Abstract
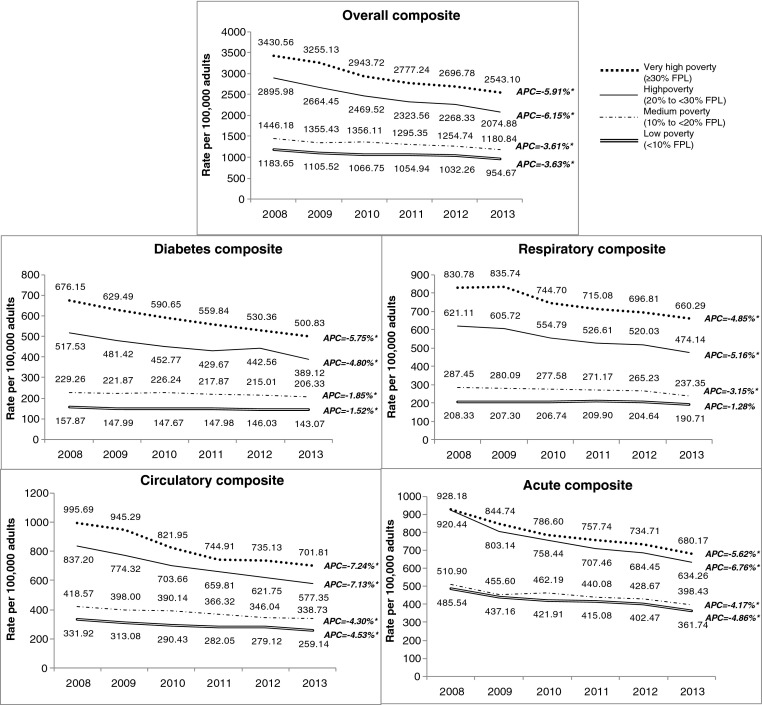
Knowing which demographic groups have higher rates of preventable hospitalizations can help identify geographic areas where improvements in primary care access and quality can be made. This study assessed whether preventable hospitalization rates by neighborhood poverty decreased from 2008 to 2013 and whether the gap between very high and low poverty neighborhoods changed. We examined trends in age-adjusted preventable hospitalization rates and rate ratios by neighborhood poverty overall and by sex using JoinPoint regression. Prevention Quality Indicators (PQIs) developed by the Agency for Healthcare Research and Quality were applied to inpatient hospitalization data from the New York State Department of Health’s Statewide Planning and Research Cooperative System. PQIs were classified into composites. From 2008 to 2013, preventable hospitalization rates per 100,000 adults across each poverty group decreased. For very high poverty neighborhoods (ZIP codes with ≥30 % of persons living below the federal poverty level (FPL)), there were significant decreases overall (3430.56 to 2543.10, annual percent change [APC] = −5.91 %), for diabetes (676.15 to 500.83, APC = −5.75 %), respiratory (830.78 to 660.29, APC = −4.85 %), circulatory (995.69 to 701.81, APC = −7.24 %), and acute composites (928.18 to 680.17, APC = −5.62 %). The rate ratios also decreased over time; however, in 2013, the rates for very high poverty neighborhoods were two to four times higher than low poverty neighborhoods (ZIP codes with <10 % of persons below the FPL). While preventable hospitalization rates have decreased over time, disparities still exist. These findings underscore the need to ensure adequate access to quality and timely primary care among individuals living in high poverty neighborhoods.
Keywords: Preventable hospitalizations, Ambulatory care sensitive hospitalizations, Neighborhood poverty
Introduction
Preventable hospitalizations are admissions that could have potentially been prevented with quality outpatient care. Delaying or not receiving care for conditions such as asthma, diabetes, and hypertension can result in hospitalizations that may have been avoided.1 Hospitalizations tend to be more resource intensive than outpatient care; therefore, preventable hospitalizations (also called ambulatory care-sensitive hospitalizations) are often used as an indicator of health system efficiency.2 Knowing which demographic groups have higher rates of preventable hospitalizations can highlight disparities in access to quality and timely primary care and help identify populations for whom improvements in the health care system may be most beneficial.3 , 4 Previous research has documented that preventable hospitalizations are associated with an individual’s lack of health insurance,5 regular medical provider or source of care,6 , 7 and continuity of care,8 and with underlying disease prevalence.4 A relationship between provider supply and preventable hospitalizations has also been found although the relationship with supply is not consistent.4 , 9 – 13 For example, not every study finds that low provider supply is a significant predictor of preventable hospitalizations. Additionally, Black race and Hispanic ethnicity8 , 14 – 16 have been associated with higher rates of preventable hospitalizations.
