Abstract
Background
Infant deaths account for a majority of all pediatric deaths. However, little is known about the factors that influence parents to use hospice care for their infant with a life- threatening health condition.
Methods
Data were used from the 2007 to 2010 California Medicaid claims files (n=207). Analyses included logistic and negative binomial multivariate regression models.
Results
Over 15% of infants enrolled in hospice care for an average of 5 days. Infant girls and infants with congenital anomalies were more likely to enroll in hospice care with longer stays. However, cardiovascular and respiratory conditions were negatively related to hospice enrollment and hospice length of stay.
Conclusions
The study provides insights for nurses and other clinicians caring for infants and their families at end of life and suggests nurses can assist families in identifying infant hospice providers that may help families understand their options for end-of-life care.
Keywords: end-of-life, hospice, infants, Medicaid, Andersen model, complex chronic conditions
The word hospice generates a host of meanings for parents. Even when faced with imminent death, families cling to the hope that their child will survive. Parent’s often have a lack of understanding regarding pediatric hospice and palliative care services and therefore depend on the health care provider for both knowledge and expertise to guide decisions regarding end of life services. Infant health care providers should have a clear understanding of what these services can provide to infants and their families eliminating potential barriers to utilization and supporting best practices (National Hospice and Palliative Care Organization, 2009).
Hospice is a collaborative team approach to care for individuals at the end of life with the guiding philosophy to die pain free and with dignity (National Hospice and Palliative Care Organization, 2009). This term is used somewhat interchangeably with palliative care in the infant community, but there are clear differences. Palliative care, according to the statement of the American Academy of Pediatrics (American Academy of Pediatrics, 2013), is medical care for the child at any age or stage of a terminal illness with the goal to improve quality of life. Both hospice and palliative care have a family centered approach. Hospice has been shown to significantly improve the end of life care in adults with slow adaptation into the neonatal and pediatric health arena. Appropriate access to pediatric palliative and hospice care can provide a layer of support for families to make appropriate end of life decisions for their child.
BACKGROUND AND SIGNIFICANCE
Infant deaths account for a majority of all pediatric deaths in the United States. In 2013, 23,440 infants less than 1 year of age died, with two-thirds of these infants in the neonatal period of less than 28 days (Osterman, Kochanek, MacDorman, Strobino, & Guyer, 2015). Infant deaths are most commonly related to short gestation or prematurity, congenital anomalies, pregnancy complications or sudden death syndrome (SIDS) (Osterman et al., 2015). Although infant mortality rates have declined since the 1990s (MacDorman & Gregory, 2013), infant deaths continue to represent over 55% of all childhood deaths (Osterman et al., 2015). Infants born with life threatening health conditions often spend their short lives in the neonatal intensive care unit (NICU) with limited access to both palliative and hospice care (Chavoski, Miller, & Siden, 2013; Moura, Costa, Rodrigues, Almedia, Maia, & Guimaraes, 2011). Recent examination of infant utilization rates of hospice care is often the lowest when compared to other pediatric age groups (Leuthner, Boldt, & Kirby, 2004; Lindley & Lyon, 2013; Lindley & Shaw, 2014). Yet, many parents desire to bring their infants home at end of life, with support from hospice care that is available in their community (Brosig, Pierucci, Kupst, & Leuthner, 2007).
Factors associated with hospice care use for children and their families are well documented and include demographic characteristics, health status, and location or geography (Knapp, Shenkman, Marcu, Madden, & Terza, 2009; Lindley & Shaw, 2014; Lindley & Edwards, 2015; Lindley & Nageswaren, 2015; Lyon et al., 2008). However, little is known about factors that may influence parents to use hospice care for their infant with life threatening health conditions. What evidence we do have suggests that those with specific health conditions more commonly utilize hospice care. Leuthner and colleagues (2004) investigated hospice and home health care use among infants in Wisconsin from 1992 to 1996. They collected information from death certificates and surveyed all hospices and home health agencies in the state. They reported on 20 infants’ home deaths with hospice and home health and found that the common health conditions were trisomy 13 or 18, other genetic syndromes, congenital anomalies, hypoxic ischemic encephalopathy, cerebral atrophy, and congenital heart disease. These findings suggest that a variety of health conditions were represented among infant hospice and home health users. This lack of current and generalizable evidence is a significant gap in our understanding of infant hospice utilization.
