Abstract
We report a rare case of osteochondritis dissecans involving the fourth proximal interphalangeal joint in a young Japanese drummer. We treated it successfully with the removal of loose body and drilling of the donor site.
Keywords: Osteochondritis dissecans, Fingers, Cumulative trauma disorders, Drum performer
Introduction
Osteochondritis dissecans can develop in young persons involved in activities that apply loading stress to their joints. It causes pain due to the associated loose body and/or secondary osteoarthritis. Ito et al. [1] reported that the distribution of osteochondritis dissecans in elbows, knees, hips, and feet was 57%, 30%, 8%, and 2%, respectively. There are only a few case reports of osteochondritis dissecans in the fingers.[1–6]
Here, we report a rare case of osteochondritis dissecans that developed in the proximal interphalangeal (PIP) joint of the fourth finger of a Japanese drummer.
Case report
An 18-year-old male reported a 6-month history of pain and swelling in the right fourth PIP joint during and after playing the Japanese drum. He denied any acute trauma. It had been his habit to practice the instrument >2 h every day from the age of 12 years. Physical examination showed swelling and tenderness of the radial side of the right fourth PIP joint. Disability scoring of the arm, shoulder, and hand (DASH) revealed 0.9 points in the disability/symptom section and 81.3 points in the sports/music section.
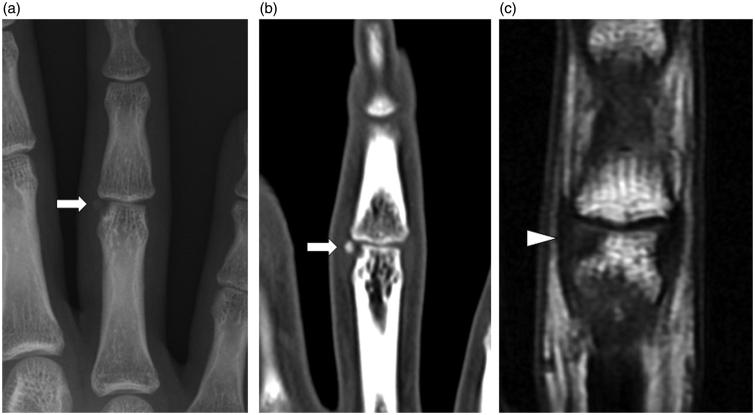
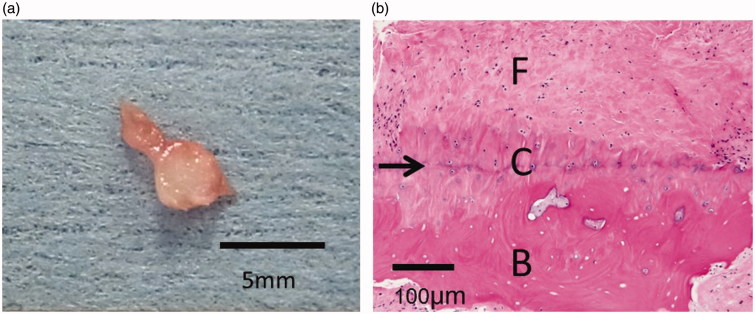
Plain X-ray and computed tomography (CT) images showed a bone defect with a tiny adjacent fragment at the radial side of the head of the fourth right proximal phalanx (Figure 1(a),(b)). T1-weighted magnetic resonance imaging (MRI) of the hand showed low signal in the fourth proximal phalangeal head without an associated radial collateral ligament tear. From these findings, we diagnosed osteochondral dissecans (Figure 1(c)), with the fragment representing a loose body. Conservative treatment with oral analgesics and rest was not successful, so we undertook surgical treatment. At operation, we identified a defect in the articular cartilage of the phalangeal head measuring approximately 7 mm2 and an adjacent loose body adherent to the joint capsule. We resected the loose body and performed drilling of the defect. The resected loose body was approximately 2.5 mm in diameter (Figure 2(a)). Pathological findings of the loose body showed osteochondral tissue covered by fibrous tissue. Pathological diagnosis was a loose body of osteochondritis dissecans (Figure 3(b)). The patient was able to return to drum practice 1 month after the operation and was pain-free at 6 months. DASH scores in both disability/symptoms and sports/music were 0 point. A follow-up plain X-ray showed no evidence of the loose body and no evidence of osteoarthritis.
