Abstract
Introduction
The standards for the management of open fractures of the lower limb published by the British Association of Plastic, Reconstructive and Aesthetic surgeons (BAPRAS) and British Orthopaedic Association (BOA) were introduced to improve the treatment received by patients after open injury to the lower limb. These Standards were released after BAPRAS/BOA published Guidelines for the management of open tibial fractures.
Methods
We wished to determine the impact of these Standards upon the surgical management of open tibial fractures by comparing patients admitted to an orthoplastic centre in the 45 months concluding December 2009 (the Guidelines era) with those admitted during 2011 (the Standards era). Surgical procedures required during the first 30 days and 12 months after injury were determined. Cases were divided into ‘directly admitted patients’ (DAP) and ‘transferred patients’ (TP). Standards-era patients were divided further into those who had surgery exclusively at the orthoplastic centre (orthoplastic patients (OPP)) and those transferred after surgery (TASP).
Results
The number of TP trebled in frequency in the Standards era, 25% of whom were transferred before surgery. Significantly fewer surgical procedures were required for DAP and OPP groups compared with TP (and TASP) groups in both eras (Mann–Whitney U-test, p=0.05). DAP and OPP groups during the Standards era underwent the fewest procedures, with the vast majority of cases treated with two or fewer procedures in the first 12 months (88% and 80%, respectively, compared with 61% in the Guidelines era). In the Guidelines era, 44% of TP cases and in the Standards era 39% of TP and 29% of TASP groups underwent two or fewer procedures.
Approximately two-thirds of open tibial fractures managed in our orthoplastic centre were patients transferred after surgery. The greatest impact of the Standards was evident for those who underwent surgery exclusively in the orthoplastic centre, reflecting a more deliberate combined strategy.
Conclusion
These findings vindicate the Standards as well as mandating reorganisation and resourcing of orthoplastic services to ensure immediate transfer and early combined surgery. By increasing the capacity to deal with time-dependent initial surgery, the surgical burden that the patient must endure, and which the service must provide, are reduced.
Keywords: Open fracture, Open tibial fracture, Orthoplastic, Hot transfer
In 1997, the British Association of Plastic, Reconstructive and Aesthetic surgeons (BAPRAS) and British Orthopaedic Association (BOA) published Guidelines for the management of open tibial fractures.1 These Guidelines made several recommendations regarding the logistical and surgical management of open tibial fractures, but implementation was variable and associated with difficulties, and their impact unclear.2,3 Principal among these difficulties was the influence of geographical constraints on the feasibility of undertaking the initial surgical debridement in an orthoplastic specialist unit <6 hours of injury.
In 2009, these guidelines were superseded by The standards for the management of open fractures of the lower limb, again produced by BAPRAS/BOA.4 This document clearly defined the management of open injuries to the lower limb in a stepwise fashion, from emergency treatment offered at the roadside to complex, late reconstructive options. Literature regarding optimal management was considered for each recommendation and justifications made.
To combat the difficulties encountered previously in the timing and location of primary debridement, the Standards state that patients should be cared for by a recognised orthoplastic service. A framework is established for initial debridement and definitive reconstructive surgery, and proposes that the same orthoplastic team should undertake the two procedures. To facilitate transfer from the site of injury and initial assessment by the orthoplastic service, the limit for primary debridement was extended from 6 hours to 24 hours post-injury. This decision was based on the prevalence of union and infection of bone, with varying times to initial debridement.3,5 Consequently, there has been a ‘paradigm shift’ from emergency initial surgery to urgent transfer to an orthoplastic service.
A study of open fractures of the ankle demonstrated that patients endure a greater surgical burden if operative treatment is undertaken before transfer to an orthoplastic centre. Such patients require at least one more procedure compared with patients who were cared for entirely by an orthoplastic service.6 A study of grade-IIIB open tibial fractures seems to support these findings, with nearly half of similarly transferred patients requiring revision of initial skeletal fixation.3
Early treatment by an orthoplastic service is now considered the standard of care for open fractures of the lower limb. However, there is little evidence regarding the surgical burden that these patients experience extending beyond their initial admission to hospital and care. Equally, the changing workload at the orthoplastic centre is incompletely understood.
