Abstract
Total hip arthroplasty is an increasingly common procedure used to address degenerative changes in the hip joint due to osteoarthritis. Although generally associated with good results, among the challenges associated with hip arthroplasty are accurate measurement of biomechanical parameters such as leg length, offset, and cup position, discrepancies of which can lead to significant long-term consequences such as pain, instability, neurological deficits, dislocation, and revision surgery, as well as patient dissatisfaction and, increasingly, litigation. Current methods of managing these parameters are limited, with manual methods such as outriggers or calipers being used to monitor leg length; however, these are susceptible to small intraoperative changes in patient position and are therefore inaccurate. Computer-assisted navigation, while offering improved accuracy, is expensive and cumbersome, in addition to adding significantly to procedural time. To address the technological gap in hip arthroplasty, a new intraoperative navigation tool (Intellijoint HIP®) has been developed. This innovative, 3D mini-optical navigation tool provides real-time, intraoperative data on leg length, offset, and cup position and allows for improved accuracy and precision in component selection and alignment. Benchtop and simulated clinical use testing have demonstrated excellent accuracy, with the navigation tool able to measure leg length and offset to within <1 mm and cup position to within <1° in both anteversion and inclination. This study describes the indications, procedural technique, and early accuracy results of the Intellijoint HIP surgical tool, which offers an accurate and easy-to-use option for hip surgeons to manage leg length, offset, and cup position intraoperatively.
Keywords: total hip arthroplasty, leg length, offset, cup position, Intellijoint HIP, intraoperative
Video abstract
Introduction
Total hip arthroplasty (THA) is a common and effective procedure for relieving pain and dysfunction associated with advanced osteoarthritis and other conditions adversely affecting mobility at the hip joint. Although generally associated with positive results and long-term improvement in patient quality of life,1,2 THA is nonetheless associated with adverse events and postprocedural deficits related to leg length discrepancies (LLDs), as well as discrepancies in offset and cup placement.3–5 Post-THA errors in these parameters are associated with gait alteration,6–9 low back pain,10 and patient dissatisfaction.11 Such discrepancies often necessitate corrective procedures and are increasingly leading to medical malpractice litigation.12,13
Maintaining accuracy in postsurgical leg length, offset, and cup placement during THA is difficult and subject to error. The sensitivity of these factors is highlighted in studies that have shown that a change of as little as 5° of leg flexion or abduction can induce alterations in leg length of up to 8 mm.14 Similarly, inaccurate sizing of implants can alter global and femoral offset, affecting abductor strength, range of motion, and overall physical function,15–18 as well as inducing long-term pain.19 Compounding the biomechanical issues associated with inaccurate leg length are the costs associated with these deficits. Per-revision costs are significant, having been reported to reach $54,000 in the US20,21 and £21,000 in the UK.22 Methods for accurately sizing hip implants during THA are therefore valuable in both improving patient satisfaction and decreasing the overall costs to the health care system.
Traditional freehand techniques of managing intraoperative parameters rely on surgeon experience and tissue tensioning to manually place components accurately. These methods, however, rely heavily on surgeon experience and are subject to inaccuracies associated with patient movement or orientation changes during surgery.14 Mechanical methods of minimizing postsurgical discrepancies, such as usage of outrigger or caliper devices, have been developed; however, these methods generally address only leg length and provide poor feedback regarding offset and center of rotation, therefore providing insufficient data to accurately achieve appropriate postsurgical leg length.
Traditional computer-assisted navigation methods provide more data regarding leg length, offset, and center of rotation but are limited by their cumbersome nature and the large capital costs associated with the systems.23,24 Originally pioneered to assist with neurosurgery, these systems require substantial alteration of the surgical space to accommodate their components and are associated with disruption of surgical workflow and prolonged surgical time.25 Currently used in only 1%–3% of procedures, these systems provide important information but do so in a manner that is neither cost-effective nor minimally intrusive.26,27
The Intellijoint HIP® 3D mini-optical navigation tool (Intellijoint Surgical, Inc, Waterloo, ON, Canada) is a new intraoperative guidance tool that provides surgeons with real-time data on leg length, offset, and cup position, thereby allowing for confident selection of the correct implant in order to ensure appropriate postsurgical biomechanics. With miniature size and without altering surgical workflow or techniques, the device enables faster decision making (fewer trial reductions) and minimizes postprocedural LLDs. This miniature, novel system offers the accuracy of traditional computer-assisted navigation systems with the ease of use of manual methods. The purpose of this study is to introduce the device, to discuss indications for use and contraindications, describe the surgical procedure, as well as summarize the validation testing of the device.
