Abstract
BACKGROUND/OBJECTIVES
This study was conducted to evaluate the feasibility of a sodium reduction program at local restaurants through nutrition education and examination of the health of restaurant owners and cooks.
SUBJECTS/METHODS
The study was a single-arm pilot intervention using a pre-post design in one business district with densely populated restaurants in Seoul, South Korea. The intervention focused on improving nutrition behaviors and psychosocial factors through education, health examination, and counseling of restaurant personnel. Forty-eight restaurant owners and cooks completed the baseline survey and participated in the intervention. Forty participants completed the post-intervention survey.
RESULTS
The overweight and obesity prevalences were 25.6% and 39.5%, respectively, and 74.4% of participants had elevated blood pressure. After health examination, counseling, and nutrition education, several nutrition behaviors related to sodium intake showed improvement. In addition, those who consumed less salt in their baseline diet (measured with urine dipsticks) were more likely to agree that providing healthy foods to their customers is necessary. This study demonstrated the potential to reduce the sodium contents of restaurant foods by improving restaurant owners' and cooks' psychological factors and their own health behaviors.
CONCLUSIONS
This small pilot study demonstrated that working with restaurant owners and cooks to improve their own health and sodium intake may have an effect on participation in restaurant-based sodium reduction initiatives. Future intervention studies with a larger sample size and comparison group can focus on improving the health and perceptions of restaurant personnel in order to increase the feasibility and efficacy of restaurant-based sodium reduction programs and policies.
Keywords: Sodium, sodium reduction, restaurant, environmental intervention, nutrition policy
INTRODUCTION
High levels of sodium intake are known to be strong risk factors for hypertension and adverse cardiovascular health [1]. High sodium intake is prevalent in South Korea, where the food culture is centered on traditional fermented seasonings with high sodium contents. The Korea Health and Nutrition Examination Survey reported that the average sodium intake level is 2.5 times higher than the upper limit (2,000 mg per day) suggested by the World Health Organization (WHO) [2]. Partly due to high sodium intake, it is estimated that one in three men and one in five women are hypertensive [2], and cardiovascular disease is one of the major causes of death [3].
People in their 30s and 40s have especially high sodium intake, and one of the possible reasons for this phenomenon is their high frequency of eating out [4]. The sodium contents of foods served at restaurants and worksite cafeterias [5,6] are higher than those of foods prepared at home, and the frequency of eating out among the adult population is continuously increasing [2].
Given the high prevalence of hypertension and cardiovascular diseases among the South Korean adult population, there is an urgent need to lower sodium intake through effective public health strategies [7]. Previous studies aimed at altering sodium intake by reducing sodium contents of foods served at worksite cafeterias have shown some promising results [8,9]. Study participants exposed to menus with lowered sodium contents at their worksite cafeterias showed lower consumption of sodium as compared to participants under control conditions. In addition, one pilot study on independent restaurants in the U.S. demonstrated the possibility to alter sodium-related cooking methods and restaurant menu items [10]. However, strategies to lower sodium intake at local restaurants require more research to develop effective methods in different settings.
Intervention studies that are planned and implemented with a theoretical background can be both effective and efficient [11]. Previous studies have shown that use of key concepts from the health belief model, including perceived benefits and barriers, was successful in improving participants' knowledge of nutrition-related diseases [12] and nutritional behaviors [13]. In addition, social cognitive theory has been widely used in nutrition intervention and health promotion programs. Originally developed as a developmental learning theory by Bandura [14], the key concepts, such as self-efficacy and outcome expectancies, have been proven to be key factors in improving nutritional behaviors and health outcomes [15,16,17].
Despite the crucial roles of restaurant owners and employees in shaping nutrition environments of food outlets, little effort has been made in understanding their perceptions and behaviors and how these factors may be related to their cooking practices. Most low-sodium initiatives at food outlets have focused on improving consumers' ability to choose healthier options, and these initiatives are mainly centered on worksite cafeterias [8,9,10]. Although numerous health promotion programs have been developed to target restaurant workers, these programs were designed to improve general health indicators among low-income or immigrant workers in the U.S. [18,19].
The hypotheses that we tested are as follows: 1) restaurant owners and cooks whose sodium intake is lower than average are more amenable to participation in sodium reduction initiatives at their restaurants and 2) improving perceptions of sodium reduction in restaurant owners and cooks through health examination and education will improve their nutrition behaviors and cooking methods at restaurants.
