Abstract
Preterm delivery (PTD), or birth before 37 completed weeks of gestation, is a serious public health issue, and racial disparities persist. In a recently published study, perceptions of the residential environment (or neighborhood context) were associated with PTD rates among urban African American women with low educational attainment (≤12 years); however, the mechanisms of these associations are unknown. Given this gap in the literature, we used data from the Life Influences on Fetal Environments Study of postpartum African American women from Metropolitan Detroit, Michigan (2009–2011; n = 399), to examine whether psychosocial factors (depressive symptomology, psychological distress, and perceived stress) mediate associations between perceptions of the neighborhood context and PTD. Validated scales were used to measure women’s perceptions of their neighborhood safety, walkability, healthy food availability (higher=better), and social disorder (higher=more disorder). The psychosocial indicators were measured with the Center for Epidemiologic Studies-Depression Scale, Kessler’s Psychological Distress Scale (K6), and Cohen’s Perceived Stress Scale. Statistical mediation was assessed using an unadjusted logistic regression-based path analysis for estimating direct and indirect effects. The associations between perceived walkability, food availability, and social disorder were not mediated by psychosocial factors. However, perceptions of neighborhood safety were inversely associated with depressive symptoms which were positively associated with PTD rates. Also, higher perceived neighborhood social disorder was associated with higher PTD rates, net of the indirect paths through psychosocial factors. Future research should identify other mechanisms of the perceived neighborhood context-PTD associations, which would inform PTD prevention efforts among high-risk groups.
Keywords: Depressive symptomology, Neighborhood context, Psychosocial factors, Preterm delivery, African Americans, Urban health
Introduction
Preterm delivery (PTD), or birth before 37 completed weeks of gestation, is a serious public health issue. This adverse birth outcome is a multifactorial syndrome whose etiology is complicated and not completely elucidated.1 Seemingly intractable racial disparities in PTD rates exist, such that African American (AA) women are disproportionately affected.2 , 3 National data from 2013 indicate that 10.3 % of all births to White women were preterm, in contrast to 16.5 % of those to AA women.4 Importantly, traditional risk factors do not explain racial disparities in PTD rates.
Contextual factors, such as the residential environment, may shed some light on the elevated risk of PTD among AA women, especially since this group, compared to Whites, is more likely to reside in adverse neighborhoods.5 , 6 Two studies with data on AA women have examined the impact of perceptions of the residential environment on PTD rates, and found associations that were non-significant (though in the expected direction).7 , 8 First, in a cohort of 1898 pregnant AA and White women, Dole and colleagues reported a 40 % increase in PTD rates for White women who perceived their neighborhoods as unsafe, compared to those who perceived their neighborhood as safe.7 However, when their analyses were restricted to AA women, there was no increase in PTD rates comparing women who reported unsafe versus safe neighborhoods. Second, in a smaller but racially homogeneous study of 72 AA women, Giurgescu et al. also reported no statistically significant association between perceptions of neighborhood social disorder or crime and PTD rates.8 While these two studies suggest that perceptions of residential environment may have no influence on PTD among AA women, neither study examined effect modification by sociodemographic characteristics, such as educational attainment.
In a recently published report by Sealy-Jefferson et al., the association between subjective reports of neighborhood context (safety, walkability, food availability, and social disorder) and PTD rates was shown to vary by educational attainment, in a cohort of 1411 AA women.9 Specifically, among women with low educational attainment (≤12 years), those who reported positive perceptions of their neighborhood context had lower PTD rates than those who had negative perceptions of their neighborhoods. No significant associations were observed for women with more than 12 years of education. The authors speculated that women with lower educational attainment may be more vulnerable to the impact of their residential environment than women with higher levels of education, and suggested that psychosocial factors might mediate these associations.9
Perceptions signify objective reality10 and operate through individual cognitive processes in individuals.11 As a result, it is possible that psychosocial factors such as depressive symptoms, psychological distress, and perceived stress during pregnancy are underlying mechanisms linking subjective reports of the quality of the residential environment and PTD. There is evidence that the neighborhood context impacts psychosocial indicators,12 – 14 but the extant literature on links between these psychosocial factors and PTD is mixed.15 , 16 In light of this gap in the literature, we sought to examine whether psychosocial indicators (i.e., depressive symptomology, perceived stress, and psychological distress) mediate associations between perceived neighborhood context and PTD among AA women with low educational attainment (≤12 years). We tested the following hypotheses: (1) perceptions of the residential environment are associated with psychosocial indicators; (2) psychosocial indicators are associated with PTD rates; and (3) the associations between perceptions of neighborhood context and PTD operate through psychosocial indicators.
