Abstract
BACKGROUND AND OBJECTIVES:
The underlying influences on different patterns of BMI development are not well understood, and psychosocial outcomes linked to BMI development have been little investigated. Objectives were to identify BMI developmental trajectories across the first decade of life, examine early life predictors of trajectory membership, and investigate whether being on a particular BMI trajectory is associated with markers of psychosocial well-being.
METHODS:
We used latent class analysis to derive BMI trajectories by using data collected at ages 3, 5, 7, and 11 years on 16 936 participants from the Millennium Cohort Study. Regression models were used to estimate predictors of BMI trajectory membership and their psychosocial correlates.
RESULTS:
Four trajectories were identified: 83.8% had an average “stable” nonoverweight BMI, 0.6% were in a “decreasing” group, 13.1% had “moderate increasing” BMIs, and 2.5% had “high increasing” BMIs. Predictors of “moderate” and “high” increasing group membership were smoking in pregnancy (odds ratios [ORs] = 1.17 and 1.97, respectively), maternal BMI (ORs = 1.10 and 1.14), skipping breakfast (ORs = 1.66 and 1.76), nonregular bedtimes (ORs = 1.22 and 1.55). Children in the “moderate” and “high” increasing groups had worse scores for emotional symptoms, peer problems, happiness, body satisfaction, and self-esteem, and those in the “high increasing” group were more likely to have tried alcohol and cigarettes.
CONCLUSIONS:
Several potentially modifiable early life factors including smoking in pregnancy, skipping breakfast, and bedtime routines were important predictors of BMI development in the overweight and obese range, and high BMI growth was linked to worse psychosocial well-being.
What’s Known on This Subject:
Distinct patterns of BMI development exist over the childhood years.
What This Study Adds:
Several potentially modifiable early life factors are linked to BMI growth patterns in the overweight and obese range through childhood. BMI growth trajectories in the overweight and obese range through childhood are associated with worse psychosocial well-being in early adolescence.
Overweight and obesity are linked to health throughout the life course. A growing body of research suggests the existence of distinct BMI development trajectories through childhood.1–12 Previous studies have identified 3 broad types of trajectories: a majority group with “healthy” BMI throughout childhood, groups who develop BMI in the overweight range at some point during childhood, and those with BMI in the overweight or obese range throughout childhood.1–6 Underlying influences on different patterns of BMI development are not well understood, but factors reported to predict childhood BMI trajectories include mother’s BMI,1,3,5,6,8,10,11 smoking during pregnancy,1,5,6 and sociodemographic background.1–5,12 Previous work suggests that a range of early life factors including infant feeding, diet, physical activity, and family routines are associated with child overweight and obesity.13 However, comparison of study findings is often hampered for 2 main reasons. The first is differences in study design used, such as representative population1–6 versus convenience samples.7–9 Second, studies often consider different potential influences for BMI growth, overweight, or obesity.
Apparent links between overweight and obesity and psychosocial well-being exist, although the direction of association is not clear, and may be bidirectional. Several studies indicate that early psychosocial stress and adverse family environments are associated with an elevated risk of obesity,14–17 and many others suggest that being overweight or obese is linked to elevated risks of poor psychosocial well-being, including low self-esteem and depressive symptoms.16,17 One previous study examined BMI development trajectories and adolescent psychosocial well-being and showed that the exploration of risky behaviors such as tobacco smoking was more common for those who were obese throughout childhood.18 Given that healthy development early in life has long-lasting consequences, improving our understanding of the factors influencing BMI development, and of how particular BMI trajectories relate to markers of well-being, could have important implications for health throughout the life course.
To our knowledge this is the first article that uses nationally representative data from the UK to address the following research objectives:
Identify BMI developmental trajectories across the first decade of life. We derive trajectories empirically by using latent class analysis to group subject with similar patterns of BMI development. We hypothesize there will be distinct BMI growth trajectories, including BMI growth patterns in the overweight and obese range, and a nonoverweight trajectory.
Examine early life predictors of trajectory membership. We hypothesize that some factors, including cigarette smoking, factors linked to family routines including skipping breakfast and nonregular bedtimes, delayed infant motor development, low levels of physical activity, and dietary indicators such as low fruit consumption and intake of sugary drinks, will increase the risk of having BMI growth in the overweight and obese range, whereas breastfeeding will have a protective role.
Investigate whether BMI trajectory membership is associated with markers of psychosocial well-being, including socioemotional difficulties, self-esteem, happiness, and risky behaviors in early adolescence. Here, we hypothesize that having BMI growth in the overweight or obese range will correlate with poorer psychosocial well-being, an umbrella term that here encompasses socioemotional difficulties, low self-esteem, unhappiness, and risky behaviors such as cigarette smoking and alcohol consumption.
Methods
Participants
Data were from the first 5 sweeps of the UK Millennium Cohort Study, a prospective study of children born into 19 244 families, sampled from all live births in the United Kingdom between September 2000 and January 2002.19 The first sweep of data was collected when cohort members were ∼9 months old, and the subsequent 4 sweeps of data were collected at ages 3, 5, 7, and 11 years. We used data from the latter 4 sweeps (ages 3, 5, 7, and 11 years) to estimate trajectories of BMI development.
A total of 17 601 families participated in at least 1 of the 4 sweeps, of which 245 multiple births (234 sets of twins and 11 sets of triplets) were excluded from analysis. Another 186 participants had no BMI data at any sweep and were excluded from our analyses. After we dealt with outlier BMI values (described below), there were 14 205, 14 790, 13 457, and 12 697 participants with BMI data at sweeps 2 to 5, respectively. A total of 16 936 participants were included in the trajectory analysis, of whom 9523 (56.2%) had data in all 4 sweeps, 3810 (22.5%) in any 3, 2024 (12.0%) in any 2, and the remaining 1579 (9.3%) in 1 sweep.
BMI
At ages 3, 5, 7, and 11 years children were weighed and had their height measured without shoes or outdoor clothing. Weights in kilograms to 1 decimal place and heights to the nearest millimeter were recorded.20 These measures were used to calculate BMI. Values were considered to be outliers if BMI was <10 or >50, resulting in 6, 0, 3, and 5 values from each of sweeps 2 to 5 being removed, respectively. Mean (SD) values at each sweep were 16.5 (2.1), 16.4 (1.9), 16.7 (2.4), and 19.3 (3.7).