Materials and methods
Device description
The Intellijoint HIP 3D mini-optical navigation tool is a miniature, surgeon-controlled surgical guidance tool for intraoperative positional measurements during THA, which has received initial approval from both Health Canada and the US Food and Drug Administration (FDA) for use in North America. This novel navigation tool uses infrared optical technology and integrated microelectronics to measure changes in leg length, offset and hip center, as well as native acetabular position and cup position (anteversion and inclination), which are measured relative to Murray’s radiographic definitions.28 The system generates positional measurements between a camera (mounted on the iliac crest) and a tracker that can be mounted on various objects (eg, the femur, the acetabular cup impactor) during surgery to measure their positions (Figure 1). The camera detects the tracker within its field of view and communicates with a workstation, which executes the application software to guide the device workflow and display measurements to the surgeon (Figure 2). Quick connect magnetic mounts allow the camera and the tracker to be removed and reattached to their respective platforms as needed throughout the procedure.
Figure 1.
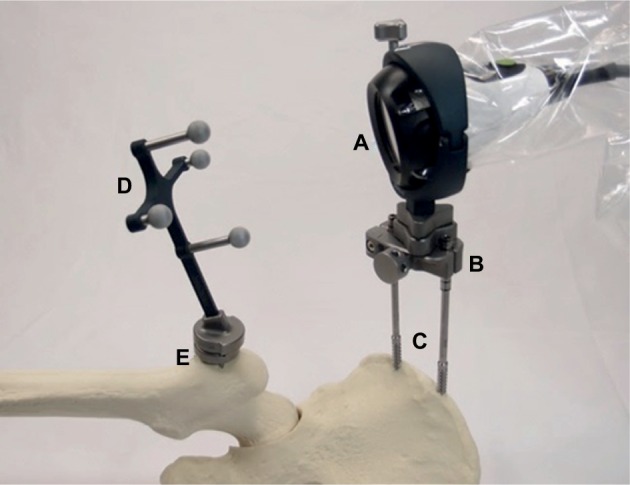
The Intellijoint HIP 3D mini-optical navigation tool.
Notes: The camera (A), enclosed in its sterile drape, is attached to the pelvic platform (B) via 2 screws (C). The tracker (D) is magnetically attached to the femur platform (E). The camera captures the movements of the tracker when registering the native orientation or while trialing the implant components and thereafter relays the information to a workstation for review by the surgeon.
Figure 2.
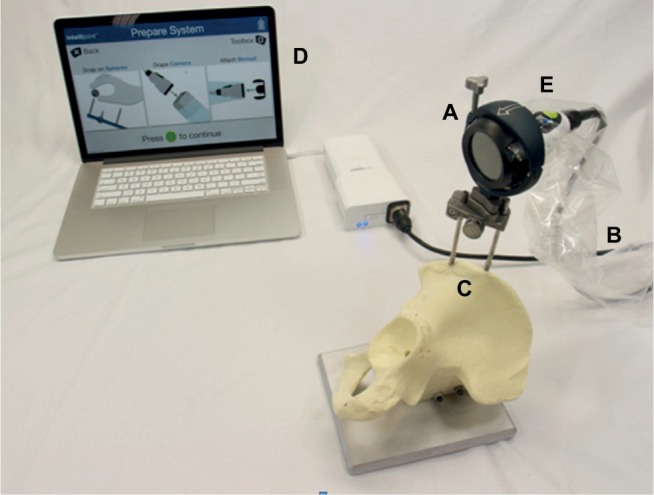
The Intellijoint HIP system.
Notes: The camera (A) is enclosed within a sterile drape (B) and fixed to the pelvis via a pelvic platform (C). The camera transmits positional data for display on the workstation (D), placed outside of the sterile field. Control buttons on the camera (E) allow the surgeon to interact with the system and manipulate the workstation display without leaving the sterile field.
Indications for use and procedural technique
The Intellijoint HIP navigation tool is indicated for patients undergoing orthopedic surgical procedures, specifically THA, using both traditional and minimally invasive techniques. It is incorporated into the normal surgical workflow without alterations to the surgical technique. The workstation is situated outside of the sterile field, in view of the surgeon, while the camera and other equipment remain within the sterile field. Real-time data regarding cup position, leg length, and offset are relayed from the device to the workstation and are available for surgeon reference during the procedure.
With the patient positioned in the lateral decubitus position and prior to primary incision, 2 stab incisions are made on the iliac crest and pelvic screws are installed securely to the iliac crest, onto which is fixed the pelvic platform. The camera, enclosed in its sterile camera drape, is secured via a shroud inside an adjustable spherical camera clamp. The camera is then attached to the pelvic platform via a magnetic attachment, with buttons on the camera allowing the surgeon to operate the software from within the sterile field. Prior to exposure of the operative hip, the patient’s horizontal and frontal planes are established through registration steps using the camera, the embedded microelectronics and the associated hardware (eg, alignment rod).
