Abstract
Objective
Research shows that people with serious mental illness are increasingly using mobile devices. Less is known about how these individuals use their mobile devices or whether they access social media. We surveyed individuals with serious mental illness to explore their use of these technologies.
Methods
Individuals with serious mental illness engaged in lifestyle interventions through community mental health centers completed a survey about their use of mobile and online technologies. Responses were compared to data from the general population.
Results
Among respondents (n=70), 93% owned cellphones, 78% used text messaging, 50% owned smartphones, and 71% used social media such as Facebook. Most respondents reported daily use of text messaging, mobile apps, and social media. Technology use was comparable to the general population, though smartphone ownership was lower.
Conclusions and Implications for Practice
These findings can inform future interventions that fully leverage this group’s use of popular digital technologies.
Keywords: serious mental illness, community mental health center, social media, technology, smartphone
Introduction
Over 3.5 billion people globally use mobile devices, about 3 billion access the Internet, and more than 2 billion are active social media users (Kemp, 2015). Researchers and clinicians are developing cutting edge interventions using emerging digital, mobile, and social technologies to address health disparities including the significantly reduced life expectancy and elevated chronic disease burden impacting individuals living with serious mental illness (Naslund, Marsch, McHugo, & Bartels, 2015; Walker, McGee, & Druss, 2015). Prior studies have documented increasing use of mobile devices among individuals living with serious mental illness (Firth et al., 2015), however little is known about how these individuals actually use their own mobile devices or whether they access popular social media such as Facebook.
The success of future technology-based interventions will depend largely on how the target population of people living with serious mental illness use and access services through their mobile devices. It is necessary to understand whether and how often these individuals use features such as text messaging, mobile apps, social media, or connecting with others in order to inform future interventions that can fully leverage this group’s use of mobile and online technology. The purpose of this study was to explore how people living with serious mental illness who receive services through community mental health centers use these technologies.
Methods
Participants were age 21 or older and had a serious mental illness defined by an axis I diagnosis of schizophrenia, schizoaffective disorder, major depressive disorder, or bipolar disorder (based on the Structured Clinical Interview for DSM-IV). Participants were excluded if they were residing in a nursing home or other institution, had cognitive impairment defined as a Mini Mental Status Exam (Folstein, Folstein, & McHugh, 1975) score <24, had an active substance use disorder, and were unable to speak English. Participants were recruited from three different community mental health centers located in urban areas in New Hampshire to participate in lifestyle intervention studies. The lifestyle interventions focused on promoting healthy eating, exercise, and weight loss, and were delivered within community mental health settings.
Participants completed a mobile health technology survey as part of their baseline assessment. A trained research interviewer met with participants in person and administered the surveys in a community mental health center setting. The mobile health survey consisted of questions about participants’ use of the Internet, mobile devices, text messaging, and social media, as well as specific questions about how they use these different mobile and online technologies. Participants were compensated for completing the assessment. Committees for the Protection of Human Subjects at Dartmouth College and the New Hampshire Department of Health and Human Services approved all study procedures.
Data Analysis
Descriptive statistics were calculated for participants’ demographic and clinical characteristics. Survey responses were tabulated and compared to national data available for the general population published by the Pew Research Center in 2015 (Anderson, 2015; Duggan, Ellison, Lampe, Lenhart, & Madden, 2015; Duggan & Page, 2015). This approach of comparing data on mobile technology use from a community sample of people living with serious mental illness and from the general population was similarly employed in a recent study (Glick, Druss, Pina, Lally, & Conde, 2015). Data collection was completed in 2014 and 2015, and data analysis was completed in 2015.
Results
Participants (N=70) had a mean age of 47.1 years (SD=12.4), and were mostly female (60%) and predominantly non-Hispanic white (96%). Most participants (81%) lived independently, 17% lived with family, many were never (46%) or previously (44%) married, 45% had a high school diploma or less education, and 80% were unemployed. About one quarter (26%) of participants had a schizophrenia spectrum disorder, 41% had major depressive disorder, and 33% had bipolar disorder.
Table 1 highlights characteristics of participants’ use of their mobile devices and social media, including the type of device they use, the frequency of use, and who they contact using these technologies. The majority (93%) of survey respondents reported owning cellphones, 78% used text messaging, and 71% used popular social media such as Facebook. Most participants reported daily use of text messaging, mobile apps or social media. About 30% of participants with a smartphone or tablet indicated that they had used mobile apps for health or wellness purposes, and about one quarter of participants who use social media reported posting (24%) or searching for health related information (26%) on these popular platforms. Participants reported mainly using text messaging and social media to connect with family or friends.
