Abstract
Median arcuate ligament syndrome (MALS) is a rare disorder due to coeliac trunk compression by the median arcuate ligament, resulting in coeliac artery stenosis characterised by chronic, recurrent abdominal pain. Patients with MALS are often middle-aged females presenting with a triad of postprandial epigastric pain, weight loss and abdominal bruit. It is a diagnosis of exclusion and confirmed by computed tomography or magnetic resonance imaging. Laparoscopic or open surgical decompression are the only treatment options in MALS. We present two cases of MALS treated by laparoscopic decompression as well as a literature review on this treatment.
Keywords: Median arcuate ligament syndrome, Coeliac artery compression syndrome, Dunbar syndrome, Laparoscopic decompression
Median arcuate ligament syndrome (MALS), also known as coeliac artery compression syndrome or Dunbar syndrome, is a rare phenomenon due to coeliac trunk compression by the median arcuate ligament (MAL). The ligament, which lies superior to the coeliac artery, is a fibrous arch connecting the crura of the diaphragm forming the aortic hiatus. An abnormally low lying ligament can cause coeliac artery stenosis, potentially resulting in chronic, recurrent abdominal pain. Diagnosis is challenging and only confirmed after exclusion of other causes of abdominal pain. Surgical treatment is the only option in MALS. While open decompression has been the traditional approach, laparoscopic decompression is an emerging therapy. We present two cases of MALS treated with laparoscopic decompression.
Case histories
Case A
A 31-year-old woman presented with several episodes of chest pain, palpitations, exercise intolerance, nausea, vertigo, tremors and hypertension. She had a history of chronic and recurrent abdominal pain, especially after meals. Gastrointestinal tract pathologies were ruled out by ultrasonography, gastroscopy and colonoscopy. Abdominal computed tomography (CT) revealed high grade stenosis (>80%) of the coeliac artery, 10mm from its origin from the aorta (Figs 1 and 2). The patient was subsequently diagnosed with MALS and admitted to our department for surgical treatment.
Figure 1.

Computed tomography showing compression of coeliac trunk by the median arcuate ligament with poststenotic dilation (arrow)
Figure 2.
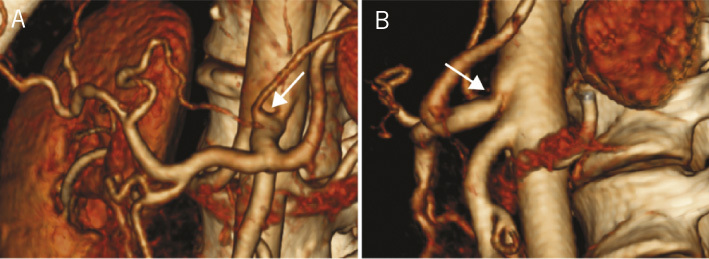
Three-dimensional computed tomography reconstruction showing anterior (A) and lateral (B) views of compression of coeliac trunk by the median arcuate ligament with poststenotic dilation (arrow)
Case B
A 26-year-old woman was admitted to a local hospital owing to worsening chronic abdominal pain exacerbated after eating, and accompanied by nausea and vomiting. Ultrasonography found significant variations in the blood flow velocity of the coeliac artery during maximum inspiration and quiet respiration. Abdominal CT was ordered and the diagnosis of MALS with 70% stenosis was made. The patient was referred to our clinic for surgical treatment.
In both cases, decompression of the coeliac trunk was performed using a laparoscopic approach. Prophylactic, intraoperative antibiotics and postoperative thromboembolytics were administered to the patients. During the surgery, the patients were placed in a supine split-leg reverse Trendelenburg position. Four ports were introduced (Figure 3). The technical access during surgery was achieved using an antegrade dissection method (Figure 4).
Figure 3.