SUBJECTS AND METHODS
General study design and theoretical framework
This study employed a single-arm intervention with a pre-post design with owners and cooks from 30 independent restaurants in the Guro District of Seoul. The pilot study included the following components: 1) health examination and counseling, 2) nutrition education, and 3) a structured survey regarding key psychosocial and behavioral factors related to sodium intake and food preparation at restaurants. The Guro Public Health Center (GPHC) also distributed salimeters along with a manual to participating restaurants. Two 1-hour long sessions of nutrition education were conducted by a professional nutrition educator, and all participants attended at least one session at their convenience. The education sessions covered the risk of high sodium intake and tips for lowering sodium contents not only in the foods they serve at restaurants but in their own diet. The pre-intervention survey and interventions were conducted in October 2014, and the post survey was administered in February 2015. The study was based on the health belief model and social cognitive theory [11]. During nutrition education and health counseling sessions, we targeted participants' beliefs about sodium-related health problems, perceived benefits of lowering sodium intake, and self-efficacy in consuming less sodium in their diet and in providing less sodium to their customers. The approach of working with restaurant personnel and their nutrition behaviors was based on social cognitive theory, which emphasizes the interrelatedness between individuals and their environments. We hypothesize that restaurant personnel's psychosocial and behavioral factors can be an important environmental construct for making the nutrition environment healthier for potential customers.
Participant recruitment
Participants were recruited with the help of the GPHC and the Association of Business Owners in Guro District. Flyers were distributed to owners and cooks through the GPHC and the president of the Association. Written consent forms were signed by all participants, and the study protocol was approved by the Institutional Review Board at Hanyang University (HYI-14-120-3).
Measurements
Standing height and weight were measured using standardized techniques and equipment [inlabs50 and InBody230, Biospace]. Body Mass Index (BMI; kg/m2) was calculated, and participants were classified as overweight (23 ≤ BMI < 25) and obese (BMI ≥ 25) according to the World Health Organization guideline for Asians [20]. Waist circumference and blood pressure were measured according to the protocol used for the national health survey [Rondo by HoechstMass, HEM-780 by Omron] [2].
Spot urine dipsticks were used to estimate the sodium intake of participants [Check salt in my body, JW Medical]. By counting the number of six indicators that changed color after contact with urine, sodium intake was approximated from 3 g to more than 21 g of salt intake per day [21,22]. To compare key behavioral and psychosocial factors (perception and self-efficacy of providing healthier foods to customers) between people with high and low sodium intake, we categorized participants into two groups using the cut-off point of three changed indicators. The cut-off correlates to an estimated 12 g of salt (4,800 mg of sodium) intake per day, which is approximately the average level of sodium intake among the Korean adult population [2].
A self-administered questionnaire was distributed before and after the interventions. The questionnaire included questions on basic sociodemographic factors, key health behaviors, knowledge and behaviors relevant to sodium intake, and healthy food provisions at their restaurants. The questions were adapted from previous international and domestic sodium reduction studies and the Korea Community Health Survey [16,17,23].
The nutrition education session included information on the potential health outcomes associated with high sodium intake and introduced cooking methods aimed at lowering sodium contents in side dishes and soups. Most psychosocial and behavioral factors were measured on a Likert scale, with responses ranging from “never” (1 point) to “all of the time” (4 points); a score of 4 indicates the greatest sodium reduction while 1 corresponds to the least.
All statistical analyses were performed using Stata 10.1 (StataCorp. 2007. College Station, TX). The survey items of the psychosocial and behavioral factors regarding healthy food provisions were collapsed into two categories for categorical analysis. Descriptive statistics were used to analyze the survey responses, and the McNemar test and paired t-test were used to analyze differences between the pre- and post-intervention surveys.