Sociodemographic Characteristics
Cohort members were classified into 7 groups based on their ethnicity as reported by their mothers: white, Indian, Pakistani, Bangladeshi, black Caribbean, black African, and other.21 Household income was categorized into equivalized quintiles. Occupational class was indicated according to the standard National Statistics Socioeconomic Classification 3-group categorization (higher managerial, administrative, and professional; intermediate; and routine and manual; with an additional category, never worked and long-term unemployed). Highest maternal education attained at sweep 1 was grouped into 6 categories: higher education including degree or professional diploma or higher; Advanced Levels [A-levels], which are UK school leaving examinations taken at age 17 to 18 years; General Certificate of Secondary Education [GCSEs], which are UK school examinations at age 15 to 16 years, broken down into A–C grades and D–G grades; other qualifications including overseas qualifications; and none).
Pregnancy and Infancy Factors
Health-related behaviors during and after pregnancy that were included were whether the mother smoked during pregnancy, ever breastfed the child, and introduced solid foods before 4 months of age. Motor delay in infancy (9 months) was estimated based on delay compared with the rest of the cohort in any key motor skills (sitting, crawling, and standing).22
Early Childhood Factors
Mother’s BMI at age 3 (sweep 2) was estimated from self-reported height and weight. Early childhood factors included markers of diet, physical activity, and sleep at age 5 years. Dietary factors were whether the child drank mainly sugary drinks (eg, cola, milkshakes, fruit juice) in between meals, ate <3 portions of fruit a day, and regularly skipped breakfast. Sports participation (less than once per week) was included as a marker of physical activity. Television viewing for >3 hours a day was included as a marker of sedentary behavior. Whether the cohort member had a regular bedtime and, if so, whether this bedtime was late (9 pm or later at age 5 years) were included as markers of sleep.
Psychosocial Well-Being Outcomes
At age 11, markers of psychosocial well-being included socioemotional difficulties and skills (as indicated by the parent-reported Strengths and Difficulties Questionnaire23), including emotional symptoms, conduct problems, hyperactivity, peer problems, and prosocial behavior. Higher emotional symptoms, conduct problems, hyperactivity, and peer problem scores indicate more difficulties, whereas high prosocial scores indicate better outcomes. Cohort members themselves reported on antisocial activity (stealing, being noisy or rude in public spaces, damaging public property), exploratory health behaviors (ever having smoked cigarettes and ever having drank alcohol), self-esteem (as indicated by the Rosenberg self-esteem scale, with lower scores indicating worse outcomes),24 and happiness (as indicated by a 6-item measure of “happiness” with school work, appearance, family, friends, school, and life as a whole, with responses to each item on a 7-point scale from completely happy to not at all happy, α = 0.83).25 Additionally, the marker of body satisfaction (happiness with appearance) from the happiness scale was examined as a separate item.
Analysis
Trajectories of BMI development were identified via Latent Class Growth Analysis in Mplus,26 with full information maximum likelihood estimation to account for missing BMI data at any time point. The selection of the number of trajectories to explore in additional analyses was based on a range of criteria including model comparison (Lo–Mendell–Rubin likelihood ratio test, likelihood ratio difference), improvement in information criteria (Akaike information criterion, adjusted Bayesian information criterion [A-BIC]), neatness of classification (entropy index), and theoretical interest.27,28 The 4-trajectory model was chosen for additional analysis (A-BIC plot indicated a clear flattening of A-BIC subsequent to the 4-trajectory model, entropy of 0.88 suggested satisfactory neatness of classification, likelihood ratio difference indicated highly significant improvement in model fit [P < .001], and Lo–Mendell–Rubin likelihood ratio test indicated that 4- versus 3-class was an improvement [P < .10], whereas ≥5-class was not [P > .50]).
Once trajectories had been derived, in the next stage, multiple imputation was carried out to ensure that no data were excluded in analysis because of missingness on the predictors of interest while also maintaining the survey structure in the data. During imputation the trajectory group of subjects was also included alongside all the other covariates to inform the imputation. Overall, 14.6% of data points across the entire sample, including the sociodemographic, infancy, childhood, and age 11 outcome variables, were missing. The proportion of data missing varied by variable; for example, no cases were missing for gender, 0.1% were missing for income, and 0.6% were missing for ethnicity (not imputed) on the lower end, and 28.5% were missing for the Strengths and Difficulties Questionnaire and 29.6% were missing for self-esteem at age 11 years on the higher end. Missingness on markers of psychosocial well-being was consistently lowest for subjects in the “moderate increasing” BMI group (average missing 18.9%), followed by the “stable” group (average missing 28.7%), and the “high increasing” BMI group (average missing 30.2%), and the highest missingness was observed in children in the smallest group, with decreasing BMI over childhood (average missing 35.8%).
Guided by best practice,29 we carried out 25 imputations and used them in subsequent analysis. Supplemental Table 4 provides information on the nonimputed and imputed descriptive statistics for all variables in the study.
Predictors of membership to different trajectory groups were investigated via multivariate multinomial logistic regressions comparing the decreasing and increasing trajectories to the reference group (the largest, “stable” trajectory). Psychosocial outcomes at age 11 (socioemotional difficulties and skills, antisocial behaviors, exploratory risky behaviors, self-esteem, and happiness) were examined by trajectory group to ascertain whether different trajectories were associated with different outcomes. Sociodemographic variables were adjusted for in these analyses, and we present odds ratios for potential predictors that are independent of all factors. In addition, we carried out sensitivity analysis for participants with data on markers of puberty, but this analysis did not alter estimates and is not reported.
