Abstract
Objective
Teenage drivers diagnosed with attention-deficit/hyperactivity disorder (ADHD) are at significant risk for negative driving outcomes related to morbidity and mortality. However, there are few viable psychosocial treatments for teens with ADHD and none focus on the key functional area of driving. The Supporting the Effective Entry to the Roadway (STEER) program was evaluated in a clinical trial to determine whether it improved family functioning as a proximal outcome and driving behavior as a distal outcome.
Method
One hundred seventy-two teenagers with ADHD, combined type, were randomly assigned to STEER or a driver education driver practice program (DEDP).
Results
Relative to parents in the DEDP condition, parents in STEER were observed to be less negative at post-treatment and 6-month follow-up, but not at 12-month follow-up and there were no significant differences for observed positive parenting. Relative to teens in the DEDP condition, teens in STEER reported lower levels of risky driving behaviors at post-treatment and six-month follow-up, but not at 12-month follow-up. They were not observed to differ on objective observations of risky driving or citations/accidents.
Conclusions
The STEER program for novice drivers with ADHD was effective in reducing observations of negative parenting behavior and teen self reports of risky driving relative to DEDP; groups did not significantly differ on observations of positive parenting or driving behaviors.
Public Health Significance Statement
Families with a teenager with ADHD may benefit from engaging in behavioral parent training around the transition to independent driving, especially via reductions in negative parenting. Teenagers with ADHD self-reported fewer risky driving behaviors within the family-focused intervention, but these findings were not replicated on objective observations of driving.
Keywords: ADHD, parent training, driving, family therapy
American drivers between 16–20 years old are the most at risk for injuries and fatalities compared to other age ranges (CDC, 2013; Insurance Institute for Highway Safety, 2014), and adolescent drivers are a prominent public health concern (American Academy of Pediatrics, 2006). The driving performance of adolescents diagnosed with attention-deficit/hyperactivity disorder (ADHD) is impaired relative to typically developing adolescents, who are already acknowledged to be highly risky drivers (Barkley & Cox, 2005; Fabiano & Schatz, 2014; Jerome, Segal, & Babinski, 2006). Multiple studies are available to illustrate that individuals with ADHD exhibit more risky driving behaviors and commit more driving errors and lapses on simulators (Narad et al., 2013; Reimer et al., 2010), in real cars (Arduen, Kofler, Cox, Sarver, & Lunsford, 2014), when distracted (Narad et al., 2013), and when intoxicated (Weafer, et al., 2008) relative to typically-developing teenage drivers. These outcomes are even more concerning given teenage drivers with attention problems drive significantly more often than other teenage drivers (Woodward et al., 2000), indicating those at most risk for untoward outcomes are driving the most often.
There is a growing literature that demonstrates stimulant medication acutely improves the behavior (Evans et al., 2001) and driving outcomes (e.g., Cox et al., 2006; Cox et al., 2004) for teenagers with ADHD. However, compliance with stimulant medication regimens at this age can be inconsistent to poor (Marcus et al., 2005) -- suggesting non-pharmacological alternatives are needed to effectively treat adolescents with ADHD. Stimulants are also not typically therapeutically effective during the most common times for car accidents (e.g., at night, early in the morning; NHTSC, 2005). This leaves the field wanting for an effective alternative to medication for teen drivers with ADHD. Unfortunately, few effective psychosocial treatment programs for ADHD adolescents exist (Evans, Serpell, Schultz, & Pastor, 2007; Fabiano et al., 2015; Pelham & Fabiano, 2008; Smith et al., 2000), and those that work are not widely available. Further, there are mixed findings within studies of parent training programs for adolescents with ADHD (Barkley et al., 2001), warranting additional study of this treatment approach. Indeed, there are few effective psychosocial interventions for helping parents of adolescents with ADHD monitor their teens and support their development of safe driving skills, even though adolescents with ADHD are clearly impaired in their driving behavior (Fischer, et al., 2007; Woodward, et al., 2000).
The few psychosocial treatment alternatives that are available for teens with ADHD have limitations. Driver education programming, where teens attend classes to learn the rules of the road, receive information about safety, and practice driving on the roadway with instructor support, is the most commonly employed approach. However, there is considerable controversy over the benefits of driver education classes. Systematic reviews suggest little to no benefit of these classes on driving outcomes with adolescents in general (Clinton & Lonero, 2006; Cochrane Injuries Group Driver Education Reviewers, 2001; Vernick, et al., 1999). In addition to driver education, most states have moved to a graduated driver license (GDL) program, where novice teen drivers are only permitted to drive during periods of relatively lower risk (e.g., during the day). The GDL approach has resulted in reductions in car crashes where implemented (e.g., Shope & Molnar, 2003; Shope, Molnar, & Elliott, 2001).
Parental monitoring and limit-setting has also been investigated as a potential effective approach to enforcing GDL limits and promoting safe driving behaviors emphasized in driver education classes. Although state law, GDL programs are largely enforced through parental monitoring and supervision, a task that can be difficult for parents managing the behavior of a teenager with ADHD. In general, parents who do not set appropriate limits regarding use of the car, have poor communication with the adolescent regarding driving rules, and are poor monitors of their teen’s driving behaviors have teens that engage in more dangerous driving behaviors (Beck, Hartos, & Simons-Morton, 2005; Beck, Shattuck, & Raleigh, 2001; Shope, et al., 2001; Simons-Morton & Hartos, 2003).
To support parents with effective monitoring, there are a number of commercially available products that parents can use to monitor driving behaviors (e.g., a camera that records teen behaviors immediately preceding a risky driving behavior, vehicle engine and driving performance monitors that record frequencies of risky events or the amount of time a teen drives in a high speed range). Emerging evidence suggests that these on-board monitoring devices result in safer driving, particularly among the teen drivers with the highest rates of risky behaviors (Fabiano et al, 2011; Farmer, Kirley, & McCartt, 2009; Lee, 2007; McGehee, Raby, Carney, Lee, & Reyes, 2007). For example, McGehee et al. (2007) reported that an event-triggered on-board video and data recording device supplemented with weekly report cards reviewed with parents, resulted in reduced risky driving events. Importantly, these positive results were largely attributable to the seven drivers in the study who exhibited high-rates of risky driving behaviors. Attenuating the promise of these tools is that teens are often unenthusiastic about the use of these products, and parents may not have a clear idea of how to use them effectively (e.g., McCartt, et al., 2007). Thus, emerging evidence suggests that monitoring of these on-board devices is only effective if parents are supported in this monitoring in practical, concrete ways (Farmer, et al., 2009).
A final tool for promoting safe driving includes the use of driving simulators. Simulators have utility for permitting practice in dangerous situations, including driving (e.g., Narad et al., 2013). An understudied role for simulators in driver training is as a place for parents and novice drivers to interact/practice/communicate about driving in a situation that is free from the danger that may be present in on-road driving practice. A further benefit would be the opportunity for parents to “try-out” parenting strategies related to teaching effective driving in a controlled setting. This may be particularly important for parents of youth with ADHD who have been shown to use few effective parenting skills in on-road driving instruction with novice drivers (Schatz, et al., 2014).
Due to the seriousness of the potential negative outcomes of risky driving, intensive treatments for youth with ADHD are needed to prevent high personal and economic costs as well as morbidity and mortality. The driving-focused interventions reviewed could be integrated within an evidence-based treatment for ADHD, behavioral parent training supported with contingency management strategies (Evans, Owens, & Bunford, 2013; Pelham & Fabiano, 2008). Thus, the psychosocial treatment components outlined above were combined with a behavioral parent training program to create an intensive treatment for youth with ADHD focused on promoting safe driving. The Supporting a Teen’s Effective Entry to the Roadway (STEER) program - a treatment designed for an ADHD population that occurs during the developmental task of learning to drive was developed (Fabiano et al., 2011). The STEER program integrates a behavioral parenting program and communication training for the teen and parents (Barkley, Edwards, & Robin, 1999; Robin & Foster, 1989; Smith, Molina, & Eggers 1997) with a number of driving-focused interventions including supervised practice in a driving simulator facilitated by clinician coaching, parental monitoring of objective driving behaviors using engine and driving performance monitors, and contingency management contracts aimed at promoting safe driving. The proximal targets of the STEER intervention were improvements in parenting an adolescent with ADHD that would lead to distal improvements in adolescent driving behavior. Because the initiation of driving is an important family transition, it may also be an opportune time to engage parents and teens with ADHD in an intervention. Adolescents, who can be difficult to engage in treatment (e.g., Barkley et al., 2001), may be optimally primed for participation in an intervention at this time due to a strong desire to drive. Parents may also be motivated for engaging in treatment given concerns about their adolescent’s safety.
This study reports the results of a randomized trial that compared the STEER program, which occurred in conjunction with teens’ participation in driver education, against a driver education and driving practice alone (DEDP) condition. The comparison condition in this study included driver education classes, supervised on-road driving practice with a driving instructor, and practice on a driving simulator in order to mirror driver training programming available in community settings. This study considered the efficacy of the STEER program for improving both proximal (parenting behaviors) and distal (driving related) outcomes. It was hypothesized that STEER would result in improved proximal outcomes relative to the DEDP group, specifically parenting behaviors as observed during parent-child interactions. It was further hypothesized that STEER would result in improved distal outcomes related to driving (i.e., observations collected from on-board cameras, teen self-report of driving), relative to DEDP.
Method
The present study was a between-group, randomized trial comparing DEDP to STEER. Participants were randomly assigned to either of the two intervention groups. Outcomes were assessed following the treatment, and at six-month and 12-month follow-ups of all participants. The University’s Institutional Review Board approved study procedures.