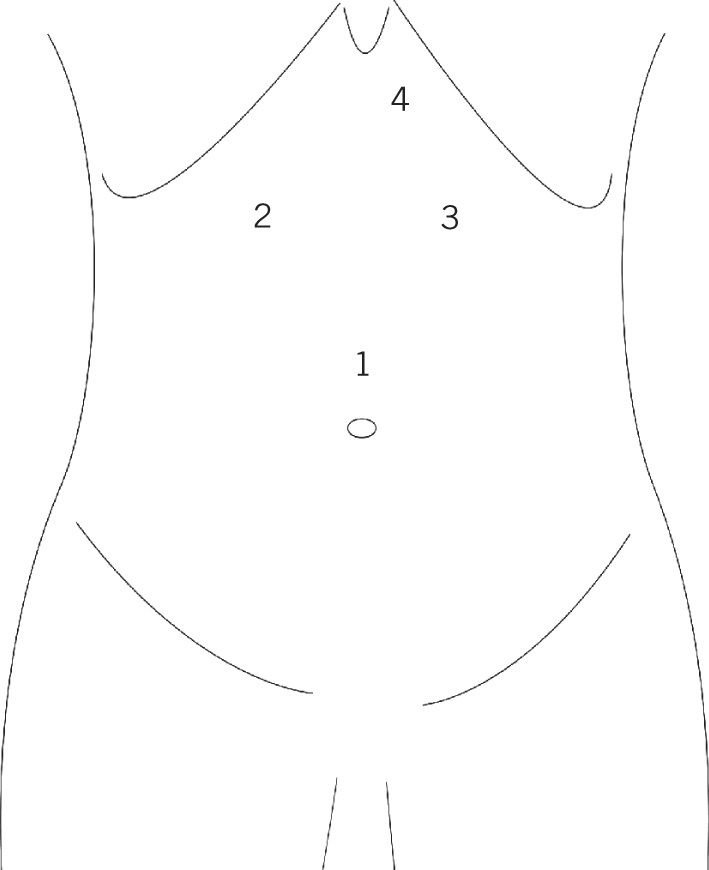
Schematic diagram of the abdomen with trocar placement: 1 = 10mm optic; 2 and 3 = 5mm for grasper and scissors/coagulating hook of the operator; 4 = fan retractor
Figure 4.
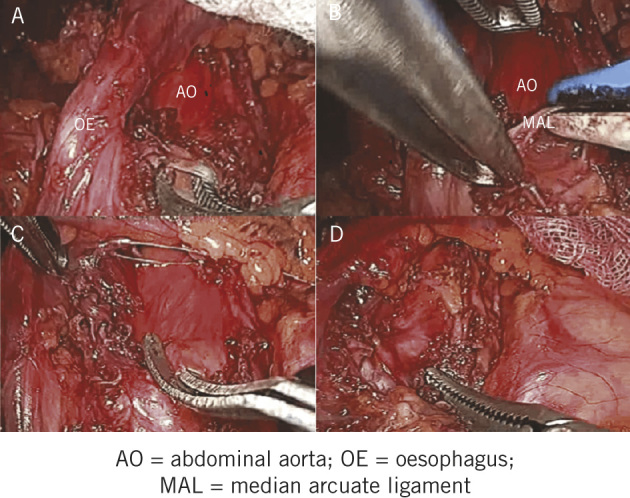
Surgical images: locating the MAL (A), cross-clamping the MAL with the ligation device (B), dividing the fibres of the MAL (C) and decompression of the coeliac trunk (D)
The gastrohepatic ligament was divided to facilitate the identification of the right crus of the diaphragm, inferior to the cardia. The oesophagus was dissected cranially to the oesophageal hiatus to facilitate mobilisation of the oesophagus, cardia and gastric fundus. The stomach was retracted laterally and caudally, exposing the anterior surface of the aorta. The left gastric artery was then identified. Following the superior aspect of the left gastric artery, the coeliac trunk was located. Poststenotic dilation and pulsation of the coeliac trunk also helped with the localisation. The MAL, which compressed the coeliac trunk, was divided, along with the surrounding neural coeliac plexus, until the coeliac trunk was completely exposed from the aorta to its primary branches (left gastric, common hepatic and splenic arteries). Complete decompression and release of the coeliac artery from the MAL was confirmed in both patients using laparoscopic ultrasonography.