Following registration and exposure, the femoral platform is fixed to the greater trochanter using the specially designed inserter and screw. The tracker is magnetically attached to the femur platform and remains in the field of view of the camera. Baseline leg position is collected by attaching the tracker to the femur platform and holding the leg in a neutral orientation (0° flexion, 0° rotation, and 0° abduction). Following baseline leg position capture, native hip center of rotation is collected by articulating the leg through an angular range of motion that encompasses flexion/extension, internal/external rotation and abduction/adduction movements.
Following collection of baseline measurements, the camera and tracker are detached from the magnetic pelvic and femur platforms, respectively. Hip dislocation, femoral head removal as well as acetabular and femoral preparation are accomplished as per surgical routine, without need for removal of the pelvic or femur platforms. Prior to acetabular preparation and cup implantation, a probe, fitted with the tracker, may be used to define a reference plane on the native acetabulum. Once defined, the tracker can be attached to the cup impactor, via an impactor adaptor, to provide real-time cup position information to assist in the implantation of the cup. Hip reduction following implantation allows for capture of the new center of rotation of the hip, registered through circumduction of the new artificial joint. The tracker can also be returned to the femoral platform to provide real-time information regarding leg length and offset to assist the surgeon in the proper selection of femoral implant sizes. All measurements from each trial are displayed in real time for the surgeon’s reference and can be saved on the workstation at any time throughout the procedure (Figure 3).
Figure 3.
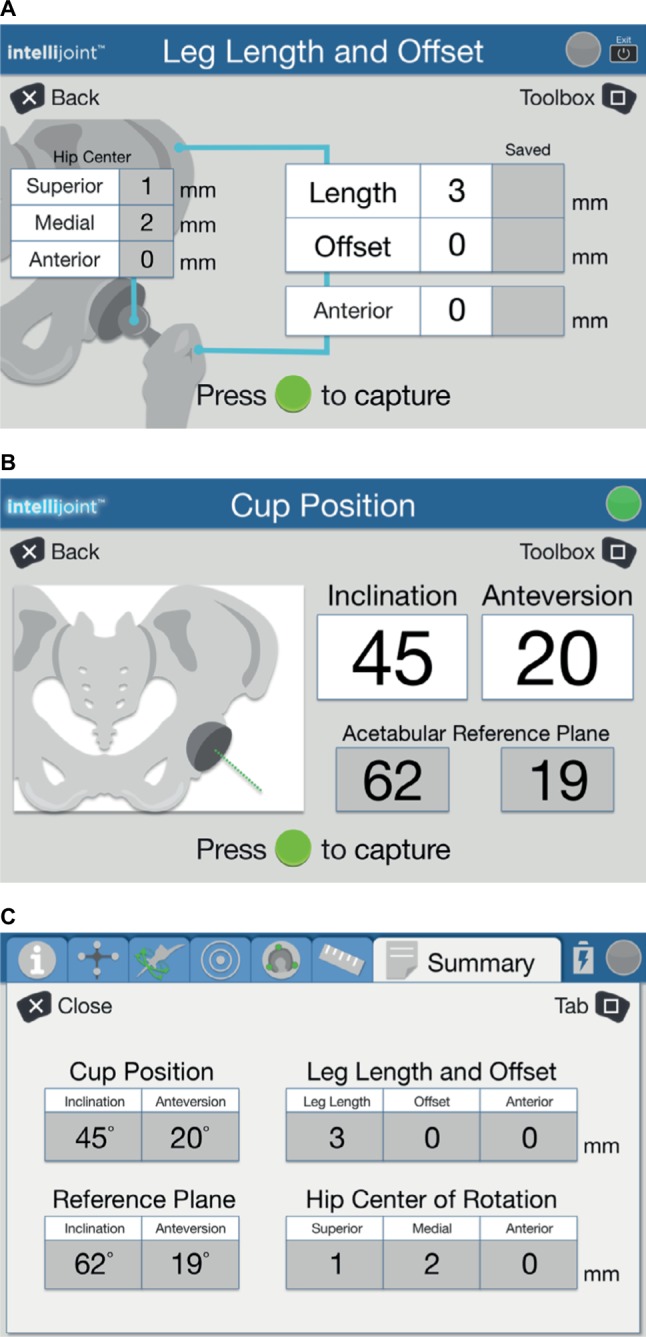
Representative images of the workstation screen indicating data provided to surgeons in real time.
Notes: Measurements of leg length and offset (A) and cup position (B) are displayed during trialing and once sizing is finalized. A summary page (C) displays all relevant data for review.
Indications and contraindications
The Intellijoint HIP navigation tool is indicated for use in orthopedic surgery procedures where the use of stereotactic surgical techniques is considered safe and effective, such as THA and minimally invasive hip arthroplasty. It is configured for use in THA performed via lateral and posterolateral surgical approaches using both traditional and minimally invasive techniques.