Participants
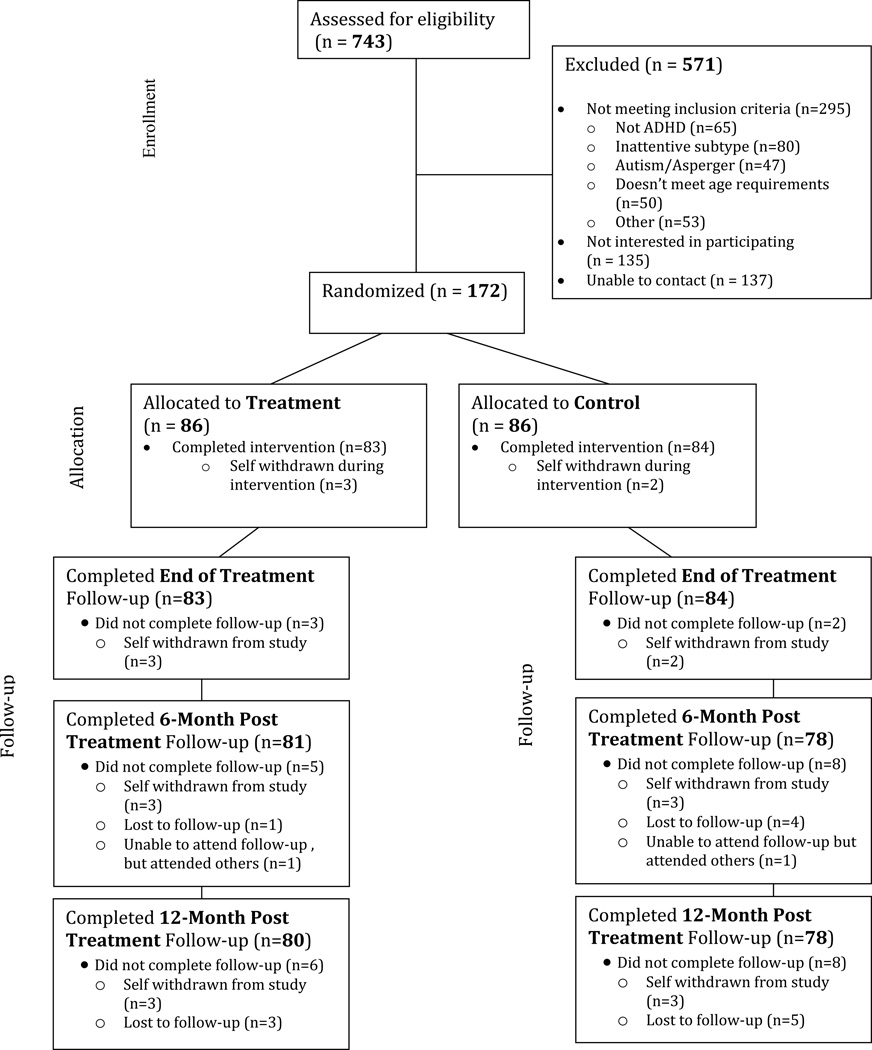
One hundred seventy-two adolescents were recruited through radio advertisements, direct mailings, and school referrals to participate in a research study in four annual cohorts of 43. Parents of potential participants called the researchers and completed a series of questions regarding study eligibility criteria (e.g., age, whether the teen has a driver’s permit, history of ADHD diagnosis). Individuals who met initial inclusion criteria were invited to attend a visit where the study was described in more detail, informed consent and assent was obtained, and intake measures/interviews were completed. See Figure 1 for a study CONSORT diagram.
Figure 1.
Study CONSORT Flow Diagram
The final sample of 172 participants were adolescents between 16 to 18 years old diagnosed with ADHD-Combined Type using the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM; American Psychiatric Association, 1994). Diagnoses were made through parent and teacher Disruptive Behavior Disorder (DBD) rating scales of ADHD symptoms (Pelham, et al., 1992), the DSM scale on the Child Behavior Checklist and Teacher Report Form (Achenbach & Rescorla, 2001), and a semi-structured DBD clinical interview with the teen’s parent(s) (Pelham, Fabiano, et al., 2005; Sibley, et al., 2012) to obtain contextual information regarding symptoms/impairment and document age of onset. Consistent with recommendations in the diagnostic literature, mothers, fathers (when available), and teachers completed DBD ratings independently, and ratings were combined across parents by taking the maximum symptom rating across parents (Anastopoulos & Shelton, 2001; Bird, Gould, & Staghezza, 1992). Cross-situational impairment was assessed through parent and teacher ratings on the Impairment Rating Scale (IRS; Fabiano et al., 2006). The DBD rating scale, interview, and IRS are all valid for use with adolescents (Evans, et al., 2005; Hartung et al., 2005; Molina, Pelham, & Smith, 2001).
Adolescents were diagnosed with ADHD-Combined Type if they met Diagnostic and Statistical Manual for Mental Disorders (American Psychiatric Association, 2000) symptom criteria for ADHD at home and school (i.e., at least six symptoms of inattentive and hyperactive/impulsive behavior), impairment ratings indicated that they exhibited impairment in home and school settings, and if they met the age of onset criterion (which was established using medical records, elementary school report cards, and parent interviews). A diagnosis of ADHD, combined type was made if a prior combined type diagnosis was documented through a review of historical reports and there were at least four current hyperactive/impulsive symptoms endorsed across raters (Range = 4–9; Mean = 6.91, SD=1.56; see Sibley et al., 2012). The study investigators and co-investigators independently reviewed child files with completed information to determine diagnosis (i.e., current symptom presence and cross-situational impairment) and raters agreed on diagnosis across 100% of files reviewed using a standard checklist. In addition to a diagnosis of ADHD, Combined type, adolescents also had to have a valid driver’s learning permit by the beginning of the study. All participants in the study had the combined subtype of ADHD to ensure participants evinced both inattention and overactivity/impulsivity as both aspects of ADHD behavior may negatively influence driving and parent-teen relationships. This also aligned our sample with the inclusion criteria in other large clinical trials within the literature such as the MTA (MTA Cooperative Group, 1999).
Participants were excluded from the study if the teen had an IQ of less than 70 (either obtained from previous assessments that occurred in the past year or obtained at intake). Teens were also excluded if there was evidence of psychosis, seizure disorders, eating disorders, substance abuse disorders, or other medical conditions or medications that prohibit driving. Further, an adolescent who already completed a driver’s education class or had a driver license was not eligible to participate. For families where the parents were separated or divorced, at least one parent had to be able to attend the program with the teenager (i.e., custody arrangements would not impede participation). Adolescents with the Inattentive or Hyperactive-Impulsive subtypes were excluded from the study as . Descriptive information is included in Table 1.
Table 1.
Sample Description
| STEER |
DEDP |
|||
|---|---|---|---|---|
| N | M (SD) or % | N | M (SD) or % | |
| Teen Age (Years) | 86 | 16.98 (0.70) | 86 | 16.88 (0.65) |
| Teen Male Gender | 86 | 73.3% | 86 | 70.9% |
| Teen Ethnicity | 86 | 86 | ||
| Non-Hispanic | 93% | 94.2% | ||
| Teen Race | 86 | 86 | ||
| Caucasian | 87.2% | 83.7% | ||
| African American | 9.3% | 12.8% | ||
| Biracial | 1.2% | 1.2% | ||
| Other | 2.3% | 2.3% | ||
| Teen WASI | 86 | 100.91 (13.34) | 86 | 98.93 (12.38) |
| Percent Medicated for ADHD |
86 | 68.6% | 86 | 68.6% |
| DBD – Hyperactive | ||||
| Impulsive Symptoms average score |
86 | 1.46 (0.60) | 86 | 1.47 (0.61) |
| DBD – ADHD Symptoms average score |
86 | 1.74 (0.49) | 86 | 1.74 (0.54) |
| DBD – ODD Symptoms average score |
86 | 1.33 (0.65) | 86 | 1.18 (0.69) |
| DBD – CD Symptoms average score |
86 | 0.25 (0.23) | 86 | 0.25 (0.27) |
| Parent Age (Years) | 83 | 47.40 (6.47) | 86 | 46.60 (6.24) |
| Parent Relationship (all female) |
86 | 86 | ||
| Mother | 97.7% | 96.5% | ||
| Grandmother | 1.2% | 1.2% | ||
| Other Relation | 1.2% | 2.3% | ||
| Parent Ethnicity | 86 | 86 | ||
| Non-Hispanic | 98.8% | 96.5% | ||
| Parent Race | 86 | 86 | ||
| Caucasian | 91.9% | 88.4% | ||
| African American | 8.1% | 11.3% | ||
| Parental Education | 86 | 86 | ||
| High School/GED | 30.2% | 25.6% | ||
| Associates | 17.4% | 23.3% | ||
| Bachelors | 34.9% | 27.9% | ||
| Masters | 10.5% | 20.9% | ||
| Doctorate | 7.0% | 2.3% | ||
Note. WASI = Wechsler Abbreviated Scale of Intelligence. DBD – Disruptive Behavior Disorder Rating Scale. STEER=Supporting a Teen’s Effective Entry to the Roadway. DEDP=Driving Education and Driving Practice. There were no significant differences across groups on any variable.
Procedures
Teens were randomly assigned to the STEER or DEDP intervention as described below in detail. A stratified sampling plan was used for treatment assignment. Specifically, teens were stratified by stimulant use at study enrollment and randomly assigned to treatment condition within strata. This ensured that teens who were prescribed medication treatment were balanced across treatment conditions. It also served to optimize statistical power for testing whether stimulant use impacted treatment response.
Participants then enrolled in their respective intervention conditions, and follow-up assessments were completed at the end of treatment (12 weeks from randomization), six-months later, and 12-months later. At each assessment point, parents and teens were asked to report on behaviors that occurred since the prior assessment. Teens were asked to come to these visits on days they withheld stimulant medication if taking it, and parents were asked to rate the teen’s unmedicated behavior. Thus, parent ratings and parent-teen interactions in the laboratory represent unmedicated behavior. It was not practical or ethical to withhold medication use within the month-long driving assessments so the driving outcomes represent teen behavior with medication as typically used by the adolescent (random assignment was used as a tool to distribute variations in use and compliance with medication equally across groups). The majority of participants were retained for all assessment points (see Figure 1).
Study Treatments
Table 2 lists the treatment components as well as the timing of the intervention components for both the DEDP and STEER groups. Parenting intervention components were administered by Ph.D.-level psychologists (N=4) or advanced graduate students supervised by Ph.D.-level psychologists (N=6). Teen interventions and driving simulator training sessions were administered by research assistants at the B.A. level, or higher (N=16). Each of the treatment groups are described in detail.
Table 2.