Neighborhood characteristics may also be relevant, as preventable hospitalizations are associated with residence in low-income neighborhoods.1 A growing literature documents the intersection between place and health, building on evidence that poor health outcomes tend to be concentrated in certain neighborhoods, due both to socioeconomic inequities and a lack of available health care resources.17 – 19 Neighborhood economic and social characteristics (e.g., average household income, racial/ethnic composition) have been shown to be associated with the prevalence and quality of management of chronic conditions such as hypertension and diabetes,20 – 22 and with factors that can undermine individual health, such as a lack of access to healthy foods23 , 24 and increased exposure to poor environmental conditions.25 , 26
Previously we found that in 2007, that adults living in high poverty neighborhoods had higher preventable hospitalization rates,27 adding to the literature on neighborhood poverty and poor health outcomes.28 – 32 Given that access to high quality primary care has been receiving renewed attention as part of efforts to transform the health care delivery system (e.g., patient centered medical home33 and advanced primary care34 , 35), and the presence of place-based initiatives in NYC to improve the overall resiliency of neighborhoods and support the health of individuals have been initiated or will be implemented,23 we examined preventable hospitalization rates in New York City by neighborhood poverty to determine if a gap between high and low poverty neighborhoods still exists. In addition, with the health insurance expansion components of the 2010 Patient Protection and Affordable Care Act and requirement of coverage for certain clinical preventive services at no cost, we would expect that preventable hospitalizations would decrease after 2014. This analysis can also serve as a baseline for future trend analyses measuring the impact of health reform.
Methods
Data Sources and Definitions
Inpatient hospitalization data were obtained from the New York State Department of Health’s Statewide Planning and Research Cooperative System (SPARCS) (2008–2013). SPARCS is a comprehensive patient level all payer data reporting system including every hospital discharge in New York State. The analysis was limited to hospitalizations of NYC residents (as determined by patient zip code of residence) in any hospital in NYS (inside or outside of NYC).
The Agency for Healthcare Research and Quality (AHRQ) Prevention Quality Indicators (PQI) version 4.5a definitions were applied to inpatient hospitalizations and categorized into the following composites: overall (any PQI); diabetes (PQI 1—diabetes short-term complications, PQI 3—diabetes long-term complications, PQI 14—uncontrolled diabetes, and PQI 16—lower-extremity amputation); respiratory (PQI 5—chronic obstructive pulmonary disease or asthma in older adults, PQI 15—asthma in younger adults); circulatory (PQI 7—hypertension, PQI 8—heart failure, PQI 13—angina without procedure); and acute (PQI 10—dehydration, PQI 11—bacterial pneumonia, PQI 12—urinary tract infection).36
We used the DOHMH’s Bureau of Epidemiology Services NYC interpolated intercensal population estimates from the US Census Bureau and ZIP code-level poverty groups with poverty status based on the American Community Survey (ACS) poverty definitions. The 2009–2013 5-year ACS file was used for all hospitalization years. This file was used to assign a neighborhood poverty level to a ZIP code and that ZIP code retained that poverty level for all 6 years. Neighborhood poverty was defined as the percent of the population in a given ZIP code with a household income below the federal poverty threshold. Population estimates and inpatient hospitalizations based on the patient’s ZIP code of residence were grouped into the standard four neighborhood poverty categories used by the DOHMH: low poverty (<10 % of the population below the federal poverty level); medium (10 to <20 %); high (20 to <30 %); and very high poverty (≥30 %).
Statistical Analysis
Preventable hospitalization rates were calculated for each neighborhood poverty level and age-adjusted to the US 2000 Standard Population using the following age groups: 18–24 years, 25–44 years, 45–64 years, and 65 years and over. Rates were also stratified by sex. We calculated the preventable hospitalization rate ratio and standard errors of very high poverty neighborhoods to low poverty neighborhoods from 2008 to 2013 using SAS version 9.2. The rate ratios for 2008 and 2013 were compared using a two-sample z-test.
