Abstract
Objectives
Dentists enrolled in the National Dental Practice-Based Research Network completed a study questionnaire about techniques and materials used for single-unit crowns and an enrollment questionnaire about dentist/practice characteristics. The objectives were to quantify dentists’ material recommendations and test the hypothesis that dentist’s and practice’s characteristics are significantly associated with these recommendations.
Methods
Surveyed dentists responded to a contextual scenario asking what material they would use for a single-unit crown on an anterior and posterior tooth. Material choices included: full metal, porcelain-fused-to-metal (PFM), all-zirconia, layered zirconia, lithium disilicate, leucite-reinforced ceramic, or other.
Results
1,777 of 2,132 eligible dentists responded (83%). The top 3 choices for anterior crowns were lithium disilicate (54%), layered zirconia (17%), and leucite-reinforced glass ceramic (13%). There were significant differences (p<0.05) by dentist’s gender, race, years since graduation, practice type, region, practice busyness, hours worked/week, and location type. The top 3 choices for posterior crowns were all-zirconia (32%), PFM (31%), and lithium disilicate (21%). There were significant differences (p<0.05) by dentist’s gender, practice type, region, practice busyness, insurance coverage, hours worked/week, and location type.
Conclusions
Network dentists use a broad range of materials for single-unit crowns for anterior and posterior teeth, adopting newer materials into their practices as they become available. Material choices are significantly associated with dentist’s and practice’s characteristics.
Clinical Significance
Decisions for crown material may be influenced by factors unrelated to tooth and patient variables. Dentists should be cognizant of this when developing an evidence-based approach to selecting crown material.
Keywords: Dentistry, prosthodontics, crowns, dental materials
INTRODUCTION
Dentists have a wide variety of options when selecting a material to fabricate a single-unit crown [1]. The dentist’s choice and recommendation to the patient can depend on various patient and tooth factors, such as tooth location, esthetics, patient desires, masticatory factors, and patient finances [2,3,4].
All-zirconia crowns have gained popularity due to their high strength [1] and toughness [2], wear compatibility with natural dentition [3] and low cost. However, some dentists may decide against this material due to its relative opaqueness and fear of long-term strength degradation from low temperature degradation [5]. Zirconia layered with a translucent ceramic, such as porcelain, is considered a more esthetic crown option, but the relatively low coefficient of thermal expansion and thermal diffusivity of zirconia compared to traditional metal coping materials led to laboratory complications. These manifested as veneer chipping and delamination [6,7,8] over time [9].
Lithium disilicate is another popular material choice for single-unit crowns. It is more translucent than zirconia [4], and can be used in the anterior region without adding a layer of veneering porcelain, which reduces the risk of porcelain chipping. Additionally, the glass matrix of lithium disilicate can be etched with hydrofluoric acid and chemically bonded to tooth structure with a silane primer and adhesive resin cement [10]. Lithium disilicate is not as strong as zirconia, with approximately 40% of its strength [1] and 57% its fracture toughness [2]. A review done by Pieger reported that 5–10 years after cementation, the majority of failures of lithium disilicate crowns occurred in the posterior region [11].
Leucite-reinforced glass ceramic is more translucent than lithium disilicate [12]; however, it is more limited in use and is only recommended as a single-unit in the anterior region [13]. In order to gain sufficient strength for function, leucite-reinforced glass ceramic should be bonded to tooth structure [14].
Porcelain-fused-to-metal (PFM) has been used for many years and studied extensively. Studies have demonstrated a 94% success rate over a 10-year period [15] and good long-term clinical reliability [16]. Although chipping of veneering porcelain is a possible complication, fracture of the metal framework is uncommon [17]. PFM restorations require sufficient tooth reduction to allow space for at least 0.3 mm of metal coping and 0.7 mm of veneering porcelain, and a minimum facial reduction of 1.2 mm according to Hobo and Shillingburg [18]. When comparing PFM crowns to zirconia crowns, several points are noteworthy. Laboratory testing has determined that the fracture strength of a PFM crown using 1.5 mm reduction is similar to zirconia crowns with only 1 mm of reduction [19]. Some manufacturers have even suggested a 0.6 mm minimum reduction for posterior zircona crowns, which has led some dentists to prescribe all-zirconia restorations to preserve tooth structure [20].
Metal crowns are among the strongest options, although their major disadvantage is esthetics. Full-metal restorations are often considered the gold standard in dentistry due to their excellent biocompatibility and strength. However, the increasing price of precious metals and patients’ demands for esthetics have limited the use of both PFM and full metal restorations [7], which could make profitability an important aspect in the dentists’ decision on crown material.
Previous studies have investigated the role that patient and dentist factors may have on material longevity [21,22,23], but none have focused on single-unit crown material selection and dentist characteristics. Therefore, the objectives of this study were to: (1) quantify dentists’ material recommendations; and (2) test the hypothesis that dentist/practice characteristics are significantly associated with these recommendations.
MATERIALS AND METHODS
This study is based on a questionnaire completed by dentists in the National Dental Practice-Based Research Network (PBRN; “network”). The network is a consortium of dental practices and dental organizations focused on improving the scientific basis for clinical decision-making [24]. Detailed information about the network is available at its web site [25]. The network’s applicable Institutional Review Boards approved the study; all participants provided informed consent after receiving a full explanation of the procedures.
Enrollment Questionnaire
As part of the enrollment process, practitioners complete an Enrollment Questionnaire that describes themselves, their practice(s), and their patient population. This questionnaire, which is publicly available at http://nationaldentalpbrn.org/enrollment.php, collects information about practitioner, practice and patient characteristics. Questionnaire items, which had documented test/re-test reliability, were taken from our previous work in a practice-based study of dental care and that PBRN ultimately led to the development of the National Dental PBRN [26,27].
