Abstract
Introduction
Osteonecrosis of femoral head (ONFH) leads to hip osteoarthritis (HOA); among joint preserving treatments (JPT), the role of core decompression (CD) is still debated. We assessed the efficacy of CD compared with all other JPT in delaying the natural osteonecrosis evolution to HOA.
Sources of data
Following the PRISMA checklist, the Medline and Scopus databases were searched. Fifteen- to 70-year-old subjects with ONFH with a minimum follow-up of 24 months were considered. The outcomes evaluated were patient clinical status, radiographic progression and total hip arthroplasty (THA) or further surgery (FS) need. Risk ratio (RR) was calculated for every outcome reported. RCT, CCT and prospective studies were included.
Areas of agreement
A total of 12 studies (776 patients) met the inclusion criteria. Clinical outcome (RR = 1.14; 95% CI 0.58–2.32; P = 0.05), radiographic progression (RR = 1.64; 95% CI 1.14–2.35; P = 0.05) and the need for THA/FS (RR = 1.52; 95% CI 0.95–2.45; P = 0.05) suggested a slight superiority of other JPT compared with CD.
Areas of controversy
High heterogeneity of the primary investigations was the main limitation of our study.
Growing points
The efficacy and effectiveness of core decompression for ONFH are, at best, no better than other joint preserving strategies. The more recent scientific evidence seems to suggest that such procedure is less successful than other joint preserving strategies.
Areas timely for developing research
Further studies are needed to identify the best therapeutic approach to the ONFH.
Keywords: osteonecrosis, femoral head, hip osteoarthritis, joint preserving treatments, core decompression
Introduction
Osteonecrosis of femoral head (ONFH) affects above all males in the fifth decade, leading to osteochondral collapse and premature hip osteoarthritis (HOA).1–3 A well-timed diagnosis is required to perform ‘joint-preserving’ treatments (JPT), finalized to delay as much as possible total hip arthroplasty (THA). Both conservative (biophysical stimulation such as pulsed electromagnetic field,4–6 extracorporeal shock waves therapy7–9) and surgical approaches (core decompression,10–14 osteotomies,15,16 not vascularized17 and vascularized bone grafting18–20) are widely described.
Forage biopsy or simple core decompression (CD) was introduced ∼50 years ago in the diagnosis and management of early stages of the condition, to prevent progression of ONFH. The results of CD are debated and controversial.18,21–24 Recently, a study24 considered several medical and surgical options in ONFH management and underlined the difficulty in identifying the optimal treatment modality. Trying to settle controversies on CD rising from apparently conflicting studies, we performed a meta-analysis of the pertinent literature. We evaluated CD in the treatment of ONFH, comparing it with all other JPTs in delaying the natural progression of the condition.
Methods
This meta-analysis was designed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Eligibility criteria
To be included in our meta-analysis, a study had to meet the following criteria: comparison of CD (with or without bone grafting) versus any other kind of JPT (either conservative or surgical) in a population with ONFH, aged from 15 to 70 years old; reporting at least one of the following outcomes: (i) clinical, through scores and questionnaires like Harris and/or Merle d'Aubigné’ Hip Score, ARCO system, etc.; (ii) radiographic, in relation to the femoral head collapse or eventual transfer from a stage to another of the disease and (iii) surgical, such as need of further surgery (FS) or THA; minimum follow-up of 24 months; randomized clinical trials (RCTs), controlled clinical trials (CCTs) and observational cohort prospective studies, in English and French.
Data sources and search
A comprehensive electronic search of the current literature was performed by Medline and Scopus databases, from the earliest records through May 22, 2015. Additional studies were identified by checking the bibliographies of the articles selected. Reviews and retrospective studies were excluded. If full texts were not available, authors were contacted. Key words used to identify studies were ‘necrosis femoral decompression’, ‘osteonecrosis femoral decompression’, ‘necrosis hip decompression’, ‘osteonecrosis hip decompression’, ‘necrosis femoral forage’, ‘osteonecrosis femoral forage’, ‘necrosis hip forage’ and ‘osteonecrosis hip forage’ on both search engines.
Study selection
All results were managed through Endnote. Duplicates were deleted, and then studies without abstract were excluded. All titles and abstracts were screened by two reviewers (A.B. and S.R.) at different places and times, according to a previously defined protocol. After applying exclusion criteria, eligible studies for meta-analysis were selected. Disagreements were solved through discussion and consensus. If disagreement remained, a senior reviewer was consulted (F.S.) and solved it through discussion and consensus with other two reviewers.
Outcomes including hip function, radiographic progression and THA/FS of the hip were also abstracted. Per each selected article, we followed the criteria of failure or success used in the article itself. If results were indicated as Improved, Unchanged and Worse, we considered Improved and Unchanged as Success and Worse as Failure. When results were indicated in per cent, rounding down (<0.5) or up (>0.5) was applied. We excluded Stage 0 patients where possible.
Risk of bias in individual studies
The methodological quality of each study was assessed using the Downs and Black checklist.25
Summary measures and synthesis of results
Effect size computed for the analyses was risk ratio (RR) with 95% confidence intervals (CI). The significance level for the overall estimates of effect was set at P < 0.05. A meta-analysis for each outcome was performed. Heterogeneity among studies was assessed through Cochrane's Q index and the Higgins' I 2 statistic. When the Q index was P < 0.05 and I 2 statistic did not exceed 50%, we selected the fixed-effects model; otherwise, the random-effects model was adopted. All analyses were performed using STATA statistical software package (Version 14.0, StataCorp, 2015).
Risk of bias across studies and additional analyses
Publication bias was assessed using plots of study results against precision of the study (metafunnel command) for each outcome. Symmetry of the funnel plots was tested using the Egger linear regression method and the Begg and Mazumdar rank correlation method (metabias command). A sensitivity analysis was carried out by excluding one trial at a time from pooled effects to weigh up the relative influence of each individual study on the pooled effect size (metainf module).
Meta-regression analyses (metareg module) were conducted to assess whether conclusions were sensitive to restricting studies to subgroups that might modify the effect size, including as covariates study publication year, sample size and overall study quality (Downs and Black checklist), each separately. For all meta-regression analyses, a random-effects model was used.
Furthermore, a subgroup analysis for the different stages of the condition was performed.
The three outcome results were presented dividing simple CDs (CD) and CD followed by non-vascularized bone grafting (CDBG), so as to highlight differences between the two subgroups.
