Abstract
Background:
Fibrosing mediastinitis (FM) is a rare disease. FM is thought to be related to prior granulomatous mediastinal infection, such as histoplasmosis or tuberculosis. The majority of cases have been reported in endemic regions for histoplasmosis. The characteristics of cases of FM in China, where the prevalence of tuberculosis is high, have not been reported. We analyzed the clinical, imaging, and bronchoscopic features of Chinese patients with FM to promote awareness of this disease.
Methods:
Between January 2005 and June 2015, twenty patients were diagnosed with FM in our hospital. Medical records and follow-up data were collected. Imaging and biopsy findings were reviewed by radiologists and pathologists.
Results:
A total of 20 patients were analyzed (8 males and 12 females). The age ranged from 43 to 88 years with a mean age of 69.5 years. Previous or latent tuberculosis was found in 12 cases. Clinical symptoms included dyspnea (18/20), cough (17/20), expectoration (7/20), and recurrent pneumonia (3/20). Chest computed tomography scans showed a diffuse, homogeneous, soft tissue process throughout the mediastinum and hila with compression of bronchial and pulmonary vessels. Calcification was common (15/20). Pulmonary hypertension was present in 9 of 20 cases. Diffuse black pigmentation in the bronchial mucosa was frequently seen on bronchoscopy (12/13). The patients’ response to antituberculosis treatment was inconsistent.
Conclusions:
FM in Chinese patients is most likely associated with tuberculosis. Some characteristics of FM are different from cases caused by histoplasmosis.
Keywords: Mediastinitis, Sclerosis, Tuberculosis
Introduction
Fibrosing mediastinitis (FM), also known as mediastinal fibrosis or sclerosing mediastinitis, is a rare disorder characterized by proliferation of fibrous tissue within the mediastinum.[1] Although FM is a benign disease, it is often progressive and leads to compression and occlusion of mediastinal structures. These structures include the tracheobronchial tree, esophagus, superior vena cava (SVC), and pulmonary vessels. Morbidity is directly related to the location and extent of fibrosis. The precise cause and pathogenesis of FM remain unknown. In most cases, FM is thought to be caused by an excessive host immune response to prior granulomatous mediastinal infection. The vast majority of cases are associated with the infection of Histoplasma capsulatum (H. capsulatum), a dimorphic fungus that is commonly found in the southeastern, mid-Atlantic, and central United States.[2] Other infectious agents, such as tuberculosis, aspergillosis, blastomycosis, and cryptococcosis, can also produce this condition.[3,4,5,6] Several examples of an idiopathic form of FM, perhaps due to an autoimmune process, such as Behçet's disease, retroperitoneal fibrosis, orbital pseudotumors, and Riedel's sclerosing thyroiditis, have also been described.[7,8]
Tuberculosis is considered to be another main cause of FM, especially in a nonendemic region of histoplastosis.[3] By screening the database of our hospital for 10 years, we identified twenty patients who had been diagnosed with FM. The history of prior tuberculosis infection was common among our patients. The clinical features, computed tomography (CT) manifestations, and bronchoscopic findings were reviewed and analyzed.
Methods
We recruited twenty patients who were diagnosed with FM in our hospital from January 2005 to June 2015. The clinical records and radiographic and bronchoscopic findings were reviewed. In the absence of universally accepted diagnostic criteria, the diagnosis of FM remains challenging. Chest radiographic findings frequently help to establish a diagnosis of FM. All the patients underwent a chest contrast-enhanced CT scan. The CT image was re-evaluated by two experienced chest radiologists independently. According to the proposed radiographic criteria of FM,[9,10] the diagnosis of FM was established when CT showed an infiltrative mediastinal process and associated airway, vascular, or esophageal compression. Other diseases, such as active pulmonary tuberculosis, mediastinal malignancies, and sarcoidosis, were ruled out by sputum smears, endobronchial examinations, and repeated CT examinations. Patients with a history of lung or mediastinal malignancies or prior mediastinal radiation therapy were excluded from the study. Follow-up data were obtained by a review of outpatient medical records or telephone calls to patients and their families. The study received approval from the Institutional Review Board of Peking University First Hospital (No. 2015 [980]).