Study Questionnaire Development
The questionnaire for this study was developed by a study team composed of the authors, dentists with clinical expertise, statisticians, and laboratory technicians. Its purpose was to measure current practices in fabricating crowns, and making treatment recommendations for single-unit crowns. The questionnaire was reviewed by Instrument Design, Evaluation, and Analysis Services (IDEA Services), a group with expertise in questionnaire development and implementation, as well as National Institute of Dental and Craniofacial Research (NIDCR) program officers and practitioners with prosthodontic content expertise. After extensive internal review, IDEA Services pre-tested the questionnaire via cognitive interviewing by telephone with a regionally diverse group of eight practicing dentists. Cognitive interviewers probed the dentist’s comprehension of each question. The interviewers also asked dentists to identify items of clinical interest that were not addressed in the questionnaire. Results from the pretest prompted further modification of the questionnaire.
Dentists enrolled in the network were eligible for the study if they met all of these criteria: (1) completed an Enrollment Questionnaire; (2) were currently practicing and treating patients in the United States; (3) were in the network’s “limited” or “full” network participation category; and (4) reported on the Enrollment Questionnaire that they currently do at least some restorative dentistry in their practices. A total of 2,299 dentists met these criteria.
Pre-printed invitation letters were mailed (postal) to eligible dentists, informing them that they would receive an email with a link to the electronic version of the questionnaire. At the time of the email, dentists were given the option to request a paper version of the questionnaire, as this has been shown to improve response rates [28]. Dentists were asked to complete the questionnaire within two weeks. A reminder letter was sent after the second and fourth weeks to those who had not completed the questionnaire. After six weeks, email and postal reminders were sent with a printed version of the questionnaire and dentists were offered the option of completing the online or paper versions. After eight weeks, a final postal questionnaire attempt was made with a letter that also encouraged the dentist to complete the questionnaire online. If a response was not received within two weeks, these dentists were considered non-respondents and were followed up by a Regional Coordinator to ensure that the network communications had been received and that the dentist was not interested in participating. Data collection was closed after 12 weeks from the original email invitation. Dentists or their business entities were remunerated $75 on completion of the questionnaire. Data were collected from February 2015 to August 2015.
Questionnaire Content
The first question confirmed that the invited clinician did at least one crown in a typical month. The Questionnaire is publicly available (http://www.nationaldentalpbrn.org/study-results/2016/#1) under the heading “Factors for Successful Crowns”. Among other questions, practitioners were asked what crown material they recommended for patients.
Material Selection
The authors had a particular interest in learning about material selection for a single-unit crown in the anterior and posterior regions. The two questions of interest for this article were as follows: “Suppose you are doing a routine single-unit crown on tooth #19. What material would you most likely recommend?” and “Suppose you have the same patient as in the previous question, but the single-unit crown is on tooth #8. What material would you most likely recommend?” For both questions the background context was identical: “Assume your patient is a 40-year male who attends his annual recall visits on a dependable basis, has no relevant medical history, is at low risk for dental decay, has satisfactory occlusion with minimal wear, and is financially able to pay for a crown out-of-pocket.”
The responses to these questions and from the network’s Enrollment Questionnaire were tested to determine whether they were significantly (p<0.05) associated with material selection. These were questions relating to dentist gender, race, years since graduation, practice type, region, practice busyness, insurance coverage, hours worked/week, and location type.
Statistical Analyses
Power analysis was based on an anticipated sample size of 1,500 completed questionnaires. This sample size would provide sufficient precision to estimate percentages within ±2.53%, at the 95% confidence level. Analyses were based on two-way frequency tables (with counts and percentages) with significance tests conducted using chi-square tests.
RESULTS
Of the 2,299 dentists invited, 101 were deemed ineligible before beginning the questionnaire (no longer in active practice; deceased, specialists who do not do conventional single-unit crowns). An additional 66 were deemed ineligible once they completed the first question (do not do at least one conventional crown each month). This left a total of 2,132 eligible persons, of whom 1,777 responded, for a response rate of 83.4% (1,777/2,132). Among the 47 test/re-test participants, the mean (SD) time between test and re-test was 15.5 (3.0) days. For categorical variables, agreement between time 1 and time 2 showed a mean weighted kappa of 0.62 (IQR: 0.46, 0.79). Mean test-retest reliability for numeric variables was 0.75.
Material selection for anterior tooth
The top three material choices for anterior teeth were lithium disilicate (54%), layered zirconia (17%), and leucite reinforced glass ceramic (13%) (Figure 1). The analysis of material selection according to dentist and practice characteristics (Table 1), statistically significant differences were found with dentist gender (p=0.022), race (p=0.014), years since graduation (p=0.022), practice type (p<.0001), region (p=0.0006), practice busyness (p=0.0005), hours worked/week (p=0.0004), and location type (p=0.002). The only characteristic that was not statistically significant was insurance coverage (p=0.062) (Table 1). Dentists who graduated more than 15 years ago, although half chose lithium disilicate, had a higher percentage who chose PFM (10%) compared to those who graduated between 5–15 years ago (5%), and those who had graduated less than 5 years ago (3%). With regard to practice busyness, almost 25% of dentists who were too busy to treat all their patients chose PFM, compared to less than 10% for dentists in the other categories. Over 50% of dentists in private practice chose lithium disilicate, compared to 36% or less of dentists in public health practices, federal facilities and academic institutions.
Figure 1. Frequency distribution of material selection, by tooth*.
