Case Report
A 41-year-old man with a history of metastatic medullary thyroid cancer presented with stridor, odynophagia, and dysphagia, worsening abruptly over the past 2 days. He had a moderate degree of dysphagia even at baseline secondary to a radiation-induced esophageal stricture, and previously had multiple esophagogastroduodenoscopies (EGDs) with dilation, most recently a year prior to presentation. He had also undergone a complete thyroidectomy and received radioactive iodine and radiation therapy. His clinical course had been complicated by cervical and thoracic cord compression from bone metastases requiring corpectomy, laminectomy, and instrumented vertebral fusion.
On admission, he was hemodynamically stable and did not exhibit tachypnea or hyperpnoea. Routine labs on admission, including a complete metabolic panel and a complete blood count, were within normal limits. Flexible laryngoscopy of the vocal cords showed mild right-sided vocal cord immobility (known on previous exams) with mild edema in the arytenoid and interarytenoid mucosa, which initially improved with dexamethasone and racemic epinephrine. Given his hemodynamic stability and low suspicion for infection, antibiotics were not given.
Computed tomography scans of the neck with contrast revealed a lucency surrounding the anterior reconstruction plate fixation screw consistent with its migration, but no airway impingement (Figure 1). On fluoroscopy, the foreign body corresponded to the previously placed neck hardware and demonstrated that the entire upper cervical esophagus had been obscured by the cervical hardware (Figure 2). The barium esophagogram ruled out esophageal leakage, but a complete evaluation by fluoroscopy was limited by the patient’s intolerance to bolus drinking and inability to swallow the barium tablet. Diagnostic EGD revealed a metallic foreign body perforating the posterior wall of the esophagus, just below the known stricture (Figure 3). The patient developed recurrent stridor, and repeat laryngoscopy showed bilateral vocal cord paresis, likely secondary to local inflammation from the hardware and post-radiation changes. The patient underwent revision cervical spine surgery with hardware removal and replacement and pectoralis flap reconstruction of the posterior pharynx and esophagus, tracheostomy, and a temporizing surgical gastrostomy tube placement, prior to being discharged (Figure 4).
Figure 1.
Computed tomography scans of the cervical spine with one end of the cervical hardware in the esophageal lumen (arrow).
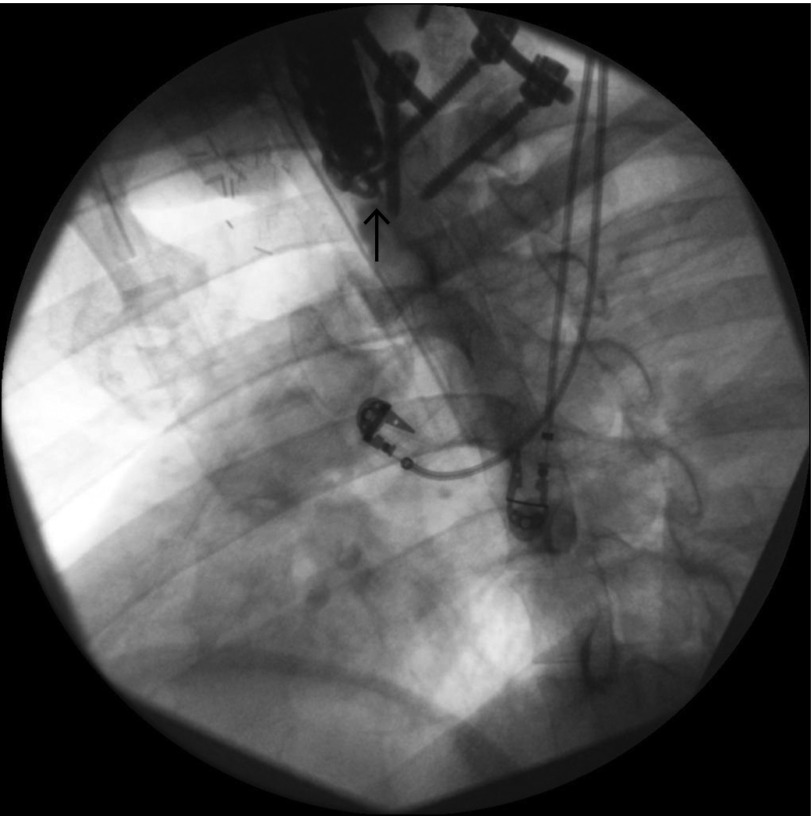
Figure 2.