Results
Characteristics of studies included
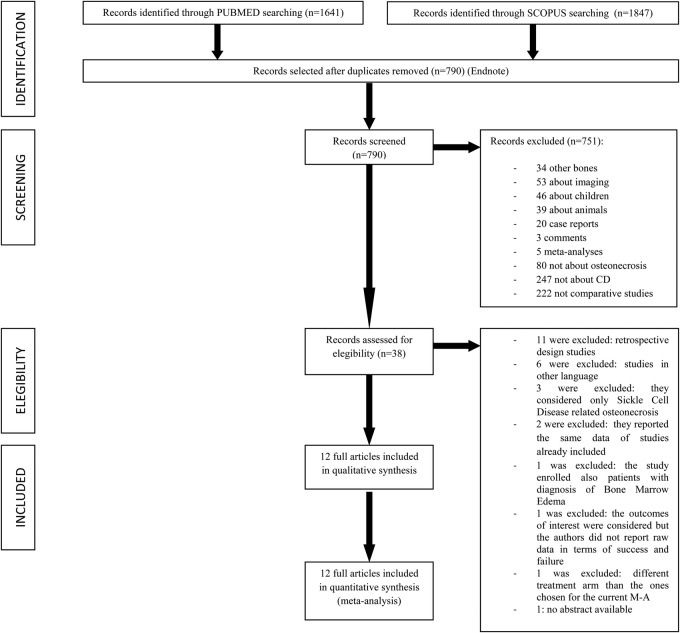
The whole studies selection process is summarized through the flow chart in Figure 1. Seven hundred and ninety works were screened. Twelve studies were considered eligible and were included in the meta-analysis.4,9,19,21,26–33 There were five RCTs, two prospective randomized studies, four prospective cohort studies and a CCT. CD was compared in three studies with bone marrow nuclear cell grafting, in two studies with conservative approach based on non-weight-bearing and analgesics, in two study with electrical stimulation, in one study with vascularized fibular grafting, in one study with extracorporeal shock wave therapy, in one with magnetic field therapy, in one with autologous bone marrow buffy coat grafting and in another one with an additional oral supplementation of alendronate. The main features of each study are listed in Table 1. Studies quality assessment according to Downs and Black checklist is given in Table 2. The 12 studies included 776 patients and contained data relevant for the outcomes assessment criteria stated above (Table 3).
Fig. 1.
Meta-analysis flow chart.
Table 1.
Studies included and main features
| N | Author (year) | Study design | Groups compared |
Years | No. of patients |
No. of hips |
Mean age (SD) |
Classification system | Follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CD (Group A) | Control (Group B) | M | F | Total | CD | Control | Total | CD | Control | ||||||
| 1 | Biltau N. (2008) | CCT | 3 mm trephine through the femoral neck into the necrotic region in the femoral head, 2–3 mm away from the cartilage | With BMNC 400 ml of bone marrow obtained from anterior iliac crest, with a mean final volume of 50 ml, about 29.0 ± 2.2% of lymphocytes, 4 ± 1% of monocytes and 6.0 ± 1.3% myeloid precursors, injected through and placed into the necrotic zone |
– | 7 | 6 | 13 | 8 | 10 | 18 | – | – | ARCO I 2 ARCO II 16 |
3, 6, 12, 24 months |
| 2 | Ganji V. (2011) | Prospective cohort study | 3 mm trephine, till 2 or 3 mm from joint cartilage | With BMNC 400 ml of bone marrow obtained from anterior iliac crest, with a mean final volume of 51 ml, about 2.0 × 109 precursors (1% CD34), injected through and placed into the necrotic zone |
– | 9 | 10 | 19 | 11 | 13 | 24 | 45.7 (2.8) | 42.2 (2.6) | ARCO I A:2 B:2 ARCO II A:9 B:11 |
3, 6, 12, 24, 36, 48, 60 months |
| 3 | Kane S.M. (1996) | Prospective case-series study | CD (Hungerford technique) | VFG (Urbaniak technique) 16 mm channel through the femoral neck, into the necrotic portion of the femoral head; the avascular portion of the femoral head was excised; local bone graft from the greater trochanter was packed in the peripheral dehrided portions of the femoral head; a vascularized fibula was then harvested from the ipsilateral central fibula and placed in the central portian of the femoral bead defect; the lateral femoral circumflex artery and vein were microsurgically anastomosed with the peroneal vessels of the graft |
1987 1991 |
25 | 9 | 34 | 19 | 20 | 39 | 42 (26–48) | Ficat IIA A:7 B:4 Ficat IIB A:7 B:4 Ficat III A:5 B:12 |
6,12 months, yearly after | |
| 4 | Kang P. (2011) | RCT | Multiple drilling as described by Kim (2004) and Mont (2004); all the patients received 500–1000 mg calcium and 400–800 UI vitamin D3 each day | With systemic ALE oral alendronate 10 mg per day or 70 mg once per week for 24 weeks, beginning the day after operation |
2002 2005 |
75 | 47 | 93 | 52 | 55 | 107 | 45.3 (22–55) | 43.8 (21–52) | Ficat mod IIA A:15 B:17 Ficat mod IIB A:24 B:25 Ficat mod III A:13 B:13 |
>48 m mean A:62 m mean B:63 m |
| 5 | Koo K. H. (1995) | RCT | Steinberg technique (1984) using a 9.5 mm trephine; the proximal deep part of tunnel was filled with the distal part of the core (of normal cancellous bone from the trochanteric area) | Conservative non-weight bearing with crutches and intermittent use of analgesics |
1990 1992 |
31 | 2 | 33 | 18 | 19 | 37 | 47 (18–68) | Steinberg I A:10 B:12 Steinberg II A:7 B:4 Steinberg III A:1 B:3 |
Every 3 months | |
| 6 | Ma Y. (2014) | RCT | A 10-mm diameter trephine was placed into the mid-line of the trochanter and driven toward the necrotic site, 2–3 mm away from the cartilage A cylinder of bone from the femoral neck and head was obtained and used for bone marrow grafting. The necrotic tissue in the femoral head was removed by using the bone curette. The bone graft was inserted into the necrotic region through the trephine | With BBC the pelvic bone was punctured from the superior posterior iliac spine with the bone marrow aspiration needle. A 50-ml heparinized syringe was connected to the bone marrow aspiration needle and used to harvest the bone marrow The BBC containing enriched bone marrow cells was collected by a sterilized transfer pipette and carefully loaded onto the porous cylindrical bone drop by drop (∼3 × 109 nucleated cells). The bone graft was inserted into the necrotic region through the trephine |
2009 2010 |