Improving knowledge related to infant hospice use has significant policy and clinical relevance. With the recent passage of Concurrent Care for Children (Section 2302) of the Patient Protection and Affordable Care Act of 2010 (ACA), all children under 21 years, including infants, now have access to hospice care concurrent with medical treatment for their health condition (Lindley, 2011). Although a 6-month to live diagnosis is still required, parents no longer need to make a choice between stopping treatment and enrolling in hospice care. Under the new guidelines, the ACA may promote increased hospice use among infants and their families. Examining pre-ACA hospice use, this study may provide important insight and baseline information regarding utilization. Exploring infant hospice use may also provide hospital and hospice clinicians with specific interventions designed to target those infants with low hospice utilization, improve access to hospice care, and ultimately improve the quality of end-of-life care for infants. Therefore, the purpose of this study was to investigate the factors associated with infant hospice utilization.
Conceptual Framework
This study used a conceptual framework based on the Andersen Behavioral Healthcare Utilization Model to explain the relationship between infant and family factors and hospice use (Lindley, 2015). The Andersen model explains why individuals use health services, defines and measures equitable access to health care, and aids practitioners in developing policies to promote equitable access to care (Andersen, 1968). The Andersen model posits that health care utilization is a function of the predisposing factors of an individual and family to use services, enabling factors that promote or impede use, and an individual’s need for services. These factors are considered the most immediate and important reasons for health care utilization (Andersen, 1968).
Infants and their families are predisposed to using health care services based on demographics. Evidence suggests that demographic factors influencing hospice use include gender (Knapp et al., 2009; Mack et al., 2013) and age (Givens, Tjia, Zhou Emanuel, & Ash 2010; Knapp et al., 2009; Mack et al., 2013). Included in the model were also race and ethnicity because these factors may account for cultural beliefs and attitudes that influence infant hospice use (Given et al., 2010; Hardy et al., 2011; Kari-Kari-Martin, McCann, Hebert, Haffer, & Phillips, 2012).
In addition, enabling resources must be present for infants and families to use specialized health services. For example, an important resource that enables families to access other health care services, including hospice care, is a usual source of care (America Academy of Pediatrics, 2002, 2008; Perrin et al., 1996). A pediatrician or pediatric nurse practitioner is the usual health care provider for infants and their family. These providers act as a health care navigator or referral agent to hospice care. Infants and families must also have access to health care within their community. In other words, health care services must be available and accessible to infants and their families where they live and families must have the means and know-how to obtain these services (Carlson, Bradley, Du, & Morrison, 2010; Jenkins, Chapman, Harshbarger, & Townsend, 2009; Madigan, Wiencek, & Vander Schrier, 2009; Virnig, Ma, Hartman, Moscovice, & Carlin, 2006). Therefore, hospice accessibility and hospital accessibility were included in the model.
In order for health care to be utilized, there must be a need identified. This need for health care services may be based on professional judgment about the infant’s current or deteriorating health status. The clinically evaluated need for hospice care is often driven by the infant’s health condition, so diagnoses were included in the model (Knapp et al., 2009; Mack et al., 2013; Thienprayoon, Lee, Leonard, & Winick, 2013). Families report that when physicians provide information regarding infant health and prognosis with supportive advice, they are able to make decisions about their infant’s health care at end of life (Sullivan, Monagle, & Gillam, 2014). Thus, the evaluated need based on the infant’s diagnosis may be a critical factor affecting hospice use. Families also have a perceived need for health care based on the deteriorating health and functional status of the infant. Infants at end of life typically have multiple health conditions or comorbidities and this disease progression severely limits the infant’s health status, including disability, psychological, and functional status (Lindley & Lyon, 2013). As an end-of-life care option, hospice specializes in managing pain and other symptoms in complex medical cases, such as those with multiple comorbidities and deteriorating health status at end of life (Mack et al., 2013). Families may perceive a need to use hospice care based on the comorbidities and health status of their infant. Thus, the research question posed by this study was whether predisposing, enabling, and need factors affect hospice use among infants and their families.
METHODS
Design and Sample
A longitudinal, correlational design with Center of Medicare and Medicaid Services (CMS) Medicaid data was used to examine the factors related to hospice use among infants. The sample consisted of infants less than 1 year of age. Inclusion criteria included death between January 1, 2007, and December 31, 2010, enrollment in the California Medicaid program for any part of their last calendar year of life, and diagnosis of a complex chronic condition (i.e., neuromuscular, cardiovascular, respiratory, renal, gastrointestinal, hematologic, metabolic, congenital, cancer) based on the International Classification of Diseases, 9th revision (ICD-9) codes as recommended by Feudtner and colleagues (2001). Exclusion criteria included missing entries, non- California resident status, and participation in Medicaid managed care plans. After applying the inclusion and exclusion criteria, the final sample was 207 infants over a period of 4 years. This study was approved by the Institutional Review Board of the University of Tennessee.
