Abstract
Objective
To determine whether an Acceptance-Based Behavioral Intervention (ABBI) produces better weight losses than standard behavioral treatment (SBT) among individuals reporting high internal disinhibition.
Methods
Participants were 162 adults with overweight or obesity (mean BMI 37.6) randomly assigned to ABBI or SBT. Both interventions provided the same calorie intake target, exercise goal, and self-monitoring skills training. SBT incorporated current best practice interventions for addressing problematic thoughts and emotions. ABBI utilized acceptance-based techniques based on Acceptance and Commitment Therapy. ABBI and SBT were compared on weight change and internal disinhibition change over 24 months.
Results
Mixed models analysis showed mean weight loss at 24 months was −4.1% (SE=0.88) for ABBI and −2.4% (SE=0.87) for SBT (p=.204). Secondary analyses showed that the ABBI group regained less weight from the end of treatment to the final follow-up (4.6 vs. 7.1kg; p=.005), and that a significantly higher proportion of ABBI participants achieved a 5% weight loss (38% vs. 25%; p=.038) at 24 months.
Conclusions
Results suggest that ABBI could be helpful for improving the maintenance of weight loss for individuals who report high internal disinhibition.
Keywords: obesity, weight loss, randomized trial, disinhibition, acceptance, mindfulness
Introduction
Behavioral weight loss programs consistently produce an average weight loss of approximately 7–10%; typically resulting in significant health improvements1,2. However, most individuals achieve maximum weight loss between 6–9 months and gradually regain weight thereafter3–6. Attempts have been made to improve the diet and exercise components (e.g. dose of exercise7, macronutrient composition of diet8) and delivery aspects (e.g. treatment length9, technological additions10, non-interventionist involvement11, incentives12) of behavioral interventions. While providing extended-care has demonstrated the ability to delay weight regain following initial treatment9, the pattern of regain remains consistent, suggesting that novel strategies are needed.
The core components included in standard behavioral weight loss interventions have gone largely unchanged for the past 40 years. Standard interventions typically include cognitive and emotional control strategies (e.g. thought replacement, distraction, relaxation) to support weight loss efforts13. However excessive attempts to change or control thoughts, feelings, or bodily sensations, referred to as experiential avoidance14, is known to contribute to a wide range of mental and chronic health problems15. Consistent with the literature on experiential avoidance, recent studies suggest that cognitive and emotional control-focused strategies could paradoxically make it more difficult for individuals with obesity to cope with food cravings and instead lead to greater caloric consumption16,17. Alternative treatment components may be necessary to help individuals cope with situations that can interfere with successful weight loss maintenance.
Acceptance-based approaches (e.g. Acceptance and Commitment Therapy; ACT)18 may provide a viable alternative. ACT uses acceptance and mindfulness strategies to increase patterns of values-consistent behavior and reduce experiential avoidance18. ACT interventions have been shown to reduce binge eating19, enhance coping with food cravings20, improve diabetes management21, and ameliorate a range of mental health problems15.
Pilot studies have demonstrated that ACT strategies could also be helpful for weight loss22–24 and maintenance25. The only randomized trial comparing an acceptance-based intervention to a standard behavioral treatment (SBT) found that both groups produced significant, but equivalent, weight loss at 18 months26. However post-hoc analyses suggested that the acceptance-based approach produced greater weight loss among participants who reported high baseline levels of emotional eating or disinhibition, suggesting a potential target population for acceptance-based interventions.
Niemeier and colleagues27 recently conducted a new factor analysis of the disinhibition scale of the Eating Inventory28 and found that it was best represented by two factors: internal disinhibition (ID), or the tendency to eat in response to cognitive or emotional cues, and external disinhibition, which is eating in response to environmental cues27. Both lower baseline levels of ID27 and greater reductions in ID early in weight loss treatment29 predicted better weight loss outcomes at 18-months and 12-months (no effect found for external disinhibition). Niemeier and colleagues30 then conducted an open trial assessing the impact of a combined SBT + ACT intervention on weight loss in 21 adults with obesity and high ID. They reported a higher then normal average weight loss of 12.0 kg after 6 months of treatment that was maintained over 3 months. While this study suggested that an ACT-enhanced weight management intervention might be particularly effective for individuals who report high ID, the study was limited by small sample size and lack of a comparison group, necessitating further study.
