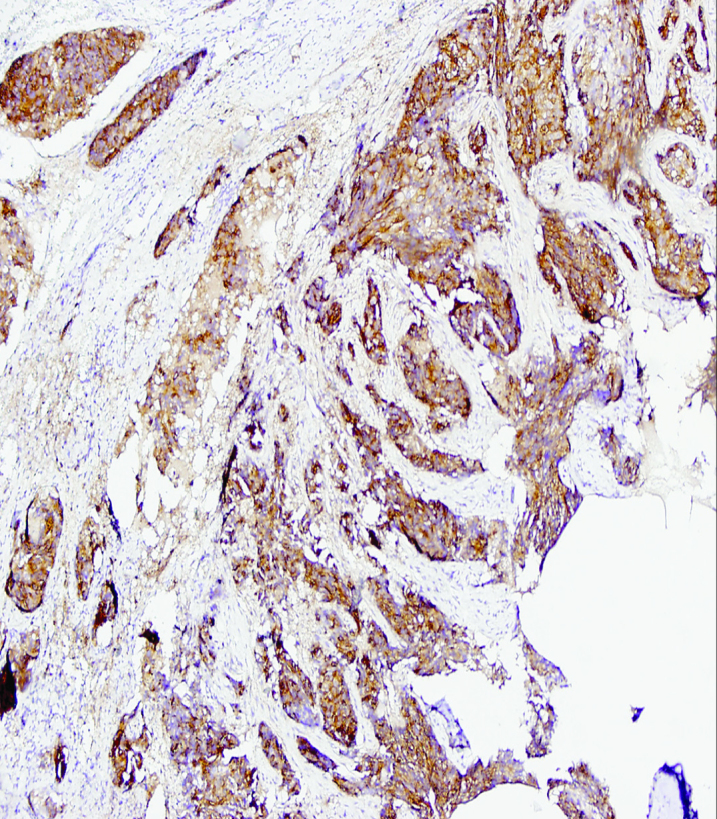
Prostatic adenocarcinoma metastasis showing positive staining of the specimens obtained from paranasal sinuses with PSA (PSA ×200)
Discussion
Metastasis of prostate cancer to the paranasal sinuses is rare.[5,6] While prostate cancer most frequently metastasizes to the bony tissue, visceral organs like the lungs, liver, and adrenal gland, also tertiary lymph nodes in the supraclavicular and mediastinal areas can also be affected.[2,6] In autopsies performed on patients with prostate cancer, incidence rates of intracranial metastasis have been found to vary between 4.2 and 4.4 percent.[1] In a study, prostate was found to be the primary source of only 12 out of 169 cases with metastasis to the paranasal sinuses.[7] In the literature, together with the publications reporting the spread of prostate cancer to paranasal sinuses and sphenoid sinus, there are very few publications reporting metastasis to the frontal and ethmoid sinus.[4,6] Patients with metastasis of the prostate cancer to the paranasal sinus generally demonstrate prevalent disease symptoms.[4,8] Malignant tumors of the nose and paranasal sinus constitute less than 1% of all malignant tumors of the head and neck.[5] Only 1% of the malignant tumors of the nose and paranasal sinus- the majority of which is primary squamous cell carcinoma- is metastatic. Tumors that most frequently show metastasis to the paranasal sinuses are hypernephroma, pulmonary, thoracic, gastrointestinal tract, adrenal cancers, skin melanoma, thyroid, pancreatic cancer, and seminoma.[3,8,9] While maxillary sinus[7] or sphenoid sinus[3,4] has been reported to be the most affected sinuses in different publications, the least affected sinuses have been reported to be the frontal and ethmoid sinuses.[3,6]
The mechanisms of metastasis to paranasal sinuses in prostate cancer have not definitely established yet; however, there are some theories that have been put forward. It has been suggested that metastasis is caused by retrograde embolisms from prevertebral plexus or by tumor embolisms through retrograde flow thanks to interconnection of low-pressure loaded venous systems and thin valves of the veins in the thorax, abdomen and pelvis. In addition, bone metastasis has been suggested to occur with the close connection and interaction of the pelvic lymphatic and venous plexus that are adjacent to each other.[3]
Primary symptoms of paranasal sinus metastasis are reduced incidence of nose bleeding, nasal mass or swelling, nasal obstruction and pain. Orbital symptoms can be diplopia, loss of vision, exophthalmos, blepharedema, and ptosis.[1,3,5] These symptoms may not clearly indicate malignancy every time. The first symptom of metastasis to the paranasal sinus can be an infection. Resistance of these infections to treatment suggests the possibility of malignancy. With the purpose of diagnosing metastasis, determining its nature, and obtaining information regarding primary focus, biopsy should be performed. Histopathologically, the most important sign is that the metastatic lesions of prostate carcinoma show positive coloration with PSA. The prognosis of the metastatic disease in the nasal and paranasal areas is rather poor, and even though long-term survival rates have been reported in some studies, the patients can be generally lost in a few months.[1]