Temporal trends examining age-adjusted rates and rate ratios were generated by fitting log-linear regression models using Joinpoint software version 4.2.0.1 (National Cancer Institute). Statistical significance was defined as P < 0.05.
Results
Very high poverty neighborhoods had the highest rates of preventable hospitalizations every year for each composite but not each individual PQI (data not shown). From 2008 to 2013, there was a decrease in preventable hospitalization rates overall and for each composite (Fig. 1). The declines were statistically significant (P < 0.05) for each poverty group, for overall preventable hospitalizations and for each composite (diabetes, respiratory, circulatory, and acute) except for respiratory hospitalizations in the low poverty group. The annual percent change was greater for high poverty and very high poverty groups than medium and low poverty groups for overall preventable hospitalizations (high poverty: −6.15 %, P < .001; very high poverty: −5.91 %, P < .001), diabetes (high poverty: −4.80 %, P = 0.004; very high poverty: −5.75 %, P < .001), respiratory (high poverty: −5.16 %, P < .001; very high poverty: −4.85 %, P = 0.002), circulatory (high poverty: −7.13 %, P < .001; very high poverty: −7.24 %, P = 0.001), and acute conditions (high poverty: −6.74 %, P = 0.001; very high poverty: −5.62 %, P < .001) (Fig. 1).
FIG. 1.
Preventable hospitalization rates for New York City residents overall and by diabetes, respiratory, circulatory, and acute conditions, by neighborhood poverty 2008–2013. Source: NYS Dept of Health SPARCS 2008–2013 (updated July 2014 for 2008–2010, December 2014 for 2011–2012, June 2015 for 2013). Preventable Hospitalizations based on AHRQ PQI version 4.5a, updated 2014. Population data for rates from NYCDOHMH interpolated intercensal Population Estimates, modified from US Census Bureau, using poverty groups from the American Community Survey 2009–2013. Neighborhood poverty (based on ZIP codes) defined as percent of residents with incomes below 100 % of the Federal Poverty Level, per American Community Survey, 2008–2013. ZIP codes with zero people for whom poverty status could be determined are excluded from the analysis. Rates per 100,000 are age-adjusted to the US 2000 Standard Population.*P < .05. APC annual percent change.
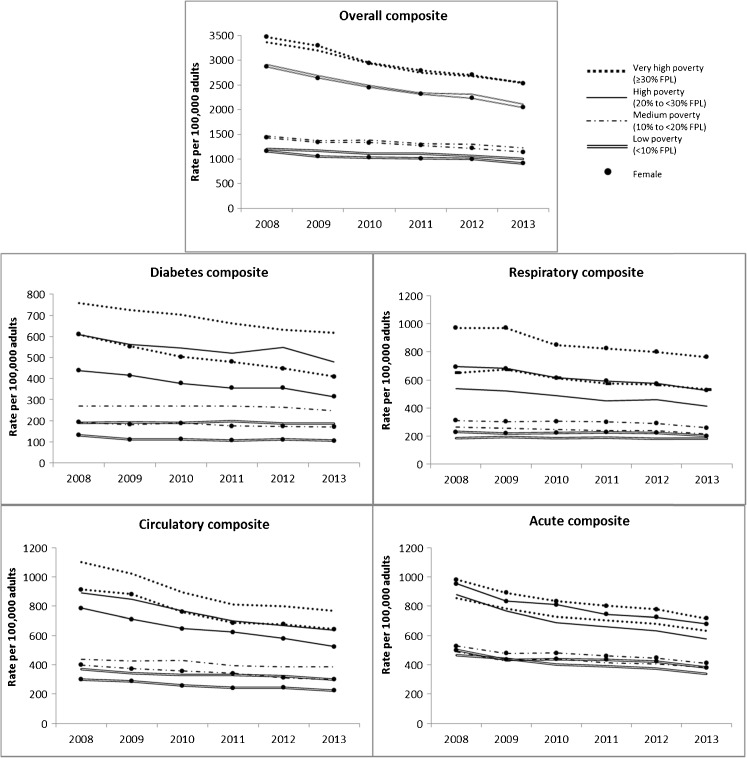
When preventable hospitalization rates were stratified by sex, the rates for the overall composite were similar for males and females. For the diabetes composite, the rates were higher for males than females in very high and high poverty neighborhoods but for the respiratory composites they were higher for females than males in very high and high poverty neighborhoods (Fig. 2). There were statistically significant declines for males and females across all poverty groups for the overall, circulatory and acute composites. However, for the diabetes composite, the decline was not significant for the low poverty group for males and females and for males in the medium poverty group. For the respiratory composite, there was no statistically significant decline in high poverty group.