Outline of Timing and Content of Intervention components for the STEER and DEDP groups
| Week | Driver’s Education (Both Groups) |
DEDP Content (Both Groups) |
STEER Intervention Content (STEER Group Only) |
|---|---|---|---|
| Week 1 | 3-hour classroom instruction |
||
| Week 2 | 3-hour classroom/1 hour driving instruction |
Parent provided CarChipPro |
Parent: Psychoeducation on risks of ADHD and teen driving; House rules and rules of the road |
|
Teen: Motivational enhancement, House rules and rules of the road | |||
|
Joint Session: CarChip Pro introduction and review, Driving contract | |||
| Week 3 | 3-hour classroom/1 hour driving instruction |
Simulation Exercise 1: Practice, Hazards Course |
Parent: Noticing and attending to positive driving behaviors |
|
Teen: Expressing feelings and knowing the feelings of others | |||
|
Joint: Review of rules, contract, CarChip Pro; Simulation exercise 1 with parent practice of parenting skills | |||
| Week 4 | 3-hour classroom/1 hour driving instruction |
Parent: Using effective instructions while teaching driving skills |
|
|
Teen: Making an appropriate complaint Joint: Review of rules, contract, CarChip Pro |
|||
| Week 5 | 3-hour classroom/1 hour driving instruction |
Simulation Exercise 2: Distracted Driving exercise, Impaired Driving exercise, Debrief |
Parent: Planned ignoring to promote safe Driving |
|
Teen: Appropriately answering a Complaint | |||
|
Joint: Review of rules, contract, CarChip Pro; Simulation Exercise 2 with parent practice of parenting skills | |||
| Week 6 | 3-hour classroom/1 hour driving instruction |
Parent: Privilege removal for violations of road rules |
|
|
Teen: Accepting limits set by others Joint: Review of rules, contract, CarChip Pro | |||
| Week 7 | 3-hour classroom/1 hour driving instruction |
Simulation Exercise 3: Practice, Hazards Course |
Parent: How to discuss driving limits and issues with the teen |
|
Teen: Introduction to communication Skills | |||
|
Joint: Review of rules, contract, CarChip Pro; Simulation Exercise 3 with parent practice of parenting skills | |||
| Week 8 | 3-hour classroom/1 hour driving instruction |
Parent: Managing and challenging unreasonable beliefs about adolescent driving |
|
|
Teen: Managing and challenging unreasonable beliefs about parents | |||
|
Joint: Review of rules, contract, CarChip Pro | |||
| Week 9 |
3-hour classroom/1 hour driving instruction |
Parent: Review STEER content, Discuss how parents and teens may continue to implement these strategies in the future |
|
|
Teen: Review STEER content, Discuss how parents and teens may continue to implement these strategies in the future | |||
|
Joint: Review of rules, contract for licensed driving discussed, CarChip Pro | |||
| Week 10 |
3-hour classroom/1 hour driving instruction |
STEER Make-up (if needed) |
|
| Week 11 |
1-hour driving instruction |
||
| Week 12 |
Driver’s instruction make-up (if needed) |
Note: STEER=Supporting a Teen’s Effective Entry to the Roadway. DEDP=Driver Education Driving Practice. Adolescent participants in both groups attended the driver’s education programming outlined in the second column. In parallel, participants assigned to DEDP and STEER received the treatment components listed in the third and fourth columns, respectively.
DEDP
All teens within DEDP were enrolled in a 10-week driver education and driving training program. The program included 30 hours of classroom instruction (including the five-hour pre-licensing course required of all novice drivers in New York state) and 10, 45-minute, individual driving lessons with a certified driving instructor. The program was created by the local automobile association to improve upon traditional driver education programs which typically emphasize observation of driving (up to 75% of in-car activity) rather than actual driving. It is available to all members of the community and as such represents a potentially generalizable and face valid intervention for novice drivers. Further, it is a more intensive driver education program than typical school-based classes as there is considerably more time spent in on-road driving practice.
The participants in the DEDP group were provided the CarChip Pro (Davis Instruments, 2015) in its original packaging and told that it was a tool they might find helpful. These instructions were intended to mimic how a parent may obtain the device via retail purchase (i.e., there was no additional clinician support). The CarChip Pro is an engine and driving performance monitor that can be inserted into cars manufactured after 1996 to track speed, hard-braking, and hard-accelerations for each driving trip. When removed from the car, the device can then be inserted into a computer, and using the included software, graphical displays of engine and driving performance can be reviewed and monitored. In this way, a parent could monitor whether excessive speed occurred during a driving trip, or there were unusual amounts of risky driving behaviors such as hard braking or acceleration.
The parent and teen were also invited to three practice sessions on a driving simulator. The simulator consisted of a 6 degree-of-freedom electrically actuated motion platform and real passenger cabin (a Ford Contour) within a 180-degree visualization theater ring for a front view along with a rear-view screen, driver input (a steering wheel and floor pedals), an on-board emergency-stop switch for safety purposes, an off-board stereo audio system, and a quad core performance PC-based computer workstation to execute the entire simulation. The residential simulation environment was modeled after an actual array of neighborhoods, streets, and landmarks adjacent to the university campus. Numerous hazards were developed and implemented to challenge drivers during their excursions: roadway cones along both sides of the road with lane narrowing, a construction zone, inclement weather/icy roads, aggressive drivers, and animal crossings.
Adolescents spent the first and third session on the simulator driving through a prescribed course, negotiating hazards and driving challenges (i.e., a tailgating, aggressive driver). During the second session, adolescents drove a course without distraction, followed by driving the same course when distracted by sending text messages and then while wearing goggles that mimicked visual impairment with a .12 blood alcohol level. Following these driving exercises, the clinician printed out driving performance metrics (i.e., speed variability, lane deviations) and shared these with the teenager and parent to demonstrate impaired driving on the latter two exercises relative to the first practice drive. There was no feedback on parenting strategies embedded within the exercises. The timing of the simulator practice in this group was comparable to the timing within the STEER intervention (See Table 2). This was done to control for the additional driving practice teens in the STEER intervention gained on the simulator.
STEER
The same driver training program described in the DEDP group was offered to all participants in the STEER group. In addition, the STEER program included an eight-week, parent-teen intervention focused on improving outcomes for adolescent drivers with ADHD. The STEER intervention included parent behavior management training and teen communication training coupled with weekly parent-teen negotiations regarding driving situations and behaviors, use of the CarChip Pro to monitor driving behavior, and practice on a driving simulator where teens were exposed to various driving scenarios and parents were coached to practice parenting strategies (e.g., positive attending, using effective instructions/commands) during the activity. All parent, teen, and shared sessions were manualized.
During each week of the STEER program, sessions were divided into two, 45-minute meetings with the first half including individual parent and teen meetings that occur in parallel and the second half including a joint activity. During the first portion of the meeting, the teen met individually with a counselor to review safe driving behaviors and learn about effective communication and social skills (Barkley, et al., 1999; Robin & Foster, 1989; Smith, Molina, & Eggers, 1997). In parallel, the parent met with a clinician to review effective parental monitoring, contingency management, and communication skills (Barkley, et al., 1999; Barkley et al., 1992; Barkley et al., 2001; Forgatch & Patterson, 1989; Patterson & Forgatch, 1989; Robin & Foster, 1989). Following these individual meetings, the family participated for the second 45 minutes in a joint activity – during three weeks this was practice on a driving simulator, and during these and other weeks a review of objective driving data were collected by the CarChip Pro. In the STEER intervention, families were instructed to insert the CarChip Pro into the car anytime the teenager was driving, and to bring it back to each weekly session. At each session, clinicians then reviewed data collected by the engine and driving performance monitor including speed (top speed, speed variability), hard braking, and hard accelerations. Teens were reinforced for evidence of safe and effective driving and clinicians discussed any risky behaviors that were present. During the driving simulation exercises, the teen drove and the parent rode as a passenger. The purpose of these simulations was two-fold: (1) they provided additional practice and experience in a safe environment for a novice driver and an opportunity for parents to practice parenting behaviors in the driving context; and (2) the exercise promoted discussion between the parent, teen, and clinician and afforded an opportunity for the provision of feedback on performance.
Each week, families created and reviewed a behavioral contract that targeted issues related to driving. Contingency contracts linked objective driving behaviors to agreed upon consequences – typically rewards but occasionally punishments. Parents and teens then agreed on how the contract would be monitored and set a date for evaluating and modifying the contract. These agreements were idiographic, and they reflected the concerns of the parent and adolescent. An example of a behavioral contract might include the target behavior of “Practice driving for at least three half-hour sessions with a parent (at least one of the practice sessions must be after dark).” The adolescent would then earn a privilege of their choice, such as driving through a drive-through for a cold drink following the final drive, as a reward. If the adolescent did not meet the contract by Friday, the driving sessions would need to occur on Saturday during the time the adolescent typically played videogames. For target behaviors that included driving outcomes (e.g., speed), CarChip Pro data were used as a means of monitoring and evaluating the outcome of the behavioral contract.
Treatment Attendance, Adherence, and Competence
Participant attendance in intervention was high. Completion was defined as attending all prescribed sessions (See Table 2). For STEER, 97% of families completed the family-based treatment (two families dropped out: one due to too many treatment demands and the other was due to concern regarding emerging teen substance use) and 95% completed the driver education program. Specifically for the STEER sessions, 67% were attended by the mother only, 19% were attended by the father only, and 14% were attended by two parents. For DEDP, 98% of teens completed treatment (two families dropped out: one due to increased family problems that precluded participation and one because a non-custodial father did not want the teen in the program) and 92% completed the driver education program.
To determine whether the interventions were implemented as prescribed (Perepletchikova & Kazdin, 2005), every session was videotaped and reviewed by a clinical supervisor to assess intervention adherence (i.e., that the intervention was implemented as intended) and competence (i.e., the quality of implementation). For STEER, 66 parent sessions, 77 teen sessions, and 55 shared sessions were reviewed, and there was at least one session reviewed for each STEER participant. For the parent session, 91% of prescribed intervention components were included, for the teen session 96% of components were included, and the shared session included 94% of required components. Following review of the videotape, supervisors also rated the clinician competence across a range of operationally defined attributes including facial expression, communication through postures/gestures, communication/social reinforcement, feedback, alliance, and overall climate. Ratings ranged from 1 indicating a lack of competence to 7 indicating strong evidence of competence. Mean ratings of overall competence were 6.5 (SD=.15), 6.62 (SD=.10), and 6.86 (SD=.04) for the parent, teen, and shared sessions, respectively in STEER. For the driving simulator sessions in DEDP, 94% of content was included as intended, and the competence rating was 6.45 (SD=.06). These data were used during supervision meetings with clinicians to guide videotape review and provide feedback to plan for subsequent treatment sessions.