Data Sources
The main data source was the 2007 to 2010 California Medicaid claims files (Medicaid Analytic Extract [MAX]). The Medicaid Person Summary files provided demographic and health status information. The MAX Other Services files provided procedure codes for health care services and ICD-9 diagnosis codes. Medicaid claims data was used because it is one of the few publicly available data sources that include infant hospice utilization and California was selected because it has the largest population of children enrolled in Medicaid of any state (Kaiser Family Foundation, 2010). The study also used the California Office of Statewide Health Planning and Development State Utilization (CA OSHPD) Data File of Home Health Agency and Hospice Facilities from fiscal year 2007 to 2010. It contains the addresses of pediatric hospice providers. Information was provided by the Children’s Hospital Association (CHA) on the location of children’s hospitals in California. To create a comprehensive data set for this study, all data were manually merged by Federal Information Processing Standards (FIPS) code.
Measures
Two dependent variables of infant hospice use were created from the MAX Other Services procedure codes: hospice enrollment and hospice length of stay. Hospice enrollment was measured as whether or not an infant used any hospice care during their last calendar year of life. The hospice length of stay variable was operationalized as a count of days of hospice care in the last calendar year of life.
A group of independent variables was composed of factors drawn from the constructs of the Andersen Behavioral Model of Health Services Use. Predisposing factors included gender, race, and ethnicity. Gender was defined as male or female. A binary measure of Caucasian or not Caucasian was created for race. Ethnicity was dichotomized as whether or not the infant was Hispanic. Enabling factors included usual source of care, hospice accessibility, and children’s hospital accessibility. Usual source of care was operationalized as whether or not an infant was an established patient with a primary care provider. Hospice accessibility was defined as residing within 10 miles of a pediatric hospice provider and was created with mapping software (ArcGIS Online). A measure of hospital accessibility was defined as whether or not a children’s hospital was present in the infant’s county of residence. Need factors included diagnoses, comorbidities, and health status. Separate variables were created for the diagnosis categories congenital anomalies (e.g., chromosomal anomalies, genetic defects), cardiovascular (e.g., heart and valve malformations, cardiomyopathies), neurological (e.g., moderate and severe intellectual disabilities, cerebral palsy, epilepsy), gastrointestinal (e.g., chronic liver disease, cirrhosis, inflammatory bowel disease and respiratory (e.g., respiratory malformations, chronic respiratory disease, cystic fibrosis). The measure of comorbidities was dichotomized as whether or not an infant had 2 or more complex chronic conditions. Disability health status was defined as whether the infant was eligible for Medicaid coverage because of their disability status. Psychological health status was measured as whether an infant received any psychiatric care. The measure of functional health status was whether or not an infant received durable medical equipment, transportation services, personal care, or occupational therapy/physical therapy.
Data Analysis
Standard descriptive statistics for all study variables were calculated, including means, percentages, minimums, and maximums, using pooled cross-sectional data from the years 2007 to 2010. Separate multivariate analyses were conducted for hospice enrollment and hospice length of stay. A logistic regression with mixed effects was used to estimate the association between factors and hospice enrollment because the measure of hospice enrollment was binary (Long & Freese, 2006). The logistic regression analysis results are presented as adjusted odds ratios (OR). A negative binomial model with mixed effects was constructed for the analysis of hospice length of stay that was well suited for estimation rates based on count data such as the number of hospice days (Long & Freese, 2006). A goodness of fit indicator determined that the data fit a negative binomial distribution rather than a Poisson distribution, and the results were reported as adjusted incidence rate ratios (IRR). All analyses were performed using Stata 11.0 (StataCorp LP, College Station, TX) and ArcGIS Online (ESRI Inc., Redlands, California).
RESULTS
Descriptive Analysis
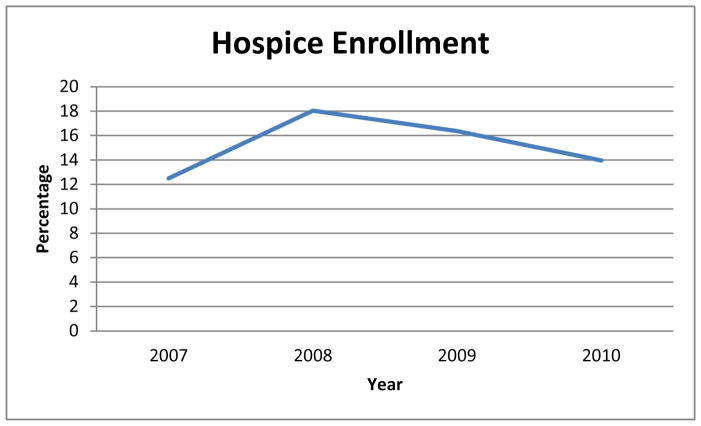
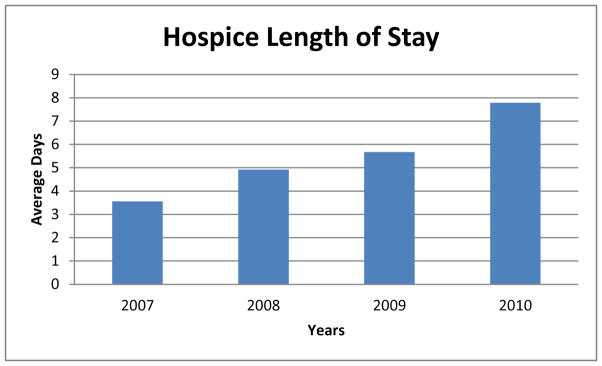
The characteristics of the infant sample are presented in Table 1. Slightly more than 15% of the infants were enrolled in hospice care, with an average length of stay of 5 days. In the study time period, the frequency of hospice enrollment increased from 2007 (12.50%) to 2008 (18.03%), but declined in 2009 (16.36%) and 2010 (13.95%) (Figure 1). However, hospice length of stay increased steadily from an average of 3.56 days in 2007 to average of 7.79 days in 2010 (Figure 2).