Neither patient experienced any operative or postoperative complications and they did not require angioplasty or coeliac stenting. Postoperatively, they experienced immediate symptomatic relief and were discharged to be followed up an outpatient basis. Follow-up review on both patients revealed improvement in the coeliac trunk flow.
Discussion
MALS was first described in a 1963 case report by Harjola1 and then by Dunbar et al in a 1965 case series.2 While asymptomatic stenosis has been reported in radiographic studies to occur in up to 6.7% of the population, stenosis resulting in clinical symptoms is a rare occurrence.3 Experimental evidence using gastric tonometry has demonstrated that MALS is directly responsible for gastric ischaemia and that surgical decompression leads to flow re-establishment with immediate resolution of symptoms.4 Although the ischaemic pathophysiology of MALS is widely accepted, there is debate whether neuropathic mechanisms are involved.5
The clinical presentation of MALS is widely variable. Patients with MALS are often middle-aged women presenting with a triad of postprandial epigastric abdominal pain, weight loss and abdominal bruit. The pain is often exacerbated by exercise, and it may be associated with bloating, nausea, vomiting and diarrhoea. In our patients, postprandial abdominal pain was the most prominent symptom, consistent with the findings by Jimenez et al, where the most commonly reported symptom in 80% of patients was abdominal pain.6 No abdominal bruits were discernible on auscultation in either of our patients. Several previous cases have reported the transient relief of symptoms with MALS when the patients bring their knees up to their chest.7
Diagnosis is difficult and is made after exclusion of other more common causes of abdominal pain. Differential diagnoses of chronic intestinal ischaemia, superior mesenteric artery syndrome and irritable bowel syndrome should be considered. While ultrasonography may be used for screening of intestinal ischaemia, confirmation of diagnosis is made by abdominal CT or magnetic resonance imaging, or by using inspiratory and expiratory arteriography, preferentially.
Four surgical options have been described for the treatment of MALS: coeliac artery decompression and coeliac ganglionectomy, coeliac artery decompression and dilatation, coeliac artery decompression and reconstruction, and coeliac artery endovascular stenting.8 Among them, decompression and coeliac ganglionectomy is the most adopted treatment since long-term positive outcomes of similar procedures have been observed. Moreover, with the increasing reports on laparoscopic approaches, the focus has now shifted to the comparison of open and laparoscopic decompression of MALS. A systematic review by Jimenez et al found that the majority of patients treated with either open decompression or laparoscopic decompression of the MAL experienced immediate postoperative pain relief.6 However, the laparoscopic approach is becoming more widely adopted owing to benefits such as shorter hospital stay,9,10 decreased time to feeding,9 smaller risk of postoperative complications,6 decreased blood loss, greater postoperative pain relief and better cosmetic outcomes.10
We performed a review of cases reported in the literature to compare and evaluate the results obtained via the laparoscopic approach in the surgical treatment of MALS (Table 1).11–38 A total of 28 studies of laparoscopic cases (186 patients) were identified, in which 171 patients (91.9%) experienced immediate symptomatic relief. Conversion to open decompression due to complications was required in 11 patients (5.9%). In 24 studies (103 patients), the patients were observed for recurrence of symptoms in a period ranging from 2 weeks to 8 years. Recurrence was reported in 9 cases (8.7%). No surgery related fatalities were reported in any of the studies.
Table 1.