Results
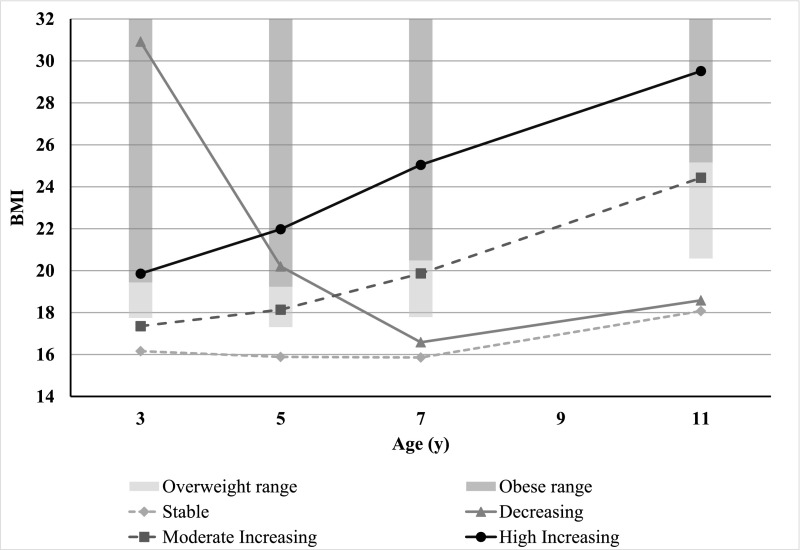
Of the 16 936 participants with BMI data in any of the sweeps, 48.8% (n = 8259) were girls. Most of the sample (83.8%) had an average nonoverweight BMI (the “stable” trajectory). The smallest decreasing trajectory group (0.6%) had BMIs in the obese range at age 3 but were similar to the stable group by age 7. The “moderate increasing” group (13.1%) had average BMIs in the nonoverweight range at age 3 and subsequent average BMIs that increased throughout the rest of childhood into the overweight but not obese range. The “high increasing” trajectory (2.5%) had average BMIs in the obese range at age 3, and their BMIs continued to increase throughout childhood (Fig 1).
FIGURE 1.
Average BMI for each of the identified trajectories at ages 3, 5, 7, and 11 years. Overweight and obese ranges use International Obesity Task Force (IOTF) age specific cut points.
What Factors Predict BMI Trajectory Membership?
Table 1 shows the distribution of predictor variables by BMI trajectory group. Fully adjusted estimates, simultaneously taking account of all variables, are shown in Table 2. Sociodemographic variations in trajectory membership were seen. Girls were more likely to be in the “moderate increasing” group (odds ratio [OR] = 1.36) and less likely to be in the “decreasing” trajectory (OR = 0.44). Indian, Pakistani, and black African children were significantly more likely to have a “moderate increasing” trajectory (ORs = 1.66, 1.29, and 2.01, respectively), and Pakistani, black Caribbean, and black African children were more likely to belong to the “high increasing” group (ORs = 1.83, 3.44, and 3.39, respectively). Compared with cohort members in the affluent income quintile, those in the other 4 income groups had higher odds of being in the “moderate increasing” BMI group. Low maternal educational attainment compared with degree or higher levels predicted membership of increasing trajectories (GCSE grades A–C and D–G “moderate increasing” ORs = 1.32 and 1.42, respectively; GCSE grades A–C and no qualifications “high increasing” ORs = 1.79 and 1.74, respectively).
TABLE 1.
Distribution of Predictor and Outcome Variables by Derived BMI Trajectories
| Stable | Decreasing | Moderate Increasing | High Increasing | Overall | |
|---|---|---|---|---|---|
| Mean % (95% CI) | Mean % (95% CI) | Mean % (95% CI) | Mean % (95% CI) | Mean % (95% CI) | |
| Sociodemographic characteristics | |||||
| Gender, % female | 47.9 (46.8 to 48.9) | 29.2 (18.3 to 40.1) | 55.6 (53.3 to 57.9) | 51.8 (46.2 to 57.5) | 48.8 (47.9 to 49.7) |
| Ethnicity | |||||
| White, % | 88.1 (86.1 to 90.1) | 84.6 (76.0 to 93.1) | 83.8 (80.5 to 87.2) | 78.5 (72.8 to 84.1) | 87.4 (85.2 to 89.5) |
| Indian, % | 2.1 (1.6 to 2.7) | 0.0 | 2.7 (1.8 to 3.6) | 1.8 (0.3 to 3.3) | 2.2 (1.6 to 2.8) |
| Pakistani, % | 2.9 (1.7 to 4.2) | 2.8 (−0.6 to 6.3) | 3.8 (2.0 to 5.6) | 4.5 (2.0 to 6.9) | 3.1 (1.8 to 4.4) |
| Bangladeshi, % | 0.9 (0.5 to 1.4) | 0.5 (−0.5 to 1.4) | 1.2 (0.5 to 1.9) | 1.7 (0.2 to 3.2) | 1.0 (0.5 to 1.4) |
| Black Caribbean, % | 2.0 (1.5 to 2.5) | 6.2 (−0.4 to 12.9) | 2.5 (1.6 to 3.5) | 6.7 (3.8 to 9.6) | 2.2 (1.6 to 2.7) |
| Black African, % | 1.6 (1.1 to 2.1) | 4.2 (−0.3 to 8.8) | 3.5 (2.0 to 5.1) | 4.7 (2.1 to 7.4) | 1.9 (1.3 to 2.6) |
| Other, % | 2.3 (1.8 to 2.8) | 1.7 (−0.9 to 4.3) | 2.4 (1.6 to 3.3) | 2.2 (0.8 to 3.5) | 2.3 (1.9 to 2.8) |
| Family income | |||||
| Most affluent quintile, % | 22.7 (20.2 to 25.2) | 13.2 (4.4 to 21.9) | 14.1 (11.7 to 16.4) | 13.0 (8.7 to 17.2) | 21.4 (19.0 to 23.7) |
| 4th quintile, % | 20.8 (19.7 to 22.0) | 15.6 (6.1 to 25.1) | 20.7 (18.4 to 23.0) | 16.8 (12.5 to 21.2) | 20.7 (19.6 to 21.8) |
| 3rd quintile, % | 19.7 (18.6 to 20.9) | 21.6 (10.7 to 32.4) | 21.3 (19.1 to 23.6) | 17.7 (13.6 to 21.8) | 19.9 (18.8 to 21.0) |
| 2nd quintile, % | 18.8 (17.7 to 20.0) | 21.6 (12.3 to 30.9) | 21.9 (19.8 to 24.0) | 24.2 (19.4 to 29.0) | 19.3 (18.2 to 20.5) |
| Least affluent quintile, % | 17.9 (16.0 to 19.2) | 28.1 (16.5 to 39.6) | 22.0 (19.5 to 24.5) | 28.3 (23.5 to 33.1) | 18.7 (17.4 to 20.0) |
| Occupational class | |||||
| Higher managerial, administrative, and professional, % | 32.3 (30.2 to 34.4) | 27.5 (15.5 to 39.6) | 27.2 (24.3 to 30.0) | 22.6 (17.9 to 27.4) | 31.4 (29.4 to 33.4) |
| Intermediate, % | 22.8 (21.7 to 23.9) | 22.6 (12.2 to 33.0) | 20.3 (18.2 to 22.4) | 17.5 (12.8 to 22.1) | 22.4 (21.3 to 23.4) |