Measures
Proximal Outcomes
Positive and negative parenting – Observational data
Parents and teens were asked to participate in a video-taped interaction in which they were asked to each discuss and attempt to resolve two recently contentious topics, each for 10 minutes. Topics were chosen from the parent and teen’s Issues Checklist (IC; Robin & Foster, 1989), a measure of parent and teen conflict wherein each rated how frequently a topic was discussed between the parent and teen in the last two weeks and how angry those conversations were. The angriest topic from each IC was used as the topics of discussion for the video-taped interactions (if there were multiple high scores for anger, the most frequent was chosen). Order of topic discussed first (parent or teen) was counterbalanced across the study.
Observations were coded using The Interaction Behavior Code (IBC). The IBC is a behavioral coding system designed to assess global impressions of parent-adolescent problem-solving and communication behavior. Coders were undergraduates who were unaware of both study hypothesis and group assignment. Coders were instructed to rate 32 behavioral items in terms of their presence or absence of the behaviors (items 1–22) or the frequency for items 23–32 (“no” = 0 points, “a little” = .5 point, and “a lot” = 1 point). Consistent with prior work using this coding system (Robin & Foster, 1989), we created a composite of positive parenting behaviors (e.g., praising, making suggestions, stating the other’s opinion, asking what the other would like) and negative parenting behaviors (e.g., yelling, ridicule, negative exaggeration, name-calling, interrupting with criticism, making demands). Undergraduate coders were trained to 80% agreement with a criterion tape and all observations of parent-teen interactions were coded three times to assess inter-rater reliability. Inter-class correlations were .67 for positive parenting and .75 for negative parenting. The IBC has documented reliability and validity (Foster, Prinz, & O’Leary, 1983; Prinz, 1977; Prinz & Kent, 1978).
Positive and negative parenting – ratings
Two parenting scales were administered to the parents of teens in the study: the Alabama Parenting Questionnaire (APQ) and the Parenting Scale (PS). The APQ (Frick, 1991) is a 42-item measure of parenting practices. Parents respond to each item based on a 5-point scale ranging from 1=never to 5=almost always. Scores are generated for several subscales used in this study including: involvement, positive parenting, poor monitoring/supervision. Higher scores indicate more frequent use of parenting behaviors within the subscale. Reliability for this measure has also been established in adolescent and in ADHD samples (Ellis & Nigg, 2009; Frick, Christian, & Wootton, 1999). There is evidence that aspects of parenting assessed by the APQ independently relate to ADHD (Ellis & Nigg, 2009).
The PS (Arnold, O’Leary, Wolff, & Acker, 1993) is a 30-item parent-report questionnaire regarding parents’ use of effective and ineffective parenting practices. For each item, parents are presented with a parenting situation (e.g., “At meal time”) and two potential parenting strategies they could use in that situation. One option is an effective parenting strategy (e.g., “I am the kind of parent that sets limits on what my child is allowed to do.”) and the other option is ineffective (e.g., “I let my child do whatever he/she wants.”). These two options are presented at the endpoints of a 7-point scale. Parents are asked to select the point on the scale that best describes their style of parenting. Scores are generated for the following subscales: Laxness, Over-reactivity, and Verbosity. Higher scores indicate more frequent use of ineffective parenting strategies. The Laxness, Over-reactivity, and Total Scores have been demonstrated to be reliable in a sample of children with ADHD (Harvey, Danforth, Ulaszek, & Eberhardt, 2001). In the present study, mothers completed these self-reported parenting measures at each assessment point. The scale evinces adequate indicators of concurrent and predictive validity (Arnold et al., 1993).
Distal Outcomes
Observations of driving behavior
Following the end of the intervention program, data regarding teen driving behavior was obtained over the course of a 4-week period following each assessment point through the use of an on-board video monitor, the T-Eye ADR3000 Mobile Event Data Recorder installed in all teens’ vehicles (kcicommunications.com/mobile/ teye.html). Teens were instructed to leave the T-Eye device plugged in each time they drove. The T-Eye device allowed for video observations of the driver’s view of the road, and video and audio recording of the vehicle’s interior cabin. The T-Eye device was activated by sudden changes in the vehicle’s trajectory (e.g., abrupt stops, fast starts, swerves, and collisions), which will be referred to as “risky events.” The device was also sensitive to relatively small bumps in the road and would be triggered even though the driver had not engaged in risky driving (referred to as “non-events”).1 Instances in which teens did not appropriately anticipate and slow down for large bumps in the road were coded as risky events due to imprudent speed. Each video was coded for teen behavior, parent behavior, and other aspects of the driving situation (e.g., cause of driving event, speed). Prior studies indicate that this recorded measurement of risky events is an accurate representation of poor driving behavior, can be reliably coded from video-taped review, and discriminates between ADHD and non-ADHD groups (Merkel et al., 2013) as well as being sensitive to treatment implementation (McGehee et al., 2007). In the present study, coders were able to reliably distinguish between risky events and non-events (Kappa = .72).
Objective negative driving events
Collisions and moving violation tickets (e.g., speeding, failure to yield right of way) were recorded based on any source including teen self-report, parent report, or official department of motor vehicles records obtained at the end of the study. These driving events consistently distinguish between ADHD and comparison groups, with ADHD groups experiencing a greater number of violations and collisions (Arduen et al., 2015; Jerome et al., 2006).
Teen self-reported driving questionnaire
Teenagers were asked whether they exhibited a wide range of driving behaviors (see Thompson, Molina, Pelham, & Gnagy, 2007). A total of 19 items were selected that were deemed to be objective indicators of driving on which teens could self-report (items related to alcohol/drug use while driving were omitted due to a low endorsement within the present and prior samples; see Thompson et al., 2007; a list of items is available from the first author). Exemplar items included making illegal turns, cutting others off while driving, ignoring stop signs, accelerating through a yellow light, driving more than 10 miles per hour beyond the posted speed limit, and switching lanes without looking. Item endorsement was dichotomized to indicate whether a teen ever reported engaging in each behavior at each assessment point. Principle components analyses of these dichotomized items indicated that a single dominant factor adequately represented these data at each assessment period (e.g., a single dominant eigenvalue was evident from scree plots). As such, an overall mean score of dichotomized items was constructed to represent teen self-report of overall risky driving behaviors at each assessment. The items used within this study were internally consistent with alphas of .74, .72, and .77, at end of treatment, six-month, and 12-month follow-ups, respectively. These items have distinguished between drivers that receive multiple violations for driving and the general population in prior work (Donovan, 1985).
Satisfaction with treatment
To obtain a measure of parent satisfaction with the STEER intervention, and compare it to satisfaction in the DEDP condition, parents and teens completed a measure of consumer satisfaction at the end of the treatment period. The measure was an adapted version of the satisfaction measure used in the MTA study (Pelham et al., under review). The measure has three factors: treatment satisfaction, perceived improvement, and demands of treatment. Averages for each factor ranged from one to seven with higher scores indicating more satisfaction, greater perceived improvement, and greater demandingness. Internal consistencies on the parent factor were acceptable for treatment satisfaction (coefficient alpha = .87), perceived improvement (coefficient alpha = .72), and demands of treatment (coefficient alpha = .84) in previous research (Pelham et al., under review). Multiple studies indicate that the measure is sensitive to treatment effects (Fabiano et al., 2012; Pelham et al., under review).
Analytic Strategy
Proximal outcomes (i.e., parenting behaviors) were measured at baseline, end of treatment and six- and 12-month follow-ups. As such, in order to maximize statistical power to detect treatment effects, intent to treat analyses used the baseline score as a covariate. Distal outcomes (i.e., driving related behaviors) were measured at end of treatment and six- and 12-month follow-ups. Baseline assessments of driving related behaviors were missing by design (because only permitted drivers were recruited into the study). Hence, intent to treat analyses for distal outcomes used treatment status as the sole predictor.
Proximal outcomes were continuously distributed. As such, analyses of covariance (ANCOVA) models were used throughout. Although not reported, we tested and confirmed that the homogeneity of regression coefficients assumption was met (i.e., none of the treatment x baseline interaction terms were statistically significant). In contrast, some of the distal outcomes were either dichotomous (e.g., presence of a ticket or accident) or represented counts (e.g., number of camera events obtained from 1-month recordings that were made at each assessment). As such, a combination of analysis of variance (for continuous outcomes—teen reports of total risky driving behaviors), negative binomial regression (for count outcomes which exhibited a preponderance of 0s—camera events), and logistic regression (for dichotomous outcomes— tickets or accidents) models were used to evaluate distal outcomes.
All intent to treat models were re-estimated twice in order to test whether the magnitude of treatment effects varied as a function of adolescent stimulant use (i.e., stimulant use and stimulant use x treatment terms were included, and the statistical significance of the stimulant use x treatment term informed moderation). In the first iteration of models, baseline stimulant use was included as a potential moderator variable. In the second iteration of models, stimulant use at the time of the outcome assessment was included as a potential moderator variable.
To reduce inferential statistical tests and improve the reliability of our measurement approach, composite variables were created for the parenting outcomes within the study. A combination of principle components (PCA) and exploratory factor analyses (EFA) were used to reduce four subscales from the Alabama Parenting Questionnaire (APQ; inconsistent discipline, positive parenting, involvement, monitoring-supervision) and three subscales from the Parenting Scale (PS; laxness, verbosity, over-reactivity) into parent self-rated composites of their own parenting behavior. PCA and EFA models were applied separately to data obtained at each of the four assessment periods (baseline, end of treatment, 6- and 12-month follow-ups). A consistent pattern of results emerged across assessments, which indicated that a two-factor solution was optimal (factors were moderately inversely correlated −.29 to −.36; indicators demonstrated simple structure). All subscales were standardized with respect to the baseline mean and standard deviation (e.g., [end treatment M - baseline M]/baseline SD), which resulted in each subscale having a comparable metric (i.e., negative values represented lower scores relative to the baseline mean, while positive values represented higher scores relative to the baseline mean). A positive parenting composite was formed by taking the mean of the positive parenting, involvement, and monitoring-supervision (reverse scored) subscales of the APQ (αs = .60 – .68 across assessments). A negative parenting composite was formed by taking the mean of the three PS subscales (laxness, verbosity, over-reactivity) and the inconsistent discipline of the APQ (αs = .73- .76 across assessments). These positive and negative composites were interpretable on the same z score metric as the standardized subscale scores.