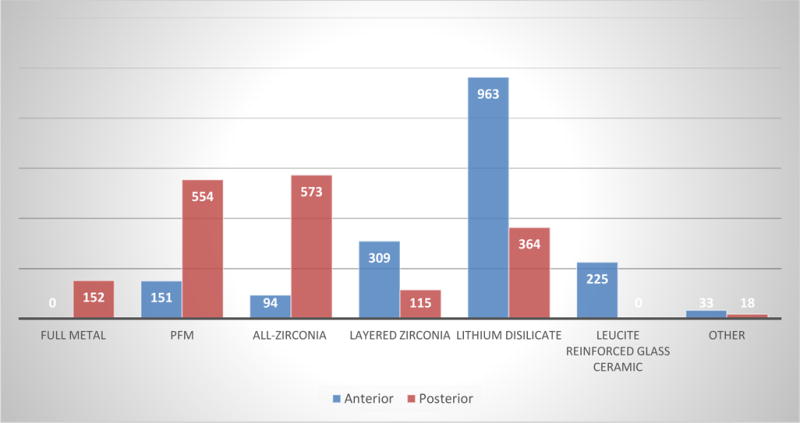
*For anterior tooth, full metal was not an option. For the posterior tooth, leucite reinforced glass ceramic was not an option.
Table 1.
Frequency (%) of material selection for anterior tooth (#8), overall and by dentist and practice characteristics
| PFM | All-zirconia (e.g., Bruxzir) |
Layered zirconia (e.g., Lava) |
Lithium disilicate (e.g., e-Max) |
Leucite-reinforced glass ceramic (e.g., Empress) | Other | P-Value | Total* | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Overall | 150 (9) | 94 (5) | 307 (17) | 956 (54) | 223 (13) | 33 (2) | – | 1763 (100) |
|
| ||||||||
| Gender | ||||||||
| Male | 120 (9) | 60 (5) | 217 (17) | 711 (55) | 151 (12) | 22 (2) | 0.022 | 1281 (73) |
| Female | 30 (6) | 34 (7) | 90 (19) | 245 (51) | 72 (15) | 11 (2) | 482 (27) | |
|
| ||||||||
| Race | ||||||||
| White/Caucasian | 128 (9) | 71 (5) | 254 (17) | 794 (55) | 178 (12) | 25 (2) | 1450 (83) | |
| Black/African-American | 7 (9) | 10 (13) | 16 (21) | 27 (36) | 15 (19) | 2 (2) | 0.014 | 77 (4) |
| Other | 3 (4) | 2 (3) | 7 (10) | 41 (59) | 14 (20) | 3 (4) | 70 (4) | |
| Asian | 13 (8) | 10 (6) | 30 (19) | 88 (55) | 17 (11) | 2 (1) | 160 (9) | |
|
| ||||||||
| Years since graduation | ||||||||
| <5 | 2 (3) | 3 (4) | 12 (17) | 43 (62) | 9 (13) | 1 (1) | 0.022 | 70 (4) |
| 5–15 | 24 (5) | 21 (5) | 76 (17) | 266 (60) | 54 (12) | 3 (1) | 444 (25) | |
| >15 | 125 (10) | 70 (6) | 221 (17) | 651 (52) | 162 (13) | 29 (2) | 1258 (71) | |
|
| ||||||||
| Practice type | ||||||||
| Owner of a private practice | 94 (7) | 67 (5) | 231 (18) | 716 (56) | 158 (12) | 27 (2) | 1293 (73) | |
| Associate/employer of a private practice | 13 (6) | 12 (6) | 32 (16) | 123 (59) | 26 (13) | 1 (0) | 207 (12) | |
| HealthPartners Dental Group | 5 (11) | 1 (2) | 3 (7) | 32 (73) | 2 (5) | 1 (2) | 44 (2) | |
| Permanente Associates Dental Group | 15 (21) | 0 (0) | 14 (20) | 33 (47) | 6 (9) | 2 (3) | <0.0001 | 70 (4) |
| Other managed care | 0 (0) | 0 (0) | 2 (20) | 6 (60) | 2 (20) | 0 (0) | 10 (1) | |
| Public health practice | 13 (20) | 12 (19) | 10 (16) | 22 (34) | 5 (8) | 2 (3) | 64 (4) | |
| Federal facility | 5 (21) | 0 (0) | 3 (12) | 5 (21) | 11 (46) | 0 (0) | 24 (1) | |
| Academic institution | 4 (8) | 2 (4) | 12 (25) | 17 (36) | 13 (27) | 0 (0) | 48 (3) | |
|
| ||||||||
| Region | ||||||||
| Western | 34 (12) | 11 (4) | 56 (19) | 150 (52) | 34 (12) | 7 (3) | 292 (17) | |
| Midwest | 11 (6) | 4 (2) | 26 (14) | 124 (69) | 12 (7) | 3 (2) | 180 (10) | |
| Southwest | 26 (8) | 30 (10) | 49 (16) | 163 (52) | 37 (12) | 5 (2) | 0.0006 | 310 (17) |
| South Central | 30 (9) | 19 (6) | 68 (21) | 159 (48) | 50 (15) | 4 (1) | 330 (19) | |
| South Atlantic | 15 (5) | 16 (5) | 54 (17) | 191 (58) | 43 (13) | 8 (2) | 327 (18) | |
| Northeast | 35 (10) | 14 (4) | 56 (17) | 176 (52) | 49 (15) | 6 (2) | 336 (19) | |
|
| ||||||||
| Practice busyness | ||||||||
| Too busy to treat all | 23 (23) | 5 (5) | 14 (14) | 47 (46) | 9 (9) | 3 (3) | 101 (6) | |
| Provided care to all, but overburdened | 22 (7) | 21 (6) | 48 (15) | 191 (58) | 38 (12) | 6 (2) | 0.0005 | 326 (18) |
| Provided care to all, not overburdened | 72 (8) | 54 (6) | 163 (18) | 484 (53) | 123 (14) | 14 (1) | 910 (51) | |
| Not busy enough | 34 (8) | 14 (3) | 83 (19) | 241 (55) | 54 (13) | 10 (2) | 436 (25) | |
|
| ||||||||
| Insurance coverage | ||||||||
| <40% | 4 (8) | 1 (2) | 9 (17) | 29 (56) | 6 (11) | 3 (6) | 52 (3) | |
| 40–79% | 66 (9) | 26 (3) | 131 (17) | 425 (56) | 96 (13) | 12 (2) | 0.062 | 756 (43) |
| >80% | 81 (9) | 67 (7) | 166 (18) | 495 (52) | 119 (12) | 17 (2) | 945 (54) | |
|
| ||||||||
| Hours work/week | ||||||||
| ≥32 hours | 118 (8) | 71 (5) | 263 (17) | 844 (56) | 183 (12) | 28 (2) | 0.0004 | 1507 (86) |
| < 32 hours | 32 (13) | 23 (9) | 45 (18) | 108 (43) | 39 (15) | 5 (2) | 252 (14) | |
|
| ||||||||
| Location type | ||||||||
| Inner city of urban area | 25 (12) | 20 (10) | 42 (20) | 86 (41) | 33 (16) | 3 (1) | 209 (12) | |
| Urban (not inner city) | 33 (7) | 26 (5) | 92 (19) | 269 (55) | 63 (13) | 7 (1) | 0.002 | 490 (28) |
| Suburban | 60 (8) | 35 (4) | 125 (16) | 467 (59) | 91 (11) | 17 (2) | 795 (45) | |
| Rural | 33 (12) | 13 (5) | 48 (18) | 135 (49) | 38 (14) | 6 (2) | 273 (15) | |
Material selection for posterior tooth