Specific contraindications include patients with severe osteoporosis, hip dislocation, or hip fracture. Surgeon discretion is advised under the following circumstances:
poor bone quality,
trochanteric osteotomy,
suspected or actual infection,
existing implanted hardware, or
severe deformities of the femoral or pelvic bone.
Validation testing
The accuracy of the Intellijoint HIP navigation tool has been evaluated in benchtop and simulated clinical use settings. Benchtop testing used precision phantoms developed to provide an accurate reference value for positional measurements, while simulated clinical use testing used Sawbones® phantoms and standard hip arthroplasty components.
Benchtop testing
Two precision benchtop phantoms (Thorlabs, Newton, New Jersey) were developed to provide accurate reference values for positional measurements: 1) To evaluate cup position (inclination and anteversion) and, 2) To evaluate leg length and offset measurements. All measurements were completed by a single observer in triplicate. Intraobserver reliability was evaluated using the intraclass correlation coefficient (ICC).29
For acetabular cup position testing, the phantom used angular positioning stages and precision fixtures to effect precise cup angles (Figure 4). Vertical and horizontal rotation stages were set at discrete angles that corresponded to impactor inclination and anteversion angles commonly observed during surgery. These angles were confirmed prior to testing using a calibrated electronic level and served as the target angles for validation testing. During testing, a precision flat plate and v-channel, mounted on the rotation stages, established the precise acetabular/implant and impactor planes, respectively. Testing involved using the probe function of the Intellijoint HIP navigation tool to localize 3 points on the precision flat plate to determine the acetabular reference plane and the acetabular implant face. The simulated cup impactor was then inserted into the v-channel to determine cup angle. Each measurement was performed bilaterally to simulate both left and right hips. A variety of inclination and anteversion angles were used to simulate cup positions likely to be encountered during surgery. Measurements were obtained for both the native acetabulum and the simulated cup and compared with the target values.
Figure 4.
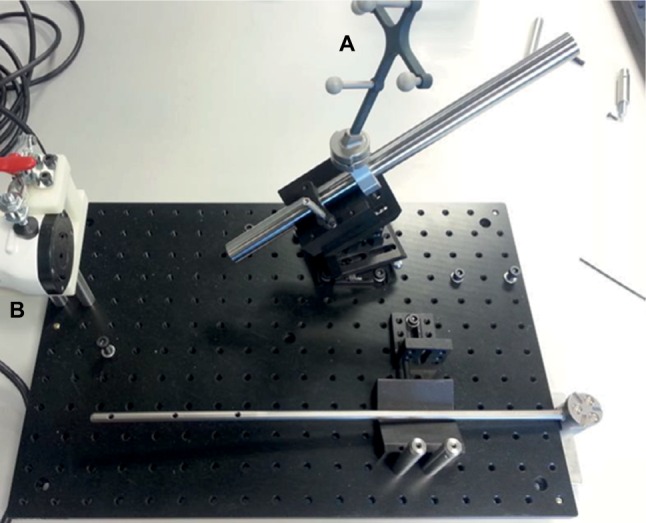
The acetabular benchtop phantom.
Notes: Discrete angles, confirmed by a calibrated electronic level, provide reference angles, which are then measured by the navigation tool. During testing, angles are computed from the movement of the tracker (A) captured by the camera (B).
Leg length and offset were tested using a separate phantom, used to simulate the pelvis and femur (Figure 5). Three precise micrometer positioning stages, verified using calibrated dial indicators, were mounted orthogonally to each other on each of the femoral and pelvic portions of the phantom. Acetabular micrometer positioning stages are used to generate hip center of rotation changes, while femoral positioning stages are used to generate leg length, offset, and anteroposterior distance changes. During testing, the camera was mounted on the pelvic portion of the phantom and the tracker was mounted on the femoral component. The phantom was set to 3 different configurations representing small, medium, and large pelvis sizes.30,31
Figure 5.
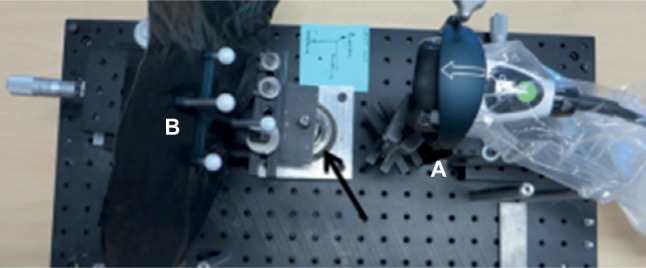
Benchtop phantom configured for leg length and offset testing.
Note: The camera (A) captures the position of the tracker (B) as it is moved about the simulated hip joint (arrow).
Simulated clinical use testing
Simulated clinical use testing was performed using Sawbones models, the anatomical phantom geometry of which was fully characterized prior to testing. Reference measurements were made prior to surgeon testing.