Methods
Study Design
Details of the Life Influences on Fetal Environments (LIFE) study have been previously published.9 In brief, LIFE is a retrospective cohort study conducted from 2009 to 2011, and women (≥18years old) who self-identified as African American and gave birth to a singleton infant at a suburban hospital in Oakland County, Michigan, were eligible to participate. The primary objective of LIFE was to determine whether and how racism is associated with PTD, among AAs. Women were excluded from the study if they (1) did not speak English or (2) had intellectual disabilities, serious cognitive deficits, or significant mental illness on the basis of history or any prior records. In-person interviews were conducted during the postpartum hospital stay, and medical history was abstracted from medical records. The original study included 1411 women which represented 71 % of the women approached for study participation. For the present analyses, we restricted the analytic sample to the women in the cohort with ≤12 years of education (n = 399), to test our mediation hypotheses. This study was approved by the institutional review boards at the University of Michigan, St. John Providence Health System, and Wayne State University. All study participants gave written informed consent.
Outcome Ascertainment
PTD was defined as delivery prior to 37 completed weeks of gestation. Gestational age was estimated from the medical record in a hierarchical fashion with priority given to the provider’s estimate of gestational age based on early ultrasound (between 6 and 20 weeks of gestation).17 In the analytic sample (n = 399), 16 % of all births were preterm (n = 64).
Exposure Ascertainment
Women reported detailed characteristics of their current residential environment (defined as “the area around where you live and around your house”) using four valid, reliable multi-item scales: safety,18 – 20 walking environment,18 , 19 , 21 healthy food availability,18 , 19 and social disorder (see Table 1 for specific scale details).19 Reverse coding was performed as necessary for residential environment questions, such that higher scale values indicate better environment for all scales, except for social disorder (higher values = more social disorder). Internal consistency reliability of the neighborhood scales was assessed with standardized Cronbach’s alpha statistics and was high for each scale (Table 1).9
TABLE 1.
Questions used in the Life Influences on Fetal Environments Study (2009–2011) to assess perceptions of the physical and social residential environment
| Scale | Scale measurement and items | Alpha |
|---|---|---|
| Safety | 5-point Likert: strongly agree, agree, neither agree nor disagree, disagree, strongly disagree | 0.90 |
| 1.Many people in your neighborhood are afraid to go outside at night. | ||
| 2.There are areas of this neighborhood where everyone knows “trouble” is expected. | ||
| 3.You’re taking a big chance if you walk in this neighborhood alone after dark. | ||
| 4.I feel safe walking in my neighborhood. | ||
| 5.Violence is a problem in my neighborhood. | ||
| 6.I feel very safe from crime in my neighborhood. | ||
| Walkability | 5-point Likert: strongly agree, agree, neither agree nor disagree, disagree, strongly disagree | 0.78 |
| 1.It is pleasant to walk in my neighborhood. | ||
| 2.The trees in my neighborhood provide enough shade. | ||
| 3.In my neighborhood, it is easy to walk to places. | ||
| 4.I often see other people walking in my neighborhood. | ||
| 5.I often see other people exercise in my neighborhood. | ||
| 6.There are stores within walking distance of my home. | ||
| Healthy food availability | 5-point Likert: strongly agree, agree, neither agree nor disagree, disagree, strongly disagree | 0.91 |
| 1.A large selection of fresh fruits and vegetables is available in my neighborhood. | ||
| 2.A large selection of low fat products is available in my neighborhood. | ||
| Social disorder | 3-point Likert: a big problem, somewhat of a problem, not a problem | 0.93 |
| 1.How much of a problem is litter, broken glass, or trash on the sidewalks and streets? | ||
| 2.How much of a problem is graffiti on buildings and walls? | ||
| 3.How much of a problem are vacant or deserted houses or storefronts? | ||
| 4.How much of a problem is drinking in public? | ||
| 5.How much of a problem is people selling or using drugs? | ||
| 6.How much of a problem are groups of teenagers or adults hanging out in the neighborhood and causing trouble? | ||
| 7.How much of a problem is noise in the neighborhood? | ||
| 8.How much of a problem is yelling or fighting? |
Mediators
Three variables were tested as possible mediators of the subjective neighborhood context-PTD associations: depressive symptomology, psychological distress, and perceived stress. Depressive symptoms were measured with the 20-item Centers for Epidemiologic Studies-Depression scale (CES-D), which is reliable and valid, and has been used in diverse populations, including pregnant women.22 – 25 Depressive symptoms occurring during the past 7 days were reported by study participants on a four-point Likert scale (rarely, some of the time, occasionally, most of the time).25 Reverse coding of individual CES-D items was performed as necessary. Next, individual items were summed, with possible scores for the aggregate variable ranging from 0 to 60 (higher scores indicate more depressive symptoms). Internal consistency reliability of the 20-item CES-D scale in the original study was 0.86, with range of scores from 0 to 53. Given that the 20-item CES-D scale includes items that are associated with common symptoms of pregnancy, we excluded the following somatic symptoms from the CES-D scale: poor appetite, being distracted, everything being an effort, and restlessness during sleep. We used the 16-item CES-D scale for the present analyses, which had good internal consistency reliability (0.84). Range of possible scores for the reduced CES-D scale was 0 to 48, and the actual range of scores for our analytic sample was 0 to 41.