The top three material choices for posterior crowns were all-zirconia (32%), PFM (31%), and lithium disilicate (21%) (Figure 1). The analysis of material selection by dentist and practice characteristics, statistically significant differences were found with dentist gender (p=0.001), practice type (p<.0001), region (p<0.0001), practice busyness (p<0.0001), insurance coverage (p<0.0001), hours worked/week (p<0.0001), and location type (p<0.0001). Two characteristics were not statistically significant: race (p=0.374) and years since graduation (p=.2380) (Table 2). For practice type, 55% of dentists from Permanente Associates Dental Group (a large group practice) chose a full metal crown compared to other practice types that varied in range from 4–25%. Practices with over 80% insurance coverage were more likely to prescribe PFM crowns. Dentists in rural practices were more likely to prescribe all-zirconia restorations than any other location type.
Table 2.
Frequency (%) of material selection for posterior tooth (#19), overall and by dentist and practice characteristics
| Full metal | PFM | All-zirconia (e.g., Bruxzir) |
Layered zirconia (e.g., Lava) |
Lithium disilicate (e.g., e-Max) | Other | P-Value | Total* | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Overall | 151(9) | 550 (31) | 571(32) | 112 (6) | 362 (21) | 18 (1) | — | 1764 (100) |
|
| ||||||||
| Gender | ||||||||
| Male | 111 (9) | 360 (28) | 446 (35) | 79 (6) | 274 (21) | 12 (1) | 0.0001 | 1282 (73) |
| Female | 40 (8) | 190 (40) | 125 (26) | 33 (7) | 88 (18) | 6 (1) | 482 (27) | |
|
| ||||||||
| Race | ||||||||
| White/Caucasian | 123 (9) | 442 (30) | 467 (32) | 96 (7) | 309 (21) | 13 (1) | 1450 (83) | |
| Black/African-American | 5 (6) | 34 (44) | 25 (33) | 5 (6) | 6 (8) | 2 (3) | 0.374 | 77 (4) |
| Other | 8 (11) | 18 (26) | 23 (33) | 5 (7) | 15 (22) | 1 (1) | 70 (4) | |
| Asian | 16 (10) | 53 (33) | 51 (31) | 9 (6) | 31 (19) | 1 (1) | 161 (9) | |
|
| ||||||||
| Years since graduation | ||||||||
| <5 | 8 (11) | 23 (36) | 17 (24) | 4 (6) | 14 (20) | 2 (3) | 70 (4) | |
| 5–15 | 36 (8) | 122 (28) | 154 (35) | 26 (6) | 104 (23) | 2 (0) | 0.2380 | 444 (25) |
| >15 | 107 (9) | 407 (32) | 400 (32) | 85 (7) | 246 (19) | 14 (1) | 1259 (71) | |
|
| ||||||||
| Practice type | ||||||||
| Owner of a private practice | 57 (4) | 397 (31) | 455 (35) | 84 (6) | 293 (23) | 8 (1) | 1291 (73) | |
| Associate/employer of a private practice | 18 (9) | 52 (25) | 71 (34) | 17 (8) | 45 (22) | 4 (2) | 207 (12) | |
| HealthPartners Dental Group | 10 (22) | 18 (41) | 10 (23) | 3 (7) | 3 (7) | 0 (0) | 44 (2) | |
| Permanente Associates Dental Group | 39 (55) | 21 (30) | 2 (3) | 4 (6) | 2 (3) | 2 (3) | <0.0001 | 70 (4) |
| Other managed care | 1 (10) | 3 (30) | 5 (50) | 0 (0) | 1 (10) | 0 (0) | 10 (1) | |
| Public health practice | 10 (16) | 29 (45) | 15 (23) | 3 (5) | 7 (11) | 0 (0) | 64 (4) | |
| Federal facility | 4 (17) | 10 (42) | 3 (12) | 1 (4) | 5 (21) | 1 (4) | 24 (1) | |
| Academic institution | 12 (25) | 18 (38) | 8 (17) | 3 (6) | 5 (10) | 2 (4) | 48 (3) | |
|
| ||||||||
| Region | ||||||||
| Western | 60 (21) | 92 (32) | 56 (19) | 14 (5) | 63 (21) | 7 (2) | 292 (16) | |
| Midwest | 26 (14) | 52 (29) | 50 (28) | 11 (6) | 41 (23) | 0 (0) | 180 (10) | |
| Southwest | 26 (8) | 97 (31) | 118 (38) | 18 (6) | 52 (17) | 0 (0) | 311 (18) | |
| South Central | 17 (5) | 95 (29) | 137 (42) | 19 (6) | 58 (17) | 4 (1) | <0.0001 | 330 (19) |
| South Atlantic | 12 (4) | 80 (24) | 123 (38) | 30 (9) | 77 (24) | 5 (1) | 327 (18) | |
| Northeast | 11 (3) | 138 (41) | 89 (26) | 23 (7) | 73 (22) | 2 (1) | 336 (19) | |
|
| ||||||||
| Practice busyness | ||||||||
| Too busy to treat all | 20 (20) | 43 (42) | 24 (24) | 6 (6) | 7 (7) | 1 (1) | 101 (6) | |
| Provided care to all, but overburdened | 42 (13) | 95 (29) | 104 (32) | 24 (7) | 57 (18) | 4 (1) | <0.0001 | 326 (18) |
| Provided care to all, not overburdened | 63 (7) | 282 (31) | 198 (33) | 59 (7) | 196 (21) | 13 (1) | 911 (51) | |
| Not busy enough | 27 (6) | 132 (30) | 147 (34) | 26 (6) | 104 (24) | 0 (0) | 436 (25) | |
|
| ||||||||
| Insurance coverage | ||||||||
| <40% | 3 (6) | 14 (27) | 20 (38) | 4 (8) | 11 (21) | 0 (0) | 52 (3) | |
| 40–79% | 47 (6) | 226 (30) | 228 (30) | 53 (7) | 196 (26) | 7 (1) | <0.0001 | 757 (43) |
| >80% | 100 (10) | 309 (33) | 319 (34) | 58 (6) | 148 (16) | 11 (1) | 945 (54) | |
|
| ||||||||
| Hours work/week | ||||||||
| ≥32 hours | 113 (7) | 458 (30) | 492 (33) | 102 (7) | 329 (22) | 13 (1) | <0.0001 | 1507 (86) |
| <32 hours | 38 (15) | 91 (36) | 74 (29) | 13 (5) | 32 (13) | 5 (2) | 253 (14) | |
|
| ||||||||
| Location type | ||||||||
| Inner city of urban area | 21 (10) | 86 (41) | 58 (28) | 14 (7) | 28 (13) | 2 (1) | 209 (12) | |
| Urban (not inner city) | 49 (10) | 137 (28) | 167 (34) | 31 (7) | 100 (20) | 6 (1) | 0.016 | 490 (28) |
| Suburban | 54 (7) | 246 (31) | 246 (31) | 55 (7) | 186 (23) | 9 (1) | 796 (45) | |
| Rural | 27 (10) | 81 (30) | 100 (37) | 15 (5) | 49 (18) | 0 (0) | 273 (15) | |
DISCUSSION