The aim of the present study was to review changes in orthoplastic activity and surgical burden borne by patients with open tibial fractures managed in Guidelines and Standards eras.
Methods
Since April 2006, data from all open fractures of the lower limb treated by orthopaedic and plastic-surgical teams at Morriston Hospital (Swansea, UK) have been collected prospectively for audit. Data include demographics of each patient and his/her injury as well as details regarding surgical procedures undertaken within Morriston Hospital and initial referring centre. Patient details were recorded upon hospital admission and throughout treatment. These details were cross-referenced with operating-theatre records, operative notes, clinical records, and the digital radiology system.
Patients were divided into two groups based upon date of injury. Patients injured between the start of data collection in October 2006 and December 2009 were deemed to have been cared for in the Guidelines era. Cases treated between January 2011 and December 2011 constituted the Standards-era group. Patients treated during 2010 (immediately after publication of the Standards) were excluded from analyses. This time period was deemed to represent changing practices within the department and surrounding region.
Patients were subdivided further into those admitted directly through the Emergency Department of Morriston Hospital and subsequently admitted for their treatment (‘directly admitted patients’ (DAP)) and those assessed and treated initially in a peripheral hospital and transferred for definitive surgery at a later date (‘transferred patients’ (TP)).
Then, the cohort from the Standards era was divided again into those who underwent surgery exclusively in the orthoplastic centre. They comprised the DAP group plus those transferred acutely from the initial hospital before surgery (sometimes referred to as ‘hot transfers’). These patients were classified as ‘orthoplastic patients’ (OPP). The remainder of the TP group for the Standards era were referred to as ‘transferred after surgery patients’ (TASP).
The database was interrogated for information on patient demographics, fracture pattern, Gustilo–Anderson classification, and surgery related to the open fracture.7,8 Surgical procedures undertaken for other injuries were recorded but not included in analyses. All information was cross-referenced with retrospective review of clinical notes, operating-department records and the digital radiology system to ensure accuracy and completeness. All surgical interventions within the first 30 days and 12 months after injury were recorded. Data relating to duration of hospital stay and out- patient follow-up were not collated because these parameters have been analysed separately as part of a detailed study examining health-service utilisation by subjects with open tibial fractures.15
Differences between Guidelines- and Standards-era groups were assessed by non-parametric statistical analyses using Quickstat Biomedical (Arcus Global, Cambridge, UK).
Results
A total of 163 open injuries of the lower limb were treated during the Guidelines era (April 2006 to December 2009) and represented a mean of 3.6 open injuries of the lower limb per month. There were 63 open tibial fractures, with complete data regarding surgical burden available for 60 of these fractures. In the Standards era, there were 63 open injuries to the lower limb in the 12 months from January 2011 to December 2011 inclusive, and represented a mean of 5.2 cases per month. Of these, 35 were open tibial fractures. These data are summarised in Table 1 along with the Gustilo–Anderson classification for the respective groups. Thus, there was a mean of 1.4 open tibial fractures per month in the Guidelines era compared with a mean of 3 per month in the Standards era. There was no significant difference between Guidelines and Standards eras with regard to distribution of age or sex or between patient groups.
Table 1.
Total number of open tibial fracture cases and Gustilo–Anderson grade in each era (mean number of cases per month are in parentheses)
|
Guidelines era
(2006–2009) |
Standards era
(2011) |
|
| DAP | 28 (0.6) | 8 (0.7) |
| TP | 35 (0.8) | 27 (2.3) |
| Total | 63 (1.4) | 35 (3) |
| II | 1 (2%) | 7 (20%) |
| IIIA | 6 (9%) | 9 (23%) |
| IIIB | 52 (88%) | 15 (49%) |
| IIIC | 1 (2%) | 4 (9%) |
In the Standards era, the TP group accounted for 27/35 (77%) patients, vs 35/63 (55%) in the Guidelines era. Gustilo-Anderson type-IIIB injuries were the most common type of open fracture, with 80% of Guidelines-era cases ascribed this classification compared with 49% of Standards-era injuries (Table 1). Tibial shaft fractures (AO Foundation and Orthopaedic Trauma Association type-42 injuries) were the most common fracture pattern, accounting for 61% and 74% of injuries in Guidelines and Standards eras, respectively (Table 2). Two transferred patients in the Standards-era group required fasciotomy for compartment syndrome, one before transfer and the other after. Both of these cases had a ‘floating knee’. The latter case in the OPP group was treated initially by acute shortening in a circular frame, thereby allowing primary closure of a type-IIIB injury.