The current study was a randomized controlled trial comparing SBT to an acceptance-based behavioral intervention (ABBI) that combined standard behavioral strategies with techniques from ACT for weight loss in individuals with obesity who report high ID. We hypothesized that participants in the ABBI condition would experience larger weight losses at 24 months compared to those in SBT, that differences in weight would be due in part to better weight loss maintenance in ABBI, and that the ABBI condition would report greater reductions in ID.
Methods
Design
The study was a randomized controlled trial of 162 participants who were allocated in a 1:1 ratio, stratified by gender, to one of two treatment conditions: (1) Acceptance-Based Behavioral Intervention (ABBI), or, (2) Standard Behavioral Treatment (SBT). The intervention lasted one year. Groups met weekly during months 1–6, then bi-weekly (every other week) during months 6–9, and then monthly during months 9–12, for a total of 32 sessions of continuous treatment over 12 months. There was no treatment contact between month 12 and the final assessment at month 24. Assessments occurred at baseline, 6, 12, 18, and 24 months. Research staff members who were blinded to condition assignment administered all assessments. All study activities were conducted at the Weight Control and Diabetes Research in Rhode Island, United States. The Miriam Hospital IRB approved all study procedures.
Participants
Inclusion Criteria
Included participants were 18–70 years of age, had a body mass index (BMIs) between 30–50 kg/m2, and a score of 5 or higher (women) or 4 or higher (men) on the ID subscale of the Eating Inventory (a detailed description of the screening process and establishment of the ID cutoff can be found in the study protocol.31).
Exclusion Criteria
Participants were excluded for current participation in another weight loss program; current pregnancy or plans to become pregnant during the study period; reported heart condition, chest pain or inability to exercise; reported conditions that would render them unlikely to follow the protocol, including terminal illness, plans to relocate, a history of substance abuse, or a recent psychiatric hospitalization.
Recruitment and screening
Participants were self-referred via newspaper ads and direct mailings and completed a phone screen that assessed BMI and obtained responses to the ID subscale of the Eating Inventory. Potential participants were required to attend an in-person group orientation session, and complete a 7-day food diary trial and subsequent baseline assessment prior to randomization.
Interventions
The intervention was delivered in a 1-hour, group format (15–16 participants per group). The groups were run by co-leader pairs, which include a mix of Ph.D. psychologists, Ph.D. exercise physiologists, and master’s level nutritionists. Each leader pair was responsible for running a matched number of groups in both conditions in order to counterbalance leader effects. All group leaders had training and experience running standard behavioral weight loss interventions. Experience with acceptance-based interventions varied from novice to expert; thus, all group leaders received a 2-day training in acceptance-based interventions and met for weekly supervision with one of the study co-investigators. See Table 1 for a summary of treatment elements (a more detailed description of the intervention can be found in the published study protocol31).
Table 1.
Comparison of intervention elements
| Shared Components | Core behavioral strategies
|
| Standard Behavioral only | Cognitive and emotional control strategies
|
| Acceptance-based Behavioral only | Acceptance and mindfulness strategies
|
Measures
Anthropometric
Weight was measured to the nearest 0.1 kg using a digital scale and height was measured to the nearest millimeter with a stadiometer, using standardized procedures, and used to calculate BMI (kg/m2).
Eating Inventory
The Eating Inventory is a widely used measure of eating behavior that includes three subscales, cognitive restraint, disinhibition, and hunger28 (higher scores indicate greater endorsement of each). The disinhibition scale is divided into two subscales, internal and external disinhibition. An example of an internal disinhibition item is the following true/false question: “When I feel anxious, I find myself eating.” The Eating Inventory has demonstrated adequate internal consistency, test-retest reliability, and sensitivity to change32,33.