Results
Descriptive Statistics
Descriptive statistics for all study outcome variables at each assessment are provided in Table 3. One point is noteworthy. With respect to driving related outcomes (see Table 3), the rates of licensed driving behavior increased substantially over the course of the study (from 7% at baseline to 67% at the 12-month follow-up), and this was statistically significant.
Table 3.
Descriptive Statistics for Proximal and Distal Study Outcomes by Assessment Occasion
| Pre |
Post |
6MO |
12MO |
|||||
|---|---|---|---|---|---|---|---|---|
| Outcome Variable | n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) |
| STEER - Proximal | ||||||||
| Positive Parenting (Obs) |
85 | 0.47 (0.13) |
80 | 0.44 (0.13) |
78 | 0.46 (0.15) |
76 | 0.44 (0.13) |
| Negative Parenting (Obs) |
85 | 0.24 (0.10) |
80 | 0.23 (0.09) |
78 | 0.23 (0.10) |
76 | 0.22 (0.10) |
| Positive Parenting (Rating) |
86 | −0.08 (0.77) |
83 | −0.14 (0.82) |
81 | −0.01 (0.93) |
79 | −0.07 (0.95) |
| Negative Parenting (Rating) |
86 | 0.08 (0.72) |
83 | −0.13 (0.70) |
81 | −0.10 (0.71) |
79 | −0.28 (0.71) |
| DEDP - Proximal | ||||||||
| Positive Parenting (Obs) |
86 | 0.47 (0.11) |
81 | 0.46 (0.12) |
76 | 0.45 (0.12) |
74 | 0.44 (0.12) |
| Negative Parenting (Obs) |
86 | 0.24 (0.09) |
81 | 0.25 (0.10) |
76 | 0.25 (0.10) |
74 | 0.23 (0.08) |
| Positive Parenting (Rating) |
86 | 0.08 (0.73) |
83 | −0.04 (0.74) |
77 | 0.16 (0.80) |
76 | 0.16 (0.80) |
| Negative Parenting (Rating) |
86 | −0.08 (0.81) |
83 | −0.14 (0.79) |
77 | −0.15 (0.75) |
76 | −0.32 (0.81) |
| STEER – Distal | ||||||||
| Is Licensed Driver | 83 | 8% | 80 | 49% | 80 | 65% | ||
| Camera Events | 76 | 3.95 (6.71) |
65 | 5.71 (10.13) |
54 | 10.98 (13.71) |
||
| Accidents | 83 | 0.07 (0.26) |
81 | 0.19 (0.39) |
79 | 0.19 (0.45) |
||
| Tickets | 83 | 0.04 (0.24) |
81 | 0.10 (0.34) |
80 | 0.13 (0.60) |
||
| Driving Risks (Self) | 74 | 0.12 (0.09) |
76 | 0.14 (0.13) |
76 | 0.18 (0.16) |
||
| DEDP – Distal | ||||||||
| Is Licensed Driver | 84 | 6% | 78 | 51% | 78 | 69% | ||
| Camera Events | 80 | 3.20 (5.21) |
72 | 6.85 (10.28) |
64 | 9.89 (13.49) |
||
| Accidents | 84 | 0.08 (0.32) |
78 | 0.12 (0.36) |
78 | 0.22 (0.53) |
||
| Tickets | 84 | 0.00 (0.00) |
78 | 0.08 (0.39) |
78 | 0.15 (0.43) |
||
| Driving Risks (Self) | 75 | 0.16 (0.14) |
76 | 0.18 (0.15) |
75 | 0.22 (0.16) |
||
Note. DEDP=Driving Education and Driving Practice; MO=month follow-up; Obs=Composite score of observational measures; Rat=Composite score of rating scale measures; Self=Self-reported risky driving behaviors; STEER=Supporting a Teen’s Effective Entry to the Roadway; Tickets=moving violation tickets.
Proximal Outcomes – Parenting
For parenting outcomes, baseline scores on the measure were entered as a covariate in analyses. As is summarized in Table 4, participants in the STEER program were observed to exhibit lower levels of observed negative parenting behaviors at the end of treatment (F (1, 158) = 8.0, p = .005, Cohen d = .38) and 6-month follow-up (F (1, 151) = 7.1, p = .009, Cohen d = .40) but not the 12-month follow-up (F (1, 147) = 1.9, p = .17, Cohen d = .19). However, the STEER program was not associated with any increases in either observed or self-rated levels of positive parenting behaviors. STEER was not associated with any reductions in self-rated negative parenting behaviors.
Table 4.
Test Values and Statistics for Proximal and Distal Study Outcomes by Assessment Occasion
| Post |
6MO |
12MO |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome Variable |
LSM (SE) |
Test Statistic |
d | LSM (SE) |
Test Statistic |
d | LSM (SE) |
Test Statistic |
d |
| Proximal Outcomes | |||||||||
| Positive Parenting (Obs) | |||||||||
| STEER | 0.44 (0.01) |
F=1.8 (1, 158) |
0.20 | 0.46 (0.01) |
F=03 (1, 151) |
−0.08 | 0.44 (0.01) |
F=0.01 (1, 147) |
−0.02 |
| DEDP | 0.46 (0.01) |
0.45 (0.01) |
0.44 (0.01) |
||||||
| Negative Parenting (Obs) | |||||||||
| STEER |
0.22 (<0.01) |
F=8.0 (1, 158)** |
0.38 |
0.22 (<0.01) |
F= 7.1 (1 151)** |
0.40 | 0.21 (<0.01) |
F=1.9 (1, 147) |
0.19 |
| DEDP |
0.26 (<0.01) |
0.26 (0.01) |
0.23 (<0.01) |
||||||
| Positive Parenting (Rat) | |||||||||
| STEER | −0.05 (0.05) |
F=1.0 (1, 163) |
0.10 | 0.08 (0.07) |
F=0.0 (1, 155) |
−0.01 | 0.02 (0.08) |
F=0.1 (1, 152) |
0.05 |
| DEDP | −0.12 (0.05) |
0.07 (0.07) |
0.06 (0.08) |
||||||
| Negative Parenting (Rat) | |||||||||
| STEER | −0.20 (0.05) |
F=2.9 (1, 163) |
0.16 | −0.16 (0.06) |
F=1.1 (1, 155) |
0.11 | −0.35 (0.06) |
F=1.7 (1, 152) |
0.15 |
| DEDP | −0.07 (0.05) |
−0.08 (0.06) |
−0.24 (0.06) |
||||||
| Distal Outcomes | |||||||||
| Driving Risk (Self) | |||||||||
| STEER |
0.12 (0.01) |
F=6.3 (1, 147)* |
0.41 |
0.14 (0.02) |
F=4.6 (1, 150)* |
0.40 | 0.18 (0.02) |
F=3.4 (1, 149) |
0.40 |
| DEDP |
0.16 (0.01) |
0.18 (0.02) |
0.22 (0.02) |
||||||
| Camera Events | |||||||||
| STEER | 3.95 (0.73) |
χ2=0.7 (1) | 5.71 (1.09) |
χ2=0.5 (1) | 10.98 (1.97) |
χ2=0.2 (1) | |||
| DEDP | 3.20 (0.58) |
6.84 (1.23) |
9.89 (1.63) |
||||||
| Post | 6MO | 12MO | |||||||
| Outcome Variable |
OR (95% CI) |
χ2 (1) | OR (95% CI) |
χ2 (1) | OR (95% CI) |
χ2 (1) | |||
| Distal Outcomes | |||||||||
| License | |||||||||
| STEER | 1.46a (0.44, 4.78) |
0.38 | 0.90a (0.48, 1.69) |
0.10 | 0.83a (0.42, 1.61) |
0.32 | |||
| DEDP | 1a(Ref) | 1a(Ref) | 1a(Ref) | ||||||
| Any Accidents or Tickets | |||||||||
| STEER | 1.20a (0.39, 3.73) |
0.10 | 1.69a (0.76, 3.76) |
1.63 | 0.78a (0.37, 1.65) |
0.43 | |||
| DEDP | 1a(Ref) | 1a(Ref) | 1a(Ref) | ||||||
Note. p<0.05,
p<0.01;
ddf=denominator degrees of freedom; DEDP=Driving Education and Driving Practice; df=degrees of freedom; LSM=Least Squares Mean (i.e., adjusted for baseline); MO=month follow-up; ndf=numerator degrees of freedom; Obs=Composite score of observational measures; OR=Odds Ratio; ndf=numerator degrees of freedom; Rat=Composite score of rating scale measures; Self=Self-reported risky driving behaviors; STEER=Supporting a Teen’s Effective Entry to the Roadway.
Distal Outcomes - Driving
As is summarized in Table 4, the STEER program was associated with statistically significant, lower levels of teen self-reported risky driving behaviors at the end of treatment (F (1, 147) = 6.3, p = .001, Cohen d = .41) and 6-month follow-up (F (1, 150) = 4.6, p = .03, Cohen d = .40), with the 12-month follow-up being non-significant (F (1, 149) = 3.4, p = .07, Cohen d = .40). In contrast, none of the treatment comparisons for observed driving behaviors (camera events; Table 4) or incidents (accidents, tickets; Table 4) were significantly different. Participation in STEER was not differentially associated with licensure status at end of treatment or follow-ups.
Moderator Analyses
All of the intent to treat analyses for proximal and distal outcomes were repeated using stimulant use as a potential moderator variable (i.e., stimulant use and stimulant use x treatment terms were added to the model). The statistical significance of the stimulant use x treatment term was a formal test of moderation. All models were estimated twice, once using stimulant use at baseline and a second time using stimulant use at the outcome assessment (e.g., stimulant use at the 6-month follow-up assessment was used as a potential moderator of 6-month follow-up outcomes). The stimulant use x treatment term was not statistically significant using either specification or any outcome. Hence, the STEER program appeared to work equally well for teens irrespective of their stimulant medication status.
Treatment Satisfaction
Participants were highly satisfied with both intervention groups. Mothers and teens receiving the STEER intervention (n=83) rated their treatment satisfaction as 6.44 (SD=0.63) and 6.06 (SD=0.89), their perceived improvement as 5.91 (SD=0.70) and 5.73 (SD=0.86), and their satisfaction with the treatment demands as 5.93 (SD=0.78) and 5.61 (SD=1.09), respectively. Likewise, mothers and teens receiving the DEDP condition (n=81) rated their treatment satisfaction as 6.24 (SD=0.71) and 6.21 (SD=0.69), their perceived improvement as 5.77 (SD=0.78) and 5.92 (SD=0.72), and treatment demands as 5.97 (SD=0.82) and 5.85 (SD=0.80), respectively. Differences in satisfaction between groups were not statistically significant.