Psychological distress during the past 30 days was assessed with the Kessler Psychological Distress Scale (K6).26 Study participants reported how often they felt nervous, hopeless, restless or fidgety, so depressed that nothing could cheer them up, that everything was an effort, and worthless, on a five-point Likert scale (all of the time to none of the time). Individual items were reverse coded and summed, and scores in our analytic sample ranged from 6 to 30. Internal consistency reliability of the Psychological Distress Scale was 0.72.
Perceived stress was reported with the Cohen’s Perceived Stress Scale,27 , 28 which contains 14 items reported on a five-point Likert scale (never to very often). The period of reference for perceived stress was the prior month. Reverse coding was performed as necessary, and individual items were summed to create the overall scale. The range of possible scores for the Perceived Stress Scale was 14–70, and higher scores represented higher levels of stress. Internal consistency reliability for this scale was 0.87.
Statistical Analysis
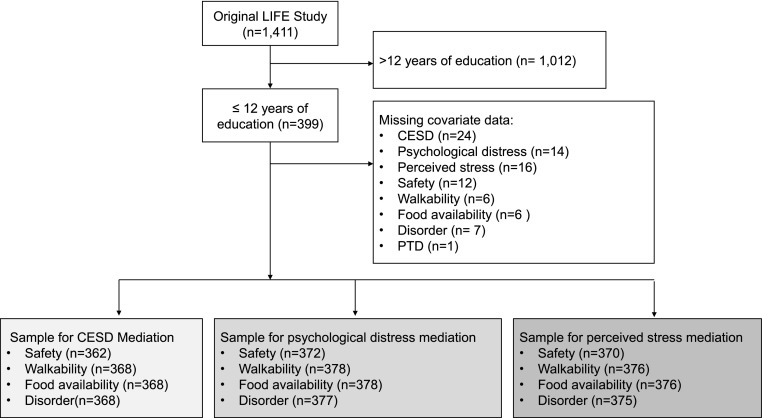
Univariate and bivariate statistics were used to describe the data, with Wilcoxon rank sum and chi-square tests used to assess group differences for continuous and categorical variables, respectively. Pearson r correlation coefficients among neighborhood as well as psychosocial variables were calculated. We tested our mediation hypotheses with a logistic regression-based path analysis (Figs. 2, 3, 4, and 5) for estimating total (c), direct (c′) ,and indirect effects (a*b). Bias-corrected 95 % confidence intervals (CIs) were obtained through bootstrapping of 10,000 resamples. We used the Process Macro for SAS to carry out the mediation analysis.29 , 30 We examined the functional form of the psychosocial indicators and modeled each variable continuously. On the basis of prior work, the variability of marital status and income in the study population was limited,9 such that most of the women were not married and had low income (see Table 1). Since there was no evidence that the associations between perceptions of neighborhood context and PTD were confounded by marital status and income, we present unadjusted models except for perceived social disorder-PTD models, which were adjusted for age (<35 and ≥35 years). All variables were assessed for missing data (all missing <7 %), and complete-case analysis was performed. Figure 1 shows exclusion criteria and final sample sizes for each mediation model. Parameter estimates with two-sided p < 0.05 or 95 % CIs that excluded 0 were considered statistically significant. All analyses were conducted using SAS version 9.4 for Windows (SAS Institute Inc., Cary, NC).
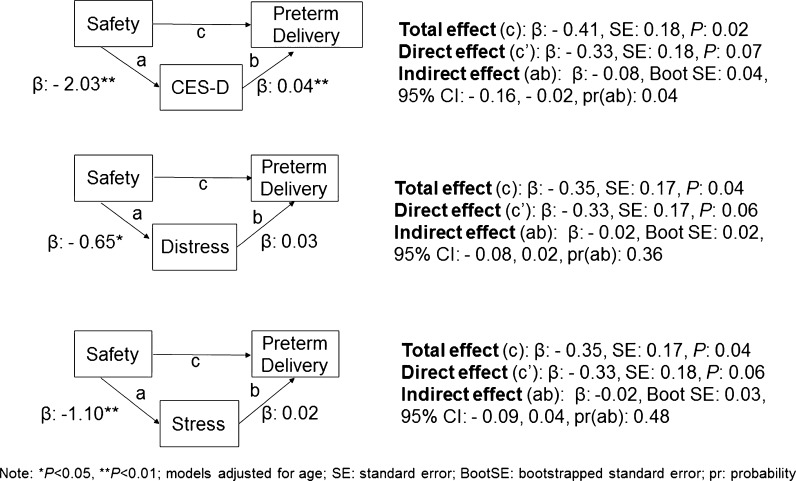
FIG. 2.
Path analyses for the association between perceived neighborhood safety and preterm delivery rates, and potential mediation by depressive symptoms, psychological distress and perceived stress; Life Influences on Fetal Environments Study, 2009–2011.