Five users, all licensed orthopedic surgeons, executed the normal device workflow on the anatomical phantom using standard hip arthroplasty instruments. Measurements of acetabular cup position (inclination and anteversion), leg length, and offset were recorded by the device and compared with the reference values calculated prior to testing. Each surgeon provided 8 separate measurements of each of the parameters, measuring parameters in both left and right hips for each of 4 commonly used femoral head components: –3.5, –5, 0, and 7 mm.
Statistical analysis
Alpha was set at 0.05 a priori for all statistical comparisons. Comparisons of mean values were performed using independent-samples t-tests. The values are presented as mean or mean (standard deviation [SD]).
Results
Benchtop testing
Intraobserver reliability was excellent (ICC =0.99). Inclination and anteversion reference values calculated prior to testing were 39.9° (SD: 16.1°) and 0° (SD: 14.5°), respectively. There was no statistically significant difference between the reference inclination angle and the inclination angles measured by the navigation tool for either the native acetabulum inclination angle (mean: 40.4° [SD: 16.1°]; p=0.83) or the simulated artificial cup inclination angle (mean: 40.9° [SD: 16.2°]; p=0.70). The mean difference between the reference inclination angle and that of the native acetabulum as measured by the navigation tool was 0.6° (SD: 0.3°), while the mean difference between the reference inclination and the simulated artificial cup angle was 1.0° (SD: 0.4°).
The mean anteversion angles measured for the native acetabulum (–0.1° [SD: 14.4°]) and the simulated cup (–0.02° [SD: 14.4°]) were not statistically different from the calculated reference anteversion (0° [SD: 14.5°]; p=0.98 and 0.99, respectively). The mean difference between the reference anteversion angle and the native acetabulum anteversion angle measured by the navigation tool was 0.4° (SD: 0.3°), while the mean difference between the reference anteversion and that of the simulated artificial cup was 0.6° (SD: 0.3°).
The mean difference in leg length measurements between the reference value and navigation tool measurements was 1.3 mm (SD: 1.3 mm), while for the offset, the mean difference was 0.5 mm (SD: 0.5 mm).
Simulated clinical use testing
The mean difference between the reference acetabular inclination angle and angles measured by the navigation tool are summarized in Table 1. Intellijoint HIP was able to measure both inclination and anteversion to within 0.8° of the native acetabulum.
Table 1.
Summary of the differences between the reference values and the values measured by the navigation tool
| Measure | Inclination
|
Anteversion
|
||
|---|---|---|---|---|
| Native acetabulum | Acetabular cup component | Native acetabulum | Acetabular cup component | |
| Mean difference | 0.8 | 1.1 | 0.8 | 1.6 |
| Standard deviation | 0.8 | 0.5 | 0.8 | 1.5 |
Leg length was measured by the navigation tool to within 0.8 mm (SD: 0.7 mm) of reference values, while the offset was measured to within 0.5 mm (SD: 0.4 mm) of reference values. There was no statistically significant difference between the reference value for the mean leg length differential (2.0 mm [SD: 3.9 mm]) and mean surgeon values (1.2 mm [SD: 3.6 mm]; p=0.66). Mean reference value for the offset was 6.9 mm (SD: 4.5 mm), while surgeon test values were a mean of 6.4 mm and SD of 4.4 mm (p=0.94).
Discussion
THA is a common orthopedic procedure associated with good results and a proven record of pain relief and restoration of mobility; however, up to 30% of patients report dissatisfaction following the procedure, often due to postsurgical discrepancies in leg length and offset.3,4 Additionally, errors in cup position can also predispose the patient to dislocation, thus increasing the rate of revision surgery.32 The lack of a cost-effective, easy-to-use, and accurate device for measuring biomechanical parameters during THA has been referred to as a procedural gap,33 one which exposes a substantial number of patients to inaccuracies in leg length, offset, and cup position. The Intellijoint HIP system represents a viable, reliable device for accurately determining these parameters intraoperatively and addresses the so-called procedural gap by offering a new, easy-to-use method for ensuring accuracy during THA.
Current methods of monitoring leg length, offset, and cup position are deficient. Traditional freehand methods are associated with LLDs of between 4 and 7 mm,34–36 discrepancies that are clinically significant, as postsurgical data indicate that patients can perceive an LLD of as little as 5 mm, and such a discrepancy can be associated with increased pain and decreased Oxford scores.37 Mechanical devices such as outriggers or calipers improve outcomes but still fall below the standard for success. Woolson et al38 used a caliper on the iliac crest to manage LLD and reported that 86% of patients achieved satisfactory results, although their threshold for success was a 6 -mm LLD. Ranawat and Rodriguez4 used a nail on the ischium as a reference point and reported that 87% of patients achieved successful results, but they too used a threshold of 6 mm. Jasty et al39 reported similar results with a caliper fixed to the iliac wing, using 5 mm as their threshold for success. While these mechanical methods provide improved results relative to freehand techniques, they are unable to provide results below the threshold of patient perception and do not address offset or cup position. By providing improved accuracy and decreasing the likelihood of a perceptible LLD, Intellijoint HIP has the potential to significantly improve patient-related outcomes and satisfaction relative to current manual methods, in addition to decreasing the need for postsurgical interventions such as heel lifts or rehabilitation.