Discussion
This study provided the first randomized, controlled trial of a psychosocial treatment aimed at reducing driving impairments in youth with ADHD. The intervention included a multiple-component effort to address parenting, family functioning and communication, technologies to monitor and support safe driving, and driver education and training. Relative to a comparison condition, the STEER intervention yielded reductions in negative parenting behaviors. Positive parenting behaviors were unchanged. During follow-up evaluations of driving outcomes, teens reported fewer risky driving behaviors in the STEER condition, but there were no significant differences on the frequency of risky driving events captured by an objective driving monitor. Whether the teen was prescribed stimulant medication at baseline, or at the specific assessment period did not moderate outcomes. Each of these major results will be discussed in turn, limitations of the study will be noted, and the implications of these findings for future intervention efforts will be described.
A key component of the STEER intervention was the parent training based on Barkley, et al. (1999). Prior research indicated that a parent training approach similar to that used within the present study resulted in mothers significantly increasing positive and decreasing negative behaviors as observed during a mother-teen interaction (Barkley et al., 2001). In the present study, the significant reduction in negative parenting was replicated whereas the positive parenting behaviors were not significantly different between groups. One difference between the present investigation and the Barkley et al. (2001) study was that the average age of the youth in the latter study was younger, at approximately 14 years of age. One might speculate that negative behaviors (i.e., sarcasm, put-downs) were relatively easier to modify as they occurred frequently during driving scenarios, the primary focus of the parenting intervention, whereas positive parenting behaviors occurred rarely (see Schatz et al., 2014). The higher frequency of negative parenting behaviors during driving may have made this a more malleable target of the intervention. These parent reductions in negative parenting behaviors maintained a full six months later, waning at the 12-month follow-up. This is different than Barkley et al. (2001) where the observations of mother behaviors were improved at post-treatment but not two-month follow-up. Perhaps the focus in the present investigation on a particular developmental transition (i.e., driving) helped parents practice and maintain alternative parenting strategies in a more effective manner than a parenting program focused on general disruptive behavior. Behavioral parent training that focuses on specific parenting skills, with practice in naturalistic settings, has resulted in remarkable follow-up (i.e., maintenance of gains over years) in samples of young children (Hood & Eyberg, 2003; Reid et al., 2003). The present study suggests that a behavioral parent training approach with adolescents, when focused on a specific set of skills (i.e., teaching a teen to drive safely) may confer similar benefits, and this idea may warrant further investigation within adolescent samples.
Parents did not self-report improvements in parenting following participation in the STEER study. One reason for this may have been the general nature of the items on the scales, which may have been less sensitive to change than the observations of behaviors within the laboratory. It is also possible that changes in negative parenting observed were less perceptible to the parents when they considered their parenting approach, in general. Finally, whereas the observational code used was developed specifically for adolescents in a parent-teen interaction that discusses current, conflictual topics (Robin & Foster, 1989), the parenting scales represent general parenting strategies and behaviors and therefore may have been less precise. These results are also consistent with Barkley et al. (2001) where parent self-reported ratings of parent-teen interactions were not changed in a clinically significant manner.
The distal outcome of the study was teen driving behavior. The study outcomes yielded mixed results wherein youth with ADHD self-reported significantly fewer risky driving behaviors yet objective observations of driving behaviors were not significantly different. Although adolescents with ADHD are typically viewed as being poor self-evaluators for their own ADHD symptoms (Sibley et al., 2012), they may be reasonable informants for behaviors that are outside of typical adult awareness (e.g., covert behaviors; Hart, Lahey, Loeber, & Hanson, 1994; Cantwell, Lewinsohn, Rohde, & Seeley, 1997). In a recent study, it was observed that teens were poor reporters of global driving behavior on a driving simulator relative to an objective observer, but this deficiency in self-reporting was considerably attenuated when teens were asked to report on specific aspects of their performance (e.g., speeding, running stop signs; Fabiano et al., 2015). The current measure of teen driving collected via self-report queried specific risky driving events, likely illustrating some improved driving at end of treatment and 6-month follow-up following the STEER intervention relative to DEDP.
The objective driving behaviors were recorded during 4-week periods at the end of treatment, 6-months later, and at 12-month follow-up. The measure was characterized by extreme positive skewness and a low baserate which impacted analyses. It is clear from a review of Table 3 that there were few camera events recorded at the end of treatment when most participants were still unlicensed, and that the frequency of risky driving events recorded increased as greater percentages of teens were licensed at each assessment point. Other scholars have utilized a much longer observation period with young adults (Arduen, Kofler, Cox, Sarver, & Lunsford, 2015). It is possible that the relatively short observation period of one-month, coupled with the focus on a low baserate behavior and relatively few licensed, independent drivers, resulted in a coarse measure of driving outcome following intervention. Future studies should time interventions and outcome assessment to the first months of licensure as this has consistently been identified as the riskiest time for teen drivers (Williams, 2003).
These apparently discrepant findings wherein teen self-report of driving was significantly improved in STEER relative to DEDP, but there were no significant differences on observed risky behaviors may be reconciled by considering the type of information provided by these two methods. When teenagers are driving they may engage in many behaviors that evince poor judgment or low skill. This might include speeding, failing to yield at intersections or rolling through stop signs, making turns too sharply, or abruptly changing lanes. The chances that any one of these errors will result in a ticket, collision, or “near miss” is low, but cumulatively, over the course of weeks of driving, increased instances of these behaviors puts the teen at greater risk. The observational measure of driving was only recorded if there was an abrupt change in vehicle trajectory – for instance if a teenager was imprudently speeding and had to stop abruptly at a light that changed from green to red. Imprudently speeding through a yellow light would not have been recorded via our measure. However, teens might be able to report poor driving behaviors such as this as occurring on the self-report measure, which generated greater variability in responses and therefore group differences. Future work is needed to determine the best measures, and combination of measures, that provide reliable and valid indicators of specific risky driving behaviors. Strategies to incorporate diverse technologies into measurement approaches (e.g., CarChip Pro, T-Eye camera) are also candidates for further study.
ADHD drivers are significantly more likely to be older when initially licensed (Curry, Pfeiffer, Durbin, & Elliott, 2015; Molina et al., 2009; Thompson et al., 2007). This was also observed in our sample where teens completed the intervention as well as the driver education training, but licensure rates were modest until the 12-month outcome assessment – even at this point a third of the adolescents were still unlicensed. It is unclear why teens with ADHD are likely to be relatively older licensed drivers. Perhaps parents decide to keep the teen in a permitted stage longer due to concerns regarding inattention or impulsive decision-making. It is also possible teens with ADHD are less motivated to become independent drivers. Regardless, graduated driver’s licensing restrictions have substantively reduced teen morbidity and mortality in states that utilize them (Shope, 2007). However, most ages targeted by graduated driver licensing policy are 16–18. One side effect of youth with ADHD remaining in the permitted stage for greater periods of time is that they may spend less time under the graduated driver licensing restrictions as novice, licensed drivers. This potential cost is even more concerning given findings that the benefits of later licensing attenuate after about six months (Curry, et al., 2015). One explanation for the waning of treatment effects at the 12-month follow-up, for both parenting and driving outcomes, may have been the long lag between intervention and independent driving. If youth with ADHD in community settings are exposed to similar lags, they may receive less benefit from driving preparation efforts relative to typically developing peers.
A final note worth mentioning is the strong attendance in the interventions within the study. Teenagers with ADHD are not known for being reliable and consistent patients in clinical settings (Wolraich et al., 2005), yet nearly every teen and their parent completed nearly every driver education session, parent/teen therapy session, and simulator practice session. These high rates of attendance may have been influenced by timing treatment to an important developmental transition – learning to drive. Parents may have been highly motivated to obtain intervention to address concerns about the safety of their teen and adolescents may have been motivated to participate due to the expectation of gaining the ability to drive independently. Future treatment efforts may explore aligning intervention efforts for ADHD with other developmental transitions (e.g., beginning kindergarten; entering the workforce) to promote family-based attendance.
Limitations
This study has limitations. There was no business as usual control group, as all teens had an intensive driver education program. It is possible that results would be interpreted differently with a different comparison group for STEER. Further, results may not generalize to families where there is less parental involvement in the transition to licensed driving due to the present study’s requirement of at least one parent participating in the treatment. It is also not possible from this study to determine the degree to which medication was effective for teen drivers as whether the adolescent was prescribed psychoactive medication was distributed across groups but not directly manipulated. As mentioned, the duration of the driving evaluations using the onboard camera may also have been of insufficient duration for adequately assessing the low baserate, negative driving behaviors. Further, the timing of assessments was not directly aligned with the first month of independent driving – studies that timed assessment to this critical transition point may yield different results (Williams, 2003). Finally, it is not clear these results would generalize to older adolescents, teens with ADHD who are diagnosed with the primarily inattentive or hyperactive/impulsive presentation of ADHD, or those with a driving license without intensive intervention during the driving training period (see Fabiano et al., 2011). It is also important to note that the STEER participants received more attention and interaction with study clinicians due to the additional treatment meetings and this may have influenced results. On the other hand, the families in the STEER intervention also had increased demands on their scheduling, time, and resources given the additional meetings, yet this did not appear to impact satisfaction with treatment for the parent or teen. Further studies that more precisely match intervention demands may be needed to rule out the influence of clinician interaction and attention on results. The measurement of the teen’s driving behavior could have been influenced by noncompliance with camera use, though most teens had camera data recorded each week when they indicated driving. Future studies might rely on hard-wired cameras that record any time the vehicle is operated as in Arduen et al. (2015). An additional limitation of this study is that intervention adherence and competence ratings were completed by supervisors rather than objective observers and that psychometric information on the ratings was not available. Finally, because this was a multi-component intervention, it is not possible to disentangle which treatment components were effective (or ineffective), for whom. Innovative study designs that systematically randomize novice teen drivers to different intensities and sequences of driving interventions (Pelham et al., 2016), including the STEER intervention components, may improve the precision of future treatment recommendations.