The results of this study show a high prevalence of prescription of ceramic crowns compared to metal-based crowns. These results are in stark contrast to a study from nearly 30 years ago which reported a higher selection rate of PFM crowns (55% of Swiss and 56% of Canadian dentists) and metal crowns (17% of Swiss and 35% of Canadian dentists) than porcelain jacket crowns (1% of Swiss and 2% of Canadian dentists).[29]. The shift in material choice from metal porcelain is likely due to significant improvements in dental ceramics, patient demands for esthetic ceramics, and the high cost of fabrication of metal-based crowns. The study results also demonstrate that material choice for single-unit crowns is associated with factors other than the clinical presentation of a patient. Generally, these associations are related to practice type, years since graduation, insurance, and practice busyness.
Regarding the interpretation of years since graduation, the dentist may either have developed preferences for restorative material by gaining exposure to materials in dental school or learning from clinical experience while in practice. The landscape of available dental materials has changed significantly over the past 20 years. A 1997 survey of US dental schools [30] revealed that the most commonly used dental ceramics at the time were the core material In-Ceram Alumina and the glass ceramic Dicor, with flexural strengths of 419 MPa and 108 MPa respectively [31,32]. In 2005, Ivoclar Vivadent released e.max Press, a lithium disilicate material with a flexural strength of 384 MPa that was esthetic enough to be used without veneering porcelain [33]. By 2013, a major US dental laboratory reported that 80% of its crowns and fixed prostheses were fabricated from all-ceramic materials, likely due to the introduction of all-zirconia restorations [34]. In other words, lithium disilicate could have been taught in dental school for all of the graduates of 5 years or less, many of the graduates of 5–15 years, and none of the graduates of >15 years. Similarly, all-zirconia restorations could have been taught in dental school for most of the graduates of 5 years, few of the graduates of 5–15 years and none of the graduates of >15 years. Graduates of >15 years showed a slightly greater tendency to use PFM crowns for anterior teeth, which may be related to less exposure to dental ceramics in dental school or an aversion to ceramics due to the inferior properties of previous generations of materials. Surprisingly, no correlation was observed with years since graduation and prescription of posterior all-zirconia crowns. The penetration of all-zirconia into the market may be the result of its excellent mechanical properties [1,2,3] and low cost.
Differences in materials selection by practice type may be related to the financial responsibility of the dentist or employer to pay the laboratory costs. For most dental laboratories, all-zirconia or all-lithium disilicate restorations can be offered at a lower price than layered restorations due to the easier fabrication process. Additionally, the price of noble or high-noble PFM restorations will be affected by the price of the precious metals present in the metal coping, which is often more expensive than the cost of purchasing ceramic materials. Likely the group of dentists who would be most directly impacted by the laboratory cost of their materials would be private practice owners. In this group, the most commonly chosen materials were also the most economical materials, which were all-zirconia for posterior crowns and lithium disilicate for anterior crowns. Although dentists in some managed care groups, federal facilities, community health clinics and academic institutions may be responsible for the cost of their laboratory fees, many of their employers will pay some or all of those fees, which could reduce their financial motivations behind material selection. For example, academic dentists selected a high proportion of layered zirconia and leucite anterior restorations, which are typically offered at higher prices than lithium disilicate. Dentists in federal facilities, public health practices, and the Permanente Associates Dental Group chose a higher proportion of anterior PFM and posterior full metal restorations, which are also higher-priced restorative materials. Another financial motivating factor for the approximately 15% of private practice dentists who utilize in-office CAD/CAM systems is that lithium disilicate is the predominant material used for in-office milling and many laboratories offer discounted prices when fabricating all-zirconia or lithium disilicate crowns from digital impressions [35,36]. The bias was difficult to assess based on the methods used for the current study.