RESULTS
Health indicators and behaviors of participants
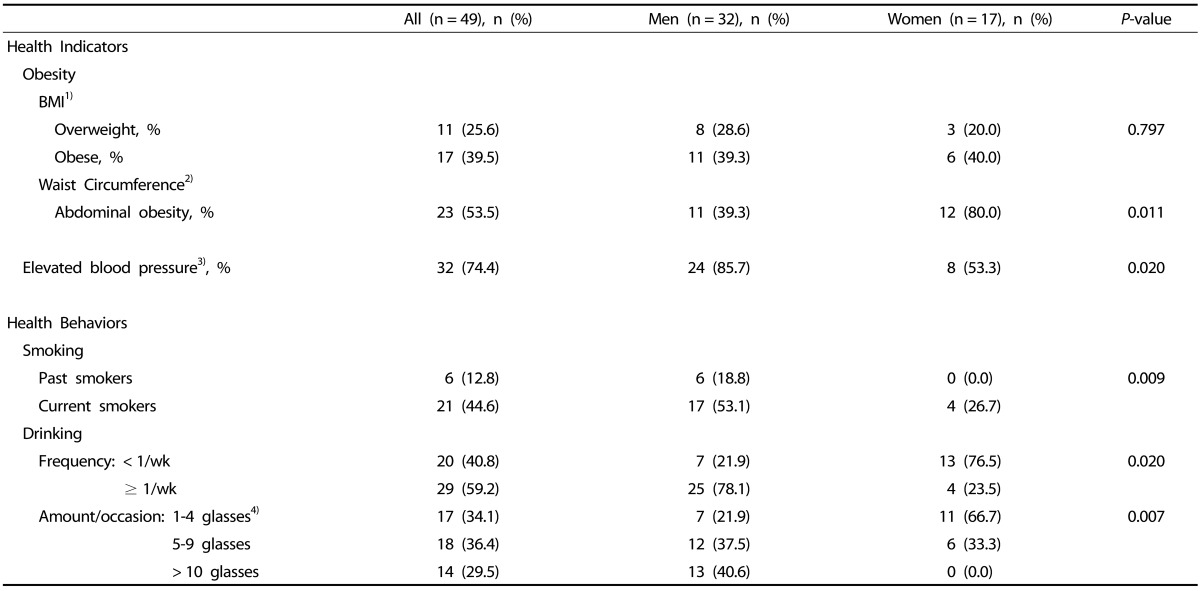
Participants ranged in age from 29 to 63 years old (mean 48.5). A total of 49 owners and cooks from 30 restaurants participated, and all serve Korean dishes, including hot stews, barbecued meat or seafood, and noodles. Table 1 indicates that 65% of the participants were overweight or obese. Only a quarter of participants had normal blood pressure. Prevalence of abdominal obesity was higher among women than men, whereas more men had elevated blood pressure than women. Approximately 45% of participants were current smokers, and 59% drank more than once a week. Most of the male drinkers were heavy drinkers; 41% of men drank more than 10 glasses (200 ml for beer and 50 ml for hard liquor) per occasion.
Table 1. Results of health examination and health behaviors among restaurants owners and cooks.
1) Overweight: overweight: 23 ≤ BMI < 25, obese: BMI ≥ 25
2) Obese: waist circumference ≥ 90 cm in men, ≥ 80 cm in women
3) Elevated blood pressure: systolic ≥ 130 mmHg or diastolic ≥ 85 mmHg
4) 200 ml for beer and 50 ml for hard liquor
Key psychosocial and behavioral factors of low-sodium restaurant initiatives by level of estimated sodium intake
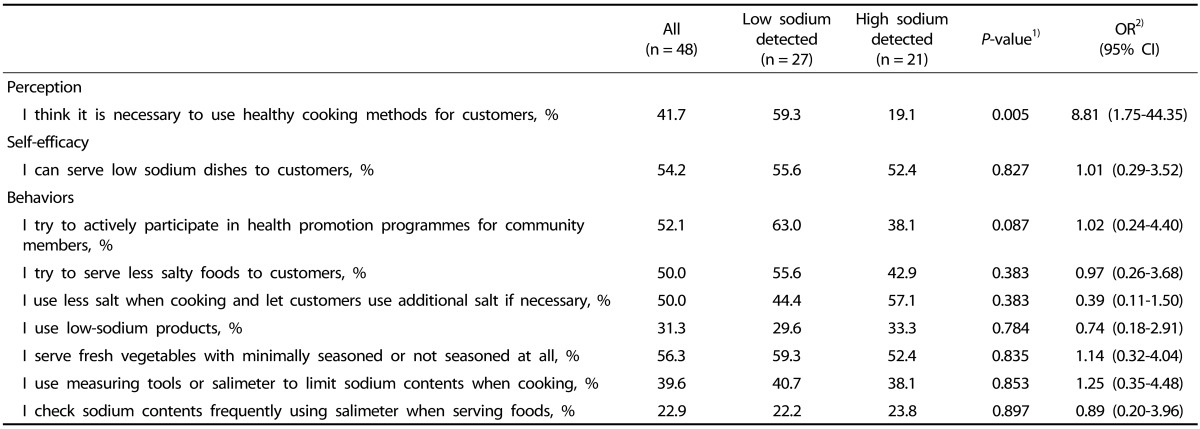
Among participants who were categorized into the lower sodium-intake group based on urine dipsticks (27 participants out of 48), 59% strongly agreed that it is necessary to use healthy cooking methods for customers. In contrast, only 19% of participants with high sodium detected in their urine strongly agreed with the necessity of healthy cooking at their restaurants. As a general tendency, the participants with low sodium detected in their urine were more willing to participate in sodium reduction initiatives. However, due to the small sample size, none of the behavioral responses reached statistical significance (Table 2). When the participants' age and sex were adjusted in the multivariate analysis, similar patterns were observed.
