Abstract
Heart disease is the leading cause of death in the United States and nearly one million Americans will have a heart attack this year. Although the risks associated with a heart attack are well established, we know surprisingly little about how marital factors contribute to survival in adults afflicted with heart disease. This study uses a life course perspective and longitudinal data from the Health and Retirement Study to examine how various dimensions of marital life influence survival in U.S. older adults who suffered a heart attack (n=2,197). We found that adults who were never married (odds ratio [OR]=1.73), currently divorced (OR=1.70), or widowed (OR=1.34) were at significantly greater risk of dying after a heart attack than adults who were continuously married; and the risks were not uniform over time. We also found that the risk of dying increased by 12% for every additional marital loss and decreased by 7% for every one-tenth increase in the proportion of years married. After accounting for more than a dozen socioeconomic, psychosocial, behavioral, and physiological factors, we found that current marital status remained the most robust indicator of survival following a heart attack. The implications of the findings are discussed in the context of life course inequalities in chronic disease and directions for future research.
For more than half a century, the life course perspective has made immeasurable contributions to our understanding of how social inequalities in health develop across age. Central to this theoretical orientation is an emphasis on individual biographies that reflect long-term patterns of stability and change over time (Elder, 1985; George, 1999; Giele and Elder, 1998). Perhaps second only to research on socioeconomic differences in health, studies have increasingly focused on the importance of past and present marital experiences as they relate to the health and well-being of older adults (Hughes and Waite, 2009; Williams and Umberson, 2004; Zhang, 2006). There is now mounting evidence to indicate that the timing, number, and duration of marital experiences have significant implications for chronic illness (Dupre and Meadows, 2007; Eaker et al., 2007; Zhang and Hayward, 2006) and mortality (Brockmann and Klein, 2004; Dupre, Beck, and Meadows, 2009; Molloy et al., 2009).
A guiding principle of recent research on marriage and health over the life course is recognition of the dynamic longitudinal associations between marital exposures and health decline (Grundy and Tomassini, 2010; Lund, Holstein, and Osler, 2004; Williams and Umberson, 2004). To date, however, the vast majority of longitudinal studies on marital life—also referred to in the literature as marital trajectories, histories, or biographies—focus on changes in aggregated indicators of health (e.g., number of chronic conditions, limitations, etc.) or the development of illness (i.e., disease incidence). Only a handful of studies examine the role of marital status after the onset of illness (Burnley, 1999; Chandra et al., 1983; Kilpi et al., 2015; Lammintausta et al. 2013; Nielsen and Mard, 2010) and no existing studies consider which aspects of the marital life course are important to survival after a major health event. This gap in the literature largely neglects an important (and often lengthy) stage in the life course—especially when considering that the leading causes of disability and death in the United States are attributable to cardiovascular disease and its management (Go et al., 2014; National Center for Health Statistics [NCHS], 2013).
This study is the first prospective investigation of how multiple dimensions of marital life are related to survival after a heart attack. Data from a nationally representative sample of U.S. older adults (1992 to 2010) is used to address four research objectives. First, examine whether individuals who are married live longer after a heart attack than individuals who are not married. Second, examine which aspects of marital life—i.e., marriage timing, current marital status, cumulative number of marital losses, and marriage duration—are associated with risks of dying after disease onset. Third, assess whether and to what degree the associations vary over time following a heart attack. Finally, examine whether socioeconomic, psychosocial, behavioral, and/or physiological risk factors explain the associations. The implications of the findings are discussed in the context of life course inequalities in chronic disease and directions for future research.
BACKGROUND
The Marital Life Course
The marital life course—also referred to here as marital history—is the conceptual and empirical aggregation of past and present marital relationships that are bounded by transitions into/out of discrete marital statuses that accumulate over adulthood (Dupre and Meadows, 2007; Zhang and Hayward, 2006). Several distinct dimensions of marital life are identified in the literature. The timing of one’s first marriage is a key turning point in the adult life course and signals whether entry into this role occurs at a normative age range for that historical period/cohort (McLaughlin, Litchter, and Johnston, 1993; Spanier, Roos, and Shockey, 1985). Marrying at an early age can lead to added stress, hardship, and long-term disadvantage because important socioeconomic resources may be forfeited (e.g., educational attainment). Although research is limited, studies suggest that early marriage is associated with poor physical and psychological health (Dupre and Meadows, 2007; Forthofer et al., 1996 McFarland et al., 2013) and increases the likelihood of marital disruption (Booth and Edwards, 1985; Heaton, 1991; Morgan and Rindfuss, 1985).
The second and perhaps most studied feature of marital life in the literature is marital status. In the absence of other information, knowing whether an adult is currently divorced, widowed, remarried, or continuously married provides a contemporaneous snapshot of one’s current history of marital life; as well as providing important insights into a wide range of socioeconomic, psychosocial, and behavioral correlates. Compared to those who are married, research consistently shows that individuals who are not married have fewer economic resources, less social support and social control, more risky behaviors, and ultimately worse health outcomes (Gove and Shin, 1989; Lillard and Waite, 1995; Umberson, 1987; Wu and Hart, 2002). Marital transitions are another dimension of marital life that represents discrete changes in marital statuses. Marital dissolutions in particular (i.e., divorce and widowhood) are important markers in the life course because they denote a change in status that is frequently stressful and often involves an adjustment to a new social role, identity, and living arrangement. Divorce and widowhood also bring a decline in the availability of social and financial resources (Ross, Mirowsky, and Goldsteen, 1990; Wilmoth and Koso, 2002). Indeed, studies show that divorce and widowhood transitions increase a person’s risk of disease, disability, and death (Hemström, 1996; Pienta, Hayward, and Jenkins, 2000; Zick and Smith, 1991) and that repeated marital losses can be especially detrimental to health and well-being (Barret, 2000; Dupre, 2016; Marks and Lambert, 1998).
A final dimension of marital life is the duration of time spent within a given status. Marital duration captures both stability in the life course and marital instability marked by several marital durations distributed across multiple statuses (i.e., marriage duration, divorce duration, etc.). Marital duration also differentiates between persons who may share the same number and type of transitions (i.e., divorce[s]) but who may accumulate unequal amounts of time in each marital status over their life course. Long durations of marriage foster economic and behavioral stability, shared obligations, and vested interests between partners, which in turn, promote healthy lifestyles and enhance socioeconomic and psychological resources (Brockmann and Klein, 2004; Elder et al., 2003; Umberson, 1987). Although few studies directly test this argument, research shows that individuals who accumulate long durations of marriage have significantly lower levels of disease, disability, and mortality than those with shorter marriage durations (Dupre et al., 2009; Lillard and Waite, 1995; Pienta et al., 2000).
The Marital Life Course and Heart Attack Survival
More than 80 million Americans—approximately 1 in 3 adults—currently live with one or more forms of cardiovascular disease (CVD) and more than 7 million hospitalizations occur each year because of CVD-related illnesses (Go et al., 2014; NCHS, 2013). According to recent estimates, nearly one million adults will have a heart attack this year—approximately one every 44 seconds—and cost the United States nearly $12 billion in hospital expenses. (Go et al., 2014; Torio and Andrews, 2013). Although classical risk factors for the incidence of heart disease are widely established—e.g., smoking, hypertension, diet, and obesity (NCHS, 2013)—our understanding of whether and to what extent marital relationships play a role in CVD prognosis is limited.
Studies show that adults who are not married are at a significantly greater risk of suffering a serious cardiovascular event such as a heart attack than married adults (Koskenvuo et al., 1980; Lindegard et al., 1985; Venters et al., 1986). However, little is known about whether and to what extent marital life influences survival after a heart attack. The research that does exist—largely from clinical studies or outside of the United States—suggests that adults who are not married are much more likely to die following a heart attack than those who are married (Case et al., 1992; Burnley, 1999; Chandra et al., 1983; Gerward et al., 2010; Lammintausta et al., 2013; Nielsen and Mard, 2010). For example, a recent study in Finland shows that men and women who are married have significantly lower short-term and long-term mortality following a heart attack than those who are not married or live alone (Kilpi et al., 2015). Relatedly, Idler, Boulifard, and Contrada (2012) show that married adults who underwent cardiac surgery have significantly better survival prospects than adults who are unmarried. Despite these contributions, the literature largely ignores how past and present exposure to marital life has consequences for the longevity of adults who suffered a heart attack.