Table 1.
Descriptive Statistics of Study Variables (N=207)
| Variables | N | Mean/Percentage | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| Hospice Enrollment (%) | 32 | 15.46 | --- | 0 | 1 |
| Hospice Length of Stay | 207 | 5.40 | 23.49 | 0 | 191 |
| Female (%) | 94 | 45.41 | --- | 0 | 1 |
| Race | |||||
| Caucasian (%) | 19 | 10.00 | --- | 0 | 1 |
| Non- Caucasian (%) | 188 | 90.00 | --- | 0 | 1 |
| Hispanic (%) | 78 | 37.68 | --- | 0 | 1 |
| Usual Source of Care (%) | 78 | 37.68 | --- | 0 | 1 |
| Hospice Accessibility (%) | 168 | 81.16 | --- | 0 | 1 |
| Hospital Accessibility (%) | 115 | 55.56 | --- | 0 | 1 |
| Diagnosis | |||||
| Congenital (%) | 68 | 32.85 | --- | 0 | 1 |
| Cardiovascular (%) | 149 | 71.98 | --- | 0 | 1 |
| Neuromuscular (%) | 64 | 30.92 | --- | 0 | 1 |
| Gastrointestinal (%) | 21 | 10.14 | --- | 0 | 1 |
| Respiratory (%) | 46 | 22.22 | --- | 0 | 1 |
| Comorbidities (%) | 113 | 54.59 | --- | 0 | 1 |
| Health Status | |||||
| Disability Status (%) | 174 | 84.06 | --- | 0 | 1 |
| Psychological Status (%) | 34 | 16.43 | --- | 0 | 1 |
| Functional Status (%) | 109 | 52.66 | --- | 0 | 1 |
| Years | |||||
| 2007 (%) | 48 | 23.19 | --- | 0 | 1 |
| 2008 (%) | 61 | 29.47 | --- | 0 | 1 |
| 2009 (%) | 55 | 26.57 | --- | 0 | 1 |
| 2010 (%) | 43 | 20.77 | --- | 0 | 1 |
Figure 1.
Infant Hospice Enrollment Frequency, 2007 to 2010
Figure 2.
Average Infant Hospice Length of Stay, 2007 to 2010
Infants were evenly divided between male (54.59%) and female (45.41%) and most were non-Caucasian (90.00%). Approximately a third of the infants were Hispanic (37.68%) and had a primary care provider as a usual source of care (37.68%). Over half of the sample had access to hospice (81.16%) and children’s hospitals (55.56%) in their county. The most common diagnosis was cardiovascular conditions (71.98%), while the least common was gastrointestinal problems (10.14%). More than half of the infants had multiple complex chronic conditions (54.49%). A majority of the sample was categorized as disabled (84.06%) with limited functional status (52.66%), while 16.43% had diminished psychological status.
Multivariate Analysis
The results of the multivariate analyses are presented in Table 2. Compared to boys, girls had increased odds of being enrolled in hospice care (OR=2.61, P<0.05) with significantly longer stays (IRR=2.21, P<0.05). Congenital anomalies were positively associated with hospice enrollment (OR=4.95, P<0.01) and length of stay (OR=4.15, P<0.01), while cardiovascular (OR=0.12, P<0.01; OR=0.23, P<0.01) and respiratory conditions (OR=0.23, P<0.05; OR=0.26, P<0.05) were significantly and negatively related to hospice enrollment and hospice length of stay, respectively. No other factors were associated with hospice enrollment or length of stay.
Table 2.