28 (H) | 11 (H) | 43 | 24 | 25 | 49 | 34.78 (11.48) | 35.60 (8.05) | Ficat I: A:4 B:3 Ficat II: A:15 B:17 Ficat III: A:5 B:5 |
3, 24 months |
| 7 | Steinberg M.E. (1989) | Prospective randomized study | 8 mm Michele trephine, to remove two cores of bone; the first was put aside to be used as a graft; two additional cores of bone were removed using a 5 mm or 6 mm Michele trephine (going lateral and medial to the central core); additional grafting material was placed at the opening in the lateral femoral cortex | With ES the cathode wire from an Osteostim or an Orthofuse constant, direct current electrical stimulator was coiled longitudinally about the graft and held in place with absorbable sutures. The cathode wire was connected to the power source which was implanted subcutaneously on the lateral aspect of the thigh |
– | – | – | – | 42 | 74 | 116 | – | – | Steinberg 0–IV |
From 24 to 96 months mean A: 33 m mean B: 44 m |
| 8 | Steinberg M.E. (1990) | RCT | Decompression and grafting procedure; the patients wore capacitive coupling units, that consisted of two self-adhering electrodes attached anteriorly and posteriorly to the skin over the femoral head; the portable power unit was suspended from a belt worn around the waist Units inactive |
Decompression and grafting procedure; the patients wore capacitive coupling units, which consisted of two self-adhering electrodes attached anteriorly and posteriorly to the skin over the femoral head; the portable power unit was suspended from a belt worn around the waist. Units active |
– | 30 | 10 | 40 | 20 | 20 | 40 | – | – | Stage I A:4 B:3 Stage II A:16 B:16 Stage III A:0 B:1 |
2–4 years (31 m mean) |
| 9 | Stulberg B.N. (1991) | Prospective randomized study | Drilling of the femoral head after intraosseous venography | Conservative restricted program of non-weight bearing with a walker or axillary crutches for a minimum of 6 weeks until symptoms subsided at the clinical examination were normal; a program of progressive weight bearing with decreasing support was tailored according to the patients' symptoms |
1983 1987 |
– | – | 36 | 29 | 23 | 52 | 38.6 (15–65) | Ficat 0: 3 Ficat I: 15 A:10 B:5 Ficat II:14 A:7 B:7 Ficat III: 21 A:11 B:10 |
3,6,12 months mean 26,8 m means Ficat I: 25 m Ficat II:26 m Ficat III:30 m |
|
| 10 | Wang C.J. (2012) | Prospective cohort study | 10 mm channel; cancellous bone grafts were harvested from the anterior iliac crest and cancellous bone chips were packed into the defect; a cortical fibular strut allograft was fashioned and sized, inserted into the bone channel to maintain the cancellous bone grafts | ESW 6000 impulses of shockwaves at 28 KV (equivalent to 0.474 mJ/mm² energy flux density) in a single session |
2001 2002 |
43 | 5 | 48 | 28 | 29 | 57 | – | – | ARCO I A:2 B:3 ARCO II A:17 B:10 ARCO III A:9 B:16 |
6,12 months, then yearly for 8–9 years |
| 11 | Windish C. (2014) | Prospective cohort study | Curettage, autologous bone grafting (autograft) from the greater trochanter and proximal femur using a 8 mm hollow—core drill | With ‘Magnetodyn®’ the treatment consisted of an external magnetic field coil and an invasive bipolar induction screw system |
2003 2005 |
26 | 9 | 35 | 18 | 22 | 40 | 42.5 (33–54) | 41.2 (33–54) | ARCO II A:13 B:18 ARCO III A:5 B:4 |
12 months |
| 12 | Zhao D. (2012) | RCT | A decompression tunnel was made using a trephine through the trochanter and femoral neck into the necrotic region in the femoral head, 2–3 mm away from the cartilage | With BMNC the subtrochanteric bone marrow-derived BMMSCs were subjected to proliferation in vitro for 2 weeks, after which ∼2 × 106 BMMSCs were harvested and prepared in 2 ml normal saline solution later injected into the osteonecrotic site in the femoral head |
2004 2006 |
46 | 47 | 93 | 44 | 53 | 97 | 33.8 32.7 (7.7) | 32.7 (10.5) | ARCO I A:2a B:3a ARCO II A:49a B:50a |
6, 12, 24, 60 months |
CCT, control clinical trial; RCT, randomized clinical trial; CD, core decompression; BMNC, autologous bone marrow mononuclear cells; VFG, vascularized fibular grafting; ALE, alendronate; BBC, bone marrow buffy coat; ES, electrical stimulation; ESW, extracorporeal shock waves.
aThe authors did not report data after the lost of 7 hips at follow-ups.
Table 2.
Methodological quality of each study assessed by the Downs and Black checklist
| Author (year) | Reporting (11 points) | External validity (3 points) | Internal validity—bias (7 points) | Internal validity—confounding (6 points) | Power (5 points) | Total score |
|---|---|---|---|---|---|---|
| Biltau N. (2008) | 7 | 1 | 5 | 0 | 4 | 17 |
| Gangji V. (2011) | 9 | 1 | 7 | 2 | 5 | 24 |
| Kane S.M. (1996) | 9 | 1 | 3 | 0 | 5 | 18 |
| Kang P. (2011) | 10 | 1 | 5 | 3 | 5 | 24 |
| Koo K.H. (1995) | 5 | 1 | 5 | 3 | 5 | 19 |
| Ma Y. (2014) | 10 | 3 | 7 | 6 | 5 | 31 |
| Steinberg M.E. (1989) | 3 | 1 | 2 | 2 | 5 | 13 |
| Steinberg M.E. (1990) | 6 | 0 | 6 | 5 | 5 | 22 |
| Stulberg B.N. (1991) | 5 | 1 | 5 | 2 | 5 | 18 |
| Wang C.J. (2012) | 11 | 3 | 5 | 3 | 5 | 27 |
| Windish C. (2014) | 6 | 0 | 5 | 2 | 5 | 18 |
| Zhao D. (2012) | 9 | 2 | 5 | 5 | 5 | 26 |
Table 3.