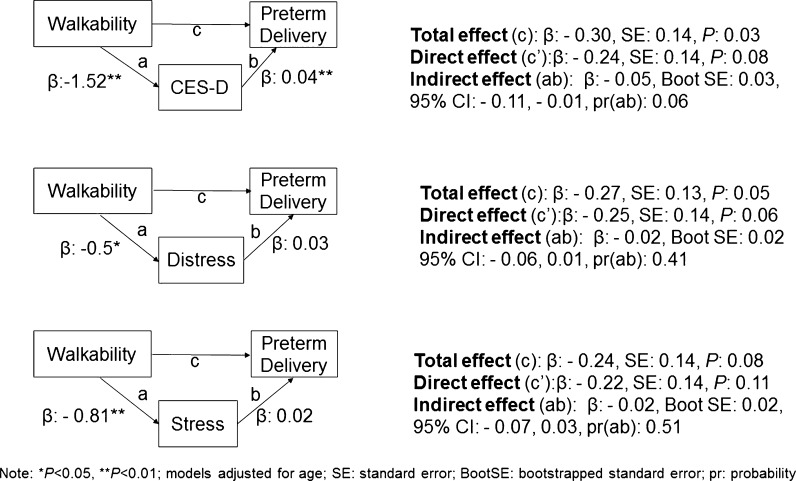
FIG. 3.
Path analyses for the association between perceived neighborhood walkability and preterm delivery rates, and potential mediation by depressive symptoms, psychological distress and perceived stress; Life Influences on Fetal Environments Study, 2009–2011.
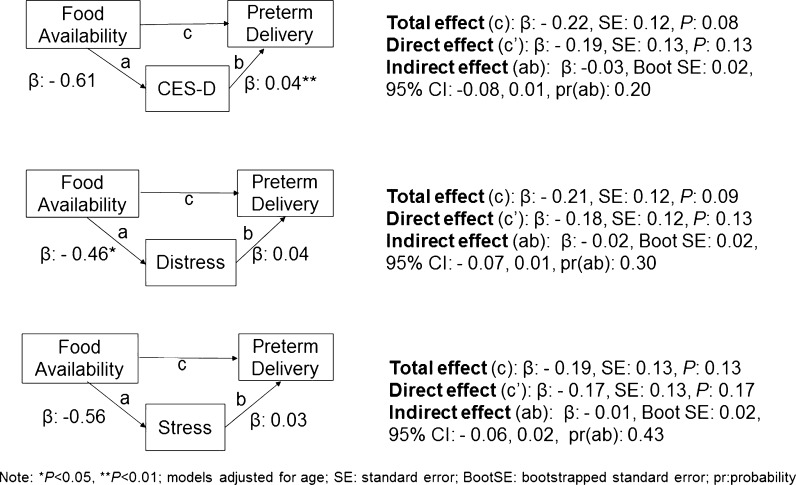
FIG. 4.
Path analyses for the association between perceived neighborhood food availability and preterm delivery rates, and potential mediation by depressive symptoms, psychological distress and perceived stress; Life Influences on Fetal Environments Study, 2009–2011.
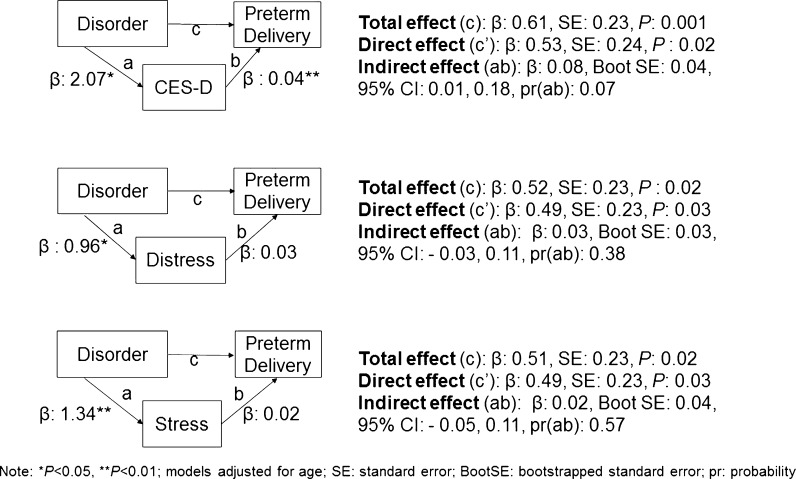
FIG. 5.
Path analyses for the association between perceived neighborhood social disorder and preterm delivery rates, and potential mediation by depressive symptoms, psychological distress and perceived stress; Life Influences on Fetal Environments Study, 2009–2011.
FIG. 1.
STrengthening the Reporting of OBservational Studies in Epidemiology [STROBE] Diagram. Life Influences on Fetal Environments Study (2009–2011). LIFE Life Influences on Fetal Environments Study, PTD preterm delivery, CESD Centers for Epidemiologic Studies-Depression.