| Routine and manual, % | 38.3 (36.3 to 40.2) | 40.2 (27.2 to 53.3) | 44.2 (41.2 to 47.2) | 50.5 (44.6 to 56.5) | 39.3 (37.4 to 41.2) |
| Never worked or unemployed, % | 6.7 (5.7 to 7.7) | 9.6 (2.9 to 16.4) | 8.3 (6.6 to 10.1) | 9.4 (6.0 to 12.7) | 6.9 (5.9 to 8.0) |
| Maternal education level | |||||
| Degree or higher, % | 30.0 (27.6 to 32.3) | 26.6 (14.3 to 38.8) | 21.7 (19.2 to 24.2) | 14.9 (10.5 to 19.3) | 28.6 (26.4 to 30.8) |
| A-levels, % | 10.2 (9.5 to 10.8) | 8.9 (3.1 to 14.8) | 8.7 (7.3 to 10.1) | 7.4 (4.5 to 10.3) | 9.9 (9.3 to 10.5) |
| GCSE (A–C), % | 33.9 (32.2 to 35.7) | 37.2 (24.5 to 50.0) | 37.5 (34.8 to 40.2) | 39.2 (33.4 to 45.0) | 34.5 (32.8 to 36.2) |
| GCSE (D–G), % | 10.0 (9.2 to 10.8) | 10.2 (2.5 to 17.8) | 13.0 (11.2 to 14.8) | 13.1 (8.8 to 17.4) | 10.4 (9.6 to 11.3) |
| Overseas qualification, % | 2.2 (1.8 to 2.6) | 1.0 (−0.2 to 2.1) | 2.9 (2.0 to 3.7) | 2.4 (0.9 to 3.9) | 2.3 (1.9 to 2.7) |
| None, % | 13.8 (12.7 to 14.9) | 16.2 (7.2 to 25.2) | 16.2 (14.2 to 18.3) | 23.0 (18.4 to 27.6) | 14.3 (13.2 to 15.4) |
| Pregnancy and infancy factors | |||||
| Smoked during pregnancy, % yes | 22.4 (21.2 to 23.6) | 27.6 (15.6 to 39.6) | 25.9 (23.6 to 28.2) | 38.4 (32.6 to 44.2) | 23.2 (22.0 to 24.4) |
| Breastfed child, % no | 27.1 (25.4 to 28.8) | 30.0 (18.9 to 41.0) | 30.9 (28.1 to 33.7) | 36.6 (30.4 to 42.8) | 27.8 (26.1 to 29.5) |
| Solids before 4 mo, % yes | 17.3 (16.2 to 18.4) | 12.0 (4.0 to 20.0) | 20.6 (18.5 to 22.6) | 24.1 (19.0 to 29.2) | 17.8 (16.9 to 18.8) |
| Motor delay, % yes | 10.4 (9.7 to 11.1) | 11.4 (2.6 to 20.1) | 9.7 (8.2 to 11.3) | 15.1 (10.9 to 19.2) | 10.4 (9.8 to 11.1) |
| Early childhood factors | |||||
| Maternal BMI, mean | 24.6 (24.5 to 24.7) | 25.4 (24.0 to 26.8) | 27.3 (27.0 to 27.6) | 28.8 (28.1 to 29.4) | 25.0 (24.9 to 25.1) |
| Sugary drinks, % yes | 40.8 (39.2 to 42.3) | 33.0 (20.3 to 45.6) | 41.9 (39.0 to 44.8) | 41.2 (35.3 to 47.0) | 40.9 (39.4 to 42.4) |
| Fruit <3 per d, % yes | 45.9 (44.4 to 47.3) | 43.6 (28.8 to 58.5) | 51.1 (48.3 to 53.9) | 55.9 (49.9 to 61.8) | 46.7 (45.3 to 48.1) |
| Skip breakfast,% yes | 6.5 (6.0 to 7.0) | 13.6 (4.3 to 22.9) | 12.0 (10.6 to 14.4) | 15.8 (11.5 to 20.1) | 7.5 (7.0 to 8.0) |
| Sport <1 per wk % no | 44.5 (42.7 to 46.3) | 55.9 (40.9 to 70.8) | 47.7 (44.6 to 50.7) | 55.9 (49.8 to 61.9) | 45.2 (43.5 to 46.9) |
| Television >3 h/d, % yes | 13.7 (12.6 to 14.9) | 25.0 (13.6 to 36.4) | 17.4 (15.4 to 20.0) | 19.7 (15.2 to 24.2) | 14.4 (13.3 to 15.5) |
| Nonregular bedtime, % yes | 8.9 (8.2 to 9.5) | 12.2 (2.7 to 21.7) | 12.6 (10.8 to 14.5) | 18.0 (13.0 to 23.1) | 9.6 (8.9 to 10.2) |
| Late bedtime, % yes | 4.7 (4.1 to 5.3) | 8.4 (2.7 to 14.1) | 6.7 (5.4 to 8.1) | 8.2 (5.2 to 11.2) | 5.0 (4.4 to 5.7) |
| Psychosocial and behavioral outcomes | |||||
| Emotional symptoms, mean | 1.81 (1.76 to 1.86) | 2.25 (1.47 to 3.03) | 2.05 (1.92 to 2.18) | 2.45 (2.18 to 2.73) | 1.85 (1.81 to 1.90) |
| Conduct problems, mean | 1.35 (1.31 to 1.39) | 1.79 (1.29 to 2.30) | 1.42 (1.34 to 1.51) | 1.88 (1.67 to 2.10) | 1.37 (1.33 to 1.41) |
| Hyperactivity, mean | 3.10 (3.03 to 3.17) | 3.19 (2.49 to 3.90) | 3.11 (2.97 to 3.25) | 3.57 (3.22 to 3.91) | 3.11 (3.05 to 3.18) |
| Peer problems, mean | 1.28 (1.24 to 1.33) | 1.83 (1.35 to 2.31) | 1.60 (1.50 to 1.71) | 2.25 (1.99 to 2.52) | 1.34 (1.30 to 1.39) |
| Prosocial behavior, mean | 8.75 (8.72 to 8.79) | 8.53 (8.08 to 8.99) | 8.92 (8.83 to 9.01) | 8.87 (8.67 to 9.06) | 8.77 (8.74 to 8.81) |
| Antisocial activities, mean | 0.27 (0.26 to 0.29) | 0.35 (0.16 to 0.55) | 0.28 (0.24 to 0.31) | 0.34 (0.25 to 0.43) | 0.28 (0.26 to 0.29) |
| Smoked cigarettes, % yes | 2.8 (2.4 to 3.2) | 0 | 2.1 (1.3 to 2.8) | 5.1 (2.2 to 8.0) | 2.7 (2.4 to 3.1) |
| Drank alcohol, % yes | 12.5 (11.7 to 13.3) | 9.8 (0.85 to 18.7) | 14.2 (12.1 to 16.3) | 20.9 (14.7 to 27.2) | 12.9 (12.1 to 13.7) |
| Low self-esteem, mean | 8.04 (7.99 to 8.10) | 7.73 (7.13 to 8.34) | 8.35 (8.23 to 8.46) | 8.88 (8.56 to 9.21) | 8.10 (8.05 to 8.15) |
| Unhappiness, mean | 12.39 (12.24 to 12.54) | 12.02 (10.19 to 13.84) | 13.08 (12.70 to 13.46) | 14.54 (13.60 to 15.47) | 12.52 (12.38 to 12.67) |
| Body dissatisfaction, mean | 2.44 (2.40 to 2.48) | 2.45 (1.94 to 2.96) | 2.93 (2.84 to 3.03) | 3.42 (3.20 to 3.63) | 2.52 (2.49 to 2.56) |
CI, confidence interval.