Multivariate Analysis Results for Infant Hospice Use (N=207)
| Variables | Hospice Enrollment | Hospice Length of Stay | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | IRR | 95 % CI | |||
| Female | 2.61 | 1.0362–6.5813 | * | 2.21 | 1.0460–4.6514 | * |
|
| ||||||
| Caucasian | 0.15 | 0.0188–1.1579 | 0.25 | 0.0553–1.1197 | ||
|
| ||||||
| Hispanic | 0.44 | 0.1549–1.2431 | 0.63 | 0.2796–1.4179 | ||
|
| ||||||
| Usual Source of Care | 0.51 | 0.1536–1.6684 | 0.51 | 0.1843–1.4332 | ||
|
| ||||||
| Hospice Accessibility | 3.01 | 0.7755–11.6746 | 2.89 | 0.9343–8.9274 | ||
|
| ||||||
| Hospital Accessibility | 0.83 | 0.3117–2.2302 | 0.66 | 0.3004–1.4563 | ||
|
| ||||||
| Congenital | 4.95 | 1.4870–16.4839 | ** | 4.15 | 1.4140–12.1919 | ** |
|
| ||||||
| Cardiovascular | 0.12 | 0.0280–0.4772 | ** | 0.23 | 0.8281–0.6122 | ** |
|
| ||||||
| Neuromuscular | 2.15 | 0.6612–6.9657 | 2.50 | 0.9109–6.8791 | ||
|
| ||||||
| Gastrointestinal | 0.21 | 0.0320–1.3216 | 0.27 | 0.0568–1.2998 | ||
|
| ||||||
| Respiratory | 0.23 | 0.5145–0.9921 | * | 0.26 | 0.0699–0.9685 | * |
|
| ||||||
| Comorbidities | 2.66 | 0.5688–12.4208 | 1.81 | 0.5264–6.2247 | ||
|
| ||||||
| Disability Status | 0.54 | 0.1553–1.8986 | 0.59 | 0.2259–1.5455 | ||
|
| ||||||
| Psychological Status | 0.83 | 0.1972–3.4965 | 0.98 | 0.2944–3.2301 | ||
|
| ||||||
| Functional Status | 0.65 | 0.2307–1.8353 | 0.50 | 0.2151–1.1588 | ||
|
| ||||||
| 2008 | 1.07 | 0.2938–3.8953 | 0.97 | 0.3296–2.8337 | ||
|
| ||||||
| 2009 | 0.93 | 0.2340–3.6708 | 0.87 | 0.2623–2.9076 | ||
|
| ||||||
| 2010 | 0.90 | 0.2224–3.6762 | 1.00 | 0.2993–3.3702 | ||
p< 0.05,
p <0.01,
p< 0.001
Note: OR, odds ratio; IRR, incidence rate ratios; CI, Confidence Intervals.
DISCUSSION
This study examined the factors associated with infant hospice use. The analyses found that just over 15% of infants enrolled in hospice care on average for 5 days. From the perspective of the Andersen Model, predisposing and need factors of the infant and their families were related to hospice enrollment and length of stay, while no enabling factors influenced hospice use. Girl infants and those with congenital anomalies had greater odds of enrolling in hospice care for longer stays, whereas those infants with cardiovascular and respiratory conditions were significantly less likely to be enrolled in hospice and overall had a decreased length of stay.
These findings were similar to Leuthner and colleagues (2004), who found that infants with congenital anomalies used hospice care. However, the results differed in relation to cardiovascular conditions. Whereas Leuthner’s study found that cardiovascular conditions were common among those in hospice and home health, results of this study revealed that patients with cardiovascular conditions were less likely to use hospice care. This difference may be a result of the measurement of hospice care. For this study, hospice use was measured as hospice enrollment and hospice length of stay. In the Leuthner study, it was measured as hospice and home health use. In addition, the Leuthner study was a descriptive analysis of data utilizing infant’s death certificates. Conversely, this study used advanced statistical analysis to estimate associations with hospice use. Therefore, the specificity of measurement and the analysis plan may have contributed to the difference in findings.
This study found an unexpected gender differences in hospice enrollment and length of stay. Compared to boys, infant girls were more predisposed to using hospice care. It is possible that infant girls are able to express emotions more than boys. In studies of gender differences among infants, girls tend to establish and maintain eye contact and are attracted to individual faces (Chaplin & Aldao, 2013). In addition, gender difference in non-verbal language often appear in infants’ through gestures, with boys lagging behind girls in initial gesturing by as much as 3 months (Ozcaliskan & Goldin-Meadow, 2010). This can be complicated by the fact that mothers typically have a communication preference for girls and respond more often to them than to boys (Johnson, Caskey, Rand, Tucker, & Vohr, 2014). Thus, infant girls may be able to communicate earlier and more effectively with their families than boys about end-of-life pain and other symptoms that encourage enrollment and longer stays in hospice care. Further research is needed to understand the gender difference in hospice utilization.