Table 2.
AO Foundation/Orthopaedic Trauma Association classification and method of definitive fracture fixation for given Gustilo–Anderson grades of fracture
| AO/OTA classification | Mode of definitive fixation | |||||||
| 41 | 42 | 43 | IMN | ORIF | Circular frame | Monolateral frame | ||
| Guidelines era | II | 4 | 0 | 1 | 1 | 0 | 0 | 0 |
| IIIA | 1 | 3 | 2 | 3 | 1 | 1 | 1 | |
| IIIB | 4 | 36 | 14 | 27 | 8 | 7 | 10 | |
| IIIC | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Standards era | II | 0 | 5 | 1 | 6 | 0 | 1 | 0 |
| IIIA | 1 | 6 | 1 | 6 | 1 | 0 | 1 | |
| IIIB | 0 | 14 | 2 | 10 | 1 | 5 | 0 | |
| IIIC | 1 | 1 | 2 | 0 | 0 | 0 | 1 | |
| Percentage of cases | Guidelines era | 16 | 62 | 27 | 49 | 14 | 13 | 17 |
| Standards era | 6 | 74 | 17 | 63 | 6 | 17 | 6 | |
Intramedullary nailing (IMN) was the most commonly used definitive mode of fracture fixation (49% and 63% of cases in Guidelines and Standards eras respectively) when reviewed 12 months after injury. Monolateral external fixation declined from 17% to 6% as a definitive mode of fixation. However, use of circular frames remained more consistent, with 13% and 17% of cases treated in this fashion in Guidelines and Standards eras.
Definitive management of soft tissue 12 months post-injury also showed differences between groups (Table 3). Direct closure (immediate or delayed primary) was achieved in 26% of Standards-era cases compared with 5% previously. Split-skin grafting (SSG) was the means of soft-tissue cover in 38% of Guidelines-era cases, including 21/54 (39%) patients whose injuries were classified as Gustilo–Anderson type IIIB. Amputation was required in three cases (5%) in the Guidelines era, two of which were carried out for type-IIIB injuries and one for the sole type-IIIC injury. There were three type-IIIC injuries in the Standards era, one of which was reconstructed and two of which were amputated. A further amputation was required for one type-IIIB injury in which free tissue transfer failed, giving a prevalence of amputation of 9%.
Table 3.
Method of definitive soft-tissue cover for given Gustilo–Anderson grades of fracture
| Closed | SSG | Local muscle | Fascio-cutaneous | Free tissue transfer | Amputation | ||
| Guidelines era | II | 1 | 0 | 0 | 0 | 0 | 0 |
| IIIA | 2 | 3 | 0 | 1 | 0 | 0 | |
| IIIB | 0 | 21 | 12 | 14 | 7 | 2 | |
| IIIC | 0 | 0 | 0 | 0 | 0 | 1 | |
| Standards era | II | 5 | 0 | 1 | 1 | 0 | 0 |
| IIIA | 3 | 4 | 1 | 0 | 0 | 0 | |
| IIIB | 1 | 0 | 6 | 4 | 5 | 1 | |
| IIIC | 0 | 0 | 1 | 0 | 0 | 2 | |
| Percentage of cases | Guidelines era | 5 | 38 | 19 | 24 | 11 | 5 |
| Standards era | 26 | 11 | 26 | 14 | 14 | 9 |
The Standards-era DAP group required significantly fewer operations at 30 days and 12 months compared with the corresponding TP group (Mann–Whitney U-test (two sided), p=0.02 and p=0.05, respectively; Figure 1 and 3). Similarly, they also required significantly fewer operations at 30 days than the Guidelines-era DAP group (Mann–Whitney U-test (two sided), p=0.04).
Figure 1.