Table 1.
How people living with serious mental illness use mobile devices and social media
| Survey Responses | Participants n (%) |
|---|---|
| Among the 63 (93%) participants who own a cellphone: | |
| Use a cellphone to access the Internet | 25 (40%) |
| Frequency of sending or receiving text messages | |
| Daily | 31 (49%) |
| Weekly | 12 (19%) |
| Less than once per week | 6 (10%) |
| Use text messaging to contact | |
| Family | 38 (60%) |
| Partner or spouse | 10 (16%) |
| Friend | 35 (56%) |
| Among the 41 (59%) participants who own a smartphone or tablet: | |
| Type of mobile device | |
| Android Smartphone | 23 (56%) |
| iPhone | 5 (12%) |
| Tablet | 10 (24%) |
| Other smartphone | 3 (8%) |
| Use mobile device to access apps | 39 (95%) |
| Frequency of using mobile apps | |
| Daily | 30 (73%) |
| Weekly | 6 (15%) |
| Less than once per week | 4 (10%) |
| Use mobile apps to connect with family and friends | 25 (61%) |
| Amount willing to pay for a mobile app | |
| Will not pay, only download free apps | 26 (63%) |
| Will pay only $0.99 for an app | 2 (5%) |
| Will pay more than $0.99 for an app | 12 (29%) |
| Use of mobile apps for health | |
| Use mobile apps for exercise | 12 (29%) |
| Use mobile apps for diet | 14 (34%) |
| Use mobile apps for weight loss | 11 (27%) |
| Use mobile apps for quitting smoking | 1 (2%) |
| Among the 50 (71%) participants who use social media: | |
| Device used to access social media | |
| Smartphone | 24 (48%) |
| Tablet | 16 (32%) |
| Computer | 32 (64%) |
| Frequency of using social media | |
| Daily | 38 (79%) |
| Weekly | 4 (8%) |
| Less than once per week | 6 (13%) |
| Use social media to connect with | |
| Family | 37 (74%) |
| Partner or spouse | 2 (4%) |
| Friend | 42 (84%) |
| Ever posted personal health information on social media | 12 (24%) |
| Ever searched for health information on social media | 13 (26%) |
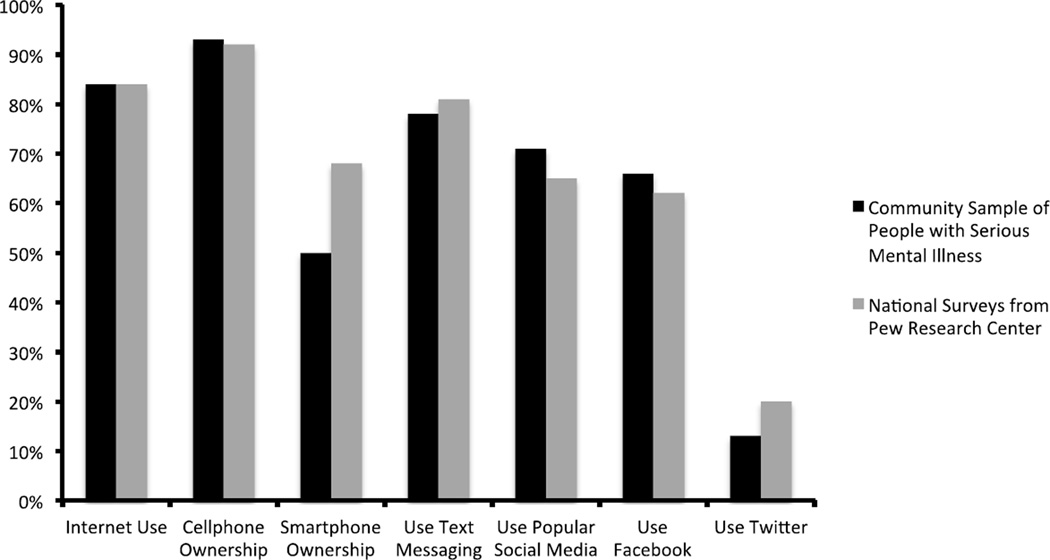
Figure 1 shows that respondents with serious mental illness engaged in lifestyle interventions through community mental health centers showed comparable rates of mobile and online connectivity as the general population. Rates of cellphone ownership, and Internet, text messaging, and social media use were comparable to the general population. Participants living with serious mental illness reported lower rates of smartphone ownership (50%) when compared to the general population (68%).