Outcomes evaluable for each study
| Author (year) | Study groups | Outcomes |
||
|---|---|---|---|---|
| Clinical (scores) | Radiographic (progression) | Surgical (THA or FS) | ||
| Biltau N. (2008) | CD vs. BMNC | − | + | + |
| Gangji V. (2011) | CD vs. BMNC | − | + | + |
| Kane S.M. (1996) | CD vs. VFG | − | − | + |
| Kang P. (2011) | CD(MD) vs. Ale | + | + | + |
| Koo K.H. (1995) | CDBG vs. Cons | + | + | + |
| Ma Y. (2014) | CDBG vs. BBC | − | + | + |
| Steinberg M.E. (1989) | CDBG vs. ES | + | + | + |
| Steinberg M.E. (1990) | CDBG vs. capacitive coupling | + | + | + |
| Stulberg B.N. (1991) | CD vs. Cons | + | + | + |
| Wang C.J. (2012) | CDBG vs. ESWT | + | − | + |
| Windish C. (2014) | CDBG vs. magnetic field | − | − | + |
| Zhao D. (2012) | CD vs. BMNC | − | − | + |
For acronyms, see Table 3.
Outcome analysis
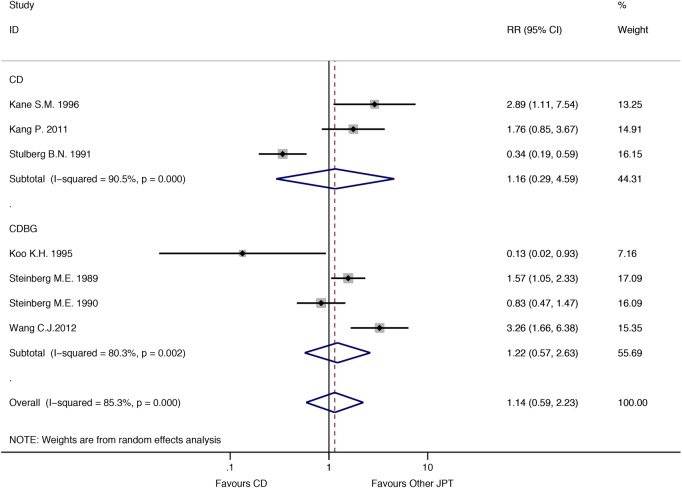
Seven studies were included for the clinical outcome analysis (425 patients followed). The success rate for the patients treated using CD and by all other JPT were 54% (108/200) and 63.1% (142/225), respectively. A random-effects model analysis (I 2 = 85.3%; P < 0.01) revealed a slight superiority of JPT group in clinical improvement compared with the CD group (RR = 1.14; 95% CI 0.58–2.32; P = 0.05). The difference between the two groups was not statistically significant, even considering separately the CD group and CDBG group (Fig. 2). After re-estimating the meta-analysis omitting each study in turn, results did not change significantly.
Fig. 2.
RR estimate of clinical outcome in CD groups compared with other JPT group. Grey squares represent relative risks (RRs) in trials. The 95% confidence intervals (CIs) for individual trials are denoted by lines and those for the pooled RRs by open diamonds. Meta-analysis is performed by random-effects model. CD, core decompression; CDBG, core decompression and bone grafting; JPT, joint preserving treatments.
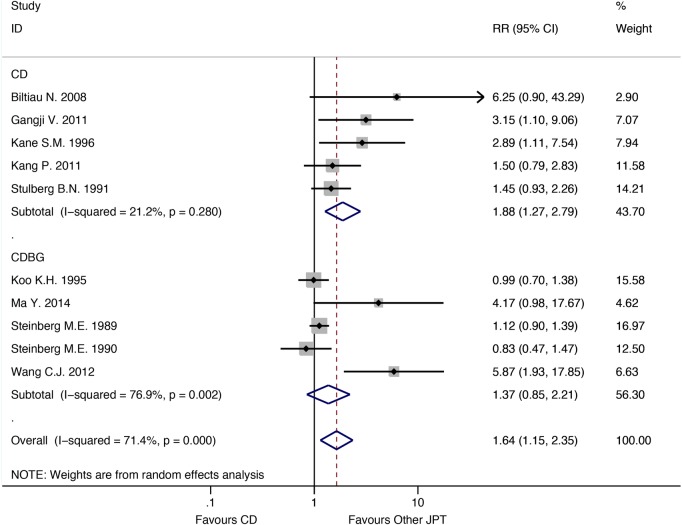
Ten studies were considered for the radiographic progression analysis (539 subjects followed). For CD-treated patients, the success rate was 42.2% (106/251); for those treated by other JPT, it was 59.7% (172/288). The random-effects model analysis of data (I 2= 71.4%; P < 0.01) also showed better results for patients treated by other JPT than for those treated by CD (RR = 1.64; 95% CI 1.14–2.35; P = 0.05), displaying a statistically significant difference (Fig. 3). No single study influenced significantly the pooled estimate.
Fig. 3.
RR estimate of radiographic outcome in CD groups compared with other JPT group. Grey squares represent relative risks (RRs) in trials. The 95% confidence intervals (CIs) for individual trials are denoted by lines and those for the pooled RRs by open diamonds. Meta-analysis is performed by random-effects model. Abbreviations as in Figure 2.