We argue that a life course perspective is critical to understanding how past and present marital experiences may influence survival after a heart attack. Current research suggests that the accumulation of past marital experiences—e.g., marital losses—are strong correlates of the development of disease (Dupre et al., 2015; Zhang and Hayward, 2006). However, for those recovering from a life-threatening cardiac event, ones’ marital status may be an especially important marker for understanding the current resources available toward a positive prognosis. It also is possible that the influence of marital factors will not be uniform over time since the occurrence of the heart attack. The purpose of this study is to examine how each dimension of marital life is prospectively related to differences in survival after a heart attack. To further understand these associations, we turn to the mechanisms thought to explain how marital timing, status, transitions, and duration may contribute to surviving after a heart attack.
Possible Mechanisms
A body of literature too large to summarize here consistently documents marital differences in a constellation of risk factors related to cardiovascular disease and mortality (Green et al., 2012; McFarland, Hayward, and Brown, 2013; Molloy et al., 2009; Ross et al., 1990; Waite 1995). Despite this volume of research, it is largely unknown the degree to which these factors play a role in how one’s marital life impacts their risk of dying after a heart attack. We anticipate that socioeconomic and behavioral factors may be especially salient to the quality of care and disease management following a heart attack. Several categories of mechanisms are proposed.
Socioeconomic factors are widely recognized as a key mechanism contributing to why married adults have better health than unmarried adults. The prevailing argument is that marriage provides a shared context of financial and material resources and that marital dissolution severs these socioeconomic bonds (Duncan and Hoffman, 1985; McManus and DiPrete, 2001; Wilmoth and Koso, 2002). Accordingly, studies show that the continuously married have greater levels of wealth, better occupations, and less unemployment than those with marital instability (Addo and Lichter, 2013; Smith, 1994; Waite, 1995). Relatedly, married couples also have greater access to medical insurance, prescription drug coverage, and higher quality health care (Fletcher, 1988; Waite 1995; Zuvekas and Taliaferro, 2003)—which may be especially important for those recovering from a heart attack (see Kilpi et al., 2015). Marrying at an early age and experiencing marital loss(es) also may diminish the acquisition and availability of these resources to improve the chances of survival following a serious cardiovascular event.
Psychosocial Factors are a second category of mechanisms that may be important for survival after a heart attack. Research shows that married adults have higher levels of social support, family cohesion, coping resources, and overall psychological well-being than their unmarried counterparts (Brown and Smith, 1992; Ross and Mirowsky, 1989; Watcherman and Sommers, 2006). Psychological disposition and coping resources are shown to be important attributes for lowering mortality after a serious health event such as a heart attack (Mookadam and Arthur, 2004; Welin, Lappas, and Wilhelmsen, 2000). Some research also suggests that religion may be an important psychosocial resource in cardiac patients and their spouses during recovery (e.g., Miller et al. 2007). Therefore, it is argued that adults who experience marital loss will have greater emotional distress and fewer psychosocial resources available during their recovery to improve their outcomes.
Behavioral Factors are a related class of mechanisms that frequently include factors such as smoking, diet, exercise, and alcohol consumption (Franks, Pienta, and Wray, 2002; Green et al., 2012). The links between these health practices and cardiovascular health are well known, but their role in explaining marital differences in survival after a heart attack is less documented. Based on the wider health literature, the expectation is that marriage—particularly a long, stable marriage—promotes social control and shared obligations that encourage the cessation/avoidance of smoking and excess alcohol consumption, regular medical checkups, and other behaviors that are important for managing illness (Husaini et al., 2001; Kamon et al., 2008; Umberson, 1992). Indeed, there is evidence to suggest that spouses with concordant health behaviors are more likely to adopt and maintain healthy lifestyles to improve recovery and survival after a cardiovascular event (Di Castelnuovo et al., 2009; Meyler, Stimpson, and Peek, 2007). Likewise, a sustained regime of medications (e.g., beta-blockers, ACE inhibitors, etc.) is common following a heart attack; therefore, we would expect that medication adherence plays an important role in survival after a heart attack.
Physiological factors are the mechanisms most proximate to mortality after a heart attack and include physiological status and pre-existing conditions. Obesity, comorbidity, and subsequent cardiac events are well-known risk factors for dying after a heart attack (Go et al., 2014; NCHS, 2013), yet they are the least studied pathways as they relate to linking marital background and disease prognosis (Profant and Dimsdale, 1999; Sbarra et al., 2009). The general expectation is that the stresses of non-normative and unstable marital union(s) are antecedents of chronic health conditions such high blood pressure, diabetes, excess body weight, and recurrent heart attacks (August and Sorkin, 2010; Das, 2013; Kamon et al., 2008). Moreover, it can be argued that lacking marital support may be most detrimental to adults with the most comorbidities and functional limitations after a cardiac event.
Research Questions
The primary objective of this study is to examine how marital experiences contribute to surviving after a heart attack. A life course perspective serves as the overarching framework to understand how past and present exposure to various dimensions of marital life exert their effect over time. The general expectation is that non-normative marital timing, marital loss, and limited exposure to stable marriage are sources of disadvantage that may be detrimental to recovery after a major illness. There are significant shortcomings in the literature and our understanding of whether and to what extent marital relationships play a role in disease prognosis. To this end, several research questions guide the current analyses. First, do older adults who are married live longer after a heart attack than older adults who are not married? Second, what aspects of marital life are associated with greater risks of dying after disease onset? Third, do the associations change over time after suffering a heart attack? And finally, what are the factors that explain significant marital differences in survival following a heart attack?
METHODS
The Health and Retirement Study (HRS) is an ongoing prospective cohort study of U.S. adults over the age of 50 sponsored by the National Institute on Aging and the Institute for Social Research at the University of Michigan (HRS, 2014). The original study cohort included 9,824 age-eligible participants born in 1931 to 1941 who have been interviewed biennially since 1992. With an initial response rate of 82%, sample attrition in the HRS due to non-response and lost tracking is especially low and re-interview response rates are generally well above 90%. Since 1998, the HRS has been supplemented with age-selective birth cohorts to replenish the nationally representative sample of older adults (i.e., steady-state sample design). Details of the multistage sampling design, survey implementation, and response rates have been documented extensively elsewhere (HRS, 2014; Juster and Suzman, 1995).
Data for this study are drawn from 10 waves of interviews (1992–2010) from 30,661 respondents in the original HRS cohort, the Asset and Health Dynamics Among the Oldest Old cohort (AHEAD: ≤ 1923), Children of Depression (CODA: 1924–1930), War Baby cohort (WB: 1942–1947), and the Early Baby-Boom cohort (EBB: 1948–1953), who were first interviewed in 1992, 1993, 1998, and 2004, respectively, and re-interviewed through 2010. Data for 2012 were not used for this analysis because information on respondent mortality is not currently complete for this period. The analyses are restricted to respondents who reported the incidence of a heart attack during the 10-wave observation period from 1992 to 2010 (n=2,349). At each interview, HRS participants were asked whether they had “a heart attack or myocardial infarction” and in what year (and month after 1994) it occurred. The time of the event was calculated from the respondents’ dates of birth and the event. We excluded 12 cases because of inconsistent or erroneous values on the timing of death. Fifty-six respondents were excluded because their marital history (if any) could not be determined and an additional 91 cases were dropped because of missing data on other baseline measures. The final analytic sample includes 2,197 adults aged 51 and older who contributed an average of 6 person-years over the 18-year observation period.