Traditional computer-assisted surgery (CAS) navigation systems improve on accuracy and decrease the likelihood of detrimental LLDs; however, they do so at a significant cost and disruption of the normal surgical workflow. Lass et al40 compared CAS with freehand techniques and found that navigation was associated with a significant improvement in postsurgical anteversion and inclination in cup position but added 18.1 minutes (p=0.01) to the procedural time. Manzotti et al41 found similar results, noting improved accuracy but also a statistically significant increase in surgical duration with navigation (89.39 vs 73.17 minutes with freehand; p<0.001). In their study, a mean LLD of 5.06 mm in the navigation group was observed, as compared to 7.64 mm in the freehand group (p<0.0043). They also reported 5 patients with an LLD >10 mm in the navigation group, as opposed to 13 patients with LLD in the freehand group.
The accuracy findings mirror those of traditional navigation systems and show that the Intellijoint HIP surgical tool is effective at measuring leg length, offset, and cup position during THA. Benchtop evaluation of CAS systems has shown the ability of Intellijoint HIP to measure leg length to within 0.9–1.3 mm and offset to within 1.0–1.2 mm.42–44 The observation that the Intellijoint HIP navigation tool is able to provide equally accurate measurements in a system that is both user-friendly and associated with a significantly lower cost burden is an important finding. Indeed, the observations indicate that the navigation tool provides superior accuracy, measuring leg length and offset accurately to within <1 mm and cup position to within 1° in simulated use on Sawbones phantoms. This accuracy in a portable, easy-to-use device has the potential to provide surgeons with a simple and reliable method of improving outcomes in THA.
Clinical studies
Intellijoint HIP is currently the subject of clinical studies evaluating its safety and accuracy. The results from the first cohort of patients treated using this device demonstrated excellent accuracy when compared with radiographic measurements, with Intellijoint HIP able to measure changes in leg length to within 0.6 mm of radiographic values.45 Current studies include a randomized, controlled trial (clinicaltrials.gov identifier: NCT02095093) comparing the leg length and offset accuracy of Intellijoint HIP with a mechanical outrigger as well as a prospective, case–control study to evaluate the accuracy of the navigation tool in measuring cup position, leg length and offset.
Conclusion
The Intellijoint HIP 3D mini-optical navigation tool provides accurate data to surgeons in real time, allowing for improved accuracy and sizing of components during THA. While further research is needed to evaluate the potential of this innovative surgical tool, early results suggest that Intellijoint HIP provides a viable option for surgeons to improve accuracy during THA without altering surgical workflow or increasing procedural time.
Footnotes
Author contributions
JMM wrote the first draft of the manuscript. WGP provided critical review and revision. All authors contributed to conception and design, acquisition of data, or analysis and interpretation of data, read and approved the final manuscript and agree to be accountable for all aspects of the work.
Disclosure
WGP has received consultancy fees from and is a shareholder in Intellijoint Surgical, Inc. JMM is an employee of Intel-lijoint Surgical, Inc. The authors report no other conflicts of interest in this work.