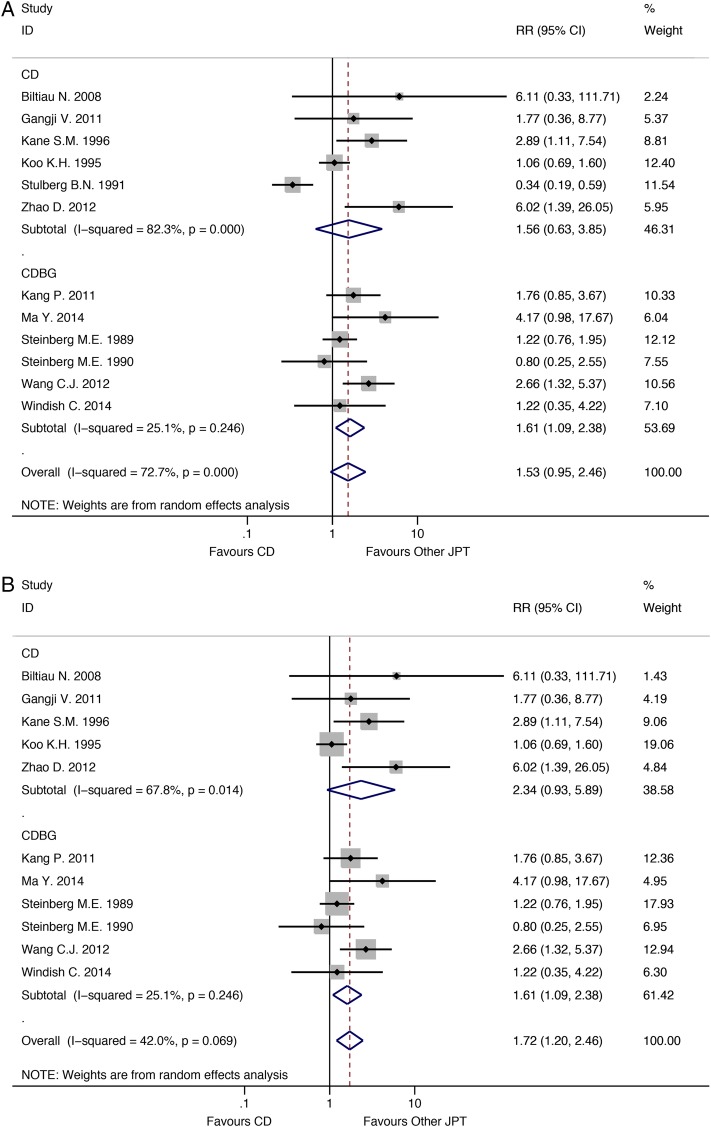
Finally, THA/FS need was investigated, including seven studies and 776 patients. The success rate for patients treated by CD and by other JPT was 63.2% (198/313) and 73.8% (268/363), respectively. The random-effects model analysis (I 2= 72.7%; P < 0.01) suggested even from a surgical point of view the slight superiority of other JPT compared with CD, but the difference was not in a (RR = 1.52; 95% CI 0.95–2.45; P = 0.05) (Fig. 4A). The one study removed analysis showed that the work by Stulberg et al. 27 influenced strongly the summary effect estimate; after its removal, the RR resulted statistically significant (RR = 1.72; 95% CI 1.20–2.46; P = 0.05), and the heterogeneity was significantly reduced (I 2 = 42%; P = 0.069) (Fig. 4B).
Fig. 4.
(A) RR estimate of surgical outcome in CD groups compared with other JPT group. Grey squares represent relative risks (RRs) in trials. The 95% confidence intervals (CIs) for individual trials are denoted by lines and those for the pooled RRs by open diamonds. Meta-analysis is performed by random-effects model. Abbreviations as in Figure 2. (B) RR estimate of surgical outcome in CD groups compared with other JPT group after Stulberg's study removal. Grey squares represent relative risks (RRs) in trials. The 95% confidence intervals (CIs) for individual trials are denoted by lines and those for the pooled RRs by open diamonds. Meta-analysis is performed by random-effects model. Abbreviations as in Figure 2.
Meta-regression analysis
Meta-regression analysis showed no relationship between the year of publication, the quality of the study, the sample size and the three single outcomes. Interestingly, a borderline correlation was found between the year of publication and the radiographic (P = 0.076, Fig. 5A) and surgical outcomes (P = 0.056, Fig. 5B).
Fig. 5.
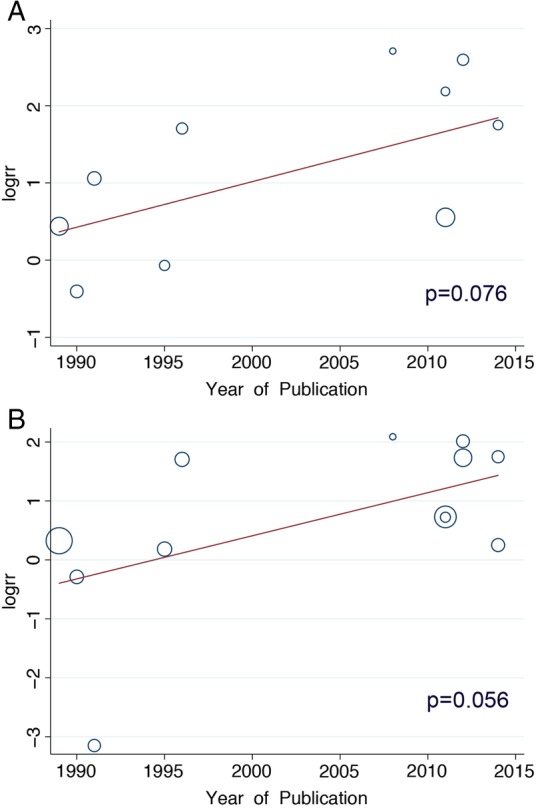
(A) Metaregression analysis between the radiographic outcome and the year of publication. (B) Metaregression analysis between the surgical outcome and the year of publication.
Subgroup analysis
Regarding the classification method, 5 of the 12 studies used the ARCO classification system, 4 the Ficat classification system and 3 the Steinberg classification system. Given the multiplicity of the classification methods in the different studies, a simple comparison between them was not possible. Furthermore, only 5 of the 12 selected studies19,21,27,30,33 at follow-up reported data for each stage of the condition, but without considering all the outcomes selected (2 studies reported data on clinical outcome, 2 on radiographic outcome and 4 on surgical one outcome) (Table 4). With this in mind, to detect differences in outcome between the different stages of OFNH, we analysed data of patients in whom different classification methods were used, considering them comparable according to the following common criteria: Stage I if there were no radiographic findings (abnormalities only on magnetic resonance images); Stage II when sclerosis and cysts formation were visualized on radiographs; Stage III when there was evidence of a subchondral fracture and Stage IV when osteoarthritis was evident.
Table 4.
Classification methods and outcomes evaluable for subgroup analysis
| Author (year) | Study groups | Classification system | Possibility to be included in a subgroup analysis | Motivation | Outcomes evaluable |
|---|---|---|---|---|---|
| Biltau N. (2008) | CD vs. BMNC | ARCO | − | No specific data for Stage I and II progression to Stage III | |
| Gangji V. (2011) | CD vs. BMNC | ARCO | − | Progressing at follow-up to Stage III pooled for Stage I and Stage II disease | |
| Kane S.M. (1996) | CD vs. VFG | Ficat | + | –Surgical | |
| Kang P. (2011) | CD(MD) vs. Ale | Ficat | + | –Clinical –Surgical |
|
| Koo K.H. (1995) | CDBG vs. Cons | Steinberg | + | –Radiographic | |
| Ma Y. (2014) | CDBG vs. BBC | Ficat | − | Patients stage provided when enrolled in the study but not at outcome evaluation | |
| Steinberg M.E. (1989) | CDBG vs. ES | Steinberg | − | Patients stage provided when enrolled in the study but not at outcome evaluation | |
| Steinberg M.E. (1990) | CDBG vs. capacitive coupling | Steinberg | − | Patients stage provided when enrolled in the study but not at outcome evaluation | |
| Stulberg B.N. (1991) | CD vs. Cons | Ficat | + | –Clinical –Radiographic –Surgical |
|
| Wang C.J. (2012) | CDBG vs. ESWT | ARCO | − | Patients stage provided when enrolled in the study but not at outcome evaluation | |
| Windisch C. (2014) | CDBG vs. magnetic field | ARCO | + | –Surgical | |
| Zhao D. (2012) | CD vs. BMNC | ARCO | − | Patients stage provided when enrolled in the study but data not complete at outcome evaluation (lost at follow-up) |
For acronyms, refer Table 3.