Measurement
A distinctive feature of the HRS is the prospective and retrospective design of data collection that allowed us to quantify the marital life of each study member over an extended period (more than 50 years). Marital information was ascertained from detailed responses to questions about the beginning and ending dates (reported in years and/or months) of all marriages, divorces, and/or widowhoods for the HRS participants. The respondents’ month/year-specific information was converted to age-specific data using date of birth, date of interview, and date of event. Although we cannot confirm the dates that respondents provided for the retrospective timing of marital events, research has shown “substantial agreement” between marital dates reported retrospectively and those reported by the same individuals in a panel design (Peters, 1988). The coding of study measures was facilitated by using cleaned data files provided by RAND’s Center for the Study of Aging (HRS, 2014).
Four categories of marital life are examined using the following measures. First, the timing of first marriage is dichotomized as early (ages 18 or younger; coded 1), on-time (reference group), or late (ages 30 or older; coded 1) marriage to capture non-normative entry in a marital union. Preliminary analyses assessed different cutpoints for men and women with early and late marriages and the results showed a generally consistent pattern of increasing risk with successively younger and older ages at first marriage. Second, several time-varying variables are dichotomized to indicate whether the individual is never married, remarried, divorced/separated, or widowed at a given age (each coded 1). The reference group is respondents who are continuously married (coded 0). Approximately 2% of older adults in the study reported cohabitation and most (~85%) had been previously married one or more times. Therefore, cohabiting respondents were categorized to their respective non-married status (i.e., never married, divorced, or widowed) to best reflect their marital history.
Third, marital transitions are operationalized as a time-varying measure of the cumulative number of marital losses (range=0–5). Preliminary analyses indicated that divorce and widowhood transitions had comparable risks for mortality; and the limited number of respondents who reported being widowed more than once (n=14) prohibited including separate measures for cumulative widowhoods and divorce. Finally, marriage duration is measured as the length of the longest marriage to capture respondents’ differential exposure to married life. Because marriage duration is dependent upon age, we operationalize marriage duration as the ratio of years married divided by age. For the majority of respondents (~85%), this duration reflects the entire time spent in a marriage (~15% are remarriages). Total marriage duration was not used because data were not available and because combining the length(s) of all marriages would confound the differentiation between marriage duration(s) from stable and multiple marital unions.
The multivariate models adjusted for background characteristics that include age at onset (in years), gender (male coded 1), race/ethnicity included as Hispanic (coded 1), non-Hispanic black (coded 1), non-Hispanic other race (coded 1), or non-Hispanic white (reference group), and geographic region (South coded 1). Several categories of previously identified risk factors and resources are also examined as possible mechanisms. Socioeconomic factors include the respondents’ educational attainment (in years), employment status (coded 1 if work limited by health), total non-housing wealth in thousands of dollars (logarithmic scale), and health insurance coverage from any source (coded 1 if no health insurance). Psychosocial factors include having no children (coded 1), no friends and/or relatives in the neighborhood (coded 1), never attends religious services (coded 1), and number of depressive symptoms measured by the 8-item abbreviated Center for Epidemiologic Studies Depression Scale (CES-D; range=0–8) Behavioral factors include current smoking status (coded 1 if currently smoking), alcohol use (coded 1 if ≥ 3 drinks per day), frequency of vigorous physical exercise (coded 1 if < 3 times per week), and medication adherence (coded 1 if does not take medication for new/existing hypertension or heart failure). Physiological factors include body mass index (BMI; calculated as weight in kilograms divided by height in meters squared; <18.5 [underweight; coded 1], 18.5–24.9 [normal weight; reference group], or ≥25.0 [overweight or obese; coded 1]), number of activities of daily living (ADL) limitations (range=0–5), diagnosed chronic illness (coded 1 if diagnosed with hypertension, diabetes, chronic obstructive pulmonary disease, or cancer), and recurrent heart attack (coded 1).
Preliminary analyses also included variables to adjust for study cohort (e.g., original HRS, CODA, EBB), urban-rural residence, lifetime occupational status, household income, and spouses sampled from the same HRS-selected households; however, results were not significant and the variables were dropped from the final models. Alternative coding strategies were also assessed for the continuous variables (e.g., logged, polynomial, and grouped-ordinal scales) and categorical variables (e.g., different cutpoints, categories, and reference groups) and did not alter the central findings. All measures are time varying and time lagged (observed in the previous wave [i.e., within the prior 24 months]—with the exception of age, gender, and race/ethnicity) in the prospective analyses to establish temporal order when estimating the associations between the covariates and subsequent mortality. Alternative lag times (e.g., no lag, 12-months, 48-months, etc.) also were assessed in preliminary analyses and produced largely consistent results.
Mortality from all causes was the outcome for analysis. Deaths from all causes were included because the majority of studies examining survival after a heart attack include all-cause mortality as the outcome (Kilpi et al. 2015; Lammintausta et al., 2013; Nielsen and Mard, 2010; Vaccarino et al., 1999) and because most adults who suffer a heart attack die from other causes (Go et al., 2014). Respondents who died were identified from the HRS tracking file and matches to the National Death Index (see HRS, 2014). Time until death was calculated from the participants’ date of onset and date of death. Individuals who could not be identified as deceased and persons who survived through 2010 were considered censored observations. We also recognize that some adults experienced sudden death following a heart attack; however, research shows that the vast majority of adults with a heart attack survive to the hospital and more than 90% are discharged alive (Floyd et al., 2009; Go et al., 2014). A person-year file was constructed from the respondents’ cumulative exposure to death so that each observation was a record for every additional year beyond their age at onset. A total of 1,217 deaths (55%) were reported during the 17,615 person-years of observation.
Statistical Analysis
Baseline distributions of the study variables were computed for all participants and by survival status. Bivariate comparisons were calculated with 2-tailed t tests for continuous and count variables and χ2 tests for categorical variables. Discrete-time hazard models were then used to estimate odds ratios (ORs) for the adjusted risks of mortality associated with marital factors and other covariates. The hazard rate is defined as the conditional probability that an individual who suffered a heart attack will die at time t, given that the individual was alive at the beginning of time t. Different functional forms were evaluated (e.g., piecewise exponential, log-linear, curvilinear) to determine the parametric specification that best captured the mortality distribution over time (t). A linear function of the log odds was the best fitting and most parsimonious of those evaluated based on graphical plots and Bayesian information criterion (BIC; Raftery, 1995). Time was also parameterized as a function of age in preliminary analyses and the results were consistent.
The discrete-time models are conducted in two steps. First, two sets of multivariate models are estimated to examine the risks of dying associated with marriage timing, marital status, marital transitions, and marriage duration. Model 1 includes age at onset, race, ethnicity, and geographic region and Model 2 further includes interactions between time and the marital variables to assess whether and how the associations change over time since the occurrence of the heart attack. The adjusted odds estimated from Model 2 are then plotted to illustrate the differences over time. The second series of multivariate analyses examine the socioeconomic, psychosocial, behavioral, and physiological factors thought to explain the marital differences in survival following a heart attack. Model fit and reductions in estimated ORs across models (i.e., mediating effects) were assessed using BIC statistics and KHB methods (Karlson, Holm, and Breen 2010), respectively. The associations are also assessed for differences by gender and race/ethnicity.
Four sets of sensitivity analyses were also conducted. First, complementary log-log models and Cox proportional hazard models were estimated (based on age and time since onset) and the results were nearly identical to those presented here, with only negligible changes in the point estimates and confidence intervals (CIs). Preliminary estimates also showed that the reported ORs approximate closely to relative risks (± .05−.001). Second, we assessed whether selective survival may have contributed to the findings. Excluding adults over the age of 90 at baseline (n=189; 9%) produced results that were largely unchanged. Third, although missing data was minimal across study variables for follow-up measurements (~ 2–3%), preliminary analyses showed that the results were unchanged using multivariate imputation, mean replacement, and forward imputation from baseline/prior interview data (used here). Finally, separate analyses were run for the four categories of marital measures to avoid over-identified models. Preliminary analyses indicated significant bivariate correlations and moderate degree of multicollinearity in the fitted models—condition values were > 60, with the largest variance decomposition proportions and variance inflation factors among the marital status and transition variables.