Treatment Fidelity Form
All treatment sessions were audio recorded and a randomly selected 20% were scored for treatment fidelity (20% of which were double coded). A 6-item measure of treatment fidelity was created for the study and completed by trained PhD level raters who were blinded to condition. This measure assessed for the presence of shared elements (e.g. behavioral goals), acceptance-based strategies (ABBI only), and cognitive or emotional change strategies (SBT only), as well as an overall assessment of the condition being presented.
Statistical analysis
All analyses were completed using IBM SPSS Statistics software version 22 for Mac in 2016. This trial was designed to detect a mean difference of approximately 4 kg at the study endpoint with 160 participants and no greater than 20% attrition. Differences in baseline characteristics between groups were analyzed using t-test and Χ2.
Treatment adherence was examined by calculating mean attendance and mean percentage of diaries completed (assuming non-completion of diaries when treatment sessions were not attended and/or diaries were not returned). Treatment fidelity was examined using descriptive data from the Treatment Fidelity Form and also by calculating an intraclass correlation coefficient for double coded sessions.
The primary outcome was percent weight change at 24 months. The effect of the two interventions was compared using linear and nonlinear mixed models. As a first step, unconditional models were used to determine whether a linear or nonlinear trend best fit the longitudinal trajectory of the outcomes (nonlinear was a better fit for the full study weight analysis, linear was better for all other analyses), and to evaluate the variance components associated with the slope of time to determine assignment as fixed versus random effects (intercepts and slopes were treated as random effects in all models). In a second step, treatment condition and the interaction between treatment condition and the slope of time were added to the conditional model in order to account for variability in the trajectory of outcomes. The unit of time was represented as months from baseline. All significance tests were two-tailed, with alpha set to .05. Estimated marginal means and standard errors for changes in study variables were calculated using the linear mixed modeling procedure described above. The analytic approach accommodated missing data by making use of all available data from all randomized participants.
Secondary analyses were conducted to examine differences between groups in weight regain. We utilized the same linear mixed modeling procedure described above looking separately at weight change during the treatment phase (0–12 months) and the maintenance phase (12–24 months), adding percent weight change during treatment as a covariate. We also calculated the proportion of participants achieving clinically meaningful weight losses of at least 5 and 10% of initial body weight at the end of treatment (12 months) and the final assessment (24 months). Participants with missing data were assumed not to have achieved clinically meaningful weight losses. We performed chi square analyses to test for differences between groups achieving 5 and 10% weight loss at the 12 and 24 months.
Between groups differences on change in ID were examined using the same mixed modeling procedure described above. Bivariate correlations were calculated to examine the association between ID change and weight change.
Results
Enrollment and Retention
A total of 748 potential participants contacted the WCDRC for information about the study. Of those, 162 were randomized after being found eligible and completing all pre-randomization study procedures. Participants who stopped attending treatment sessions continued to be followed/contacted for assessment. See Figure 1 for details on participant flow.
Figure 1.