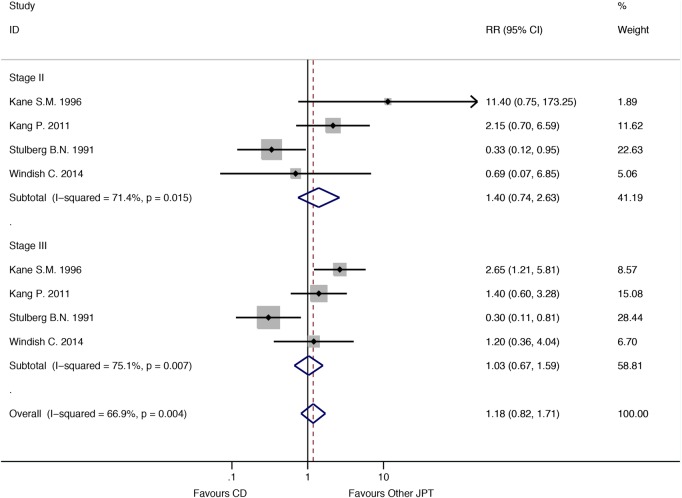
We conducted this sub-analysis on surgical outcome, for a total of 148 patients in Stage II (73 and 75 for the CD group and for the other JPT group, respectively) and 73 in Stage III (34 and 39 for the CD group and for the other JPT group, respectively). Only one study provided data on Stage I patients, and therefore, we did not consider them.
No difference in risk to undergo THA or further surgery was evident between CD and other JPT therapy, neither in Stage II (RR = 1.40; 95% CI 0.74–2.63; P = 0.050) nor in Stage III patients (RR = 1.03; 95% CI 0.67–1.59; P = 0.05). In both instances, a random-effects model analysis was performed given the high heterogeneity of primary studies (I 2 = 71.4%; P = 0.015 for Stage II and I 2 = 75.1%; P < 0.01 for Stage III sub-analysis) (Fig. 6).
Fig. 6.
RR estimate of surgical outcome in CD group compared with other JPT considering Stage II and Stage III patients separately. Grey squares represent relative risks (RRs) in trials. The 95% confidence intervals (CIs) for individual trials are denoted by lines and those for the pooled RRs by open diamonds. The meta-analysis was performed using a random-effects model. Abbreviations as in Figure 2.
Publication bias
No publication bias was detected for single outcome analysis.
Discussion
In the early 1960s, Arlet and Ficat proposed to investigate ischaemia and necrosis of bone by a ‘forage-biopsie’,34 and they introduced the core biopsy concept, later popularized by Hungerford as CD.35 CD soon became the reference technique for each other therapeutic proposal on the basis of highly gratifying and promising results. For many years, it has been considered highly cost-effective, minimally invasive and at low complication rate35,36 in preventing THA in early ONFH stages. Given its unpredictable medium- and long-term results, several other conservative JPT have been proposed in the last 30 years.
However, in relation to the natural evolution of ONFH,5 the 6-month non-weight-bearing approach is nowadays to consider unacceptable,21,27 while all different JPT seemed somewhat comparable among them.37
All studies considered here, analyzing the combination of CD with other techniques (bone marrow nuclear cells grafting, also with a buffy coat, vascularized fibular grafting, electrical stimulation, magnetic fields, alendronate supplementation) versus simple CD, showed a better impact on ONFH outcomes by the first group encountered, as also found by Rajagopal et al. 23 The only exception was represented by electrical stimulation through capacitive coupling units26 that, with surgical decompression, seemed to add nothing to simple CD. This result probably resulted from the type of electrical stimulation, since the same author had previously reported different results by another type of stimulation.4
Wang's et al. 9 study was the only one to compare CD with ESW therapy, demonstrating that this latter could be considered a good alternative to surgery. Actually, some other articles confirmed the effectiveness of ESW,37,38 but a systematic review on the topic8 highlighted that there are no controlled studies demonstrating the efficacy of ESW therapy in the treatment of ONFH. Thus, further research is required.
From our findings, CD is not superior to other JPT in the management of ONFH. In fact, in terms of both clinical evaluations and THA/FS need, there was no significant difference between CD and other approaches. Furthermore, examining the data on radiographic progression, other JPT seem statistically superior to CD. In addition to this, from the influence analysis performed, omitting Stulberg et al.'s27 study from the THA/FS data pool reduced the substantial heterogeneity among studies, demonstrating a clear significant difference in surgical outcome against CD. The borderline association between the year of publication and both the radiographic than the surgical outcome could be probably related to the availability and diffusion in the more recent years of more ‘modern’ treatment strategies, such as bone marrow nuclear cells grafting. Subgroup analysis showed no superiority of other JPT over simple CD in Stage II or III patients. This result would confirm that joint sparing treatments (either CD or other JPTs) in advanced ONFH, after subchondral collapse (Stage III), are not effective.
Reviewing the current literature, Rajagopal et al. 23 concluded that data on CD effectiveness are difficult to interpret and that there is no clear evidence that CD significantly improves clinical outcome. They finally suggested to consider also other treatment options in the early stage of ONFH. Similarly, in another systematic review, Mont et al. 39 underlined the variability in methodology and data reporting among the studies on this subject, precluding rigorous statistical analysis.
To date, only two meta-analyses on CD have been published. Castro and Barrack40 compared CD with conservative treatment only. Their investigation showed that CD was successful in no more that 23% of the cases when compared to conservative management in Steinberg Stage I. In accordance to our findings, CD was not as effective in Steinberg Stage II. Furthermore, more recently Li et al. 41 focused on CD and BMMC versus simple CD, demonstrating better outcomes in the combined approach group.