Table 2. Key psychosocial and behavioral factors of low-sodium restaurant initiatives by level of estimated sodium intake tested with spot urine dipstick among restaurant owners and cooks.
All of the above psychosocial and behavioral factors were measured on a 4-point Likert-type scale. The percentages presented here counted respondents who answered "strongly agree" or "all the time"
1) Chi-square test, 2) Logistic regression adjusted for age and sex.
Pre- and post-measurements of behavioral and psychosocial factors regarding sodium intake among restaurants owners and cooks after intervention
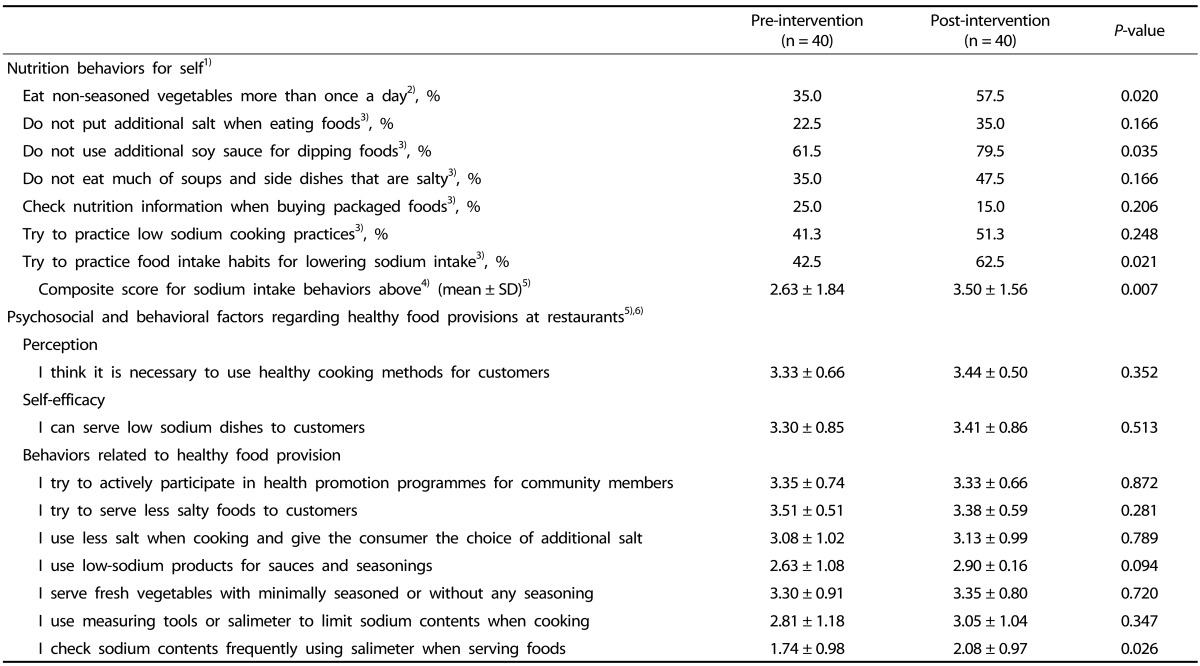
Table 3 presents the differences in key psychosocial and behavioral factors regarding lower consumption of sodium and less sodium provided to their customers before and after the interventions. Except for the question regarding checking nutritional information when buying packaged foods, all behavioral factors exhibited an upward trend for lowering participants' sodium intake. Among these, consumption of non-seasoned vegetables, not using additional soy sauce for dipping foods, and trying to apply food intake habits to lower sodium intake exhibited statistical significance. We created a composite score summarizing sodium intake-related behaviors (giving a value of 1 when participants answered “yes” to questions asking whether or not they apply sodium-lowering behaviors and 0 when they answered “no”). Greater scores mean a higher probability that individuals were trying to reduce their sodium intake (ranges from 0 to 7). The data indicate that the mean value increased from 2.63 to 3.50 at 4 months after the interventions (P = 0.007). The factors related to providing healthier foods at their restaurants were improved by usage of a salimeter for checking sodium content when the participants served food; this improvement was significant at a level of 0.026.