TABLE 2.
Predictors of BMI Trajectory Membership, Compared With the “Stable” Group
| Decreasing | Moderate Increasing | High Increasing | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Sociodemographic characteristics | |||
| Gender, female | 0.44 (0.27 to 0.71)*** | 1.36 (1.22 to 1.51)*** | 1.20 (0.94 to 1.53) |
| Ethnicitya | |||
| Indian | 0.00 (0.00 to 0.00)*** | 1.66 (1.24 to 2.23)** | 1.63 (0.70 to 3.80) |
| Pakistani | 0.68 (0.23 to 2.04) | 1.29 (1.02 to 1.65)* | 1.83 (1.07 to 3.12)* |
| Bangladeshi | 0.34 (0.04 to 2.86) | 1.34 (0.91 to 1.96) | 0.46 (0.96 to 6.32) |
| Black Caribbean | 2.74 (0.82 to 9.11) | 1.21 (0.90 to 1.61) | 3.44 (2.11 to 5.62)*** |
| Black African | 2.17 (0.60 to 7.89) | 2.01 (1.42 to 2.86)*** | 3.39 (1.94 to 5.94)*** |
| Other | 0.64 (0.13 to 3.13) | 1.21 (0.89 to 1.65) | 1.37 (0.71 to 2.63) |
| Family incomeb | |||
| 4th quintile | 1.29 (0.54 to 3.11) | 1.43 (1.15 to 1.79)** | 1.11 (0.70 to 1.77) |
| 3rd quintile | 1.98 (0.83 to 4.72) | 1.37 (1.12 to 1.68)** | 0.89 (0.53 to 1.50) |
| 2nd quintile | 2.14 (0.84 to 5.48) | 1.30 (1.03 to 1.65)* | 0.94 (0.56 to 1.57) |
| Least affluent quintile | 2.79 (1.08 to 7.18)* | 1.38 (1.10 to 1.73)** | 1.01 (0.57 to 1.81) |
| Occupational classc | |||
| Intermediate | 1.01 (0.52 to 1.97) | 0.84 (0.71 to 1.01) | 0.81 (0.54 to 1.22) |
| Routine and manual | 0.82 (0.36 to 1.87) | 0.92 (0.77 to 1.10) | 0.96 (0.63 to 1.45) |
| Never worked or unemployed | 1.14 (0.32 to 4.10) | 0.92 (0.71 to 1.19) | 0.79 (0.44 to 1.43) |
| Maternal education leveld | |||
| A-levels | 0.85 (0.36 to 1.99) | 1.12 (0.89 to 1.40) | 1.39 (0.83 to 2.32) |
| GCSE (A–C) | 0.88 (0.40 to 1.91) | 1.32 (1.11 to 1.57)** | 1.79 (1.14 to 2.79)* |
| GCSE (D–G) | 0.72 (0.27 to 1.90) | 1.42 (1.13 to 1.78)** | 1.68 (0.95 to 2.96) |
| Overseas qualification | 0.30 (0.07 to 1.19) | 1.30 (0.88 to 1.93) | 1.32 (0.67 to 2.62) |
| None | 0.65 (0.26 to 1.65) | 1.18 (0.95 to 1.48) | 1.74 (1.01 to 2.98)* |
| Pregnancy and infancy factors | |||
| Smoked in pregnancy, yes | 1.08 (0.57 to 2.07) | 1.17 (1.03 to 1.33)* | 1.97 (1.51 to 2.58)*** |
| Breastfed child, no | 1.05 (0.59 to 1.85) | 1.03 (0.90 to 1.19) | 1.18 (0.88 to 1.59) |
| Solids before 4 mo, yes | 0.52 (0.25 to 1.10) | 1.15 (0.98 to 1.34) | 1.26 (0.95 to 1.67) |
| Gross motor delay, yes | 1.04 (0.45 to 2.37) | 0.92 (0.76 to 1.13) | 1.47 (1.05 to 2.04)* |
| Early childhood factors | |||
| Maternal BMI | 1.03 (0.97 to 1.09) | 1.10 (1.09 to 1.11)*** | 1.14 (1.12 to 1.16)*** |
| Sugary drinks, yes | 0.65 (0.37 to 1.14) | 1.05 (0.93 to 1.18) | 0.99 (0.77 to 1.27) |
| Fruit <3 per d, yes | 0.72 (0.40 to 1.29) | 1.06 (0.94 to 1.19) | 1.08 (0.83 to 1.42) |
| Skip breakfast, yes | 2.01 (1.03 to 3.92)* | 1.66 (1.37 to 2.02)*** | 1.76 (1.21 to 2.56)** |
| Sport <1 per wk, no | 1.27 (0.66 to 2.44) | 0.85 (0.74 to 0.98)* | 0.90 (0.69 to 1.19) |
| Television >3 h/d, yes | 1.86 (0.97 to 3.57) | 1.15 (0.99 to 1.33) | 1.17 (0.87 to 1.58) |
| Nonregular bedtime, yes | 1.12 (0.49 to 2.59) | 1.22 (1.01 to 1.46)* | 1.55 (1.08 to 2.22)* |
| Late bedtime, yes | 1.79 (0.83 to 3.88) | 1.26 (1.00 to 1.57)* | 1.50 (0.93 to 2.41) |
CI, confidence interval.