References
- 1.Shan L, Shan B, Graham D, Saxena A. Total hip replacement: a systematic review and meta-analysis on mid-term quality of life. Osteoarthr Cartil. 2014;22(3):389–406. doi: 10.1016/j.joca.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A(5):963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Wylde V, Whitehouse SL, Taylor AH, Pattison GT, Bannister GC, Blom AW. Prevalence and functional impact of patient-perceived leg length discrepancy after hip replacement. Int Orthop. 2009;33(4):905–909. doi: 10.1007/s00264-008-0563-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ranawat CS, Rodriguez JA. Functional leg-length inequality following total hip arthroplasty. J Arthroplasty. 1997;12(4):359–364. doi: 10.1016/s0883-5403(97)90190-x. [DOI] [PubMed] [Google Scholar]
- 5.Sathappan SS, Ginat D, Patel V, Walsh M, Jaffe WL, Di Cesare PE. Effect of anesthesia type on limb length discrepancy after total hip arthroplasty. J Arthroplasty. 2008;23(2):203–209. doi: 10.1016/j.arth.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka R, Shigematsu M, Motooka T, Mawatari M, Hotokebuchi T. Factors influencing the improvement of gait ability after total hip arthroplasty. J Arthroplasty. 2010;25(6):982–985. doi: 10.1016/j.arth.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Robb C, Harris R, O’Dwyer K, Aslam N. Radiographic assessment of biomechanical parameters following hip resurfacing and cemented total hip arthroplasty. Hip Int. 2009;19(3):251–256. doi: 10.1177/112070000901900311. [DOI] [PubMed] [Google Scholar]
- 8.Foucher KC, Hurwitz DE, Wimmer MA. Relative importance of gait vs. joint positioning on hip contact forces after total hip replacement. J Orthop Res. 2009;27(12):1576–1582. doi: 10.1002/jor.20935. [DOI] [PubMed] [Google Scholar]
- 9.Rosler J, Perka C. The effect of anatomical positional relationships on kinetic parameters after total hip replacement. Int Orthop. 2000;24(1):23–27. doi: 10.1007/s002640050006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mihalko WM, Phillips MJ, Krackow KA. Acute sciatic and femoral neuritis following total hip arthroplasty. A case report. J Bone Joint Surg Am. 2001;83-A(4):589–592. doi: 10.2106/00004623-200104000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Ranawat CS. The pants too short, the leg too long! Orthopedics. 1999;22(9):845–846. doi: 10.3928/0147-7447-19990901-16. [DOI] [PubMed] [Google Scholar]
- 12.Danner D, Turner RH. Medical malpractice in revision hip surgery. In: Bono JV, McCarthy JC, Thornhill TS, Bierbaum BE, Turner RH, editors. Revision Total Hip Arthroplasty. New York: Springer; 1999. pp. 583–598. [Google Scholar]
- 13.Upadhyay A, York S, Macaulay W, McGrory B, Robbennolt J, Bal BS. Medical malpractice in hip and knee arthroplasty. J Arthroplasty. 2007;22(6 Suppl 2):2–7. doi: 10.1016/j.arth.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Sarin VK, Pratt WR, Bradley GW. Accurate femur repositioning is critical during intraoperative total hip arthroplasty length and offset assessment. J Arthroplasty. 2005;20(7):887–891. doi: 10.1016/j.arth.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Husby VS, Bjorgen S, Hoff J, Helgerud J, Benum P, Husby OS. Unilateral vs. bilateral total hip arthroplasty – the influence of medial femoral head offset and effects on strength and aerobic endurance capacity. Hip Int. 2010;20(2):204–214. doi: 10.1177/112070001002000211. [DOI] [PubMed] [Google Scholar]
- 16.Yamaguchi T, Naito M, Asayama I, Ishiko T. Total hip arthroplasty: the relationship between posterolateral reconstruction, abductor muscle strength, and femoral offset. J Orthop Surg (Hong Kong) 2004;12(2):164–167. doi: 10.1177/230949900401200205. [DOI] [PubMed] [Google Scholar]
- 17.Kiyama T, Naito M, Shinoda T, Maeyama A. Hip abductor strengths after total hip arthroplasty via the lateral and posterolateral approaches. J Arthroplasty. 2010;25(1):76–80. doi: 10.1016/j.arth.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Cassidy KA, Noticewala MS, Macaulay W, Lee JH, Geller JA. Effect of femoral offset on pain and function after total hip arthroplasty. J Arthroplasty. 2012;27(10):1863–1869. doi: 10.1016/j.arth.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Incavo SJ, Havener T, Benson E, McGrory BJ, Coughlin KM, Beynnon BD. Efforts to improve cementless femoral stems in THR: 2- to 5-year follow-up of a high-offset femoral stem with distal stem modification (Secur-Fit Plus) J Arthroplasty. 2004;19(1):61–67. doi: 10.1016/j.arth.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Crowe JF, Sculco TP, Kahn B. Revision total hip arthroplasty: hospital cost and reimbursement analysis. Clin Orthop Relat Res. 2003;413:175–182. doi: 10.1097/01.blo.0000072469.32680.b6. [DOI] [PubMed] [Google Scholar]
- 21.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1):128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 22.Vanhegan IS, Malik AK, Jayakumar P, Ul Islam S, Haddad FS. A financial analysis of revision hip arthroplasty: the economic burden in relation to the national tariff. J Bone Joint Surg Br. 2012;94(5):619–623. doi: 10.1302/0301-620X.94B5.27073. [DOI] [PubMed] [Google Scholar]
- 23.Dong H, Buxton M. Early assessment of the likely cost-effectiveness of a new technology: a Markov model with probabilistic sensitivity analysis of computer-assisted total knee replacement. Int J Technol Assess Health Care. 2006;22(2):191–202. doi: 10.1017/S0266462306051014. [DOI] [PubMed] [Google Scholar]
- 24.Desai AS, Dramis A, Kendoff D, Board TN. Critical review of the current practice for computer-assisted navigation in total knee replacement surgery: cost-effectiveness and clinical outcome. Curr Rev Musculoskelet Med. 2011;4(1):11–15. doi: 10.1007/s12178-011-9071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu K, Li YM, Zhang HF, Wang CG, Xu YQ, Li ZJ. Computer navigation in total hip arthroplasty: a meta-analysis of randomized controlled trials. Int J Surg. 2014;12(5):528–533. doi: 10.1016/j.ijsu.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 26.Jassim SS, Benjamin-Laing H, Douglas SL, Haddad FS. Robotic and navigation systems in orthopaedic surgery: How much do our patients understand? [Accessed August 15, 2016];Clin Orthop Surg. 2014 6(4):462–467. doi: 10.4055/cios.2014.6.4.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hemel Hampstead: National Joint Registry; c2008-2014. [Accessed August 15, 2016]. Available from: www.njrcentre.org.uk.