Table 3. Pre- and post-measurements of behavioral and psychosocial factors regarding sodium intake among restaurants owners and cooks after health examination and a nutrition education session.
1) McNemar test
2) The percentages presented here counted the respondents who answered "yes".
3) The percentages presented here counted the respondents who answered "all the time" or "sometimes"/"strongly agree" or "agree".
4) Composite scores for each sodium-related behaviors: if answered positively to the 7 behaviors under nutrition behaviors, then received 1 point, if answered negatively to each behavior, then received 0 points (maximum possible score is 7 and minimum possible score is 0).
5) paired t-test
6) 4-point Likert scale responses were treated as ordinal variables to compare pre- and post-intervention (1 being the least beneficial for sodium intake and 4 being the most beneficial
DISCUSSION
This study demonstrated that short-term interventions aimed at increasing awareness of sodium intake among independent restaurants owners and cooks can improve nutritional behaviors and potentially practices in preparing foods at restaurants. Due to the limited scope of the pilot study, we did not reach statistical significance for certain measures. However, this study suggests that restaurant owners and cooks who are more aware of their dietary intake, specifically sodium intake, better perceived the necessity to provide healthy food to their customers.
Regarding efforts to lower a population's sodium intake [26], empirical data from independent restaurants are particularly scarce [10,24]. One study specifically targeted Chinese take-out restaurants in the US and demonstrated that most owners and chefs are willing to modify the sodium contents of their restaurant's foods [24]. This current study also revealed that a large portion of participants agreed with the necessity to improve cooking methods for customers and to lower sodium contents of their menus. For instance, 92% of participants “strongly agreed” or “agreed” with the statement “it is necessary to use healthy cooking methods or customers”.
This result illustrates that even before the intervention, most restaurant owners and cooks perceived the importance of sodium reduction for themselves as well as their customers. It can be assumed that the national campaign and public messages disseminated through the Korea Ministry of Food and Drug Safety over the past 4-5 years have affected key psychosocial factors of the participants [27].
However, our data demonstrate that although many participants agreed with the idea of providing healthier foods at their restaurants, their own nutritional behaviors exhibited much room for improvement (Table 3). Moreover, agreement with the idea of providing healthier options at their restaurants did not directly translate into actual modification of their cooking practices and recipes. A previous study conducted at worksite cafeterias reported many barriers to serving low-sodium menus [28], such as fear of losing customers and profits. This concern can be applicable to the restaurant settings evaluated in our study. Future studies should determine which strategies could work to lower known barriers.
Finally, poor health status and health behaviors among owners and cooks are worth noting. The prevalence of obesity and elevated blood pressure among this study group were much higher than among the general population (23.2% for obesity and 21.6% for hypertension among the adult population in Seoul) [29]. No previous study has highlighted the health status of food providers, and this study demonstrated that the owners and cooks of restaurants should be given special attention by public health authorities as a high-risk group. We can further hypothesize that improvement of these individuals' health behaviors, including sodium intake, can translate into actual reduction of sodium contents at their restaurants. This hypothesis should be tested in future studies.