FIG. 2.
Preventable hospitalization rates for New York City residents by neighborhood poverty and sex, 2008–2013. Source: NYS Dept of Health SPARCS 2008–2013 (updated July 2014 for 2008–2010, December 2014 for 2011–2012, June 2015 for 2013). Preventable Hospitalizations based on AHRQ PQI version 4.5a, updated 2014. Population data for rates from NYCDOHMH interpolated intercensal Population Estimates, modified from US Census Bureau, using poverty groups from the American Community Survey 2009–2013. Neighborhood poverty (based on ZIP codes) defined as percent of residents with incomes below 100 % of the Federal Poverty Level, per American Community Survey, 2008–2013. ZIP codes with zero people for whom poverty status could be determined are excluded from the analysis. Rates per 100,000 are age-adjusted to the US 2000 Standard Population. Trends in preventable hospitalization rates not statistically significant for diabetes for females in low poverty neighborhoods, and males in low and medium poverty neighborhoods, and respiratory conditions for females and males in low poverty neighborhoods.
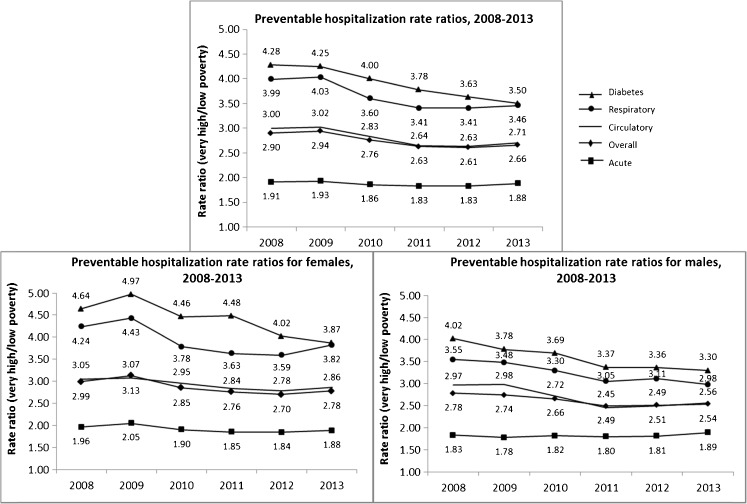
There was a statistically significant decline in the rate ratio of very high to low poverty groups for overall preventable hospitalizations (annual percent change [APC] = −2.35 %, P = 0.023), diabetes (APC = −4.15 %, P < .001), respiratory (APC = −3.40 %, P = 0.022), and circulatory (APC = −2.76 %, P =0.033) composites. A similar finding was found by sex for males (significant decline for rate ratios for all composites except for the acute composite). For females, the decline was not statistically significant for the rate ratio for the overall, respiratory, and acute composites (Fig. 3). The difference between the two rate ratios in 2008 and 2013 was only statistically significant for diabetes in the overall population (4.28 vs. 3.50, P = 0.043) and among males (4.02 vs. 3.30, P = 0.025); there were no differences between the rate ratios in 2008 and 2013 for females (Fig. 3). Preventable hospitalization rates in 2013 for very high poverty neighborhoods ranged from two to four times higher than low poverty neighborhoods.
FIG. 3.