- 28.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75(2):228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 29.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 30.Krebs V, Incave SJ, Shields WH. The anatomy of the acetabulum: What is normal? Clin Orthop Relat Res. 2009;467(4):868–875. doi: 10.1007/s11999-008-0317-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Theivendran K, Hart WJ. Is the tip of the greater trochanter a reliable reference for the rotation centre of the femoral head in total hip arthroplasty? Acta Orthop Belg. 2009;75(4):472–476. [PubMed] [Google Scholar]
- 32.Dargel J, Oppermann J, Bruggemann GP, Eysel P. Dislocation following total hip replacement. Dtsch Arztebl Int. 2014;111(51–52):884–890. doi: 10.3238/arztebl.2014.0884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gross AE, Muir JM. Identifying the procedural gap and improved methods for maintaining accuracy during total hip arthroplasty. Med Hypotheses. 2016;94:93–98. doi: 10.1016/j.mehy.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 34.Matsuda K, Nakamura S, Matsushita T. A simple method to minimize limb-length discrepancy after hip arthroplasty. Acta Orthop. 2006;77(3):375–379. doi: 10.1080/17453670610046280. [DOI] [PubMed] [Google Scholar]
- 35.Barbier O, Ollat D, Versier G. Interest of an intraoperative limb-length and offset measurement device in total hip arthroplasty. Orthop Traumatol Surg Res. 2012;98(4):398–404. doi: 10.1016/j.otsr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 36.Takigami I, Itokazu M, Itoh Y, Matsumoto K, Yamamoto T, Shimizu K. Limb-length measurement in total hip arthroplasty using a calipers dual pin retractor. Bull NYU Hosp Jt Dis. 2008;66(2):107–110. [PubMed] [Google Scholar]
- 37.Sykes A, Hill J, Orr J, et al. Patients’ perception of leg length discrepancy post total hip arthroplasty. Hip Int. 2015;25(5):452–456. doi: 10.5301/hipint.5000276. [DOI] [PubMed] [Google Scholar]
- 38.Woolson ST, Hartford JM, Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14(2):159–164. doi: 10.1016/s0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]
- 39.Jasty M, Webster W, Harris W. Management of limb length inequality during total hip replacement. Clin Orthop Relat Res. 1996;333:165–171. [PubMed] [Google Scholar]
- 40.Lass R, Kubista B, Olischar B, Frantal S, Windhager R, Giurea A. Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplasty. 2014;29(4):786–791. doi: 10.1016/j.arth.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 41.Manzotti A, Cerveri P, De Momi E, Pullen C, Confalonieri N. Does computer-assisted surgery benefit leg length restoration in total hip replacement? Navigation versus conventional freehand. Int Orthop. 2011;35(1):19–24. doi: 10.1007/s00264-009-0903-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Renkawitz T, Gneiting S, Schaumburger J, et al. In-vitro investigation of a noninvasive referencing technology for computer-assisted total hip arthroplasty. Orthopedics. 2010;33(4) doi: 10.3928/01477447-20100225-10. [DOI] [PubMed] [Google Scholar]
- 43.Renkawitz T, Sendtner E, Grifka J, Kalteis T. Accuracy of imageless stem navigation during simulated total hip arthroplasty. Acta Orthop. 2008;79(6):785–788. doi: 10.1080/17453670810016858. [DOI] [PubMed] [Google Scholar]
- 44.Renkawitz T, Wegner M, Gneiting S, et al. Experimental validation of a pinless femoral reference array for computer-assisted hip arthroplasty. J Orthop Res. 2010;28(5):583–588. doi: 10.1002/jor.21039. [DOI] [PubMed] [Google Scholar]
- 45.Grosso P, Snider M, Muir JM. A smart tool for intraoperative leg length targeting in total hip arthroplasty: a retrospective cohort study. Open Orthop J. 2016;10:490–499. doi: 10.2174/1874325001610010490. [DOI] [PMC free article] [PubMed] [Google Scholar]