The data are not weighted because the study focuses on a selective subsample of HRS respondents (heart attack survivors) and the multivariate models include variables related to initial sample selection (age, sex, race, region) to produce unbiased estimates (Winship and Radbill, 1994). Preliminary analyses confirmed that the overall patterns and conclusions were similar between the weighted and unweighted data. Analyses were conducted using Stata 13.0.
RESULTS
Table 1 presents the baseline characteristics of the study participants for the entire sample and by survival status. Following a heart attack, respondents who died are significantly more likely to be older, non-Hispanic black, have less education, lower levels of wealth, and less employment due to their health compared with respondents who survived through the study period. Those who survived are also more likely to exercise, have fewer depressive symptoms, take their medications, have higher BMI, fewer ADL limitations, and are less likely to have other diagnosed chronic illness. In terms of marital experiences, adults who married on-time (ages 19–29) and those who are currently married—either in a stable 1st marriage or remarriage—are significantly more likely to survive after a heart attack than their non-married counterparts. There are no significant differences in survival for the cumulative number of marital losses and duration of marriage at baseline.
Table 1.
Characteristics of Study Participants from the Health and Retirement Study at Baseline
| Total (n = 2,197) |
Survived (n = 980) |
Died (n = 1,217) |
|
|---|---|---|---|
| Sociodemographic Background | |||
| Age at onset | 69.46 (11.30) | 65.45 (9.61) | 72.69 (11.52)*** |
| Male | 55.08 | 56.02 | 54.31 |
| Non-Hispanic black | 13.93 | 11.84 | 15.61 * |
| Non-Hispanic other race | 2.00 | 2.24 | 1.81 |
| Hispanic | 7.46 | 8.27 | 6.82 |
| Lives in the South | 44.24 | 43.57 | 44.78 |
| Marriage Timing | |||
| Early 1st marriage | 14.83 | 15.69 | 14.13 |
| On-time 1st marriage | 68.16 | 72.59 | 64.60 *** |
| Late 1st marriage | 17.02 | 11.72 | 21.28 *** |
| Marital Status | |||
| Never married | 2.37 | 2.45 | 2.30 |
| Continuously married | 41.65 | 46.43 | 37.80 *** |
| Remarried | 20.07 | 23.88 | 17.10 *** |
| Divorced | 12.34 | 12.55 | 12.16 |
| Widowed | 23.58 | 14.69 | 30.73 *** |
| Marital Transitions | |||
| Number of marital losses (0–5) | 0.64 (0.76) | 0.64 (0.80) | 0.64 (0.72) |
| Marriage Duration† | |||
| Length of longest marriage (%) | 49.49 (21.11) | 49.53 (20.45) | 49.46 (21.63) |
| Socioeconomic Factors | |||
| Years of education | 11.44 (3.37) | 12.06 (3.18) | 10.94 (3.43)*** |
| Wealth in thousands of dollars | 168.01 (478.52) | 194.39 (508.09) | 146.78 (452.40)* |
| Employment limited by health | 53.39 | 42.55 | 62.12 *** |
| No health insurance | 5.96 | 6.53 | 6.90 |
| Psychosocial Factors | |||
| No children | 6.33 | 5.61 | 6.90 |
| No nearby friends and/or relatives | 20.35 | 21.73 | 19.23 |
| Never attends religious services | 26.22 | 26.33 | 26.13 |
| CES-D depressive symptoms (0–8) | 2.24 (2.27) | 1.96 (2.25) | 2.46 (2.26)*** |
| Behavioral Factors | |||
| Current smoker | 19.03 | 18.37 | 19.56 |
| Drinks alcohol in excess | 12.29 | 15.82 | 9.45 *** |
| No vigorous exercise | 77.15 | 70.71 | 82.33 *** |
| Does not take medication | 16.25 | 12.76 | 19.06 *** |
| Physiological Factors | |||
| Underweight, BMI < 18.5 | 2.46 | 1.12 | 3.53 *** |
| Overweight or obese, BMI ≥ 25.0 | 65.73 | 73.27 | 59.65 *** |
| ADL limitations (0–5) | 0.65 (1.27) | 0.35 (.885) | 0.90 (1.46)*** |
| Diagnosed chronic illness | 78.33 | 73.78 | 82.00 *** |
| Recurrent heart attack | 18.02 | 18.27 | 17.83 |
p ≤ .05;
p ≤ .01;
p ≤ .001 (two-tailed test).
Measured as a ratio of (years married/age) × 100.
Table 2 presents the discrete-time estimates for the associations between each measure of marital life and the risk of dying while adjusting for sociodemographic background. Model 1 shows that surviving after a heart attack is significantly related to marital status, marital transitions, and marital duration; but not marital timing. Respondents who never married (OR=1.73 [=exp(0.55)]; p < .008), currently divorced (OR=1.70 [=exp(0.53)]; p ≤ .001), or widowed (OR=1.34 [=exp(0.29)]; p ≤ .001) are at greater risk of dying than respondents who are continuously married. Likewise, the risk of dying after a heart attack increases by 12% (= 100*[exp(0.11) − 1]; p=.012) for every additional marital loss. Alternatively, for every 10% increase in the proportion of years married, the risk of dying decreases by approximately 7% (p ≤ .001).
TABLE 2.
Discrete-Time Estimates for Mortality after a Heart Attack Associated with Marital History in U.S. Older Adults
| Coefficient (SE) | ||
|---|---|---|
| Model 1 | Model 2 | |
| I. Marriage Timing | ||
| Early marriage | .16 (.10) |
−.06 (.18) |
| Late marriage | .14 (.08) |
−.03 (.15) |
| Early marriage × Time | .03 (.02) |
|
| Late marriage × Time | .03 (.02) |
|
| II. Marital Status | ||
| Never married | .55** (.21) |
1.23*** (.34) |
| Remarried | .05 (.09) |
.52** (.17) |
| Divorced | .53*** (.10) |
.66*** (.19) |
| Widowed | .29*** (.08) |
.23 (.15) |
| Never married × Time | −.11* (.05) |
|
| Remarried × Time | −.07** (.02) |
|
| Divorced × Time | −.02 (.02) |
|
| Widowed × Time | .01 (.02) |
|
| III. Marital Transitions | ||
| Number of marital losses | .11* (.04) |
.15 (.08) |
| Number of marital losses × Time | −.01 (.01) |
|
| IV. Marriage Duration† | ||
| Length of longest marriage | −.07*** (.02) |
−.07* (.03) |
| Length of longest marriage × Time | −.00 (.00) |
|
Note: The reference group for marital timing is on-time marriage; the reference group for marital status is continuously married. Analyses were conducted separately for each category of marital variables.
Models adjust for age at onset, gender, race, ethnicity, and geographic region.
Measured as a ratio of years married/age.
p ≤ .05;
p ≤ .01;
p ≤ .001 (two-tailed test).