The finding that infants with congenital anomalies were more likely to enroll in hospice with extended stays was interesting. A reason for this finding might relate to new, innovative care models such as perinatal hospice and palliative care. Perinatal hospice and palliative care is support for parents who find out during pregnancy that their baby has a life-limiting condition and who choose to continue their pregnancies (Hoeldtke & Calhoun, 2001). Perinatal hospice and palliative care supports families from the time of diagnosis through the infant’s birth and death by relieving pain and uncomfortable symptoms in infants and providing emotional and spiritual support to family members (Wool, 2013). As prenatal testing continues to advance, congenital conditions are more often diagnosed during pregnancy providing needed time to make decisions regarding postnatal care including hospice (Calhoun, Napolitano, Terry, Bussey, & Hoeldtke, 2003). This is different than neurologic, cardiac and/or respiratory conditions, which are generally diagnosed after birth. Thus, the needs of infants with congenital anomalies and their families may be met with hospice care because of their early exposure to the perinatal model.
There are several limitations of this study. The study was conducted with Medicaid data from California, which limits the generalizability of the findings to other states. However, California often has health care practices, patterns, and policies that are influential nationally. It has been a leader in hospice care by implementing new and emerging pediatric end-of-life care services before they are adopted in other states (Dabbs, Butterworth, & Hall, 2007). As such, exploring infant hospice use in California may provide important insight into infant hospice use for other states and the nation. Another limitation was that the data set included the last calendar year of life for the infant and did not include a comprehensive claims history. The hospice length of stay may have been truncated for some infants because the study data was date limited. Thus, infant hospice length of stay may be under-reported. However, in this study the average length of stay was only a matter of days, which makes it less likely that the stay reported would be significantly truncated.
Future research to understand the factors associated with infant hospice use nationally and the meaning of these predictors for families and clinicians is needed. Research that explores the differences in hospice use among the various infant health conditions, particularly fatal congenital anomalies versus cardiovascular and respiratory conditions, is also needed.
This study provides important insights for nurses and other clinicians caring for infants and their families at end of life. Findings also suggest actionable practices by nurses to engage and support families in their decision-making process about discharging home with the support of hospice care. Nurses can assist in identifying infant hospice providers that may help families understand their options because infant hospices vary in the services offered (Lindley, 2013). Clinicians may not be aware of local pediatric hospices within the community. Many children’s hospitals are referral centers therefore this lack of knowledge regarding distance resources can be intensified when infants and their families are from out of state (Thompson, Knapp, Madden, & Shenkman, 2009). Establishing a resource list of infant hospice providers may assist families in the discharge planning process. Sources of provider information include state Departments of Health, which licenses hospice providers, pediatric end-of-life advocacy groups including the National Hospice and Palliative Care Organization Children’s Project on Palliative/Hospice Services, and online hospice communities such as Hospice Analytics (http://www.nationalhospiceanalytics.com). Nurses have a critical role in improving the quality of end-of-life care for infants by educating families about resources.
In summary, understanding the unique factors related to infant hospice use is essential for advancing knowledge and compassion in this area of end-of-life care. This study showed that gender differences and a diagnosis of congenital anomalies is critical in hospice enrollment and length of stay, while infants with cardiac and respiratory problems were less likely to use hospice. With this knowledge, nurses and other clinicians can target education for those families regarding available resources for infant hospice care, thus influencing infant and family quality of end-of-life care.
Acknowledgments
Funding Source: This publication was made possible by Grant Number K01NR014490 from the National Institute of Nursing Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no potential conflicts of interest to disclose.
Institution Where Work Performed: University of Tennessee
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lisa C. Lindley, Assistant Professor, University of Tennessee, College of Nursing.
Katherine M. Newnam, Assistant Professor, University of Tennessee, College of Nursing.