Results
Clinical manifestations
A total of twenty patients (age ranged from 43 to 88 years, mean age of 69.5 years) were studied including 8 males and 12 females. Eight patients had a history of old tuberculosis, including pulmonary tuberculosis, bone tuberculosis, scrofula, intestinal tuberculosis, tuberculous pleuritis, tuberculous pericarditis, and tuberculosis of the parotid gland. None of the patients had a history of connective tissue diseases or malignant tumors, except for two patients who had surgeries for gastric cancer and kidney cancer. Thirteen patients were nonsmokers, five patients were smokers, and two patients were ex-smokers. None of them reported heavy exposure to atmospheric soot particles. The course of disease ranged from 1 month to 20 years (mean course, 5.4 years) at admission, and most of them had been misdiagnosed with chronic pulmonary disease, asthma, or chronic bronchitis. Clinical symptoms primarily manifested as dyspnea (18/20), cough (17/20), and expectoration (7/20). Fever was present in three patients accompanied by recurrent pneumonia. Constitutional symptoms, such as night sweats, fatigue, and weight loss, were not reported. Wheezing (5/20) or wet rales (3/20) was sometimes heard at a physical examination. General lymph node swelling was not palpable.
T-SPOT. TB interferon-γ release assays (Oxford Immunotec, Abingdon, UK) were performed in seven patients who denied a previous history of tuberculosis. Positive results in four patients suggested latent tuberculosis infection.[11] A small to moderate amount of bilateral (five patients) or right-sided (one patient) pleural effusion was present in six patients. Thoracentesis had been performed in three of these patients. According to Light criteria,[12] transudate in two patients and exudate in one patient were observed. Biopsy by thoracoscopy in patients with pleural exudate suggested old pleural tuberculosis.
A total of 14 patients were tested for pulmonary function. All of them showed obstructive ventilatory dysfunction, and of these, one patient was accompanied by restrictive ventilatory dysfunction. We classified the severity of airflow limitation in these patients according to the Global Initiative for Chronic Obstructive Lung Disease criteria.[13] Among the 14 patients, three had mild airflow obstruction (forced expiratory volume 1 s [FEV1] ≥80% predicted value), seven had moderate airflow obstruction (FEV1 ≥50% and <80% predicted value), two had severe airflow obstruction (FEV1 ≥30% and <50% predicted value), and two had very severe airflow obstruction (FEV1 <30% predicted value). The bronchial dilation test in all the patients was negative.
Chest computed tomography
Chest CT scans showed a diffuse, homogeneous, soft tissue process throughout the mediastinum, particularly involving the middle mediastinum and bilateral pulmonary hila, sometimes extending into pulmonary parenchyma along the bronchial vascular bundle [Figure 1a]. The fibrotic tissue had mild-to-moderate enhancement on postcontrast scans. Calcification in the mediastinum or surrounding the hilum was observed in 15 of 20 patients. Multiple stenosis and obstruction of the lobar or segmental bronchi were frequently present [Figure 1b]. Bronchial narrowing resulted from extrinsic compression with marked thickening of the bronchial walls. Segmental or subsegmental atelectasis was present in half of the patients, and pneumonia was present in three patients. Various degrees of pulmonary vessel compression were observed in all the patients. Two patients had a single compression site (right upper pulmonary artery and left pulmonary artery separately), while the other patients had bilateral multiple compression sites. Widening of the pulmonary artery trunk (≥30 mm) was observed in nine of twenty patients, in whom pulmonary arterial hypertension was demonstrated by echocardiography or right heart catheterization [Figure 2]. Enlargement of the right heart in two patients suggested cor pulmonale. Pulmonary venous compression was present in ten patients, and it was frequently accompanied by unilateral or localized interstitial pulmonary edema and pleural effusion [Figure 3]. The characteristics of FM on CT scans are shown in Table 1.
Figure 1.