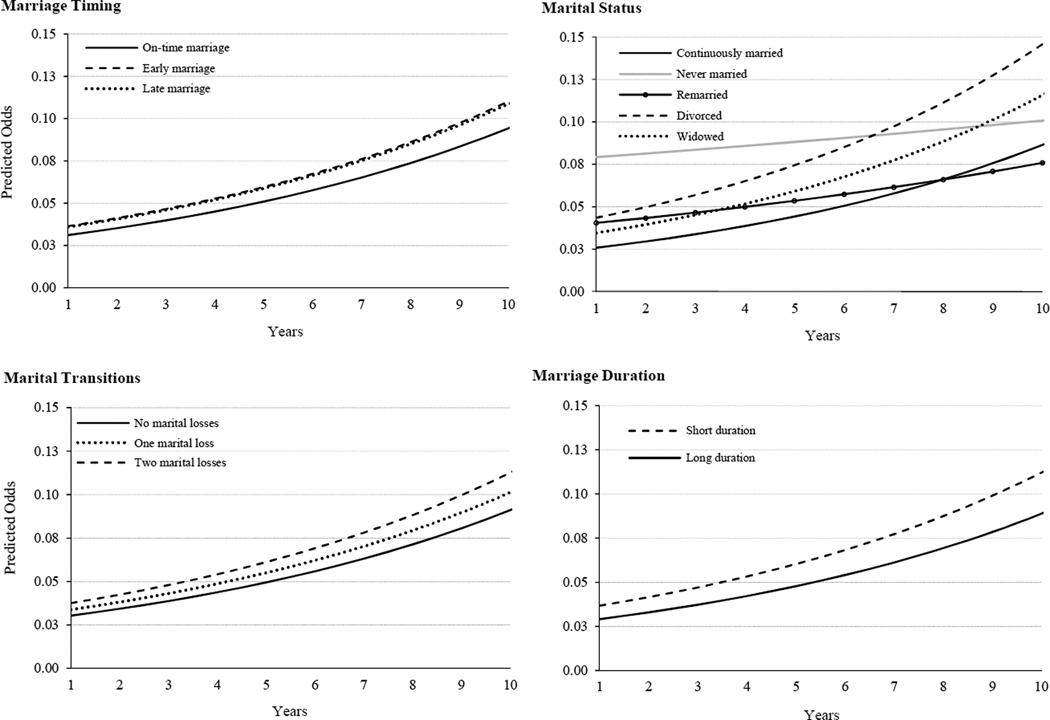
Model 2 includes interaction terms for time (since heart attack) and each of the marital factors and shows significant changes in the associations for marital status, but not for marital timing, marital transitions, or marriage duration. To better illustrate these findings, the predicted odds of mortality in Model 2 are plotted in Figure 1. Overall, the risks associated with current marital status are more pronounced than the risks associated with other dimensions of marital history. The predicted odds of dying associated with the number of marital losses and the duration of marriage are similar in magnitude and patterning over time—with slightly larger disparities in predicted odds in later years as a cumulative function of the log-linear risks that increase with time. The elevated risks in adults who are currently divorced or widowed are larger and follow the same pattern of increase over time. In the time immediately after a heart attack, the odds of dying are greatest in adults who never married. The results for remarriage follow a similar pattern. Older adults who are remarried have the largest increase in mortality in the first years after suffering a heart attack compared with older adults who remained continuously married. After approximately 8 years, however, the predicted rates for remarried and continuously married adults are largely the same.
Figure 1.
Predicted Odds of Mortality after a Heart Attack by Marital History in U.S. Older Adults
Note: Predicted odds are based on estimates in Model 2 in Table 2. Non-significant interaction terms were omitted from the equations when illustrating the results in the figure. Marriage duration is illustrated at 33% (short) and 66% (long) as the ratio of longest marriage in years/age.
Table 3 presents the results from a series of models examining the potential factors contributing to marital differences in mortality following a heart attack. As previously shown, marital timing has no significant association with survival. For marital status, the adjusted models suggest that socioeconomic factors (predominantly wealth) contribute to the largest reductions in mortality risks associated with being never married, divorced, and widowed (18%, 30%, and 40% reductions, respectively, according to KHB estimates). The increased mortality associated with remarriage is attenuated most by behavioral factors in Model 4 (40% reduction)—and primarily attributable to smoking and exercise. With the exception of widowhood in the final model, the overall patterning of mortality risks related to marital status remained robust and statistically significant despite accounting for nearly two dozen explanatory variables (Model 6).
Table 3.
Adjusted Discrete-Time Estimates for Mortality after a Heart Attack Associated with Marital History in U.S. Older Adults
| Coefficient (SE) | ||||||
|---|---|---|---|---|---|---|
| Model 1: Demographic Factors |
Model 2: SES Factors |
Model 3: Psychosocial Factors |
Model 4: Behavioral Factors |
Model 5: Physiological Factors |
Model 6: Full Model |
|
| I. Marriage Timing | ||||||
| Early marriage | .16 (.10) |
.05 (.10) |
.11 (.10) |
.11 (.10) |
.05 (.10) |
−.03 (.10) |
| Late marriage | .14 (.08) |
.06 (.08) |
.11 (.08) |
.10 (.08) |
−.03 (.08) |
−.06 (.08) |
| II. Marital Status | ||||||
| Never married | 1.23*** (.33) |
1.13*** (.34) |
1.22*** (.35) |
1.27*** (.34) |
1.15*** (.34) |
1.32*** (.35) |
| Remarried | .51*** (.15) |
.49** (.15) |
.49** (.16) |
.47** (.15) |
.48** (.16) |
.44** (.16) |
| Divorced | .52*** (.10) |
.37*** (.11) |
.42*** (.11) |
.47*** (.10) |
.47*** (.10) |
.35** (.11) |
| Widowed | .29*** (.08) |
.18* (.09) |
.24** (.08) |
.23** (.08) |
.20* (.09) |
.13 (.09) |
| Never married × Time | −.11* (.05) |
−.11* (.05) |
−.11* (.05) |
−.11* (.05) |
−.10* (.05) |
−.12* (.05) |
| Remarried × Time | −.06*** (.02) |
−.06*** (.02) |
−.07*** (.02) |
−.06*** (.02) |
−.06*** (.02) |
−.06*** (.02) |
| III. Marital Transitions | ||||||
| Number of marital losses | .11* (.04) |
.04 (.04) |
.06 (.04) |
.06 (.04) |
.06 (.04) |
−.02 (.04) |
| IV. Marriage Duration† | ||||||
| Length of longest marriage | −.07*** (.02) |
−.05** (.02) |
−.06*** (.02) |
−.06*** (.02) |
−.07*** (.02) |
−.05** (.02) |
Note: The reference group for marital timing is on-time marriage; the reference group for marital status is continuously married. Analyses were conducted separately for each category of marital variables.
Measured as a ratio of years married/age.
Model 1 adjusts for age at onset, gender, race, ethnicity, and geographic region.
Model 2 includes model 1 covariates and adds education level, limited employment, wealth, and health insurance.
Model 3 includes model 1 covariates and adds any children, nearby friends/relatives, religious attendance, and CES-D depressive symptoms.
Model 4 includes model 1 covariates and adds smoking, alcohol use, physical exercise, and medication use.
Model 5 includes model 1 covariates and adds body mass index, limitations in activities of daily living, diagnosed chronic illness, and recurrent heart attack.
Model 6 includes all covariates.
p ≤ .05;
p ≤ .01;
p ≤ .001 (two-tailed test).
The cumulative number of marital losses has the overall weakest relationship with the risks of dying after a heart attack (OR=1.12; p < .05) and the association is mediated by a similar degree for three categories of covariates (Models 3–5) and mediated most by the socioeconomic factors in Model 2 (61% overall reduction; with 42% due to wealth). The protective effect of marriage duration remains significant and largely unchanged across each of the explanatory models. However, the inclusion of the socioeconomic covariates in Model 2 exhibits the largest attenuation of the association between marriage duration and survival after a heart attack (with the largest reduction attributable to wealth [24%]).
According to estimated BIC statistics (not presented), current marital status has more overall explanatory power than other dimensions of marital history. With regard to the explanatory variables, the models with physiological factors (Model 5) exhibit the greatest overall model fit for estimating the risk of dying after a heart attack—although these factors appear to be operating largely independent of the marital variables. Among the key mediating factors, the lowest estimated BIC values are consistent with the reductions in coefficients and significance levels described above. Supplementary analyses were also conducted to examine whether the associations for the marital factors varied for men and women or by race/ethnicity. Of the more than two dozen interactions that were tested, there was no evidence that the key findings significantly differed by gender or race/ethnicity.