Figure 1.
Plain x-ray, computed tomography (CT), and magnetic resonance imaging (MRI) of the right fourth finger. (a) Plain X-ray, (b) coronal CT section, (c) T1-weighted MRI image. Plain X-ray and CT images show a bone defect on the radial side of the head of the proximal phalanx and a fragment (white arrows). MRI image shows an osteochondral lesion without associated radial collateral ligament tear (white triangle).
Figure 2.
Macro- and microscopic findings of the loose body. (a) Extracted loose body (approximately 2.5 mm in diameter) with synovial tissue. (b) Histological findings of the loose body, which consists of cartilage with a tide mark (black arrow) separating it from bone tissue. The surface of the cartilage is covered with fibrous tissue (F: fibrous tissue, C: cartilage tissue, B: bone tissue).
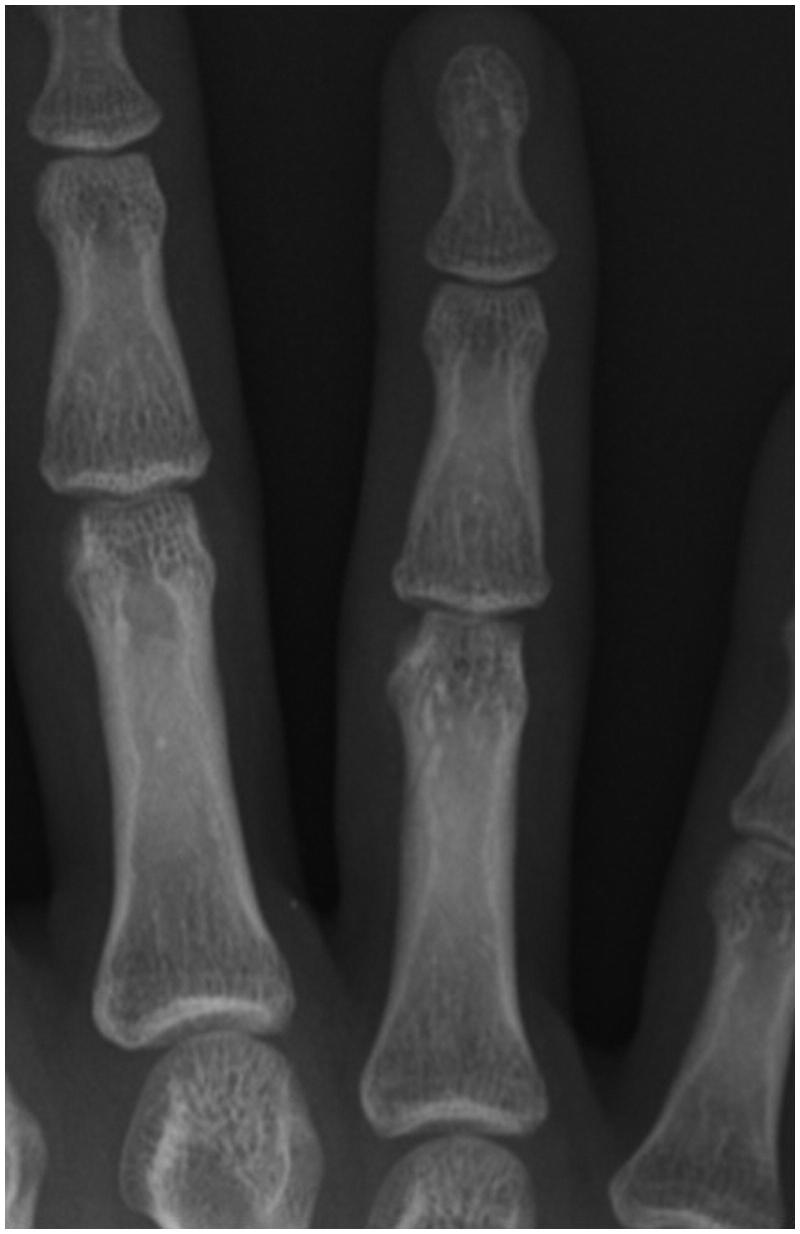
Figure 3.
Plain X-rays of the right fourth finger at final examination 6 months after surgery. The loose body is no longer visible, and there is no evidence of osteoarthritis.