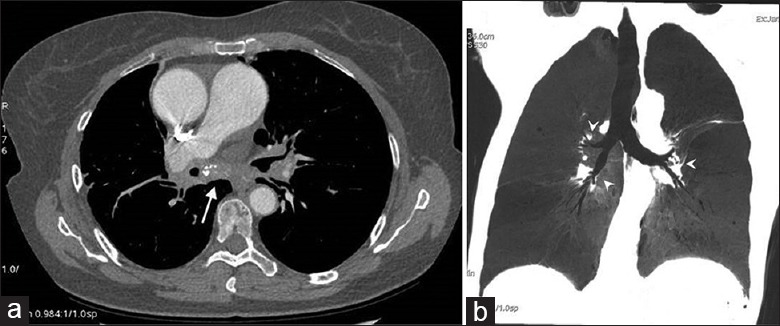
FM in a 55-year-old woman who presented with cough and dyspnea and had a history of tuberculous pleuritis 20 years ago. Contrast-enhanced CT scan (mediastinal window) shows soft tissue attenuation diffusely infiltrating the mediastinum (arrow) with punctate calcification (a). Minimum intensity project image shows multiple bronchial stenosis (arrowheads) (b). CT: Computed tomography; FM: Fibrosing mediastinitis.
Figure 2.
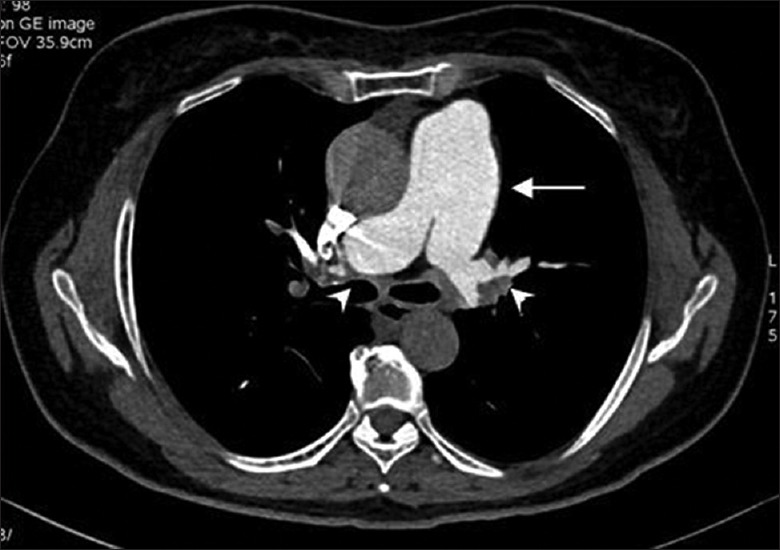
FM in a 70-year-old woman who presented with dyspnea on exertion and had a positive result of T-SPOT.TB. CT pulmonary angiogram shows widening of the pulmonary artery trunk (arrow) and compression of pulmonary arteries by surrounding soft tissue at the hila (arrowheads). CT: Computed tomography; FM: Fibrosing mediastinitis.
Figure 3.
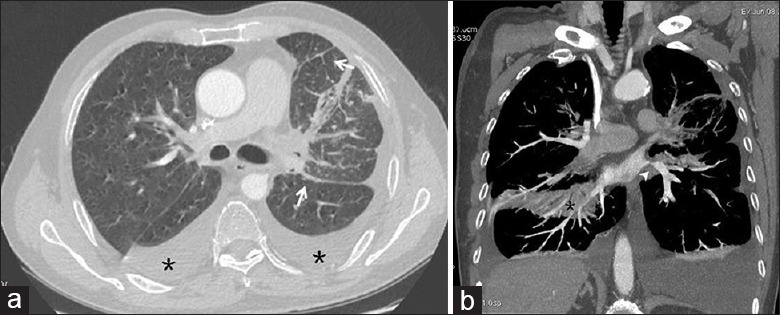
A 69-year-old male patient with FM. CT image (lung window) shows bilateral pleural effusions (asterisks) and thickening of the interlobular septa and interlobar fissures (arrows) (a). CT image (mediastinal window) shows compression of the left lower lobe vein (arrowhead) and right lower lobe partial collapse (asterisk) (b). CT: Computed tomography; FM: Fibrosing mediastinitis.
Table 1.
