Abstract
Celiac crisis is a rare presentation of celiac disease that is characterized by life-threatening electrolyte abnormalities, vitamin and mineral deficiencies, and diarrhea. Triggers for celiac crisis include major surgeries, pancreatitis, and infections of cytomegalovirus, and salmonella. A 24-year-old woman presented with celiac crisis associated with severe herpes simplex virus (HSV) esophagitis. This case demonstrates that nutritional deficiencies seen in celiac disease can result in a relative immunodeficiency, which may lead to other infectious complications. Additionally, early recognition of celiac crisis is imperative as the metabolic derangements may be life-threatening, and therapy with gluten restriction and nutritional repletion is effective.
Introduction
Celiac disease is an immune-mediated enteropathy triggered by gluten proteins that causes mucosal inflammation, crypt hyperplasia, and villous atrophy. This injury to the small intestine leads to malabsorption of nutrients.1 Patients usually also have weight loss, diarrhea, abdominal pain, and bloating. Celiac disease is almost always an indolent disease that causes chronic gastrointestinal (GI) symptoms and nutritional abnormalities. In very rare cases, however, it can present in an acute form characterized by life-threatening diarrhea, dehydration, and metabolic abnormalities of hypokalemia, hyponatremia, hypocalcemia, hypomagnesemia, and hyoproteinemia. This severe form of celiac disease is called celiac crisis, a term first used in the literature in 1953 when Andersen and Di Sant’ Agnese described 58 children with celiac disease, of which 35 presented with celiac crisis.2 They showed a 9% mortality in children with celiac crisis.3
Case Report
A 24-year-old white woman with no significant past medical or surgical history presented to the hospital with 8 days of profuse watery diarrhea. She reported 6–8 loose watery bowel movements per day, mild cramping abdominal pain, nausea, vomiting, heartburn symptoms, odynophagia, fatigue, and a 4.5-kg weight loss over the week leading up to presentation. She denied any laxative use, weight loss pills, recent travel, camping, swimming, unusual food, antibiotic use, sick contacts, or day-care exposure. Her only medication was the birth control pill Loestrin 24 Fe (norethindrone acetate, ethinyl estradiol, and ferrous sulfate). Her family history was unremarkable. She never smoked tobacco, only used alcohol occasionally, and did not use recreational drugs. Her vital signs on admission showed tachycardia, with a heart rate of 113 bpm, but was otherwise normal. Her body mass index was underweight at 17.5 kg/m2. On physical exam, she appeared thin, alert and oriented, and in no acute distress. Her abdomen was soft, non-tender, non-distended, and she had normal bowel sounds, no masses, and no hepatosplenomegaly. She had no thyromegaly, and the rest of the physical exam was normal.
Initial blood chemistry showed hyponatremia with sodium 125 mmol/L, hypokalemia with potassium 2.4 mmol/L, hypochloremia with chloride 94 mmol/L, and anion gap acidosis 14 mmol/L. Complete blood count showed a microcytic anemia with hemoglobin 9.3 g/dL and mean corpuscular volume <60 fL. The reticulocyte index was <1.1%, indicating underproduction. Iron studies were consistent with severe iron deficiency anemia, with ferritin 1 ng/mL. Vitamin B12 and folic acid levels were normal. Stool studies and cultures were all negative, including tests for Clostridium difficile polymerase chain reaction, Salmonella, Shigella, Yersinia, Campylobacter, E. coli, Giardia lamblia, Entamoeba histolytica, and Cryptosporidium parvum. Fecal leukocytes and lactoferrin were negative. Liver function test and thyroid function tests were normal. Human immunodeficiency virus (HIV) antibodies were negative. Coagulopathy was present with an international normalized ratio elevated at 3.2. Her tissue transglutaminase (TTG) IgA antibody was markedly elevated at 99 U/mL.