It could be hypothesized that exploring the pathophysiological mechanisms of ONFH, as recent studies are trying to do,42 could explain success and failure after CD or after combined techniques. We agree that applying a more selective approach to the use of CD and its variants only in selected ONFH cases, such as those presenting venous stasis without artery insufficiency, could produce higher success rates and reduce the rate of unsuccessful surgery and its related costs.
Study limitations
The current meta-analysis does not compare CD with another one specific technique, given the lack of adequate primary studies. So, we combined different studies in a single work, despite it is recognized as a common criticism of secondary studies.43 Comparative studies published at the moment and eligible for a meta-analysis on CD are few and heterogeneous, as already reported in a recent systematic review.42 In our sample, the main reasons of such heterogeneity are probably represented from a different study design; the use of different clinical scores; the assessment of ‘radiographic failure’, intended both as head collapse of >2 mm both as transition from a stage to the further; differences in terms of number of drillings and trephines diameter. All these differences are probably the result of general disagreement about the most effective way in performing CD and in selecting appropriate tools to assess success and failure. Furthermore, the majority of meta-analyses on orthopaedic surgery topics have methodological limitations;43 thus, we strictly followed PRISMA checklist to minimize methodological flaws.44
Given the data collected, the current meta-analysis suggests that CD is not superior with respect to other JPT in delaying THA or FS. Combining CD with other techniques seems to provide better outcomes in ONFH. Detecting venous stasis and artery insufficiency could be the key to select the right indications for this kind of surgery and to reduce failures. It would be desirable to consider again the necessity of a meta-analysis in the future and to compare RCTs, with a same control group and using the same classification system, to allow further sub-analyses in relation to disease stage and to length of follow up.
Authors’ contributions
F.S. (frasadil@unina.it): study concept and design, manuscript drafting and revision, statistical analysis and interpretation of data, study supervision. A.B. (alebernas@gmail.com): study concept and design, manuscript drafting, statistical analysis and interpretation of data. S.R. (serghiey@hotmail.com): study design, manuscript drafting. N.M. (n.maffulli@qmul.ac.uk): manuscript drafting and revision, study supervision. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. We acknowledge Dr Elisa Vitullo for her helpful advices and web search; Teresa Busiello MD Orthopaedist, Flavio Carbone MD Orthopaedist, Immacolata Cozzolino MD Cytologist, Vincenzo Franzese MD Orthopaedist, Patrizia Maiorano MD Specialist in Physical Medicine & Rehabilitation, and Gelsomina Mansueto MD Histologist, for their active part in the whole osteonecrosis project.
References
- 1.Merle D'Aubigné R, Postel M, Mazabraud A et al. Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg Br 1965;47:612–33. [PubMed] [Google Scholar]
- 2.Ohzono K, Saito M, Takaoka K et al. Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br 1991;73:68–72. [DOI] [PubMed] [Google Scholar]
- 3.Takatori Y, Kokubo T, Ninomiya S et al. Avascular necrosis of the femoral head. Natural history and magnetic resonance imaging. J Bone Joint Surg Br 1993;75:217–21. [DOI] [PubMed] [Google Scholar]
- 4.Steinberg ME, Brighton CT, Corces A et al. Osteonecrosis of the femoral head. Results of core decompression and grafting with and without electrical stimulation. Clin Orthop Relat Res 1989;249:199–208. [PubMed] [Google Scholar]
- 5.Bassett CA, Schink-Ascani M, Lewis SM. Effects of pulsed electromagnetic fields on Steinberg ratings of femoral head osteonecrosis. Clin Orthop Relat Res 1989;246:172–85. [PubMed] [Google Scholar]
- 6.Aaron RK, Lennox D, Bunce GE et al. The conservative treatment of osteonecrosis of the femoral head. A comparison of core decompression and pulsing electromagnetic fields. Clin Orthop Relat Res 1989;249:209–18. [PubMed] [Google Scholar]
- 7.Lin PC, Wang CJ, Yang KD et al. Extracorporeal shockwave treatment of osteonecrosis of the femoral head in systemic lupus erythematosis. J Arthroplasty 2006;21:911–5. [DOI] [PubMed] [Google Scholar]
- 8.Alves EM, Angrisani AT, Santiago MB. The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: a systematic review. Clin Rheumatol 2009;28:1247–51. [DOI] [PubMed] [Google Scholar]
- 9.Wang CJ, Huang CC, Wang JW et al. Long-term results of extracorporeal shockwave therapy and core decompression in osteonecrosis of the femoral head with eight- to nine-year follow-up. Biomed J 2012;35:481–5. [DOI] [PubMed] [Google Scholar]
- 10.Fairbank AC, Bhatia D, Jinnah RH et al. Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br 1995;77:42–9. [PubMed] [Google Scholar]
- 11.Smith SW, Fehring TK, Griffin WL et al. Core decompression of the osteonecrotic femoral head. J Bone Joint Surg Am 1995;77:674–80. [DOI] [PubMed] [Google Scholar]
- 12.Markel DC, Miskovsky C, Sculco TP et al. Core decompression for osteonecrosis of the femoral head. Clin Orthop Relat Res 1996;323:226–33. [DOI] [PubMed] [Google Scholar]
- 13.Mont MA, Carbone JJ, Fairbank AC. Core decompression versus nonoperative management for osteonecrosis of the hip. Clin Orthop Relat Res 1996;324:169–78. [DOI] [PubMed] [Google Scholar]
- 14.Mont MA, Fairbank AC, Petri M et al. Core decompression for osteonecrosis of the femoral head in systemic lupus erythematosus. Clin Orthop Relat Res 1997;334:91–7. [PubMed] [Google Scholar]
- 15.Scher MA, Jakim I. Intertrochanteric osteotomy and autogenous bone-grafting for avascular necrosis of the femoral head. J Bone Joint Surg Am 1993;75:1119–33. [DOI] [PubMed] [Google Scholar]
- 16.Sugioka Y, Hotokebuchi T, Tsutsui H. Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head. Indications and long-term results. Clin Orthop Relat Res 1992;277:111–20. [PubMed] [Google Scholar]