Characteristics of patients with fibrosing mediastinitis on computed tomography scans
| Patient number | Mediastinal mass | Bronchus | Compression of pulmonary vessels | Interstitial pulmonary edema | Pleural effusion | |||
|---|---|---|---|---|---|---|---|---|
| Diffuse/local | Calcification | Stenosis | Atelectasis | Artery | Vein | |||
| 1 | Diffuse | + | + | + | + | + | + | + |
| 2 | Diffuse | + | + | + | + | + | − | − |
| 3 | Diffuse | − | + | + | + | + | + | + |
| 4 | Diffuse | + | + | − | + | − | − | − |
| 5 | Diffuse | + | + | − | + | − | − | − |
| 6 | Diffuse | + | + | + | + | − | − | − |
| 7 | Diffuse | + | + | − | + | + | + | − |
| 8 | Diffuse | + | + | + | + | − | − | − |
| 9 | Diffuse | + | + | + | + | + | − | − |
| 10 | Local | − | + | − | + | − | − | − |
| 11 | Diffuse | − | + | − | + | + | − | + |
| 12 | Diffuse | + | + | − | + | + | + | + |
| 13 | Diffuse | + | + | + | + | − | − | − |
| 14 | Diffuse | + | + | + | + | + | − | + |
| 15 | Diffuse | − | + | − | + | + | + | + |
| 16 | Diffuse | + | + | + | + | − | − | − |
| 17 | Diffuse | − | + | − | + | − | − | − |
| 18 | Diffuse | + | + | − | + | − | − | − |
| 19 | Diffuse | + | + | − | + | − | − | − |
| 20 | Diffuse | + | + | + | + | + | + | − |
+: existent; − : nonexistent.
Electronic bronchoscopy
Among the twenty patients, 13 undertook bronchoscopy. An examination showed diffused swelling of bronchial mucosa and multiple bronchial distortion and stenosis. Diffuse black pigmentation in the bronchial mucosa was found in almost all patients (12/13) [Figure 4]. In addition, lesions of the bronchial mucosa bled easily during bronchoscopic biopsy. Neither acid-fast bacilli nor fungi were detected in protected specimen brush samples, bronchial washings, bronchoalveolar lavage fluid, and biopsy samples. All the cultures of bronchoscopic samples were sterile. Histological or cytological examinations of biopsy samples from bronchial mucosa, transbronchial lung biopsy, and endobronchial ultrasound-guided transbronchial needle aspiration biopsy of mediastinal masses were performed by experienced pathologists. There was no evidence of malignancy or other benign disorders, such as sarcoidosis. Granuloma was present in one patient, but special stains did not show evidence of tuberculosis or fungi.
Figure 4.
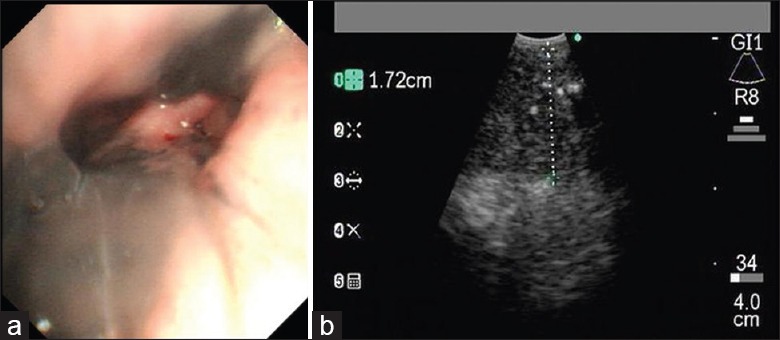
A 57-year-old male patient with FM. A bronchoscopic image shows mucosal pigmentation in the bronchus intermedius of the right lung with obvious narrowing of the bronchus intermedius (a). Endobronchial ultrasound shows a mediastinal heteroechoic mass at the subcarinal region (b). FM: Fibrosing mediastinitis.