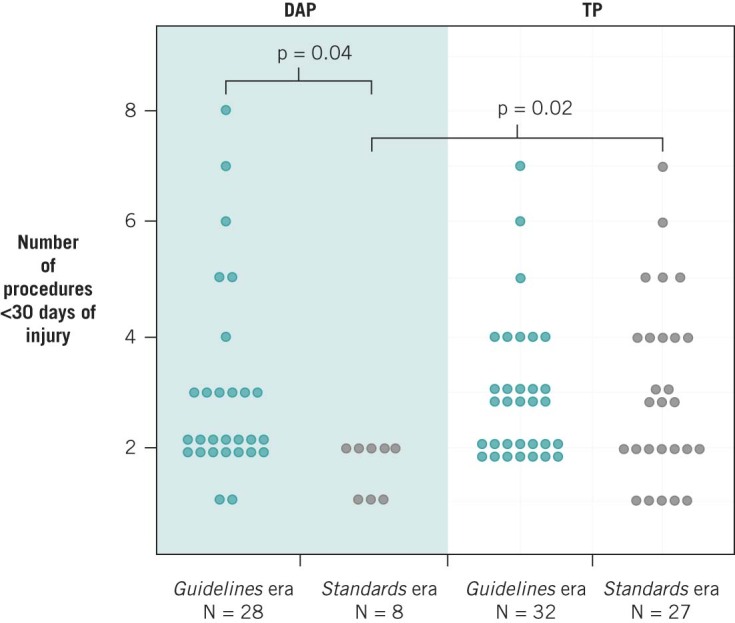
Operations within the first 30 days following injury comparing Directly Admitted and Transferred Patients between the Guide Lines & Standards Eras. P values – Mann-Whitney U test (Two sided).
Figure 3.
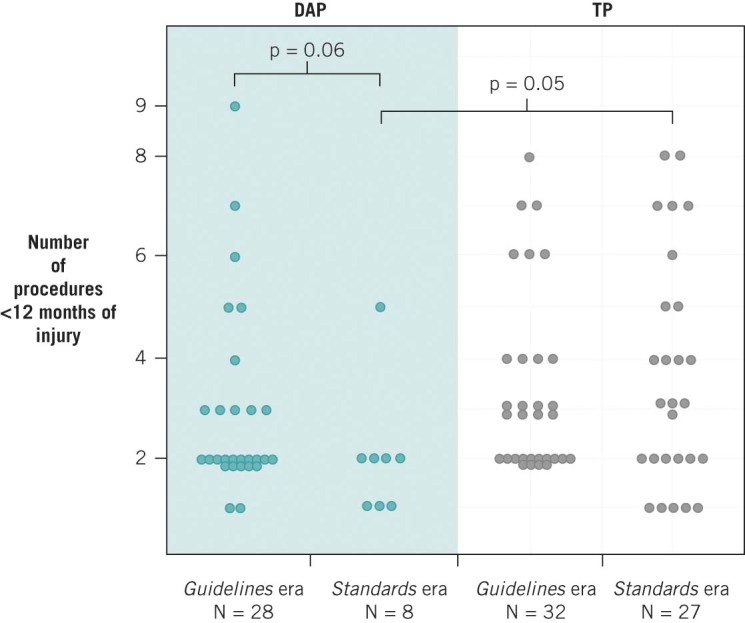
Operations within the first year following injury comparing Directly Admitted and Transferred Patients between the Guide Lines & Standards Eras. P values – Mann-Whitney U test (Two sided).
The OPP group required significantly fewer operations at 30 days and 12 months compared with the TASP and Guidelines DAP group (Mann–Whitney U-test OPP vs TASP (two sided), p=0.0042 and p=0.0098 and OPP vs DAP p=0.036 and p=0.04, respectively; Figures 2 and 4).
Figure 2.