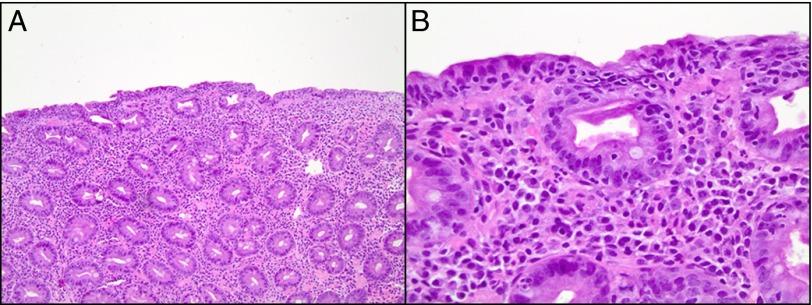
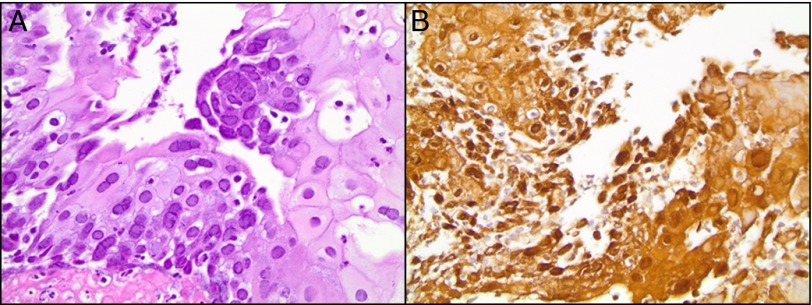
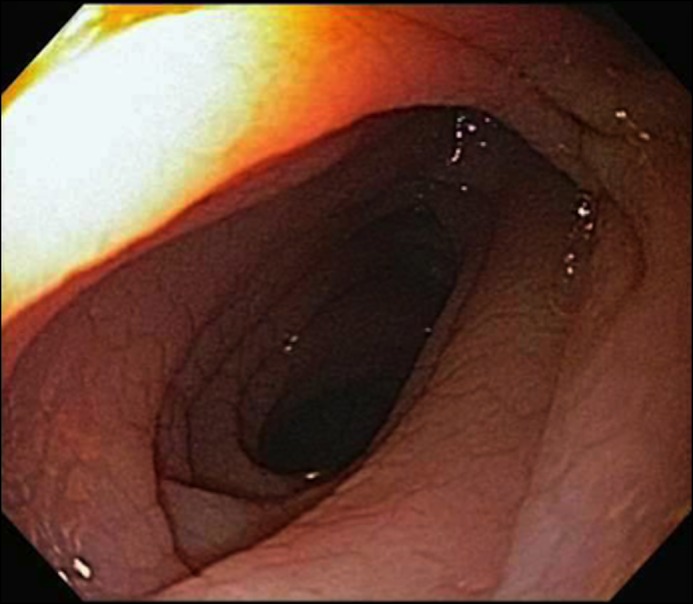
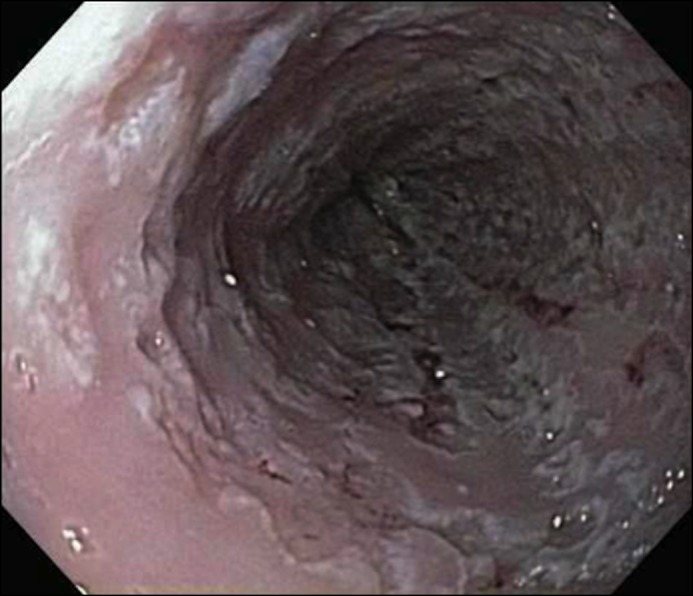
Upper endoscopy demonstrated diffuse cobblestoning and scalloping of the duodenal mucosa (Figure 1). Duodenal biopsies showed a totally flat mucosa and markedly increased intraepithelial lymphocytes and plasma cells in the lamina propria consistent with modified Marsh 3c classification (Figure 2). Upper endoscopy also demonstrated severe ulcerative esophagitis throughout the entire esophagus (Figure 3). Esophageal biopsies revealed acute esophagitis with herpes simplex virus (HSV) cytopathic effect, with multinucleation and characteristic ground-glass nuclear inclusions and positive for HSV immunohistochemical stain (Figure 4). The colonoscopy was normal.
Figure 1.
Upper endoscopy showing duodenal mucosa with diffuse cobblestoning and scalloping.
Figure 2.
Hematoxylin and eosin staining of small intestinal biopsy showing (A) totally flat mucosa consistent with modified Marsh 3c classification (100x) and (B) markedly increased intraepithelial lymphocytes and plasma cells in lamina propria (400x).
Figure 3.
Upper endoscopy showing severe ulcerative esophagitis throughout the entire esophagus.
Figure 4.
(A) Hematoxylin and eosin staining of esophageal biopsy showing HSV cytopathic effect with multinucleation and characteristic ground-glass nuclear inclusions (400x). (B) Immunohistochemical staining of esophageal biopsy showing positive HSV (400x).