Cases with laparoscopic approach in the surgical treatment of median arcuate ligament syndrome
| Author | Number of cases | Mean follow-up duration | Conversion to open surgery | Ligament release | Improvement of symptoms | Recurrence of symptoms |
| Roayaie, 200211 | 1 | 3 mths | 0 | 1 | 1 | 0 |
| Dordoni, 200212 | 1 | 6 mths | 0 | 1 | 1 | 0 |
| Carbonell, 200513 | 1 | 7 mths | 0 | 1 | 1 | 0 |
| Baldassarre, 200714 | 1 | 3 mths | 0 | 1 | 1 | 0 |
| Jaik, 200815 | 1 | 6 mths | 0 | 1 | 1 | 0 |
| Jarry, 200816 | 1 | 1.5 mths | 0 | 1 | 1 | 0 |
| Duffy, 200817 | 1 | 10 mths | 0 | 1 | 1 | 0 |
| Vaziri, 200918 | 3 | 6 mths | 0 | 3 | 3 | 0 |
| Rotellar, 200919 | 7 | 6 mths (to 8 yrs) | 0 | 7 | 3 | Not available |
| Van Petersen, 200920 | 42 | 20 mths | 1 | 42 | 41 | Not available |
| Baccari, 200921 | 16 | 28 mths | 2 | 16 | 14 | 0 |
| Roseborough, 200922 | 15 | 44 mths | 4 | 15 | 14 | 1 |
| Tulloch, 201023 | 12 | 14 mths | 2 | 12 | 12 | 5 |
| Gander, 201024 | 1 | 4 mths | 0 | 1 | 1 | 0 |
| Aschenbach, 201025 | 22 | Not available | 0 | 22 | 22 | Not available |
| Kohn, 201126 | 2 | 48.6 mths | 0 | 2 | 2 | 0 |
| Berard, 201227 | 11 | 35 mths | 2 | 11 | 10 | 1 |
| Relles, 201228 | 3 | 11 mths | 0 | 3 | 2 | 1 |
| Wani, 201229 | 2 | 1.5 mths | 0 | 2 | 2 | 0 |
| Tsujimoto, 201230 | 1 | Not available | 0 | 1 | 1 | 0 |
| Nguyen, 201231 | 5 | 20 mths | 0 | 5 | 5 | 0 |
| Lainez, 201332 | 1 | 0.5 mths | 0 | 1 | 1 | 0 |
| You, 201333 | 1 | 0.5 mths | 0 | 1 | 1 | 0 |
| Joyce, 201334 | 6 | 13 mths | 0 | 6 | 6 | 0 |
| Do, 201335 | 12 | 22 mths | 0 | 12 | 8 | Not available |
| El-Hayek, 201336 | 15 | 15 mths | 0 | 15 | 14 | 1 |
| Muqeetadnan, 201337 | 1 | Not available | 0 | 1 | 1 | 0 |
| Fajer, 201438 | 1 | 3 mths | 0 | 1 | 1 | 0 |
| Total | 186 | 11 | 171 | 9 |
Conclusions
Our case demonstrates the importance of investigating MALS as a possible diagnosis in patients with chronic, recurrent postprandial abdominal pain of unknown aetiology. CT angiography is a highly effective diagnostic modality when this pathology is suspected. Laparoscopic decompression is an effective treatment for MALS and can provide immediate symptomatic relief. While large clinical trials are unavailable owing to the rarity of the syndrome, a careful review of the literature demonstrates the efficacy and advantages of the laparoscopic approach.