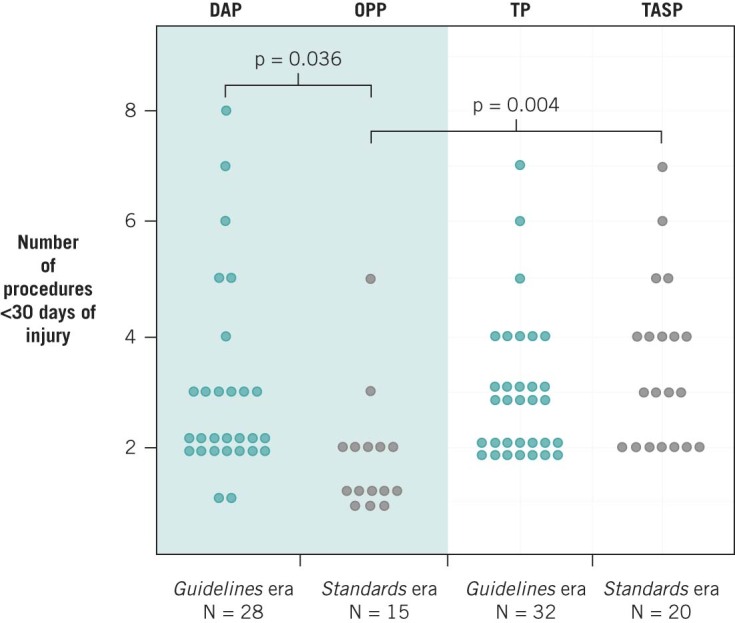
Operations within the first 30 days following injury comparing Ortho-Plastic and Transferred After Surgery Patient groups. P values – Mann-Whitney U test (Two sided).
Figure 4.
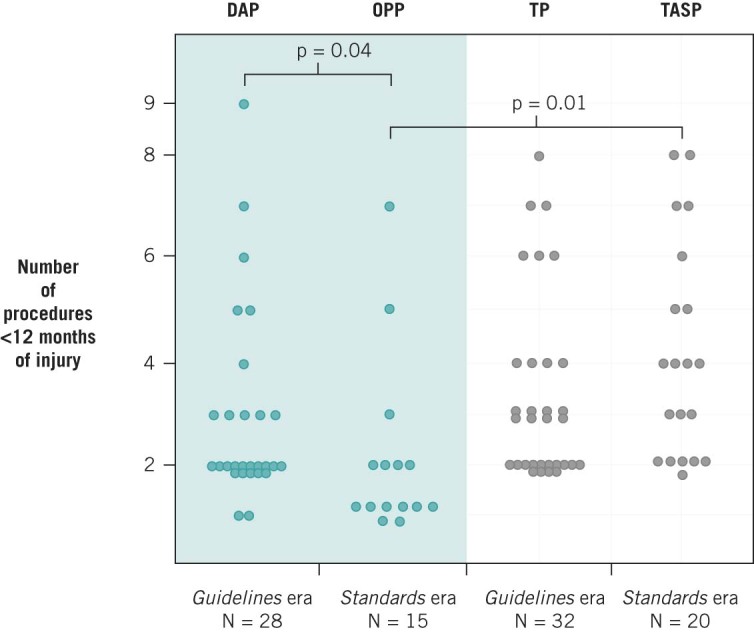
Operations within the first year following injury comparing Ortho-Plastic and Transferred After Surgery Patient groups. P values – Mann-Whitney U test (Two sided).
Most DAP and OPP cases in the Standards era were treated with two or fewer procedures (88% and 80%, respectively). This parameter was significant compared with TP, TASP and DAP groups in Guidelines-era patients (Standards DAP vs TP, Fisher’s exact test (two sided by summation), p=0.04; OPP vs TASP, Yates-corrected χ²=8.259822, p=0.0041; OPP vs Guidelines DAP, Yates-corrected χ²= 5.217927, p=0.0224; Table 4).
Table 4.
Percentage of patients managed successfully with 1 or 2 operations within 12 months of injury
| Guidelines (2006–2009) | Standards (2011) | |
| DAP | 61% | 88% |
| TP | 41% | 39% |
| OPP | 80% | |
| TASP | 29% |
In total, the TASP group required one additional procedure compared with the total number of procedures required by the DAP and OPP groups combined. When accounting for procedures carried out elsewhere, the mean number of procedures undertaken within the orthoplastic unit was 2.45 for DAP and OPP groups combined, and 2.46 for the TASP group, regardless of how many procedures had been carried out at the admitting centre (mean number of procedures before transfer = 1.23). For a small (but significant) proportion of patients, such surgery may be vital (eg if re-vascularisation of compartment decompression is required). It appears that the surgical burden for the orthoplastic unit was constant between the two groups (TASP vs DAP and OPP combined) but the burden was increased in patients who underwent surgery before transfer. Whether this is phenomenon was due solely to factors related to injury and surgical debridement, or the result of the orthoplastic team requiring more detailed assessment of wounds after transfer, is not clear.