Preventable hospitalization rate ratios for New York City residents living in very high poverty neighborhoods versus low poverty neighborhoods, overall and by sex, 2008–2013. Source: NYS Dept of Health SPARCS 2008–2013 (updated July 2014 for 2008–2010, December 2014 for 2011–2012, June 2015 for 2013). Preventable Hospitalizations based on AHRQ PQI version 4.5a, updated 2014. Population data for rates from NYCDOHMH interpolated intercensal Population Estimates, modified from US Census Bureau, using poverty groups from the American Community Survey 2009–2013. Neighborhood poverty (based on ZIP codes) defined as percent of residents with incomes below 100 % of the Federal Poverty Level, per American Community Survey, 2008–2013. ZIP codes with zero people for whom poverty status could be determined are excluded from the analysis. Rates per 100,000 are age-adjusted to the US 2000 Standard Population. Trends in rate ratios not statistically significant for acute conditions (overall, for males and for females), and not statistically significant for females for respiratory and overall preventable hospitalizations.
The rate ratios for the individual PQIs for diabetes and respiratory conditions—the composites with the larger disparities between very high and low poverty neighborhoods—showed even greater differences than when rolled up in their respective composites. Lower-extremity amputations were rare (<450 hospitalizations per year for each neighborhood poverty group) and only made up approximately 5 % of preventable diabetes hospitalizations. However, the hospitalization rate for lower-extremity amputation increased over time in very high poverty neighborhoods while it decreased in low poverty neighborhoods, resulting in a rate ratio of 5.22 in 2013 compared to a rate ratio of 3.42 in 2008. A large difference was also observed for uncontrolled diabetes in 2008, 6.98 times higher in very high poverty neighborhoods, which has since decreased to 3.89 in 2013. For respiratory conditions, the proportion of the PQI asthma in younger adults 18–39 years was on average 15 % in very high poverty neighborhoods compared with 6 % in low poverty neighborhoods. The rate ratio for asthma hospitalizations in 2013 was 5.35 (See appendix for rate ratios for each PQI).
Discussion
We found that preventable hospitalization rates decreased from 2008 to 2013 for all neighborhood poverty groups. However, the overall disparity between very high and low poverty neighborhoods did not significantly decrease between 2008 and 2013. Further, we found that improvements differed by sex. Our finding that very high neighborhood poverty is associated with higher preventable hospitalization rates builds on Billings and colleagues’ analysis of New York City hospitalizations 20 years ago (1982 to 1993), although they found the disparity between low-income and high-income neighborhoods increased during that time period.1 Studies in countries with universal health coverage have also found that preventable hospitalizations are higher for low-income populations and residents living in low-income neighborhoods,37 , 38 suggesting that quality and availability of primary care may be an issue for people living in high poverty neighborhoods regardless of insurance status. In New York City, every very high poverty neighborhood also qualifies as a federally designed Health Professional Shortage Area or Medically Underserved Area in whole or in part, indicating that these areas or populations have a shortage of primary medical care.39
There are several limitations with this analysis. We did not analyze patient race/ethnicity because it is not coded reliably for some hospitals in New York State. The New York State Department of Health (NYS DOH) conducted a concordance analysis of race and ethnicity data elements in linked data between SPARCS (hospitalization data) and Medicaid and between SPARCS and Vital Statistics and found that concordance rates varied significantly across hospitals; for 22 of 62 New York City hospitals, fewer than 50 % of matched patients’ race was the same in both data sets.40 As of 2014, NYS DOH is requiring New York State hospitals to collect expanded race and ethnicity data to improve data quality. Although we did not specifically look at race/ethnicity in this analysis, we do know that high poverty areas in New York City also have a high concentration of non-Hispanic Black and Hispanic residents (e.g., approximately three-quarters of very high poverty ZIP codes have populations where 80 % or more of the population was Black or Hispanic41). Other analyses have found that Blacks and Hispanics have higher preventable hospitalization rates than other racial/ethnic groups.8 , 14 – 16 Second, coding of conditions may differ by hospital and may change over time. Third, this was an ecologic study. We did not have data on individual or household income and thus do not know the relative extent to which neighborhood versus individual socioeconomic status drove our findings. Last, we do not know the direction of causality. Living in high poverty neighborhoods may contribute to poorer health that can lead to hospitalization or poor health might lead to residence in high poverty neighborhoods.