Reference group: white.
Reference group: richest income quintile.
Reference group: higher managerial, administrative, and professional.
Reference group: degree or higher.
P < .05.
P < .01.
P < .001.
Cohort members whose mothers smoked during pregnancy had higher odds of being in the “moderate increasing” and “high increasing” trajectories (ORs = 1.17 and 1.97, respectively). Breastfeeding and the early introduction of solid food were not independently associated with trajectory membership. Having motor (sitting, standing, crawling) delays in infancy were associated with higher odds of being in the “high increasing” group (OR = 1.47). A unit increase in maternal BMI was associated with a 10% increase in the odds of being in the “moderate increasing” and “high increasing” trajectories. Skipping breakfast and having nonregular bedtimes in early childhood were associated with higher odds of increasing trajectory membership (for “moderate increasing,” skipping breakfast OR = 1.66, nonregular bedtimes OR = 1.22; for “high increasing,” ORs = 1.76 and 1.55, respectively). Sugary drink consumption, fruit intake, television viewing, and sports participation appeared not to predict trajectory membership.
Are BMI Trajectories Linked to Psychosocial Well-Being at the Start of Adolescence?
Compared with the “stable” group, cohort members in the “moderate increasing” group had worse scores for emotional symptoms, peer problems, happiness, body satisfaction, and self-esteem but had better prosocial behavior scores. Cohort members in the “high increasing” group had worse scores for emotional symptoms, peer and conduct problems, happiness, body satisfaction, and self-esteem and were more likely to have drank alcohol and smoked cigarettes. In addition, cohort members in the “moderate increasing” group were more likely to have scores in the clinical range for emotional and peer problems, and those in the “high increasing” group were more likely to have scores in the clinical range for emotional, peer, and conduct problems (data not shown). Belonging to the decreasing trajectory did not appear to predict any significantly different outcomes at age 11 years. The distributions of psychosocial well-being markers are shown in Table 1, and fully adjusted estimates by BMI trajectory are shown in Table 3.
TABLE 3.
Psychosocial Well-Being at Age 11 y by BMI Trajectory Compared With the “Stable” Group
| Stable | Decreasing | Moderate Increasing | High Increasing | |
|---|---|---|---|---|
| Emotional symptoms | 0 | 0.39 (−0.33 to 1.11) | 0.18 (0.05 to 0.32)** | 0.53 (0.25 to 0.80)*** |
| Conduct problems | 0 | 0.29 (−0.16 to 0.74) | 0.03 (−0.06 to 0.11) | 0.38 (0.17 to 0.60)*** |
| Hyperactivity | 0 | −0.23 (−0.87 to 0.40) | −0.04 (−0.19 to 0.11) | 0.27 (−0.07 to 0.60) |
| Peer problems | 0 | 0.41 (−0.02 to 0.84) | 0.27 (0.16 to 0.38)*** | 0.84 (0.58 to 1.11)*** |
| Prosocial behavior | 0 | −0.08 (−0.52 to 0.36) | 0.16 (0.06 to 0.25)** | 0.16 (−0.04 to 0.35) |
| Antisocial activities | 0 | 0.02 (−0.16 to 0.20) | 0.00 (−0.04 to 0.03) | 0.03 (−0.06 to 0.11) |
| Smoked cigarettes | 1 | — | 2.03 (1.65 to 2.75)** | 5.05 (2.56 to 16.11)** |
| Drank alcohol | 1 | 0.64 (0.24 to 1.72) | 1.19 (0.98 to 1.43) | 1.82 (1.23 to 2.66)* |
| Low self-esteem | 0 | −0.26 (−0.84 to 0.31) | 0.28 (0.15 to 0.41)*** | 0.84 (0.51 to 1.16)*** |
| Unhappiness | 0 | −0.54 (−2.25 to 1.17) | 0.66 (0.27 to 1.06)** | 2.07 (1.15 to 2.99)*** |
| Body dissatisfaction | 0 | 0.05 (−0.43 to 0.53) | 0.47 (0.37 to 0.57)*** | 0.98 (0.76 to 1.19)*** |
Regression analysis included all sociodemographic factors as control variables. All outcomes are linear regressions except smoked cigarettes and drank alcohol which are logistic regressions. —, no available cases.
P < .05.
P < .01.
P < .001.
Discussion
In this large population-based sample of children we identified 4 BMI development trajectories. The majority of children belonged to a stable, nonoverweight group. About 1 in 7 belonged to a group with increasing BMIs with average BMIs just under the overweight range at age 3 and subsequent average BMIs increasing throughout the rest of childhood into the overweight but not obese range. A smaller group (2.5%) had average BMIs in the obese range at age 3, and their BMIs continued to increase throughout childhood. A small group (<1%) of children had BMIs in the obese range at age 3, but by age 7 their BMIs were in the nonoverweight range. Factors that predicted membership in the 2 increasing BMI trajectories included socioeconomic disadvantage, being from certain ethnic minority backgrounds, maternal smoking during pregnancy, maternal BMI, and family routines, such as skipping breakfast and not having regular bedtimes. We found that, in general, having BMIs in the overweight and obese range throughout childhood was associated with worse psychosocial well-being at 11 years of age.
Similar to other reports, a large proportion of our study sample had BMIs in the nonoverweight range throughout childhood,1–5,9,11 and we identified groups of children belonging to BMI trajectories in the overweight or obese range. We found a small proportion of children in a decreasing trajectory that has been seen elsewhere.7 We did not identify a group of children with BMIs consistently in the underweight range. There were differences from other reports also; for example, some studies have identified groups of children who develop overweight or obesity at different points in childhood, including a late-onset group.1–4,9,11 Dissimilarities in observed trajectories might not be surprising given different study settings (eg, the United States,2–4,7,8 Canada,5,6,11,12 Australia)1,9,10 and different empirical approaches used to identify groups.