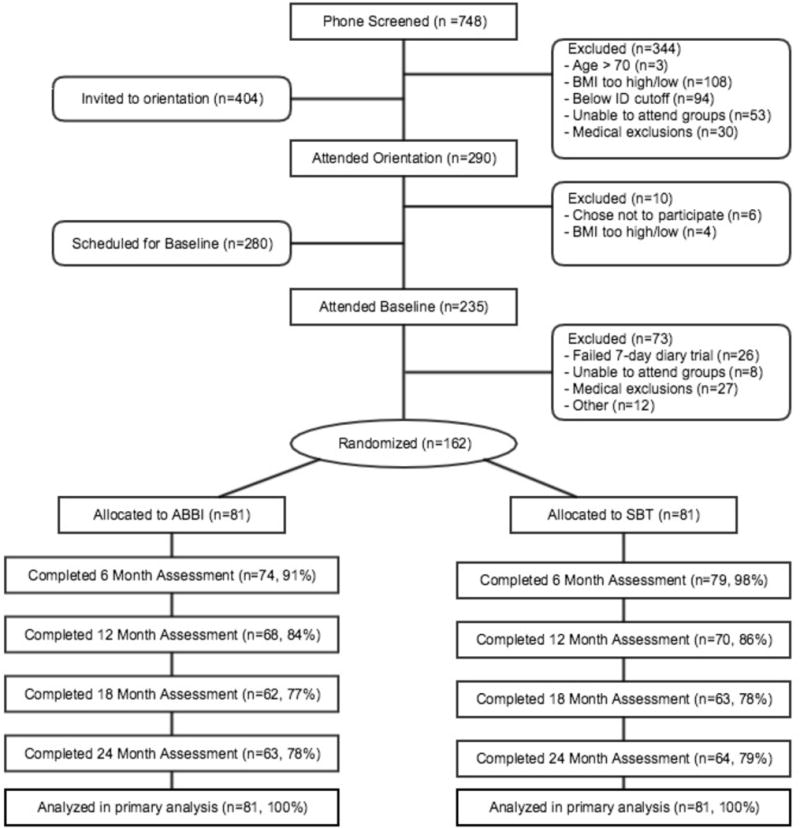
Participant Flow
Baseline Characteristics
The sample was predominantly middle-aged, Caucasian, and female: Table 2 presents the baseline characteristics of participants in the ABBI and SBT groups. There were no significant differences between groups at baseline on any study variable.
Table 2.
Baseline characteristics of participants
| Characteristics | ABBI (N=81) | SBT (N=81) | Total (N=162) |
|---|---|---|---|
| Sex, N (%) | |||
| Female | 69 (85%) | 69 (85%) | 138 (85%) |
| Male | 12 (15%) | 12 (15%) | 24 (12%) |
| Race/ethnicity, N (%) | |||
| Black/African American | 6 (7.5%) | 2 (2.5%) | 8 (5%) |
| Hispanic | 5 (6%) | 5 (6%) | 10 (6%) |
| Asian | 2 (2.5%) | 0 (0%) | 2 (1%) |
| Caucasian (Non-Hispanic) | 68 (84%) | 74 (91.5%) | 142 (88%) |
| Education, N (%) | |||
| High School/G.E.D. | 6 (7%) | 6 (7%) | 12 (7.5%) |
| Some college/Vocational | 24 (30%) | 20 (25%) | 44 (28%) |
| Bachelor’s degree | 29 (37%) | 29 (37%) | 58 (36.5%) |
| Graduate or professional | 21 (26%) | 24 (31%) | 45 (28%) |
| Age (year) | 50.7 ± 11.3 | 49.8 ± 10.7 | 50.2 ± 10.9 |
| Weight (kg) | 102.5 ± 17.3 | 102.2 ± 17.7 | 102.3 ± 17.4 |
| BMI (kg/m2) | 37.5 ± 5.4 | 37.7 ± 5.3 | 37.6 ± 5.3 |
| Internal Disinhibition | 6.2 ± 1.5 | 6.1 ± 1.6 | 6.2 ± 1.6 |
Values shown are mean ± standard deviation
Treatment Adherence
Mean number of sessions attended was 28.5/32 (89%) for ABBI and 28.7/32 (89%) for SBT. Treatment completion for both groups was 74% (at least 70% of sessions attended and continued attendance throughout the 12 months). Average weekly food and exercise diary completion was 60% for ABBI and 61% for SBT.
Treatment Fidelity
The correct condition was identified in 69 of 70 coded treatment sessions. Core, shared elements were present in 96% of coded sessions, while contraindicated elements were present in 4%. For double coded sessions, the intraclass correlation coefficient was .92 and there was 100% agreement between coders for identifying study condition.
Weight Change
Table 3 presents the changes in weight. At month 24, participants in the ABBI condition had a mean weight change of −4.1% (SE=0.88) compared to −2.4% (SE=0.87; p=.204) for SBT participants (−4.3 vs −2.6 kg). Although overall weight change at month 24 did not differ between groups, the time by condition interaction in the model approached significance (p=.067). Thus, we conducted secondary analyses to compare the weight changes in ABBI versus SBT (a) during the intervention phase (0–12 months), and, (b) during post-treatment follow-up phase (12–24 months). The interaction was not significant during the treatment phase (p=.680), but there was a significant time by condition interaction (p=.005) during the post-treatment phase, where participants in the ABBI condition gained an average of 4.6 kg versus 7.1 kg for SBT participants.