This analysis shows that preventable hospitalization rates have been decreasing since 2008 but that the disparity between very high and low poverty neighborhoods still persists. While better access to and utilization of quality health care in high poverty neighborhoods may reduce preventable hospitalization rates and narrow the gap between very high and low poverty neighborhoods, place-based initiatives to improve the physical environment and increase access to healthy food and physical activity are important prevention interventions as well. Additionally, current efforts to transform the Medicaid delivery system and payment reform programs in New York State will likely drive down future preventable hospitalizations for low-income populations. For example, the overall goal of the New York State Delivery System Reform Incentive Program is a 25 % reduction in avoidable hospital use (avoidable hospitalizations, emergency department visits, readmissions) over 5 years42. Furthermore, health care delivery models, such as Patient-Centered Medical Homes and Advanced Primary Care, may improve primary care delivery outcomes, especially for chronic conditions, through better delivery and care coordination. It will be important to monitor over time whether the disparity in rates of preventable hospitalizations by neighborhood poverty decreases as health delivery reform initiatives are more fully implemented and to understand what additional efforts can reduce the preventable hospitalization gap between very high and low poverty neighborhoods.
Acknowledgments
We thank Shadi Chamany for her review and constructive comments on the preparation of this manuscript.
Appendix
TABLE 1.
Rate ratios by Prevention Quality Indicator (PQI) for New York City residents living in very high poverty neighborhoods versus low poverty neighborhoods, 2008–2013
| Rate ratio | P value | APC | P value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | (trend) | (2008 vs 2013) | ||
| Diabetes | |||||||||
| Short-term complications (PQI 01) | 4.68 | 5.29 | 4.87 | 4.57 | 4.20 | 3.67 | 0.179 | −3.14 | 0.057 |
| Long-term complications (PQI 03) | 3.70 | 3.56 | 3.44 | 3.38 | 3.32 | 3.30 | 0.004 | −2.35 | 0.147 |
| Uncontrolled diabetes (PQI 14) | 6.98 | 6.52 | 5.73 | 4.95 | 4.71 | 3.89 | 0.000 | −10.34 | <.0001 |
| Lower-extremity amputation PQI 16) | 3.42 | 3.72 | 4.39 | 3.78 | 3.09 | 5.22 | 0.372 | 4.38 | 0.000 |
| Respiratory | |||||||||
| COPD (PQI 05) | 3.77 | 3.78 | 3.47 | 3.23 | 3.24 | 3.30 | 0.017 | −3.28 | 0.305 |
| Asthma (PQI 15) | 6.66 | 7.22 | 5.25 | 5.79 | 5.51 | 5.35 | 0.083 | −4.84 | 0.224 |
| Circulatory | |||||||||
| Hypertension (PQI 07) | 3.77 | 3.73 | 3.30 | 2.73 | 2.84 | 3.03 | 0.013 | −7.1 | 0.099 |
| Heart failure (PQI 08) | 2.75 | 2.80 | 2.71 | 2.58 | 2.55 | 2.61 | 0.041 | −1.64 | 0.431 |
| Angina without procedure (PQI 13) | 3.90 | 3.69 | 2.73 | 3.12 | 2.95 | 2.89 | 0.193 | −9.73 | 0.000 |
| Acute | |||||||||
| Dehydration (PQI 10) | 1.71 | 1.71 | 1.88 | 1.87 | 1.93 | 1.78 | 0.228 | 2.16 | 0.410 |
| Bacterial pneumonia (PQI 11) | 1.85 | 1.93 | 1.79 | 1.86 | 1.78 | 2.02 | 0.710 | 0.54 | 0.408 |
| Urinary tract infection (PQI 12) | 2.24 | 2.14 | 1.95 | 1.76 | 1.80 | 1.82 | 0.010 | −4.91 | 0.199 |
References
- 1.Billings J, Anderson GM, Newman LS. Recent findings on preventable hospitalizations. Health Aff. 1996;15(3):239–249. doi: 10.1377/hlthaff.15.3.239. [DOI] [PubMed] [Google Scholar]
- 2.Moy E, Chang E, Barrett M. Potentially preventable hospitalizations—United States, 2001–2009. MMWR. 2013;62(3):139–143. [PubMed] [Google Scholar]