Treatment and follow-up
Nine patients were treated with antituberculosis drugs. One patient with wheezing and severe obstructive ventilatory dysfunction was administered prednisone 40 mg/d for 1 month. For the remaining ten patients, inhaled bronchial dilators with or without inhaled steroids, cough suppressants, and expectorants were administrated to relieve symptoms. Antibiotics were used to treat pneumonia. Clinical follow-up was available in 18 of the 20 patients, ranging from 2 months to 5 years (mean follow-up duration, 18.9 months). Three of the nine patients who were treated with antituberculosis drugs reported obvious relief of the symptoms, but they did not accept repeated CT examinations. The rest of the patients had no clinical improvement after antituberculosis treatment. One patient had no response to 40 mg of prednisone and died of respiratory failure and major hemoptysis several months later. The remaining seven patients without specific treatment were clinically stable, but one patient had a worsening course. Follow-up of longer than 1 year was available in 12 patients. Eight patients had undergone repeated CT examinations, and four of them presented with radiographic progression. However, none of these patients reported major exacerbation of symptoms, partly due to the slow and slight progression. Clinical features, treatment, and follow-up outcomes are shown in Table 2.
Table 2.
Clinical features and treatment outcomes of patients with fibrosing mediastinitis
| Patient number | Age (years) | Gender | Symptoms | Tuberculosis | Airway flow obstruction | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 81 | Male | Dyspnea, cough, expectoration | No | – | Bronchial dilator | Radiographic progression |
| 2 | 55 | Female | Dyspnea, cough, expectoration | Tuberculous pleuritis | Severe | Antituberculosis | No improvement |
| 3 | 69 | Male | Dyspnea | Pulmonary tuberculosis | Moderate | Bronchial dilator | Radiographic progression |
| 4 | 70 | Female | Dyspnea, cough | T-SPOT.TB (+) | Mild | Antituberculosis | No improvement |
| 5 | 71 | Male | Dyspnea | Pulmonary tuberculosis | – | Antituberculosis | No improvement |
| 6 | 86 | Female | Dyspnea | No | – | Bronchial dilator | Stable |
| 7 | 73 | Female | Dyspnea, cough, expectoration | No | Moderate | Antituberculosis | Improvement |
| 8 | 87 | Male | Cough, expectoration | No | – | Expectorant | Stable |
| 9 | 66 | Female | Dyspnea, cough | No | Moderate | Cough suppressant | Stable |
| 10 | 70 | Female | Dyspnea, cough | T-SPOT.TB (+) | Moderate | Antituberculosis | Improvement |
| 11 | 88 | Male | Dyspnea, cough, fever | No | Very severe | Bronchial dilator, antibiotics | – |
| 12 | 77 | Female | Dyspnea, cough, expectoration, fever | Scrofula | Moderate | Bronchial dilator, antibiotics | Stable |
| 13 | 57 | Male | Dyspnea, cough | T-SPOT.TB (+) | Severe | Bronchial dilator | Radiographic progression |
| 14 | 73 | Male | Dyspnea, cough | Bone tuberculosis | Moderate | Antituberculosis | No improvement |
| 15 | 80 | Male | Cough, dyspnea | T-SPOT.TB (+) | Mild | Antituberculosis | No improvement |
| 16 | 55 | Female | Dyspnea, cough, expectoration | Tuberculosis of the parotid gland | Mild | Antituberculosis | Improvement |
| 17 | 43 | Female | Dyspnea, cough | No | Very severe | Prednisone | Died |
| 18 | 50 | Female | Dyspnea, cough | Tuberculous pericarditis | – | Cough suppressant | – |
| 19 | 66 | Female | Fever, cough, expectoration | No | – | Antibiotics | Improvement |
| 20 | 72 | Female | Dyspnea, cough | Intestinal tuberculosis | Moderate | Antituberculosis | Radiographic progression |
Discussion
FM is a rare, benign, but often progressive and potentially lethal disorder, characterized by proliferation of dense fibrous tissue within the mediastinum. The majority of case series has been reported by the Mayo Clinic[2,14,15,16,17,18] and other American hospitals,[10,19,20] in which most patients resided in endemic areas for H. capsulatum. Serology for histoplasmosis is positive in one third or less in most series. H. capsulatum organisms are sometimes identified in histopathological specimens. Therefore, many cases in the United States have been linked to H. capsulatum infection. However, the precise cause and pathogenesis of FM remains elusive.