Our findings suggest that a range of early life factors are associated with children being on particular BMI trajectories. As found in other studies, we show sociodemographic factors including socioeconomic position1,2,4,12,30 and ethnicity2–4,12 to be linked to membership of trajectories in the overweight and obese range. Other work from the United Kingdom has shown variations in the risk of overweight and obesity for children from black and South Asian groups and for children living in economically disadvantaged circumstances.13,31 In keeping with previous reports, behavioral influences appeared important, including smoking in pregnancy,3,5,6,32 maternal BMI,1–3,5,6,8,10,11,30,32 and markers of family routines such as skipping breakfast and sleep schedules.11 Exposure to tobacco products during fetal life has long been thought to increase the risk of overweight in childhood,33 and hypothesized pathways include altered growth and weight gain, metabolic processes, and epigenetic mechanisms. Previous work suggests links between fetal tobacco exposure and infant motor coordination,34 and this link in turn could be on a developmental pathway to BMI growth.35 Maternal BMI appears strongly predictive of children’s BMI growth, probably reflecting the wider obesogenic environment along with genetic predisposition. Disrupted routines, exemplified here by nonregular sleep schedules and skipping breakfast, are hypothesized to influence weight gain via increased appetite and consumption of energy-dense foods. Interestingly, skipping breakfast was also associated with being in the “decreasing” trajectory, but the potential mechanisms at play here are not clear. We cannot rule out, nor were we able to tease out, a bidirectional relationship between BMI growth and psychosocial well-being. As in previous work,14,16,17 our findings suggest that trajectories in the overweight and obese range correlate strongly with worse psychosocial outcomes, and it may be that the strength of these associations increases as adolescence proceeds, as suggested elsewhere.14,15 Social stigmatization, isolation, and victimization are factors hypothesized to form links between overweight and negative psychosocial outcomes and the exploration of risky health behaviors. Thus, we found that common psychosocial correlates of “moderate increasing” and “high increasing” BMI trajectories were socioemotional difficulties, low self-esteem, low overall happiness, and body dissatisfaction. In addition, children with BMIs in the obese range throughout childhood (the “high increasing” group) were more likely to report having drunk alcohol and smoked cigarettes.
This study has distinct strengths, being the first to examine nationally representative UK data with repeated measures allowing for the empirical derivation of BMI trajectories across the first decade of life. We estimated associations between a wide range of early life factors, including mother’s health behaviors (smoking during pregnancy, infant feeding, and BMI), infant motor skills, family routines, diet, and physical activity in relation to different patterns of BMI development. Another strength is that we examined identified BMI trajectories in conjunction with a range of markers of psychosocial well-being, such as socioemotional difficulties, self-esteem, happiness, and risky behaviors. This study has important potential limitations too. For example, even though we included in our analyses a wide range of potential risk factors, we were not able to fully characterize influences (including gestational diabetes and growth in infancy) that might play a role. Imperfect measurement was also a feature for some of our early life predictor variables, such as sugary drinks, fruit consumption, and markers of physical activity including sports participation and television viewing, all of which had no apparent link with BMI trajectories; however, these markers are crude, and conclusions based on null findings should be avoided. Furthermore, these data on early life predictors were mother reported. However, data were collected contemporaneously, thus minimizing problems of recall bias.
Conclusions
Most children in this contemporary UK study belonged to BMI trajectories in the nonoverweight range. Several potentially modifiable early life factors, including smoking in pregnancy and family routines (skipping breakfast and not having a regular bedtime), appeared important in predicting BMIs in the overweight and obese ranges. These findings support the need for intervention strategies aimed at multiple spheres of influence on BMI growth. In general, having BMI growth in the overweight and obese range was linked to poorer psychosocial well-being, supporting the need for health care providers to monitor these occurrences in children with high BMI growth. Given continuities in overweight or obesity and mental health from childhood into adolescence and adulthood, intervening early could alter trajectories and have important implications for physical health, psychosocial well-being, and health behaviors across the life course.
Acknowledgments
We thank the Millennium Cohort Study families for their time and cooperation, as well as the Millennium Cohort Study team at the Institute of Education. The Millennium Cohort Study is funded by Economic and Social Research Council grants.