Results
Table 2 shows demographic characteristics of the study participants, by PTD status. The mean age of the sample was roughly 25 years (standard deviation 5.7). The majority (84 %) of women were not married, and 62 % reported an annual income of <$35,000/year. More than half of the study participants resided in the central city (compared to the surrounding suburbs), and most (65 %) were residents in their current neighborhood for ≤2 years. More women who had a PTD reported poor psychosocial indicators, as measured by the CES-D, perceived stress, and psychological distress scales, than women who had a term birth.
TABLE 2.
Participant characteristics by preterm delivery status, Life Influences on Fetal Environments Study, 2009–2011 (n = 399)
| Total sample | Term delivery | Preterm | P | |
|---|---|---|---|---|
| N = 399 | N = 334 | N = 64 | ||
| N (%) | N (%) | N (%) | ||
| Age | 0.21 | |||
| 18–19 | 71 (17.8) | 61 (18.3) | 9 (14.1) | |
| 20–24 | 151 (37.8) | 122 (36.5) | 29 (45.3) | |
| 25–29 | 89 (22.3) | 80 (23.9) | 9 (14.1) | |
| 30–34 | 51 (12.8) | 43 (12.9) | 8 (12.5) | |
| 35+ | 37 (9.3) | 28 (8.4) | 9 (14.1) | |
| Marital status | 0.42 | |||
| Married | 63 (15.8) | 55 (16.5) | 8 (12.5) | |
| Not married | 335 (84) | 278 (83.5) | 56 (87.5) | |
| Income | 0.19 | |||
| Under $35,000 | 246 (61.7) | 201 (76.7) | 45 (84.9) | |
| $35,000 or more | 69 (17.3) | 61 (23.3) | 8 (15.1) | |
| Current city of residence | 0.58 | |||
| Detroit | 213 (53.4) | 176 (55.2) | 36 (59) | |
| Suburb | 168 (42.1) | 143 (44.8) | 25 (41) | |
| Time in current neighborhood | 0.48 | |||
| ≤24 months | 258 (64.7) | 219 (65.6) | 39 (60.9) | |
| >24 months | 141 (35.3) | 115 (34.4) | 25 (39) | |
| CES-D (median split)a | 0.005 | |||
| <10 | 187 (49.9) | 167 (52.9) | 19 (32.8) | |
| ≥10 | 188 (50.1) | 149 (47.2) | 39 (67.2) | |
| Perceived stress | 0.13 | |||
| <41 | 188 (47.1) | 163 (50.6) | 24 (40) | |
| ≥41 | 195 (48.9) | 159 (49.4) | 36 (60) | |
| Psychological distress | 0.15 | |||
| <13 | 172 (43.1) | 149 (46.1) | 22 (36.1) | |
| ≥13 | 213 (53.4) | 174 (53.9) | 39 (63.9) |
aMissing n = 25
Table 3 shows the correlations among the perceived neighborhood and psychosocial variables. All correlations were significantly different from 0 (p < 0.05), except for those between CES-D and food availability (p = 0.10). The highest correlation among the perceived neighborhood variables was between social disorder and safety (−0.72), and the lowest was between social disorder and food availability (−0.28). Among the psychosocial variables, all of the correlations were moderate (<0.70).
TABLE 3.
Correlations between neighborhood and psychosocial variables; Life Influences on Fetal Environments Study 2009–2011 (n = 399)
| Variable no. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| Perceived neighborhood scales | ||||||||
| 1 | Safety | 1 | ||||||
| 2 | Walkability | 0.59 | 1 | |||||
| 3 | Food availability | 0.27 | 0.50 | 1 | ||||
| 4 | Social disorder | −0.72 | −0.54 | −0.28 | 1 | |||
| Psychosocial indicators | ||||||||
| 5 | CES-D subscale | −0.18 | −0.15 | −0.08 | 0.14 | 1 | ||
| 6 | Psychological distress | −0.12 | −0.11 | −0.11 | 0.13 | 0.65 | 1 | |
| 7 | Perceived stress | −0.17 | −0.15 | −0.12 | 0.15 | 0.67 | 0.54 | 1 |
| Mean | 20.42 | 23 | 7.18 | 12.67 | 11.58 | 13.67 | 40.93 | |
| Standard deviation | 5.72 | 4.10 | 2.23 | 5.07 | 8.74 | 4.43 | 5.26 | |
CES-D Centers for Epidemiologic Studies-Depression
In Figs. 2, 3, 4, and 5, we present path analyses which test for mediation by three psychosocial indicators (CES-D, psychological distress, and perceived stress) of the associations between perceived neighborhood safety, walkability, food availability, and social disorder (respectively), and PTD rates. We found evidence of mediation by CES-D of the association between perceived safety and PTD, but not by psychological distress or perceived stress. Said differently, lower perceived neighborhood safety was associated with higher levels of depressive symptoms which was associated with higher PTD rates. The associations between PTD and perceived walkability, food availability, and social disorder were not mediated by the psychosocial indicators examined. However, we found evidence that perceived neighborhood social disorder may have a direct effect on PTD rates. In other words, higher levels of neighborhood social disorder was associated with higher PTD rates, net of indirect paths through the psychosocial indicators examined.