Table 3.
Estimated marginal means, standard errors, and p values for between groups differences for changes in weight and internal disinhibition from baseline to 6, 12, 18, and 24 month
| Month | ABBI | SE | SBT | SE | p |
|---|---|---|---|---|---|
| Percent Weight Change | |||||
| 6 | −8.71 | 0.69 | −9.28 | 0.68 | 0.55 |
| 12 | −8.52 | 0.97 | −9.31 | 0.96 | 0.51 |
| 18 | −6.97 | 0.99 | −7.04 | 0.97 | 0.89 |
| 24 | −4.16 | 0.88 | −2.47 | 0.87 | 0.20 |
| Weight Change in KG | |||||
| 6 | −9.04 | 0.76 | −9.57 | 0.75 | 0.62 |
| 12 | −8.92 | 1.05 | −9.70 | 1.03 | 0.55 |
| 18 | −7.30 | 1.04 | −7.40 | 1.03 | 0.89 |
| 24 | −4.29 | 0.89 | −2.65 | 0.88 | 0.22 |
| Internal Disinhibition Change | |||||
| 6 | −2.73 | 0.24 | −2.50 | 0.23 | 0.48 |
| 12 | −2.41 | 0.21 | −2.15 | 0.21 | 0.36 |
| 18 | −2.10 | 0.22 | −1.79 | 0.22 | 0.33 |
| 24 | −1.78 | 0.26 | −1.44 | 0.26 | 0.36 |
Clinical Cutoffs
We also examined the percentage of participants meeting meaningful clinical weight loss cutoffs (5% and 10%) at both post-treatment (12 months) and the study endpoint (24 months). At 12 months, 53% of ABBI and 55% of SBT participants had a weight loss of at least 5% (p=.899), while 31% of ABBI and 37% of SBT participants had a weight loss of at least 10% of their baseline weight (p=.464). At 24 months, 38% of ABBI and 25% of SBT participants had a weight loss of at least 5% (p=.038), while 22% of ABBI and 12% of SBT participants had a weight loss of at least 10% of their baseline weight (p=.078).
Internal Disinhibition
Table 3 presents the mean changes in ID. Internal disinhibition decreased significantly over time (Time variable, p<.001), but the changes did not differ by condition (Time × Condition interaction, p=.777). Although the largest reductions in ID occurred during treatment, at 24 months both groups had lower ID scores than at baseline. Changes in ID from baseline were significantly correlated (all P-values <0.01) with changes in weight in both conditions at 6 months (r=.52 in ABBI and r=.37 in SBT) and 12 months (r=.50 in ABBI and .53 in SBT); at 18 and 24 months ID change was significantly correlated with weight change in the ABBI group (r=.25, r=.28 respectively, p’s<0.05) but was not significantly correlated with weight change in the SBT group (r=−.07, r=.18 respectively, p’s=NS).
Discussion
This study compared the effect of a standard behavioral weight management intervention to an intervention that incorporated both standard behavioral and acceptance-based techniques on 24-month weight loss using a sample of individuals selected for high internal disinhibition. Overall there were no significant differences in mean weight loss between groups at 24 months. This result is consistent with the only other randomized trial comparing an acceptance-based intervention with a standard behavioral intervention26. Secondary analyses, however, demonstrated that participants in the ABBI group regained significantly less weight during the post-treatment phase compared to those in the SBT condition. In addition, a higher proportion of ABBI participants achieved clinically meaningful weight losses of >5% at 24 months. Taken together, results suggest that ABBI had a positive impact on weight outcomes by reducing the magnitude of weight regain after treatment ended. These results are consistent with a previous randomized trial that showed improved weight loss maintenance for individuals receiving an acceptance-based intervention25.