DISCUSSION
Nearly one million Americans will have a heart attack this year and upwards of 9 million adults are currently alive after suffering a heart attack (Go et al., 2014). This study provides new evidence of how various dimensions of marital life contribute to survival in those who are afflicted with this prevalent cardiovascular event. The results from this study are a departure from recent research demonstrating the cumulative and lasting effects of marital loss on the onset of disease. Instead, we find that current marital status is the most robust indicator of survival in adults who suffered a heart attack. Furthermore, we find that some associations vary over time since the occurrence of a heart attack and many of the marital factors are not fully accounted for by socioeconomic, psychosocial, behavioral, or physiological factors.
Contrary to existing research on the incidence of a heart attack (Dupre et al., 2015; Lindegard et al., 1985; Zhang and Hayward, 2006), we find limited or no evidence of an association between past marital transitions and the timing of first marriage with the risk of dying after a heart attack. Rather, we demonstrate that indicators of marital life that are more contemporaneous with the cardiac event are more salient for understanding how long older adults survive after a heart attack. Compared with adults who are continuously married, we find that those who are not currently married are at the greatest risk of dying after suffering a heart attack. The odds of dying after a heart attack are large and especially pronounced immediately following the health event for adults who never married. This finding is consistent with previous research in other countries showing sizeable risks of mortality in never married adults following a coronary event (Gerward et al., 2010; Lammintausta et al., 2013). Although the increased mortality among the never married in the current study was explained most by socioeconomic resources such as wealth, our study does not fully explain the sizeable risks of death relative to their continuously married counterparts—particularly in the first two years after a heart attack (OR=3.32–2.64 in years 1–3).
In terms of divorce and widowhood, we also find that the elevated risks of dying after a heart attack are large over time (ORs=1.69 and 1.34, respectively) compared with continuous marriage. Much of these risks are explained by the socioeconomic resources available for recovery; a finding that is supported by recent research in Finland (Kilpi et al., 2015); however, divorce status remains a significant risk factor for dying after a heart attack. We suspect that more detailed measures of instrumental and emotional support may further account for how being unmarried is detrimental to survival after a heart attack. Therefore, we encourage additional research to explore these and other potential mechanism(s)—particularly as they relate to unmeasured dimensions of psychosocial stress (e.g., anxiety, low self-efficacy) that may accompany the lower socioeconomic standing of those who are not married.
In terms of marriage duration, we find that those who spent the largest proportion of their adult life in a marital union have a significant survival advantage over those who spent less time married. It is argued that long, continuous marriages provide stability in socioeconomic, behavioral, and psychosocial resources that accumulate and solidify over time. However, much like marital status, accounting for more than a dozen covariates did not fully explain the association. Faced with a heart attack, we suspect that those with long durations of marriage draw from multiple protracted resources to better manage disease and prolong survival after experiencing a life-threatening event. Therefore, future studies are needed to test these arguments and to explore alternative measures that better capture long-term exposure to such risks and resources.
Two notable findings also warrant comment. First, we find that remarried adults have slightly greater odds of dying compared with continuously married adults in the first years after a heart attack but not thereafter. We also find that this association is attributed most to differences in behavioral factors such as exercise and smoking. This suggests that having a spouse from a subsequent marriage (relative to one stable partner) may not confer the same level of social control, shared obligations, and concordant behaviors that promote the avoidance/cessation of smoking, medication adherence, and other behaviors that are important for managing illness (Husaini et al., 2001; Kamon et al., 2008; Umberson, 1992). Indeed, recent research suggests that smoking behavior plays a significant role in marital differences in long-term survival following cardiac surgery (Idler et la., 2012). A second notable finding is that marital timing has no association with survival after a heart attack. Other studies have demonstrated significant risks associated with early marriage and disease incidence (Dupre 2016; Zhang and Hayward, 2006); however, this study suggests that marriage timing does not influence the likelihood of dying following the onset of a major cardiovascular event. Although more research is needed to further substantiate these results, this finding is consistent with demonstrating the importance of marital factors that are most proximate to the health event.
Our analysis of potential mediators suggests that socioeconomic resources—namely available wealth and assets—play an important role for those recovering from a heart attack. This finding supports recent research from Finland that suggests the lack of material resources contributes to the survival disadvantage of persons living alone after a heart attack compared with those who were married (Kilpi et al., 2015). These findings are also largely consistent with previous research showing that married couples generally have greater access to medical insurance, prescription drugs, and overall higher quality of health care (Fletcher, 1988; Zuvekas and Taliaferro, 2003). Conversely, lacking shared financial resources that often accompany marital unions may have consequences for purchasing equipment for physical fitness, maintaining a heart-healthy diet, and affording other resources for cardiac rehabilitation to improve chances of survival (Go et al., 2014; Lillard and Waite, 1995; Zuvekas and Taliaferro, 2003).
The results of this study are not without limitations. First, we recognize that the analyses are based on self-reported heart attacks and not medical evaluations. However, studies show considerable consistency between diagnostic reports of heart attacks from survey respondents and those from medical evaluations—with self-reported data having a high degree of overall agreement—i.e., sensitivity and specificity—with medical data (Harlow and Linet, 1989; Okura et al., 2004). Furthermore, recent studies from Sweden and Finland report similar associations to those shown here when using data from patient registries (Gerward et al., 2010; Kilpi et al., 2015; Lammintausta et al., 2013). Nevertheless, future studies may be warranted to validate the current findings with medical assessments. Second, and relatedly, the study is limited to adults who survive to hospital discharge. Although studies show that the majority of adults with a heart attack survive to the hospital and most (~90%) are discharged alive (Floyd et al., 2009; Go et al., 2014), we cannot rule out potential selection bias related to those who died shortly after suffering a heart attack. Therefore, it is possible that the associations may be underestimated due to selective mortality occurring prior to hospitalization in those with marital instability. Relatedly, we recognize that some of the association(s) may be due to the selection of individuals into/out of marriage.
Third, although the data were rich in the number and scope of measured covariates, it is possible that additional unmeasured factors may have contributed to the findings. For example, data were not available for the treatment and control of hypertension and diabetes; or other clinical factors (e.g., cardiac rehabilitation) that improve the likelihood of survival after an acute cardiovascular event. We also could not identify the characteristics or quality of past marriages or the circumstances of marital loss. Likewise, we lacked direct measures of stress and anxiety that follow a heart attack (and divorce/widowhood), which may contribute to the association between marital experiences and subsequent mortality. Finally, we lacked data on the timing—start/end dates—for cohabitation and separation and encourage other studies to explore how these (non)marital relationships may also impact survival after a heart attack.
In sum, the results from this study provide new evidence that has the potential to inform health policy and practice. Although marital events are not amenable to medical intervention or treatment, knowledge about the risks associated with marital life may be useful for personalizing care and improving prognoses for those who suffered a heart attack. For example, older adults who are divorced—as well as those who were married for a short period of time—may benefit from additional screening and/or monitoring during their recovery period. Likewise, older adults who never married or remarried may benefit most from immediate follow-up after their event to prevent a recurrent heart attack or premature mortality. Greater recognition and understanding of these processes will enable health care providers to better identify and treat older adults with illness who are at potentially high risk of dying, as well as provide older adults a new (or heightened) awareness of their social risks that go beyond the cautionary litany of poor diet, inactivity, and smoking. Future studies are needed to further examine the mechanisms contributing to these associations and to assess how such information can be used to aggressively treat these vulnerable segments of the population.
Highlights.
Deepens our understanding of how social relationships impact disease prognosis.
Marital status is a robust indicator of survival after a heart attack.
Risks from past marital loss are not ameliorated with remarriage.
Implications for health policy and practice are discussed.