Practice busyness was also shown to correlate with material selection. The trend in the data indicates that the busiest dentists were more likely to select PFM materials and less likely to select lithium disilicate and leucite based restorations for anterior restorations. This preference may be related to the increased time required to use these ceramic materials clinically. The relative translucency of leucite and lithium disilicate materials requires that dentists adequately communicate the shade of the prepared tooth to the laboratory and select a color-matched cement to achieve ideal color of the final restoration [37]. Additionally, leucite and lithium disilicate crowns achieve optimum strength when they are bonded to tooth structure with a ceramic primer and resin cement [14]. The busiest dentists also preferred full metal and PFM posterior crowns, which may also be related to perceived ease of use. Tooth preparation is simplified because minimal tooth reduction is required if metal is used for the occlusal surface. Adjustment and polishing of metal restorations is also faster and more forgiving than adjusting or polishing zirconia.
Two practice characteristics that can be related to the type of practice are the percentage of patients who have insurance coverage and the practice location. However, conclusions about these characteristics can be difficult to interpret. For instance, a practice with a low percentage of insurance coverage may treat patients in a low socioeconomic status (SES) that cannot afford dental insurance or may treat patients in a high SES and operate a fee-for-service practice. Similarly, a practice in the inner city could treat high SES patients in a major metropolitan area or low SES patients in a distressed inner-city neighborhood. Dentists with over 80% of their patients with insurance coverage were more likely to select full metal and PFM posterior restorations, which could be related to insurance reimbursement and difficulties justifying to an insurance company the use of a ceramic crown on a posterior tooth. Another interesting observation was that rural dentists were the most frequent prescribers of posterior all-zirconia restorations. This observation highlights the prevalent role of large national laboratories that can ship cases throughout the country, as well as the increasing tendency for a local laboratory to scan and design a crown, and then send to a milling center for production.
The results of this study suggest that factors other than clinical evidence influence the dentist’s selection of materials. Part of the difficulty in utilizing evidence for crown material selection is that many of these materials have relatively short clinical histories with few reported long-term clinical trials. A 2015 systematic review of survival rates of single crowns revealed that PFM, lithium disilicate, leucite reinforced, and zirconia restorations had statistically similar 5-year survival rates. The authors noted that layered zirconia and PFM restorations showed a greater incidence of chipping, whereas leucite and lithium disilicate materials showed a higher incidence of framework fracture [38]. The good 5-year clinical success rate of all of these restorative materials implies that dentists need to use their judgment to match the esthetic and mechanical properties of their restorative materials with the clinical presentation of their patient.
Few other studies have examined practice and practitioner characteristics related to material selection or performance. Burke et al. performed a 10-year study on porcelain veneers and found that tooth position was not associated with longevity of the restoration, but did find that veneers placed in female patients had a longer survival, although it was not significant. However, there was a significant difference by patient age, showing poor survival in patients over 60 and under 30 years of age [21]. Dentist factors, such as years since graduation, gender, and place of graduation, were not significantly associated with the survival of the veneer [21].
Haj-Ali et al. developed a survey of material selection for posterior restorations [39], with a focus on amalgam versus composite materials only. The only practice characteristic noted was whether or not the practice was amalgam-free. Another study looking at dentist factors and a 10-year outcome of porcelain laminate veneers [21] found no difference in survival as a function of the dentist factors, which were gender, years since graduation, and country of qualification. This same study also investigated the outcomes of direct restorations and dentist factors and found that age, country of qualification, and employment status were associated with survival of direct restorations [22].
This study does have certain limitations, and conclusions should consider these issues. This study relied on questionnaire information rather than direct observation of procedures; therefore, the inferences made are based on responses from this questionnaire. Questions related to continuing education courses or other sources for information by which these dentists make their decisions was not included in the questionnaire. Additionally, the response rate was very good, but it is possible that non-respondents would have reported different behavior. Although network dentists have much in common with dentists at large [40], it is possible that their material selection is not representative of a wider representation of dentists. Network members are not recruited randomly, so factors associated with network participation (e.g., an interest in clinical research) may make network dentists unrepresentative of dentists at large. While we cannot assert that network dentists are entirely representative, we can state that they have much in common with dentists at large, while also offering substantial diversity in these characteristics. This assertion is warranted because: 1) substantial percentages of network general dentists are represented in the various response categories of the characteristics in the Enrollment Questionnaire; 2) findings from several network studies document that network general dentists report patterns of diagnosis and treatment that are similar to patterns determined from non-network general dentists [41,42,43,44] and 3) the similarity of network dentists to non-network dentists using the best available national source, the 2010 ADA Survey of Dental Practice [45].
CONCLUSION
To our knowledge, this is the first study to report the association between single-unit crown material and dentist/practice characteristics. These results indicate that there are many factors that are significantly associated with material selection for single-unit crowns in the anterior and posterior region. Network dentists use a broad range of materials for single-unit crowns for anterior and posterior teeth, adopting newer materials into their practices as they become widely available. Clinical studies are currently underway in the network to document material selection as part of a larger study about crown preparations and clinical success, so additional work will be done to further explore these associations.
Acknowledgments
This work was supported by NIH grant U19-DE-22516. An Internet site devoted to details about the nation’s network is located at http://NationalDentalPBRN.org. We are very grateful to the network’s Regional Coordinators who followed-up with network dentists to improve the response rate (Midwest Region: Tracy Shea, RDH, BSDH; Western Region: Stephanie Hodge, MA; Northeast Region: Christine O’Brien, RDH; South Atlantic Region: Hanna Knopf, BA, Deborah McEdward, RDH, BS, CCRP; South Central Region: Claudia Carcelén, MPH, Shermetria Massengale, MPH, CHES, Ellen Sowell, BA; Southwest Region: Stephanie Reyes, BA, Meredith Buchberg, MPH, Colleen Dolan, MPH). Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully.