Discussion
The main finding of this study is that among AA women with low educational attainment (≤12 years), perceptions of neighborhood safety are inversely associated with depressive symptoms which are positively associated PTD rates. Said differently, among AA women with ≤12 years of education, the association between perceptions of neighborhood safety and PTD operates, to some degree, through depressive symptoms. We also found evidence that negative perceptions of neighborhood social disorder are positively associated with PTD rates (regardless of any pathway through the psychosocial indicators examined). Contrary to our study hypotheses, we found no evidence that the associations between perceived walkability, food availability or social disorder, and PTD were mediated by psychosocial indicators. To our knowledge, ours is the first study to examine and report evidence for the mediating role of psychosocial factors on associations between perceptions of the residential environment and PTD.
African American women who reside in urban environments can experience significant psychological stress due to neighborhood poverty and violence.31 Chronic or cumulative stress such as that resulting from living in poor and unsafe neighborhoods may increase allostatic load (dysregulation of the adaptive system that can lead to disease) and alter allostasis, leading to alterations in immune functions and negative health outcomes.32 – 34 Stress and its consequent psychological dysfunction (i.e., depressive symptoms) has been related to higher levels of systemic inflammation in pregnant women.35 – 37 Systemic inflammation during pregnancy may lead to premature rupture of membranes, preterm labor, and ultimately PTD.35 , 37 – 44 Therefore, systemic inflammation may be the pathway by which perceived neighborhood safety and depressive symptoms impact PTD. Future research needs to examine the impact of systemic inflammation on the relationships among perceived neighborhood safety, depressive symptoms, and PTD.
We found that for women who were similar in terms of psychosocial indicators, those who reported more neighborhood social disorder had higher PTD rates than those who reported less disorder. Neighborhood social disorder, which is defined as “visible cues indicating a lack of order and social control”,11 is likely stress-inducing.45 The “broken windows” theory of urban decline suggests that public disorder causes urban decay and serious crime, and has been linked to adverse mental and physical health outcomes.46 On the other hand, perceptions of social disorder have been associated with social influences including racial and socioeconomic composition.47 It may be that perceptions of disorder vary based on actual disorder and individual characteristics of the residents and social structure of the neighborhood.10 The women in our study who had a PTD may reside in neighborhoods with more poverty than women who did not, especially since neighborhood poverty has been shown to be a significant predictor of perceived disorder. Additional research is needed to better understand the relationship between perceptions of neighborhood social disorder and PTD.
While related, the CES-D, perceived stress, and psychological distress scales measure different psychological processes.48 Despite this, we hypothesized that all three processes could be impacted by residing in adverse neighborhoods. However, we found no evidence that psychological distress or perceived stress were on the pathway linking perceived neighborhood context to PTD. Perceived stress measures have not be consistently predictive for PTD, among African American women. This may suggest that the survey instruments that are widely used in population-based research may not be applicable across all race/ethnic and socioeconomic groups. More research on the measurement of stress using survey methods, as well as biological indicators of stress, among high-risk groups is warranted.
Our study has several strengths that distinguish it from the existing literature. First, we used primary data collection for social risk factors, rather than relying on secondary analysis of birth certificate data, in an effort to understand the increased risk of PTD among urban AA women. As a result, we were able to identify and examine a potential pathway linking subjective reports of the residential environment to PTD rates, among high-risk women. Our study also included women recruited in the immediate postpartum period, who received late or no prenatal care, as well as earlier yet interrupted or irregular care. As a result, the likelihood of heterogeneity in PTD risk in the sample, as well as the generalizability of our findings, may be increased. Finally, this study builds on previously reported findings of moderation of the association between perceptions of neighborhood context and PTD, by educational attainment,9 in that we explicitly test hypotheses that these associations operate through psychosocial factors, among AA women.
In interpreting the results of this study, the following limitations should be considered. First, this study used retrospectively collected data, and as a result, it is possible that women may have reported depressive symptoms based on the outcome of their birth. Future studies should utilize a prospective study design and examine the impact of neighborhood context and depressive symptoms during pregnancy on risk of PTD. The CES-D is a screening tool that may capture symptoms that are correlated with major depression.49 , 50 The LIFE study does not include diagnostic mental health measures, which are considered the gold standard for mental health assessment, and we could not account for pharmacologic treatment for clinical depression. Our study design also does not allow for inferences regarding causality. Finally, it is possible that women with higher levels of depressive symptoms may have reported worse neighborhood environments.