Discussion
Since the publication of the BOA/BAPRAS Standards, the mean number of cases of open fractures of the lower limb managed at Morriston Hospital (an orthoplastic centre) has increased, thereby trebling the number of open tibial fractures transferred into the unit.4 One of the principal aims of the Standards was to improve the consistency of care provided to this group of patients. Experience has shown that adherence to previously published guidance is inconsistent, with a higher prevalence of revisions of fracture fixation and wound-healing problems encountered in patients who undergo surgery before transfer for orthoplastic input.3,9 Thoroughness of debridement, rather than performance within a 6-hour window from injury, has increasingly been recognised as being paramount.
With the notable exceptions of gross contamination (with marine, farmyard or sewage material), compartment syndrome, or vascular injury requiring repair, hot transfer to an orthoplastic unit before surgery is now recommended.4 Development of combined surgical teams was posited by Godina, and has been implemented worldwide.10–13 In England, initiation of ‘trauma networks’ has changed patterns of referral/transfer in response to designation of trauma centres, with workloads increasing correspondingly.14 The orthoplastic unit within the Morriston Hospital does not function in an established trauma network but has a long-established tertiary referral role as a trauma unit with specialist services. Publication of the Standards has reshaped practice in a manner that demands considerable re-organisation.
In 2011, only six hot transfers were achieved out of 24 potential patients. Of the remaining TP-group patients, two required vascular reconstruction of grade-IIIC injuries, and another underwent fasciotomy and provisional debridement for acute compartment syndrome. The latter patient was transferred and underwent definitive orthoplastic reconstruction within 24 hours of the original injury, with IMN of tibial and femoral fractures as well as local coverage of the muscle flap in the open tibial fracture. The remaining 75% of the TP group may have benefited from earlier transfer in terms of having to endure fewer surgical procedures.
Our study had limitations. There was a stark difference in the prevalence of injuries ascribed the Gustilo–Anderson type-IIIB classification between Guidelines and Standards eras. The Gustilo–Anderson classification is relatively simple and its use has become almost universal. Nevertheless, studies have highlighted its shortcomings, particularly in relation to the wide range of surgical reconstruction that may be required to deal with type-IIIB injuries.12,13 Indeed, injuries ascribed this classification were the majority of cases in the Guidelines-era cohort, accounting for 54/67 cases. The fact that 21 (39%) of these cases were treated with SSG alone strongly suggests that these injuries were misclassified even though classification was done after debridement. Reconstructive procedures required for the Standards cohort are more in keeping with the type-IIIB classification. No attempt has been made to re-classify these cases retrospectively because the accepted method is to classify after debridement. However, an argument could be made for a classification system of open fractures that determines whether the bone and soft-tissue injuries are ‘simple’ or ‘complex’, respectively, and then is refined in the light of final management.
In addition, data were collected only for transferred patients in whom the initial surgical team felt a specialist orthopaedic or plastic-surgical opinion was warranted. Several patients could probably have been cared for without input from the orthoplastic team. Consequently, the transferred patients received in this orthoplastic service may have represented a skewed sample of the overall population treated across this region. Injuries perceived to be more severe may have been more likely to be referred, and assessment of the injury framed consistently in terms of the Gustilo–Anderson classification, application of which is not without potential flaws.
The OPP group appeared to have benefitted most from early combined orthoplastic care, requiring significantly fewer procedures than TASP or DAP groups. A combined surgical team undertaking the first debridement may have allowed the wound to be managed more confidently than if initial surgery had been undertaken elsewhere. Thus, planning and execution of definitive treatment was accomplished more expeditiously. Increasing the proportion of hot transfers would decrease the total number of procedures required. However, the burden would shift from semi-elective second-look surgery to time-dependent first debridement and fracture stabilisation. Ensuring access to the operating theatre with appropriately skilled surgeons seven days a week to maintain the required level of performance should be achievable, but would require resourcing and planning.