List of abbreviations
- PBRN
practice-based research network
- PFM
Porcelain-fused-to-metal
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Homaei E, Farhangdoost K, Tsoi JK, Pow EH. Static and fatigue mechanical behavior of three dental CAD/CAM ceramics. Journal of the Mechanical Behavior of Biomedical Materials. 2016;59:304–13. doi: 10.1016/j.jmbbm.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 2.Quinn JB, Sundar V, Lloyd IK. Influence of microstructure and chemistry on the fracture toughness of dental ceramics. Dental Materials. 2003;19:603–11. doi: 10.1016/s0109-5641(03)00002-2. [DOI] [PubMed] [Google Scholar]
- 3.Janyavula S, Lawson N, Cakir D, Beck P, Ramp LC, Burgess JO. The wear of polished and glazed zirconia against enamel. Journal of Prosthetic Dentistry. 2013;109:22–9. doi: 10.1016/S0022-3913(13)60005-0. [DOI] [PubMed] [Google Scholar]
- 4.Harada K, Raigrodski AJ, Chung KH, Finn BD, Dogan S, Manci LA. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. Journal of Prosthetic Dentistry. 2016 doi: 10.1016/j.prosdent.2015.11.019. in press. [DOI] [PubMed] [Google Scholar]
- 5.Chevalier J, Gremillard L, Deville S. Low-temperature degradation of zirconia and implications for biomedical implants. Annual Review of Materials Research. 2007;37:1–32. [Google Scholar]
- 6.Sailer I, Gottnerb J, Kanelb S, Hammerle CH. Randomized controlled clinical trial of zirconia-ceramic and metal-ceramic posterior fixed dental prostheses: a 3-year follow-up. The International Journal of Prosthodontics. 2009;22:553–60. [PubMed] [Google Scholar]
- 7.Crisp RJ, Cowan AJ, Lamb J, et al. A clinical evaluation of all-ceramic bridges placed in UK general dental practices: first-year results. British Dental Journal. 2008;205:477–82. doi: 10.1038/sj.bdj.2008.937. [DOI] [PubMed] [Google Scholar]
- 8.Christensen RP, Ploeger BJ. A clinical comparison of zirconia, metal and alumina fixed-prosthesis frameworks veneered with layered or pressed ceramic: a three-year report. Journal of the American Dental Association. 2010;141:1317–29. doi: 10.14219/jada.archive.2010.0076. [DOI] [PubMed] [Google Scholar]
- 9.Håff A, Löf H, Gunne J, Sjögren G. A retrospective evaluation of zirconia-fixed partial dentures in general practices: an up to 13-year study. Dental Materials. 2015;31:162–70. doi: 10.1016/j.dental.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Aboushelib MN, Sleem D. Microtensile bond strength of lithium disilicate ceramics to resin adhesives. Journal of Adhesive Dentistry. 2014;16:547–52. doi: 10.3290/j.jad.a33249. [DOI] [PubMed] [Google Scholar]
- 11.Pieger A, Salman A, Bidra A. Clinical outcomes of lithium disilicate single crowns and partial fixed denture prostheses: a systematic review. Journal of Prosthetic Dentistry. 2014;112:22–30. doi: 10.1016/j.prosdent.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Heffernan MJ, Aquilino SA, Diaz-Arnold AM, Haselton DR, Stanford CM, Vargas MA. Relative translucency of six all-ceramic systems. Part I: core materials. Journal of Prosthetic Dentistry. 2002;88:4–9. [PubMed] [Google Scholar]
- 13.Fradeani M, Redemagni M. An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: a retrospective study. Quintessence International. 2002;33:503–510. [PubMed] [Google Scholar]
- 14.Heintze SD, Cavalleri A, Zellweger G, et al. Fracture frequency of all-ceramic crowns during dynamic loading in a chewing simulator using different loading and luting protocols. Dental Materials. 2008;24:1352–61. doi: 10.1016/j.dental.2008.02.019. [DOI] [PubMed] [Google Scholar]
- 15.Griggs JA. Recent advances in materials for all-ceramic restorations. Dental Clinics of North America. 2007;51:713–727. doi: 10.1016/j.cden.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lekesiz H. Reliability estimation for single-unit ceramic crown restorations. Journal of Dental Research. 2014;93:923–928. doi: 10.1177/0022034514544215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs) Dental Materials. 2015;31:603–23. doi: 10.1016/j.dental.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 18.Hobo S, Shillingburg HT., Jr Porcelain fused to metal: tooth preparation and coping design. Journal of Prosthetic Dentistry. 1973;30:28–36. doi: 10.1016/0022-3913(73)90075-9. [DOI] [PubMed] [Google Scholar]
- 19.Sun T, Zhou S, Lai R, et al. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. Journal for the Mechanical Behavior of Biomedical Materials. 2014;35:93–101. doi: 10.1016/j.jmbbm.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 20.Baladhandayutham B, Lawson NC, Burgess JO. Fracture load of ceramic restorations after fatigue loading. Journal of Prosthetic Dentistry. 2015 Aug;114:266–71. doi: 10.1016/j.prosdent.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 21.Burke FJT, Lucarotti PSK. Ten-year outcome of porcelain laminate veneers placed wtihin the general dental services in England and Wales. Journal of Dentistry. 2009;37:31–38. doi: 10.1016/j.jdent.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 22.Lucarotti PSK, Holder RL, Burke FJT. Outcome of direct restorations placed within the general dental services in England and Wales (Part 3): variation by dentist factors. Journal of Dentistry. 2005;33:827–835. doi: 10.1016/j.jdent.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 23.Burke FJT, Lucarotti PSK, Hohlder RL. Outcome of direct restorations placed within the general dental services in England and Wales (Part 2): variation by patients’ characteristics. Journal of Dentistry. 2005;33:817–826. doi: 10.1016/j.jdent.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Gilbert GH, Williams OD, Korelitz JJ, Fellows JL, Gordan VV, Makhija SK, et al. Purpose, structure, and function of the United States National Dental Practice-Based Research Network. Journal of Dentistry. 2013;41:1051–1059. doi: 10.1016/j.jdent.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The National Dental Practice-Based Research Network. Accessed July, 2016 http://www.NationalDentalPBRN.org.