It appeared that the differential impact of ABBI was strongest between 18–24 months, well after treatment ended. Previous studies testing methods from ACT have demonstrated between group differences that occur after treatment had been discontinued. For example, Gifford and colleagues34 found no differences in smoking cessation quit rates between ACT and nicotine replacement therapy at post-treatment; however there were significant differences at both 6 and 12 months after treatment ended, with the percentage of ACT participants quitting increasing during the final follow up assessment period. Current ACT theory suggests that successful ACT increases psychological flexibility, or the ability to take action consistent with one’s values in the face of difficult cognitive and emotional barriers. This functionally based skill set should help participants meet new challenges without interventionist assistance. The results of the current study are consistent with ACT theory and are encouraging given that weight regain after treatment termination continues to be the biggest problem with behavioral weight loss interventions. However it should be noted that, on average, the ABBI group still regained a significant amount of weight during the post-treatment phase.
In a prior study26, post hoc analyses suggested that the beneficial effects of ACT might be most apparent in those with high emotional eating or high disinhibition. Given that participants in the current study were selected for high ID, it cannot be determined whether ABBI was particularly beneficial for this subgroup. However, the trend for better maintenance of weight loss in ABBI occurred within this subgroup. Moreover, both ABBI and SBT led to significant reductions in ID, with no significant difference between the two approaches. The changes observed in ID were consistent with a previous open trial testing an acceptance-based intervention, which found significant mean reductions in ID after a 3 month intervention (−2.6) and at 6 months (−2.1)30. The correlation pattern in the current study indicated that changes in ID were related to changes in weight in both groups during treatment. However after treatment was discontinued changes in ID were related to weight change only in the ABBI group.
The results of this trial point to gaps in our current understanding of the potential role of acceptance-based strategies in weight management. In the current study and a previous randomized controlled trial, acceptance-based strategies did not improve weight loss during treatment. It is possible that these strategies do not add utility in the weight loss phase, or perhaps that they are weakly targeted when integrated with an already demanding core of strategies found in standard behavioral interventions. Another possibility is that structural aspects of the study limited the impact of ABBI. The average group size in the current study was larger than typical ACT intervention studies, while the session length was shorter15. ACT experiential exercises and metaphors are interactive and build on each other, and it is possible that a traditional weight loss intervention structure does not allow for adequate time to cover content and adequately engage all group members. Despite these potential conflicts, acceptance-based strategies seem to have the potential to improve weight loss maintenance. Perhaps a targeted weight loss maintenance program, focusing solely on acceptance-based strategies and administered after an initial weight loss intervention, might have a greater impact on long-term outcomes. Future research is needed to explore this possibility.
This study had many strengths, including a randomized design, a gold standard comparison group, objective measurement of weight, blinded assessors, and the recruitment of a sample of individuals who typically demonstrate poor response to treatment. This study targeted perhaps the biggest problem in behavioral weight loss, long-term maintenance, and tested a novel intervention incorporating innovative acceptance-based strategies that theoretically target barriers to maintenance.
The study also had limitations. The sample was primarily middle-aged, Caucasian women, limiting the generalizability of the findings. In addition, ID was assessed via a self-report measure, which was subject to the same potential biases as all self-report measures. It is unknown whether ID would decrease over time (regression to the mean) in the absence of any treatment. Although the training of therapist pairs was standardized, the study did not include an assessment of therapist skill. Finally, treatment fidelity focused only on interventionist adherence to the protocol and did not assess other aspects of treatment fidelity.
In conclusion, the results of the current study suggested that an intervention combining acceptance-based strategies with standard behavioral strategies might benefit individuals who report high ID by reducing the rate of weight regain after treatment is discontinued. Both standard behavioral and acceptance-based approaches appeared effective at reducing ID. Future research needs to replicate this finding, examine the mechanisms of change, and further explore the most effective use of acceptance-based strategies for improving weight control.
What is already known about this subject?