According to previous studies, patients with FM are typically young at presentation and present with cough, dyspnea, recurrent pulmonary infection, hemoptysis, and pleuritic chest pain.[2,18,20] FM typically manifests on CT scans as an infiltrative mass of soft tissue attenuation that obliterates normal mediastinal fat planes and encases or invades adjacent structures. The histopathological findings include extensive paucicellular fibrous tissue infiltrating and obliterating adipose tissue with or without patchy infiltration of mononuclear cells in the absence of malignancy.[2] In the appropriate clinical setting, characteristic imaging findings may suffice for diagnosis, and sampling is generally not required to establish a diagnosis of FM.
However, the cases in our study were not related to H. capsulatum infection because histoplasmosis is rare in the mainland of China. We found several differences between our patients and those in previous studies.[2,14,15,16,17,18,19,20] First, our patients were older at presentation than those in previous reports. The mean age of our patients was 69.5 years. They usually presented with dyspnea, cough, expectoration, and recurrent pneumonia. Notably, more than half of our patients had a previous history of tuberculosis or a positive result of the T-SPOT.TB test. Second, diffuse soft tissue attenuation with calcification in the mediastinum is a typical feature on CT scans. According to previous studies, there are two distinct patterns of FM on CT scans.[1] In a relatively large radiological series,[17] Sherrick et al. observed that 82% of affected patients had a localized mediastinal mass and only 18% of patients had diffuse infiltration. However, in our study, only one patient had a local mass at the left hilum. Diffuse infiltration is the predominant pattern, which is frequently accompanied by calcification. In the United States, FM is the most common benign cause of obstruction of the SVC.[21] Obstruction or narrowing of the SVC was reported in approximately 40% of patients of FM.[2,17] However, none of the patients in our study presented with compression of the SVC. Compression and narrowing of the pulmonary arteries (100%) and pulmonary veins (50%) were more common in our study than in a previous study (42% and 13%, respectively).[2]
Bronchoscopic findings of FM have seldom been described in the literature. Manali et al. described endoscopic manifestations in three patients with FM, most likely related to histoplasmosis.[22] They presented with tracheobronchial concentric narrowing with severe hyperemia and mucosal edema. In our study, endoscopic manifestations were characterized by diffuse black pigmentation of the bronchial mucosa, mucosal edema, bronchial distortion, and bronchial stenosis. This bronchial black pigmentation has seldom been described in cases of FM linked to histoplasmosis. A relationship between dark anthracotic pigmentation in the bronchial mucosa and tuberculosis has been demonstrated.[23,24,25] Therefore, markedly bronchial pigmentation that was observed in our study is consistent with the hypothesis that FM in Chinese patients is associated with tuberculosis.
Treatment of FM is particularly challenging. Most of the available data on treatment of FM are based either on case reports or small case series. There have been few prospective, randomized, controlled trials conducted to date. Although limited data suggest that antifungal therapy might stabilize disease progression or lead to limited symptomatic improvement,[19,26] no convincing evidence has been shown. Similar to the uncertain effectiveness of antifungal therapy in previous studies,[2] patients’ responses to antituberculosis therapy were inconsistent in our study. Glucocorticoids also did not appear to be beneficial, which is consistent with the previous reports.[2,15,16,20] In contrast to previous studies[2] in which balloon dilation, intravascular or endobronchial stent placement, and surgical intervention were usually performed to relieve stenosis of bronchi or vessels, none of our patients undertook these interventions. The reason for not undertaking these interventions is because of diffuse involvement of lobar and/or segmental bronchial and pulmonary vessels.
The current study is limited by its retrospective design, small sample size, and incomplete long-term follow-up information. Therefore, we do not precisely know the progression of FM in Chinese patients who are assumed to be associated with tuberculosis and cannot verify the effectiveness of antituberculosis therapy. Further study is necessary including more cases.