Conclusions
Publication of Standards intended to improve the care of patients requiring transfer to an orthoplastic unit has, to date, yielded the greatest benefits to those admitted directly from the scene of injury. However, similar benefits can be conferred to those transferred rapidly before surgery undertaken elsewhere. However, accurate assessment of open fractures will always be needed to ascertain if immediate limb-saving interventions (eg fasciotomy, re-vascularisation) are required.
We have intentionally taken a narrow view of the surgical activity of a single orthoplastic unit in terms of the surgical care delivered and endured by patients. Research to examine health-service utilisation before and after open tibial fractures is ongoing, and we wish to develop a ‘recovery scale’ to quantify the prevalence and extent of recovery in patients sustaining these potentially life-changing injuries.
References
- 1.Court-Brown CMCxs , Cross AT, Hahn DM, et al. . The Management of Open Tibial Fractures: A Report by the BOA/BAPS Working Party on The Management of Open Tibial Fractures. London: BOA/BAPS; 1997. [Google Scholar]
- 2.Allison K, Wong M, Bolland B, Peart F, Porter K. The management of compound leg injuries in the West Midlands (UK): are we meeting current guidelines? Brit J Plast Surg 2005; : 640–645. [DOI] [PubMed] [Google Scholar]
- 3.Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures: the need for combined orthopaedic and plastic surgical treatment in specialist centres. J Bone Joint Surg (Br) 2006; : 351–357. [DOI] [PubMed] [Google Scholar]
- 4.Nanchahal J, Nayagam S, Khan U, et al. Standards for the Management of Open Fractures of the Lower Limb. London: Royal Society of Medicine Press; 2009. [Google Scholar]
- 5.Webb LX, Bosse MJ, Castillo RC, MacKenzie EJ. Analysis of surgeon-controlled variables in the treatment of limb-threatening type-III open tibial diaphyseal fractures. J Bone Joint Surg 2007; : 923–928. [DOI] [PubMed] [Google Scholar]
- 6.Khan U, Smitham P, Pearse M, Nanchahal J. Management of severe open ankle injuries. Plast Reconstr Surg 2007; : 578–589. [DOI] [PubMed] [Google Scholar]
- 7.Gustilo R, Anderson J. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg (Am) 1976; : 453–458. [PubMed] [Google Scholar]
- 8.Müller ME, Koch P, Nazarian S. The comprehensive classification of fractures of long bones. Berlin: Springer-Verlag; 1990. [Google Scholar]
- 9.Trickett R, Harding E, Nguyen D, Potokar T, Pallister I. Time to debride? The primary treatment of open tibial fractures and rates of subsequent infection. Injury Extra 2009; : 190. [Google Scholar]
- 10.Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg 1986; : 285–292. [DOI] [PubMed] [Google Scholar]
- 11.Gopal S, Majumder S, Batchelor A, Knight S, De Boer P, Smith R. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg (Br). 2000; : 959–966. [DOI] [PubMed] [Google Scholar]
- 12.Rajasekaran S, Naresh Babu J, Dheenadhayalan J, et al. A score for predicting salvage and outcome in Gustilo type-IIIA and type-IIIB open tibial fractures. J Bone Joint Surg (Br) 2006; 88: ,351–1,360. [DOI] [PubMed] [Google Scholar]
- 13.Rajasekaran S, Sabapathy SR. A philosophy of care of open injuries based on the Ganga hospital score. Injury 2007; : 137–146. [DOI] [PubMed] [Google Scholar]
- 14.Stammers J, Williams D, Hunter J, Vesely M, Nielsen D. The impact of trauma centre designation on open tibial fracture management. Ann R Coll Surg Engl 2013; : 184–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page PR, Trickett RW, Rahman SM, et al. The use of secure anonymised data linkage to determine changes in healthcare utilisation following severe open tibial fractures. Injury. (In press.) (cited April 2015). [DOI] [PubMed] [Google Scholar]