Cognitive and emotional factors play a role in poor adherence to weight loss intervention, and emotional and cognitive control strategies may be ineffective for addressing these factors.
Pilot studies have shown that acceptance-based methods could be helpful for improving weight loss or maintenance.
The only published randomized trial testing acceptance-based methods combined with standard behavioral weight loss strategies for 18-month weight loss showed no differences in comparison to a gold standard behavioral intervention, however secondary analyses showed that acceptance-base strategies were better for specific subgroups.
What does this study add?
An additional, large scale, randomized trial testing the efficacy of acceptance-based methods in an area of growing interest with very little published clinical trial data.
Results suggesting that acceptance-based methods may be more useful for weight loss maintenance.
Results suggesting that acceptance-based strategies might contribute to a higher proportion of clinically significant weight loss.
Acknowledgments
Funding: This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK087704).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.MacLean PS, Wing RR, Davidson T, et al. NIH Working Group Report: Innovative Research to Improve Maintenance of Weight Loss. Obesity. 2015;23:7–15. doi: 10.1002/oby.20967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butryn ML, Webb V, Wadden TA. Behavioral Treatment of Obesity. Psychiatric Clinics of North America. 2011;34:841–+. doi: 10.1016/j.psc.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loveman E, Frampton GK, Shepherd J, et al. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: a systematic review. Health Technology Assessment. 2011;15:1–+. doi: 10.3310/hta15020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeffery RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: Current status. Health Psychology. 2000;19:5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- 5.Perri MG. The maintenance of treatment effects in the long-term management of obesity. Clinical Psychology-Science and Practice. 1998;5:526–43. [Google Scholar]
- 6.Barte JCM, ter Bogt NCW, Bogers RP, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obesity Reviews. 2010;11:899–906. doi: 10.1111/j.1467-789X.2010.00740.x. [DOI] [PubMed] [Google Scholar]
- 7.Jakicic J, Wing R, Winters C. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women. Journal of the American Medical Association. 1999;282:1554–60. doi: 10.1001/jama.282.16.1554. [DOI] [PubMed] [Google Scholar]
- 8.Wadden T, Stunkard A, Liebschutz J. Three year follow-up of the treatment of obesity by very-low-calorie diet, behavior therapy, and their combination. Journal of Consulting and Clinical Psychology. 1988;56:925–8. doi: 10.1037//0022-006x.56.6.925. [DOI] [PubMed] [Google Scholar]
- 9.Middleton KMR, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obesity Reviews. 2012;13:509–17. doi: 10.1111/j.1467-789X.2011.00972.x. [DOI] [PubMed] [Google Scholar]
- 10.Wang J, Sereika SM, Chasens ER, Ewing LJ, Matthews JT, Burke LE. Effect of adherence to self-monitoring of diet and physical activity on weight loss in a technology-supported behavioral intervention. Patient Preference and Adherence. 2012;6:221–6. doi: 10.2147/PPA.S28889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murphy JK, Williamson DA, Buxton AE, Moody SC, Absher N, Warner M. The long-term effects of spouse involvement upon weight loss and maintenance. Behavrio Therapy. 1982;13:681–93. [Google Scholar]
- 12.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial Incentive-Based Approaches for Weight Loss A Randomized Trial. Jama-Journal of the American Medical Association. 2008;300:2631–7. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diabetes Prevention Program Research Group. The Diabetes Prevention Program: Description of the Lifestyle Intervention. Diabetes care. 2002;25:2165–71. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hayes SC, Strosahl K, Wilson KG, et al. Measuring experiential avoidance: A preliminary test of a working model. Psychological Record. 2004;54:553–78. [Google Scholar]