Esophagogram demonstrating that the entire upper cervical esophagus is obscured by the cervical hardware (arrow).
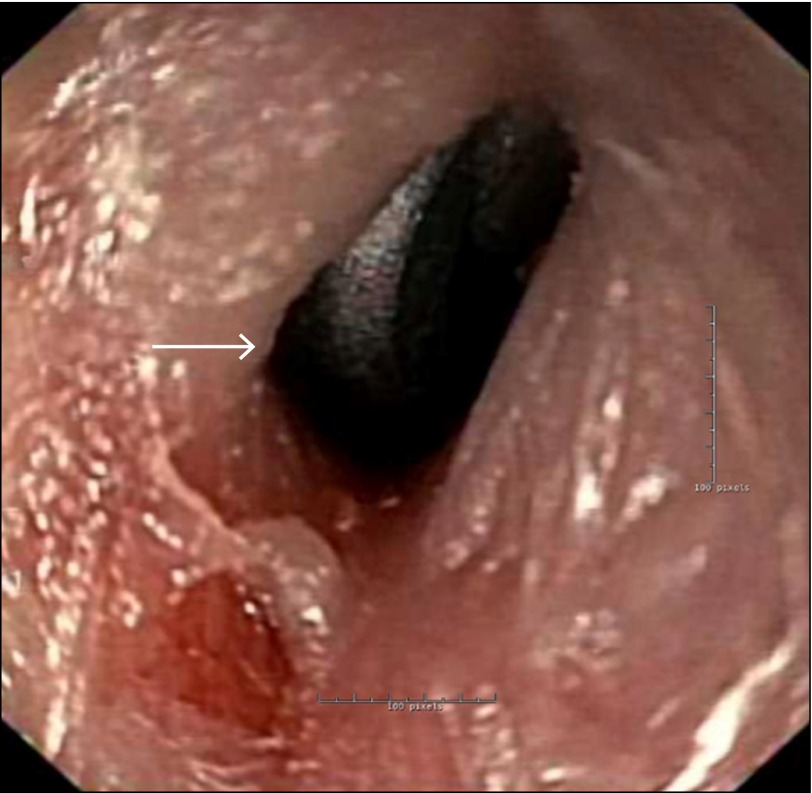
Figure 3.
Metallic cervical hardware seen perforating the posterior wall of the esophagus during EGD (arrow).
Figure 4.

Revision cervical spine surgery with hardware removal, replacement, and pectoralis flap reconstruction of the posterior pharynx and esophagus.
After surgery, the patient was allowed to eat by mouth, but primarily received nutrition through his gastrostomy tube. At 3 months he was weaned from tube feeding and the patient had returned to normal oral intake at 7 months. The transition to normal oral intake was delayed by postoperative neck pain and radiation-induced esophageal strictures requiring dilation. Fortunately, his postsurgical course was relatively uneventful, and the area of the perforation healed appropriately as seen on subsequent EGDs. Unfortunately, the patient required 5 EGDs in the 8 months since surgery for Savary-guided dilation of radiation-induced esophageal strictures in other areas of his esophagus. He still had a tracheostomy, and plans for the tracheostomy reversal with cordotomy were discussed at his last outpatient visit.
While migration and erosion of cervical surgical hardware into the esophageal lumen is extremely rare, cases have been reported up to 9 years after surgery.1 Transient dysphagia (not related to esophageal injury) following anterior cervical spine surgery can be seen at up to 2 years after surgery in 57% of cases,2 but persistent or worsening esophageal symptoms should prompt repeat investigations to rule out hardware migration and esophageal erosion. Although radiation exposure has been known to cause esophageal strictures, cervical hardware migration secondary to radiation is not known. Revision cervical spine surgery and myofascial repair are the standard of care for this condition.3
Disclosures
Author contributions: All authors contributed equally to the creation of the manuscript. A. Bhatt is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Lu DC, Theodore P, Korn WM, Chou D. Esophageal erosion 9 years after anterior cervical plate implantation. Surg Neurol. 2008; 69(3):310–2. [DOI] [PubMed] [Google Scholar]
- 2.Nathani A, Weber AE, Wahlquist TC, et al. . Delayed presentation of pharyngeal erosion after anterior cervical discectomy and fusion. Case Rep Orthop. 2015; 2015:173687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davison SP, Yoder BE, Boehmler JH. Repairing esophageal perforations with a transverse cervical musculofascial flap. Ann Plast Surg. 2006; 57(2):164–8. [DOI] [PubMed] [Google Scholar]