In our case, detection of a mass in the paranasal sinuses in MR imaging and CT scans, and also observation of an intravesical mass in urinary ultrasound performed on the patient with concomitant vision problems, hematuria and difficulty in urinating raised the suspicion of a urologic malignancy, and with the aim of excluding possibility of a bladder tumor which was considered in the first plan, cystourethroscopy was performed on the patient. The patient, who was accepted having metastatic prostate carcinoma as a consequence of the histopathological examinations, was started on maximal androgen blockade treatment. However, the general state of the patient deteriorated due to a cerebrovascular event and the patient was lost in the intensive care unit without having received any treatment for the metastatic lesions in the paranasal sinuses.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - F.A.; Design - F.A., H.Ç.; Supervision - F.A., M.A.; Resources - F.A., H.Ç.; Materials - F.A.; Data Collection and/or Processing - F.A., H.Ç., G.G.; Analysis and/or Interpretation - F.A., M.A.; Literature Search - F.A., H.Ç.; Writing Manuscript - F.A., H.Ç.; Critical Review - F.A., M.A.; Other - F.A., M.A., H.Ç., G.G.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Saleh HA, O’Flynn P, Jones NS. Prostatic metastases in the nose and paranasal sinuses. Laryngol Otol. 1993;107:629–32. doi: 10.1017/s0022215100123928. https://doi.org/10.1017/S0022215100123928. [DOI] [PubMed] [Google Scholar]
- 2.Patrick C, Walsh MD. Campbell’s Urology. 8 edition. Philadelphia: W.B. Saunders; 2002. [Google Scholar]
- 3.Viswanatha B. Prostatic carcinoma metastatic to the paranasal sinuses:a case report. Ear Nose Throat J. 2008;87:519–20. [PubMed] [Google Scholar]
- 4.Fortson JK, Bezmalinovic ZL, Moseley DL. Bilateral ethmoid sinusitis with unilateral proptosis as an initial manifestation of metastatic prostate carcinoma. J Natl Med Assoc. 1994;86:945–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Abrahao M, Gonçalves AP, Yamashita R, Dedivitis RA, Santos RO, Nascimento LA, et al. Frontal sinus adenocarcinoma. Sao Paulo Med J. 2000;118:118–20. doi: 10.1590/S1516-31802000000400009. https://doi.org/10.1590/S1516-31802000000400009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jimenez Oliver V, Lazarich Valdes A, Davila Morillo A, Ruiz del Portal JM, Conde Jimenez M, Fernandez Ruiz E, et al. Frontal ethmoid metastases of prostatic carcinoma. Report of one case and review of the literature. Acta Otorrinolaringol Esp. 2001;52:151–4. doi: 10.1016/s0001-6519(01)78191-5. [DOI] [PubMed] [Google Scholar]
- 7.Prescer A, Brors D. Metastases to the paranasal sinuses: case report and review of the literatüre. Laryngorhinootologie. 2001;80:583–94. doi: 10.1055/s-2001-17835. [DOI] [PubMed] [Google Scholar]
- 8.Puche-Sanz I, Vázquez-Alonso F, Flores-Martín JF, Almonte-Fernández H, Cózar-Olmo JM. Sphenoid sinus metastasis as the presenting manifestation of a prostatic adenocarcinoma: case report andoverview of the literature. Case Rep Oncol Med. 2012:819809. doi: 10.1155/2012/819809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maschka DA, McCulloch TM, Nerad JA. Prostate cancer metastatic to the orbit. Ann Otol Rhinol Laryngol. 1996;105:70–1. doi: 10.1177/000348949610500113. https://doi.org/10.1177/000348949610500113. [DOI] [PubMed] [Google Scholar]
- 10.Flocks RH, Boatman DL. Incidence of head and neck metastases from genitourinary neoplasms. Laryngoscope. 1973;83:1527–32. doi: 10.1288/00005537-197309000-00011. https://doi.org/10.1288/00005537-197309000-00011. [DOI] [PubMed] [Google Scholar]