Despite the implementation of new sodium reduction initiatives at local restaurants, this study has many limitations since it is a small-scale pilot study. First, only one district with a small numbers of volunteers in Seoul was evaluated, and we lacked a comparison group. Since single group intervention studies can pose various threats to internal validity, including testing bias [30], we need future intervention studies to confirm causal effects with a comparison group. Second, checking the sodium contents of foods provided at restaurants before and after intervention was beyond the scope of this research. Third, due to participants' busy schedules, we could not check their usual sodium intake levels using more accurate methods, such as 24-hour urine collection. We also understand the possibility of selection bias and social desirability bias in the survey responses. Fourth, we tried to keep the survey questionnaires short in order to minimize response burden and increase the response rate among busy restaurant personnel. However, we acknowledge the limited performance of measuring perception and self-efficacy of low-sodium restaurant initiatives using only one question each. Lastly, sub-group analyses are not presented in this paper. It would be meaningful to examine the differences in psychosocial and behavioral factors according to the type of restaurant and characteristics of the participants.
This small pilot study demonstrated that working with restaurant owners and cooks to improve their own health and sodium intake may have an effect on participation in restaurant-based sodium reduction initiatives. Much more research is needed to confirm this hypothesis; however, given the urgency of reducing sodium intake, considering restaurant personnel as both intervention providers and intervention recipients may broaden the spectrum of sodium reduction strategies.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the study participants and the Association of Business Owners in Guro District in Seoul.
Footnotes
This work was supported by the District Office of Guro-gu in Seoul, South Korea. The Public Health Center in Guro-gu helped the research team recruit participants of this study, design the program, and draft this manuscript. Dr. Sohyun Park's efforts in the study was supported in part by a post-doctoral fellowship from the National Research Fund in the Republic of Korea (2015S1A5B5A01014062) and the research grant from Hallym University (H20160079). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
CONFLICT OF INTEREST: The authors declare no potential conflicts of interests.
References
- 1.Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANES VI-1) Cheongju: Korea Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 3.Lee KS, Park JH. Burden of disease in Korea during 2000-10. J Public Health (Oxf) 2014;36:225–234. doi: 10.1093/pubmed/fdt056. [DOI] [PubMed] [Google Scholar]
- 4.Kwon YS, Ju SY. Trends in nutrient intakes and consumption while eating-out among Korean adults based on Korea National Health and Nutrition Examination Survey (1998-2012) data. Nutr Res Pract. 2014;8:670–678. doi: 10.4162/nrp.2014.8.6.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park HR, Jeong GO, Lee SL, Kim JY, Kang SA, Park KY, Ryou HJ. Workers intake too much salt from dishes of eating out and food service cafeterias; direct chemical analysis of sodium content. Nutr Res Pract. 2009;3:328–333. doi: 10.4162/nrp.2009.3.4.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon YS, Park YH, Choe JS, Yang YK. Investigation of variations in energy, macronutrients and sodium intake based on the places meals are provided: using the Korea National Health and Nutrition Examination Survey (KNHANES, 1998-2009) Nutr Res Pract. 2014;8:81–93. doi: 10.4162/nrp.2014.8.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Appel LJ, Frohlich ED, Hall JE, Pearson TA, Sacco RL, Seals DR, Sacks FM, Smith SC, Jr, Vafiadis DK, Van Horn LV. The importance of population-wide sodium reduction as a means to prevent cardiovascular disease and stroke: a call to action from the American Heart Association. Circulation. 2011;123:1138–1143. doi: 10.1161/CIR.0b013e31820d0793. [DOI] [PubMed] [Google Scholar]
- 8.Geaney F, Harrington J, Fitzgerald A, Perry I. The impact of a workplace catering initiative on dietary intakes of salt and other nutrients: a pilot study. Public Health Nutr. 2011;14:1345–1349. doi: 10.1017/S1368980010003484. [DOI] [PubMed] [Google Scholar]
- 9.Perlmutter CA, Canter DD, Gregoire MB. Profitability and acceptability of fat- and sodium-modified hot entrees in a worksite cafeteria. J Am Diet Assoc. 1997;97:391–395. doi: 10.1016/S0002-8223(97)00097-7. [DOI] [PubMed] [Google Scholar]