- 26.Study, F. D. C. Florida Dental Care Study. Retrieved July 1, 2016, from http://nersp.nerdc.ufl.edu/~gilbert/
- 27.Gilbert GH, Richman JS, Gordan VV, Rindal DB, Fellows JL, Benjamin PL, et al. Lessons learned during the conduct of clinical studies in the dental PBRN. Journal of Dental Education. 2011;75:453–465. [PMC free article] [PubMed] [Google Scholar]
- 28.Funkhouser E, Fellows JL, Gordan VV, Rindal DB, Foy PJ, Gilbert GH, et al. Supplementing online surveys with a mailed option to reduce bias and improve response rate: the National Dental Practice-Based Research Network. Journal of Public Health Dentistry. 2014;74:276–282. doi: 10.1111/jphd.12054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Macentee MI, Belser UC. Fixed restorations produced by commercial dental laboratories in Vancouver and Geneva. Journal of Oral Rehabilitation. 1988;15:301–305. doi: 10.1111/j.1365-2842.1988.tb00160.x. [DOI] [PubMed] [Google Scholar]
- 30.Frazier KB, Mjör IA. The teaching of all-ceramic restorations in North American dental schools: materials and techniques employed. Journal of Esthetic Dentistry. 1997;9:86–93. doi: 10.1111/j.1708-8240.1997.tb00922.x. [DOI] [PubMed] [Google Scholar]
- 31.Bottino MA, Salazar-Marocho SM, Leite FP, Vásquez VC, Valandro LF. Flexural strength of glass-infiltrated zirconia/alumina-based ceramics and feldspathic veneering porcelains. Journal of Prosthodontics. 2009;18:417–20. doi: 10.1111/j.1532-849X.2009.00462.x. [DOI] [PubMed] [Google Scholar]
- 32.Giordano RA, 2nd, Pelletier L, Campbell S, Pober R. Flexural strength of an infused ceramic, glass ceramic, and feldspathic porcelain. Journal of Prosthetic Dentistry. 1995;73:411–8. doi: 10.1016/s0022-3913(05)80067-8. [DOI] [PubMed] [Google Scholar]
- 33.Xiaoping L, Dongfeng R, Silikas N. Effect of etching time and resin bond on the flexural strength of IPS e.max Press glass ceramic. Dental Materials. 2014;30:e330–6. doi: 10.1016/j.dental.2014.08.373. [DOI] [PubMed] [Google Scholar]
- 34.Christensen GJ. Is the rush to all-ceramic crowns justified? Journal of the American Dental Association. 2014;145:192–4. doi: 10.14219/jada.2013.19. [DOI] [PubMed] [Google Scholar]
- 35.DiMatteo AM, Latanyshyn K. Relevant or relic? If current trends hold, PFMs may become obsolete. Inside Dentistry. 2014;10:114–19. [Google Scholar]
- 36.Fasbinder DJ. Chairside CAD/CAM: an overview of restorative material options. Compendium of Continuing Education in Dentistry. 2012;33:2–8. [PubMed] [Google Scholar]
- 37.Öztürk E, Chiang YC, Coşgun E, Bolay S, Hickel R, Ilie N. Effect of resin shades on opacity of ceramic veneers and polymerization efficiency through ceramics. Journal of Dentistry. 2013;41(Suppl 5):e8–14. doi: 10.1016/j.jdent.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 38.Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs) Dental Materials. 2015;31:603–23. doi: 10.1016/j.dental.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 39.Haj-Ali R, Walker MP, Williams K. Survey of general dentists regarding posterior restorations, selection criteria, and associated clinical problems. General Dentistry. 2005;53:369–375. [PubMed] [Google Scholar]
- 40.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, et al. Dentists in practice-based research networks have much in common with dentists at large: evidence from the Dental Practice-Based Research Network. General Dentistry. 2009;57:270–275. [PMC free article] [PubMed] [Google Scholar]
- 41.Gordan VV, Garvan CW, Heft MW, Fellows JL, Qvist V, Rindal DB, et al. Restorative treatment thresholds for interproximal primary caries based on radiographic images: findings from the Dental Practice-Based Research Network. General Dentistry. 2009;57:654–663. [PMC free article] [PubMed] [Google Scholar]
- 42.Gordan VV, Garvan CW, Richman JS, Fellows JL, Rindal DB, Qvist V, et al. How dentists diagnose and treat defective restorations: evidence from the dental practice-based research network. Operative Dentistry. 2009;36:664–673. doi: 10.2341/08-131-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Norton WE, Funkhouser E, Makhija SK, Gordan VV, Bader JD, Rindal DB, et al. Concordance between clinical practice and published evidence: finding from the National Dental PBRN. Journal of the American Dental Association. 2014;145:22–31. doi: 10.14219/jada.2013.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gilbert GH, Riley JL, Eleazer PD, Benjamin PL, Funkhouser E, National Dental PBRN Collaborative Group Discordance between presumed standard of care and actual clinical practice: the example of rubber dam use during root canal treatment in the National Dental Practice-Based Research Network. BMJ Open. 2015;5:1–8. doi: 10.1136/bmjopen-2015-009779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.American Dental Association. Survey Center: The 2010 Survey of Dental Practice. Chicago: American Dental Association; [Google Scholar]