References
- American Academy of Pediatrics. The medical home. Pediatrics. 2002;110:184–186. [Google Scholar]
- American Academy of Pediatrics. The medical home - statement reaffirmation. Pediatrics. 2008;122:450. [Google Scholar]
- American Academy of Pediatrics. Police statement on Pediatric Palliative Care and Hospice Care Commitments, Guidelines, and Recommendations. Pediatrics. 2013;132(5):966–972. doi: 10.1542/peds.2013-2731. [DOI] [PubMed] [Google Scholar]
- Andersen RA. Behavioral Model of Families’ Use of Health Services. Chicago: Center for Health Administration Studies; 1068. [Google Scholar]
- Brosig CL, Pierucci RL, Kupst MJ, Leuthner SR. Infant end-of-life care: The parents’ perspective. Journal of Perinatology. 2007;27(8):510–516. doi: 10.1038/sj.jp.7211755. [DOI] [PubMed] [Google Scholar]
- Calhoun BC, Napolitano P, Terry M, Bussey C, Hoeldtke NJ. Perinatal hospice: Comprehensive care for the family of the fetus with a lethal condition. Journal of Reproductive Medicine. 2003;48(5):343–348. [PubMed] [Google Scholar]
- Carlson M, Bradley E, Du Q, Morrison S. Geographic access to hospice in the United States. Journal of Palliative Medicine. 2010;13:1331–1338. doi: 10.1089/jpm.2010.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplin TM, Aldao A. Gender differences in emotion expression in children: A meta-analytic review. Psychological Bulletin. 2013;139(4):735–765. doi: 10.1037/a0030737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavoski N, Miller T, Siden H. Resource utilization among individuals dying of pediatric life-threatening disease. Journal of Palliative Medicine. 2013;16(10):1–5. doi: 10.1089/jpm.2013.0110. [DOI] [PubMed] [Google Scholar]
- Dabbs D, Butterworth L, Hall E. Tender mercies: Increasing access to hospice end-of-life care in rural areas of the United States. Policy, Politics, and Nursing Practice. 2007;10:71–81. [Google Scholar]
- Feudtner C, Hays R, Haynes G, Geyer J, Neff J, Koepsell T. Deaths attributed to pediatric complex chronic conditions: National trends and implications for supportive care services. Pediatrics. 2001;107:e99–e103. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- Givens JL, Tjia J, Zhou C, Emanuel E, Ash AS. Racial and ethnic differences in hospice use among patients with heart failure. Archives of Internal Medicine. 2010;170:427–432. doi: 10.1001/archinternmed.2009.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy D, Chan W, Liu C, Cormier JN, Xia R, Bruera E, Du XL. Racial disparities in the use of hospice services according to geographic residence and socioeconomic status in an elderly cohort with non-small cell lung cancer. Cancer. 2011;117(7):1506–1515. doi: 10.1002/cncr.25669. [DOI] [PubMed] [Google Scholar]
- Hoeldtke NJ, Calhoun BC. Perinatal hospice. American Journal of Obstetrics and Gynecology. 2001;185(3):525–529. doi: 10.1067/mob.2001.116093. [DOI] [PubMed] [Google Scholar]
- Jenkins T, Chapman K, Harshbarger D, Townsend J. Hospice use among cancer decedents in Alabama, 2002–2005. Preventing Chronic Disease. 2009;6:1–8. [PMC free article] [PubMed] [Google Scholar]
- Johnson K, Caskey M, Rand K, Tucker R, Vohr B. Gender differences in adult-infant communication in the first months of life. Pediatrics. 2014;134(6):e1603–e1610. doi: 10.1542/peds.2013-4289. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Distribution of Medicaid Enrollees by Enrollment Group, FY. 2009 http://www.statehealthfacts.org/comparemaptable.jsp?ind=200&cat=4. Published 2010.
- Knapp C, Shenkman E, Marcu M, Madden V, Terza J. Pediatric palliative care: Describing hospice users and identifying factors that affect hospice expenditures. Journal of Palliative Medicine. 2009;12:1–7. doi: 10.1089/jpm.2009.9657. [DOI] [PubMed] [Google Scholar]
- Leuthner S, Boldt A, Kirby R. Where infants die: Examination of place of death and hospice/home health care options in the state of Wisconsin. Journal of Palliative Medicine. 2004;7(2):269–277. doi: 10.1089/109662104773709396. [DOI] [PubMed] [Google Scholar]
- Lindley LC, Edwards SL. Geographic access to hospice care for children with cancer in Tennessee, 2009 to 2011. American Journal of Hospice and Palliative Medicine. 2015;32(8):849–854. doi: 10.1177/1049909114543641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC. Health care reform and concurrent curative care for terminally ill children: A policy analysis. Journal of Hospice and Palliative Nursing. 2011;13(2):81–88. doi: 10.1097/NJH.0b013e318202e308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC. Trends in services among pediatric hospice providers during 2002 to 2008. American Journal of Hospice and Palliative Medicine. 2013;30(1):68–74. doi: 10.1177/1049909112444001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC. Determinants of access to pediatric hospice care: A conceptual model. Journal of Hospice and Palliative Nursing. 