- 3.Russo CA, Andrews RM, Coffey RM. Racial and ethnic disparities in potentially preventable hospitalizations, 2003. HCUP Statistical Brief #10 2006;July 2006. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/statbriefs/sb10.pdf. Accessed March 2015. [PubMed]
- 4.Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274(4):305–311. doi: 10.1001/jama.1995.03530040033037. [DOI] [PubMed] [Google Scholar]
- 5.Weissman JS, Gatsonia C, Epstein AM. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992;268(17):2388–2394. doi: 10.1001/jama.1992.03490170060026. [DOI] [PubMed] [Google Scholar]
- 6.Falik M, Needleman J, Wells BL, Korb J. Ambulatory care sensitive hospitalizations and emergency visits: experiences of Medicaid patients using Federally Qualified Health Centers. Med Care. 2001;39(6):551–561. doi: 10.1097/00005650-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Wright B, Potter AJ, Trivedi A. Federally Qualified Health Center use among dual eligibles: rates of hospitalizations and emergency department visits. Health Aff. 2015;34(7):1147–1155. doi: 10.1377/hlthaff.2014.0823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng A, Chen C, Hou Y. A longitudinal examination of continuity of care and avoidable hospitalization. Arch Intern Med. 2010;170(18):1671–1677. doi: 10.1001/archinternmed.2010.340. [DOI] [PubMed] [Google Scholar]
- 9.Nayar P, Nguyen AT, Apenteng B, Yu F. Preventable hospitalizations: does rurality or non-physician clinician supply matter? J Community Health. 2012;37:487–494. doi: 10.1007/s10900-011-9468-1. [DOI] [PubMed] [Google Scholar]
- 10.Laditka JN. Physician supply, physician diversity, and outcomes of primary health care for older persons in the United States. Health Place. 2004;10(3):231–244. doi: 10.1016/j.healthplace.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 11.Falster MO, Jorm LR, Douglas KA, Blyth FM, Elliott RF, Leyland AH. Sociodemographic and health characteristics, rather than primary care supply, are major drivers of geographic variation in preventable hospitalizations in Australia. Med Care. 2015;53(5):436–445. doi: 10.1097/MLR.0000000000000342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laditka JN, Laditka SB, Probst JC. More may be better: evidence of a negative relationship between physician supply and hospitalization for ambulatory care sensitive conditions. Health Serv Res. 2005;40(4):1148–1166. doi: 10.1111/j.1475-6773.2005.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodman DC, Grumbach K. Does having more physicians lead to better health system performance? JAMA. 2008;299(3):335–337. doi: 10.1001/jama.299.3.335. [DOI] [PubMed] [Google Scholar]
- 14.Stranges E, Coffey RM, Andrews RM. Potentially preventable hospital stays among Hispanics, 2006. HCUP Statistical Brief #61 2008;October 2008. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb61.pdf. Accessed March 2015.
- 15.Will JC, Nwaise IA, Schieb L, Zhone Y. Geographic and racial patterns for preventable hospitalizations for hypertension: Medicare beneficiaries, 2004–2009. Public Health Rep. 2014;129(1):8–18. doi: 10.1177/003335491412900104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Neill SS, Lake T, Merrill A, Wilson A, Mann DA, Bartnyska LM. Racial disparities in hospitalizations for ambulatory care-sensitive conditions. Am J Prev Med. 2010;38(4):381–388. doi: 10.1016/j.amepre.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 17.Toprani A, Hadler JL. Selecting and applying a standard area-based socioeconomic status measure for public health data: analysis for New York City. New York City Department of Health and Mental Hygiene: Epi Research Report 2013:1–12.