- 10.Schuldt J, Levings JL, Kahn-Marshall J, Hunt G, Mugavero K, Gunn JP. Reducing sodium across the board: a pilot program in Schenectady County independent restaurants. J Public Health Manag Pract. 2014;20:S31–S37. doi: 10.1097/PHH.0b013e31829d7b7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco (CA): Jossey-Bass; 2008. [Google Scholar]
- 12.Sharifirad G, Entezari MH, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. J Res Med Sci. 2009;14:1–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Abood DA, Black DR, Feral D. Nutrition education worksite intervention for university staff: application of the health belief model. J Nutr Educ Behav. 2003;35:260–267. doi: 10.1016/s1499-4046(06)60057-2. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Social Foundations of Thought and Action: a Social Cognitive Theory. Englewood Cliffs (NJ): Prentice-Hall; 1986. [Google Scholar]
- 15.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 2007;13:623–649. [Google Scholar]
- 16.Miller CK, Edwards L, Kissling G, Sanville L. Nutrition education improves metabolic outcomes among older adults with diabetes mellitus: results from a randomized controlled trial. Prev Med. 2002;34:252–259. doi: 10.1006/pmed.2001.0985. [DOI] [PubMed] [Google Scholar]
- 17.Rinderknecht K, Smith C. Social cognitive theory in an after-school nutrition intervention for urban native American youth. J Nutr Educ Behav. 2004;36:298–304. doi: 10.1016/s1499-4046(06)60398-9. [DOI] [PubMed] [Google Scholar]
- 18.Allen CL, Hammerback K, Harris JR, Hannon PA, Parrish AT. Feasibility of workplace health promotion for restaurant workers, Seattle, 2012. Prev Chronic Dis. 2015;12:E172. doi: 10.5888/pcd12.150093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Minkler M, Lee PT, Tom A, Chang C, Morales A, Liu SS, Salvatore A, Baker R, Chen F, Bhatia R, Krause N. Using community-based participatory research to design and initiate a study on immigrant worker health and safety in San Francisco's Chinatown restaurants. Am J Ind Med. 2010;53:361–371. doi: 10.1002/ajim.20791. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization Western Pacific Region; International Association for the Study of Obesity; International Obesity Task Force. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Sydney: Health Communications Australia Pty Limited; 2000. pp. 1–56. [Google Scholar]
- 21.Luft FC, Fineberg NS, Sloan RS. Overnight urine collections to estimate sodium intake. Hypertension. 1982;4:494–498. doi: 10.1161/01.hyp.4.4.494. [DOI] [PubMed] [Google Scholar]
- 22.Tochikubo O, Sasaki O, Umemura S, Kaneko Y. Management of hypertension in high school students by using new salt titrator tape. Hypertension. 1986;8:1164–1171. doi: 10.1161/01.hyp.8.12.1164. [DOI] [PubMed] [Google Scholar]
- 23.Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. 2014 Korea Community Health Survey: Survey Questionnaires. Cheongwon: Korea Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 24.Ma GX, Shive S, Zhang Y, Aquilante J, Tan Y, Zhao M, Solomon S, Zhu S, Toubbeh J, Colby L, Mallya G, Zeng Q. Knowledge, perceptions, and behaviors related to salt use among Philadelphia Chinese take-out restaurant owners and chefs. Health Promot Pract. 2014;15:638–645. doi: 10.1177/1524839914538816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shin EK, Lee HJ, Ahn MY, Lee YK. Study on the development and evaluation of validity of salty taste assessment tool. Korean J Nutr. 2008;41(2):184–191. [Google Scholar]
- 26.Webster JL, Dunford EK, Hawkes C, Neal BC. Salt reduction initiatives around the world. J Hypertens. 2011;29:1043–1050. doi: 10.1097/HJH.0b013e328345ed83. [DOI] [PubMed] [Google Scholar]
- 27.Ministry of Food and Drug Safety (KR) Decreasing sodium intake level by 20% by 2017 [Internet] Cheongju: Ministry of Food and Drug Safety; 2016. [cited 2016 September 5]. Available from: http://www.mfds.go.kr/index.do?x=0&searchkey=title:contents&mid=675&searchword=%B3%AA%C6%AE%B7%FD&y=0&pageNo=4&seq=22795&cmd=v. [Google Scholar]
- 28.Park S, Lee J. 'When operating a cafeteria, sales come before nutrition'-finding barriers and facilitators to serving reduced-sodium meals in worksite cafeterias. Public Health Nutr. 2016;19:1506–1516. doi: 10.1017/S1368980015002827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Results from the National Community Health Survey 2014. Cheongju: Korea Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 30.Krauth J. Experimental Design: a Handbook and Dictionary for Medical and Behavioral Research. New York (NY): Elsevier; 2000. [Google Scholar]