2015;17(2):113–118. doi: 10.1097/NJH.0000000000000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC, Lyon ME. A profile of children with complex chronic conditions at end of life among Medicaid-beneficiaries: Implications for healthcare reform. Journal of Palliative Medicine. 2013;16(11):1388–1393. doi: 10.1089/jpm.2013.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC, Nageswaran S. Pediatric primary care involvement in end-of-life care for children. American Journal of Hospice and Palliative Medicine. 2015 doi: 10.1177/1049909115609589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC, Shaw SL. Who are the children enrolled in hospice care? Journal for Specialists in Pediatric Nursing. 2014;19(4):308–315. doi: 10.1111/jspn.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long JS, Freese J. Regression Models for Categorical Dependent Variables Using Stata. College Station, TX: Stata Press Publications; 2006. [Google Scholar]
- Lyon M, Williams P, Woods E, Hutton N, Butler A, Siblinga E, Oleske JM. Do-not-resuscitate orders and/or hospice care, psychological health, and quality of life among children/adolescents with acquired immune deficiency syndrome. Journal of Palliative Medicine. 2008;11:459–469. doi: 10.1089/jpm.2007.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDorman MF, Gregory ECW. National vital statistics reports. 8. Vol. 64. Hyattsville, MD: National Center for Health Statistics; 2015. Fetal and Perinatal Mortality, United States, 2013; p. 24. [PubMed] [Google Scholar]
- Mack JW, Chen K, Boscoe FP, Gesten FC, Roohan PJ, Weeks JC, … Schrag D. Underuse of hospice care by Medicaid-insured patients with stage IV lung cancer in New York and California. Journal of Clinical Oncology. 2013;31:2569–2579. doi: 10.1200/JCO.2012.45.9271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan EA, Wiencek CA, Vander Schrier AL. Patterns of community-based services for children with life-threatening conditions. The American Journal of Maternal/Child Nursing. 2009;32:311–319. [Google Scholar]
- Martin P, McCann JJ, Hebert LE, Haffer SC, Phillips M. Do community and caregiver factors influence hospice use at the end of life among older adults with Alzheimer disease. Journal of Hospice and Palliative Nursing. 2012;14(3):225–237. doi: 10.1097/NJH.0b013e3182433a15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moura H, Costa V, Rodrigues M, Almeida F, Maia T, Guimaraes H. End of life in the neonatal intensive care unit. Clinics. 2011;66:1569–1572. doi: 10.1590/S1807-59322011000900011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Hospice and Palliative Care Organization. Standards of practice for pediatric palliative care and hospice. 2009;2009 Retrieved from http://www.nhpco.org/sites/default/files/public/quality/Ped_Pall_Care%20_Standard.pdf.pdf. [Google Scholar]
- National Hospice and Palliative Care Organization. NHPCO Facts and Figures: Pediatric Palliative & Hospice Care in America. National Hospice & Palliative Care Organization website. 2015 http://www.nhpco.org/sites/default/files/public/quality/Pediatric_Facts-Figures.pdf.
- Osterman MJ, Kochanek KD, MacDorman MF, Strobino DM, Guyer B. Annual summary of vital statistics: 2012–2013. Pediatrics. 2015;135:1115–1125. doi: 10.1542/peds.2015-0434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozcaliskan S, Goldin-Meadow S. Sex differences in language first appear in gestures. Developmental Science. 2010;13(5):752–760. doi: 10.1111/j.1467-7687.2009.00933.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrin JM, Greenspan P, Bloom SR, Finkelstein D, Yazdgerdi S, Leventhal JM, Rodewald L, Szilagyi P, Homer CJ. Primary care involvement among hospitalized children. Archives of Pediatric and Adolescent Medicine. 1996;150:479–86. doi: 10.1001/archpedi.1996.02170300033007. [DOI] [PubMed] [Google Scholar]
- Sullivan J, Monagle P, Gillam L. What parents want from doctors in end-of-life decision-making for children. Archives of Disabled Children. 2014;99:216–20. doi: 10.1136/archdischild-2013-304249. [DOI] [PubMed] [Google Scholar]
- Thienprayoon R, Lee SC, Leonard D, Winick N. Racial and ethnic difference in hospice enrollment among children with cancer. Pediatric Blood Cancer. 2013;60:1662–1666. doi: 10.1002/pbc.24590. [DOI] [PubMed] [Google Scholar]
- Thompson LA, Knapp C, Madden V, Shenkman E. Pediatricians’ perceptions of and preferred timing for pediatric palliative care. Pediatrics. 2009;123(5):e777–e782. doi: 10.1542/peds.2008-2721. [DOI] [PubMed] [Google Scholar]
- Virnig B, Ma H, Hartman L, Moscovice I, Carlin B. Access to home-based hospice care for rural populations: Identification of areas lacking service. Journal of Palliative Medicine. 2006;9:1292–1299. doi: 10.1089/jpm.2006.9.1292. [DOI] [PubMed] [Google Scholar]
- Wool C. State of the science on perinatal palliative care. Journal of Obstetric Gynecological and Neonatal Nursing. 2013;42(3):372–382. doi: 10.1111/1552-6909.12034. [DOI] [PubMed] [Google Scholar]