In summary, our study is the first to provide evidence that suggests that (1) decreased perceived neighborhood safety may be associated with increased levels of depressive symptomology, which may increase PTD rates, and (2) net of the impact of psychosocial factors, higher perceived neighborhood social disorder is associated with higher PTD rates among urban AA women with low educational attainment. Future research should examine other potential mediators, such as behavioral and other psychosocial factors (e.g., stress coping). If depressive symptoms are on the causal pathway linking perceptions of neighborhood safety and PTD, individual-level interventions aimed at stress coping, as well as neighborhood-level initiatives focused on increasing physical and social features of urban, low-income areas, may result in decreased PTD rates.
Acknowledgments
This work was funded in part by a grant from National Institutes of Health #1F32HD080338.
Compliance with Ethical Standards
This study was approved by the institutional review boards at the University of Michigan, St. John Providence Health System, and Wayne State University. All study participants gave written informed consent.
References
- 1.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Reproductive Health: Preterm Birth. 2013; http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/PretermBirth.htm. Accessed April 26, 2013.
- 3.Martin J, Hamilton B, Osterman M, Curtin S, Matthews T. Births: Final Data for 2012. National Vital Statistics Reports; Volume 62 Number 9. Vol 62 No 9. Hyattsville, MD: U.S Department of Health & Human Services; 2013. [PubMed] [Google Scholar]
- 4.National Center for Health Statistics, first natality data. 2015; http://www.marchofdimes.org/Peristats/ViewSubtopic.aspx?reg=99&top=3&stop=63&lev=1&slev=1&obj=1. Accessed 8 Dec 2015.
- 5.Osypuk TL, Galea S, McArdle N, Acevedo-Garcia D. Quantifying separate and unequal: racial-ethnic distributions of neighborhood poverty in Metropolitan America. Urban Aff Rev. 2009;45(1):25–65. doi: 10.1177/1078087408331119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Logan J, Stults B. Separate and Unequal: the Neighborhood Gap for Blacks, Hispanics and Asians in Metropolitan America. Providence, RI: Russell Sage Foundation and The American Communities Project of Brown University; 2011. [Google Scholar]
- 7.Dole N, Savitz DA, Siega-Riz AM, Hertz-Picciotta I, McMahon MJ, Buekens P. Psychosocial factors and preterm birth among African American and white women in central North Carolina. Am J Public Health. 2004;94(8):1358–1365. doi: 10.2105/AJPH.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giurgescu C, Zenk SN, Dancy BL, Park CG, Dieber W, Block R. Relationships among neighborhood environment, racial discrimination, psychological distress, and preterm birth in African American women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E51–E61. doi: 10.1111/j.1552-6909.2012.01409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sealy-Jefferson S, Giurgescu C, Helmkamp L, Misra DP, Osypuk TL. Perceived physical and social residential environment and preterm delivery in African-American women. Am J Epidemiol. 2015;182(6):485–493. doi: 10.1093/aje/kwv106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sampson RJ, Raudenbush SW. Seeing disorder: neighborhood stigma and the social construction of “broken windows”. Soc Psychol Q. 2004;67(4):319–342. doi: 10.1177/019027250406700401. [DOI] [Google Scholar]
- 11.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42(3):258–276. doi: 10.2307/3090214. [DOI] [PubMed] [Google Scholar]
- 12.Schulz A, Williams D, Israel B, et al. Unfair treatment, neighborhood effects, and mental health in the Detroit metropolitan area. J Health Soc Behav. 2000;41(3):314–332. doi: 10.2307/2676323. [DOI] [PubMed] [Google Scholar]
- 13.Hill TD, Ross CE, Angel RJ. Neighborhood disorder, psychophysiological distress, and health. J Health Soc Behav. 2005;46(2):170–186. doi: 10.1177/002214650504600204. [DOI] [PubMed] [Google Scholar]
- 14.Gary TL, Stark SA, LaVeist TA. Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Health & place. 2007;13(2):569–575. doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Accortt EE, Cheadle AC, Dunkel SC. Prenatal depression and adverse birth outcomes: an updated systematic review. Matern Child Health J. 2015;19(6):1306–1337. doi: 10.1007/s10995-014-1637-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunkel SC. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62(1):531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- 17.Kramer MS, Platt RW, Wen SW, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108(2):e35–e35. doi: 10.1542/peds.108.2.e35. [DOI] [PubMed] [Google Scholar]
- 18.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165(8):858–867. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- 19.Echeverria SE, Diez-Roux AV, Link BG. Reliability of self-reported neighborhood characteristics. J Urban Health. 2004;81(4):682–701. doi: 10.1093/jurban/jth151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 21.Stahl T, Rutten A, Nutbeam D, et al. The importance of the social environment for physically active lifestyle—results from an international study. Soc Sci Med. 2001;52(1):1–10. doi: 10.1016/S0277-9536(00)00116-7. [DOI] [PubMed] [Google Scholar]
- 22.Orr ST, James SA, Blackmore PC. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156(9):797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- 23.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 24.Canady RB, Stommel M, Holzman C. Measurement properties of the centers for epidemiological studies depression scale (CES-D) in a sample of African American and non-Hispanic White pregnant women. J Nurs Meas. 2009;17(2):91–104. doi: 10.1891/1061-3749.17.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 26.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 27.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 28.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- 29.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- 30.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: a Regression-Based Approach. New York, NY: Guilford Press; 2013.