In summary, FM is an uncommon disease and its diagnosis can be established mainly using characteristic manifestations on contrast-enhanced CT scans. Based on the analysis of current studies, there are some differences between the cases of FM in China where tuberculosis is prevalent and cases in the United States where histoplasmosis is endemic. Chinese patients with FM are older at presentation than patients in other countries. Diffuse, infiltrative, soft tissue density that obliterates normal mediastinal fat planes and leads to multiple compression of bronchi and/or pulmonary vessels, with calcification within the lesion, is the most common pattern. Black pigmentation in the bronchial mucosa is frequently found on bronchoscopy. However, the clinical prognosis of FM in Chinese patients, the link to tuberculosis, and the effectiveness of antituberculosis treatment need to be determined by further large-scale studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yuan-Yuan Ji
References
- 1.Rossi SE, McAdams HP, Rosado-de-Christenson ML, Franks TJ, Galvin JR. Fibrosing mediastinitis. Radiographics. 2001;21:737–57. doi: 10.1148/radiographics.21.3.g01ma17737. doi: 10.1148/radiographics. 21.3.g01ma17737. [DOI] [PubMed] [Google Scholar]
- 2.Peikert T, Colby TV, Midthun DE, Pairolero PC, Edell ES, Schroeder DR, et al. Fibrosing mediastinitis: Clinical presentation, therapeutic outcomes, and adaptive immune response. Medicine (Baltimore) 2011;90:412–23. doi: 10.1097/MD.0b013e318237c8e6. doi: 10.1097/MD.0b013e318237c8e6. [DOI] [PubMed] [Google Scholar]
- 3.Fijolek J, Wiatr E, Blasinska-Przerwa K, Roszkowski-Sliz K. Fibrosing mediastinitis as an untypical complication of tuberculosis: Case report. Pol Arch Med Wewn. 2009;119:752–5. [PubMed] [Google Scholar]
- 4.Chatterjee D, Bal A, Singhal M, Vijayvergiya R, Das A. Fibrosing mediastinitis due to Aspergillus with dominant cardiac involvement: Report of two autopsy cases with review of literature. Cardiovasc Pathol. 2014;23:354–7. doi: 10.1016/j.carpath.2014.05.005. doi: 10.1016/j.carpath2014.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Lagerstrom CF, Mitchell HG, Graham BS, Hammon JW., Jr Chronic fibrosing mediastinitis and superior vena caval obstruction from blastomycosis. Ann Thorac Surg. 1992;54:764–5. doi: 10.1016/0003-4975(92)91025-5. doi: 10.1016/0003-4975(92)91025-5. [DOI] [PubMed] [Google Scholar]
- 6.Mole TM, Glover J, Sheppard MN. Sclerosing mediastinitis: A report on 18 cases. Thorax. 1995;50:280–3. doi: 10.1136/thx.50.3.280. doi: 10.1136/thx.50.3.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanne JP, Mohammed TL. Fibrosing mediastinitis associated with Behçet's disease: CT findings. Clin Radiol. 2007;62:1124–6. doi: 10.1016/j.crad.2007.07.007. doi: 10.1016/j.crad2007.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Bahler C, Hammoud Z, Sundaram C. Mediastinal fibrosis in a patient with idiopathic retroperitoneal fibrosis. Interact Cardiovasc Thorac Surg. 2008;7:336–8. doi: 10.1510/icvts.2007.166033. doi: 10.1510/icvts2007.166033. [DOI] [PubMed] [Google Scholar]