Discussion
To the best of our knowledge, only seven cases of osteochondritis dissecans in the fingers have been reported. Three cases occurred in patients with brachydactyly,[2,5] while four others were in adolescents and were assumed to have developed due to external forces or a blood circulation disorder related to occupation or sports.[1,4,6] These previous cases occurred in the MP joints and thumb IP joint. The present case is the first report of osteochondritis dissecans developing in a PIP joint.
Although the pathogenesis of osteochondritis dissecans is not completely understood, several mechanisms have been suggested, including inhibition of bone union due to recurrent external forces after a subchondral trabecular fracture, necrosis due to a blood circulation disorder caused by repeated microtrauma and genetic predisposition.[7] In our case, because the proximal end of the drumstick exerted continuous pressure against his right fourth finger during drum performance, we considered that repeated microtrauma to the joint was the likely cause.
In general, treatment of osteochondritis dissecans of the elbow or knee depends on the stage of the disease. In the early stage, in the absence of loose bodies, conservative treatment such as temporarily refraining from sports activities and, in the case of the lower extremities, partial- or non-weight-bearing is effective. In the unstable and terminal stages, surgical treatment such as fixation or resection of the loose body, osteochondral autograft, autologous chondrocyte implantation, or drilling of the defect is performed. Due to its rarity, the treatment for osteochondritis dissecans in a finger has not been completely elucidated. Conservative treatment for the early stage of this disease in the fingers has not been reported. In the previous reports, surgical treatment was performed, typically by extraction of the loose body,[2,3,6] although one operator performed loose body removal followed by autologous bone grafting.[1] Both removal and grafting were separately reported to relieve symptoms. In our case, we combined the extraction of the loose body with drilling of the cartilage defect. Kim et al. [8] compared drilling with autologous bone cartilage grafting of the osteochondral defect in the great toe following the extraction of loose bodies. They reported that the symptoms improved with either treatment when the osteochondral defect was small.
We report a rare case of osteochondritis dissecans in the fourth PIP joint in the finger of a Japanese drummer. Orthopaedists should include osteochondritis dissecans in the differential diagnosis in young patients complaining of joint pain with swelling in the finger. Examination by not only plain X-ray but also MRI may enable diagnosis in the early phase of osteochondral dissecans before formation of a loose body and will distinguish osteochondral lesions from avulsion fractures.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Ito Y, Fujio K, Yanase Y. Osteochondritis dissecans of the metacarpal head; a case report. Cent Jpn J Orthop Traumat. 2003;46:1155–6. [Google Scholar]
- Andren L, Carstam N, Linden B. Osteochondritis dissecans and brachymesophalangia: a hereditary syndrome. J Hand Surg Am. 1978;3:117–22. doi: 10.1016/s0363-5023(78)80058-6. [DOI] [PubMed] [Google Scholar]
- Allan B, Joseph W. Osteochondritis dissecans of an interphalangeal joint. US Armed Forces Med J. 1951;2:883–6. [PubMed] [Google Scholar]
- Barrueco JL, Zapatero M. Osteochondritis dissecans of the head of the second metacarpal bone. J Hand Surg Am. 1992;17:1079–81. doi: 10.1016/s0363-5023(09)91066-8. [DOI] [PubMed] [Google Scholar]
- Renton P, Hallett JP. Abnormal metacarpal heads in brachymesophalangy – report of a case and review of the literature. J Hand Surg Am. 1981;6:545–9. doi: 10.1016/s0363-5023(81)80126-8. [DOI] [PubMed] [Google Scholar]
- Iwata S, Taniguchi Y, Ishimoto Y, Kitano T, Yoshida M. Osteochondritis in the metacarpophalangeal joint of a Japanese kendo player. Clinical Orthop Surg. 2004;39:757–60. [Google Scholar]
- Yoshizu T. Osteochondritis dissecans. Orthop surg. 1986;37:101–11. [Google Scholar]
- Kim YS, Park EH, Lee HJ, Koh YG, Lee JW. Clinical comparison of the osteochondral autograft transfer system and subchondral drilling in osteochondral defects of the first metatarsal head. Am J Sports Med. 2012;40:1824–33. doi: 10.1177/0363546512449292. [DOI] [PubMed] [Google Scholar]