The diagnosis of celiac crisis was made on the basis of serologic and pathologic findings consistent with celiac disease in the setting of severe and life-threatening metabolic abnormalities and malnutrition. She was placed on a gluten-free diet and treated with aggressive repletion of fluids, electrolytes, vitamin K, vitamin D, and iron. Her symptoms improved gradually over 8 days in the hospital. Blood chemistry and coagulation studies normalized by the day of discharge. For the HSV esophagitis, she was treated with oral acyclovir and a proton pump inhibitor (PPI). At primary care follow up 2 months after discharge, she was doing well and was asymptomatic. Recheck of labs at that time showed that the TTG IgA antibody had drastically decreased to 11 U/mL. Her complete blood count, blood chemistry, iron studies, and vitamin D level were normal as well.
Discussion
Since the first reports of celiac crisis in 1953, there has been very little literature on this presentation other than infrequent case reports. In 1972, Lloyd-Still et al. showed through treatment of 3 children that corticosteroids can be used in celiac crisis to induce a dramatic clinical response.4 Celiac crisis is fairly rare in adults. In 2010, Jamma et al. described the largest number of adults with celiac crisis in a case series of 12 patients from two referral centers.5 They defined celiac crisis as an acute onset or rapid progression of GI symptoms attributable to celiac disease requiring hospitalization and/or parenteral nutrition along with at least 2 objective signs of malnutrition, dehydration, or electrolyte disturbance.5 Their data estimated an incidence of less than 1% for celiac crisis in patients with celiac disease. All of the patients had confirmed celiac disease with serology and small bowel biopsy. The patients presented with electrolyte abnormalities, renal insufficiency, and dehydration. They required invtravenous fluids and hospitalization, and 6 patients required corticosteroids. Only 1 patient had a prior known diagnosis of celiac disease, and he was not following a gluten-free diet. All 12 patients had a full response to a gluten-free diet.5
It is unknown why most patients with celiac disease present with an indolent disease, whereas a small subset of patients present with an acute life-threatening form. Interestingly, a general immune stimulus such as infection, surgery, or pregnancy may precipitate celiac crisis.5 The report by Jamma et al. showed that 5 of their 12 patients had a major medical event before their crisis.5 Infections associated with celiac crisis described in the literature are sparse. Salmonella infantis isolated from blood and stool was reported in one case report of celiac crisis.4 Another case report showed celiac crisis presenting with cytomegalovirus hepatitis and postulated that the immunosuppression in celiac disease was related to functional hyposlenism, malnutrition, and a decreased number circulating T cells.6-8
We present the first case of celiac crisis likely precipitated by HSV esophagitis reported in the literature. HSV esophagitis typically occurs in immunocompromised patients, such as solid organ and bone marrow transplant recipients on immunosuppression, or in patients with other immunocompromised states, such as patients with AIDS. It has also been described rarely in immunocompetent patients in case reports. Although difficult to demonstrate causality, we postulate that this patient’s severe HSV esophagitis likely precipitated her celiac crisis, in the setting of previously undiagnosed celiac disease. It is likely that her underlying celiac disease and severe nutritional deficiencies resulted in a relative immunodeficient state, which led to HSV esophagitis infection. Fortunately, the patient improved with acyclovir, PPI, and a gluten-free diet, and at her 2-month follow-up visit her symptoms had resolved. At her 3-month follow-up visit, she had gained 19 pounds, and her body mass index was in the normal range.
Disclosures
Author contributions: All authors contributed equally to the creation of the manuscript. A. Chen is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Rubio-Tapia A, Hill ID, Kelly CP, et al. . ACG clinical guidelines: Diagnosis and management of celiac disease. Am J Gastroenterol. 2013; 108(5):656–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersen DH, Di Sant'Agnese PA. Idiopathic celiac disease. I. Mode of onset and diagnosis. Pediatrics. 1953; 11(3):207–23. [PubMed] [Google Scholar]
- 3.Di Sant'Agnese PA. Idiopathic celiac disease. II. Course and prognosis. Pediatrics. 1953; 11(3):224–37. [PubMed] [Google Scholar]
- 4.Lloyd-Still JD, Grand RJ, Khaw KT, Shwachman H. The use of corticosteroids in celiac crisis. J Pediatr. 1972; 81(6):1074–81. [DOI] [PubMed] [Google Scholar]
- 5.Jamma S, Rubio-Tapia A, Kelly CP, et al. . Celiac crisis is a rare but serious complication of celiac disease in adults. Clin Gastroenterol Hepatol. 2010; 8(7):587–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly E, Cullen G, Aftab AR, Courtney G. Coeliac crisis presenting with cytomegalovirus hepatitis. Eur J Gastroenterol Hepatol. 2006; 18(7):793–5. [DOI] [PubMed] [Google Scholar]
- 7.Marsh GW, Stewart JS. Splenic function in adult coeliac disease. Br J Haematol. 1970; 19(4):445–57. [DOI] [PubMed] [Google Scholar]
- 8.O'Donoghue DP, Lancaster-Smith M, Laviniere P, Kumar PJ. T cell depletion in untreated adult coeliac disease. Gut. 1976; 17(5):328–31. [DOI] [PMC free article] [PubMed] [Google Scholar]