Conclusion
The present study is the first to empirically evaluate a psychosocial intervention to support teenagers with ADHD during their transition to independent driving. The STEER intervention was strongly attended by both parents and teens in spite of a demanding regimen. The intervention was implemented with a high degree of integrity and fidelity. Relative to a DEDP control, youth with the STEER intervention had parents who utilized fewer negative parenting strategies as measured in the laboratory at end of treatment and 6-months later, but these effects dissipated 12-months later. Positive parenting observations and parental self-report did not differ across groups. Distal outcomes of interventions yielded significantly reduced rates of teen self-report of risky driving in STEER versus DEDP at end of treatment and 6-month assessments, but not 12-month. Rates of observed risky driving and accidents/citations did not differ across groups. This study represents the first to directly target teenage driving using a psychosocial intervention for families of youth with ADHD, and yielded mixed outcomes. Future work is needed to determine the best time to implement intensive family-focused interventions for youth with ADHD (i.e., pre-licensure, post-licensure, or across pre- to post-licensure), the intensity of treatment needed to offset negative driving outcomes, and the appropriate sequencing of driver training, family-focused interventions, and combined pharmacological treatment. For example, parents were trained in STEER to support the teen during efforts to learn to drive, but many outcome assessments occurred when the teenager had moved on to independent driving. Future treatment efforts might incorporate continued treatment throughout this transition to support parents and teenagers with negotiating new situations such as curfew, being responsible with the car (e.g., filling the gas tank after use, returning it when planned) as well as assisting the parents with continued monitoring and contingency management after their presence within the car cabin is reduced (see Farmer et al., 2009). Given the potential seriousness of the negative outcomes associated with risky driving, the present study should be used as a stepping stone for continued study within this area, with the ultimate goal of increasing the safety for youth with ADHD and the others who share the roadway with them.
Footnotes
The device was set at a conservative g-force trigger level for the first 23 participants in the study. This was modified to a moderate setting to increase the sensitivity of the data collection of the device for the remaining participants. There was no difference in the pattern of results when the initial subjects were removed from the analyses, so analyses include all participants regardless of the setting. Within subjects, the same setting was used throughout all assessment points in the study.
Contributor Information
Gregory A. Fabiano, University at Buffalo, State University of New York
Nicole K. Schatz, University at Buffalo, State University of New York
Karen L. Morris, University at Buffalo, State University of New York
Michael T. Willoughby, RTI International
Rebecca K. Vujnovic, University at Buffalo, State University of New York
Kevin F. Hulme, University at Buffalo, State University of New York
Jessica Riordan, University at Buffalo, State University of New York.
Marlana Howard, University at Buffalo, State University of New York.
Dwight Hennessy, Buffalo State College, State University of New York.
Kemper Lewis, University at Buffalo, State University of New York.
Larry Hawk, University at Buffalo, State University of New York.
Amanda Wylie, RTI International.
William E. Pelham, Jr, Florida International University.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- American Academy of Pediatrics, Committee on Injury, Violence, and Poison Prevention, Committee on Adolescence. The Teen Driver. Pediatrics. 2006;118:2570–2581. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Arduen PA, Kofler MJ, Cox DJ, Sarver DE, Lunsford E. Motor vehicle driving in high incidence psychiatric disability: Comparison of drivers with ADHD, depression, and no known psychopathology. Journal of Psychiatric Research. 2015;64:59–66. doi: 10.1016/j.jpsychires.2015.03.009. [DOI] [PubMed] [Google Scholar]
- Arnold DS, O’Leary SG, Wolff LS, Acker MM. The parenting scale: A measure of dysfunctional parenting in discipline situations. Psychological Assessment. 1993;5(2):137–144. [Google Scholar]
- Anastopoulos AD, Shelton TL. Assessing Attention-Deficit/Hyperactivity Disorder. New York: Kluwer Academic Publishing; 2001. [Google Scholar]
- Barkley RA, Cox D. A review of driving risks and impairments associated with attention-deficit/hyperactivity disorder and the effects of stimulant medication on driving performance. Journal of Safety Research. 2007;38:113–128. doi: 10.1016/j.jsr.2006.09.004. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Edwards GH, Laneri M, Fletcher K, Metevia L. The efficacy of problem-solving communication training alone, behavior management training alone, and their combination for parent-adolescent conflict in teenagers with ADHD and ODD. Journal of Consulting and Clinical Psychology. 2001;69(6):926–941. [PubMed] [Google Scholar]
- Barkley RA, Edwards GH, Robin AL. Defiant Teens, First Edition: A Clinician’s Manual for Assessment and Family Intervention. New York, NY: The Guilford Press; 1999. [Google Scholar]
- Barkley RA, Guevremont DG, Anastopoulos AD, Fletcher KF. A comparison of three-family therapy programs for treating family conflicts in adolescents with attention-deficit hyperactivity disorder. Journal of Consulting and Clinical Psychology. 1992;60:450–462. doi: 10.1037/0022-006X.60.3.450. [DOI] [PubMed] [Google Scholar]
- Beck KH, Hartos JL, Simons-Morton BG. Parent-teen disagreement of parent-imposed restrictions on teen driving after one month of licensure: Is discordance related to risky teen driving? Prevention Science. 2005;6:177–185. doi: 10.1007/s11121-005-0001-6. [DOI] [PubMed] [Google Scholar]
- Beck KH, Shattuck T, Raleigh R. Parental predictors of teen driving risk. American Journal of Health Behavior. 2001;25:10–20. doi: 10.5993/ajhb.25.1.2. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza BM. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Cantwell DP, Lewinsohn PM, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 10 Leading Causes of Death, United States: 2013 All races, both sexes. 2013 Downloaded from: http://webappa.cdc.gov/cgi-bin/broker.exe.
- Clinton KM, Lonero L. Evaluating Driver Education Programs: Comprehensive Guideline. Cobourg, Ontario: Northport Associates; 2006. [Google Scholar]
- Cochrane Injuries Group Driver Education Reviewers. Evidence based road safety: The Driving Standards Agency’s Schools Programme. Lancet. 2001;358:230–232. doi: 10.1016/S0140-6736(01)05416-2. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Humphrey JW, Merkel L, Penberthy JK, Kotatchev B. Controlled-release methylphenidate improves attention during on-road driving by adolescents with attention-deficit/hyperactivity disorder. Journal of the American Board of Family Practice. 2004;17:235–239. doi: 10.3122/jabfm.17.4.235. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Merkel L, Moore M, Thorndike F, Muller C, Kovatchev B. Relative benefits of stimulant therapy with OROS methylphenidate versus mixed amphetamine salts extended release in improving the driving performance of adolescent drivers with attention-deficit/hyperactivity disorder. Pediatrics. 2006;118:e704–e710. doi: 10.1542/peds.2005-2947. [DOI] [PubMed] [Google Scholar]
- Curry A, Metzger K, Pfeiffer M, Power T, Winston F, Elliott M. Driver licensing rates and crash risk among adolescents with ADHD: A retrospective cohort study; Chicago, IL. Poster presented at the American Public Health Association conference.2015. [Google Scholar]
- Curry AE, Pfeiffer MR, Durbin DR, Elliott MR. Young driver crash rates by licensing age, driving experience, and license phase. Accident Analysis and Prevention. 2015;80:243–250. doi: 10.1016/j.aap.2015.04.019. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Queisser HR, Salzberg PM, Umlauf RL. Intoxicated and bad drivers: Subgroups within the same population of high-risk, men drivers. Journal of Studies on Alcohol. 1985;46:375–382. doi: 10.15288/jsa.1985.46.375. [DOI] [PubMed] [Google Scholar]
- Ellis B, Nigg J. Parenting practices and attention-deficit/hyperactivity disorder: New findings suggest partial specificity of effects. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(2):146–154. doi: 10.1097/CHI.0b013e31819176d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, Allen J, Moore S, Strauss V. Measuring symptoms and functioning of youth with ADHD in middle schools. Journal of Abnormal Child Psychology. 2005;33:695–706. doi: 10.1007/s10802-005-7648-0. [DOI] [PubMed] [Google Scholar]
- Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2013;43:527–551. doi: 10.1080/15374416.2013.850700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, Pelham WE, Smith BH, Bukstein O, Gnagy EM, Greiner AR, et al. Dose-response effects of methylphenidate on ecologically valid measures of academic performance and classroom behavior in adolescents with ADHD. Experimental and Clinical Psychopharmacology. 2001;9:163–175. doi: 10.1037//1064-1297.9.2.163. [DOI] [PubMed] [Google Scholar]
- Evans SW, Serpell ZN, Schultz B, Pastor D. Cumulative benefits of secondary school-based treatment of students with ADHD. School Psychology Review. 2007;36:256–273. [Google Scholar]
- Fabiano GA, Hulme KF, Linke S, Nelson-Tuttle C, Pariseau M, Gangloff B, Lewis K, Pelham WE, Waschbusch DA, Waxmonsky JG, Gormley M, Gera S, Buck M. The supporting a teen’s effective entry to the roadway (STEER) program: Feasibility and preliminary support for a psychosocial intervention for teenage drivers with ADHD. Cognitive and Behavioral Practice. 2011;18(2):267–280. [Google Scholar]
- Fabiano GA, Pelham WE, Waschbusch D, Gnagy EM, Lahey BB, Chronis AM, Onyango AN, Kipp H, Lopez-Williams A, Burrows-MacLean L. A practical impairment measure: Psychometric properties of the Impairment Rating Scale in samples of children with attention-deficit/hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology. 2006;35:369–385. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Schatz NK. Driving Interventions for Youth with Attention-deficit/Hyperactivity Disorder. In: Barkley RA, editor. Handbook on Diagnosis and Treatment of ADHD. New York, NY: The Guilford Press; 2014. pp. 705–727. [Google Scholar]
- Fabiano GA, Schatz NK, Aloe AA, Chacko A, Chronis-Tuscano A. A systematic review of meta-analyses of psychosocial treatment for attention-deficit/hyperactivity disorder. Clinical Child and Family Psychology Review. 2015;18:77–97. doi: 10.1007/s10567-015-0178-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabiano GA, Schatz NK, Hulme KF, Morris KL, Vujnovic RK, Willoughby MT, Hennessy D, Lewis KE, Owens J, Pelham WE. Positive bias in teenage drivers with Attention-Deficit/Hyperactivity Disorder within a simulated driving task. Journal of Attention Disorders. 2015 doi: 10.1177/1087054715616186. DOI: 10.1177/1087054715616186. [DOI] [PubMed] [Google Scholar]
- Farmar CM, Kirley BB, McCartt AT. In-vehicle monitoring and the driving behavior of teenagers. Arlington, VA: Insurance Institute for Highway Safety; 2009. [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Smallish L, Fletcher K. Hyperactive children as young adults: Driving abilities, safe driving behavior, and adverse driving outcomes. Accident Analysis and Prevention. 2007;39:94–105. doi: 10.1016/j.aap.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Christian RE, Wooton JM. Age trends in the association between parenting practices and conduct problems. Behavior Modification. 1999;23:106–128. [Google Scholar]
- Foster SL, Prinz RJ, O’Leary KD. Impact of problem-solving communication training and generalization procedures on family conflict. Child and Family Behavior Therapy. 1983;5:1–24. [Google Scholar]
- Frick PJ. The Alabama Parenting Questionnaire. Unpublished rating scale, University of Alabama; 1991. [Google Scholar]
- Forgatch M, Patterson G. Parents and adolescents living together, Part 2: Family problem solving. Eugene, OR: Castalia; 1989. [Google Scholar]
- Hart EL, Lahey BB, Loeber R, Hanson KS. Criterion validity of informants in the diagnosis of disruptive behavior disorders in children: A preliminary study. Journal of Consulting and Clinical Psychology. 1994;62:410–414. doi: 10.1037/0022-006X.62.2.410. [DOI] [PubMed] [Google Scholar]
- Hartung CM, McCarthy DM, Milich R, Martin CA. Parent-adolescent agreement on ADHD symptoms: A multi-trait, multi-method model. Journal of Psychopathology and Behavioral Assessment. 2005;27:159–168. [Google Scholar]
- Harvey E, Danforth JS, Ulaszek WR, Eberhardt TL. Validity of the parenting scale for parents of children with attention-deficit/hyperactivity disorder. Behaviour Research and Therapy. 2001;39(6):731–743. doi: 10.1016/s0005-7967(00)00052-8. [DOI] [PubMed] [Google Scholar]
- Hood KK, Eyberg SM. Outcomes of parent-child interaction therapy: Mothers’ reports of maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology. 2003;32:419–429. doi: 10.1207/S15374424JCCP3203_10. [DOI] [PubMed] [Google Scholar]
- Insurance Institute for Highway Safety. Teenagers: Driving Carries Extra Risk for Them. 2014 Downloaded from: http://www.iihs.org/iihs/topics/t/teenagers/fatalityfacts/teenagers.