Acknowledgments
Support for this study was provided by the National Institute on Aging (R03AG042712).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Addo Fenaba R, Lichter Daniel T. Marriage, marital history, and Black–White wealth differentials among older women. Journal of Marriage and Family. 2013;75(2):342–362. [Google Scholar]
- August Kristin J, Sorkin Dara H. Marital status and gender differences in managing a chronic illness: The function of health-related social control. Social Science & Medicine. 2010;71(10):1831–1838. doi: 10.1016/j.socscimed.2010.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth Alan, Edwards John N. Age at marriage and marital instability. Journal of Marriage and the Family. 1985:67–75. [Google Scholar]
- Brockmann Hilke, Klein Thomas. Love and death in Germany: The marital biography and its effect on mortality. Journal of Marriage and Family. 2004;66(3):567–581. [Google Scholar]
- Brown Peter C, Smith Timothy W. Social influence, marriage, and the heart: cardiovascular consequences of interpersonal control in husbands and wives. Health Psychology. 1992;11(2):88. doi: 10.1037//0278-6133.11.2.88. [DOI] [PubMed] [Google Scholar]
- Burnley Ian H. Transitions and inequalities in acute myocardial infarction mortality in New South Wales, 1969–94. Australian and New Zealand journal of public health. 1999;23(4):343–351. doi: 10.1111/j.1467-842x.1999.tb01273.x. [DOI] [PubMed] [Google Scholar]
- Chandra Vijay, Szklo Moyses, Goldberg Robert, Tonascia James. The impact of marital status on survival after an acute myocardial infarction: a population-based study. American Journal of Epidemiology. 1983;117(3):320–325. doi: 10.1093/oxfordjournals.aje.a113544. [DOI] [PubMed] [Google Scholar]
- Das Aniruddha. Spousal Loss and Health in Late Life Moving Beyond Emotional Trauma. Journal of aging and health. 2013;25(2):221–242. doi: 10.1177/0898264312464498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Castelnuovo Augusto, Quacquaruccio Gianni, Donati Maria Benedetta, de Gaetano Giovanni, Iacoviello Licia. Spousal concordance for major coronary risk factors: a systematic review and meta-analysis. American journal of epidemiology. 2009;169(1):1–8. doi: 10.1093/aje/kwn234. [DOI] [PubMed] [Google Scholar]
- Duncan Greg J, Hoffman Saul D. A reconsideration of the economic consequences of marital dissolution. Demography. 1985;22(4):485–497. [PubMed] [Google Scholar]
- Dupre Matthew E. Race, Marital History, and Risks for Stroke in US Older Adults. Social Forces. 2016 doi: 10.1093/sf/sow040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre Matthew E, Beck Audrey N, Meadows Sarah O. Marital trajectories and mortality among US adults. American Journal of Epidemiology. 2009;170(5):546–555. doi: 10.1093/aje/kwp194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre Matthew E, George Linda K, Liu Guangya, Peterson Eric D. Association between divorce and risks for acute myocardial infarction. Circulation: Cardiovascular Quality and Outcomes. 2015;8(3):244–251. doi: 10.1161/CIRCOUTCOMES.114.001291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaker Elaine D, Sullivan Lisa M, Kelly-Hayes Margaret, D’Agostino Ralph B, Sr, Benjamin Emelia J. Marital status, marital strain, and risk of coronary heart disease or total mortality: the Framingham Offspring Study. Psychosomatic medicine. 2007;69(6):509–513. doi: 10.1097/PSY.0b013e3180f62357. [DOI] [PubMed] [Google Scholar]
- Elder Jr, Monica Glen H, Johnson Kirkpatrick, Crosnoe Robert. The emergence and development of life course theory. Springer; 2003. [Google Scholar]
- Fletcher Ben C. Occupation, marriage and disease-specific mortality concordance. Social Science & Medicine. 1988;27(6):615–622. doi: 10.1016/0277-9536(88)90009-3. [DOI] [PubMed] [Google Scholar]
- Floyd KC, Yarzebski J, Spencer FA, et al. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circulation Cardiovascular quality and outcomes. 2009;2(2):88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forthofer Melinda S, Kessler Ronald C, Story Amber L, Gotlib Ian H. The effects of psychiatric disorders on the probability and timing of first marriage. Journal of Health and Social Behavior. 1996:121–132. [PubMed] [Google Scholar]
- Franks Melissa M, Pienta Amy Mehraban, Wray Linda A. It Takes Two Marriage and Smoking Cessation in the Middle Years. Journal of Aging and Health. 2002;14(3):336–354. doi: 10.1177/08964302014003002. [DOI] [PubMed] [Google Scholar]
- Gerward S, Tydén P, Engström G, Hedblad B. Marital status and occupation in relation to short-term case fatality after a first coronary event-a population based cohort. BMC Public Health. 2010;10(1):1. doi: 10.1186/1471-2458-10-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go Alan S, Mozaffarian Dariush, Roger Veronique L, Benjamin Emelia J, Berry Jarett D, Blaha Michael J, Dai Shifan, Ford Earl S, Fox Caroline S, Franco Sheila. Heart disease and stroke statistics-2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gove Walter R, Shin Hee-Choon. The psychological well-being of divorced and widowed men and women an empirical analysis. Journal of Family Issues. 1989;10(1):122–144. [Google Scholar]
- Green Kerry M, Doherty Elaine E, Fothergill Kate E, Ensminger Margaret E. Marriage trajectories and health risk behaviors throughout adulthood among urban African Americans. Journal of Family Issues. 2012 doi: 10.1177/0192513X11432429. 0192513X11432429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy Emily MD, Tomassini Cecilia. Marital history, health and mortality among older men and women in England and Wales. BMC public health. 2010;10(1):554. doi: 10.1186/1471-2458-10-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harlow Sioban D, Linet Martha S. Agreement between questionnaire data and medical records: the evidence for accuracy of recall. American Journal of Epidemiology. 1989;129(2):233–248. doi: 10.1093/oxfordjournals.aje.a115129. [DOI] [PubMed] [Google Scholar]
- Heaton Tim B. Time-related determinants of marital dissolution. Journal of Marriage and the Family. 1991:285–295. [Google Scholar]
- Hemström Örjan. Is marriage dissolution linked to differences in mortality risks for men and women? Journal of Marriage and the Family. 1996:366–378. [Google Scholar]
- Hughes Mary Elizabeth, Waite Linda J. Marital biography and health at mid-life. Journal of health and social behavior. 2009;50(3):344–358. doi: 10.1177/002214650905000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husaini Baqar A, Sherkat Darren E, Bragg Richard, Levine Robert, Emerson Janice S, Mentes Christina M, Cain Van A. Predictors of breast cancer screening in a panel study of African American women. Women & health. 2001;34(3):35–51. doi: 10.1300/J013v34n03_03. [DOI] [PubMed] [Google Scholar]
- Idler EL, Boulifard DA, Contrada RJ. Mending broken hearts: Marriage and survival following cardiac surgery. Journal of Health and Behavior. 2012;53(1):33–49. doi: 10.1177/0022146511432342. [DOI] [PubMed] [Google Scholar]
- Juster F Thomas, Suzman Richard. An overview of the Health and Retirement Study. Journal of Human Resources. 1995:S7–S56. [Google Scholar]
- Kilpi F, Konttinen H, Silventoinen K, Martikainen P. Living arrangements as determinants of myocardial infarction incidence and survival: A prospective register study of over 300,000 Finnish men and women. Social Science & Medicine. 2015;133:93–100. doi: 10.1016/j.socscimed.2015.03.054. [DOI] [PubMed] [Google Scholar]
- Koskenvuo Markku, Kaprio Jaakko, Kesäniemi Antero, Sarna Seppo. Differences in mortality from ischemic heart disease by marital status and social class. Journal of chronic diseases. 1980;33(2):95–106. doi: 10.1016/0021-9681(80)90033-8. [DOI] [PubMed] [Google Scholar]