- 31.Gruenberg DA, Wright RJ, Visness CM, et al. Relation between stress and cytokine responses in inner-city mothers. Ann Allergy Asthma Immunol. 2015;115(5):439–445. doi: 10.1016/j.anai.2015.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McEwen BS. Brain on stress: how the social environment gets under the skin. Proc Natl Acad Sci U S A. 2012;109(SUPPL.2):17180–17185. doi: 10.1073/pnas.1121254109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peters A, McEwen BS. Introduction for the allostatic load special issue. Physiol Behav. 2012;106(1):1–4. doi: 10.1016/j.physbeh.2011.12.019. [DOI] [PubMed] [Google Scholar]
- 34.McEwen BS. Stressed or stressed out: what is the difference? J Psychiatry Neurosci. 2005;30(5):315–318. [PMC free article] [PubMed] [Google Scholar]
- 35.Cassidy-Bushrow AE, Peters RM, Johnson DA, Templin TN. Association of depressive symptoms with inflammatory biomarkers among pregnant African-American women. J Reprod Immunol. 2012;94(2):202–209. doi: 10.1016/j.jri.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 36.Christian LM, Franco A, Glaser R, Iams JD. Depressive symptoms are associated with elevated serum proinflammatory cytokines among pregnant women. Brain Behav Immun. 2009;23(6):750–754. doi: 10.1016/j.bbi.2009.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coussons-Read ME, Lobel M, Carey JC, et al. The occurrence of preterm delivery is linked to pregnancy-specific distress and elevated inflammatory markers across gestation. Brain Behav Immun. 2012;26(4):650–659. doi: 10.1016/j.bbi.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coussons-Read ME, Okun ML, Schmitt MP, Giese S. Prenatal stress alters cytokine levels in a manner that may endanger human pregnancy. Psychosom Med. 2005;67(4):625–631. doi: 10.1097/01.psy.0000170331.74960.ad. [DOI] [PubMed] [Google Scholar]
- 39.Schminkey DL, Groer M. Imitating a stress response: a new hypothesis about the innate immune system’s role in pregnancy. Med Hypotheses. 2014;82(6):721–729. doi: 10.1016/j.mehy.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 40.Chatterjee P, Chiasson VL, Bounds KR, Mitchell BM. Regulation of the anti-inflammatory cytokines interleukin-4 and interleukin-10 during pregnancy. Front Immunol. 2014;5:253. doi: 10.3389/fimmu.2014.00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Giurgescu C, Engeland CG, Zenk SN, Kavanaugh K. Stress, inflammation and preterm birth in African American Women. Newborn and Infant Nursing Reviews. 2013;13(4):171–177. doi: 10.1053/j.nainr.2013.09.004. [DOI] [Google Scholar]
- 42.Gargano JW, Holzman C, Senagore P, et al. Mid-pregnancy circulating cytokine levels, histologic chorioamnionitis and spontaneous preterm birth. J Reprod Immunol. 2008;79(1):100–110. doi: 10.1016/j.jri.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ruiz RJ, Jallo N, Murphey C, Marti CN, Godbold E, Pickler RH. Second trimester maternal plasma levels of cytokines IL-1Ra, Il-6 and IL-10 and preterm birth. J Perinatol. 2012;32(7):483–490. doi: 10.1038/jp.2011.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vogel I, Goepfert AR, Thorsen P, et al. Early second-trimester inflammatory markers and short cervical length and the risk of recurrent preterm birth. J Reprod Immunol. 2007;75(2):133–140. doi: 10.1016/j.jri.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 45.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010; 1186.1: 125–145. [DOI] [PubMed]
- 46.Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. J Health Soc Behav. 1996;37(4):293–310. doi: 10.2307/2137258. [DOI] [PubMed] [Google Scholar]
- 47.Franzini L, Caughy MOB, Nettles SM, O’Campo P. Perceptions of disorder: contributions of neighborhood characteristics to subjective perceptions of disorder. J Environ Psychol. 2008;28(1):83–93. doi: 10.1016/j.jenvp.2007.08.003. [DOI] [Google Scholar]
- 48.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Wiley; 2008.
- 49.Radloff LS, Locke BZ. The Community Mental Health Assessment Survey and CES-D Scale. In: Weissman MM, J.K. M, eds. Community Surveys of Psychiatric Disorders. eds. ed. New Brunswick, NJ: Rutgers University Press; 1986:177-189.
- 50.Orr ST, Blazer DG, James SA, Reiter JP. Depressive symptoms and indicators of maternal health status during pregnancy. J Women’s Health. 2007;16(4):535–542. doi: 10.1089/jwh.2006.0116. [DOI] [PubMed] [Google Scholar]