- Jerome L, Segal A, Habinski L. What we know about ADHD and driving risk: A literature review, meta-analysis, and critique. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2006;15:105–125. [PMC free article] [PubMed] [Google Scholar]
- Lee JD. Technology and teen drivers. Journal of Safety Research. 2007;38:203–213. doi: 10.1016/j.jsr.2007.02.008. [DOI] [PubMed] [Google Scholar]
- Marcus SC, Wan GJ, Kemner JE, Olfson M. Continuity of methylphenidate treatment for attention-deficit/hyperactivity disorder. Archives of Pediatric and Adolescent Medicine. 2005;159:572–578. doi: 10.1001/archpedi.159.6.572. [DOI] [PubMed] [Google Scholar]
- McCartt AT, Hellinga LA, Haire ER. Age of licensure and monitoring teenagers’ driving: Survey of parents of novice teen drivers. Journal of Safety Research. 2007;38:697–706. doi: 10.1016/j.jsr.2007.10.002. [DOI] [PubMed] [Google Scholar]
- McGehee DV, Raby M, Carney C, Lee JD, Reyes ML. Extending parental mentoring using an event-triggered video intervention in rural teen drivers. Journal of Safety Research. 2007;38:215–227. doi: 10.1016/j.jsr.2007.02.009. [DOI] [PubMed] [Google Scholar]
- Merkel RL, Nichols JQ, Fellers JC, Hidalgo P, Martinez LA, Putzinger I, Burket RC, Cox DJ. Comparison of on-road driving between young adults with and without ADHD. Journal of Attention Disorders. 2013 doi: 10.1177/1087054712473832. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. MTA at 8 years: Prospective followup of children treated for combined-type ADHD in a multi-site study. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Smith BH, Pelham WE. Factor structure and criterion validity of secondary school teacher ratings of ADHD and ODD. Journal of Abnormal Child Psychology. 2001;29:71–82. doi: 10.1023/a:1005203629968. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. Moderators and mediators of treatment response for children and attention-deficit/hyperactivity disorder: The Multimodal Treatment Study of children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 1999;56:1088–1096. doi: 10.1001/archpsyc.56.12.1088. [DOI] [PubMed] [Google Scholar]
- Narad M, Garner AA, Brassell AA, Saxby D, Antonini TN, O’Brien KM, Tamm L, Matthews G, Epstein JN. Impact of distraction on the driving performance of adolescents with and without attention-deficit hyperactivity disorder. JAMA Pediatrics. 2013;167:933–938. doi: 10.1001/jamapediatrics.2013.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traffic Safety Facts 2005: A Compilation of Motor VehicleCrash Data from the Fatality Analysis Reporting System and the General Estimates System. Washington DC: U.S. Department of Transportation; 2005. National Highway Traffic Safety Administration, National Center for Statistics and Administration, U.S. Department of Transportation. [Google Scholar]
- Patterson G, Forgatch M. Parents and adolescents living together, Part 1: The basics. Eugene, OR: Castalia; 1989. [Google Scholar]
- Pelham WE, Fabiano GA. Evidence-based treatments for children and adolescents with ADHD: An update. Journal of Clinical Child and Adolescent Psychology. 2008;37:184–214. doi: 10.1080/15374410701818681. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Fabiano GA, Massetti GM. Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:449–476. doi: 10.1207/s15374424jccp3403_5. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms of the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Perepletchikova F, Kazdin AE. Treatment integrity and therapeutic change: Issues and research recommendations. Clinical Psychology: Science and Practice. 2005;12:365–383. [Google Scholar]
- Prinz RJ. The assessment of parent-adolescent relations: Discriminating distressed and non-distressed dyads. Unpublished doctoral dissertation, State University of New York at Stony Brook; 1977. [Google Scholar]
- Prinz RJ, Kent RN. Recording parent-adolescent interactions without the use of frequency or interval-by-interval coding. Behavior Therapy. 1978;9(4):602–604. [Google Scholar]
- Reid MJ, Webster-Stratton C, Hammond M. Follow-up of children who received the Incredible Years intervention for oppositional defiant disorder: Maintenance and prediction of 2-year outcome. Behavior Therapy. 2003;34:471–491. [Google Scholar]
- Reimer B, Mehler B, D’Ambrosio LA, Fried R. The impact of distractions on young adult drivers with attention deficit hyperactivity disorder. Accident Analysis and Prevention. 2005;42:842–851. doi: 10.1016/j.aap.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Robin AL, Foster AL. Negotiating Parent-Adolescent Conflict: A Behavioral-Family Systems Approach. New York, NY: The Guilford Press; 1989. [Google Scholar]
- Schatz NK, Fabiano GA, Morris KL, Shucard JM, Leo BA, Bieniek C. Parenting behaviors during risky driving by teens with attention-deficit/hyperactivity disorder. Behavior Therapy. 2014;45(2):168–176. doi: 10.1016/j.beth.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shope JT. Graduated driver licensing: Review of evaluation results since 2002. Journal of Safety Research. 2007;38:165–175. doi: 10.1016/j.jsr.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Shope JT, Molnar LJ. Graduated driver licensing in the United States: Evaluation results from early programs. Journal of Safety Research. 2003;34:63–69. doi: 10.1016/s0022-4375(02)00080-4. [DOI] [PubMed] [Google Scholar]
- Shope JT, Molnar LJ, Elliot MB. Graduated driver licensing in Michigan: Early impact on motor vehicle crashes among 16-year-old drivers. JAMA. 2001;286:1593–1598. doi: 10.1001/jama.286.13.1593. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Garefino AC, Kuriyan AB, Babinski DE, Karch KM. Diagnosing ADHD in adolescence. Journal of Consulting and Clinical Psychology. 2012;80:139–150. doi: 10.1037/a0026577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons-Morton BG, Hartos JL. How well do parents manage young driver crash risks. Journal of Safety Research. 2003;34:91–97. doi: 10.1016/s0022-4375(02)00085-3. [DOI] [PubMed] [Google Scholar]
- Smith BH, Molina BSG, Eggers SE. Parent-Teenager Negotiation Manual, Version 2.0. Unpublished treatment manual; 1997. [Google Scholar]
- Smith BH, Waschbusch DA, Willoughby MT, Evans S. The efficacy, safety, and practicality of treatments for adolescents with attention-deficit/hyperactivity disorder. Clinical Child and Family Psychology Review. 2000;3:243–267. doi: 10.1023/a:1026477121224. [DOI] [PubMed] [Google Scholar]
- Thompson AL, Molina BSG, Pelham WE, Gnagy EM. Risky driving in adolescents and young adults with childhood ADHD. Journal of Pediatric Psychology. 2007;32:745–759. doi: 10.1093/jpepsy/jsm002. [DOI] [PubMed] [Google Scholar]
- Weafer J, Camarillo D, Fillmore MT, Milich R, Marczinski CA. Simulated driving performance of adults with ADHD: Comparisons with alcohol intoxication. Experimental and Clinical Psychopharmacology. 2008;16:251–263. doi: 10.1037/1064-1297.16.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams AF. Teenage drivers: patterns of risk. Journal of Safety Research. 2005;34:5–15. doi: 10.1016/s0022-4375(02)00075-0. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, Wibbelsman CJ, Brown TE, Evans SW, Knight JR, Ross EC, Wilens T. Attention deficit hyperactivity disorder among adolescents: A review of the diagnosis, treatment, and clinical implications. Pediatrics. 2005;115:1734–1746. doi: 10.1542/peds.2004-1959. [DOI] [PubMed] [Google Scholar]
- Vernick JS, Guoha L, Ogaitis S, MacKenzie EJ, Baker SP, Gielen AC. Effects of high school driver education on motor vehicle crashes, violations, and licensure. American Journal of Preventive Medicine. 1999;16:40–46. doi: 10.1016/s0749-3797(98)00115-9. [DOI] [PubMed] [Google Scholar]
- Woodward LJ, Fergusson DM, Horwood LJ. Driving outcomes of young people with attentional difficulties in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:627–634. doi: 10.1097/00004583-200005000-00017. [DOI] [PubMed] [Google Scholar]