References
- 1. Harjola PT. A rare obstruction of the coeliac artery. Report of a case . Ann Chir Gynaecol Fenn 1963. ; : 547–550. [PubMed] [Google Scholar]
- 2. Dunbar JD, Molnar W, Beman FF, Marable SA. Compression of the celiac trunk and abdominal angina . Am J Roentgenol Radium Ther Nucl Med 1965. ; : 731–744. [DOI] [PubMed] [Google Scholar]
- 3.Kazan V, Qu W, Al-Natour M et al. Celiac artery compression syndrome: a radiological finding without clinical symptoms? Vascular 2013 March 18. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 4. Faries PL, Narula A, Veith FJ. et al. The use of gastric tonometry in the assessment of celiac artery compression syndrome . Ann Vasc Surg 2000. ; : 20–23. [DOI] [PubMed] [Google Scholar]
- 5. Roseborough GS. Laparoscopic management of celiac artery compression syndrome . J Vasc Surg 2009. ; : 124–133. [DOI] [PubMed] [Google Scholar]
- 6. Jimenez JC, Harlander-Locke M, Dutson EP. Open and laparoscopic treatment of median arcuate ligament syndrome . J Vasc Surg 2012. ; : 869–873. [DOI] [PubMed] [Google Scholar]
- 7. Lainez RA, Richardson WS. Median arcuate ligament syndrome: a case report . Ochsner J 2013. ; : 561–564. [PMC free article] [PubMed] [Google Scholar]
- 8. Kohn GP, Bitar RS, Farber MA. et al. Treatment options and outcomes for celiac artery compression syndrome . Surg Innov 2011. ; : 338–343. [DOI] [PubMed] [Google Scholar]
- 9. Tulloch AW, Jimenez JC, Lawrence PF. et al. . Laparoscopic versus open celiac ganglionectomy in patients with median arcuate ligament syndrome. J Vasc Surg 2010. ; 52: 1,283 – 1 , 289 . [DOI] [PubMed] [Google Scholar]
- 10. Baccari P, Civilini E, Dordoni L. et al. Celiac artery compression syndrome managed by laparoscopy . J Vasc Surg 2009. ; : 134–139. [DOI] [PubMed] [Google Scholar]
- 11. Roayaie S, Jossart G, Gitlitz D. et al. Laparoscopic release of celiac artery compression syndrome facilitated by laparoscopic ultrasound scanning to confirm restoration of flow . J Vasc Surg 2000. ; : 814–817. [DOI] [PubMed] [Google Scholar]
- 12. Dordoni L, Tshomba Y, Giacomelli M. et al. Celiac artery compression syndrome: successful laparoscopic treatment – a case report . Vasc Endovascular Surg 2002. ; : 317–321. [DOI] [PubMed] [Google Scholar]
- 13.Carbonell AM, Kercher KW, Heniford BT, Matthews BD. Laparoscopic management of median arcuate ligament syndrome. Surg Endosc 2005; 19: 729. [DOI] [PubMed] [Google Scholar]
- 14. Baldassarre E, Torino G, Siani A. et al. The laparoscopic approach in the median arcuate ligament syndrome . Swiss Med Wkly 2007. ; : 353–354. [DOI] [PubMed] [Google Scholar]
- 15. Jaik NP, Stawicki SP, Weger NS, Lukaszczyk JJ. Celiac artery compression syndrome: successful utilization of robotic-assisted laparoscopic approach . J Gastrointestin Liver Dis 2007. ; : 93–96. [PubMed] [Google Scholar]
- 16. Jarry J, Berard X, Ducasse E. et al. Laparoscopic management of median arcuate ligament syndrome . J Mal Vasc 2008. ; : 30–34. [DOI] [PubMed] [Google Scholar]
- 17. Duffy AJ, Panait L, Eisenberg D. et al. Management of median arcuate ligament syndrome: a new paradigm . Ann Vasc Surg 2009. ; : 778–784. [DOI] [PubMed] [Google Scholar]
- 18. Vaziri K, Hungness ES, Pearson EG, Soper NJ. Laparoscopic treatment of celiac artery compression syndrome: case series and review of current treatment modalities . J Gastrointest Surg 2009. ; : 293–298. [DOI] [PubMed] [Google Scholar]
- 19. A-Cienfuegos J, Rotellar F, Valentí V et al. The celiac axis compression syndrome (CACS): critical review in the laparoscopic era . Rev Esp Enferm Dig 2010. ; : 193–201. [DOI] [PubMed] [Google Scholar]