Figure 1.
Technology use among people living with serious mental illness compared to the general populationa, b
a Values represent proportions of the entire community sample (n=70) of people living with serious mental illness surveyed.
b National survey data was obtained from the Pew Research Center reports from 2015 on Internet, smartphone, and social media use (Anderson, 2015; Duggan et al., 2015; Duggan & Page, 2015).
Discussion
Our findings are consistent with prior surveys and reviews that have demonstrated trends of increasing mobile device ownership and digital technology use among people living with serious mental illness recruited through community mental health settings (Ben-Zeev, Davis, Kaiser, Krzsos, & Drake, 2013; Firth et al., 2015; Glick et al., 2015; Miller, Stewart, Schrimsher, Peeples, & Buckley, 2015). A recent study of a community sample of people living with serious mental illness found similarly high rates of text messaging (78%), but lower rates of smartphone ownership (37%) (Glick et al., 2015). While half of our sample reported owning smartphones, this was considerably lower than smartphone ownership in the general population (68%) (Anderson, 2015). Research suggests that this gap in smartphone ownership, which has been largely attributed to the high costs of these devices, is rapidly closing as the devices and data plans become more affordable and widely available (Firth et al., 2015).
Importantly, our study expands on prior surveys by exploring how this high-risk group uses popular social media such as Facebook or Twitter among a middle-age sample of adults with serious mental illness. One recent survey of inpatients and outpatients with schizophrenia and mean age of 41 years found that close to half (47%) used social media, of which most (79%) reported using these websites at least once each week (Miller et al., 2015). We found that a higher proportion (71%) of our sample used social media, which may be reflective of the fact that our respondents were community dwelling and did not have impaired cognitive functioning. We also found that among respondents who reported using social media, they used these websites frequently (87% reported using these websites weekly) and several reported posting or searching for health related information. Another recent survey of youth ages 12 to 21 with serious mental illness recruited from inpatient units and outpatient departments at a New York hospital found that over 97% were social media users with Facebook as the most popular (94%), followed by Instagram (61%), Twitter (45%), YouTube (39%), and Tumblr (36%) (Birnbaum, Rizvi, Correll, & Kane, 2015). Our survey also expands on recent studies that have suggested that people with serious mental illness are increasingly turning to popular social media to connect with others, to seek advice, and to share their illness experiences (Highton-Williamson, Priebe, & Giacco, 2015; Naslund, Grande, Aschbrenner, & Elwyn, 2014). Additionally, characterizing the use of social media among community samples of people with serious mental illness is critical in order to inform efforts to leverage these online networks for delivering interventions aimed at promoting the mental and physical wellbeing of people living with serious mental illness (Naslund, Aschbrenner, Marsch, & Bartels, 2016).
Limitations
There are several limitations with our study that should be considered when interpreting these findings. Given the small sample size and lack of racial or ethnic diversity, our findings may not be representative of the broader population of people with serious mental illness receiving services through public mental health settings. Further, our respondents were recruited through community mental health centers located in urban areas from New Hampshire, and therefore the findings may not generalize to other settings or geographic regions. Lastly, our survey respondents were enrolled in lifestyle interventions suggesting that they were already interested in health and wellness. Therefore, our respondents may have been more likely to post or search for health information on social media or use mobile apps for exercise, diet, or weight loss. Despite these limitations, our findings offer new insights about how these individuals use their mobile devices and whether they use social media, text messaging, and mobile apps.
Conclusions and Implications for Practice
This study contributes to a growing body of evidence highlighting the potential of using smartphone technologies to reach people living with serious mental illness and to support illness self-management (Ben-Zeev et al., 2014), symptom monitoring (Alvarez-Jimenez et al., 2014), and health promotion efforts targeting this high-risk group (Aschbrenner, Naslund, Barre, et al., 2015; Aschbrenner, Naslund, Shevenell, Mueser, & Bartels, 2015; Naslund, Aschbrenner, & Bartels, 2016). The successful development and dissemination of mobile health interventions likely will be dependent on whether these interventions can be seamlessly integrated into the patterns of daily mobile device use among the target group of people with serious mental illness. For example, mobile health interventions must capitalize on the ways in which people with serious mental illness use their devices, further highlighting the importance of understanding how these individuals use mobile and online technologies. Our findings can inform efforts that take full advantage of the different features of these technologies and could support the design of tailored interventions to extend the reach and quality of services delivered through community mental health settings.