Glossary
- A-BIC
adjusted Bayesian information criterion
- A-level
Advanced Level
- GCSE
General Certificate of Secondary Education
- OR
odds ratio
Footnotes
Prof Kelly conceptualized and designed the study and drafted the initial manuscript; Dr Patalay carried out the analyses and reviewed and revised the manuscript; Prof Montgomery critically reviewed the manuscript; Prof Sacker assisted in the design of the study, advised on data analysis, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The alcohol use and attitudes variables in MCSS were co funded by grant AA019606 from the U.S. National Institute on Alcohol Abuse and Alcoholism. All phases of this study were supported by a grant from the Economic and Social Research Council RES-596-28-0001. The funders had no role in the interpretation of these data or in the writing of this article. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Magee CA, Caputi P, Iverson DC. Identification of distinct body mass index trajectories in Australian children. Pediatr Obes. 2013;8(3):189–198 [DOI] [PubMed] [Google Scholar]
- 2.Danner FW, Toland MD. The interactive role of socioeconomic status, race/ethnicity, and birth weight on trajectories of body mass index growth in children and adolescents. J Early Adolesc. 2013;33(3):293–314 [Google Scholar]
- 3.Li C, Goran MI, Kaur H, Nollen N, Ahluwalia JS. Developmental trajectories of overweight during childhood: role of early life factors. Obesity (Silver Spring). 2007;15(3):760–771 [DOI] [PubMed] [Google Scholar]
- 4.Balistreri KS, Van Hook J. Trajectories of overweight among US school children: a focus on social and economic characteristics. Matern Child Health J. 2011;15(5):610–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pryor LE, Tremblay RE, Boivin M, et al. Developmental trajectories of body mass index in early childhood and their risk factors: an 8-year longitudinal study. Arch Pediatr Adolesc Med. 2011;165(10):906–912 [DOI] [PubMed] [Google Scholar]
- 6.Carter MA, Dubois L, Tremblay MS, Taljaard M, Jones BL. Trajectories of childhood weight gain: the relative importance of local environment versus individual social and early life factors. PLoS One. 2012;7(10):e47065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Brien M, Nader PR, Houts RM, et al. The ecology of childhood overweight: a 12-year longitudinal analysis. Int J Obes. 2007;31(9):1469–1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ventura AK, Loken E, Birch LL. Developmental trajectories of girls’ BMI across childhood and adolescence. Obesity (Silver Spring). 2009;17(11):2067–2074 [DOI] [PubMed] [Google Scholar]
- 9.Garden FL, Marks GB, Simpson JM, Webb KL. Body mass index (BMI) trajectories from birth to 11.5 years: relation to early life food intake. Nutrients. 2012;4(10):1382–1398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giles LC, Whitrow MJ, Davies MJ, Davies CE, Rumbold AR, Moore VM. Growth trajectories in early childhood, their relationship with antenatal and postnatal factors, and development of obesity by age 9 years: results from an Australian birth cohort study. Int J Obes. 2015;39(7):1049–1056 [DOI] [PubMed] [Google Scholar]
- 11.Pryor LE, Brendgen M, Tremblay RE, et al. Early risk factors of overweight developmental trajectories during middle childhood. PLoS One. 2015;10(6):e0131231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tu AW, Mâsse LC, Lear SA, Gotay CC, Richardson CG. Body mass index trajectories from ages 1 to 20: results from two nationally representative Canadian longitudinal cohorts. Obesity (Silver Spring). 2015;23(8):1703–1711 [DOI] [PubMed] [Google Scholar]
- 13.Goisis A, Sacker A, Kelly Y. Why are poorer children at higher risk of obesity and overweight? A UK cohort study. Eur J Public Health. 2016;26(1):7–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heerman WJ, Krishnaswami S, Barkin SL, McPheeters M. Adverse family experiences during childhood and adolescent obesity. Obesity (Silver Spring). 2016;24(3):696–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stenhammar C, Olsson G, Bahmanyar S, et al. Family stress and BMI in young children. Acta Paediatr. 2010;99(8):1205–1212 [DOI] [PubMed] [Google Scholar]
- 16.Griffiths LJ, Parsons TJ, Hill AJ. Self-esteem and quality of life in obese children and adolescents: a systematic review. Int J Pediatr Obes. 2010;5(4):282–304 [DOI] [PubMed] [Google Scholar]
- 17.Sanders RH, Han A, Baker JS, Cobley S. Childhood obesity and its physical and psychological co-morbidities: a systematic review of Australian children and adolescents. Eur J Pediatr. 2015;174(6):715–746 [DOI] [PubMed] [Google Scholar]
- 18.Huang DYC, Lanza HI, Wright-Volel K, Anglin MD. Developmental trajectories of childhood obesity and risk behaviors in adolescence. J Adolesc. 2013;36(1):139–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Millennium Cohort Study, A Guide to the Datasets (Eighth Edition) First, Second, Third, Fourth and Fifth Surveys. Available at: www.cls.ioe.ac.uk/shared/get-file.ashx?id=1806&itemtype=document. Accessed July 21, 2016
- 20.Gallop K, Rose N, Wallace E, et al. Millennium Cohort Study Fifth Sweep (MCS5) Technical Report. Centre for Longitudinal Studies, Institute of Education. 2013. Available at: www.cls.ioe.ac.uk/shared/get-file.ashx?id=1655&itemtype=document. Accessed July 21, 2016
- 21.Kelly Y, Sacker A, Schoon I, Nazroo J. Ethnic differences in achievement of developmental milestones by 9 months of age: the Millennium Cohort Study. Dev Med Child Neurol. 2006;48(10):825–830 [DOI] [PubMed] [Google Scholar]
- 22.Sacker A, Quigley MA, Kelly YJ. Breastfeeding and developmental delay: findings from the Millennium Cohort Study. Pediatrics. 2006;118(3). Available at: www.pediatrics.org/cgi/content/full/118/3/e682 [DOI] [PubMed] [Google Scholar]
- 23.Information for Researchers and Professionals About the Strengths & Difficulties Questionnaires. Available at: www.sdqinfo.org/. Accessed July 21, 2016 [DOI] [PubMed]
- 24.Rosenberg M. Society and the Adolescent Self-Image. Middletown, CT: Wesleyan University Press; 1989 [Google Scholar]
- 25.Booker CL, Skew AJ, Sacker A, Kelly YJ. Well-being in adolescence—an association with health-related behaviors: findings from Understanding Society, the UK Household Longitudinal Study. J Early Adolesc. 2014;34(4):518–538 [Google Scholar]
- 26.Muthén LK, Muthén BO. Mplus User’s Guide. 7th ed Los Angeles, CA: Muthén & Muthén; 1998–2015 [Google Scholar]
- 27.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–569 [Google Scholar]
- 28.Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2008;2(1):302–317 [Google Scholar]
- 29.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–399 [DOI] [PubMed] [Google Scholar]
- 30.Börnhorst C, Siani A, Russo P, et al. Early life factors and inter-country heterogeneity in BMI growth trajectories of European children: the IDEFICS study. PLoS One. 2016;11(2):e0149268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zilanawala A, Davis-Kean P, Nazroo J, Sacker A, Simonton S, Kelly Y. Race/ethnic disparities in early childhood BMI, obesity and overweight in the United Kingdom and United States. Int J Obes. 2015;39(3):520–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robinson SM, Crozier SR, Harvey NC, et al. Modifiable early-life risk factors for childhood adiposity and overweight: an analysis of their combined impact and potential for prevention. Am J Clin Nutr. 2015;101(2):368–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oken E, Levitan EB, Gillman MW. Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis. Int J Obes. 2008;32(2):201–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Larsson M, Montgomery SM. Maternal smoking during pregnancy and physical control and coordination among offspring. J Epidemiol Community Health. 2011;65(12):1151–1158 [DOI] [PubMed] [Google Scholar]
- 35.Osika W, Montgomery SM; Longitudinal Birth Cohort Study . Physical control and coordination in childhood and adult obesity: Longitudinal Birth Cohort Study. BMJ. 2008;337:a699. [DOI] [PMC free article] [PubMed] [Google Scholar]