- 17.Buckley PD, Gearen PF, Petty RW. Structural bone-grafting for early atraumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 1991;73:1357–64. [PubMed] [Google Scholar]
- 18.Mont MA, Carbone JJ, Fairbank AC. Preventing collapse in early osteonecrosis of the femoral head. A randomised clinical trial of core decompression. Clin Orthop Relat Res 1995;77:870–4. [PubMed] [Google Scholar]
- 19.Kane SM, Ward WA, Jordan LC et al. Vascularized fibular grafting compared with core decompression in the treatment of femoral head osteonecrosis. Orthopedics 1996;19:869–72. [DOI] [PubMed] [Google Scholar]
- 20.Ali SA, Christy JM, Griesser MJ et al. Treatment of avascular necrosis of the femoral head utilising free vascularised fibular graft: a systematic review. Hip Int 2014;24:5–13. [DOI] [PubMed] [Google Scholar]
- 21.Koo KH, Kim R, Ko GH et al. Preventing collapse in early osteonecrosis of the femoral head. A randomised clinical trial of core decompression. J Bone Joint Surg Br 1995;77:870–4. [PubMed] [Google Scholar]
- 22.McGrory BJ, York SC, Iorio R et al. Current practices of AAHKS members in the treatment of adult osteonecrosis of the femoral head. J Bone Joint Surg Am 2007;89:1194–204. [DOI] [PubMed] [Google Scholar]
- 23.Rajagopal M, Balch Samora J, Ellis TJ. Efficacy of core decompression as treatment for osteonecrosis of the hip: a systematic review. Hip Int 2012;22:489–93. [DOI] [PubMed] [Google Scholar]
- 24.Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg 2014;22:455–64. [DOI] [PubMed] [Google Scholar]
- 25.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Commun Health 1998;52:377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steinberg ME, Brighton CT, Bands RE et al. Capacitive coupling as an adjunctive treatment for avascular necrosis. Clin Orthop Relat Res 1990;261:11–8. [PubMed] [Google Scholar]
- 27.Stulberg BN, Davis AW, Bauer TW et al. Osteonecrosis of the femoral head. A prospective randomized treatment protocol. Clin Orthop Relat Res 1991;268:140–51. [PubMed] [Google Scholar]
- 28.Biltiau N, Hauzeur JP, Toungouz M et al. Traitement de l'ostéonécrose de la tête fémorale par implantation de moelle autologue = Stem cell therapy for osteonecrosis of the femoral head. Revue médicale de Bruxelles 2008;29:26–30. [Google Scholar]
- 29.Gangji V, De Maertelaer V, Hauzeur JP. Autologous bone marrow cell implantation in the treatment of non-traumatic osteonecrosis of the femoral head: five year follow-up of a prospective controlled study. Bone 2011;49:1005–9. [DOI] [PubMed] [Google Scholar]
- 30.Kang P, Pei F, Shen B et al. Are the results of multiple drilling and alendronate for osteonecrosis of the femoral head better than those of multiple drilling? A pilot study. Joint Bone Spine 2012;79:67–72. [DOI] [PubMed] [Google Scholar]
- 31.Zhao D, Cui D, Wang B et al. Treatment of early stage osteonecrosis of the femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal stem cells. Bone 2012;50:325–30. [DOI] [PubMed] [Google Scholar]
- 32.Ma Y, Wang T, Liao J et al. Efficacy of autologous bone marrow buffy coat grafting combined with core decompression in patients with avascular necrosis of femoral head: a prospective, double-blinded, randomized, controlled study. Stem Cell Res Ther 2014;5:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Windisch C, Kolb W, Röhner E et al. Invasive electromagnetic field treatment in osteonecrosis of the femoral head: a prospective cohort study. Open Orthop J 2014;8:125–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ficat RP, Arlet J. Forage-biopsie de la tete femorale dans I'osteonecrose primitive. Observations histo-pathologiques portant sur huit forages. Rev Rhum 1964;31:257–64. [Google Scholar]
- 35.Marker DR, Seyler TM, Ulrich SD et al. Do modern techniques improve core decompression outcomes for hip osteonecrosis. Clin Orthop Relat Res 2008;466:1093–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tran TN, Warwas S, Haversath M et al. Experimental and computational studies on the femoral fracture risk for advanced core decompression. Clin Biomech (Bristol, Avon) 2014;29:412–7. [DOI] [PubMed] [Google Scholar]
- 37.Kong FR, Liang YJ, Qin SG et al. Clinical application of extracorporeal shock wave to repair and reconstruct osseous tissue framework in the treatment of avascular necrosis of the femoral head (ANFH). Zhongguo Gu Shang 2010;23:12–5. [PubMed] [Google Scholar]
- 38.Vulpiani MC, Vetrano M, Trischitta D et al. Extracorporeal shock wave therapy in early osteonecrosis of the femoral head: prospective clinical study with long-term follow-up. Arch Orthop Trauma Surg 2012;132:499–508. [DOI] [PubMed] [Google Scholar]
- 39.Mont MA, Zywiel MG, Marker DR et al. The natural history of untreated asymptomatic osteonecrosis of the femoral head: a systematic literature review. J Bone Joint Surg Am 2010;92:2165–70. [DOI] [PubMed] [Google Scholar]
- 40.Castro FP Jr, Barrack RL. Core decompression and conservative treatment for avascular necrosis of femoral head: a meta-analysis. Am J Orthop 2000;29:187–94. [PubMed] [Google Scholar]
- 41.Li X, Xu X, Wu W. Comparison of bone marrow mesenchymal stem cells and core decompression in treatment of osteonecrosis of the femoral head: a meta-analysis. Int J Clin Exp Pathol 2014;7:5024–30. [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao DW, Yu XB. Core decompression treatment of early-stage osteonecrosis of femoral head resulted from venous stasis or artery blood supply insufficiency. J Surg Res 2015;194:614–21. [DOI] [PubMed] [Google Scholar]
- 43.Bhandari M, Morrow F, Kulkarni AV et al. Meta-analyses in orthopaedic surgery. A systematic review of their methodologies. J Bone Joint Surg Am 2001;83:15–24. [PubMed] [Google Scholar]
- 44.Dijkman BG, Abouali JA, Kooistra BW et al. Twenty years of meta-analyses in orthopaedic surgery: has quality kept up with quantity. J Bone Joint Surg Am 2010;92:48–57. [DOI] [PubMed] [Google Scholar]
- 45.Hungerford DS. Bone marrow pressure, venography and core decompression in ischemic necrosis of the femoral head. In: The Hip: proceedings of the seventh open scientific meeting of The Hip Society, 1979, pp.218–37. CV Mosby, St Louis. [Google Scholar]