Acknowledgments
This study was supported by grants from the National Institute of Mental Health (R01 MH089811), the Agency for Healthcare Research and Quality (K12 HS021695-01) and from the United States Centers for Disease Control and Prevention Health Promotion and Disease Prevention Research Center (Cooperative Agreement Number U48 DP005018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Disclosure: Each of the authors contributed to the data collection, analysis, and preparation of this brief report. The authors report no competing interests.
References
- Alvarez-Jimenez M, Alcazar-Corcoles M, Gonzalez-Blanch C, Bendall S, McGorry P, Gleeson J. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophrenia research. 2014;156(1):96–106. doi: 10.1016/j.schres.2014.03.021. [DOI] [PubMed] [Google Scholar]
- Anderson M. Technology device ownership: 2015. 2015 Retrieved from http://www.pewinternet.org/files/2015/10/PI_2015-10-29_device-ownership_FINAL.pdf.
- Aschbrenner KA, Naslund JA, Barre LK, Mueser KT, Kinney A, Bartels SJ. Peer health coaching for overweight and obese individuals with serious mental illness: intervention development and initial feasibility study. Translational Behavioral Medicine. 2015;5(3):277–284. doi: 10.1007/s13142-015-0313-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschbrenner KA, Naslund JA, Shevenell M, Mueser KT, Bartels SJ. Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health technology for individuals with serious mental illness. Psychiatric Quarterly. 2015:1–15. doi: 10.1007/s11126-015-9395-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Brenner CJ, Begale M, Duffecy J, Mohr DC, Mueser KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophrenia Bulletin. 2014;40(6):1244–1253. doi: 10.1093/schbul/sbu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, Drake RE. Mobile technologies among people with serious mental illness: opportunities for future services. Adm Policy Ment Health. 2013;40(4):340–343. doi: 10.1007/s10488-012-0424-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum ML, Rizvi AF, Correll CU, Kane JM. Role of social media and the Internet in pathways to care for adolescents and young adults with psychotic disorders and non-psychotic mood disorders. Early intervention in psychiatry. 2015 doi: 10.1111/eip.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M, Ellison NB, Lampe C, Lenhart A, Madden M. Social media update 2014. 2015 Retrieved from http://www.pewinternet.org/files/2015/01/PI_SocialMediaUpdate20144.pdf.
- Duggan M, Page D. Mobile messaging and social media 2015. 2015 Retrieved from http://www.pewinternet.org/files/2015/08/Social-Media-Update-2015-FINAL2.pdf.
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, Yung AR. Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies. Schizophrenia Bulletin. 2015:sbv132. doi: 10.1093/schbul/sbv132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Glick G, Druss B, Pina J, Lally C, Conde M. Use of mobile technology in a community mental health setting. Journal of telemedicine and telecare. 2015:1357633X15613236. doi: 10.1177/1357633X15613236. [DOI] [PubMed] [Google Scholar]
- Highton-Williamson E, Priebe S, Giacco D. Online social networking in people with psychosis: A systematic review. International Journal of Social Psychiatry. 2015;61(1):92–101. doi: 10.1177/0020764014556392. [DOI] [PubMed] [Google Scholar]
- Kemp S. Digital, social and mobile worldwide in 2015. 2015 Retrieved from http://wearesocial.com/uk/special-reports/digital-social-mobile-worldwide-2015.
- Miller BJ, Stewart A, Schrimsher J, Peeples D, Buckley PF. How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Research. 2015;225(3):458–463. doi: 10.1016/j.psychres.2014.11.067. [DOI] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Bartels SJ. Wearable devices and smartphones for activity tracking among people with serious mental illness. Mental Health and Physical Activity. 2016;10:10–17. doi: 10.1016/j.mhpa.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiology and psychiatric sciences. 2016;25(2):113–122. doi: 10.1017/S2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Grande SW, Aschbrenner KA, Elwyn G. Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLOS ONE. 2014:e110171. doi: 10.1371/journal.pone.0110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Marsch LA, McHugo GJ, Bartels SJ. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of Mental Health. 2015;24(5):321–332. doi: 10.3109/09638237.2015.1019054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]