- 15.Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Forman EM, Hoffman KL, McGrath KB, Herbert JD, Brandsma LL, Lowe MR. A comparison of acceptance- and control-based strategies for coping with food cravings: an analog study. Behav Res Ther. 2007;45:2372–86. doi: 10.1016/j.brat.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 17.Hoffman KL, Forman EM, Herbert JD, et al. Comparison of acceptance-based and standard cognitive-based coping strategies for craving sweets in overweight and obese women. In: Herbert (Chair) J, editor. Cognitive Reappraisal vs Experiential Acceptance; 43rd Annual Convention of the Association for Behavioral and Cognitive Therapies; New York, NY. 2009. [Google Scholar]
- 18.Hayes SC, Strosahl K, Wilson KG. Acceptance and Commitment Therapy: An experiential approach to behavior change. New York: The Guilford Press; 1999. [Google Scholar]
- 19.Lillis J, Hayes SC, Levin ME. Binge Eating and Weight Control: The Role of Experiential Avoidance. Behavior Modification. 2011;35:252–64. doi: 10.1177/0145445510397178. [DOI] [PubMed] [Google Scholar]
- 20.Hooper N, Sandoz EK, Ashton J, Clarke A, McHugh L. Comparing thought suppression and acceptance as coping techniques for food cravings. Eating Behaviors. 2012;13:62–4. doi: 10.1016/j.eatbeh.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Gregg JA, Callaghan GA, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2007;75:336–43. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- 22.Forman EM, Butryn ML, Hoffman KL, Herbert JD. An open trial of an acceptance-based behavioral intervention for weight loss. Cognitive and Behavioral Practice. 2009;16:223–35. [Google Scholar]
- 23.Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite. 2009;52:396–404. doi: 10.1016/j.appet.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 24.Goodwin CL, Forman EM, Herbert JD, Butryn ML, Ledley GS. A Pilot Study Examining the Initial Effectiveness of a Brief Acceptance-Based Behavior Therapy for Modifying Diet and Physical Activity Among Cardiac Patients. Behavior Modification. 2012;36:199–217. doi: 10.1177/0145445511427770. [DOI] [PubMed] [Google Scholar]
- 25.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: A preliminary test of a theoretical model. Annals of Behavioral Medicine. 2009;37:58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- 26.Forman EM, Butryn ML, Juarascio AS, et al. The Mind Your Health Project: A Randomized Controlled Trial of an Innovative Behavioral Treatment for Obesity. Obesity. 2013;21:1119–26. doi: 10.1002/oby.20169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niemeier HM, Phelan S, Fava JL, Wing RR. Internal disinhibition predicts weight regain following weight loss and weight loss maintenance. Obesity. 2007;15:2485–94. doi: 10.1038/oby.2007.295. [DOI] [PubMed] [Google Scholar]
- 28.Stunkard AJ, Messick S. The 3-Factor Eating Questionnaire to Measure Dietary Restraint, Disinhibition and Hunger. Journal of Psychosomatic Research. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 29.Butryn ML, Thomas JG, Lowe MR. Reductions in Internal Disinhibition During Weight Loss Predict Better Weight Loss Maintenance. Obesity. 2009;17:1101–3. doi: 10.1038/oby.2008.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Niemeier HM, Leahey T, Reed KP, Brown RA, Wing RR. An Acceptance-Based Behavioral Intervention for Weight Loss: A Pilot Study. Behavior Therapy. 2012;43:427–35. doi: 10.1016/j.beth.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lillis J, Niemeier HM, Ross KM, et al. Weight loss intervention for individuals with high internal disinhibition: Design of the Acceptance BAsed Behavioral INtervention (ABBI) randomized controlled trial. BMC Psychology. doi: 10.1186/s40359-015-0075-2. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wing RR, Phelan S. Behavioral treatment of obesity: strategies to improve outcome and predictors of success. In: Eckel RH, editor. Obesity: An Academic Basis for Clinical Evaluation and Treatment. Lippincott: Williams & Wilkens; 2002. pp. 415–35. [Google Scholar]
- 33.Wing RR, Papandonatos G, Fava JL, et al. Maintaining large weight losses: the role of behavioral and psychological factors. J Consult Clin Psychol. 2008;76:1015–21. doi: 10.1037/a0014159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gifford EV, Kohlenberg BS, Hayes SC, et al. Acceptance-based treatment for smoking cessation. Behavior Therapy. 2004;35:689–705. [Google Scholar]