- 9.Goodwin RA, Nickell JA, Des Prez RM. Mediastinal fibrosis complicating healed primary histoplasmosis and tuberculosis. Medicine (Baltimore) 1972;51:227–46. doi: 10.1097/00005792-197205000-00008. doi: 10.1097/00005792-197205000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Loyd JE, Tillman BF, Atkinson JB, Des Prez RM. Mediastinal fibrosis complicating histoplasmosis. Medicine (Baltimore) 1988;67:295–310. doi: 10.1097/00005792-198809000-00002. doi: 10.1097/00005792-198809000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Zhang LF, Liu XQ, Zhang Y, Deng GH, Pareek M, Lalvani A. A prospective longitudinal study evaluating a T-cell-based assay for latent tuberculosis infection in health-care workers in a general hospital in Beijing. Chin Med J. 2013;126:2039–44. doi: 10.3760/cma.j.issn.0366-6999.20130355. [PubMed] [Google Scholar]
- 12.Light RW. The light criteria: The beginning and why they are useful 40 years later. Clin Chest Med. 2013;34:21–6. doi: 10.1016/j.ccm.2012.11.006. doi: 10.1016/j.ccm.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65. doi: 10.1164/rccm.201204-0596PP. doi: 10.1164/rccm. 201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 14.Kunkel WM., Jr Clagett OT, Mcdonald JR. Mediastinal granulomas. J Thorac Surg. 1954;27:565–74. [PubMed] [Google Scholar]
- 15.Strimlan CV, Dines DE, Payne WS. Mediastinal granuloma. Mayo Clin Proc. 1975;50:702–5. [PubMed] [Google Scholar]
- 16.Dines DE, Payne WS, Bernatz PE, Pairolero PC. Mediastinal granuloma and fibrosing mediastinitis. Chest. 1979;75:320–4. doi: 10.1378/chest.75.3.320. doi: 10.1378/chest.75.3.320. [DOI] [PubMed] [Google Scholar]
- 17.Sherrick AD, Brown LR, Harms GF, Myers JL. The radiographic findings of fibrosing mediastinitis. Chest. 1994;106:484–9. doi: 10.1378/chest.106.2.484. doi: 10.1378/chest.106.2.484. [DOI] [PubMed] [Google Scholar]
- 18.Parish JM, Rosenow EC., 3rd Mediastinal granuloma and mediastinal fibrosis. Semin Respir Crit Care Med. 2002;23:135–43. doi: 10.1055/s-2002-25302. doi: 10.1055/s-2002-25302. [DOI] [PubMed] [Google Scholar]
- 19.Urschel HC, Jr, Razzuk MA, Netto GJ, Disiere J, Chung SY. Sclerosing mediastinitis: Improved management with histoplasmosis titer and ketoconazole. Ann Thorac Surg. 1990;50:215–21. doi: 10.1016/0003-4975(90)90737-q. [DOI] [PubMed] [Google Scholar]
- 20.Mathisen DJ, Grillo HC. Clinical manifestation of mediastinal fibrosis and histoplasmosis. Ann Thorac Surg. 1992;54:1053–7. doi: 10.1016/0003-4975(92)90069-g. doi: 10.1016/0003-4975(92)90069-G. [DOI] [PubMed] [Google Scholar]
- 21.Parish JM, Marschke RF, Jr, Dines DE, Lee RE. Etiologic considerations in superior vena cava syndrome. Mayo Clin Proc. 1981;56:407–13. [PubMed] [Google Scholar]
- 22.Manali ED, Saad CP, Krizmanich G, Mehta AC. Endobronchial findings of fibrosing mediastinitis. Respir Care. 2003;48:1038–42. [PubMed] [Google Scholar]
- 23.Mirsadraee M, Saffari A, Sarafraz Yazdi M, Meshkat M. Frequency of tuberculosis in anthracosis of the lung: A systematic review. Arch Iran Med. 2013;16:661–4. doi: 0131611/AIM.0010. [PubMed] [Google Scholar]
- 24.Kim HJ, Kim SD, Shin DW, Bae SH, Kim AL, Kim JN, et al. Relationship between bronchial anthracofibrosis and endobronchial tuberculosis. Korean J Intern Med. 2013;28:330–8. doi: 10.3904/kjim.2013.28.3.330. doi: 10.3904/kjim.2013.28.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Han FF, Yang TY, Song L, Zhang Y, Li HM, Guan WB, et al. Clinical and pathological features and imaging manifestations of bronchial anthracofibrosis: The findings in 15 patients. Chin Med J. 2013;126:2641–6. doi: 10.3760/cma.j.issn.0366-6999.20121895. [PubMed] [Google Scholar]
- 26.Maholtz MS, Dauber JH, Yousem SA. Case report: Fluconazole therapy in histoplasma mediastinal granuloma. Am J Med Sci. 1994;307:274–7. doi: 10.1097/00000441-199404000-00006. [DOI] [PubMed] [Google Scholar]