- Lammintausta Aino, Airaksinen Juhani KE, Immonen-Räihä Pirjo, Torppa Jorma, Kesäniemi Antero Y, Ketonen Matti, Koukkunen Heli, et al. Prognosis of acute coronary events is worse in patients living alone: the FINAMI myocardial infarction register. European journal of preventive cardiology. 2013;21(8):989–996. doi: 10.1177/2047487313475893. [DOI] [PubMed] [Google Scholar]
- Lillard Lee A, Waite Linda J. 'Til death do us part: Marital disruption and mortality. American Journal of Sociology. 1995:1131–1156. [Google Scholar]
- Lindegård B, Langman MJ. Marital state, alcohol consumption, and liability to myocardial infarction, stroke, diabetes mellitus, or hypertension in men from Gothenburg. British medical journal (Clinical research ed.) 1985;291(6508):1529. doi: 10.1136/bmj.291.6508.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund Rikke, Holstein Bjørn Evald, Osler Merete. Marital history from age 15 to 40 years and subsequent 10-year mortality: a longitudinal study of Danish males born in 1953. International Journal of Epidemiology. 2004;33(2):389–397. doi: 10.1093/ije/dyh065. [DOI] [PubMed] [Google Scholar]
- Marks Nadine F, Lambert James David. Marital status continuity and change among young and midlife adults longitudinal effects on psychological well-being. Journal of Family Issues. 1998;19(6):652–686. [Google Scholar]
- McFarland Michael, Hayward Mark D, Brown Dustin. I've Got You Under My Skin: Marital Biography and Biological Risk. Journal of Marriage and Family. 2013;75(2):363–380. doi: 10.1111/jomf.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin Diane K, Lichter Daniel T, Johnston Gail M. Some women marry young: Transitions to first marriage in metropolitan and nonmetropolitan areas. Journal of Marriage and the Family. 1993:827–838. [Google Scholar]
- McManus Patricia A, DiPrete Thomas A. Losers and winners: The financial consequences of separation and divorce for men. American Sociological Review. 2001:246–268. [Google Scholar]
- Meyler Deanna, Stimpson Jim P, Peek M Kristen. Health concordance within couples: a systematic review. Social science & medicine. 2007;64(11):2297–2310. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Miller Joan F, McConnell Timothy R, Klinger Troy A. Religiosity and spirituality: Influence on quality of life and perceived patient self-efficacy among cardiac patients and their spouses. Journal of Religion and Health. 2007;46(2):299–313. [Google Scholar]
- Molloy Gerard John, Stamatakis Emmanuel, Randall Gemma, Hamer Mark. Marital status, gender and cardiovascular mortality: behavioural, psychological distress and metabolic explanations. Social science & medicine. 2009;69(2):223–228. doi: 10.1016/j.socscimed.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mookadam Farouk, Arthur Heather M. Social support and its relationship to morbidity and mortality after acute myocardial infarction: systematic overview. Archives of Internal Medicine. 2004;164(14):1514–1518. doi: 10.1001/archinte.164.14.1514. [DOI] [PubMed] [Google Scholar]
- Morgan S Philip, Rindfuss Ronald R. Marital Disruption: Structual and Temporal Dimensions. American Journal of Sociology. 1985:1055–1077. [Google Scholar]
- Nielsen Finn Erland, Mard Shan. Single-living is associated with increased risk of long-term mortality among employed patients with acute myocardial infarction. Clinical epidemiology. 2010;2:91. doi: 10.2147/clep.s8975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okura Yuji, Urban Lynn H, Mahoney Douglas W, Jacobsen Steven J, Rodeheffer Richard J. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. Journal of clinical epidemiology. 2004;57(10):1096–1103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Peters H Elizabeth. Retrospective versus panel data in analyzing lifecycle events. Journal of Human Resources. 1988:488–513. [Google Scholar]
- Pienta Amy Mehraban, Hayward Mark D, Jenkins Kristi Rahrig. Health consequences of marriage for the retirement years. Journal of Family Issues. 2000;21(5):559–586. [Google Scholar]
- Profant Judi, Dimsdale Joel E. Race and Diurnal Blood Pressure Patterns A Review and Meta-Analysis. Hypertension. 1999;33(5):1099–1104. doi: 10.1161/01.hyp.33.5.1099. [DOI] [PubMed] [Google Scholar]
- Ross Catherine E, Mirowsky John, Goldsteen Karen. The impact of the family on health: The decade in review. Journal of Marriage and the Family. 1990;52(4):1059–1078. [Google Scholar]
- Sbarra David A, Law Rita W, Lee Lauren A, Mason Ashley E. Marital dissolution and blood pressure reactivity: Evidence for the specificity of emotional intrusion-hyperarousal and task-rated emotional difficulty. Psychosomatic Medicine. 2009;71(5):532–540. doi: 10.1097/PSY.0b013e3181a23eee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith James P. Marriage assets and savings. 1995 [Google Scholar]
- Spanier Graham B, Roos Patricia A, Shockey James. Marital trajectories of American women: Variations in the life course. Journal of Marriage and the Family. 1985:993–1003. [Google Scholar]
- Torio CM, Andrews RM. National inpatient hospital costs: the most expensive conditions by payer, 2011. Healthcare Cost and Utilization Project Statistical Brief#. 2013;160 [PubMed] [Google Scholar]
- Umberson Debra. Family status and health behaviors: Social control as a dimension of social integration. Journal of health and social behavior. 1987:306–319. [PubMed] [Google Scholar]
- Vaccarino Viola, Parsons Lori, Every Nathan R, Barron Hal V, Krumholz Harlan M. Sex-based differences in early mortality after myocardial infarction. New England journal of medicine. 1999;341(4):217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- Venters Maurine, Jacobs David R, Jr, Pirie Phyllis, Luepker Russell V, Folsom Aaron R, Gillum Richard F. Marital status and cardiovascular risk: the Minnesota Heart Survey and the Minnesota Heart Health Program. Preventive medicine. 1986;15(6):591–605. doi: 10.1016/0091-7435(86)90064-2. [DOI] [PubMed] [Google Scholar]
- Waite Linda J. Does marriage matter? Demography. 1995;32(4):483–507. [PubMed] [Google Scholar]
- Welin Catharina, Lappas Georg, Wilhelmsen Lars. Independent importance of psychosocial factors for prognosis after myocardial infarction. Journal of Internal medicine. 2000;247(6):629–639. doi: 10.1046/j.1365-2796.2000.00694.x. [DOI] [PubMed] [Google Scholar]
- Williams Kristi, Umberson Debra. Marital status, marital transitions, and health: A gendered life course perspective. Journal of Health and Social Behavior. 2004;45(1):81–98. doi: 10.1177/002214650404500106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmoth Janet, Koso Gregor. Does marital history matter? Marital status and wealth outcomes among preretirement adults. Journal of Marriage and Family. 2002;64(1):254–268. [Google Scholar]
- Winship Christopher, Radbill Larry. Sampling weights and regression analysis. Sociological Methods & Research. 1994;23(2):230–257. [Google Scholar]
- Wu Zheng, Hart Randy. The effects of marital and nonmarital union transition on health. Journal of Marriage and Family. 2002;64(2):420–432. [Google Scholar]
- Zhang Zhenmei. Marital history and the burden of cardiovascular disease in midlife. The Gerontologist. 2006;46(2):266–270. doi: 10.1093/geront/46.2.266. [DOI] [PubMed] [Google Scholar]
- Zhang Zhenmei, Hayward Mark D. Gender, the marital life course, and cardiovascular disease in late midlife. Journal of Marriage and Family. 2006;68(3):639–657. [Google Scholar]
- Zick Cathleen D, Smith Ken R. Marital transitions, poverty, and gender differences in mortality. Journal of Marriage and the Family. 1991:327–336. [Google Scholar]
- Zuvekas Samuel H, Taliaferro Gregg S. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996–1999. Health Affairs. 2003;22(2):139–153. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]