- 18.Krieger N, Chen C, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—The Public Health Disparities Geocoding Project. Am J Public Health. 2003;93(10):1655–1671. doi: 10.2105/AJPH.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones K, Duncan C. Individuals and their ecologies: analysing the geography of chronic illness within a multilevel modelling framework. Health Place. 1995;1(1):27–40. doi: 10.1016/1353-8292(95)00004-6. [DOI] [Google Scholar]
- 20.Gaskin DJ, Thorpe RJ, McGinty EE, Bower K, Rohde C, Young JH, et al. Disparities in diabetes: the nexus of race, poverty, and place. Am J Public Health. 2014;104(11):2147–2155. doi: 10.2105/AJPH.2013.301420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kershaw KN, Diez-Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and black-white disparities in hypertension. Am J Epidemiol. 2011;174(5):537–545. doi: 10.1093/aje/kwr116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coulon SM, Wilson DK, Alia KA, Van Horn ML. Multilevel associations of neighborhood poverty, crime, and satisfaction with blood pressure in African-American adults. Am J Hypertens. 2016;29(1): 90–95. [DOI] [PMC free article] [PubMed]
- 23.Sacks R, Yi SS, Nonas C. Increasing access to fruits and vegetables: perspectives from the New York City experience. Am J Public Health. 2015;105(5):e29–e37. doi: 10.2105/AJPH.2015.302587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cannuscio CC, Tappe K, Hillier A, Buttenheim A, Karpyn A, Glanz K. Urban food environments and residents’ shopping behaviors. Am J Prev Med. 2013;45(5):606–614. doi: 10.1016/j.amepre.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 25.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 26.Camacho-Rivera M, Kawachi I, Bennett GG, Subramanian SV. Associations of neighborhood concentrated poverty, neighborhood racial/ethnic composition, and indoor allergen exposures: a cross-sectional analysis of Los Angeles households, 2006–2008. J Urban Health. 2014;91(4):661–676. doi: 10.1007/s11524-014-9872-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tria M, Jasek J, Summers C. Preventing hospitalizations in New York City. NYC Vital Signs 2012; 11(3): 1–4.
- 28.Gusmano MK, Rodwin VG, Weisz D. A new way to compare health systems: avoidable hospital conditions in Manhattan and Paris. Health Aff. 2006;25(2):510–520. doi: 10.1377/hlthaff.25.2.510. [DOI] [PubMed] [Google Scholar]
- 29.Winkleby M, Sundquist K, Cubbin C. Inequities in CHD incidence and case fatality by neighborhood deprivation. Am J Prev Med. 2007;32(2):97–106. doi: 10.1016/j.amepre.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Aff. 2014;33(5):778–785. doi: 10.1377/hlthaff.2013.0816. [DOI] [PubMed] [Google Scholar]
- 31.Taylor CB, Ahn D, Winkleby MA. Neighborhood and individual socioeconomic determinants of hospitalization. Am J Prev Med. 2006;31(2):127–134. doi: 10.1016/j.amepre.2006.03.025. [DOI] [PubMed] [Google Scholar]
- 32.Fitzpatrick T, Rosella LC, Calzavara A, Petch J, Pinto AD, Manson H, et al. Looking beyond income and education. Am J Prev Med. 2015;49(2):161–171. doi: 10.1016/j.amepre.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 33.Agency for Healthcare Research and Quality. https://www.pcmh.ahrq.gov/. Accessed January 2016. [DOI] [PubMed]
- 34.Centers for Medicare and Medicaid Services. https://innovation.cms.gov/initiatives/Advanced-Primary-Care/.
- 35.Burke G. Advancing Patient-Centered Medical Homes in New York. 2015;United Hospital Fund (Issue Brief):1–14.
- 36.Agency for Healthcare Research and Quality (AHRQ). Prevention Quality Indicators Technical Specifications v4.5. Available at www.qualityindicators.ahrq.gov. Accessed February 2014.
- 37.Roos LL, Walld R, Uhanova J, Bond R. Physician visits, hospitalizations, and socioeconomic status: ambulatory care sensitive conditions in a Canadian setting. Health Serv Res. 2005;40(4):1167–1185. doi: 10.1111/j.1475-6773.2005.00407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ansari Z, Laditka JN, Laditka SB. Access to health care and hospitalization for ambulatory care sensitive conditions. Med Care Res Rev. 2006;63(6):719–741. doi: 10.1177/1077558706293637. [DOI] [PubMed] [Google Scholar]
- 39.UDS Mapper. http://www.udsmapper.org/index.cfm. Accessed 9/1/2015.
- 40.New York State Department of Health. Facility race/ethnicity concordance reports. Accessed May 2015; Available at http://www.health.ny.gov/statistics/sparcs/reports/race_eth/. Accessed May 2015.
- 41.NYC DOHMH intercensal population estimates. U.S. Census Bureau. American Community Survey. 2009–2013. Data set updated February 2014, Generated November 2015.
- 42.New York State Department of Health. http://www.health.ny.gov/health_care/medicaid/redesign/dsrip/overview.htm. Accessed January 2016.