- 20. van Petersen AS, Vriens BH, Huisman AB. et al. Retroperitoneal endoscopic release in the management of celiac artery compression syndrome . J Vasc Surg 2009. ; : 140–147. [DOI] [PubMed] [Google Scholar]
- 21. Baccari P, Civilini E, Dordoni L. et al. Celiac artery compression syndrome managed by laparoscopy . J Vasc Surg 2009. ; : 134–139. [DOI] [PubMed] [Google Scholar]
- 22. Roseborough GS. Laparoscopic management of celiac artery compression syndrome . J Vasc Surg 2009. ; : 124–133. [DOI] [PubMed] [Google Scholar]
- 23. Tulloch AW, Jimenez JC, Lawrence PF. et al. Laparoscopic versus open celiac ganglionectomy in patients with median arcuate ligament syndrome. J Vasc Surg 2010. ; : 1,283–1,289 . [DOI] [PubMed] [Google Scholar]
- 24. Gander S, Mulder DJ, Jones S. et al. Recurrent abdominal pain and weight loss in an adolescent: celiac artery compression syndrome . Can J Gastroenterol 2010. ; : 91–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Aschenbach R, Basche S, Vogl TJ. Compression of the celiac trunk caused by median arcuate ligament in children and adolescent subjects: evaluation with contrast-enhanced MR angiography and comparison with Doppler US evaluation . J Vasc Interv Radiol 2011. ; : 556–561. [DOI] [PubMed] [Google Scholar]
- 26. Kohn GP, Bitar RS, Farber MA. et al. Treatment options and outcomes for celiac artery compression syndrome . Surg Innov 2011. ; : 338–343. [DOI] [PubMed] [Google Scholar]
- 27. Berard X, Cau J, Déglise S et al. Laparoscopic surgery for coeliac artery compression syndrome: current management and technical aspects . Eur J Vasc Endovasc Surg 2012. ; : 38–42. [DOI] [PubMed] [Google Scholar]
- 28. Relles D, Moudgill N, Rao A. et al. Robotic-assisted median arcuate ligament release . J Vasc Surg 2012. ; : 500–503. [DOI] [PubMed] [Google Scholar]
- 29. Wani S, Wakde V, Patel R. et al. Laparoscopic release of median arcuate ligament . J Minim Access Surg 2012. ; : 16–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tsujimoto H, Hiraki S, Sakamoto N. et al. Laparoscopic treatment for median arcuate ligament syndrome: the usefulness of intraoperative Doppler ultrasound to confirm the decompression of the celiac artery . Surg Laparosc Endosc Percutan Tech 2012. ; : e71–e75. [DOI] [PubMed] [Google Scholar]
- 31. Nguyen T, Neale M, Lane R. et al. Laparoscopic management of the median arcuate ligament syndrome . ANZ J Surg 2012. ; : 265–268. [DOI] [PubMed] [Google Scholar]
- 32. Lainez RA, Richardson WS. Median arcuate ligament syndrome: a case report . Ochsner J 2013. ; : 561–564. [PMC free article] [PubMed] [Google Scholar]
- 33. You JS, Cooper M, Nishida S. et al. Treatment of median arcuate ligament syndrome via traditional and robotic techniques . Hawaii J Med Public Health 2013. ; : 279–281. [PMC free article] [PubMed] [Google Scholar]
- 34. Joyce DD, Antiel RM, Oderich G. et al. Pediatric median arcuate ligament syndrome: surgical outcomes and quality of life . J Laparoendosc Adv Surg Tech A 2014. ; : 104–110. [DOI] [PubMed] [Google Scholar]
- 35. Do MV, Smith TA, Bazan HA. et al. Laparoscopic versus robot-assisted surgery for median arcuate ligament syndrome. Surg Endosc 2013. ; 27: 4,060 – 4 , 066 . [DOI] [PubMed] [Google Scholar]
- 36. El-Hayek KM, Titus J, Bui A. et al. Laparoscopic median arcuate ligament release: are we improving symptoms? J Am Coll Surg 2013. ; : 272–279. [DOI] [PubMed] [Google Scholar]
- 37. Muqeetadnan M, Amer S, Rahman A. et al. Celiac artery compression syndrome . Case Rep Gastrointest Med 2013; 934052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fajer S, Cornateanu R, Ghinea R. et al. Laparoscopic repair of median arcuate ligament syndrome: a new approach . J Am Coll Surg 2014. ; : e75–e78. [DOI] [PubMed] [Google Scholar]


